In the Blackfeet Tribal community, a positive relationship between early life trauma and immune system inflammation is observed for individuals with a low sense of belonging to the community.
Keywords: American Indian Health, Adverse childhood experiences, Community belonging, Health disparities, Inflammation
Abstract
Background
Previous research documents an association between adverse childhood experiences (ACEs) and immune system inflammation. High chronic inflammation is believed to be one biological pathway through which childhood adversity may affect health into adulthood. The Blackfeet tribal community has high rates of childhood trauma and community members are disproportionately affected by inflammatory diseases.
Purpose
To investigate whether belonging to the tribal community may moderate the relationship between childhood trauma and immune system inflammation in the Blackfeet tribal community.
Methods
In a sample of 90 adults residing on the Blackfeet reservation, we measured ACEs belonging to the tribal community and two markers of immune system inflammation, interleukin-6 (IL-6) and C-reactive protein (CRP).
Results
We found that independent of age, gender, annual income, body mass index, and depressive symptoms, belonging to the tribal community and ACEs interacted to predict levels of both IL-6 and CRP (B= −.37, t[81] = −3.82, p < .001, R2 change = .07 and B = −.29, t[81] = −2.75, p = .01, R2 change = .08, respectively). The association between ACEs and markers of immune system inflammation was statistically significant for community members who reported low levels of belonging to the community.
Conclusions
The findings of this study have important implications for intervention research seeking to reduce risk for inflammatory diseases for at-risk populations. Fostering stronger connections to the larger tribal community may positively affect risk for inflammatory diseases. Future work should examine the behavioral and psychosocial pathways through which stronger connections to community may confer health benefits.
A robust literature links adverse childhood experiences (ACEs) with negative physical and mental health outcomes and higher rates of morbidity and mortality [1–3]. Previous research indicates that this relationship is graded, with greater self-report of ACEs predicting greater risk for mental and physical health problems in adulthood [4, 5]. More specifically, greater report of ACEs has been previously associated with increased anxiety and prevalence of anxiety disorder [6], poorer self-rated health and greater mental distress [7], and increased risk for heart attack and diabetes [8].
Low-grade inflammation is believed to be a likely pathway through which early-life adversity imparts enduring effects on health [9]. In line with this, previous work documents an association between ACEs and a pro-inflammatory phenotype that could contribute to increased disease incidence [10, 11]. However, not all individuals who experience ACEs suffer from ill-health. As an example, two independent investigations recently reported that resilience resources (e.g., social and emotional support, meaningful engagement, life satisfaction, and sleep quality) moderate the association between ACEs and inflammation in adulthood [12, 13]. Thus, factors that promote positive outcomes (i.e., reduced levels of inflammation) in the face of adversity are important to understand, particularly in populations that experience high rates of trauma and inflammatory diseases, such as American Indian (AI) communities.
The indigenous people of North America suffered tremendously during the period of European colonialism as a result of disease, war, and genocide. The population was reduced from an estimated 10 million to fewer than a million people [14]. Their culture was under further attack during the boarding school era when the federal government worked to eradicate tribal languages and practice by removing youth from their elders, family, and community. Through all this adversity, commonly referred to as historical trauma, AIs have demonstrated tremendous resilience.
Resilience has been defined as processes that individuals, families, and communities use to cope, adapt, and take advantage of assets when facing significant acute or chronic stress [15]. In recent years, resilience research has begun to focus on cultural resilience or the role that culture may play as a resource for resilience in the individual [16]. Ethnic identification reflects the extent to which individuals positively view and connect with their ethnic background and feel that their ethnicity is a central part of their overall identity. The development of ethnic identity is particularly important for individuals from minority groups given the heightened salience of their ethnicity from the perspective of the larger society [17]. In previous work, among Asian, Black, and Latino youth, ethnic identification was positively associated with well-being and protected from the negative consequences of discrimination [18, 19]. Specific to AI communities, in a previous investigation focused on AI youth, greater identification with one’s community was associated with resilience in academic outcomes and in the context of risky health behaviors [20].
