History
Spondylolisthesis, from the Greek root spondyl, referring to vertebrae, and oliothesis, referring to slipping or dislocation, is a pathologic defect that refers to the translation of one vertebral body on another [26]. Spondylolisthesis has a reported incidence of 4% to 6% in childhood, with most being isthmic and occurring at L5 to S1 [11, 23]. Incidence increases to 5% to 10% in adults, becoming predominately degenerative, is more common in women, and most frequently occurs at L4 to L5, followed by L5 to S1 [11, 16, 43, 44]. Although there is evidence to suggest that spondylolisthesis is not present at birth, it has been shown to have a genetic component in 15% to 69% of patients [25, 37]. The most common symptoms in children include lower back or buttock pain that is worse with activity, pain with back hyperextension, and hamstring tightness [37, 43]. For adults with degenerative spondylolisthesis, symptoms may consist of lower back pain, radiculopathy or neurogenic claudication, with possible relief of symptoms occurring when sitting [16]. Worsening spondylolisthesis can have specific neurologic involvement, including radicular pain, potential bowel and bladder symptoms among other neurologic deficits, and in severe cases, cauda equina syndrome [23, 31]. Progression of spondylolisthesis and symptoms has been demonstrated to be quite variable, however, worse grades may have a higher predilection for progression [15, 16, 37].
As spondylolisthesis is most often asymptomatic, there may be inconsistency in presentation as well as during the physical exam; although the exam is not reliable for diagnosing spondylolisthesis, it can aid in evaluation [10]. Physical exam findings include flattening of the lumbar spine, pain with flexion and extension and muscle spasm [26]. The etiology of spondylolisthesis may present with specific physical exam findings. For example, in degenerative spondylolisthesis one may feel a step-off at the level above the slip, whereas in isthmic the step-off may be palpated below [16, 26, 40]. A prominent sacrum and hamstring tightness is also apparent [16, 26, 40, 45]. Other findings more common in children with isthmic deformity include a positive one-legged hyperextension test, also called the stork test, that produces ipsilateral back pain and an associated scoliotic deformity [23, 45]. Nerve root compression and spinal stenosis signs such as motor weakness, reflex changes, or sensory deficit are more commonly seen in the elderly who have degenerative spondylolisthesis and in patients with more severe translation [23, 45].
Wiltse et al. [45] categorized spondylolisthesis into five types based on etiology. Type I is congenital dysplasia with doming of the S1 vertebra, allowing the L5 vertebra to slip anteriorly. Type II, or isthmic, is caused by stress fractures in the pars interarticularis and occurs most frequently in children. Type III is degenerative, occurs in older people, and is caused by degenerative changes as a result of stress loading, leading to anterior slip. Type IV, traumatic, is caused by an acute injury as a result of trauma. Type V is pathologic fracture of the pars [45]. Although this classification provides valuable information, it is more of a descriptive classification and does not allow for tracking of progression, account for severity, or aid in treatment planning.
Marchetti and Bartolozzi [22] developed another classification system that distinguishes between developmental and acquired disease. Developmental is further subdivided into high dysplastic versus low dysplastic, with or without elongation, and lysis. Acquired is subdivided into traumatic, post-surgical, pathologic, and degenerative [22]. Although this classification can be helpful with prognosis, and to some degree treatment, it lacks the ability to accommodate for progression.
The Spinal Deformity Study Group (SDSG) classification system tried to address some of the shortcomings seen in previous classifications. They incorporated the Meyerding classification to assess severity of displacement, degree of dysplasia, and sacropelvic balance to help guide surgical management [20, 21]. However, with the initial proposed classification, there was low interobserver reliability and it has since been modified. Although this classification shows promise for spondylolisthesis evaluation, it has complex evaluation measurements, can be difficult to communicate, and has not been universally accepted.
Although the natural history and management of spondylolisthesis can be very broad, it is important to have a way to measure spondylolisthesis and monitor its progression. Many factors influence the symptoms of spondylolisthesis; however, the degree of translation clearly plays an important role and helps guide management [2, 14, 31]. Thus, it is important to have a standardized classification system to quantify the degree of displacement as well as monitor slip progression. The Meyerding classification system of spondylolisthesis was developed to address this need and is graded on a I to V scale according to the severity of the slip, as determined with plain radiographs [27].
