Abstract
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) continues to spread across the globe, and millions of people may be affected. While knowledge regarding epidemiologic features and diagnostic tools of coronavirus disease 2019 (COVID-19) is rapidly evolving, uncertainties surrounding various aspects of its optimal management strategies persist. A subset of these patients develop a more severe form of the disease characterized by expanding pulmonary lesions, sepsis, acute respiratory distress syndrome, and respiratory failure. Due to lack of data on treatment strategies specific to this subset of patients, currently available evidence on management of the critically ill needs to be extrapolated and customized to their clinical needs. The article calls attention to fluid stewardship in the critically ill with COVID-19 by judiciously applying the evidence-based resuscitation principles to their specific clinical features such as high rates of cardiac injury. As we await more data from treating these patients, this strategy is likely to help reduce potential complications.
Keywords: Congestion, COVID-19, critically ill, resuscitation, SARS-CoV-2
The coronavirus disease of 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), continues to spread around the world1,2; the World Health Organization recently declared it a public health emergency of international concern.3 While knowledge regarding epidemiologic features and diagnostic tools of COVID-19 is rapidly evolving, health care systems are challenged by uncertainties surrounding various aspects of optimal management strategies.
The infection by SARS-CoV-2 is characterized by substantial variability of clinical syndromes, from asymptomatic infected persons to mild symptoms up to a small proportion of patients with a fatal outcome. At an early stage, infected patients generally present with mild upper respiratory infection symptoms similar to the common cold. Reports from China indicate that most patients with COVID-19 had mild symptoms such as fever, fatigue, dry cough, upper airway congestion, shortness of breath, and myalgia/arthralgia.4 A subset of these patients presented with gastrointestinal manifestations such as nausea, vomiting, and diarrhea.4 Among the 14% with more severe disease, additional manifestations (e.g., respiratory rate ≥30/min and blood oxygen saturation ≤93%) were present, and 5% were critical, with respiratory failure, septic shock, and/or multiorgan dysfunction or failure.4,5 A significant subset of these patients develop acute respiratory distress syndrome (ARDS). Hypoxemic respiratory failure is the most common cause of admission to the intensive care unit (ICU).6,7 Additionally, it is becoming clear that there is a sequence of distributive shock, abrupt renal failure, and death that occurs despite all forms of supportive care. Older age, the presence of comorbidities such as cardiovascular and pulmonary disease, and the development of complications such as early acute kidney injury (AKI) are among poor prognostic factors.6,7
Of special note, the cause of death in >80% of patients is reported to be respiratory failure alone or concomitant respiratory and heart failure.6 Due to lack of data on treatment strategies specific to more severe cases of COVID-19, available evidence on management of the critically ill needs to be extrapolated to the clinical features of this potentially fatal disease.
COVID-19 AS A CRITICAL ILLNESS
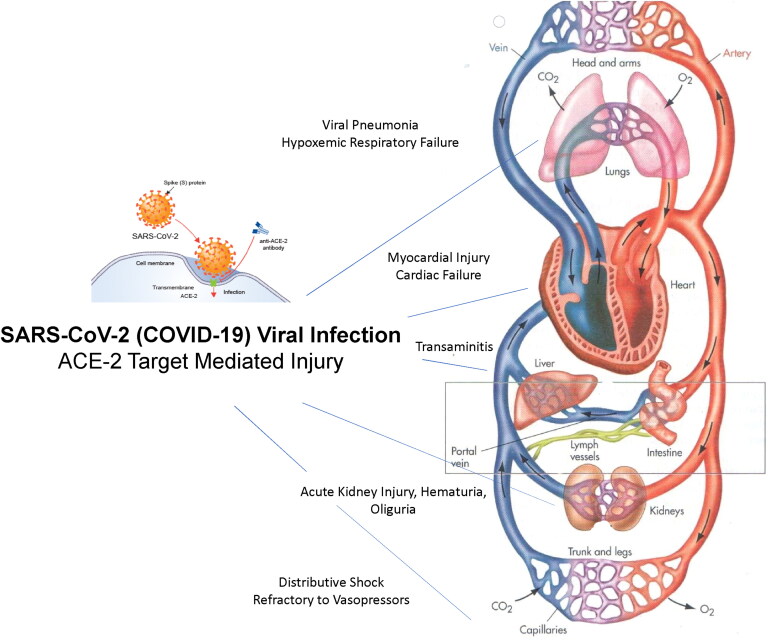
Aberrancy in immune response can result in failure to clear virus and viral sepsis. While proinflammatory cytokines such as interleukin-6 are essential to mediate innate immunity, they can cause host damage as part of a maladaptive process. Viral sepsis remains highly heterogeneous and is likely to encompass a complex and not yet fully understood pattern of pathophysiologic pathways and immune responses that are distinct from bacterial infections.8 However, the current consensus guidelines are primarily based on studies of bacterial sepsis and are not pathogen specific.9 About 5% of patients with COVID-19 develop critical illness and are admitted to the ICU.5 Respiratory failure due to expansion of pulmonary infiltrates and secondary bacterial infection, septic shock, and multiorgan failure are among the reasons for an untoward clinical course in this setting.4 The expression and distribution of angiotensin converting enzyme II (ACE-2), the primary host cell receptor of SARS-CoV2, in various systems make it possible for the virus to infect a variety of cells and induce multiple organ failure (Figure 1).
