Abstract
Introduction
Young adults have high smoking rates and low utilization of evidence-based smoking cessation strategies. We investigated smoking cessation intentions, strategy use, and socioeconomic predictors of strategy use among young adult smokers (age 18–24) and compared patterns with those of older adults (age 25–64).
Methods
We used a population-based sample from the Population Assessment of Tobacco and Health (PATH) study of young adult (n = 1,881) and older adult (n = 6,366) established smokers of conventional cigarettes at Wave 1 (2013–2014), who were surveyed at Wave 2 (2014–2015). Simple regression analysis compared intentions to quit between age groups. Among Wave 1 smokers who reported a Wave 2 quit attempt (young adults [YA] n = 748; older adults [OA] n = 2,068), bivariate and multinomial logistic regression estimated differences in use of behavioral support, pharmacotherapy, product substitution, and unassisted quit attempts. Interaction terms estimated age-group differences in relationships between predictors and cessation strategy use.
Results
Young adults planned to quit on a longer time frame, expressed lower interest in quitting, and were more confident they would be successful, compared with older adults. Young adults were significantly less likely to use pharmacotherapy (adjusted odds ratio: 0.15; confidence interval: 0.09, 0.24; reference: quitting unassisted). Both groups reported using product substitution (YA: 31.6%; OA: 28.5%), primarily with e-cigarettes, more than any evidence-based cessation strategy. Socioeconomic predictors of cessation strategy use did not differ between age groups.
Conclusions
More research on why young adult smokers underutilize evidence-based cessation support is needed, as are innovative efforts to increase intentions to quit and utilization of cessation assistance.
Implications
Young adulthood is a key transition time for tobacco use, and early cessation substantially reduces the risk of morbidity and mortality from smoking. In the context of high e-cigarette and polytobacco use, this study finds young adults have significantly less intention to quit than older adults and are less likely to use evidence-based cessation strategies to help quit. Innovative methods are needed to increase young adult intentions to quit and use of evidence-based cessation assistance.
Introduction
Despite declining smoking prevalence over the last decade, 14.2% of young adults in the United States between 19 and 28 years old currently smoke conventional cigarettes.1 Young adulthood is a key transition time for tobacco use2 and smoking onset is now more common among young adults than adolescents.3 Early cessation substantially reduces the risk of morbidity and mortality from smoking; quitting before the age of 40 can reduce the risk of death from tobacco-related disease by 90%.4
Many young adult smokers are interested in quitting smoking and make quit attempts.5 Evidence-based smoking cessation strategies are equally as effective for young adults and the general adult population.6 Yet, studies conducted a decade ago found young adults predominantly try to quit without assistance7 and underutilize evidence-based smoking cessation support, including nicotine replacement therapy.8,9 Few studies have compared cessation strategy use between young adults and older adults. For example, compared with older age groups, young adults aged 18–24 had the highest likelihood of unassisted quit attempts,10 the lowest likelihood of receiving and filling smoking cessation medication prescriptions,11 and the lowest likelihood of cessation medication use.8
Given the recent emergence and heavy marketing of noncigarette tobacco and nicotine products including electronic cigarettes (e-cigarettes) to young adult audiences,12–15 the use of these novel products and polytobacco use is increasing in young adulthood.16,17 Although marketing e-cigarettes and other tobacco products as cessation aids is not allowed in the United States,18 many e-cigarette advertisements imply cigarette cessation benefits19 and many smokers trying to quit have turned to e-cigarettes.20 Studies investigating smoking cessation among young adults therefore need to be updated in the context of increasing e-cigarette and polytobacco use.21 Moreover, few studies have investigated sociodemographic predictors of smoking cessation strategy use among young adults. Specifically, a previous study in this area suggests that there is not an educational gradient in trying to quit, meaning that young adults of different educational levels have similar interest in quitting as well as quit attempts.7 With regard to pharmacotherapy use for quitting smoking, another study reported that among young adults, non-Hispanic white young adults were less likely than other young adults to use medication, while more education was consistently associated with a higher likelihood of medication use.8
To update knowledge about young adult cessation in light of recent changes in the tobacco use landscape, we used data from the Population Assessment of Tobacco and Health (PATH) study to compare youth and young adults along three dimensions: (1) intentions to quit smoking, (2) cigarette cessation strategy use, and (3) socioeconomic predictors of cigarette cessation strategy use.
Methods
Participants and Procedures
We used a population-based sample of young adults (age 18–24; n = 1,881) and older adults (age 25–64; n = 6,366) who had regularly smoked conventional cigarettes at Wave 1 of the PATH study and were surveyed at Wave 2 (2014–2015). The PATH study was administered via in-home computer-assisted interviews, and oversampled young adults, tobacco users, and African Americans. Details on the administration of the PATH study have been published elsewhere.22 This study used the PATH study’s Restricted-Use Files and was certified exempt by the University of California, San Francisco Institutional Review Board.
Measures
Tobacco Use
An individual was labeled a “current established smoker” at each wave if they had ever smoked a cigarette, had smoked more than 100 cigarettes in their lifetime, and currently smoked every day or some days at the time of survey administration.
“Current established use” of noncigarette tobacco products was defined as whether a respondent had ever used the product, had used the product fairly regularly, and currently used the product every day or some days at the time of survey administration. Several products were combined due to small sample size. Our final analysis included cigarettes, e-cigarettes, noncigarette combustible tobacco (traditional cigars, filtered cigars, cigarillos, and pipes), smokeless tobacco (chewing tobacco, moist snuff, snus, and dissolvable tobacco), and hookah. We use “tobacco products” to encompass all tobacco and nicotine products, including e-cigarettes, consistent with the US Food and Drug Administration’s regulation of e-cigarettes as a tobacco product.