In addition to the experience of historical trauma, AI communities suffer from disproportionately high rates of exposure to early-life trauma and diseases in which inflammatory processes are implicated, including cardiovascular disease and depression [21]. To date, there is limited knowledge about what factors may offset the association between early-life trauma and physiological profiles linked to increased risk for disease in adults in tribal communities.
Given that previous work has highlighted the importance of community belonging for AI populations, it is possible that greater levels of community belonging may buffer the negative effects of stress on health. This would be in line with a large body of work indicating that varying forms of social support (including belonging support) reduce the association between stress and negative health outcomes [22–24]. In line with this, AI community members with a greater sense of belonging to their community may be protected from the association between early-life trauma and inflammation.
The Blackfeet Nation, located 40 miles south of the Canadian border in Browning, MT, has roughly 18,000 enrolled members. Before the reservation era, the Blackfeet territory stretched all the way north to Canada from Calgary Alberta and all the way south to Wyoming. The Blackfeet is one of the only tribes that remain on their original territory.
In a sample of 90 adult community members from the Blackfeet Nation, we examine the relationships between adversity in early childhood, sense of belonging to the tribal community, and immune system inflammation. We first investigate whether the relationship between ACEs and immune system inflammation observed in other ethnic groups (i.e., greater adversity in childhood associating with higher levels of systemic inflammation) exists in the Blackfeet community, and then consider whether sense of belonging to the tribal community moderates the relationship between early-life adversity and levels of inflammation.
Method
Participants (N = 90 Age: M = 37.58, standard deviation [SD] = 15.90) were recruited by student interns at Blackfeet Community College (BCC) through advertisement at a community health fair and other community centers. One hundred participants were screened for eligibility, and 10 participants were excluded based on their self-report of chronic health conditions. BCC student interns developed this research and managed the project from inception to completion. Given that the BCC student interns are community members of the Blackfeet Nation, this project was community driven. The selection of questionnaires and focus of the research was informed by their experiences as community members. Participants arrived at BCC, completed informed consent, and completed the following procedures. Height, weight, and blood pressure were measured by a research assistant. Participants self-reported medication use. Before conducting our analyses, we screened for use of cold medications, antihistamines, and inhaled corticosteroids. Blood samples were drawn between 9 am and 12 pm by research assistants with phlebotomy training. Finally, participants completed a series of paper-based questionnaires. Upon completion of these procedures, participants received 75 dollars.
Measures
Adverse childhood experiences
We used the ACE Study Questionnaire [25] as a measure of exposure to traumatic experiences in childhood. The questionnaire includes dichotomous items (yes/no) asking participants whether they experienced any of the 10 adverse experiences before age 18.
Belonging and identification with one’s tribal community and its practices
Participants answered the following questions with yes or no: Being part of my tribe is important to me? Do you practice your native language? Do you take part in traditional ceremonies? Do you worship/pray in your own belief? Do you participate in community activities or social events? Do you have respect for your community? A response of yes was scored as a 1, and a response of no was scored as a 0. Higher overall scores on this measure reflect stronger connection or belonging to their community (α = .71). This measure was developed by BCC students and faculty based on a previous investigation in a sample of community members. The data from this research indicated that these items were associated with self-reported health outcomes. Overall, this scale was intended to reflect community members’ sense of belonging to the tribal community and identification with its practices and values.
Markers of immune system inflammation
Levels of interleukin-6 (IL-6) and C-reactive protein (CRP) in serum samples were determined using a high sensitivity quantitative sandwich enzyme immunoassay kit (R&D systems) run according to manufacturer’s directions. IL-6 and CRP levels were extrapolated from a standard curve with linear regression from a log linear curve. All samples were run in duplicate and the average interassay and intra-assay coefficient of variation was <8%. Natural log transformation was applied to normalize raw score distributions of IL-6 values and CRP as distributions were skewed. This is in line with previous papers examining IL-6 and CRP as markers of inflammation [26, 27].
