Abstract
Background
The presence of a Frank’s sign ear crease is closely correlated with coronary artery disease (CAD). The SYNTAX score indicates the complexity of coronary lesions. This present investigation sought to identify the correlation between SYNTAX score and several specific ear creases.
Material/Methods
Four specific types of ear creases – crossing crease not originated from ear hole (CC-NEH), crossing crease originated from ear hole (CC-EH), vertical creases on the face side (VC-F), and vertical creases dividing earlobe and face (VC-EF) – were investigated in patients undergoing coronary angiography. A Frank’s sign score system was introduced based on the 4 creases. Demographic data, clinical data, and SYNTAX score were also documented. The association between ear creases and SYNTAX score, as well as the correlation between Frank’s score and SYNTAX score, were statistically analyzed.
Results
CC-NEH had the highest positive predictive value (positive predictive value=0.439), and VC-F had the highest negative predictive value for the detection of intermediate and high SYNTAX score (negative predictive value=1.000). VC-EF and CC-NEH were associated with intermediate and high SYNTAX scores (OR=2.913–7.694, all P<0.05). Only 2.9% of patients with Frank’s score=0 had intermediate or high SYNTAX scores, and 52.2% and 50.0% of patients with Frank’s sign score=3 and 4 had intermediate or high SYNTAX scores, respectively. The Frank’s sign score was significantly and positively correlated with SYNTAX score (r=0.457, P<0.001).
Conclusions
Features of specific ear creases and Frank’s sign scores were associated with intermediate and high complexity of coronary lesions.
MeSH Keywords: Coronary Artery Disease, Coronary Stenosis, Myocardial Ischemia
Background
Coronary artery disease (CAD) is now a global problem, and patients with complicated coronary lesions have higher cardiovascular risk [1,2]. The SYNTAX score is based on coronary angiographic results and indicates the complexity of coronary lesions [3,4]. Some studies have also confirmed the ability of the SYNTAX score to predict major adverse cardiac events (MACE) in patients with multi-vessel coronary arterial disease [5–7], left main disease [8], myocardial infarction [9], stable CAD complicated with type 2 diabetes [10], and even all-comers [11] undergoing elective percutaneous coronary intervention. Previous studies have classified the SYNTAX score into low (≤22), intermediate (23 to 32), and high (≥33) according to the cardiovascular risk [12,13].
Frank’s sign is a typical ear crease first discovered by S. T. Frank in 1973, which was associated with coronary artery disease [14,15]. However, some controversies remain regarding this association [16–18]. After careful observation of ears of patients with coronary artery disease, we noticed that some specific ear creases – vertical creases on the face side (VC-F), vertical creases dividing earlobe and face (VC-EF), crossing crease not originated from ear hole (CC-NEH), and crossing crease originated from ear hole (CC-EH) – were more frequent in patients with intermediate and high SYNTAX scores. Therefore, the features of these creases may have significance for coronary lesions evaluation.
Since the intermediate and high SYNTAX scores suggest higher complexity of coronary lesions, it is reasonable to speculate that these ear creases are correlated with complexity of coronary lesions, and could thus be a promising method to preliminarily evaluate the coronary artery status by evaluating presence of specific ear creases.
Material and Methods
Study design and participants
The present cross-sectional and observational study was conducted from Jan 2018 to Oct 2018 at the Department of Cardiology, Shaanxi Provincial People’s Hospital. Patients who received coronary angiography (CAG) and were willing to cooperate were enrolled in the study. We photographed ear creases of enrolled patients and the SYNTAX scores were calculated based on the CAG results. A total of 346 patients were finally enrolled in this study, including 232 (67.1%) men and 112 (32.9%) women. The average age was 59.83±11.14 years with a range of 22 to 83 years. The average SYNTAX score was 12.76±11.91, with a range from 0 to 69. There were 74 (21.4%) patients with SYNTAX scores ≥23 and 272 (78.6%) had SYNTAX scores ≤22.
Ear creases evaluation
The photos of ears were taken before the CAG examination in all enrolled patients. Four prominent ear creases were documented: Vertical Creases on the Face side (VC-F, Figure 1A) on both ears, Vertical Creases dividing Earlobe and Face (VC-EF, Figure 1A) on both ears, Crossing Crease originated from the Ear Hole (CC-EH, Figure 1A) on both ears, and Crossing Crease Not originated from the Ear Hole (CC-NEH, Figure 1B) on both ears. Both of the 2 crossing creases documented had to be full-length, dividing the earlobe into 2 different parts, and half-length crossing creases were not documented. The photos were analyzed by 2 cardiologists for detection and documentation of the ear creases on both sides of the ears. A third cardiologist was involved in evaluation and confirmation of ear creases when the opinions of the previous 2 cardiologists disagreed.