We examined several indicators of intention to quit at Wave 1: whether a respondent ever planned to quit their tobacco use for good (0, 1); interest in quitting (on a scale of 1 = not interested at all to 10 = extremely interested); intention to quit within a year (among those who reported intending to ever quit for good); and perceived likelihood of success (on a scale of 1 = not at all likely to be successful to 4 = very likely; among those who reported intending to quit in the next 6 months).
At Wave 2, a current user was determined to have made a quit attempt if they reported having tried to quit completely in the last 12 months or tried to reduce or cut back their tobacco use and reported at least one quit attempt in the past 12 months. Individuals who were established users at Wave 1 but were not using at Wave 2 were assumed to have made a quit attempt by the PATH study team (implied by their successful cessation). We referred to this population as having made a PATH-defined cessation attempt.
Tobacco Cessation
In Wave 2, those who made a PATH-defined cessation attempt were then asked the number of times they had attempted to quit any tobacco product in the past year, to which some replied zero. Respondents who reported at least one quit attempt were asked a series of questions about the last time they tried to quit. The PATH study asked about e-cigarette cessation attempts and other tobacco cessation attempts separately. If an established smoker at Wave 1 reported no other current established use of any tobacco product at Wave 1, they were asked exclusively about cessation strategies the last time they tried to quit cigarette smoking at Wave 2. If they were current established users of cigarettes and e-cigarettes in Wave 1, they were asked about cessation strategies for each product separately. If they used two or more “non-e-cigarette” tobacco products, they were asked about their general “tobacco” cessation strategies. For this subset of polytobacco users (weighted percent: 16.52%), we cannot isolate their last “cigarette” cessation attempt. Because this survey design complexity prevents us from isolating the last cigarette cessation attempt for some respondents, we examined the most recent cessation attempt for each respondent, regardless of what tobacco product(s) they were asked about. Thus, our study describes tobacco cessation strategies of cigarette smokers, rather than strictly cigarette cessation strategies. We conducted a robustness check (see Analyses) to test the validity of these estimates for cigarette-only smokers.
Cessation strategies were categorized as behavioral support, nicotine replacement therapy (NRT), prescription drugs, product substitution, and unassisted quitting (see Table 1 for definitions). In accordance with the US Food and Drug Administration (FDA) and clinical practice guidelines of the US Preventative Services Task Force (https://epss.ahrq.gov), we did not classify product substitution as an evidence-based cessation strategy. Due to a limited number of individuals reporting quit attempts using noncigarette combustibles, smokeless tobacco, and hookah, we combined these individuals with those reporting a quit attempt using e-cigarettes. We described individuals as making a quit attempt unassisted if they did not use any evidence-based cessation strategy and did not substitute with another product. We considered an individual who only relied on social support of friends or family to have made a quit attempt unassisted.
Table 1.
Cessation Strategy Definitions
| Behavioral support | Used counseling, telephone help line, books, pamphlets, videos, quit tobacco clinic, class, support group, or web-based program |
| Pharmacotherapya | Used nicotine replacement therapy or prescription drug |
| Nicotine replacement therapy (NRT)a | Used (1) a nicotine patch, (2) gum, (3) lozenge or pill, or (4) inhaler, nasal spray, or other NRT |
| Prescription druga | Used (1) Chantix/Varenicline or (2) Wellbutrin, Zyban, or Bupropion |
| Substitution | Used a different tobacco or nicotine product, including (1) cigarettes, (2) e-cigarettes, (3) cigars, (4) pipes, (5) smokeless tobacco, or (6) hookah |
| Social support | Relied on the support of friends and family to help |
| Unassisted | Did not use behavioral support, pharmacotherapy, or product substitution |
aEvidence-based cessation strategy.
Covariates
Socioeconomic and tobacco use characteristics were measured in Wave 1. Measures included female sex (reference: male), race and ethnicity (non-Hispanic African American or Black, Latinx or Hispanic, and Other race; reference: non-Hispanic White), and lesbian, gay, bisexual, or other nonheterosexual sexual orientation (“LGB+,” reference: heterosexual). We measured socioeconomic characteristics using two measures: achievement of at least a high school education (else, not a high school graduate/GED) and financial instability (unable to pay important bills on time in the past 30 days because of shortage of money). Urban residence (as defined by the PATH study) was also included (reference: nonurban). We included a measure of whether an individual was a polytobacco user (established use of a noncigarette tobacco product at Wave 1) and the number of cigarettes smoked per day at Wave 1.
Analyses
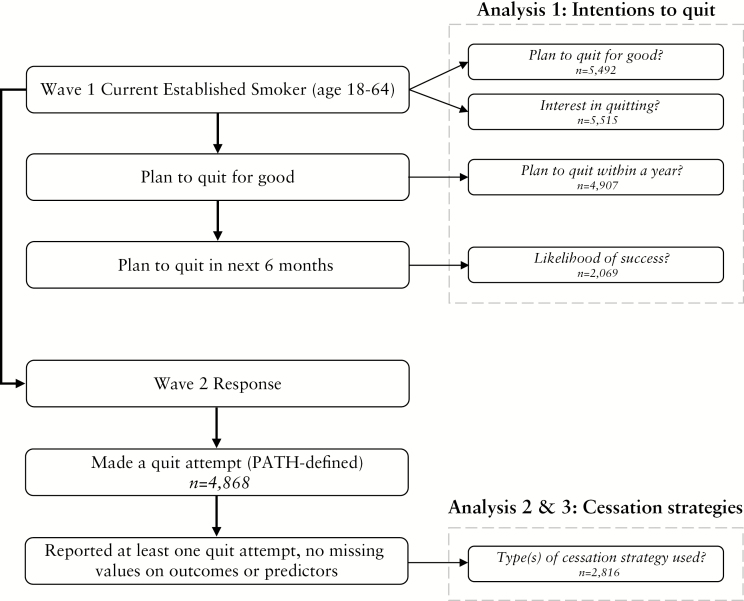
Sample selection and sample size for each analysis are reported in Figure 1. Our first set of analyses compared intentions to quit reported by young adult and older adult cigarette smokers at Wave 1. We used logistic (for binary variables), multiple logistics (for categorical variables; categories ≤ 5), and ordinary least squares (for continuous variables; categories ≥ 6) regression to estimate age-group differences in planning to quit, interest in quitting, time frame for quitting, and perceived likelihood of success.