Depressive symptoms
We used the Patient Health Questionnaire-9 (PHQ-9) instrument to measure the presence and severity of depressive symptoms [28]. The PHQ-9 incorporates Diagnostic and Statistical Manual of Mental Disorders-IV depression diagnostic criteria into a brief self-report instrument. The instructions for the scale are as follows: “Over the past 2 weeks how often have you been bothered by any of the following problems?” Possible responses are: not at all (0), several days (1), more than half the days (2), and nearly every day (3). Items include having little or no interest in doing things, poor appetite or overeating, and trouble concentrating on things. Scores are summed across all nine items (α = .85).
Standard control variables
Control variables were collected at screening: age (continuous), sex (male, female), body mass index (BMI; weight in kilograms/height in meters), depressive symptoms, and annual income. Annual income was measured across four categories: (a) less than $2,000 per year, (b) between $2,001 and $20,000 per year, (c) between $20,0001 and $50,000 per year, and (d) between $50,001 and $100,000 per year.
Data Analysis
Statistical analyses were conducted using SPSS (version 24; IBM, Armonk, NY). From the original sample of 90 participants, we excluded 1 participant who reported that they were taking antihistamines, given their ability to affect immune function. Four participants had CRP values greater than or equal to 10 mg/L (<10.5 mg/L). We opted to keep these individuals in our analyses given that they were less than 3 SD above the mean in the sample. Thus, our analytic sample for reported analyses includes 89 community members. Continuous covariates were centered with z-scores before being used in analyses. Participant sex was coded as male = 1 and female = 2. Initial Pearson product-moment correlation analyses were performed to determine bivariate associations between ACEs, sense of belonging, demographic variables, BMI, and circulating levels of IL-6 and CRP. Before conducting our central regression analyses, we examined the distribution of both ACEs and sense of belonging to the community. These predictors were not highly skewed. Next, linear regressions were utilized to conduct the main analyses. We first examined associations between ACEs and IL-6 and CRP and sense of belonging to the tribal community and IL-6 and CRP. In these models, age, sex, BMI, depressive symptoms, and annual income were entered in Step 1 as covariates. Next, we created an interaction term between ACEs and sense of belonging to the tribal community to utilize as a predictor of both IL-6 and CRP. To probe interactions, we conducted simple slopes analyses at 1 SD above and below the mean of community belonging in this sample. We also used the Johnson–Neyman technique [29] to identify specific values of community belonging for which the association between ACEs and markers of inflammation is statistically significant in this sample.
Results
The sample was 50% female and the mean age was 37.55 (SD = 15.74). The mean ACEs score was 2.41 (SD = 2.24). Descriptive statistics for the main variables of interest and covariates are listed in Table 1 and correlations between main variables of interest are reported in Table 2.
Table 1.
Descriptive statistics
| Mean | SD | Possible range | Observed range | |
|---|---|---|---|---|
| Age | 37.55 | 15.74 | 19–80 | |
| Sex (% female) | 50% | |||
| C-reactive protein (CRP) | 3.97 | 2.90 | 0.20–10.40 | |
| Interleukin-6 (IL-6) | 2.82 | 2.06 | 0.06–9.17 | |
| Adverse childhood experiences | 2.41 | 2.24 | 0–10 | 0–9 |
| Belonging to tribal community | 2.81 | 2.06 | 0–6 | 1–6 |
| Body mass index | 30.71 | 7.32 | 17.13–44.15 | |
| Depressive symptoms (PHQ-9) | 0–27 | 0–24 | ||
| Annual income (category range: 1–4) | 2.50 | 0.84 | 1–4 | 1–4 |
PHQ-9 Patient Health Questionnaire-9; SD standard deviation.
Table 2.
