Highlights
-
•
Identifying at-risk students for binge-eating and alcohol use disorder is priority.
-
•
Negative urgency relationship to risky drinking and binge-eating is key.
-
•
High levels of risky drinking, binge-eating, and both were identified.
-
•
Effects were particularly strong related to male students’ binge-eating.
-
•
Important to identify key mechanisms of binge-eating and drinking in students.
Keywords: Negative urgency, Binge-eating, Risky drinking, Alcohol problems, Hazardous drinking, Students
Abstract
Identifying students at risk of developing binge-eating and alcohol use disorders is a priority in the United Kingdom (UK). Although relationships between negative urgency (impulsive behavior during times of negative emotion), risky drinking, and binge-eating have been established in students from other countries, these links have yet to be replicated in male and female UK students. UK students aged 18–30 (n = 155) completed the: (1) the Urgency, Pre-meditation, Perseverance, Sensation Seeking (UPPS-P) negative urgency subscale; (2) Alcohol Use Disorders Identification Test (AUDIT); and (3) Binge-Eating Scale (BES). For categorical analysis, participants were assigned to one of four groups as a function of AUDIT and BES clinical cut-off scores: (1) no risk (28%); (2) risky drinkers (47%); (3) binge-eaters (6%); and (4) risky drinkers + binge-eaters (19%). For dimensional analysis, across students with non-zero AUDIT and BES scores (n = 141), BES, AUDIT, gender, and their interactions were entered as predictors in the same block of a regression. UPPS-P negative urgency was the dependent variable. Categorical results indicated that binge-eaters with and without risky drinking endorsed significantly higher negative urgency than students with no risk. Dimensional results showed that although higher BES and AUDIT scores were positively linked to higher negative urgency, but only the BES was significantly associated. Furthermore, BES shared substantially more variance with negative urgency than the AUDIT, and the BES-negative urgency relationship was stronger in male students than female students. High risk students may benefit the most from interventions that help regulate negative emotion.
1. Introduction
A growing number of students are diagnosed with binge-eating disorder (BED), which has a higher lifetime prevalence than other eating disorders (Guerdjikova et al., 2017, Hudson et al., 2007), and a lower gender discrepancy in diagnosis, with 40% of BED diagnosed in men (Hay et al., 2015, Westerberg and Waitz, 2013). BED is characterized by binge-eating without compensation (i.e. purging), accompanied by feelings of loss of control, distress, and intense negative emotions (DSM-5; American Psychiatric Association, 2013). Although BED is distinguishable from alcohol use disorder (AUD), both problems reflect substance over-consumption, have been suggested to share some key features such as impulsivity, neuroticism, and reward dysfunction, and have the potential for overlapping negative emotional (e.g., anxiety, depression, guilt) and physical harm (e.g., gastrointestinal and sleep problems) (see for example: Bujanda, 2000, Ferriter and Ray, 2011, Olguin et al., 2017, Rolland et al., 2017, Schulte et al., 2016).
Problem alcohol consumption is common for students residing in the United Kingdom (UK), with 70–85% reporting weekly binge-drinking and 63–84% endorsing hazardous drinking; moreover, the gender gap in risky alcohol use appears to be closing, with women catching up to men (Davoren, Demant, Shiely, & Perry, 2016). Although women and men aged 16–24 report disconcerting binge-drinking rates in England (26% and 29% respectively), alcohol-related deaths are 2:1 male to female (15 compared to 7 per 100,000; National Health Survey (NHS), 2019). Alarmingly, between 2007 and 2017, there was a 16% increase in UK alcohol-specific deaths (National Health Survey (NHS), 2019).
It is estimated that up to half of individuals who abuse alcohol also engage in problematic binge-eating behaviors (Bahji et al., 2019, Gregorowski et al., 2013, Ulfvebrand et al., 2015). Although a multilevel approach (Penny & Armstrong-Hallam, 2010) advocates identifying those at risk for developing multiple problems and intervening based on their specific needs, there appears to be a dearth of appropriate screenings for eating disorders in the UK (BEAT, 2014). Early identification of AUD and BED is crucial, and since over 50% of UK patients wait for 3 + months to begin mental health treatment (Mind, 2013), development of effective screening measures should be prioritized to facilitate early intervention.