Figure 1.
Sample size for each analysis, by outcome variable. Wave 1 current established smokers were asked whether they plan to quit for good and their level of interest in quitting. Those who planned to quit for good were asked when they planned to quit, and those who planned to quit within the next 6 mo were asked to report their perceived likelihood of success.
Our second set of analyses used simple bivariate regression to compare cessation strategy use between young adult and older adult Wave 1 smokers. Analyses were conducted using the 2,816 respondents who had no missing data for any of the Wave 1 covariates and Wave 2 cessation strategy variables (young adults [YA]: 748; older adults [OA]: 2,068).
In a third set of analyses, we used multinomial logistic regression to predict the extent to which age group, socioeconomic characteristics, and tobacco use patterns explained use of the following cessation strategies for young and older adults: behavioral support alone, pharmacotherapy alone, product substitution alone, and two or more strategies compared with the base outcome (an unassisted cessation attempt). To determine whether the relationship between Wave 1 characteristics and Wave 2 cessation strategy use varied across age groups, we introduced an interaction term between each predictor and age group (young adult vs. older adult) in a series of fully adjusted multinomial logistic regression models.
As a robustness check, we replicated the bivariate regression analyses using individuals who were established users of only cigarettes at Wave 1. This check served two purposes. First, it provided a clean set of models where the cessation strategy reports referred to cigarette cessation specifically. Second, it helped to identify whether any observed differences in strategy use by age were driven by differences in polytobacco use prevalence between age groups or some other factors that potentially differ with age. Sample size constraints precluded us from reporting cigarette smoker only results for the multinomial logistic regression models.
All data cleaning and analyses were conducted using Stata 15. Descriptive statistics including cessation rates and quit attempt strategies were weighted using Wave 2 respondent-level sample weights (provided by the PATH study) that adjust for loss to follow-up. Statistical tests were weighted with Wave 2 replicate weights using the brr Stata command for balanced repeated replication.
Results
Sample Description
At Wave 2, 84.5% of young adult and 89.4% of older adult Wave 1 established cigarette smokers were still established smokers and 88.9% of young adult and 92.4% of older adult established smokers at Wave 1 were still established users of at least one tobacco product. A total of 68.5% of young adult and 56.5% of older adult Wave 1 cigarette smokers reported having made a quit attempt in the past year at Wave 2. Of those who reported a quit attempt (n = 4,868), 81.2% of young adults and 77.4% of older adults were still smoking cigarettes at Wave 2. Among Wave 1 cigarette smokers, two fifths of young adults (39.9%) and one fifth older adults (20.5%) were also Wave 1 established users of another tobacco product, including e-cigarettes (YA: 11.5%, OA: 8.3%), noncigarette combustible tobacco (YA: 17.5%, OA: 9.1%), smokeless tobacco (YA: 10.6%, OA: 5.1%), and hookah (YA: 13.0%, OA: 1.4%).
Table 2 reports Wave 1 descriptive statistics for young and older adults for the primary analytic sample used in Analyses 2 and 3—respondents who were current smokers at Wave 1, who reported a quit attempt at Wave 2, and had no missing data on outcomes or predictors of interest.
Table 2.
PATH Wave 1 (2013–2014) Descriptive Statistics for US Young and Older Adults Who Reported a Quit Attempt at Wave 2
| Young adultsa (n = 748) | Older adultsa (n = 2,068) | |
|---|---|---|
| % | % | |
| Female | 43.3 | 46.2 |
| Race | ||
| White | 65.2 | 66.3 |
| African American | 9.9 | 14.7 |
| Latinx/Hispanic | 16.0 | 11.2 |
| Other race/ethnicity | 9.0 | 7.8 |
| LGB+ | 13.1 | 6.8 |
| High school education or higher | 76.5 | 78.2 |
| Urban residence | 81.7 | 78.1 |
| Trouble paying bills | 27.0 | 30.8 |
| Polytobacco user | 39.7 | 22.3 |
| Cigarettes per day (mean #) | 9.73 | 14.4 |
aWeighted using population-based weights.
Analysis 1: Intentions to Quit Among Younger and Older Adult Smokers
At Wave 1, almost all young and older adult smokers reported planning to quit at some point in their lifetime (YA: 91.1%, OA: 91.9%; OR: 0.90; confidence interval [CI]: 0.70, 1.16). The majority reported planning to quit within a year (YA: 66.9%; OA: 79.9%), although younger adults were significantly less likely to do so (OR: 0.51; CI: 0.43, 0.59). Younger adult smokers expressed a significantly lower level of interest in quitting (scale 1–10) than older adults (YA: = 7.04; OA: = 8.21; OR: 0.36; CI: 0.30, 0.44), and among those who intended to quit within 6 months, young adults were more confident they would be very successful (a score of 4 out of 4) (YA: 48.38%; OA: 40.83%; OR: 1.31; CI: 1.01, 1.71).
Analysis 2: Young Adult Versus Older Adult Strategies for Smoking Cessation
Among young adults who made a quit attempt, 7.6% reported using only evidence-based strategies, in contrast to 23.3% of older adults. A total of 26.9% of young adults reported using product substitution only, 3.1% reported using both an evidence-based strategy and product substitution, and 62.4% attempting to quit unassisted. Both young and older adults reported using product substitution to help quit (alone or in combination with other strategies; Table 3) more than using any of the evidence-based cessation strategies, and almost all of the product substitution for both age groups was to e-cigarettes.