Purpose
In general, orthopaedic classification systems are used for four purposes: communication, prognosis, research, and to guide treatment. The Meyerding classification was initially designed to facilitate communication and evaluate prognosis, as well as to assist with treatment guidance [2, 27]. It has since been used for these purposes and for research. By itself, the Meyerding classification system is not an excellent prognostic tool for progression. However, it has been used as a part of other classifications for prognostic evaluation [20, 40].
The Meyedering classification has also been shown to be reliable, easy to use, and simple to understand [19, 29].
Although by itself the classification has somewhat limited prognostic value, with all other factors being equal, such as etiology, higher grades do correlate to an increased progression risk [15, 16, 37]. When used in combination with etiology and sagittal parameters, it has been used for tracking and evaluation of spondylolisthesis, as in the aforementioned SDSG classification [20, 21].
All papers evaluating spondylolisthesis for research purposes account for the grade of slip. The Meyerding classification may be instrumental for tracking prior progression of displacement and assisting in the evaluation of the other factors involved with spondylolisthesis [18, 20]. Therefore, while in itself not a great classification for prognostic purposes, it does play an role.
In Meyerding’s original paper, the degree of slip was used as a guide for both nonoperative treatment and surgical decision making [27,12]. Although other factors besides the Meyerding grade now help guide treatment, the degree of slip still impacts decision-making [27, 20]. For example, symptomatic Grade I and II slips that have failed conservative measures are amenable to fusion, or in some patients, decompression alone, depending on the degree of instability on flexion and extension films, among other factors. Higher-grade symptomatic slips such as Grade III to V slips usually result in a reduction and fusion or in situ fusion. However, the amount of reduction may be limited because reduction may create a traction injury to the nerve.
Description
The Meyerding classification grade is determined by measuring the degree of slip using standing, neutral lateral radiographs of the lumbar spine [27]. The classification system divides slip into five grades: 0% to 25% is Grade I, 25% to 50% is Grade II, 50% to 75% is Grade III, 75% to 100% is Grade IV, and greater than 100% is Grade V (Table 1). The grade percent is determined by drawing a line through the posterior wall of the superior and inferior vertebral bodies and measuring the translation of the superior vertebral body as a percentage of the distance between the two lines. This line is considered the numerator over the denominator which is length of the vertebral body below (Fig. 1A-F). Grades I and II are generally considered low-grade slip, whereas Grades III, IV, and V are considered high-grade slip [27]. Grade V is also called spondyloptosis and is a complete slip greater than 100%. Further assessment might include lateral flexion and extension views to evaluate segmental translation, which allows for a further assessment of mobility and slip severity.
Table 1.
Correlation of the percentage of slip with the Meyerding classification grade

Fig. 1-.
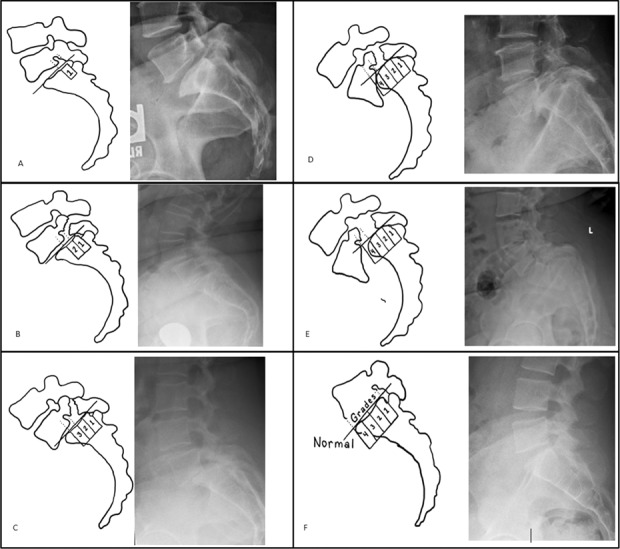
AF According to the Meyerding classification (A) 0% to 25% is a Grade I slip, (B) 25% to 50% is a Grade II slip, (C) 50% to 75% is a Grade III slip, (D) 75% to 100% is a Grade IV slip, and (E) spondyloptosis > 100% is a Grade V slip; (F) this image shows all grades compared with normal alignment.
