Abstract
Background
We developed an augmented reality (AR)-based portable navigation system in which the surgeon can view the pelvic plane and placement angle of an acetabular cup on the display of a smartphone during THA.
Questions/purposes
(1) Is acetabular component placement more accurate using the AR-based portable navigation system compared with the conventional freehand technique? (2) Is intraoperative measurement of placement angle more accurate when using the AR-based portable navigation system compared with a goniometer?
Methods
Forty-six patients were randomly assigned to undergo acetabular cup placement during THA using the AR-based portable navigation system (AR navigation group) or placement of a mechanical alignment guide (conventional group). All surgeries were performed with the patient in the lateral decubitus position. We compared the absolute value of the difference between the targeted placement angle and postoperative measured placement angle between the groups using two types of imaging (radiography and CT).
Results
In terms of radiographic inclination, the mean differences between the targeted placement angle and postoperative measured angle were smaller in the AR navigation group than in the conventional group for both radiographs and CT images (2.3° ± 1.4° versus 3.9° ± 2.4°, respectively; p = 0.009 and 1.9° ± 1.3° versus 3.4° ± 2.6°, respectively; p = 0.02). There were no differences in radiographic anteversion between the two groups. No complications were associated with the use of the AR-based portable navigation system.
Conclusions
This system yielded no differences in acetabular anteversion accuracy, and no clinically important differences in acetabular inclination. Therefore, at this time we cannot recommend this device as its costs and risks cannot be justified based on the absence of a clinically meaningful difference in cup placement accuracy. Although we detected no complications, this was a small series, and this approach adds both surgical time and pins in the ilium.
Level of Evidence
Level I, therapeutic study.
Introduction
The inaccuracy of typical methods for aligning acetabular components during THA remains a clinical problem [9]. There have been many reports that inaccuracies of acetabular components cause intra- and extra-articular impingements, ROM restriction, joint instability, and polyethylene wear [5].
Although several investigators have attempted to address the inaccuracy of acetabular component placement with use of intraoperative radiograph [6], fluoroscopy [3], and computer-assisted navigation systems [7, 15] the solutions proposed have substantial limitations, including X-ray exposure to the patient and personnel, lack of accuracy due to parallax or operator error with fluoroscopy, cost, or change in pelvis position during the operation. Therefore, we developed a novel system for cup placement using augmented reality (AR), which uses a camera to superimpose computer-generated images or information on real-world images, and which has recently been used in the field of orthopaedic surgery [4,12,13]. In our system, the surgeon can view an image of an acetabular cup superimposed on the real surgical field during THA, and determine the placement angle of the acetabular cup through the smartphone display. Once we achieved a level of acceptable dependability and ease of use in the lab that made it reasonable for daily use, we tested our system in clinical practice.
We therefore asked: (1) Is acetabular component placement more accurate using the AR-based portable navigation system compared with the conventional freehand technique? (2) Is intraoperative measurement of placement angle more accurate when using the AR-based portable navigation system compared with a goniometer?
Patients and Methods
This was a two-arm, parallel-group, assessor-blinded randomized controlled trial with 1:1 treatment allocation conducted in two hospitals with adult hip reconstruction departments in Tokyo, Japan. The study was approved by the local ethics committees of both hospitals. All participants provided written informed consent after receiving an explanation of the procedures, radiological studies, follow-up schedules, and possible risks of the study. The research was performed in compliance with the Declaration of Helsinki. The study was registered with the University Hospital Medical Information Network (Registration Number UMIN000031602).
Study Participants
The inclusion criteria for participation in this study were patients aged 20 years or older at the time of providing consent and THA performed by a single surgeon (HO). The surgeon performed surgeries in both hospitals during the study period. No exclusion criteria were set, ensuring that the results of the study could be readily generalized to the wider population.
Recruitment and Randomization of Participants
Between April and December 2018, we performed THA in 48 surgeries. All patients were approached to participate in the study, and 46 provided consent to participation. Of these 46 initially enrolled, 41 completed the study (Fig. 1). There were no substantial differences between the patients who were included in the study and those who were not (Table 1). We created a randomization sequence with permuted block randomization, with a block size of 4 and 1:1 allocation that was generated using R software (The R Foundation for Statistical Computing, Vienna, Austria). After confirming the patients’ eligibility and obtaining consent, we randomly assigned them to undergo acetabular cup placement using either the AR-based portable navigation system or mechanical alignment guide during THA.
Fig. 1.

This flow diagram illustrates patient enrollment, randomization, and analysis for this study.