Heightened negative urgency, or the tendency to behave impulsively when experiencing (and/or attempting to avoid) negative emotions, appears to characterize both problem eating and drinking behaviors and may be an effective screening tool for AUD and BED vulnerability (Bardone-Cone et al., 2016, Cyders, 2013, Fischer et al., 2004, Fischer et al., 2007, Fischer et al., 2008, Jones et al., 2014, Lynam et al., 2007, Verdejo-García et al., 2007). UK students who experience negative consequences from their drinking endorse higher levels of negative urgency (Jones et al., 2014). As such, students higher in negative urgency may be at risk of both AUD and BED, as both alcohol and food may be used as a maladaptive method to cope with negative emotions (Fischer et al., 2004). Within student samples in the United States (US): (1) women with heightened negative urgency endorse greater symptoms of BED and substance use disorders (Fischer, Settles, Collins, Gunn, & Smith, 2012); (2) men and women may share similar levels of negative urgency (Cyders, 2013); and (3) negative urgency is linked to both problem drinking and eating behaviors (Dir, Karyadi, & Cyders, 2013). As AUD and eating disorders show high rates of comorbidity (Khaylis et al., 2009, Mikheeva and Tragesser, 2016, Sinha et al., 1996, Stewart et al., 2006), negative urgency may be a common mechanism by which young adults increase risk for both disorders (Luce et al., 2007, von Ranson et al., 2002).
Although relationships between negative urgency, risky drinking, and binge-eating have been established in students from other countries, and one meta-analysis suggests that heightened negative urgency presents at similar rates for men and women (Coskunpinar & Cyders, 2013), these links have yet to be replicated in male and female students in the UK. Additionally, although trends seem to be shifting, currently, men still consume more alcohol than women in the UK, and women are more likely to develop BED. Still, it is unclear if there may be gender differences in the degree to which negative urgency shares variance with risky drinking and binge-eating behaviors in UK students, which in turn will impact the success of employing negative urgency as a screening tool for AUD/BED vulnerability in the UK. This study aims to replicate prior findings of shared variance between negative urgency, risky drinking, and binge eating within UK students, evaluating gender as a moderator. We hypothesize that higher negative urgency will be positively associated with AUD and BED symptoms across students of both genders.
2. Materials and methods
2.1. Participants and recruitment
A total of 183 students completed a web-based survey advertised via the University of Nottingham’s Research Participation Scheme and social media announcements posting access to the online link. In order to be included in the study, participants were required to be aged 18–30 years old, a student at a UK-based University and residing in the UK. Twenty-eight (15.3%) participants were excluded due to not residing in the UK (n = 19), not being a student (n = 4) or being aged over 30 (n = 5), leaving a final sample of 155 participants: 18–30 year-olds (M = 20.28, SD = 1.68), 71.6% female (n = 111) and 28.4% male (n = 44).
2.2. Measures
Negative urgency. The Urgency, Pre-meditation, Perseverance, Sensation Seeking (UPPS-P) Scale (Lynam et al., 2007) contains 59 items to measure impulsivity traits. This study only collected data on the negative urgency subscale (Cronbach’s alpha = 0.95), as it has been linked to alcohol abuse and binge eating (e.g., Fischer et al., 2012, VanderVeen et al., 2016). Items relate to regretted impulsive behavior, or lack of self-control, deriving from emotional distress (e.g., “Sometimes when I feel bad, I can’t seem to stop what I am doing even though it is making me feel worse.”). Scores are based on a scale from 1 (agree strongly) to 4 (disagree strongly).
