Abstract
Background
Reverse shoulder arthroplasty has been proven to improve function in shoulders with cuff-tear arthropathy, but existing studies are primarily single-center studies with a small number of patients, which limits their ability to identify patients who have an increased risk of revision or a worse functional outcome.
Questions/purposes
(1) What is the estimated 10-year cumulative revision rate after reverse shoulder arthroplasty for cuff-tear arthropathy, and what factors are associated with the risk of revision? (2) What is the patient-reported outcome 1 year after surgery, and what factors are associated with a worse patient-reported outcome?
Methods
We included all patients treated with reverse shoulder arthroplasty for cuff-tear arthropathy reported in the Danish Shoulder Arthroplasty Registry from 2006 to 2015. During the study period, the completeness of reporting was 93% for both primary and revision arthroplasties. Estimated revision rates were illustrated using the Kaplan-Meier method, and hazard ratios were calculated using a Cox regression model. Patient-reported outcome was measured with a postal survey at 12 months (range 10-14 months) postoperatively using the Western Ontario Osteoarthritis of the Shoulder (WOOS) index. The WOOS is a patient-administered questionnaire that measures the quality of life of patients with glenohumeral osteoarthritis. A visual analog scale that ranges from 0 to 100 is used for each question. There are 19 questions, giving a total score ranging from 0 to 1900, with 1900 being the worst. For simplicity of presentation, raw scores were converted to a percentage of the maximum score, with 100 being the best. There is no defined minimal clinically important difference of the WOOS, but the Danish Shoulder arthroplasty registry has for many years regarded an arbitrary difference of 10 or above as being clinically relevant. The rate of response to the WOOS was 71%.
Results
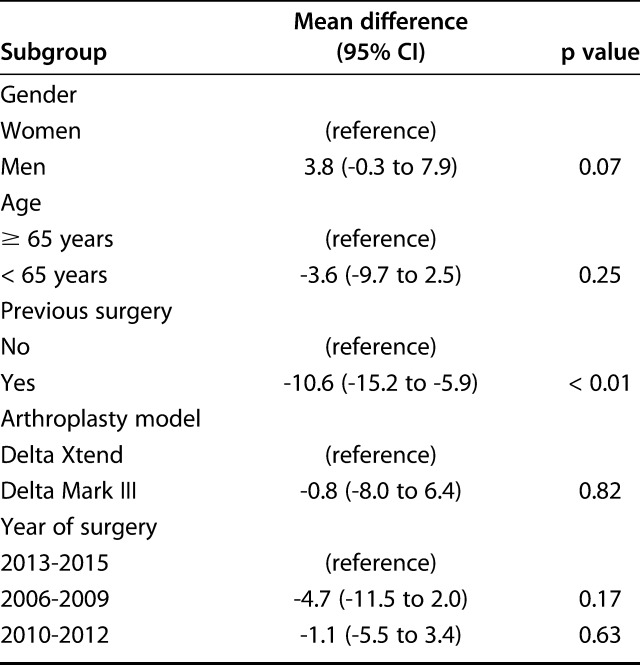
The estimated 10-year cumulative revision rate was 8.5% (95% confidence interval, 5.7%-11.3%) with differences between the arthroplasty model (21.0%; 95% CI, 11.8% to 30.8% for the Delta Mark III and 5.5%; 95% CI, 3.7% to 7.3% for the Delta Xtend) and gender (6.0%; 95% CI, 3.0% to 9.0% for women and 13.1%; 95% CI, 7.1% to 19.1% for men). After controlling for potential confounding variables including gender, previous surgery, arthroplasty model, and period of surgery, the risk of revision was higher with the Delta Mark III than with the Delta Xtend (hazard ratio 2.7; 95% CI, 1.3 to 5.4; p < 0.01) and higher in men than in women (hazard ratio 2.7; 95% CI, 1.6 to 4.7; p < 0.01). Thirty-three percent (19 of 57) of the revision arthroplasties were performed for dislocation and 32% (18 of 57) were to treat periprosthetic joint infection. After controlling for confounding variables, only previous surgery was associated with a worse WOOS score (mean difference -10.6; 95% CI, -15.2 to -5.9; p < 0.01); there were no associations between a worse score and gender, arthroplasty model, age group, or period of surgery.