Table 3.
Cessation Strategies at Wave 2 (2014–2015) of the PATH Study for US Young and Older Adults Who Reported a Quit Attempt at Wave 2 (n = 2,816)
| Weighted use rate | ||||
|---|---|---|---|---|
| Young adults | Older adults | OR | (95% CI) | |
| Behavioral support | 4.8 | 8.1 | 0.578* | (0.371, 0.901) |
| Pharmacotherapy | 7.9 | 24.3 | 0.268*** | (0.191, 0.376) |
| NRT | 6.3 | 19.8 | 0.272*** | (0.188, 0.393) |
| Patch | 3.4 | 11.4 | 0.273*** | (0.133, 0.402) |
| Gum | 3.3 | 5.3 | 0.611 | (0.949, 1.415) |
| Other NRT | 1.8 | 5.6 | 0.306** | (1.312, 1.882) |
| Prescription drug | 2.3 | 9.1 | 0.231*** | (0.180, 0.413) |
| Varenicline | 0.9 | 6.3 | 0.141*** | (0.350, 1.067) |
| Bupropion | 1.4 | 3.1 | 0.446* | (0.134, 0.696) |
| Substitution | 31.6 | 28.5 | 1.159 | (0.064, 0.311) |
| Cigarette | 1.7 | 1.7 | 0.996 | (0.202, 0.983) |
| e-cigarette | 26.3 | 25.2 | 1.057 | (0.521, 1.906) |
| Non cigarette combustibles | 1.8 | 1.3 | 1.476 | (0.851, 1.314) |
| Smokeless tobacco | 4.0 | 1.6 | 2.505** | (0.777, 2.804) |
| Hookah | 1.2 | 0.5 | 2.298 | (0.805, 6.564) |
| Social support | 33.3 | 33.2 | 1.007 | (0.846, 1.199) |
| Unassisted | 62.4 | 51.4 | 1.571*** | (1.419, 4.425) |
CI, confidence interval; NRT, nicotine replacement therapy; OR, odds ratio.
*p < .01, **p < .05, ***p < .001.
Young adults were significantly less likely to employ evidence-based cessation strategies (Table 3), including behavioral support, any pharmacotherapy, nicotine replacement therapy, and prescription drugs, and were more likely to quit unassisted. Significant differences were evident in all NRT and prescription drug types except for nicotine gum. There was no significant difference between young and older adult use of social support to help quit. Although young and older adults reported product substitution at similar rates, young adults were significantly more likely to report using smokeless tobacco to quit.
Analysis 3: Predictors of Strategies for Smoking Cessation by Age Group
Findings after introducing a categorical outcome and controlling for Wave 1 covariates in a multinomial logistic regression model were consistent with those of the first analysis: Young adults were significantly less likely to use pharmacotherapy (compared with quitting unassisted) but were just as likely to use product substitution (Table 4 “All Adults”). Young adults were less likely to use two or more strategies to quit compared with their older counterparts.
Table 4.
Wave 1 (2013–2014) Predictors of Cessation Strategy Use at Wave 2 (2014–2015) of the PATH Study for US All Adults, Young Adults, and Older Adults Who Reported a Quit Attempt at Wave 2
| All adults | Young adults | Older adults | Interaction effectsa | ||||||
|---|---|---|---|---|---|---|---|---|---|
| AOR | (95% CI) | AOR | (95% CI) | AOR | (95% CI) | AOR | (95% CI) | ||
| Behavioral support | |||||||||
| Female | 1.347 | (0.771, 2.353) | 0.528 | (0.131, 2.133) | 1.595 | (0.878, 2.899) | 0.378 | (0.090, 1.584) | |
| Race/ethnicityb | African American | 0.894 | (0.454, 1.763) | NRd | NR | 0.926 | (0.457, 1.875) | NR | NR |
| Latinx/Hispanic | 0.537 | (0.257, 1.122) | 1.888 | (0.510, 6.991) | 0.386 | (0.128, 1.167) | 4.413 | (0.785, 24.799) | |
| Other race/ethnicity | 0.407 | (0.097, 1.699) | NR | NR | 0.170 | (0.025, 1.137) | NR | NR | |
| LGB+ | 1.031 | (0.373, 2.849) | NR | NR | 1.278 | (0.413, 3.956) | NR | NR | |
| High school education or higher | 1.294 | (0.703, 2.383) | 3.202 | (0.361, 28.40) | 1.122 | (0.579, 2.172) | 2.161 | (0.280, 16.68) | |
| Urban residence | 2.062 | (0.925, 4.597) | 3.501 | (0.232, 52.84) | 1.941 | (0.821, 4.591) | 2.372 | (0.141, 40.02) | |
| Trouble paying bills | 1.513 | (0.809, 2.830) | 3.026 | (0.679, 13.49) | 1.297 | (0.623, 2.698) | 2.064 | (0.444, 9.585) | |
| Polytobacco userc | 1.422 | (0.652, 3.101) | NR | NR | 1.967 | (0.881, 4.393) | 0.124 | (0.014, 1.109) | |
| Cigarettes per day | 0.994 | (0.969, 1.019) | 1.011 | (0.916, 1.116) | 0.992 | (0.962, 1.022) | 1.009 | (0.897, 1.133) | |
| Young adult | 0.619 | (0.277, 1.379) | |||||||
| Pharmacotherapy | |||||||||
| Female | 1.177 | (0.890, 1.555) | 0.939 | (0.323, 2.730) | 1.220 | (0.925, 1.610) | 0.630 | (0.237, 1.676) | |