Treatment is often guided by grade, etiology, the patient’s symptoms, and examination findings. Instability is another factor to be considered. This is evaluated by flexion-extension radiographs which help to determine whether spondylolisthesis is static or dynamic. Instability is considered significant if there is greater than 4 mm of translation or greater than 10° change is observed on dynamic flexion-extension films [3]. All these factors should be considered when determining nonoperative versus surgical management and directing specific surgical management [5, 10, 39].
In general, spondylolisthesis itself does not need treatment because the natural history of Grade 1 degenerative slips is that they do not progress. Patients with Grade I or II slip who are asymptomatic or mildly symptomatic generally have a lower chance of progression and are candidates for nonoperative management or may not need treatment [9, 31]. Nonoperative treatment is successful in most patients, particularly those with mild symptoms. Surgical intervention is reserved for those patients whose symptoms are refractory to these measures, or patients with more severe neurologic involvement. Specific nonoperative measures may vary depending on etiology and may include activity modification. For example, nonoperative measurements in young athletes with isthmic spondylolisthesis who participate in hyperextension athletics such as gymnastics can be treated with nonsteroidal medications, bracing, physical therapy, and selective nerve or pars injections. Typically, physical restrictions may be relaxed as symptoms improve. Most patients experience symptom resolution [6, 17]. Multiple studies have shown such measures to be an effective treatment method and most patients do not need surgical intervention. One meta-analysis showed an overall success rate of 84% in children with spondylolisthesis using nonoperative methods [17]. Several studies evaluating adults with spondylolisthesis demonstrated symptom improvement and pain reduction [33, 39].
If patients do not respond to this nonoperative management after 6 months of care, have a Meyerding Grade of III or greater (high-grade slip), progression of slippage greater than one grade, or a high degree of instability on flexion-extension radiographs, they may be considered candidates for surgery. When making this decision, specific attention to symptoms, health of the patient, and desire for surgery must also be considered [6, 13].
Surgical treatment of spondylolisthesis is controversial. For Grades I and II slips, decompression and/or fusion is generally considered. Decompression alone is considered for those with minimal instability; however, fusion may be necessary for iatrogenic instability created by decompression [38, 42]. The etiology and disc height, factors that are associated with increased instability, may also be considered in determining surgical management. For example, in patients with isthmic spondylolisthesis and increased disc height, interbody fusion is more strongly considered [16, 32].
Surgical decision making for high-grade slips, which includes Grades III, IV, and V is also based on other factors, such as mobility with flexion and extension, sagittal alignment, etiology, and disc height [1, 8, 9, 14, 18]. For high-grade slips, fusion and decompression are generally considered [5, 7]. Both the type of fusion and use of instrumentation are controversial [14, 39]. Specific surgical approaches that have been compared when treating high-grade spondylolisthesis are stand-alone anterior lumbar interbody fusion, posterior spinal instrumented fusion, posterior spinal non-instrumented fusion, interbody instrumented fusion, and in situ fusion [7, 34, 38]. Overall results have been inconclusive as to which method provides the best outcomes, with the exception of interbody fusion having the possibility of lower rates of pseudarthrosis in isthmic spondylolisthesis [16, 32]. The Bohlman procedure has been proposed as a good option for the treatment of non-mobile high-grade spondylolisthesis where global alignment is not a major concern [3, 4, 12]. This technique involves a single-stage posterior procedure that includes posterior decompression, posterolateral fusion, and transvertebral interbody fusion with grafting [4]. This procedure initially demonstrated issues with reduction in the slip angle and graft failure [4]. However, a newer study with the addition of posterior instrumentation has shown improved fusion rates [12]. Reduction and fusion are also considerations for patients with high-grade slips when considering overall global alignment. This combination has theoretically been proposed to allow sagittal malalignment correction and to increase the contact area between two vertebrae resulting in improved fusion results [34, 35]. However, with a greater the degree of reduction, there is a greater the risk of neurologic injury [28, 30, 35, 36]. Several methods have also been proposed for the protection of nerve roots while maximizing the degree of reduction. Preoperative interventions such as traction can help reduce the translation before the procedure. Intraoperative techniques such as hip extension to decrease strain on the nerve, exposure of the whole nerve root for visualization, reduction screw placement to facilitate translation, and neuroforaminal decompression are all methods to assist with reduction and prevent neurological injury [7, 45].