Correlation matrix for key variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Age | – | .13 | −.02 | .05 | −.17 | −.11 | .18 | .01 | .18 |
| 2. Gender | – | .21* | −.04 | −.10 | .04 | .09 | −.08 | −.08 | |
| 3. Depressive symptoms | – | .07 | −.08 | .30** | .10 | −.12 | −.09 | ||
| 4. Body mass index | – | .08 | −.04 | .05 | .12* | .25** | |||
| 5. Annual income | – | −.05 | −.06 | −.03 | −.10 | ||||
| 6. Adverse childhood experiences | – | −.26** | .14 | .12 | |||||
| 7. Sense of belonging to tribal community | – | −.26** | −.18 | ||||||
| 8. C-reactive protein | – | .31** | |||||||
| 9. Interleukin-6 | – |
Gender: Male = 1, Female = 2.
*p < .05 (two tailed). **p < .01 (two tailed).
ACEs and Inflammatory Markers
Separate linear regressions with the described covariates indicated that ACEs were not a significant predictor of IL-6 or CRP (B =.08, t[83] = 0.75, p = .45 and B = .14, t[83] = 1.28, p = .21, respectively).
Belonging to the Tribal Community and Inflammatory Markers
Separate linear regressions with the described covariates indicated that community belonging was a significant predictor of IL-6 and a marginally significant predictor of CRP (and B = −.26, t[83] = −2.54, p = .01 and B = .20, t[83] = −1.89, p =.06, respectively).
ACEs by Belonging to the Tribal Community Predicting Inflammatory Markers
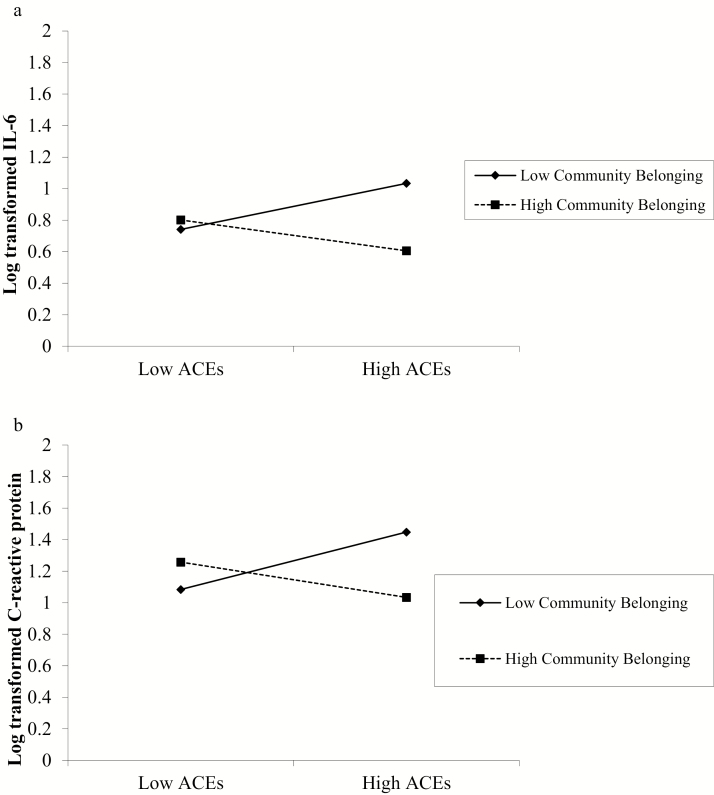
Finally, in an independent linear regression utilizing the same control variables, we added the interaction term between ACEs and belonging to the tribal community. The interaction term was a significant predictor of both IL-6 and CRP (B = −.37, t[81] = −3.82, p < .001, R2 change = .07 and B = −.29, t[81] = −2.75, p = .01, R2 change = .08, respectively). The patterns of these interactions are displayed in Fig. 1a and b (IL-6 and CRP, respectively).
Fig 1.
Log-transformed (a) interleukin-6 (IL-6) and (b) C-reactive protein (CRP) as a function of reported belonging and connection to the tribal community and number of adverse childhood events (ACEs). Results from linear regression analyses controlling for age, gender, annual income, depressive symptoms, and body mass index.