Table 1.
Patient demographics and baseline clinical characteristics
Blinding of the surgical team was not possible because of the nature of the intervention. The two investigators (KK, ST) who performed the postoperative radiographic measurements were blinded to treatment allocation throughout the study.
AR-based Portable Navigation System
AR is defined as an interactive experience of a real-world environment where the objects that reside in the real-world are augmented by computer-generated perceptual information; in the surgical field, this information usually consists of radiological data or images and is reflected on the monitor through the camera. Currently, there are roughly two types of AR. The first is marker-based AR, wherein a camera captures the position and tilt of a pattern, referred to as a marker that overlaps the three-dimensional (3-D) image. The second type is marker-less AR in which the camera captures the approximate shape of the target space upon which the image is overlaid. In this study, we used marker-based AR, which is the most common and accurate of the various types of AR available [1]. The basic mechanism of marker-based AR is the same as that of the conventional infrared optical navigation system. First, relative coordinates from a camera are created. Then, a 3-D model is displayed after recognition by the camera markers. Although infrared optical navigation systems use infrared irradiation to recognize reflective balls or infrared lights with infrared cameras [14], AR uses visible light to recognize patterns, called markers, with ordinary cameras.
The actual procedure during the study was as follows. First, with the patient in the supine position, we disinfected the skin surrounding the iliac crest. Then, we inserted two 2.0-mm pins into the iliac crest in parallel using a guide with the guide marker (Fig. 2). A pelvis marker with a large marker in the center was placed manually at three points, that is, the right and left anterior superior iliac spine and pubic symphysis, and it came to the anterior pelvic plane (APP) [11].
Fig. 2.
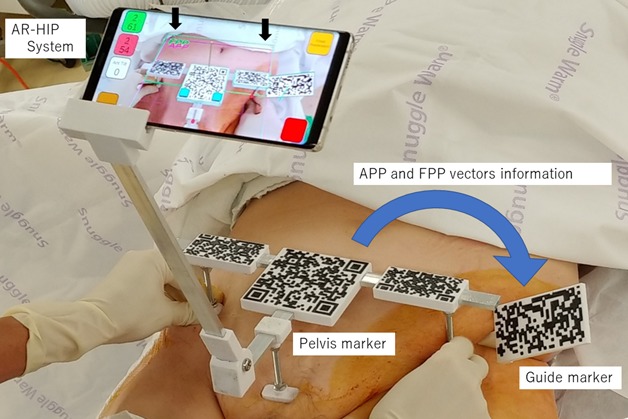
The anterior pelvic plane (APP) and functional pelvic plane (FPP) coordinates were acquired with the patient in the supine position. A guide marker with two 2-mm pins was placed at the iliac crest. The pelvis markers were placed at the right and left anterior iliac spine and pubic symphysis. The AR system acquired APP and FPP coordinates by recognizing the pelvis marker, and it copied their information to the guide marker (blue arrow). The APP and FPP were superimposed on the surgical field on the display of a smartphone.
In the AR function, the direction vectors of the marker could be acquired by recognizing the marker. In addition, gravitational vectors could be obtained from the gyro sensor built into the smartphone. Using these vectors, normal and direction vectors of the functional pelvic plane (FPP) could be calculated (Fig. 3). By recognizing the guide marker and the pelvis marker simultaneously, we copied the FPP vector information from the pelvis marker to the guide marker (Fig. 2). After copying, the pelvis marker became unnecessary, and this system could use the FPP vector information with only the guide marker.
Fig. 3.

A-B (A) Each vector of the APP and (B) FPP and the gravitational vector are shown here. The vector  is the direction vector from R (right anterior superior iliac spine) to L (left anterior superior iliac spine). The vector
is the direction vector from R (right anterior superior iliac spine) to L (left anterior superior iliac spine). The vector  is the direction vector from R to P (pubic symphysis). The vector
is the direction vector from R to P (pubic symphysis). The vector  is the gravitational vector. The vector
is the gravitational vector. The vector  is defined as the normal vector of APP and is calculated with the cross product of
is defined as the normal vector of APP and is calculated with the cross product of  and
and  . The vector
. The vector  is defined as the cross product of
is defined as the cross product of  and
and  and it is perpendicular to both
and it is perpendicular to both  and
and  . The vector
. The vector  is defined as the normal vector of FPP and is calculated with the cross product of
is defined as the normal vector of FPP and is calculated with the cross product of  and
and  .
.