Validation
In a previous study that compared the reliability of several different spondylolisthesis and risk progression markers, the only markers that had consistent intra-observer reliability and inter-observer reliability were the Meyerding classification system, pelvic tilt, and C7 balance [29]. In that study, the Meyerding classification demonstrated an intra-observer reliability of 0.95 and inter-observer reliability of 0.93 among five different participants reading the radiographs. Within subset groups, the reliability of some other radiographic markers were decreased because of doming of the sacrum or other complicating radiographic findings. However, the Meyerding classification only exhibited a decrease from 0.95 to 0.92 and from 0.93 to 0.88 for intra-rater and inter-rater reliability, respectively, demonstrating its high level of consistency even when other complicating findings were present.
Another study compared intra-rater and inter-rater reliability among fellows with less than 6 months of experience and attending physicians regarding eight possible spondylolisthesis markers [41]. These included the slip percentage, Meyerding grade, slip angle, lumbosacral angle, kyphosis angle, lumbar index, sagittal rotation, and sacral inclination. The only three markers that had inter-observer and intra-observer reliabilities greater than 0.75 for correlation coefficients were the slip percentage, Meyerding grade, and slip angle. The slip percentage and Meyerding grade had an intra-observer reliability of 0.94 and 0.79, respectively, and an inter-observer reliability of 0.89 and 0.78, respectively. Several other measures believed to be associated with the risk of spondylolisthesis progression, including sacral table angle, sacral slope, pelvic radius angle, lumbosacral angle, and pelvic incidence, do not appear to have robust inter-observer and intra-observer reliability [19, 29, 41].
Limitations
This classification system has been demonstrated to be a reasonable tool for communication, based on the validation showing excellent inter- and intra-observer reliability. With regard to its application toward future research, the Meyerding classification alone is not sufficient. Multiple factors other than degree of slip have now been demonstrated to be involved in the pathogenesis of spondylolisthesis. Although several of these other factors are generally used in the evaluation of spondylolisthesis, the Meyerding classification is still included as part of newer classification systems when discussing future directions for research.
This classification system does have limitations, specifically in regard to prognosis and treatment management. Although it can be used as a marker to track anatomic progression over time, it is not a good predictor of progression risk by itself, particularly in those with low-grade spondylolisthesis. Progression risk has also been correlated with other factors such as etiology, lumbopelvic parameters, sacral morphology, and global alignment, which are not addressed in this classification [15, 19].
Slip severity also does not correspond well with symptoms and is not a reliable prognostic tool for symptom progression [1, 28]. A further study was unable to find a high correlation of slip progression or increasing Meyerding classification grade with worsening symptoms [24].
Finally, although it may be used to guide treatment, the Meyerding classification alone is inadequate for treating spondylolisthesis. In general, high-grade spondylolisthesis is more likely to be treated with surgical intervention, but it is far less common than low-grade spondylolisthesis. This limits the classification as an effective guide for surgical management in patients with low-grade spondylolisthesis. This is partly because it lacks predictive value for progression risk, limiting its usefulness in determining whether surgical intervention is indicated to prevent progression in this population. In addition, no specific surgical intervention has been shown to produce superior outcomes to other surgical interventions when the Meyerding classification system is used alone [8, 23].
Conclusion
The Meyerding classification describes the degree of translation of spondylolisthesis. Despite its limitations, this classification system is widely used and accepted because of its relative simplicity as well as its substantial intra-observer and inter-observer reliability. This classification is also used to track and evaluate progression; however, it has not demonstrated predictive value for slip progression. Another predictive classification, the SDSG, considers not only factors evaluated in the Meyerding classification but also the causes of spondylolisthesis and other anatomic markers as described above [20]. Although these other classification systems allow us to assess the risk of slip progression and symptoms and might be used to improve treatment outcomes with nonoperative and surgical treatments, they are much more complex, decreasing the ease of communication, universality, and reliability. Therefore, until or unless these new classification systems gain wider acceptance, we recommend those using the Meyerding classification use it with caution and awareness of its strengths and limitations.