Conclusions
The results from the present study can be used to inform patients about their individual risk of revision or a disappointing functional outcome. The study also demonstrates the need for proper patient selection and attention to technical details to reduce the risk of revision, especially for men. Our follow-up time was, however, short, with only an estimate of the 10-year revision rate. Future studies with a long-term follow-up duration are needed to confirm our results.
Level of Evidence
Level III, therapeutic study.
Introduction
Cuff-tear arthropathy (CTA) has been a surgical challenge in the past. Hemiarthroplasty with or without reconstruction of the rotator cuff or a hemiarthroplasty with an extended articular surface was used with varying and in many cases disappointing outcomes [8, 21, 27]. The reverse shoulder arthroplasty (RSA) has shown more reliable outcomes with improvement in pain and shoulder function [13, 26].
Current information about RSA for CTA is primarily based on single-center studies with a small number of patients, which limits their ability to identify patients who have an increased risk of revision or a worse functional outcome [1, 4, 6, 7, 9, 15, 20, 23-25].
By using data from a large nationwide arthroplasty registry, we asked the following questions: (1) What is the estimated 10-year cumulative revision rate after reverse shoulder arthroplasty for cuff-tear arthropathy, and what factors are associated with the risk of revision? (2) What is the patient-reported outcome 1 year after surgery, and what factors are associated with a worse patient-reported outcome?
Patients and Methods
Data Source
The Danish Shoulder Arthroplasty Registry is financed by the Danish counties and is independent of commercial interests. It was established in 2004 and since 2006, reporting has been mandatory for all Danish hospitals and private clinics performing shoulder arthroplasty. Data related to the patient and the operation are reported by the surgeon online at the time of the operation. Every year, the completeness of reporting is calculated by comparing the number of arthroplasties collected by the Danish Shoulder Arthroplasty Registry with the number of arthroplasties collected by the National Patient Register, which is an administrative dataset used by the Danish healthcare authorities to reimburse expenses for any hospitalization including shoulder arthroplasty surgery. The completeness is above 90% each year and was 93% for the entire study period for both primary and revision arthroplasties [5]. Each Danish citizen is given a unique civil registration number at the time of birth or immigration. This number was used to accurately link the primary procedure to the revision arthroplasty and to track patients who died or emigrated during the study period. Data reporting was checked manually.
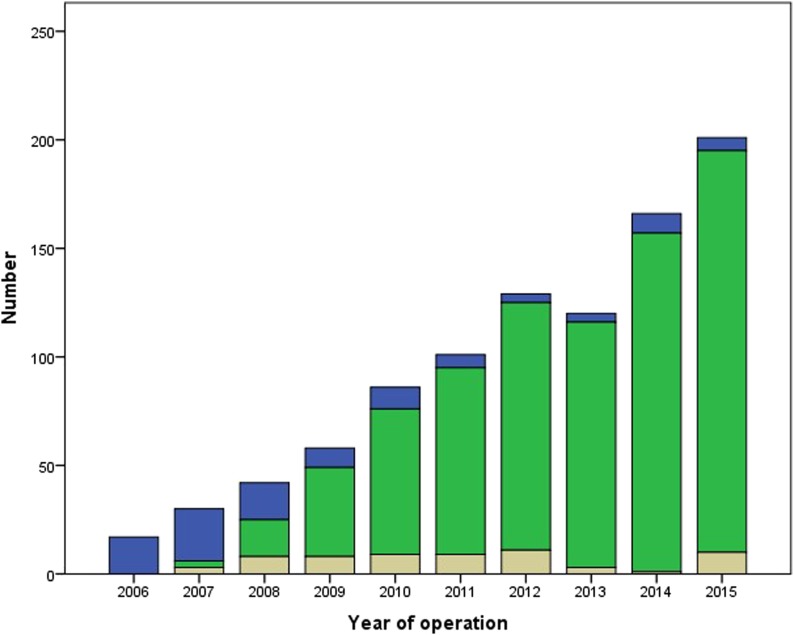
The Danish Shoulder Arthroplasty Registry collected information on 8930 shoulder arthroplasties from January 1, 2006 to December 31, 2015, 1699 of which were RSAs. A total of 1203 arthroplasties were used to treat CTA, 323 were for rheumatoid arthritis, 2882 were for osteoarthritis, 4088 were for fracture, and 245 were for avascular necrosis. In 154 arthroplasties, the diagnosis was reported as “other” and in 35 arthroplasties, information about the diagnosis was missing. Of the 1203 arthroplasties to treat CTA, 950 were RSAs, 105 were resurfacing hemiarthroplasties, and 135 were stemmed hemiarthroplasties. Five arthroplasties were reported as “other,” and for eight arthroplasties, information on the arthroplasty type was missing. Thus, for the present study, 950 RSAs performed to treat CTA were eligible. The mean age was 73 years (range 43-95 years). Fourteen percent (133 of 950) of the patients were younger than 65 years, and 62% (590 of 950) were women. Twenty-six percent (244 of 950) of the patients had previously undergone non-arthroplasty of the same shoulder. The number of RSAs increased from 2006 to 2016 (Fig. 1). Sixteen percent (147 of 950) of the arthroplasties were performed from 2006 to 2009, 33% (316 of 950) were performed from 2010 to 2012, and 51% (487 of 950) were performed from 2013 to 2015. Eighty-three percent (782 of 950) used the Delta Xtend (Depuy, Leeds, UK) and 11% (106 of 950) used the Delta Mark III (Depuy, Leeds, UK). Six percent (62 of 950) were recorded as “other.” Fourteen percent (131 of 950) of the patients died during the study period.