Second, the patient’s operative position could be changed to the surgeon’s preferred position. In this study, we investigated the accuracy of the AR-based portable navigation system with patients in the lateral decubitus position. Therefore, the patient’s position was changed to the lateral decubitus position.
Third, after sterilizing the operating field, a sterilized guide marker and cup handle marker were prepared in the operating field (Fig. 4). We inserted a smartphone into a sterilized smartphone case. The radiographic inclination and anteversion [10] of the acetabular cup at the FPP were calculated with the direction vector of the cup handle obtained from the handle marker and each vector of the FPP (Fig. 5) and could be observed on the display of the smartphone in real time. Finally, we installed and measured the acetabular component according to the angles displayed on the smartphone (Fig. 6). This application was developed using the Unity and Vuforia SDK software (Unity Technologies, San Francisco, CA, USA).
Fig. 4.

The AR-based portable navigation system during THA (left hip in the lateral decubitus position) is shown. The assistant held the smartphone, which recognized the handle and pelvis markers. The surgeon placed the acetabular cup according to the AR-based portable navigation system.
Fig. 5.

(A) Each vector of the FPP and the cup handle and (B) the top-down view of the FPP. The vector  is the direction vector of the cup handle. The angle of radiographic anteversion is calculated with the inner product of
is the direction vector of the cup handle. The angle of radiographic anteversion is calculated with the inner product of  and
and  . The angle of radiographic inclination is calculated with the cross product of
. The angle of radiographic inclination is calculated with the cross product of  and
and  and the inner product of
and the inner product of  and this cross product.
and this cross product.
Fig. 6.
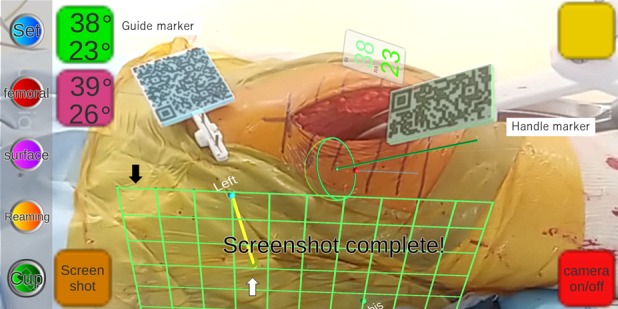
This is a screenshot of the image in Fig. 4. The surgeon can see the placement angle of the acetabular cup, images of the FPP, and direction of gravity on the smartphone display in real time. The black arrow indicates the FPP image. The white arrow indicates the direction of gravity, which enabled the surgeon to determine the pelvic tilt or rotation.
Surgical Planning
We obtained preoperative and postoperative CT images as a standard practice. Three-dimensional templating software (ZedHip; LEXI, Tokyo, Japan) using CT images was used for preoperative planning and postoperative measurement of acetabular component angles. The horizontal plane of the CT table during preoperative CT with the patient in the supine position was defined as the FPP [11]. We initially set the targeted acetabular component placement angle as a radiographic inclination of 40° and a radiographic anteversion of 15° or 20° relative to the FPP and according to the shape of each patient’s acetabulum to avoid anterior protrusion of the cup rim [10].
Surgery
All surgeries were performed by a single surgeon (HO) with the patient under general anesthesia. The modified Watson-Jones approach in the lateral decubitus position was routinely used as the surgical approach. Before skin incision for THA, we obtained the APP and FPP coordinates using the AR-based portable navigation system. After preparing the femur, the surgeon placed the acetabular cup during surgery. An uncemented acetabular cup was used in all patients.
Interventions
The study treatments involved acetabular cup placement using the AR-based portable navigation system and acetabular cup placement using the conventional freehand technique with a mechanical alignment guide (Fig. 7). Before the operation, the same preoperative assessment process was followed for all patients. Other perioperative procedures were the same for all patients.
Fig. 7.

The conventional technique during THA (left hip in the lateral decubitus position) is shown. We used an alignment rod designed for 40° radiographic inclination and 15° or 20° radiographic anteversion.
In patients allocated to the AR navigation group, acetabular components were placed at the targeted placement angle using the AR-based portable navigation system. In patients allocated to the conventional group, acetabular components were placed at the targeted placement angle using a mechanical alignment guide. For the conventional group, two 2.0-mm pins were inserted into the pelvis immediately before skin incision for THA, and the AR-based portable navigation system was only used for intraoperative measurement of the acetabular cup angle after acetabular component placement. In both groups, after placement of the acetabular components, a surgical assistant measured the placement angles using AR-based portable navigation and a goniometer (Fig. 8). After surgery, all pins and markers were removed in both groups. Their pin holes were so small that no special stitching was required.