Alcohol use. The Alcohol Use Disorders Identification Test (AUDIT; Saunders, Aasland, Babor, de la Fuente, & Grant, 1993) contains ten questions used to generate consumption (e.g., “How often do you have six or more drinks?”), harm (e.g., “How often during the last year have you had a feeling of guilt or remorse after drinking?”) and dependence (e.g., “How often during the last year have you found you were not able to stop drinking once you started?”) subscales and a total score. Items are rated on a 5-point Likert scale from 0 (“never”) to 4 (“4 or more times a week”), with higher scores indicating a greater level of alcohol use. A score of 8 or more indicates an ‘at risk’ drinker (Babor, Higgins-Biddle, Saunders, & Monteiro, 2001). Cut-offs applied to this sample were: 0–7 low or no risk, 8–15 increasing risk, 16–19 high risk and 20–40 possible dependence (Cronbach’s alpha = 0.86).
Binge-eating. The Binge-Eating Scale (BES; Gormally, Black, Daston, & Rardin, 1982) is a 16-item questionnaire assessing presence and severity of BED behaviors, emotions, and cognitions (Burton et al., 2015, Greeno et al., 1995, Ricca et al., 2000) (e.g., “Usually about once a month, I eat such a quantity of food, I end up feeling very stuffed”). Individual items have three to four responses, which are rated on a continuum from 0 (no severity of binge-eating symptoms), to 3 (severe binge-eating symptoms). Based on the BES total score, which ranges from 0 to 46, participants were categorized into three groups according to established severity cut-offs, which are: none (score < 17), mild-moderate (score of 18–26), and severe (score > 27; Marcus, Wing, & Hopkins, 1988). The BES was used as a screening measure to classify those with scores greater than or equal to 17 as “binge-eaters” (Cronbach’s alpha = 0.88).
2.3. Procedure
Ethical approval for the study was obtained from the Faculty Ethics Committee. The survey was created using Qualtrics (Qualtrics.com). Informed consent was obtained from all participants. Participants completed the survey (average time = 20 minutes) and were debriefed and signposted to appropriate support services.
2.4. Statistical analysis
Statistical analyses were performed in SPSS Version 24. Categorical and dimensional analyses were computed, with categorical analyses based on established clinical cut-offs to evaluate percentage of participants meeting criteria for comorbid binge-eating and drinking problems. Dimensional analyses evaluated relationships between binge-eating/drinking and negative urgency across the entire sample who had non-zero values for all measures.
Categorical. Risk groups were produced for binge-eating, alcohol use and presence of both based on BES and AUDIT cut-off scores. A one-way analysis of variance (ANOVA) tested differences on UPPS-P negative urgency between four groups: (1) no risk of binge-eating or alcohol problems (BES < 17 and AUDIT < 8; n = 44); (2) risky drinkers (AUDIT > 8 but BES < 17; n = 73); (3) binge-eaters (BES > 17 but AUDIT < 8; n = 9), and (4) risky drinkers + binge-eaters (BES > 17 and AUDIT > 8; n = 29). Levene’s test evaluated the homogeneity of variance assumption, while Scheffe post-hoc tests were conducted to follow-up the overall F test. Partial η2 is reported as a measure of effect size.
Dimensional. Shapiro-Wilk tests were computed to assess the normality of distributions for men and women separately. A total of 14 participants (13F, 1M) endorsed an AUDIT score of ‘0′ and were therefore removed from analysis. BES distributions did not approach normality for men (W = 0.94, p = .02) or women (W = 0.92, p < .001), while AUDIT distributions approached normality for men (p = .41) but not women (W = 0.94, p < .001). Square-root transformations [SQRT(variable + 1] were therefore applied to BES and AUDIT scores for the remaining 95 participants (all W tests p > .22). Negative urgency scores were normally distributed for both genders and required no transformation. The following independent variables were entered in the same step of a multiple regression to predict negative urgency: BES, AUDIT, gender, BES*gender, AUDIT*gender, BES*AUDIT, and BES*AUDIT*gender. All variables were standardized prior to regression entry and calculation of interaction terms. Residuals were relatively uncorrelated (Durbin-Watson = 1.98) and normally distributed (per visual histogram inspection). No multivariate outliers (+/- 3 standard deviations) were detected. R2 is reported as a measure of effect size.