Fig. 1.
The numbers of Delta Mark III (blue), Delta Xtend (green) and other arthroplasty models (beige) from 2006 to 2015 are shown.
Revision
Revision was defined as the exchange or removal of any component. The arthroplasty revision rates were calculated from revisions reported to the Danish Shoulder Arthroplasty Registry up to December 31, 2015 and by checking deaths and emigration with the Danish National Register of Persons. The surgeon reported the indication for revision at the time of the revision procedure.
Patient-reported Outcome Measures
The patient-reported outcome was assessed by a postal survey at 12 months (range 10-14 months) postoperatively using the Western Ontario Osteoarthritis of the Shoulder (WOOS) index [14]. The WOOS is a patient-administered questionnaire that measures the quality of life of patients with glenohumeral osteoarthritis. The questionnaire consists of four domains (physical symptoms, sports/recreation/work, lifestyle, and emotion). A VAS score that ranges from 0 to 100 is used for each question. There are 19 questions, giving a total score ranging from 0 to 1900, with 1900 being the worst. For simplicity of presentation, the raw scores were converted to a percentage of the maximum score, with 100 being the best. We used a Danish version of the WOOS that has been translated according to the guidelines of Guillemin et al. [11] and validated using classical test theory [19]. There is no defined minimal clinically important difference of the WOOS, but the Danish Shoulder arthroplasty registry has for many years regarded an arbitrary difference of 10 or above as being clinically relevant. In case of revision or death within 1 year of the operation, the WOOS questionnaire was not sent to the patient. In case of revision later than 1 year after the operation, the WOOS score was recorded as usual and included in the analysis. Thus, 4% (34 of 950) of the patients died, emigrated, or underwent revision surgery within the first year. Of the remaining 96% (916 of 950) patients, 71% (654 of 916) returned a complete questionnaire, 1% (9 of 916) returned an incomplete questionnaire, and 27% (253 of 916) did not respond.
Statistical Analysis
The Kaplan–Meier method was used to illustrate the unadjusted cumulative revision rates. A log-rank test was used to compare the implant survival rates in different age groups. A Cox proportional hazards regression model was used to calculate hazard ratios, with 95% confidence intervals when subgroups were compared. Gender, arthroplasty model, age group (65 years or younger or older than 65 years, based on the Danish retirement age), period of surgery (2006 to 2009, 2010 to 2012, and 2013 to 2015) and previous non-arthroplasty surgery of the same shoulder were included in the model. Log-log plots and Schoenfeld residuals were used to check that the proportional hazards assumption was fulfilled. The inclusion of patients with bilateral procedures violates the assumption of independence. However, this may have little practical consequence in implant survival analyses [17]. By using the Kaplan-Meier method and the Cox proportional hazards regression model we also ignored the risk of competing risk. The time to revision did not follow the assumption of normal distribution and was therefore given as median and interquartile range. A general linear model was used to compare subgroups with regards to the WOOS. Gender, arthroplasty model, age group (65 years or younger or older than 65 years), period of surgery (2006 to 2009, 2010 to 2012, and 2013 to 2015) and previous non-arthroplasty surgery of the same shoulder were included in the model. The analysis was performed using SPSS version 22.0 (IBM Corp., Armonk, NY, USA). The level of statistical significance was set at p < 0.05, and p values were two-tailed.