Figure 1.
(A, B) Four prominent ear creases on the ears. VC-F – Vertical Creases on the Face side; VC-EF – Vertical Creases dividing Earlobe and Face; CC-NEH – Crossing Creases Not originated from Ear Hole; CC-EH – Crossing Creases originated from Ear Hole.
SYNTAX score evaluation
CAG examinations were administrated for all enrolled subjects. The SYNTAX score calculator (current version of 2.28; http://www.syntaxscore.com) was applied to calculate the SYNTAX score right after the standard CAG procedure. Two cardiologists with up to 5 years of interventional experience calculated the SYNTAX score independently. An additional interventional cardiologist participated in the evaluation procedure when the scores were different. Based on the SYNTAX score results, subjects were divided into a low SYNTAX score group (with SYNTAX scores ≤22) and an intermediate and high SYNTAX score group (with SYNTAX scores ≥23).
General data
Demographic and clinical information were collected. On the morning of the day after administration, fasting peripheral blood samples were acquired. The white blood cells (WBC) counts, NEUT%, platelet counts, red blood cells (RBC) counts, hemoglobin, TC, triglyceride, HDL-C, LDL-C, glycosylated hemoglobin-A1c (HbA1c), brain natriuretic peptide (BNP), total bilirubin (TBIL), direct bilirubin (DBIL), urea nitrogen (BUN), creatinine, uric acid, cystatin C, and albumin levels were assessed [19]. Echocardiography was performed and left ventricular ejection fraction (LVEF) was evaluated [20].
Definitions
Hypertension was defined according to current guidelines: systolic blood pressure ≥140 mmHg, or diastolic blood pressure ≥90 mmHg, or previous antihypertensive medication or medical history [21].
Diabetes was defined according to fasting plasma glucose ≥7.0 mmol/L, or random plasma glucose ≥11.1 mmol/L, or the oral glucose tolerance test (OGTT) plasma glucose ≥11.1 mmol/L, or previous anti-hypoglycemic medication or medical history [22].
Smoking was defined as continuous or cumulative smoking time for 6 months or more in a lifetime.
Statistical analysis
The statistical analysis was performed using SPSS (version 16.0, SPSS Inc.). The Mann-Whitney U test was used for comparison of continuous variables. Categorical variables are presented as proportions. The chi-square test was used for comparison of categorical variables. The sensitivity, specificity, and positive and negative likelihood ratios of different ear creases for the detection of intermediate and high SYNTAX scores were also calculated. Logistic regression analysis was performed to assess the association between different ear creases and intermediate and high SYNTAX scores, and an unadjusted model and 3 adjusted models adjusting for different confounding factors were established. Since the VC-EF and CC-NEH were associated with intermediate and high SYNTAX scores, the LVC-EF, RVC-EF, LCC-NEH, and RCC-NEH were assigned as 1 point each. The total score was termed “Frank’s sign score”. Each patient could have 0–4 kinds of ear creases, with Frank’s sign scores of 0–4 points. The percentages of the intermediate and high SYNTAX scores and SYNTAX scores were calculated in patients with different Frank’s sign scores. The correlation between Frank’s sign score and SYNTAX score was assessed using Pearson correlation analysis. P<0.05 was set as statistical significance.
Results
Baseline data
The baseline data of subjects are presented in Table 1. The percentage of men, RVC-F, VC-F, LVC-EF, RVC-EF, VC-EF, LCC-NEH, RCC-NEH, CC-NEH, LCC-EH, CC-EH, age, WBC, NEUT%, HB, creatinine, BNP, and SYNTAX scores in patients with intermediate and high SYNTAX scores significantly higher compared with patients with low SYNTAX scores (all P<0.05). ALB, HDL-C, and LVEF in patients with intermediate and high SYNTAX scores were significantly higher than in patients with low SYNTAX scores (all P<0.05). The percentage of patients with hypertension, diabetes mellitus, smoking, LVC-F, RCC-EH and HR, SBP, DBP, RBC, PLT, TBIL, DBIL, BUN, UA, Cys-c, TC, TG, LDL-C, and HbA1c were no significantly different in patients with low SYNTAX score and patients with intermediate and high SYNTAX scores (all P>0.05).