3. Results
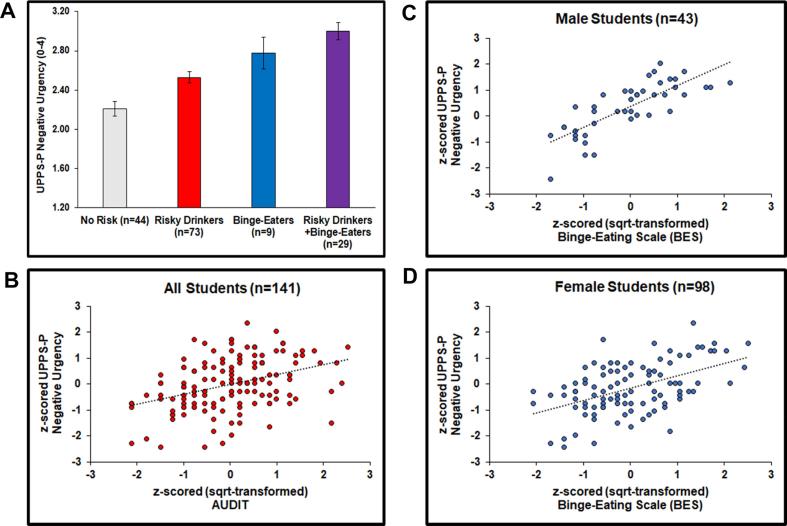
Categorical. Levene’s test indicated that groups showed similar variances for negative urgency (p = .46). Fig. 1A demonstrates that groups differed on negative urgency, F(3, 151) = 16.00, p < .001, partial η2 = 0.24, and Scheffe tests demonstrated that risky drinkers + binge-eaters endorsed higher urgency scores than risky drinkers and those with no risk (both p < .001). Binge-eaters also reported higher urgency scores than those with no risk (p = .02) but did not differ from risky drinkers with (p = .70) or without binge-eating (p = .56). Finally, risky drinkers endorsed higher urgency scores than students with no risk (p = .01).
Fig. 1.
(A) Categorical analysis: Group differences in negative urgency. Bars reflect one standard error. (B) Dimensional analysis: Relationship between Alcohol Use Disorders Identification Test (AUDIT) and negative urgency across male and female students. (C) Dimensional analysis: Relationship between Binge-Eating Scale (BES) and negative urgency in male students. (D) Dimensional analysis: Relationship between Binge-Eating Scale (BES) and negative urgency in female students.
Dimensional. The overall regression model significantly related to negative urgency, F(7, 133) = 13.78, p < .001, Adjusted R2 = 0.39), and Fig. 1B illustrates that higher AUDIT scores (β = 0.14, t = 1.88, p = .06) was positively related with higher negative urgency scores, although this was not significant. Main effects of BES scores (β = 0.54, t = 7.39, p < .001) and gender (β = −0.26, t = −3.33, p < .01) were qualified by a BES*gender interaction (β = −0.18, t = −2.26, p = .03), which showed that the relationship between BES and urgency was stronger in men (R2 = 0.61; Fig. 1C) than women (R2 = 0.25; Fig. 1D). In contrast, BES*AUDIT (β = −0.05, p = .51), AUDIT*gender (β = 0.11, p = .18, and BES*AUDIT*gender (β = 0.05, p = .55) did not contribute significant variance to urgency.
4. Conclusions
This is the first study to explore relationships between negative urgency, risky drinking, and binge-eating in UK students. With respect to categorization of AUD/BED risk, two-thirds of our sample screened positive for AUD, one-fourth screened positive for BED, and almost one-fifth screened positive for comorbid AUD/BED. Pure BED and comorbid AUD/BED groups endorsed higher levels of negative urgency than the no-risk group. Negative urgency was only significantly positively correlated with BES, there was a positive association with AUDIT but this was not significant (p = .06). This was partially consistent with our hypothesis, and BES shared more variance with negative urgency than AUDIT. Furthermore, the BES-negative urgency relationship shared significantly more variance within male than female students. Taken together, our findings replicate prior work suggesting that heightened negative urgency is associated with (and may underlie) problematic relationships with alcohol and food (Anestis et al., 2011, Fischer et al., 2012, Pearson et al., 2012); we also extend this work to show that negative urgency may be a stronger mechanism involved in binge-eating behaviors within male students. As this is a cross-sectional self-report study with UK University students, longitudinal research including more implicit assessment within a clinical population is warranted to determine whether heightened negative urgency predicts future development of binge-eating behaviors, especially in young men. Additionally, self-report clinical assessment data could be compared with behavioral data on impulsivity in future studies.