Fig. 8.

Measurement of acetabular component angles using a goniometer during THA (left hip in the lateral decubitus position) is shown. The assistant held the goniometer and measured the angle of the cup introducer.
Outcomes
Immediately after surgery, we measured the placement angle of the acetabular cup with radiography, and measured it again at 3 months with CT according to the radiographic definition [10]. To determine inclination and anteversion of the acetabular cup, we used 2-D template software (Kyocera Medical, Osaka, Japan) for radiography and 3-D template software (ZedHip; LEXI) for CT. We used the FPP as the reference plane of measurement. Postoperative measurements for each patient were performed twice by two investigators (KK, ST), and the mean value was taken as the postoperative measurement.
In radiograph measurements, the intraclass correlation coefficients (ICCs) between the two observers were 0.85 (95% CI 0.69 to 0.93) in radiographic inclination and 0.78 (95% CI 0.57 to 0.90) in radiographic anteversion. In CT measurements, the ICCs between the two observers were 0.88 (95% CI 0.77 to 0.93) in radiographic inclination and 0.79 (95% CI 0.64 to 0.89) in radiographic anteversion.
First, we investigated the accuracy of acetabular cup placement using the AR-based portable navigation system. We compared the absolute value of the difference between the targeted placement angle and postoperatively measured placement angle between the AR navigation group (n = 22) and the conventional group (n = 19).
Second, we assessed the accuracy of the intraoperative measurement angle using the AR-based portable navigation system. Among 41 patients, we compared the absolute value of the difference between the intraoperative placement angle measured using the AR-based portable navigation system and the postoperative measured angle and absolute value of the difference between the intraoperative placement angle measured using a goniometer and the postoperative measured angle.
Statistical Analysis
The enrollment of 16 patients per group was estimated to provide a power of 80% to detect a between-group difference of 2.0° in acetabular placement angle with a type I error rate of 5%. Based on the results of our pilot study [12], we used an SD of 2.0° for the difference between the targeted angle and measured angle. To compare the accuracy of the acetabular cup placement angle between patients allocated to the AR navigation group and those allocated to the mechanical alignment guide group, the differences in the mean absolute difference of the placement angle and 95% CIs were calculated using the t-test. To assess the accuracy of the AR-based portable navigation system as an intraoperative measurement device, we compared the difference between the intraoperative measured angle of the acetabular cup using AR-based portable navigation and postoperative measured angle using radiographic tests. We also compared the intraoperative measured angle of the acetabular cup using a goniometer and postoperative measured angle using radiographic tests with the t-test. Outcomes and baseline demographic characteristics were compared using the t-test for continuous variables and the chi-square test for categorical variables. A two-sided p < 0.05 was considered statistically significant. To test interobserver reliability, two assessors (KK, ST) calculated the ICCs of postoperative measurements of the cup placement angle. All statistical analyses were performed using R software.
Results
We found no clinically important differences in acetabular component placement using the AR-based portable navigation system compared with the conventional freehand technique. The mean absolute values of the differences between the targeted placement angles and measured placement angles in the AR navigation group versus the conventional group using CT and X-ray were: 1.9° (SD 1.3° [95% CI 1.3 to 2.5] versus 3.4°(SD 2.5° [95% CI 2.1 to 4.6]; p = 0.02) and 2.3° (SD 1.4° [95% CI 1.7 to 2.9] versus 3.9° (SD 2.4° [95% CI 2.8 to 5.1]; p = 0.009) in inclination and 2.8° (SD 2.2° [95% CI 1.9 to 3.8] versus 3.8° (SD 3.0° [95% CI 2.4 to 5.3]); p = 0.22) and 2.3 (SD 1.8° [95% CI 1.5 to 3.1] versus 2.9 (SD 2.2° [95% CI 1.8 to 4.0]; p = 0.34) in anteversion (Table 2).
Table 2.
The absolute values of difference between targeted angles of acetabular cup orientation and postoperative measurement angle using radiographs and CT scan.