| Race/ethnicityb | African American | 0.501** | (0.331, 0.760) | NR | NR | 0.501** | (0.326, 0.769) | NR | NR |
| Latinx/Hispanic | 0.259*** | (0.152, 0.441) | NR | NR | 0.245*** | (0.142, 0.424) | NR | NR | |
| Other race/ethnicity | 0.531* | (0.304, 0.928) | NR | NR | 0.554* | (0.310, 0.990) | NR | NR | |
| LGB+ | 0.766 | (0.408, 1.438) | NR | NR | 0.815 | (0.417, 1.592) | NR | NR | |
| High school education or higher | 0.879 | (0.643, 1.202) | 2.139 | (0.495, 9.236) | 0.848 | (0.614, 1.172) | 2.194 | (0.501, 9.614) | |
| Urban residence | 1.204 | (0.833, 1.740) | 1.213 | (0.321, 4.579) | 1.207 | (0.805, 1.808) | 1.003 | (0.221, 4.557) | |
| Trouble paying bills | 0.959 | (0.733, 1.256) | NR | NR | 0.984 | (0.739, 1.310) | NR | NR | |
| Polytobacco userc | 1.092 | (0.749, 1.590) | 2.149 | (0.740, 6.242) | 1.071 | (0.688, 1.668) | 2.207 | (0.722, 6.747) | |
| Cigarettes per day | 1.003 | (0.998, 1.009) | 1.027 | (0.986, 1.070) | 1.003 | (0.998, 1.008) | 1.020 | (0.980, 1.061) | |
| Young adult | 0.150*** | (0.092, 0.244) | |||||||
| Substitution | |||||||||
| Female | 1.078 | (0.839, 1.384) | 0.873 | (0.587, 1.297) | 1.137 | (0.860, 1.505) | 0.792 | (0.521, 1.205) | |
| Race/ethnicityb | African American | 0.282*** | (0.181, 0.441) | 0.332*** | (0.182, 0.606) | 0.275*** | (0.164, 0.459) | 1.133 | (0.533, 2.406) |
| Latinx/Hispanic | 0.377*** | (0.265, 0.536) | 0.615 | (0.376, 1.005) | 0.321*** | (0.202, 0.511) | 1.809 | (0.960, 3.409) | |
| Other race/ethnicity | 0.441*** | (0.299, 0.650) | 0.455 | (0.199, 1.042) | 0.442** | (0.267, 0.732) | 0.989 | (0.329, 2.972) | |
| LGB+ | 1.731** | (1.242, 2.412) | 1.469 | (0.861, 2.507) | 1.884** | (1.212, 2.929) | 0.748 | (0.352, 1.588) | |
| High school education or higher | 1.154 | (0.893, 1.491) | 1.116 | (0.706, 1.764) | 1.173 | (0.855, 1.609) | 0.854 | (0.486, 1.500) | |
| Urban residence | 0.937 | (0.696, 1.260) | 1.032 | (0.632, 1.684) | 0.932 | (0.661, 1.314) | 1.065 | (0.616, 1.838) | |
| Trouble paying bills | 1.284* | (1.007, 1.638) | 1.314 | (0.866, 1.995) | 1.264 | (0.947, 1.686) | 1.041 | (0.628, 1.726) | |
| Polytobacco userc | 2.549*** | (2.009, 3.235) | 1.777** | (1.228, 2.571) | 2.858*** | (2.166, 3.770) | 0.660 | (0.430, 1.012) | |
| Cigarettes per day | 0.999 | (0.993, 1.005) | 1.022 | (0.984, 1.062) | 0.997 | (0.989, 1.006) | 1.022 | (0.986, 1.059) | |
| Young adult | 0.861 | (0.681, 1.089) | |||||||
| Two or more strategies | |||||||||
| Female | 1.600** | (1.192, 2.147) | 0.978 | (0.441, 2.170) | 1.728** | (1.252, 2.385) | 0.617 | (0.281, 1.358) | |
| Race/ethnicityb | African American | 0.396*** | (0.251, 0.625) | NR | NR | 0.414*** | (0.258, 0.664) | NR | NR |
| Latinx/Hispanic | 0.492* | (0.286, 0.846) | 0.849 | (0.309, 2.336) | 0.438* | (0.231, 0.829) | 1.705 | (0.504, 5.767) | |
| Other race/ethnicity | 0.628 | (0.272, 1.451) | NR | NR | 0.740 | (0.315, 1.739) | NR | NR | |
| LGB+ | 0.815 | (0.411, 1.618) | 0.903 | (0.174, 4.688) | 0.853 | (0.394, 1.848) | 0.911 | (0.158, 5.251) | |
| High school education or higher | 1.155 | (0.752, 1.773) | 1.327 | (0.560, 3.147) | 1.125 | (0.713, 1.776) | 0.984 | (0.444, 2.181) | |
| Urban residence | 1.191 | (0.822, 1.726) | 1.118 | (0.411, 3.038) | 1.222 | (0.840, 1.778) | 0.817 | (0.314, 2.124) | |
| Trouble paying bills | 1.210 | (0.864, 1.694) | 1.923 | (0.786, 4.708) | 1.142 | (0.784, 1.664) | 1.507 | (0.570, 3.982) | |
| Polytobacco userc | 2.941*** | (2.110, 4.099) | 3.048* | (1.203, 7.718) | 3.014*** | (1.972, 4.608) | 1.108 | (0.386, 3.176) | |
| Cigarettes per day | 1.002 | (0.996, 1.007) | 1.028 | (0.988, 1.069) | 1.001 | (0.995, 1.006) | 1.023 | (0.984, 1.063) | |
| Young adult | 0.412*** | (0.266, 0.636) | |||||||
| N | 2,816 | 748 | 2,068 | 2,816 | |||||
| F | 6.649 | 2.975 | 5.554 |
AOR, adjusted odds ratio; CI, confidence interval.
aEach interaction term was introduced in a separate model. Interaction models were adjusted for all other covariates. Main effects from interaction models not shown.
bReference category: white.
cReference category: cigarette only smoker at baseline.
dNR, results not reported because of limited sample size.