Results suggest that early screening for negative urgency in UK University students may have some benefits. For example, if further testing established a reliable cut-off score used in screening to flag a consultation with a mental health professional, further assessment and short-term therapy may allow vulnerable students to learn new skills to cope with stress and aversive mood states. Our data suggest this may be particularly beneficial for male students, although further research is needed to support such implementation. In addition to the survey-based assessments available, more implicit tools to detect higher levels of negative urgency could be preventative for those who are vulnerable. Interventions targeting adaptive regulation of negative emotion for those vulnerable to problems with alcohol and food can result in decreased clinical symptoms and successful long-term recovery (Patton et al., 2014, Reas et al., 2000, Rodgers et al., 2014). Understanding the function of maladaptive eating and drinking behaviors may result in a more effective intervention (Jones et al., 2014). Compassion-focused therapy (CFT; Kelly et al., 2014, Gilbert, 2005, Gilbert, 2009) could be a useful intervention tool for students engaging in binge-eating. As CFT improves self-compassion in early stages of eating disorder treatment (Kelly, Carter, & Borairi, 2014), techniques could be adapted for students to change a self-critical mindset, leading to awareness of the body’s indicators to direct the intake of food (Webb & Hardin, 2016). Engaging with one’s emotions may help reduce negative urgency, and the tendency to escape self-awareness or disengage emotionally during binge-eating.
Acknowledgments
Acknowledgements
We thank Phoebe Nicholas for collecting data for this study.
Declaration of Competing Interest
The authors declare that they have no conflict of interest.
Funding
This research was supported by the William K. Warren Foundation.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.abrep.2020.100274.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders, (DSM-5®). American Psychiatric Pub.
- Anestis M.D., Bagge C.L., Tull M.T., Joiner T.E. Clarifying the role of emotion dysregulation in the interpersonal-psychological theory of suicidal behavior in an undergraduate sample. Journal of Psychiatric Research. 2011;45(5):603–611. doi: 10.1016/j.jpsychires.2010.10.013. [DOI] [PubMed] [Google Scholar]
- Babor T.F., Higgins-Biddle J.C., Saunders J.B., Monteiro M.G. 2nd ed. World Health Organization; Geneva: 2001. The alcohol use disorders identification test (AUDIT): Guidelines for use in primary care. [Google Scholar]
- Bardone-Cone A.M., Butler R.M., Balk M.R., Koller K.A. Dimensions of impulsivity in relation to eating disorder recovery. International Journal of Eating Disorders. 2016;49(11):1027–1031. doi: 10.1002/eat.22579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bahji A., Mazhar M.N., Hudson C.C., Nadkarni P., MacNeil B.A., Hawken E. Prevalence of substance use disorder comorbidity among individuals with eating disorders: A systematic review and meta-analysis. Psychiatry Research. 2019;273:58–66. doi: 10.1016/j.psychres.2019.01.007. [DOI] [PubMed] [Google Scholar]
- BEAT. (2014). Raising awareness at universities. Retrieved on April 1, 2020 at: https://www.beat.co.uk/assets/000/000/827/Universitycampaignsurveyresults_original .pdf?1456223110.