We found no clinically important differences in the intraoperative measurement of the placement angle when using the AR-based portable navigation system compared with a goniometer. The absolute values of the differences between intraoperative measurement angles using the AR-based portable navigation system and goniometer and postoperative measurement angles determined with CT and radiographs were 2.0° (SD 1.5° [95% CI 1.5 to 2.5] versus 3.1° (SD 2.3° [95% CI 2.4 to 3.9]; p = 0.009) and 2.9° (SD 2.1° [95% CI 2.2 to 3.5] versus 3.5° (SD 2.2° [95% CI 2.8 to 4.2]; p = 0.19) in inclination and 2.9° (SD 2.0° [95% CI 2.3 to 3.5] versus 7.5° (SD 3.6° [95% CI 6.4 to 8.6]; p = 0.001) and 2.5 (SD 2.1° [95% CI 1.8 to 3.2] versus 5.3 (SD 3.2° [95% CI 4.3 to 6.4]; p = 0.001) in anteversion (Table 3).
Table 3.
The absolute value of difference between the intraoperative measurement angles using AR-based portable navigation system and goniometer and postoperative measurement angles
Although there were no complications, such as infections or fractures, in either group during the study period. Two patients complained about their pin scar in terms of esthetics. None complained about pain, numbness, or discomfort.
Discussion
Aligning the acetabular components during THA is the critical factor for preventing intra- and extraarticular impingements, ROM restriction, joint instability, and polyethylene wear. Although several investigators have attempted to address the inaccuracy of acetabular component placement, the solutions proposed to date have substantial limitations. To resolve this problem, we developed a novel system for cup placement using augmented reality. Here, we investigated the accuracy of the AR-based portable navigation system compared with a goniometer. However, the results indicated that this system yielded no difference in acetabular anteversion accuracy and no clinically important difference in acetabular inclination.
This study had some limitations. First, we examined only measurement of angles on images. There were no clinical data, and there may have been issues such as pin site irritation, infection, and fracture related to the technique that would not be an issue with conventional techniques. Second, it is unclear whether CT data obtained in the supine position can be reliably translated into surgical data when the patient is placed in a lateral decubitus position. Third, a single surgeon performed all the operations in this study, which did not allow evaluation of variability between surgeons. Fourth, in this study, surgery was performed only in the lateral decubitus position, although this system could also be used with the patient in the supine position. In the lateral position, although it was possible that the accuracy may change due to the movement of pins or guide marker with position changes, in this study, we could not evaluate the differences due to position change. Further studies are needed to address these issues. Finally, we did not report on clinical outcomes but confined our study to radiographic findings.
Our new AR-based portable navigation system yielded no differences in acetabular anteversion accuracy, and no clinically important differences in acetabular inclination. Our navigation did not improve the anteversion of the acetabular component due to the relative high accuracy of the conventional technique. Minoda et al. [9] reported that the accuracy of the conventional technique evaluated by radiograph examination was 5.2° ± 3.9° in inclination and 5.3° ± 4.0° in anteversion. Jolles et al. [7] reported that the accuracy was 4.0° in inclination and 8.0° in anteversion. In this study, the accuracy of our conventional technique was 3.9° ± 2.4° and 2.9° ± 2.2°, which was apparently higher than in other reports. We assumed that this was a limitation of a study with a single surgeon, as mentioned above. In addition, routine preoperative CT for surgical planning in both AR and conventional groups may have affected the better accuracy of acetabular cup placement compared with previous studies [7,9]. Recently, Bohl et al. [2] reported that computer navigation is associated with reductions in the proportions of dislocation and acetabular component revision after primary THA in a multicenter cohort study. However, they did not distinguish between navigation types and did not discuss the accuracy of each navigation. Therefore, it is still unclear which type of navigation contributed to their results, and it is not possible to determine which type of navigation would show clinical improvement. There have been several reports regarding the accuracy of each navigation system. For example, the angles determined using 2-D and 3-D matched navigation were 2.5° ± 2.2° for inclination and 2.3° ± 1.7° for anteversion [16], and the angles determined with CT-based navigation were 1.5° ± 1.3° for inclination and 2.1° ± 1.8° for anteversion [15]. Although they showed better accuracy, there were no clinical improvements in these reports due to the sample size. We did not compare our system with these previous studies, so it is not clear whether our system has equivalent or inferior accuracy. The sample size in this randomized controlled trial was so small that it was underpowered to assess the clinical effects or complications like these reports.
In conclusion, we developed a new AR-based portable navigation system for THA. This system showed no differences in acetabular anteversion accuracy and no clinically important differences in acetabular inclination. Therefore, at this time, we cannot recommend this device because its costs and risks cannot be justified based on the absence of a clinically meaningful difference in cup placement accuracy. Although we detected no complications, this series was small, and this approach adds both surgical time and pins in the ilium, which added costs and risks. Further studies are needed to evaluate these complications and to determine which clinically relevant advantages are provided to justify its continued use in THA.