Acknowledgments
None.
Footnotes
Each author certifies that neither he, nor any member of his immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
References
- 1.Albanese M, Pizzutillo PD. Family study of spondylolysis and spondylolisthesis. J Pediatr Orthop. 1982;2:496-499. [DOI] [PubMed] [Google Scholar]
- 2.Attiah MA, Macyszyn L, Cahill PJ. Management of spondylolysis and spondylolisthesis in the pediatric population a review. Semin Spine Surg. 2014;6:230-237. [Google Scholar]
- 3.Boden SD, Wiesel SW. Lumbosacral segmental motion in normal individuals. Have we been measuring instability properly? Spine . 1990;15:571-576. [DOI] [PubMed] [Google Scholar]
- 4.Bohlman HH, Cook SS. One-stage decompression and posterolateral and interbody fusion for lumbosacral spondyloptosis through a posterior approach. Report of two cases. J Bone Joint Surg Am. 1982;64:415-418. [PubMed] [Google Scholar]
- 5.Boxall D, Bradford DS, Winter RB, Moe JH. Management of severe spondylolisthesis in children and adolescents. J Bone Joint Surg Am. 1979;61:479-495. [PubMed] [Google Scholar]
- 6.Cheung EV, Herman MJ, Cavalier R, Pizzutillo PD. Spondylolysis and spondylolisthesis in children and adolescents: II. Surgical management. J Am Acad Orthop Surg. 2006;14:488-498. [DOI] [PubMed] [Google Scholar]
- 7.DeWald CJ, Vartabedian JE, Rodts MF, Hammerberg KW. Evaluation and management of high-grade spondylolisthesis in adults. Spine (Phila Pa 1976). 2005;30:S49-59. [DOI] [PubMed] [Google Scholar]
- 8.Eismont FJ, Norton RP, Hirsch BP. Surgical management of lumbar degenerative spondylolisthesis. J Am Acad Orthop Surg. 2014;22:203-213. [DOI] [PubMed] [Google Scholar]
- 9.Epstein NE. Decompression in the surgical management of degenerative spondylolisthesis: advantages of a conservative approach in 290 patients. J Spinal Disord. 1998;11:116-122. [DOI] [PubMed] [Google Scholar]
- 10.Fredrickson BE, Baker D, McHolick WJ, Yuan HA, Lubicky JP. The natural history of spondylolysis and spondylolisthesis. J Bone Joint Surg Am. 1984;66:699-707. [PubMed] [Google Scholar]
- 11.Frymoyer JW. Degenerative spondylolisthesis: diagnosis and treatment. J Am Acad Orthop Surg. 1994;2:9-15. [DOI] [PubMed] [Google Scholar]
- 12.Hart RA, Domes CM, Goodwin B, D’Amato CR, Jung UY, Turker RJ, Halsey MF. High-grade spondylolisthesis treated using a modified Bohlman technique: results among multiple surgeons. J Neurosurg Spine. 2014;20:523-530. [DOI] [PubMed] [Google Scholar]
- 13.Hensinger RN, Lang JR, MacEwen GD. Surgical management of spondylolisthesis in children and adolescents. Spine (Phila Pa 1976). 1976;1:207-216. [Google Scholar]
- 14.Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am. 1991;73:802-808. [PubMed] [Google Scholar]
- 15.Huang RP, Bohlman HH, Thompson GH, Poe-Kochert C. Predictive value of pelvic incidence in progression of spondylolisthesis. Spine (Phila Pa 1976). 2003;28:2381-2385. [DOI] [PubMed] [Google Scholar]
- 16.Jones TR, Rao RD. Adult isthmic spondylolisthesis. J Am Acad Orthop Surg. 2009;17:609-617. [DOI] [PubMed] [Google Scholar]
- 17.Klein G, Mehlman CT, McCarty M. Nonoperative treatment of spondylolysis and grade I spondylolisthesis in children and young adults: a meta-analysis of observational studies. J Pediatr Orthop. 2009;29:146-156. [DOI] [PubMed] [Google Scholar]