Results
Revision
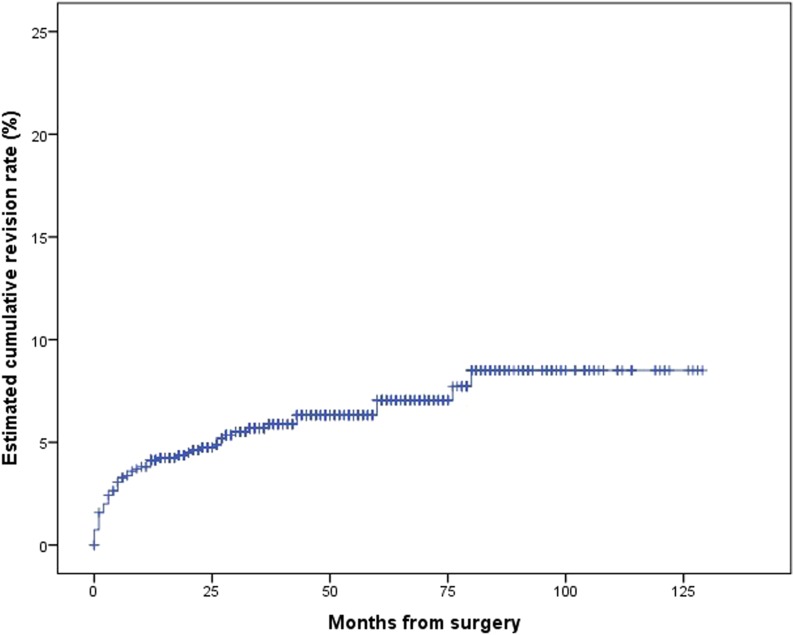
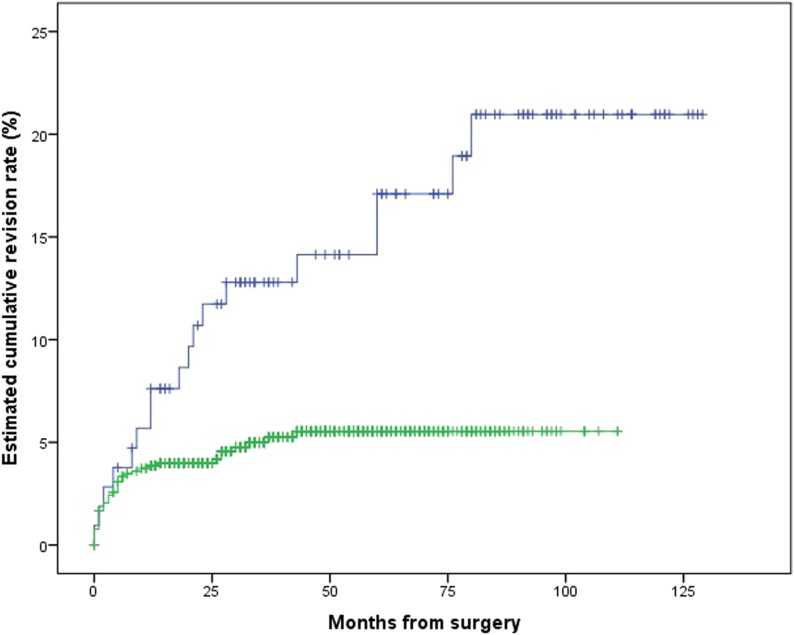
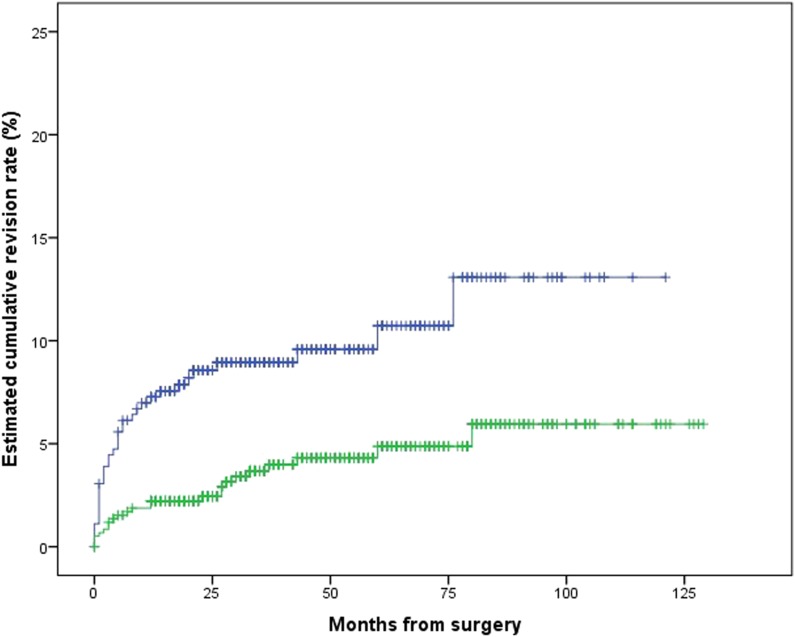
The estimated 10-year cumulative revision rate was 8.5% (95% CI, 5.8% to 11.2%) (Fig. 2), with differences between the Delta Xtend and Delta Mark III (Fig. 3) and between men and women (Fig. 4). After controlling for potential confounding variables such as gender, previous surgery, arthroplasty model, age groups, and period of surgery, we found the risk of revision was higher with the Delta Mark III than with the Delta Xtend (hazard ratio 2.7; 95% CI, 1.3 to 5.4; p < 0.01) and higher in men than in women (hazard ratio 2.7; 95% CI, 1.6 to 4.7; p < 0.01). We found no differences in the risk of revision for age groups, previous surgery, and period of surgery (Table 1). Thirty-three percent (19 of 57) of the arthroplasties