- Bujanda L. The effects of alcohol consumption upon the gastrointestinal tract. The American Journal of Gastroenterology. 2000;95(12):3374–3382. doi: 10.1111/j.1572-0241.2000.03347.x. [DOI] [PubMed] [Google Scholar]
- Burton A.L., Abbott M.J., Modini M., Touyz S. Psychometric evaluation of self-report measures of binge eating symptoms and related psychopathology: A systematic review of the literature. International Journal of Eating Disorders. 2015;49(2):123–140. doi: 10.1002/eat.22453. [DOI] [PubMed] [Google Scholar]
- Coskunpinar A., Cyders M.A. Impulsivity and substance-related attentional bias: A meta-analytic review. Drug and Alcohol Dependence. 2013;133(1):1–14. doi: 10.1016/j.drugalcdep.2013.05.008. [DOI] [PubMed] [Google Scholar]
- Cyders M.A. Impulsivity and the sexes: Measurement and structural invariance of the UPPS-P Impulsive Behavior Scale. Assessment. 2013;20(1):86–97. doi: 10.1177/1073191111428762. [DOI] [PubMed] [Google Scholar]
- Davoren M.P., Demant J., Shiely F., Perry I.J. Alcohol consumption among university students in Ireland and the United Kingdom from 2002 to 2014: A systematic review. BMC Public Health. 2016;16(1):173. doi: 10.1186/s12889-016-2843-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dir A.L., Karyadi K., Cyders M.A. The uniqueness of negative urgency as a common risk factor for self-harm behaviors, alcohol consumption, and eating problems. Addictive Behaviors. 2013;38(5):2158–2162. doi: 10.1016/j.addbeh.2013.01.025. [DOI] [PubMed] [Google Scholar]
- Ferriter C., Ray L.A. Binge eating and binge drinking: An integrative review. Eating Behaviors. 2011;12:99–107. doi: 10.1016/j.eatbeh.2011.01.001. [DOI] [PubMed] [Google Scholar]
- Fischer S., Anderson K.G., Smith G.T. Coping with distress by eating or drinking: Role of trait urgency and expectancies. Psychology of Addictive Behaviors. 2004;18(3):269. doi: 10.1037/0893-164X.18.3.269. [DOI] [PubMed] [Google Scholar]
- Fischer S., Settles R., Collins B., Gunn R., Smith G.T. The role of negative urgency and expectancies in problem drinking and disordered eating: Testing a model of comorbidity in pathological and at-risk samples. Psychology of Addictive Behaviors. 2012;26(1):112. doi: 10.1037/a0023460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischer S., Smith G.T., Annus A., Hendricks M. The relationship of neuroticism and urgency to negative consequences of alcohol use in women with bulimic symptoms. Personality and Individual Differences. 2007;43(5):1199–1209. [Google Scholar]
- Fischer S., Smith G.T., Cyders M.A. Another look at impulsivity: A meta- analytic review comparing specific dispositions to rash action in their relationship to bulimic symptoms. Clinical Psychology Review. 2008;28(8):1413–1425. doi: 10.1016/j.cpr.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert P. Compassion and cruelty: A biopsychosocial approach. In: Gilbert P., editor. Compassion: Conceptualisations, research and use in psychotherapy. Routledge; London: 2005. pp. 9–74. [Google Scholar]
- Gilbert P. Introducing compassion-focused therapy. Advances in Psychiatric Treatment. 2009;15(3):199–208. [Google Scholar]
- Gormally J., Black S., Daston S., Rardin D. The assessment of binge eating severity among obese persons. Addictive Behaviors. 1982;7(1):47–55. doi: 10.1016/0306-4603(82)90024-7. [DOI] [PubMed] [Google Scholar]
- Greeno C.G., Marcus M.D., Wing R.R. Diagnosis of binge eating disorder: Discrepancies between a questionnaire and a clinical interview. International Journal of Eating Disorders. 1995;17(2):153–160. doi: 10.1002/1098-108x(199503)17:2<153::aid-eat2260170208>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- Gregorowski C., Seedat S., Jordaan G.P. A clinical approach to the assessment and management of co-morbid eating disorders and substance use disorders. BMC Psychiatry. 2013;13(1):289. doi: 10.1186/1471-244X-13-289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerdjikova A.I., Mori N., Casuto L.S., McElroy S.L. Binge Eating Disorder. Psychiatric Clinics. 2017;40(2):255–266. doi: 10.1016/j.psc.2017.01.003. [DOI] [PubMed] [Google Scholar]