Simple slopes analyses revealed that the association between ACEs and IL-6 was statistically significant for community members with low levels of community belonging (B = .15, t[85] = 2.06, p < .05) but not for community members with high reported community belonging (B = −.10, t[85] = −1.39, p = .17). Similarly, the association between ACEs and CRP was significant for community members with low levels of belonging to the community (B = .16, t[85] = 2.20, p < .05) but not for community members with high reported community belonging (B = −.11, t[85] = −1.58, p = .12). More specifically, ACEs were associated with higher levels of IL-6 and CRP for individuals with low reported sense of belonging to their community. The Johnson–Neyman technique [29] revealed that the association between ACEs and IL-6 was statistically significant for community members with a reported sense of community belonging between 1 and 3.63, while the association between ACEs and CRP was statistically significant for community members with a reported sense of community belonging between 1 and 3.28.
Discussion
To our knowledge, this is the first investigation to examine the relationships between adverse childhood events, sense of belonging and identification with one’s tribal community and its practices, and levels of immune system inflammation. The mean ACEs score in this sample was 2.41 (SD = 2.24), a slightly lower average than that observed in a previous investigation focused on AI women. In this research, the mean ACEs score for AI women was 3.92 [30]. Interestingly, the relationship between adverse childhood events and immune system inflammation observed previously was not present in this sample of community members of the Blackfeet Nation. Instead, the relationship between adverse childhood events and markers of immune system inflammation was moderated by individuals’ current sense of belonging and identification with their tribal community. Specifically, the association between ACEs and inflammation was only statistically significant for individuals who reported low levels of sense of belonging to their community. It is important to note that ACEs was not a significant predictor of one’s report of their current sense of belonging and identification with their tribal community and its values and practices.
The pattern of these findings suggests that in this sample of Blackfeet community members, the relationship between ACEs and inflammation is not evident for individuals who report high levels of belonging to their current community. This lack of an association indicates that identification with the tribal community may be capable of offsetting the risk profile previously associated with a high number of ACEs—high levels of immune system inflammation [11, 31, 32]. As such, belonging to the tribal community could act as a resilience factor for individuals who have faced early-life adversity. These findings are in line with a large body of work highlighting the importance of ethnic identification for minority groups and its potential to dampen the negative effects of stress [18, 19]. They also extend previous work indicating the particular importance of belonging to the larger community for AI populations [20, 33].
The current data did not explore coping strategies, and this will be an important line of future research. Individuals who have higher levels of belonging to the larger tribal community may be able to cope more efficiently with the trauma they faced in their childhood and with current life stress. Further, we did not have measures of important health behaviors that may in part contribute to the reported findings. It is possible that a greater connection to the community and its associated practices and values may positively affect health behaviors including sleep, diet, physical activity, and substance use, particularly for individuals who experienced a high amount of adversity during their childhood. This is an important future direction given that these behaviors in turn affect circulating levels of markers of immune system inflammation. In addition, it will be important to understand how ACEs and connection to the tribal community affect daily life patterns of these factors.
There are important limitations to note. First, this research is cross sectional in design and so causality cannot be inferred. While the measure of community belonging was developed based on community input, it is not a validated instrument. Finally, the associations observed in this investigation only reflect the sample of 90 community members and cannot be generalized to the entire Blackfeet Nation at large. For example, generalizability may be limited based on the recruitment approach used in this study. Since recruitment took place at a community health fair, it is possible that the participants in this sample are more interested in their health and improving their health compared to the general population on the reservation. Future research should aim for a larger more representative sample.
Given that belonging and identification with the community appears to positively affect the association between early-life adversity and immune system inflammation in adulthood, it could be viewed as a source of resilience. Future work should aim to understand the factors that contribute to an individual’s sense of connection to their tribal community, and the findings from this research should then be utilized to inform evidence-based community-driven interventions.
Acknowledgments
Funding Research reported in this publication was supported by the National Institute of General Medical Sciences of the National Institutes of Health under award numbers P20GM104417, P20GM103474, S06GM110777, and U54GM115371. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Compliance with Ethical Standards
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards Authors John-Henderson, Henderson-Matthews, Ollinger, Racine, Gordon, Higgins, Horn, Reevis, Running Wolf, and Rynda-Apple declare that they have no conflict of interest.