- 18.Kristof RA, Aliashkevich AF, Schuster M, Meyer B, Urbach H, Schramm J. Degenerative lumbar spondylolisthesis-induced radicular compression: nonfusion-related decompression in selected patients without hypermobility on flexion-extension radiographs. J Neurosurg. 2002;97:281-286. [DOI] [PubMed] [Google Scholar]
- 19.Labelle H, Roussouly P, Berthonnaud E, Dimnet J, O’Brien M. The importance of spino-pelvic balance in L5–S1 developmental spondylolisthesis: a review of pertinent radiologic measurements. Spine (Phila Pa 1976). 2005;30:S27-S34. [DOI] [PubMed] [Google Scholar]
- 20.Mac-Thiong JM, Duong L, Parent S, Hresko MT, Dimar JR, Weidenbaum M, Labelle H. Reliability of the SDSG classification of lumbosacral spondylolisthesis. Spine . 2012;37:E95-102. [DOI] [PubMed] [Google Scholar]
- 21.Mac-Thiong JM, Labelle H, Parent S, Hresko MT, Deviren V, Weidenbaum M, members of the Spinal Deformity Study Group. Reliability and development of a new classification of lumbosacral spondylolisthesis. Scoliosis. 2008;3:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marchetti PG, Bartolozzi P. Classification of spondylolisthesis as a guideline for treatment, in Bridwell KH, DeWald RL, eds: The Textbook of Spinal Surgery, 2nd ed 1997;2:1211-1254. [Google Scholar]
- 23.Marawar SV. The radiographic parameters for the prediction of spondylosis and spondylolisthesis. Semin Spine Surg. 2014;26:219-224. [Google Scholar]
- 24.Mataliotakis GI, Tsirikos AI. Spondylolysis and spondylolisthesis in children and adolescents: current concepts and treatment. Orthop Trauma. 2017;31:395-401. [Google Scholar]
- 25.Matsunaga S, Sakou T, Morizono Y, Masuda A, Demirtas AM. Natural history of degenerative spondylolisthesis. Pathogenesis and natural course of the slippage. Spine (Phila Pa 1976). 1999;15:1204-1210. [DOI] [PubMed] [Google Scholar]
- 26.McPhee IB, O’Brien JP, McCall IW, Park WM. Progression of lumbosacral spondylolisthesis. Austalas Radiol. 1981;25:91-95. [DOI] [PubMed] [Google Scholar]
- 27.Meyerding H. Low backache and sciatic pain associated with spondylolisthesis and protruded intervertebral disc: incidence, significance, and treatment. J Bone Joint Surg Am. 1941;23:461-470. [Google Scholar]
- 28.Meyerding HW. Spondylolisthesis. Surg Gynecol Obstet. 1932;54:371-377. [Google Scholar]
- 29.Molinari RW, Bridwell KH, Lenke LG. Complications in the surgical treatment of pediatric high-grade, isthmic dysplastic spondylolisthesis. A comparison of three surgical approaches. Spine (Phila Pa 1976). 1999;24:1701-1711. [DOI] [PubMed] [Google Scholar]
- 30.Montgomery RA, Hresko MT, Kalish LA. Spondylolisthesis: intra-rater and inter-rater reliabilities of radiographic sagittal spinopelvic parameters using standard picture archiving and communication system measurement tools. Spine Deform. 2013;1:412-418. [DOI] [PubMed] [Google Scholar]
- 31.Muschik M, Zippel H, Perka C. Surgical management of severe spondylolisthesis in children and adolescents. Anterior fusion in situ versus anterior spondylolisthesis with posterior transpedicular instrumentation and reduction. Spine (Phila Pa 1976). 1997;22:2036-2042. [DOI] [PubMed] [Google Scholar]
- 32.Neymar U, Shepard N, Cho W, Sharan A. Conservative management of spondylolysis and spondylolisthesis. Semin Spine Surg. 2014;26:225-229. [Google Scholar]