- Hay P., Girosi F., Mond J.M. Prevalence and sociodemographic correlates of DSM-V eating disorders in the Australian population. Journal of Eating Disorders. 2015;3:19. doi: 10.1186/s40337-015-0056-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson J.I., Hiripi E., Pope H.G., Kessler R.C. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 2007;61(3):348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones K.A., Chryssanthakis A., Groom M.J. Impulsivity and drinking motives predict problem behaviours relating to alcohol use in University students. Addictive Behaviors. 2014;39(1):289–296. doi: 10.1016/j.addbeh.2013.10.024. [DOI] [PubMed] [Google Scholar]
- Kelly A.C., Carter J.C., Borairi S. Are improvements in shame and self- compassion early in eating disorders treatment associated with better patient outcomes? International Journal of Eating Disorders. 2014;47(1):54–64. doi: 10.1002/eat.22196. [DOI] [PubMed] [Google Scholar]
- Kelly N.R., Cotter E.W., Mazzeo S.E. Examining the role of distress tolerance and negative urgency in binge eating behavior among women. Eating Behaviors. 2014;15(3):483–489. doi: 10.1016/j.eatbeh.2014.06.012. [DOI] [PubMed] [Google Scholar]
- Khaylis A., Trockel M., Taylor C.B. Binge drinking in women at risk for developing eating disorders. International Journal of Eating Disorders. 2009;42(5):409–414. doi: 10.1002/eat.20644. [DOI] [PubMed] [Google Scholar]
- Luce K.H., Engler P.A., Crowther J.H. Eating disorders and alcohol use: Group differences in consumption rates and drinking motives. Eating Behaviors. 2007;8(2):177–184. doi: 10.1016/j.eatbeh.2006.04.003. [DOI] [PubMed] [Google Scholar]
- Lynam, D., Smith, G. T., Cyders, M. A., Fischer, S., & Whiteside, S. A. (2007). The UPPS- P: A multidimensional measure of risk for impulsive behavior. Unpublished technical report.
- Marcus M.D., Wing R.R., Hopkins J. Obese binge eaters: Affect, cognitions, and response to behavioral weight control. Journal Consultation of Clinical Psychology. 1988;3:433–439. doi: 10.1037//0022-006x.56.3.433. [DOI] [PubMed] [Google Scholar]
- Mind. (2013). We still need to talk. A report on access to talking therapies. Retrieved on April 1, 2020 at: https://www.mind.org.uk/media/494424/we-still-need-to- talk_report.pdf.
- Mikheeva O.V., Tragesser S.L. Personality features, disordered eating, and alcohol use among college students: A latent profile analysis. Personality and Individual Differences. 2016;94:360–365. [Google Scholar]
- National Health Survey (NHS). (2019). Statistics on alcohol, England, 2019. Retrieved on April 1, 2020 at: https://digital.nhs.uk/data-and-information/publications/statistical/statistics-on-alcohol/2019/part-4.
- Olguin P., Fuentes M., Gabler G., Guerdjikova A.I., Keck P.E., McElroy S.L. Medical comorbidity of binge eating disorder. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity. 2017;22(1):13–26. doi: 10.1007/s40519-016-0313-5. [DOI] [PubMed] [Google Scholar]
- Patton R., Deluca P., Kaner E., Newbury-Birch D., Phillips T., Drummond C. Alcohol screening and brief intervention for adolescents: The how, what and where of reducing alcohol consumption and related harm among young people. Alcohol and Alcoholism. 2014;49:207–212. doi: 10.1093/alcalc/agt165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson M.R., Kite B.A., Henson J.M. The assessment of protective behavioral strategies: Comparing prediction and factor structures across measures. Psychology of Addictive Behaviors. 2012;26(3):573. doi: 10.1037/a0028187. [DOI] [PubMed] [Google Scholar]
- Penny, G. N., & Armstrong-Hallam, S. (2010). Student choices and alcohol matters (SCAM): A multi-level analysis of student alcohol (mis)use and its implications for policy and prevention strategies within universities, cognate educational establishments and the wider community. Report on project funded by the Alcohol and Education Research Council: Grant R07/02. London: Alcohol Education & Research Council. Retrieved on April 1, 2020: http://www.aerc.org.uk/documents/pdfs/finalReports/AERC_FinalReport_0062.pdf.