*p < .01, **p < .05, ***p < .001.
In the age group subsample analyses, few socioeconomic and tobacco use variables predicted young adult cessation strategy use. However, Wave 1 polytobacco users of both age groups were more likely to use product substitution and multiple cessation strategies, and African American young and older adults were less likely to use product substitution. Due to small cell sizes in the young adult model, we were unable to report some race/ethnicity and LGB+ estimates.
Additional predictors were significant in the all-adult and older adult models, for example, African American and Latinx respondents were significantly less likely to use pharmacotherapy, substitution, and two or more strategies and respondents reporting another non-white race or ethnicity were significantly less likely to use pharmacotherapy and substitution. In all-adult and older adult models, LGB+ respondents were significantly more likely to use product substitution than their heterosexual counterparts. Female respondents were more likely to report using two or more strategies in the all-adult and older adult models. Participants who reported having trouble paying bills were less likely to use product substitution in the all-adult model. Interaction terms between predictors and age group were not significant (Table 4 “Interaction Effects”), suggesting no difference in the relationship between cessation strategy use and socioeconomic and tobacco use factors across age groups.
Robustness Check
To isolate cigarette cessation attempts, we restricted the bivariate analyses to established cigarette smokers with no current established use of any other tobacco product. Results were consistent with models including polyusers. However, odds ratios (ORs) were slightly different in magnitude. For cigarette-only smokers, there was no significant difference in use of behavioral support by age (see Supplementary Material).
Discussion
We used the PATH study Waves 1 and 2 data to describe intentions to quit and cessation strategies among young adult established cigarette smokers. In comparison to older adults, we found that although most adults intend to quit smoking, young adults have lower interest, a longer time horizon, and higher perceived likelihood of success. We found that young adults use evidence-based cessation strategies (NRT and prescription drugs) less than their older adult counterparts, even after controlling for sociodemographic and tobacco use characteristics, and young adults are more likely to try to quit unassisted. Combined, these findings affirm that young adults are interested in quitting tobacco use and highlight a continuing challenge: encouraging evidence-based cessation among this population.
Previous research has demonstrated the effectiveness of evidence-based smoking cessation strategies for young adult smokers.6 Despite the effectiveness of these strategies, we found that NRT, other smoking cessation medications, and behavioral support were relatively unpopular among young adult smokers in PATH, consistent with previous research.7,8 There are several potential reasons why young adults underutilize evidence-based smoking cessation support. Previous research has shown that greater confidence in ability to quit is related to less use of cessation assistance,23 which is consistent with our finding that young adults were significantly more confident that they would be able to quit and less likely to use cessation assistance compared with older adults. Young adults may perceive evidence-based strategies as ineffective,24 they may be concerned about side effects and harms from use of NRT or medication,24 or they may not perceive these treatment options as relevant for them.25–27 Moreover, young adults have expressed concern about the cost of evidence-based cessation aids and may not know about low cost or free evidence-based treatment,27,28 though some research has suggested that young adults may not use these treatment options despite being aware of them.9 Self-identified social smoking young adults were found to have lower intentions to quit and fewer quit attempts (quitting for 1 month or more) compared with regular smokers.29
More work is needed to motivate young adults to seek evidence-based treatments.6,30,31 Interventions should reduce the barriers to NRT and medication use, for example by addressing and correcting preconceptions about use of and side effects from NRT and medications,24,27 by comparing the costs of medication to those of continued tobacco use, and by improving awareness of free NRT and counseling through state quitlines.27,28 More efforts should be undertaken to frame evidence-based smoking cessation strategies in a way that makes them appear relevant for young adult smokers.
The aggressive use of social media to advertise e-cigarettes32 might also contribute to young adults’ disproportionate use of these devices as a cessation strategy. As an alternative to digital promotion of tobacco products, digital and mobile health interventions, including text messaging, apps, social media, and online interventions, may be effective tools to improve the relevance and reach of evidence-based cessation for young adult smokers.33–35 Moreover, there is emerging evidence that digital interventions can support smoking cessation among young adults,35,36 though studies have also found that young adults engaged less with an online smoking cessation intervention compared with older smokers.37 Given the promise of digital interventions to increase reach to young adult smokers, future research should investigate effective strategies for improving engagement among young adults and for helping them achieve abstinence through digital smoking cessation interventions.
Notably, over 30% of young and older adults in the PATH study who tried to quit between Waves 1 and 2 reported switching to another tobacco product, almost exclusively to e-cigarettes, to help them quit smoking. In our study, 3.6 times more young adults who made a quit attempt used product substitution than an evidence-based strategy. The implications of this finding depend on the effectiveness of e-cigarettes for young adult cigarette cessation. High-quality research on the effectiveness of e-cigarettes for cessation is limited, observational trials report mixed findings,38 and few studies have isolated young adults for study. A comprehensive review by the National Academies of Sciences, Engineering, and Medicine concluded that “overall, there is limited evidence that e-cigarettes may be effective aids to promote smoking cessation.”38 The effectiveness of e-cigarettes as a cessation aid for young adults, who have been smoking for fewer years, are likely more susceptible to new tobacco products, and report an array of reasons to use e-cigarettes, might be different than that for older adults. There is limited evidence regarding e-cigarette-assisted cessation for young adults.39,40
Our findings also illuminate that differences in cessation assistance might contribute to tobacco-related health disparities. For example, smokers who identified as a racial or ethnic minority were more likely to attempt to quit unassisted, a finding consistent with previous studies.10 LGB+ individuals were no different from their heterosexual counterparts in likelihood of using evidence-based strategies when trying to quit (consistent with previous work, e.g., Fallin et al.41), but were more likely to substitute to a different tobacco product. Disparities in cigarette use among sexual minority individuals are well documented (e.g., Rath et al.42), including in a previous study of PATH Wave 1 that found both young (18–24) and older (≥25) lesbian/gay and bisexual women and young gay men had higher relative odds of regularly smoking cigarettes compared with their heterosexual counterparts.43 That study also found that young and older lesbian/gay and bisexual women were significantly more likely to be established e-cigarette users, and older gay men had significantly higher experimental use of e-cigarette.43 If e-cigarettes are found not to be generally effective for cessation, higher use of e-cigarettes as a cessation aid among LGB+ smokers might exacerbate already present tobacco-related health disparities.