Authors’ Contributions: N.A.J.-H. and A.R.-A. analyzed the data and wrote the manuscript. B.H.-M., S.R.O., J.R., M.R.G., A.A.H., W.C.H., S.A.R., J.A.R.W. and D.G. collected the data and helped with the interpretation of the data and preparation of the manuscript.
Ethical Approval: All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional review boards and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
References
- 1. Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. JAMA. 2007;298:1685–1687. [DOI] [PubMed] [Google Scholar]
- 2. Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: moving toward a model of behavioral and biological mechanisms. Psychol Bull. 2011;137:959–997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Steptoe A, Kivimäki M. Stress and cardiovascular disease: an update on current knowledge. Annu Rev Public Health. 2013;34:337–354. [DOI] [PubMed] [Google Scholar]
- 4. Reiser SJ, McMillan KA, Wright KD, Asmundson GJ. Adverse childhood experiences and health anxiety in adulthood. Child Abuse Negl. 2014;38:407–413. [DOI] [PubMed] [Google Scholar]
- 5. Ramiro LS, Madrid BJ, Brown DW. Adverse childhood experiences (ACE) and health-risk behaviors among adults in a developing country setting. Child Abuse Negl. 2010;34:842–855. [DOI] [PubMed] [Google Scholar]
- 6. Cambron C, Gringeri C, Vogel-Ferguson MB. Physical and mental health correlates of adverse childhood experiences among low-income women. Health Soc Work. 2014;39:221–229. [DOI] [PubMed] [Google Scholar]
- 7. Crouch E, Strompolis M, Bennett KJ, Morse M, Radcliff E. Assessing the interrelatedness of multiple types of adverse childhood experiences and odds for poor health in South Carolina adults. Child Abuse Negl. 2017;65:204–211. [DOI] [PubMed] [Google Scholar]
- 8. Monnat SM, Chandler RF. Long term physical health consequences of adverse childhood experiences. Sociol Q. 2015;56:723–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Miller GE, Chen E, Fok AK, et al. . Low early-life social class leaves a biological residue manifested by decreased glucocorticoid and increased proinflammatory signaling. Proc Natl Acad Sci USA. 2009;106:14716–14721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chen M, Lacey RE. Adverse childhood experiences and adult inflammation: findings from the 1958 British birth cohort. Brain Behav Immun. 2018;69:582–590. [DOI] [PubMed] [Google Scholar]
- 11. Danese A, Pariante CM, Caspi A, Taylor A, Poulton R. Childhood maltreatment predicts adult inflammation in a life-course study. Proc Natl Acad Sci USA. 2007;104:1319–1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gouin JP, Caldwell W, Woods R, Malarkey WB. Resilience resources moderate the association of adverse childhood experiences with adulthood inflammation. Ann Behav Med. 2017;51:782–786. [DOI] [PubMed] [Google Scholar]
- 13. Logan-Greene P, Green S, Nurius PS, Longhi D. Distinct contributions of adverse childhood experiences and resilience resources: a cohort analysis of adult physical and mental health. Soc Work Health Care. 2014;53:776–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zinn H. A People’s History of the United States: 1492 to Present. New York, NY: Harper Collins Publishers; 2000. [Google Scholar]
- 15. Ungar M. Researching and theorizing resilience across cultures and contexts. Prev Med. 2012;55:387–389. [DOI] [PubMed] [Google Scholar]
- 16. Fleming J, Ledogar RJ. Resilience, an evolving concept: a review of literature relevant to aboriginal research. Pimatisiwin. 2008;6:7–23. [PMC free article] [PubMed] [Google Scholar]
- 17. Phinney JS. Ethnic identity in adolescents and adults: review of research. Psychol Bull. 1990;108:499–514. [DOI] [PubMed] [Google Scholar]