- Reas D.L., Williamson D.A., Martin C.K., Zucker N.L. Duration of illness predicts outcome for bulimia nervosa: A long-term follow-up study. International Journal of Eating Disorders. 2000;27(4):428–434. doi: 10.1002/(sici)1098-108x(200005)27:4<428::aid-eat7>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- Ricca V., Mannucci E., Moretti S., Di Bernardo M., Zucchi T., Cabras P.L., Rotella C.M. Screening for binge eating disorder in obese outpatients. Comprehensive Psychiatry. 2000;41(2):111–115. doi: 10.1016/s0010-440x(00)90143-3. [DOI] [PubMed] [Google Scholar]
- Rodgers R.F., Paxton S.J., McLean S.A. A biopsychosocial model of body image concerns and disordered eating in early adolescent girls. Journal of Youth and Adolescence. 2014;43(5):814–823. doi: 10.1007/s10964-013-0013-7. [DOI] [PubMed] [Google Scholar]
- Rolland B., Naassila M., Duffau C., Houchi H., Gierski F., André J. Binge eating, but not other disordered eating symptoms, is a significant contributor of binge drinking severity: Findings from a cross-sectional study among French students. Frontiers in Psychology. 2017;8:1878. doi: 10.3389/fpsyg.2017.01878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders J.B., Aasland O.G., Babor T.F., de la Fuente J.R., Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption- II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schulte E.M., Grilo C.M., Gearhardt A.N. Shared and unique mechanisms underlying binge eating disorder and addictive disorders. Clinical Psychology Review. 2016;44:125–139. doi: 10.1016/j.cpr.2016.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R., Robinson J., Merikangas K., Wilson G.T., Rodin J., O'Malley S. Eating pathology among women with alcoholism and/or anxiety disorders. Alcoholism: Clinical and Experimental Research. 1996;20(7):1184–1191. doi: 10.1111/j.1530-0277.1996.tb01109.x. [DOI] [PubMed] [Google Scholar]
- Stewart S.H., Brown C.G., Devoulyte K., Theakston J., Larsen S.E. Why do women with alcohol problems binge eat? Exploring connections between binge eating and heavy drinking in women receiving treatment for alcohol problems. Journal of Health Psychology. 2006;11(3):409–425. doi: 10.1177/1359105306063313. [DOI] [PubMed] [Google Scholar]
- Ulfvebrand S., Birgegard A., Norring C., Hogdahl L., von Hausswolff-Juhlin Y. Psychiatric comorbidity in women and men with eating disorders results from a large clinical database. Psychiatry Res. 2015;230(2):294–299. doi: 10.1016/j.psychres.2015.09.008. [DOI] [PubMed] [Google Scholar]
- VanderVeen J.D., Plawecki M.H., Millward J.B., Hays J., Kareken D.A., O’Connor S., Cyders M.A. Negative urgency, mood induction, and alcohol seeking behaviors. Drug and Alcohol Dependence. 2016;165:151–158. doi: 10.1016/j.drugalcdep.2016.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdejo-García A., Bechara A., Recknor E.C., Pérez-García M. Negative emotion-driven impulsivity predicts substance dependence problems. Drug and Alcohol Dependence. 2007;91(2):213–219. doi: 10.1016/j.drugalcdep.2007.05.025. [DOI] [PubMed] [Google Scholar]
- von Ranson K.M., Iacono W.G., McGue M. Disordered eating and substance use in an epidemiological sample: I. Associations within individuals. International Journal of Eating Disorders. 2002;31(4):389–403. doi: 10.1002/eat.10050. [DOI] [PubMed] [Google Scholar]
- Webb J.B., Hardin A.S. An integrative affect regulation process model of internalized weight bias and intuitive eating in college women. Appetite. 2016;1(102):60–69. doi: 10.1016/j.appet.2016.02.024. [DOI] [PubMed] [Google Scholar]
- Westerberg D.P., Waitz M. Binge-eating disorder. Osteopathic Family Physician. 2013;5(6):230–233. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.