Limitations
The PATH study questionnaire precludes us from isolating cigarette cessation attempts for smokers who use another non-e-cigarette tobacco product. However, findings were consistent when we isolated exclusive cigarette smokers in a robustness check. Furthermore, a comparison of cigarette cessation attempts and strategy choice between cigarette-only smokers and polytobacco users conducted before the proliferation of e-cigarettes (2010–2011) found that both cigarette-only and dual users had similar odds of having made a past year cigarette smoking quit attempt and of having used counseling or medication during that quit attempt.21 Both previous research and our robustness check suggest our findings reflect cigarette cessation attempts specifically.
Despite the PATH study’s large sample size, we were unable to report results for some of the race and ethnicity covariates in the young adult sociodemographic model due to insufficient cell size. However, this limitation serves as additional evidence of the underutilization of evidence-based cessation aids by young adults of color. This study relies on self-reported cessation attempts, which are subject to recall-bias. In addition to inaccurate or incomplete responses because of memory, respondents who tried to quit in the study period but were unsuccessful might have reframed the experience and no longer classified it as a quit attempt when asked at Wave 2. If this is the case, it is likely that underreporting is higher for unassisted quit attempts than assisted quit attempts, which would make our estimates of strategy use rates conservatively high.
Conclusion
The present study used the detailed and large PATH study to explore differences in cessation intentions and strategies between young adult established smokers and their older counterparts. Our findings that young adults desire to quit but continue to attempt to do so without help emphasize the need to provide appropriate cessation services to this population. Young adulthood is a key transition time for tobacco use, and tailored cessation services could help young adults quit smoking before long-term health effects of tobacco use are manifest.
Funding
This research was funded by the National Cancer Institute (T32CA113710-11), the California Tobacco Related Disease Research Program (TRDRP 25FT-0009), and UCSF funds from the Center for Tobacco Control Research and Education. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Declaration of Interests
Authors report no conflicts of interest.
Supplementary Material
References
- 1. Schulenberg JE, Johnston LD, O’Malley PM, Bachman JG, Miech RA, Patrick ME.. Monitoring the Future National Survey Results on Drug Use, 1975–2016: Volume II, College Students and Adults Ages 19–55. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2017. [Google Scholar]
- 2. Villanti AC, Niaura RS, Abrams DB, Mermelstein R. Preventing smoking progression in young adults: the concept of prevescalation. Prev Sci. 2018;1–8. doi:10.1007/s11121-018-0880-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Thompson AB, Mowery PD, Tebes JK, McKee SA. Time trends in smoking onset by sex and race/ethnicity among adolescents and young adults: findings from the 2006-2013 National Survey on Drug Use and Health. Nicotine Tob Res. 2018;20(3):312–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jha P, Ramasundarahettige C, Landsman V, et al. 21st-century hazards of smoking and benefits of cessation in the United States. N Engl J Med. 2013;368(4):341–350. [DOI] [PubMed] [Google Scholar]
- 5. Diemert LM, Bondy SJ, Brown KS, Manske S. Young adult smoking cessation: predictors of quit attempts and abstinence. Am J Public Health. 2013;103(3):449–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Suls JM, Luger TM, Curry SJ, Mermelstein RJ, Sporer AK, An LC. Efficacy of smoking-cessation interventions for young adults: a meta-analysis. Am J Prev Med. 2012;42(6):655–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Solberg LI, Asche SE, Boyle R, McCarty MC, Thoele MJ. Smoking and cessation behaviors among young adults of various educational backgrounds. Am J Public Health. 2007;97(8):1421–1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Curry SJ, Sporer AK, Pugach O, Campbell RT, Emery S. Use of tobacco cessation treatments among young adult smokers: 2005 National Health Interview Survey. Am J Public Health. 2007;97(8):1464–1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hughes JR, Cohen B, Callas PW. Treatment seeking for smoking cessation among young adults. J Subst Abuse Treat. 2009;37(2):211–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. McCarthy M, Siahpush M, Shaikh RA, Sikora Kessler A, Tibbits M. Social disparities in unaided quit attempts among daily current and former smokers: results from the 2010–2011 tobacco use supplement to the current population survey. Nicotine Tob Res. 2016;18(8):1705–1710. [DOI] [PubMed] [Google Scholar]
- 11. Solberg LI, Parker ED, Foldes SS, Walker PF. Disparities in tobacco cessation medication orders and fills among special populations. Nicotine Tob Res. 2010;12(2):144–151. [DOI] [PubMed] [Google Scholar]
- 12. Cobb NK, Brookover J, Cobb CO. Forensic analysis of online marketing for electronic nicotine delivery systems. Tob Control. 2015;24(2):128–131. [DOI] [PubMed] [Google Scholar]
- 13. Duke JC, Lee YO, Kim AE, et al. Exposure to electronic cigarette television advertisements among youth and young adults. Pediatrics. 2014;134(1):e29–e36. [DOI] [PubMed] [Google Scholar]
- 14. Grana RA, Ling PM. “Smoking revolution”: a content analysis of electronic cigarette retail websites. Am J Prev Med. 2014;46(4):395–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Richardson A, Ganz O, Stalgaitis C, Abrams D, Vallone D. Noncombustible tobacco product advertising: how companies are selling the new face of tobacco. Nicotine Tob Res. 2014;16(5):606–614. [DOI] [PubMed] [Google Scholar]
- 16. Kalkhoran S, Padilla JL, Neilands TB, Ling PM. Multiple tobacco product use among young adult bar patrons in New Mexico. Prev Med. 2016;83:16–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Richardson A, Williams V, Rath J, Villanti AC, Vallone D. The next generation of users: prevalence and longitudinal patterns of tobacco use among US young adults. Am J Public Health. 2014;104(8):1429–1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Family Smoking and Prevention and Tobacco Control Act, Pub L No. 111-31, 123 Stat. 1776–1858 (2009).