Figure 1.
SARS-CoV-2 (COVID-19)–mediated organ injury in critically ill patients mediated by viral entry and target mediated destruction of the angiotensin converting enzyme II (ACE-2) receptor enzyme.
Similar to other patients with hemodynamic instability, these patients are likely to undergo aggressive fluid administration as the mainstay of management. In fact, fluid resuscitation remains the most enduring of sepsis treatments, predating even antibiotics, although mounting evidence has recently challenged its central role in this setting.10 A potentially simplistic and possibly incorrect reasoning at the foundation of such conjecture is the presumed hypoperfusion resulting in an increase in serum lactate levels accompanied by low blood pressure, oliguria, hepatic dysfunction, and altered mental status in patients with sepsis.11 In this hypoperfusion-centric paradigm, the microcirculatory dysfunction is the key driver of sequential pathophysiologic mechanisms ultimately leading to multiorgan failure. Not only have some observations challenged the validity of this hypothesis (e.g., lack of correlation between oliguria and renal blood flow in sepsis),12,13 but alternative plausible biological explanations (e.g., bioenergetics failure) have also been offered.11 Moreover, due to known changes in the glycocalyx structure and hyperpermeability of vasculature in sepsis, the administered fluid is rapidly redistributed into an extravascular compartment.14 In keeping with these concepts, there is clinical evidence that the increase in intravascular volume after fluid bolus therapy might be small and short lived, leading to only transient improvement in hemodynamic parameters such as cardiac output.15
These observations coupled with the strong evidence on the association of adverse outcomes with extravascular volume overload (an unintended consequence of aggressive fluid therapy in sepsis—see below) make fluid stewardship a serious consideration for the care of these patients. This concept is even more crucial in critically ill patients with COVID-19 in whom expanding lung infiltrates, ARDS, and respiratory failure often coexist with sepsis.
ACQUIRED VOLUME OVERLOAD
Pragmatic endpoints for fluid resuscitation are difficult to delineate. In general, the goal is for cardiac output to become preload independent (i.e., reaching the plateau portion of the Frank-Starling curve), but this is difficult to assess clinically.16 In the absence of universally accepted objective measurement tools that are validated in a wide spectrum of patients admitted for sepsis syndromes, acquired volume overload remains an obvious risk of aggressive fluid resuscitation.17 There is ample evidence of the detrimental impact of interstitial edema and congestion on the function of multiple organ systems, including the kidney and the lungs.18
Since the ventricular pressure–volume relationship is curvilinear, atrial pressures increase rapidly as the patients reach the plateau of their Frank-Starling curve. Increased atrial pressure is associated with an increase in pulmonary and venous hydrostatic pressures, leading to a shift of fluid into the interstitial space, further disturbing capillary blood flow and oxygen diffusion.19 This effect is more pronounced in those clinical settings, such as COVID-19, where lung tissue architecture is already disturbed by an active and rapidly expanding inflammatory process. Moreover, a significant subset of patients with COVID-19 develops ARDS, which is characterized by pulmonary edema resulting from increased capillary permeability, making these patients even more vulnerable to resuscitation-induced lung congestion.