- 33.Osterman K, Schlenzka D, Poussa M, Seitsalo S, Virta L. Isthmic spondylolisthesis in symptomatic and asymptomatic subjects, epidemiology, and natural history with special reference to disk abnormality and mode of treatment. Clin Orthop Relat Res. 2003;297:65-70. [PubMed] [Google Scholar]
- 34.O’Sullivan PB, Phyty GD, Twomey LT, Allison GT. Evaluation of specific stabilizing exercise in the treatment of chronic low back pain with radiologic diagnosis of spondylolysis or spondylolisthesis. Spine (Phila Pa 1976) 1997;22:2959-2967. [DOI] [PubMed] [Google Scholar]
- 35.Passias PG, Poorman CE, Yang S, Boniello AJ, Jalai CM, Worley N, Lafage V. Surgical treatment strategies for high-grade spondylolisthesis: a systematic review. Int J Spine Surg . 2015;9:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Poussa M, Remes V, Lamberg T, Tervahartiala P, Schlenzka S, Yrjonen T, Osterman K, Seitsalo S, Helenius I. Treatment of severe spondylolisthesis in adolescence with reduction or fusion in situ: long-term clinical, radiologic, and functional outcome. Spine (Phila Pa 1976). 2006;31:583-590. [DOI] [PubMed] [Google Scholar]
- 37.Sailhan F, Gollogly S, Roussouly P. The radiographic results and neurologic complications of instrumented reduction and fusion of high-grade spondylolisthesis without decompression of the neural elements: a retrospective review of 44 patients. Spine (Phila Pa 1976). 2006;31:161-169. [DOI] [PubMed] [Google Scholar]
- 38.Seitsalo S, Osterman K, Hyvãrinen H, Tallroth K, Schlenzka D, Poussa M. Progression of spondylolisthesis in children and adolescents. A long-term follow-up of 272 patients. Spine (Phila Pa 1976). 1991;16:417-421. [DOI] [PubMed] [Google Scholar]
- 39.Sengupta DK, Herkowitz HN. Degenerative spondylolisthesis: review of current trends and controversies. Spine (Phila Pa 1976). 2005;30:S71-S81. [DOI] [PubMed] [Google Scholar]
- 40.Sinaki M, Lutness MP, Ilstrup DM, Chu CP, Gramse RR. Lumbar spondylolisthesis: retrospective comparison and three-year follow-up of two conservative treatment programs. Arch Phys Med Rehabil. 1989;70:594-559 [PubMed] [Google Scholar]
- 41.Smith JA, Hu SS. Management of spondylolysis and spondylolisthesis in the pediatric and adolescent population. Orthop Clin North Am 1999;30:487-499. [DOI] [PubMed] [Google Scholar]
- 42.Timon SJ, Gardner MJ, Wanich T, Poynton A, Pigeon R, Widmann RF, Rawlins BA, Burke SW. Not all spondylolisthesis grading instruments are reliable. Clin Orthop Relat Res. 2005:157-162. [DOI] [PubMed] [Google Scholar]
- 43.Vibert BT, Sliva CD, Herkowitz HN. Treatment of Instability and Spondylolisthesis: Surgical versus Nonsurgical Treatment. Clin Orthop Relat Res. 2006;443:222-227. [DOI] [PubMed] [Google Scholar]
- 44.Virta L, Ronnemaa T, Osterman K, Aalto T, Laakso M. Prevalence of isthmic lumbar spondylolisthesis in middle-aged subjects from eastern and western Finland. J Clin Epidemiol. 1992;45:917-922. [DOI] [PubMed] [Google Scholar]
- 45.Wiltse LL, Newman PH, Macnab I. Classification of spondylolysis and spondylolisthesis. Clin Orthop Relat Res. 1976;117:23-29. [PubMed] [Google Scholar]
- 46.Williams KD, Canale ST, Azar FM, Beaty JH, Campbell WC. Campbells Operative Orthopaedics. 13th ed. Philadelphia, PA: Elsevier; 2017:1728-1755. [Google Scholar]