- 19. Ramamurthi D, Gall PA, Ayoub N, Jackler RK. Leading-brand advertisement of quitting smoking benefits for E-cigarettes. Am J Public Health. 2016;106(11):2057–2063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Patel D, Davis KC, Cox S, et al. Reasons for current E-cigarette use among U.S. adults. Prev Med. 2016;93:14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Schauer GL, Malarcher AM, Babb SD. Prevalence and correlates of switching to another tobacco product to quit smoking cigarettes. Nicotine Tob Res. 2015;17(5):622–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hyland A, Ambrose BK, Conway KP, et al. Design and methods of the Population Assessment of Tobacco and Health (PATH) study. Tob Control. 2017;26(4):371–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Myers MG, Strong DR, Linke SE, Hofstetter CR, Al-Delaimy WK. Predicting use of assistance when quitting: a longitudinal study of the role of quitting beliefs. Drug Alcohol Depend. 2015;149:220–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ryan MP, Hinojosa JJ. Conceptual obstacles to making use of four smoking-cessation strategies: what reasons do light smokers give for rejecting strategies? Health Psychol Open. 2015;2(2):1–2. doi:10.1177/2055102915624928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kishchuk N, Tremblay M, Lapierre J, Heneman B, O’Loughlin J. Qualitative investigation of young smokers’ and ex-smokers’ views on smoking cessation methods. Nicotine Tob Res. 2004;6(3):491–500. [DOI] [PubMed] [Google Scholar]
- 26. Morphett K, Partridge B, Gartner C, Carter A, Hall W. Why don’t smokers want help to quit? A qualitative study of smokers’ attitudes towards assisted vs. unassisted quitting. Int J Environ Res Public Health. 2015;12(6):6591–6607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Amos A, Wiltshire S, Haw S, McNeill A. Ambivalence and uncertainty: experiences of and attitudes towards addiction and smoking cessation in the mid-to-late teens. Health Educ Res. 2006;21(2):181–191. [DOI] [PubMed] [Google Scholar]
- 28. Silla K, Beard E, Shahab L. Nicotine replacement therapy use among smokers and ex-smokers: associated attitudes and beliefs: a qualitative study. BMC Public Health. 2014;14:1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Song AV, Ling PM. Social smoking among young adults: investigation of intentions and attempts to quit. Am J Public Health. 2011;101(7):1291–1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Husten CG. Smoking cessation in young adults. Am J Public Health. 2007;97(8):1354–1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. McClure LA, Arheart KL, Lee DJ, Sly DF, Dietz NA. Young adult former ever smokers: the role of type of smoker, quit attempts, quit aids, attitudes/beliefs, and demographics. Prev Med. 2013;57(5):690–695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Huang J, Duan Z, Kwok J, et al. Vaping versus JUULing: how the extraordinary growth and marketing of JUUL transformed the US retail E-cigarette market. Tob Control. 2018. In press. doi:10.1136/tobaccocontrol-2018–054382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Baskerville NB, Struik LL, Dash D. Crush the crave: development and formative evaluation of a smartphone app for smoking cessation. JMIR Mhealth Uhealth. 2018;6(3):e52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Squiers L, Brown D, Parvanta S, et al. The SmokefreeTXT (SFTXT) study: web and mobile data collection to evaluate smoking cessation for young adults. JMIR Res Protoc. 2016;5(2):e134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ramo DE, Thrul J, Chavez K, Delucchi KL, Prochaska JJ. Feasibility and quit rates of the tobacco status project: a Facebook smoking cessation intervention for young adults. J Med Internet Res. 2015;17(12):e291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ramo DE, Thrul J, Delucchi KL, et al. A randomized controlled evaluation of the tobacco status project, a Facebook intervention for young adults. Addiction. 2018;113(9):1683–1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cantrell J, Ilakkuvan V, Graham AL, et al. Young adult utilization of a smoking cessation website: an observational study comparing young and older adult patterns of use. JMIR Res Protoc. 2016;5(3):e142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Committee on the Review of the Health Effects of Electronic Nicotine Delivery Systems. Public Health Consequences of E-cigarettes. In: Stratton K, Kwan LY, Eaton DL, eds. Washington, DC: The National Academic Press; 2018. [Google Scholar]
- 39. Mantey DS, Cooper MR, Loukas A, Perry CL. E-cigarette use and cigarette smoking cessation among Texas college students. Am J Health Behav. 2017;41(6):750–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Chen JC. Flavored e-cigarette use and cigarette smoking reduction and cessation—a large national study among young adult smokers. Subst Use Misuse. 2018;53(12):2017–2031. [DOI] [PubMed] [Google Scholar]
- 41. Fallin A, Lee YO, Bennett K, Goodin A. Smoking cessation awareness and utilization among lesbian, gay, bisexual, and transgender adults: an analysis of the 2009-2010 National Adult Tobacco Survey. Nicotine Tob Res. 2016;18(4):496–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Rath JM, Villanti AC, Rubenstein RA, Vallone DM. Tobacco use by sexual identity among young adults in the United States. Nicotine Tob Res. 2013;15(11):1822–1831. [DOI] [PubMed] [Google Scholar]
- 43. Wheldon CW, Kaufman AR, Kasza KA, Moser RP. Tobacco use among adults by sexual orientation: findings from the Population Assessment of Tobacco and Health study. LGBT Health. 2018;5(1):33–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.