The incidence of AKI in COVID-19 varies widely; estimates range from 0.5% to 29%.1,4,20 It is noteworthy that a subset of patients experiences fever, malaise, nausea, vomiting, and possibly diarrhea for several days before seeking medical care. As such, they are prone to intravascular volume depletion and prerenal AKI. In these patients, early aggressive volume resuscitation is indicated to avoid development of extensive acute tubular injury due to prolonged severe renal hypoperfusion. While it has been suggested that direct cellular injury via ACE-2 that is expressed in proximal renal tubules could contribute to AKI,21 it remains likely that shock (and in some cases cytokine storm) are the primary causes of acute tubular necrosis in this setting. Moreover, similar to right-sided heart failure, following aggressive fluid administration the increased right atrial pressure is transmitted retrograde, leading to elevated venous pressure in abdominal organs such as the kidney, liver, and the guts. Kidneys are particularly vulnerable to a rise in interstitial pressure and tubular compression due to the capsule surrounding them (i.e., renal intracapsular tamponade).
The detrimental impact of high “backward venous pressure” on renal hemodynamics and development of congestive renal failure has been well studied in heart failure.22 In the Fluids and Catheters Treatment Trial (FACCT), the incidence of AKI was similar between restrictive and liberal fluid management groups.23 However, Liu et al showed that after correcting serum creatinine levels for fluid balance, the incidence of AKI was lower with a restrictive fluid strategy.24 Besides, venous wall stretch is a stimulus for activation of endothelium and subsequent release of inflammatory mediators, which in turn may lead to interstitial damage and functional abnormalities such as diminished tubular reabsorption and retention of sodium and water.25 Increasing intra-abdominal pressure due to progressive volume overload can also contribute to further impairment of renal hemodynamics and function.
In keeping with these pathophysiologic mechanisms, an accumulating body of evidence has established positive fluid balance as a strong and independent predictor of poor outcomes in the critically ill.26–28 For example, a large international study on more than 1800 patients with sepsis found that a higher cumulative fluid balance 3 days after ICU admission was proportionately associated with an increased risk of death.29 Similarly, the Sepsis Occurrence in Acutely Ill Patients (SOAP) study on more than 1100 patients with sepsis from 198 European ICUs reported positive fluid balance as an independent risk factor for mortality.30 Further supporting this notion is the observation that achieving a negative fluid balance in volume-overloaded patients with sepsis is associated with improvement in survival rates.27
TIMING OF FLUID RESUSCITATION
With the increase in our understanding of the adverse consequences of aggressive fluid administration and volume overload, several studies have tried to compare a conservative fluid or deresuscitation (i.e., active removal of fluid) strategy with a standard care or liberal fluid strategy in critically ill patients.23,31,32 While a comprehensive review of these studies is beyond the scope of this article, improved outcomes have generally been reported with conservative or deresuscitative fluid strategies in patients with sepsis or ARDS.33
Importantly, there has also been greater recognition of “phases” of shock and the importance of a dynamic approach that takes into consideration the distinct clinical characteristics of each phase. The widely accepted international guidelines for management of severe sepsis and septic shock (i.e., Surviving Sepsis Campaign), which have gone through much scrutiny and updates, emphasize early fluid resuscitation (30 mL/kg within the first 3 h).34 Recently, Vincent et al proposed separating management of shock into four distinct phases: rescue, optimization, stabilization, and de-escalation.16 While the primary focus of the first phase is to reach the minimum effective blood volume through fluid administration, the main goal of the de-escalation phase is to reach a negative fluid balance. Interestingly, not only has early fluid resuscitation been shown to reduce mortality in patients with sepsis,35 but earlier negative volume balance during the de-escalation phase is also associated with an improved survival rate.27 In support of this notion, Murphy et al reported that among patients with acute lung injury secondary to septic shock, those who received both adequate initial fluid resuscitation as well as conservative late fluid management (i.e., negative to even fluid balance on 2 consecutive days during the first week after sepsis) had the best survival rates compared with those who achieved only one of these goals or neither of the two.36 Therefore, a dynamic approach and optimal timing (i.e., early administration followed by early termination or active removal) appear to be the key in fluid resuscitation of patients with sepsis. It remains to be explored whether more precise assessment of volume status through invasive methods (e.g., central venous pressure measurement or pulmonary arterial catheterization) or noninvasive techniques (e.g., bioimpedance spectroscopy or cardiac echography) can prove helpful in certain subsets of patients such as those with preexisting heart failure or renal dysfunction.