- 18. Greene ML, Way N, Pahl K. Trajectories of perceived adult and peer discrimination among Black, Latino, and Asian American adolescents: patterns and psychological correlates. Dev Psychol. 2006;42:218–236. [DOI] [PubMed] [Google Scholar]
- 19. Potochnick S, Perreira KM, Fuligni A. Fitting in: the roles of social acceptance and discrimination in shaping the daily psychological well-being of Latino youth. Soc Sci Q. 2012;93:173–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. LaFromboise TD, Hoyt DR, Oliver L, Whitbeck LB, Kim IJ, Lorion RP. Family, Community and School influences on resilience among American Indian Adolescents in the Upper Midwest. J Comm Psychol. 2006;34:193–209. [Google Scholar]
- 21. Espey DK, Jim MA, Cobb N, et al. . Leading causes of death and all-cause mortality in American Indians and Alaska Natives. Am J Public Health. 2014;104(suppl 3):S303–S311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bowen KS, Uchino BN, Birmingham W, Carlisle M, Smith TW, Light KC. The stress-buffering effects of functional social support on ambulatory blood pressure. Health Psychol. 2014;33:1440–1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Janicki Deverts D, Cohen S, Doyle WJ. Dispositional affect moderates the stress-buffering effect of social support on risk for developing the common cold. J Pers. 2017;85:675–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Takizawa T, Kondo T, Sakihara S, Ariizumi M, Watanabe N, Oyama H. Stress buffering effects of social support on depressive symptoms in middle age: reciprocity and community mental health. Psychiatry Clin Neurosci. 2006;60:652–661. [DOI] [PubMed] [Google Scholar]
- 25. Felitti VJ, Anda RF, Nordenberg D, et al. . Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The adverse childhood experiences (ACE) study. Am J Prev Med. 1998;14:245–258. [DOI] [PubMed] [Google Scholar]
- 26. John-Henderson NA, Marsland AL, Kamarck TW, Muldoon MF, Manuck SB. Childhood socioeconomic status and the occurrence of recent negative life events as predictors of circulating and stimulated levels of interleukin-6. Psychosom Med. 2016;78:91–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. John-Henderson NA, Stellar JE, Mendoza-Denton R, Francis DD. Socioeconomic status and social support: social support reduces inflammatory reactivity for individuals whose early-life socioeconomic status was low. Psychol Sci. 2015;26:1620–1629. [DOI] [PubMed] [Google Scholar]
- 28. Spitzer RL, Williams JB, Kroenke K, Hornyak R, McMurray J. Validity and utility of the PRIME-MD patient health questionnaire in assessment of 3000 obstetric-gynecologic patients: the PRIME-MD Patient Health Questionnaire Obstetrics-Gynecology Study. Am J Obstet Gynecol. 2000;183:759–769. [DOI] [PubMed] [Google Scholar]
- 29. Rast P, Rush J, Piccinin A, Hofer SM. The identification of regions of significance in the effect of multimorbidity on depressive symptoms using longitudinal data: an application of the Johnson-Neyman technique. Gerontology. 2014;60:274–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mersky JP, Janczewski CE. Racial and ethnic differences in the prevalence of adverse childhood experiences: findings from a low-income sample of U.S. women. Child Abuse Negl. 2018;76:480–487. [DOI] [PubMed] [Google Scholar]
- 31. Pollitt RA, Kaufman JS, Rose KM, Diez-Roux AV, Zeng D, Heiss G. Early-life and adult socioeconomic status and inflammatory risk markers in adulthood. Eur J Epidemiol. 2007;22:55–66. [DOI] [PubMed] [Google Scholar]
- 32. Taylor SE, Lehman BJ, Kiefe CI, Seeman TE. Relationship of early life stress and psychological functioning to adult C-reactive protein in the coronary artery risk development in young adults study. Biol Psychiatry. 2006;60:819–824. [DOI] [PubMed] [Google Scholar]
- 33. Hill DL. Sense of belonging as connectedness, American Indian worldview, and mental health. Arch Psychiatr Nurs. 2006;20:210–216. [DOI] [PubMed] [Google Scholar]