were revised to treat dislocation and 32% (18 of 57) were revised to treat periprosthetic joint infection (Table 2), with differences between genders (Table 3) and between arthroplasty models (Table 4). The median time to revision was 5 months (IQR 1 to 22 months)
Fig. 2.
This Kaplan Meier survival curve shows an estimated revision rate of 8.5% (95% CI, 5.7% to 11.3%) for all RSAs.
Fig. 3.
Kaplan Meier survival curves show an estimated revision rate of 21.0% (95% CI, 11.8% to 30.8%) for Delta Mark III (blue) and 5.5% (95% CI, 3.7% to 7.3% for Delta Xtend (green).
Fig. 4.
Kaplan Meier survival curves show an estimated revision rate of 13.1% (95% CI, 7.1% to 19.1%) for men (blue) and 6.0% (95% CI, 3.0% to 9.0% for women) (green).
Table 1.
Risk of revision for subgroups in the Cox regression analysis
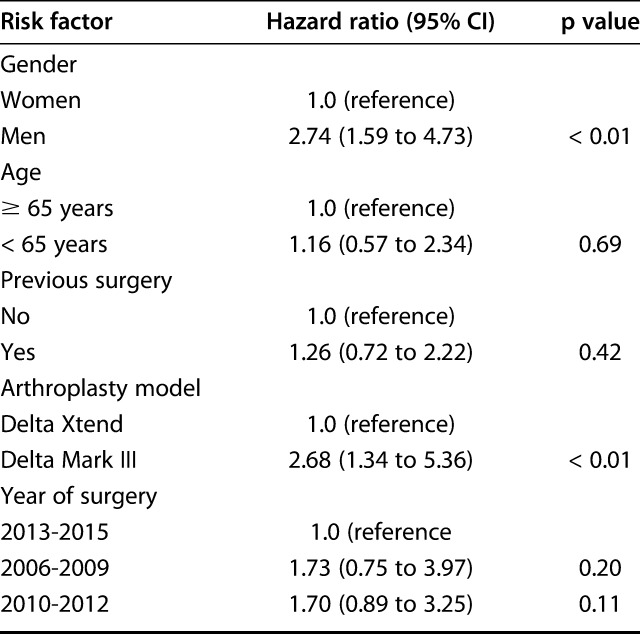
Table 2.