ACTIVE FLUID REMOVAL
While fluid management goals beyond the resuscitation or salvage phase of critical illness remain the subject of considerable uncertainty, it is clear that reaching an even or negative fluid balance in the de-escalation phase would be crucial in order to avoid complications associated with lingering congestion. Loop diuretics are often used to counter positive fluid balance in ICU patients.37 Studies evaluating the impact of loop diuretics in the ICU have yielded inconsistent results, with some showing benefit,38 others reporting no benefit,39 and some suggesting harm.40 Interestingly, in a recent study on 14,896 patients, Libório et al found that loop diuretic use in critically ill patients with positive fluid balance was associated with prolonged mechanical ventilation.41 Since patients receiving diuretics had a serum bicarbonate level of 2 mEq/L above others, and metabolic alkalosis can reduce the neural respiratory drive and minute ventilation, the authors argued that the metabolic side effect of diuretics could contribute to the observed mechanical ventilation weaning difficulties.41,42
In the face of positive fluid balance during the de-escalation phase of sepsis management, one might consider earlier application of renal replacement therapy (RRT), especially in those patients with more severe volume overload, progressive metabolic alkalosis with diuretic use, suboptimal diuretic response or diuretic refractoriness, and development of oliguric AKI. In light of evidence on the detrimental impact of RRT use for treatment of sepsis (through clearance of inflammatory mediators and cytokines),43 RRT should be considered only if indicated for optimization of volume status or treatment of azotemia. While a modality that provides clearance (e.g., continuous venovenous hemofiltration) will be needed for those cases with progressive renal function impairment, isolated ultrafiltration is an optimal strategy that primarily focuses on fluid extraction and optimization of volume status. Extraction of sodium-rich fluid represents an advantage over diuretics because use of balanced or unbalanced fluids during the salvage phase is associated with significant sodium loading, while urine generated with the use of diuretics typically remains hypotonic. Portable ultrafiltration devices could prove particularly helpful, in that their extremely small extracorporeal volume (i.e., 35 mL) will help avoid a potential adverse hemodynamic impact in the critically ill. Moreover, the predictability of the fluid extraction will make it more likely to achieve the precise goal for the de-escalation process.44
COVID-19 IN THE SPOTLIGHT
Applying the aforementioned general concepts of management to specific features of COVID-19 is the key for optimized therapy plans. Pulmonary involvement can rapidly progress in a significant subset of these patients. In a study on 416 patients with COVID-19, Shi et al reported the incidence of ARDS as high as 23.3%.45 In addition to respiratory failure and shock, the course of the critically ill patients with COVID-19 is characterized by some patients developing refractory heart failure with features of cardiogenic shock.6 It remains unclear whether this results from direct myocardial damage by infection, stress cardiomyopathy similar to other forms of shock, or right heart failure due to prolonged ARDS. Myocardial injury, identified by elevated cardiac biomarkers, was reported among early cases in China. In a study of 138 hospitalized patients with COVID-19, cardiac injury (elevated high-sensitivity troponin I or new electrocardiographic or echocardiographic abnormalities) was present in 22% of the patients who required ICU care.46 The concomitant increase in other inflammatory biomarkers (e.g., D-dimer, ferritin, and interleukin-6) implies that the rise in high-sensitivity troponin I is more reflective of cytokine storm or secondary hemophagocytic lymphohistiocytosis than isolated cardiac injury. Similar to the kidney, there has been a yet not well-studied proposal for direct viral injury (i.e., myocarditis) through ACE-2–dependent entry of the SARS-CoV2 into cardiomyocytes. A few cases of COVID-19 have been reported where the patients predominantly presented with cardiac manifestations and cardiogenic shock.47,48 Histological findings have not been reported in such cases yet. As respiratory failure worsens, there is a need for extracorporeal membrane oxygenation due to hypoxemia and distributive and cardiogenic shock.49 The large majority of mortality in these patients is attributed to respiratory failure and shock.6
These observations—the frequent development of ARDS and the possibility of cardiac dysfunction in addition to active expanding lung infiltrates—make it crucial for physicians to be vigilant with fluid management strategies. We should remain mindful that fluid resuscitation exerts its potentially therapeutic effect mainly by increasing the stressed volume of the circulation, leading to improved venous return and cardiac output. If these effects are not anticipated due to concomitant pathophysiologic mechanisms (e.g., onslaught of cytokine storm and declining cardiac function), aggressive fluid administration is likely to result in volume overload and its extensive adverse consequences in patients with already diminished respiratory reserve due to pulmonary infiltrates. It has been reported that a restricted initial resuscitation strategy (i.e., “preventing” overload) might be advantageous compared to fluid removal after more liberal administration.50 A proactive and collaborative approach to achieve a negative fluid balance is also warranted once the patient’s clinical status is deemed stabilized. In addition to the aforementioned benefits of RRT in this setting, rapid device deployment capability and ease of use of the dedicated ultrafiltration machines (e.g., possibility of using peripheral venous access) can be advantageous, as the number of infected patients is rapidly escalating worldwide with overutilization of available resources.