Acknowledgments
We thank Yoshiharu Yonekawa and Maiko Yagishita for their contributions as study coordinators for the duration of the study period.
Footnotes
Each author certifies that neither he nor she, nor any member of his or her immediate family, has funding or commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Houksuikai Kinen Hospital, Ibaraki, Japan.
References
- 1.Ankita G, Kriti B, Kritika G, Manu V. Comparative study of marker-based and marker-less indoor navigation in augmented reality. International Research Journal of Engineering and Technology. 2018;5:3569-3572. [Google Scholar]
- 2.Bohl DD, Nolte MT, Ong K, Lau E, Calkins TE, Della Valle CJ. Computer-Assisted Navigation Is Associated with Reductions in the Rates of Dislocation and Acetabular Component Revision Following Primary Total Hip Arthroplasty. J Bone Joint Surg Am . 2019;101(3):250-256. [DOI] [PubMed] [Google Scholar]
- 3.Christopher R, Blake E, Julia R, James L, Brett D. The use of fluoroscopy during direct anterior hip arthroplasty: powerful or misleading? J Arthroplasty . 2018;33:1775-1779. [DOI] [PubMed] [Google Scholar]
- 4.Cho HS, Park MS, Gupta S, Han I, Kim HS, Choi H, Hong J. Can augmented reality be helpful in pelvic bone cancer surgery? An In Vitro Study. Clin Orthop Relat Res. 2018;476:1719-1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.D'Lima DD, Urquhart AG, Buehler KO, Walker RH, Colwell CW., Jr The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Joint Surg Am. 2000;82:315-321. [DOI] [PubMed] [Google Scholar]
- 6.Ezzet KA, McCauley JC. Use of intraoperative X-rays to optimize component position and leg length during total hip arthroplasty. J Arthroplasty. 2014;29:580-585 [DOI] [PubMed] [Google Scholar]
- 7.Jolles BM, Genoud P, Hoffmeyer P. Computer-assisted cup placement techniques in total hip arthroplasty improve accuracy of placement. Clin Orthop Relat Res. 2004;426:174-179. [DOI] [PubMed] [Google Scholar]
- 8.Joshua S, Mark J, Jeremy T, Michael J, Adam J. Does intraoperative fluoroscopy improve limb-length discrepancy and acetabular component positioning during direct anterior total hip arthroplasty? J Arthroplasty . 2018;33:2927-2931. [DOI] [PubMed] [Google Scholar]
- 9.Minoda Y, Kadowaki T, Kim M. Acetabular component orientation in 834 total hip arthroplasties using a manual technique. Clin Orthop Relat Res. 2006;445:186-191. [DOI] [PubMed] [Google Scholar]
- 10.Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75:228-232. [DOI] [PubMed] [Google Scholar]
- 11.Nishihara S, Sugano N, Nishii T, Ohzono K, Yoshikawa H. Measurements of pelvic flexion angle using three-dimensional computed tomography. Clin Orthop Relat Res. 2003;411:140-151. [DOI] [PubMed] [Google Scholar]
- 12.Ogawa H, Hasegawa S, Tsukada S, Matsubara M. A pilot study of augmented reality technology applied to the acetabular cup placement during total hip arthroplasty. J Arthroplasty. 2018;33:1833-1837. [DOI] [PubMed] [Google Scholar]
- 13.Ponce BA, Jennings JK, Clay TB, May MB, Huisingh C, Sheppard ED. Telementoring: use of augmented reality in orthopaedic education. J Bone Joint Surg Am. 2014;96:84. [DOI] [PubMed] [Google Scholar]
- 14.Sugano N. Computer-assisted orthopaedic surgery and robotic surgery in total hip arthroplasty. Clin Orthop Surg . 2013;5:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tsutsui T, Goto T, Wada K, Takasago T, Hamada D, Sairyo K. Efficacy of a computed tomography-based navigation system for placement of the acetabular component in total hip arthroplasty for developmental dysplasia of the hip. J Orthop Surg (Hong Kong) . 2017;25:1-7. [DOI] [PubMed] [Google Scholar]
- 16.Yamada K, Endo H, Tetsunaga T, Miyake T, Sanki T, Ozaki T. Accuracy of cup positioning with the computed tomography-based two-dimensional to three-dimensional matched navigation system: a prospective, randomized controlled study. J Arthroplasty. 2018;33:136-143. [DOI] [PubMed] [Google Scholar]