Indications for revision (n = 57)
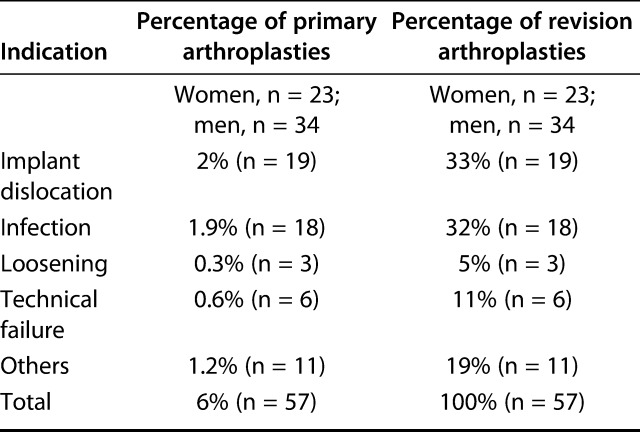
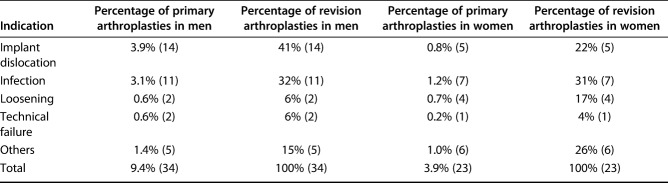
Table 3.
Indications for revision in men and women
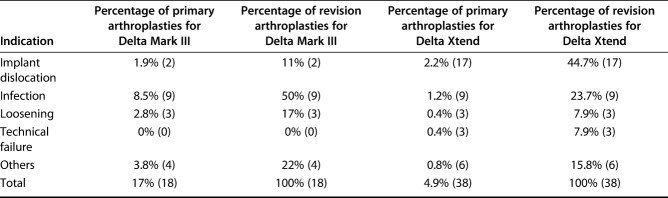
Table 4.
Indications for revision for the Delta Mark III and Delta Xtend
Patient-reported Outcome
After controlling for confounding variables, only previous surgery was associated with a worse WOOS score (mean difference -10.6; 95% CI, -15.2 to -5.9; p < 0.01), which also exceeded the clinically relevant difference. There were no associations between a worse score and gender, arthroplasty model, age groups, or period of surgery (Table 5).
Table 5.
Linear regression model comparing subgroups with regard to the WOOS score
Discussion
Previous studies have documented that RSA for CTA is associated with pain relief and improved shoulder function, but they have not been able to identify patients who have an increased risk of revision or a worse functional outcome [1, 4, 6, 7, 9, 15, 20, 23-25]. By using a nationwide cohort of patients treated with RSA for CTA, we found that men and patients who were treated with the Delta Mark III had a higher risk of revision and that patients who have had previous non-arthroplasty surgery of the same shoulder had a worse WOOS score 1 year after surgery.
Methodological considerations and limitations
The lack of a preoperative WOOS score prevents an assessment of improvement in functional outcome after surgery, and a 1-year follow-up of patient-reported outcome may not be adequate in clinical studies. In general, Clinical Orthopaedics and Related Research® disqualifies the use of scores in clinical studies if those scores are obtained only after surgery or if the follow-up duration is shorter than 2 years. In this case, these patients were retained because they allowed us to gain some insight into risk factors contributing to poorer scores after surgery. Furthermore 29% of the patients did not return the WOOS questionnaire. The consequences are unknown, but a previous study from the Danish Shoulder Arthroplasty Registry showed that non-responders had similar characteristics to responders [16].
The Danish Shoulder arthroplasty registry uses the Kaplan-Meier method to illustrate revision rates, and it is important to consider that some patients had a short follow-up time and that the curves only show the estimated and not the actual revision rate 10 years after surgery. Furthermore, whether to use the Kaplan Meier method or other methods such as the cumulative incidence method is controversial [3, 17, 22]. Fourteen percent of the patient died during our study period, which always precludes the occurrence of a subsequent revision. This introduces competing risk to the Kaplan Meier method, and as a consequence, the revision rates will be overestimated [17]. When a patient is contemplating arthroplasty surgery it is adequate to consider what happens during the lifetime of that patient. When doing so, the Kaplan Meier method seems adequate because the patients will be alive until the arthroplasty fails. For this reason, statisticians have argued that from a patient’s point of view, the Kaplan Meier method gives a logical, understandable, and clinically relevant estimate of the revision rates [10, 17, 22]. The Danish Shoulder arthroplasty registry uses the Cox proportional hazards regression model to report risk factors for revision that, similar to the Kaplan Meier method, is associated with competing risk. Other statistical methods such as the Fine and Gray model have been suggested, but they have also been criticized. A recent study [18] used data simulation with estimates from the Swedish Knee arthroplasty registry to report the theoretical effects of the Cox proportional hazards regression model and Fine and Gray model on the studied risk factors (age, gender, and arthroplasty type). The authors concluded that the estimates of the Fine and Gray models were misleading and recommended the use of a Cox proportional hazards regression model in analyzing arthroplasty registry data.