CONCLUSION
The outbreak of COVID-19 is undoubtedly one of the most challenging global health care problems in recent years. Yet, due to its explosive nature and resource utilization potential, it can help us refine our skills and reconsider our approaches. Constantly reminding ourselves of the currently available evidence on fluid resuscitation strategies, and judiciously applying those principles to the specific features of this disease as we learn them (e.g., high percentage of heart failure, volume overload, and circulatory failure), is likely to help optimize the care of these patients.
DISCLOSURES
No specific financial support was obtained for preparation of this article. AK has the following potential conflicts of interest: Baxter, Inc. (Cardiology Advisory Board and consultancy fee), CHF Solutions, Inc. (Medical Advisory Board and consultancy fee), and W. L. Gore Inc. (consultancy fee).
References
- 1.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . WHO director-general’s opening remarks at the media briefing on COVID-19—25 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—25-march-2020. Accessed March 30, 2020.
- 3.World Health Organization . WHO director-general’s opening remarks at the media briefing on COVID-19—11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020. Accessed March 30, 2020.
- 4.Guan W-J, Ni Z-Y, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Eng J Med. 2020. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. [DOI] [PubMed] [Google Scholar]
- 6.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cao J, Hu X, Cheng W, Yu L, Tu WJ, Liu Q. Clinical features and short-term outcomes of 18 patients with corona virus disease 2019 in intensive care unit. Intensive Care Med. 2020. doi: 10.1007/s00134-020-05987-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lin GL, McGinley JP, Drysdale SB, Pollard AJ. Epidemiology and immune pathogenesis of viral sepsis. Front Immunol. 2018;9:2147. doi: 10.3389/fimmu.2018.02147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rhodes A, Evans LE, Alhazzani W, et al. Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43(3):304–377. doi: 10.1007/s00134-017-4683-6. [DOI] [PubMed] [Google Scholar]
- 10.Marik PE, Byrne L, van Haren F. Fluid resuscitation in sepsis: the great 30 mL per kg hoax. J Thorac Dis. 2020;12(S1):S37–S47. doi: 10.21037/jtd.2019.12.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Byrne L, Van Haren F.. Fluid resuscitation in human sepsis: time to rewrite history? Ann Intensive Care. 2017;7(1):4. doi: 10.1186/s13613-016-0231-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bihari S, Prakash S, Bersten AD. Post resuscitation fluid boluses in severe sepsis or septic shock: prevalence and efficacy (price study). Shock. 2013;40(1):28–34. doi: 10.1097/SHK.0b013e31829727f1. [DOI] [PubMed] [Google Scholar]
- 13.Egal M, Erler NS, de Geus HR, van Bommel J, Groeneveld AB. Targeting oliguria reversal in goal-directed hemodynamic management does not reduce renal dysfunction in perioperative and critically ill patients: a systematic review and meta-analysis. Anesth Analg. 2016;122(1):173–185. doi: 10.1213/ANE.0000000000001027. [DOI] [PubMed] [Google Scholar]
- 14.Uchimido R, Schmidt EP, Shapiro NI. The glycocalyx: a novel diagnostic and therapeutic target in sepsis. Crit Care. 2019;23(1):16. doi: 10.1186/s13054-018-2292-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Glassford NJ, Eastwood GM, Bellomo R. Physiological changes after fluid bolus therapy in sepsis: a systematic review of contemporary data. Crit Care. 2014;18(6):1. doi: 10.1186/s13054-014-0696-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vincent JL, De Backer D. Circulatory shock. N Engl J Med. 2013;369(18):1726–1734. doi: 10.1056/NEJMra1208943. [DOI] [PubMed] [Google Scholar]