Risk of Revision
The risk of revision was higher in men than in women. Recently published data from the Nordic Arthroplasty Register Association showed that men had a risk ratio for revision of 3.8 (95% CI, 2.4 to 6.1) compared with women after RSA. The study also found that 0.9% of women and 5% of men underwent revision because of infection [12]. In our study, 32% of the revisions were done to treat periprosthetic joint infection, and a higher prevalence of infection seems to be one of the main factors for the higher revision rate in men than in women. The higher prevalence of infection in men is potentially related to abundant colonization with Cutibacterium acnes. The Delta Mark III had a higher risk of revision than did the Delta Xtend. This confirms the results of a previous study describing that the Delta Mark II has a poor design and mechanical properties [25]. The higher risk of revision could also be related to an early learning curve of the RSA procedure; however, the year of surgery did not have an effect on the revision rate. The Delta Mark III is no longer on the market. The later-introduced Delta Xtend has a low revision risk, which is similar to the results reported by the Australian Joint Registry [2].
Patient-reported Outcome
Not surprisingly, previous surgery of the same shoulder was associated with a worse patient-reported outcome. It confirms the results reported by Frankle et al. [9]. They included 25 patients who previously had non-arthroplasty surgery and compared their outcome with the outcome of 35 patients without previous surgery and found a difference in American Shoulder and Elbow Surgeons score in favor of patients without previous surgery. The reason for the worse outcome is unknown. It may be related to colonization with Cutibacterium acnes, stiffness caused by limited use of the shoulder for a long period of time, or formation of scar tissue.
Conclusion
The results from the present study can be used to inform patients about their individual risk of revision or a disappointing functional outcome. The study also demonstrates the need for proper patient selection and attention to technical details to reduce the risk of revision, especially for men. Our follow-up time was, however, short, with only an estimate of the 10-year revision rate, and future studies with a long-term follow-up are needed to confirm our results.
Acknowledgments
We thank Danish orthopaedic surgeons for data reporting and the patients who returned their WOOS questionnaire.
Footnotes
Each author certifies that neither he, nor any member of his immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his institution waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Herlev and Gentofte Hospital, University of Copenhagen, Copenhagen, Denmark.
References
- 1.Al-Hadithy N, Domos P, Sewell MD, Pandit R. Reverse shoulder arthroplasty in 41 patients with cuff tear arthropathy with a mean follow-up period of 5 years. J Shoulder Elbow Surg. 2014;23:1662-1668. [DOI] [PubMed] [Google Scholar]
- 2.Australian Ortopaedic Asssociation National Joint Replacement Registry. 2017. annual report. Demographics and outcome of shoulder arthroplasty. Available at: https://aoanjrr.sahmri.com/fi/annual-reports-2017. Accessed December 19, 2017.
- 3.Baui DJ, Latouche A, Porcher R. Competing events influence estimated survival propability: when is Kaplan Meier analysis appropriate? Clin Orthop Relat Res. 200:229-233. [DOI] [PubMed] [Google Scholar]
- 4.Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. Neer Award 2005: the Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg. 2006;15:527-540. [DOI] [PubMed] [Google Scholar]
- 5.Danish Shoulder Arthroplasty Registry. 2017. annual report. Available at: https://www.sundhed.dk/content/cms/3/4703_dansk-skulderalloplastik-register-dsr-aarsrapport-2017.pdf. Accessed December 19, 2017.