- 17.Kelm DJ, Perrin JT, Cartin-Ceba R, et al. Fluid overload in patients with severe sepsis and septic shock treated with early goal-directed therapy is associated with increased acute need for fluid-related medical interventions and hospital death. Shock. 2015;43(1):68–73. doi: 10.1097/SHK.0000000000000268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jaffee W, Hodgins S, McGee WT. Tissue edema, fluid balance, and patient outcomes in severe sepsis: an organ systems review. J Intensive Care Med. 2018;33(9):502–509. doi: 10.1177/0885066617742832. [DOI] [PubMed] [Google Scholar]
- 19.Hilton AK, Bellomo R. A critique of fluid bolus resuscitation in severe sepsis. Crit Care. 2012;16(1):302. doi: 10.1186/cc11154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Deng Y, Liu W, Liu K, et al. Clinical characteristics of fatal and recovered cases of coronavirus disease 2019 (COVID-19) in Wuhan, China: a retrospective study. Chin Med J (Engl). 2020:1. doi: 10.1097/CM9.0000000000000824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Diao B, Feng Z, Wang C, et al. Human kidney is a target for novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. medRxiv. 2020. doi: 10.1101/2020.03.04.20031120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rosenkranz S, Howard LS, Gomberg-Maitland M, Hoeper MM. Systemic consequences of pulmonary hypertension and right-sided heart failure. Circulation. 2020;141(8):678–693. doi: 10.1161/CIRCULATIONAHA.116.022362. [DOI] [PubMed] [Google Scholar]
- 23.Wiedemann HP, Wheeler AP, Bernard GR, et al. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354:2564–2575. doi: 10.1056/NEJMoa062200. [DOI] [PubMed] [Google Scholar]
- 24.Liu KD, Thompson BT, Ancukiewicz M, et al. Acute kidney injury in patients with acute lung injury: impact of fluid accumulation on classification of acute kidney injury and associated outcomes. Crit Care Med. 2011;39:2665–2671. doi: 10.1097/CCM.0b013e318228234b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Husain-Syed F, McCullough PA, Birk HW, et al. Cardio-pulmonary-renal interactions: a multidisciplinary approach. J Am Coll Cardiol. 2015;65(22):2433–2448. doi: 10.1016/j.jacc.2015.04.024. [DOI] [PubMed] [Google Scholar]
- 26.Acheampong A, Vincent JL. A positive fluid balance is an independent prognostic factor in patients with sepsis. Crit Care. 2015;19(1):251. doi: 10.1186/s13054-015-0970-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dhondup T, Tien JC, Marquez A, Kennedy CC, Gajic O, Kashani KB. Association of negative fluid balance during the de-escalation phase of sepsis management with mortality: a cohort study. J Crit Care. 2020;55:16–21. doi: 10.1016/j.jcrc.2019.09.025. [DOI] [PubMed] [Google Scholar]
- 28.Sirvent JM, Ferri C, Baro A, Murcia C, Lorencio C. Fluid balance in sepsis and septic shock as a determining factor of mortality. Am J Emerg Med. 2015;33(2):186–189. doi: 10.1016/j.ajem.2014.11.016. [DOI] [PubMed] [Google Scholar]
- 29.Sakr Y, Rubatto Birri PN, Kotfis K, et al. Higher fluid balance increases the risk of death from sepsis: results from a large international audit. Crit Care Med. 2017;45(3):386–394. doi: 10.1097/CCM.0000000000002189. [DOI] [PubMed] [Google Scholar]
- 30.Vincent JL, Sakr Y, Sprung CL, et al. Sepsis in European intensive care units: results of the SOAP study. Crit Care Med. 2006;34(2):344–353. doi: 10.1097/01.ccm.0000194725.48928.3a. [DOI] [PubMed] [Google Scholar]
- 31.Chen C, Kollef MH. Targeted fluid minimization following initial resuscitation in septic shock: a pilot study. Chest. 2015;148(6):1462–1469. doi: 10.1378/chest.15-1525. [DOI] [PubMed] [Google Scholar]
- 32.Richard J-C, Bayle F, Bourdin G, et al. Preload dependence indices to titrate volume expansion during septic shock: a randomized controlled trial. Crit Care. 2015;19(1):5. doi: 10.1186/s13054-014-0734-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Silversides JA, Major E, Ferguson AJ, et al. Conservative fluid management or deresuscitation for patients with sepsis or acute respiratory distress syndrome following the resuscitation phase of critical illness: a systematic review and meta-analysis. Intensive Care Med. 2017;43(2):155–170. doi: 10.1007/s00134-016-4573-3. [DOI] [PubMed] [Google Scholar]