- 6.Drake GN, O’Connor DP, Edwards TB. Indications for reverse total shoulder arthroplasty in rotator cuff disease. Clin Orthop Relat Res. 2010;468:1526-1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Favard L, Levigne C, Nerot C, Gerber C, De Wilde L, Mole D. Reverse prostheses in arthropathies with cuff tear: are survivorship and function maintained over time? Clin Orthop Relat Res. 2011;469:2469-2475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Field LD, Dines DM, Zabinski SJ, Warren RF. Hemiarthroplasty of the shoulder for rotator cuff arthropathy. J Shoulder Elbow Surg . 1997;6:18-23. [DOI] [PubMed] [Google Scholar]
- 9.Frankle M, Siegal S, Pupello D, Saleem A, Mighell M, Vasey M. The reverse shoulder prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency. A minimum two-year follow-up study of sixty patients. J Bone Joint Surg Am. 2005;87:1697-1705. [DOI] [PubMed] [Google Scholar]
- 10.Gillam MH, Ryan P, Graves SE, Miller LN, Steiger RN, Salter A. Competing risks survival analysis applied to data from the Australian Orthopaedic Association National Joint Replacement Registry. Acta Orthop. 2010;81:548-555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol.1993;46:1417-1432. [DOI] [PubMed] [Google Scholar]
- 12.Lehtimaki K, Rasmussen J V, Mokka J, Salomonsson B, Hole R, Jensen SL, Aarimaa V. Risk and risk factors for revision after primary reverse shoulder arthroplasty for cuff tear arthropathy and osteoarthritis: a Nordic Arthroplasty Register Association study. J Shoulder Elbow Surg. 2018;27:1596-1601. [DOI] [PubMed] [Google Scholar]
- 13.Leung B, Horodyski M, Struk AM, Wright TW. Functional outcome of hemiarthroplasty compared with reverse total shoulder arthroplasty in the treatment of rotator cuff tear arthropathy. J Shoulder Elbow Surg . 2012;21:319-323. [DOI] [PubMed] [Google Scholar]
- 14.Lo IK, Griffin S, Kirkley A. The development of a disease-specific quality of life measurement tool for osteoarthritis of the shoulder: the Western Ontario Osteoarthritis of the Shoulder (WOOS) index. Osteoarthritis Cartilage. 2001;9:771-778. [DOI] [PubMed] [Google Scholar]
- 15.Nolan BM, Ankerson E, Wiater JM. Reverse total shoulder arthroplasty improves function in cuff tear arthropathy. Clin Orthop Relat Res. 2011;469:2476-2482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Polk A, Rasmussen J V, Brorson S, Olsen BS. Reliability of patient-reported functional outcome in a joint replacement registry. A comparison of primary responders and nonresponders in the Danish Shoulder Arthroplasty Registry. Acta Orthop. 2013;84:12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ranstam J, Karrholm J, Pulkkinen P, Makela K, Espehaug B, Pedersen AB, Mehnert F, Furnes O; NARA study group. Statistical analysis of arthroplasty data. II. Guidelines. Acta Orthop. 2011;82:258-267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ranstam J, Robertsson O, The Cox model is better than the Fine and Gray model when estimating relative revision risks from arthroplasty register data. Acta Orthop . 2017;88:578-580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rasmussen JV, Jakobsen J, Olsen BS, Brorson S. Translation and validation of the Western Ontario Osteoarthritis of the Shoulder (WOOS) index - the Danish version. Patient Relat Outcome Meas. 2013;4:49-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Samitier G, Alentorn-Geli E, Torrens C, Wright TW. Reverse shoulder arthroplasty. Part 1: systematic review of clinical and functional outcomes. Int J Shoulder Surg. 2015;9:24-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sanchez-Sotelo J, Cofield RH, Rowland CM. Shoulder hemiarthroplasty for glenohumeral arthritis associated with severe rotator cuff deficiency. J Bone Joint Surg Am. 2001;83:1814-1822. [DOI] [PubMed] [Google Scholar]
- 22.Sayers A, Evans JT, Whitehouse MR, Blom AW. Are competing risks models appropriate to describe implant failure? Acta Orthop. 2018;89:256-258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Mole D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004;86:388-395. [DOI] [PubMed] [Google Scholar]
- 24.Stechel A, Fuhrmann U, Irlenbusch L, Rott O, Irlenbusch U. Reversed shoulder arthroplasty in cuff tear arthritis, fracture sequelae, and revision arthroplasty. Acta Orthop. 2010;81:367-372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Werner CM, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am. 2005;87:1476-1486. [DOI] [PubMed] [Google Scholar]
- 26.Young SW, Zhu M, Walker CG, Poon PC. Comparison of functional outcomes of reverse shoulder arthroplasty with those of hemiarthroplasty in the treatment of cuff-tear arthropathy: a matched-pair analysis. J Bone Joint Surg Am. 2013;95:910-915. [DOI] [PubMed] [Google Scholar]
- 27.Zuckerman JD, Scott AJ, Gallagher MA. Hemiarthroplasty for cuff tear arthropathy. J Shoulder Elbow Surg. 2000;9:169-172. [PubMed] [Google Scholar]