- 34.De Backer D, Dorman T. Surviving Sepsis guidelines: a continuous move toward better care of patients with sepsis. JAMA. 2017;317(8):807–808. doi: 10.1001/jama.2017.0059. [DOI] [PubMed] [Google Scholar]
- 35.Lee SJ, Ramar K, Park JG, Gajic O, Li G, Kashyap R. Increased fluid administration in the first three hours of sepsis resuscitation is associated with reduced mortality—a retrospective cohort study. Chest. 2014;146(4):908–915. doi: 10.1378/chest.13-2702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Murphy CV, Schramm GE, Doherty JA, et al. The importance of fluid management in acute lung injury secondary to septic shock. Chest. 2009;136(1):102–109. doi: 10.1378/chest.08-2706. [DOI] [PubMed] [Google Scholar]
- 37.Jones SL, Martensson J, Glassford NJ, Eastwood GM, Bellomo R. Loop diuretic therapy in the critically ill: a survey. Crit Care Resusc. 2015;17(3):223–226. [PubMed] [Google Scholar]
- 38.Grams ME, Estrella MM, Coresh J, Brower RG, Liu KD. Fluid balance, diuretic use, and mortality in acute kidney injury. Clin J Am Soc Nephrol. 2011;6(5):966–973. doi: 10.2215/CJN.08781010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Uchino S, Doig GS, Bellomo R, et al. Diuretics and mortality in acute renal failure. Crit Care Med. 2004;32(8):1669–1677. doi: 10.1097/01.ccm.0000132892.51063.2f. [DOI] [PubMed] [Google Scholar]
- 40.Mehta RL, Pascual MT, Soroko S, Chertow GM. Diuretics, mortality, and nonrecovery of renal function in acute renal failure. JAMA. 2002;288(20):2547–2553. doi: 10.1001/jama.288.20.2547. [DOI] [PubMed] [Google Scholar]
- 41.Libório AB, Barbosa ML, Sá VB, Leite TT. Impact of loop diuretics on critically ill patients with a positive fluid balance. Anaesthesia. 2020;75(S1):e134–e142. doi: 10.1111/anae.14908. [DOI] [PubMed] [Google Scholar]
- 42.Oppersma E, Doorduin J, van der Hoeven JG, et al. The effect of metabolic alkalosis on the ventilatory response in healthy subjects. Respir Physiol Neurobiol. 2018;249:47–53. doi: 10.1016/j.resp.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 43.Payen D, Mateo J, Cavaillon JM, et al. Impact of continuous venovenous hemofiltration on organ failure during the early phase of severe sepsis: a randomized controlled trial. Crit Care Med. 2009;37(3):803–810. doi: 10.1097/CCM.0b013e3181962316. [DOI] [PubMed] [Google Scholar]
- 44.Kazory A. Cardiorenal syndrome: ultrafiltration therapy for heart failure—trials and tribulations. Clin J Am Soc Nephrol. 2013;8(10):1816–1828. doi: 10.2215/CJN.02910313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shi S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020:25. doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zeng JH, Liu YX, Yuan J, et al. First case of COVID-19 infection with fulminant myocarditis complication: case report and insights. Preprints. 2020. doi: 10.20944/preprints202003.0180.v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hu H, Ma F, Wei X, Fang Y. Coronavirus fulminant myocarditis saved with glucocorticoid and human immunoglobulin. Eur Heart J. 2020. doi: 10.1093/eurheartj/ehaa190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ramanathan K, Antognini D, Combes A, et al. Planning and provision of ECMO services for severe ARDS during the COVID-19 pandemic and other outbreaks of emerging infectious diseases. Lancet Respir Med. 2020. doi: 10.1016/S2213-2600(20)30121-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Semler MW, Wheeler AP, Thompson BT, Bernard GR, Wiedemann HP, Rice TW; Acute Respiratory Distress Syndrome Network. Impact of initial central venous pressure on outcomes of conservative versus liberal fluid management in acute respiratory distress syndrome. Crit Care Med. 2016;44(4):782–789. doi: 10.1097/CCM.0000000000001555. [DOI] [PMC free article] [PubMed] [Google Scholar]