Table 1.
Baseline characteristics of patients with low SYNTAX scores vs. intermediate and high SYNTAX scores.
| Low SYNTAX score (SYNTAX score <23; n=272) | Intermediate and high SYNTAX score (SYNTAX score ≥23; n=74) | P value | |
|---|---|---|---|
| Male (%) | 168 (71.8%) | 66 (28.2%) | |
| Female (%) | 104 (92.9%) | 8 (7.1%) | 0.001* |
| Hypertension (%) | 138 (50.7%) | 36 (48.6%) | 0.750 |
| Diabetes mellitus (%) | 54 (19.9%) | 8 (10.8%) | 0.072 |
| Smoking (%) | 80 (29.4%) | 28 (37.8%) | 0.165 |
| LVC-F (%) | 256 (90.4%) | 70 (94.6%) | 0.353 |
| RVC-F (%) | 252 (92.6%) | 74 (100.0%) | 0.010* |
| VC-F (%) | 256 (94.1%) | 74 (100.0%) | 0.028* |
| LVC-EF (%) | 168 (61.8%) | 62 (83.8%) | <0.001* |
| RVC-EF (%) | 184 (67.6%) | 64 (86.5%) | 0.001* |
| VC-EF (%) | 200 (73.5%) | 70 (94.6%) | <0.001* |
| LCC-NEH (%) | 28 (10.3%) | 28 (37.8%) | <0.001* |
| RCC-NEH (%) | 28 (10.3%) | 22 (29.7%) | <0.001* |
| CC-NEH (%) | 46 (16.9%) | 36 (48.6%) | <0.001* |
| LCC-EH (%) | 102 (37.5%) | 44 (59.5%) | 0.001* |
| RCC-EH (%) | 144 (52.9%) | 48 (64.9%) | 0.067 |
| CC-EH (%) | 152 (55.9%) | 58 (78.4%) | 0.001* |
| Age (yrs) | 62.16±41.29 | 63.97±8.45 | 0.001* |
| HR (b/min) | 71.35±12.63 | 73.43±17.05 | 0.285 |
| SBP (mmHg) | 128.62±19.64 | 133.00±21.25 | 0.104 |
| DBP (mmHg) | 78.53±11.97 | 80.41±13.62 | 0.378 |
| WBC (×109/L) | 7.19±2.39 | 8.43±2.53 | <0.001* |
| NEUT% | 0.69±0.36 | 0.69±0.09 | 0.016* |
| RBC (×1012/L) | 4.51±0.97 | 4.58±0.49 | 0.038 |
| HB (g/L) | 136.51±16.06 | 143.51±12.62 | <0.001* |
| PLT (×109/L) | 194.15±65.03 | 179.83±61.82 | 0.112 |
| TBIL (umol/L) | 16.95±11.48 | 17.57±8.24 | 0.264 |
| DBIL (umol/L) | 5.34±2.42 | 6.27±3.92 | 0.098 |
| ALB (g/L) | 39.18±4.18 | 37.67±3.86 | 0.007* |
| BUN (mmol/L) | 5.18±1.62 | 5.71±2.43 | 0.106 |
| Creatinine (umol/L) | 74.38±18.61 | 83.54±28.48 | 0.004* |
| UA (umol/L) | 345.40±297.48 | 318.46±82.83 | 0.889 |
| Cys-c (mg/L) | 1.02±0.26 | 1.07±0.28 | 0.157 |
| TC (mmol/L) | 3.90±1.04 | 3.73±0.92 | 0.183 |
| TG (mmol/L) | 1.92±1.86 | 1.51±0.68 | 0.072 |
| HDL-C (mmol/L) | 1.05±0.23 | 0.97±0.18 | 0.003* |
| LDL-C (mmol/L) | 2.25±0.78 | 2.25±0.72 | 0.838 |
| HbA1c (%) | 6.16±1.59 | 6.13±1.11 | 0.966 |
| BNP (pg/mL) | 276.28±640.53 | 371.65±338.92 | <0.001* |
| LVEF (%) | 59.03±9.81 | 56.79±8.60 | 0.006* |
| SYNTAX score (points) | 7.83±6.96 | 30.85±8.26 | <0.001* |
LVC-F – Left Vertical Creases on the Face side; RVC-F – Right Vertical Creases on the Face side; VC-F – Vertical Creases on the Face side; LVC-EF – Left Vertical Creases dividing Earlobe and Face; RVC-EF – Right Vertical Creases dividing Earlobe and Face; VC-EF – Vertical Creases dividing Earlobe and Face; LCC-NEH – Left Crossing Creases Not originated from Ear Hole; RCC-NEH – Left Crossing Creases Not originated from Ear Hole; CC-NEH – Crossing Creases Not originated from Ear Hole; LCC-EH – Left Crossing Creases originated from Ear Hole; RCC-EH – Right Crossing Creases originated from Ear Hole; CC-EH – Crossing Creases originated from Ear Hole; HR – Heart Rate; SBP – Systolic Blood Pressure; DBP – Diastolic Blood Pressure; WBC – White Blood Cells; NEUT% – NEUTrophilic granulocyte percentage; RBC – Red Blood Cells; HB – HemogloBin; PLT – PLateleT; TBIL – Total Bilirubin; DBIL – Direct Bilirubin; ALB – ALBumin; BUN – Urea Nitrogen; UA – uric acid; Cys-C – Cystatin C; TC – Total Cholesterol; TG – TriGlyceride; HDL-C – High-Density Lipoprotein-Cholesterol; LDL-C – Low-Density Lipoprotein-Cholesterol; HbA1c – Glycosylated Hemoglobin-A1c; BNP – Brain Natriuretic Peptide; LVEF – left ventricular ejection fraction;
P<0.05
Specific ear creases were correlated with SYNTAX score
The sensitivity, specificity, positive predictive value, negative predictive value, positive likelihood ratio, and negative likelihood ratio of different ear creases for the detection of intermediate and high SYNTAX score are presented in Table 2. VC-F had the highest sensitivity (sensitivity=1.000) and CC-NEH had the highest specificity for the prediction of intermediate and high SYNTAX scores (specificity=0.897). CC-NEH had highest positive predictive value (positive predictive value=0.439) and VC-F had the highest negative predictive value (1.000) for the prediction of intermediate and high SYNTAX scores. CC-NEH had the highest positive likelihood ratio (2.876) and VC-F had the lowest negative likelihood ratio (0.000) for the prediction of intermediate and high SYNTAX scores.
Table 2.
Sensitivity, specificity, positive predictive value, negative predictive value, positive likelihood ratio, and negative likelihood ratio of different ear creases for the detection of intermediate and high SYNTAX scores.
| Sensitivity | Specificity | Positive predictive value | Negative predictive value | Positive likelihood ratio | Negative likelihood ratio | |
|---|---|---|---|---|---|---|
| LVC-F | 0.946 | 0.096 | 0.215 | 0.800 | 1.046 | 0.563 |
| RVC-F | 1.000 | 0.074 | 0.227 | 1.000 | 1.080 | 0.000 |
| VC-F | 1.000 | 0.059 | 0.224 | 1.000 | 1.063 | 0.000 |
| LVC-EF | 0.838 | 0.382 | 0.270 | 0.897 | 1.356 | 0.424 |
| RVC-EF | 0.865 | 0.324 | 0.258 | 0.900 | 1.280 | 0.417 |
| VC-EF | 0.946 | 0.265 | 0.259 | 0.947 | 1.287 | 0.204 |
| LCC-NEH | 0.378 | 0.897 | 0.500 | 0.841 | 3.670 | 0.693 |
| RCC-NEH | 0.297 | 0.897 | 0.440 | 0.824 | 2.883 | 0.784 |
| CC-NEH | 0.486 | 0.831 | 0.439 | 0.856 | 2.876 | 0.619 |
| LCC-EH | 0.595 | 0.625 | 0.306 | 0.850 | 1.587 | 0.648 |
| RCC-EH | 0.649 | 0.471 | 0.250 | 0.829 | 1.227 | 0.745 |
| CC-EH | 0.784 | 0.441 | 0.276 | 0.882 | 1.403 | 0.490 |
LVC-F – Left Vertical Creases on the Face side; RVC-F – Right Vertical Creases on the Face side; VC-F – Vertical Creases on the Face side; LVC-EF – Left Vertical Creases dividing Earlobe and Face; RVC-EF – Right Vertical Creases dividing Earlobe and Face; VC-EF – Vertical Creases dividing Earlobe and Face; LCC-NEH – Left Crossing Creases Not originated from Ear Hole; RCC-NEH – Left Crossing Creases Not originated from Ear Hole; CC-NEH – Crossing Creases Not originated from Ear Hole; LCC-EH – Left Crossing Creases originated from Ear Hole; RCC-EH – Right Crossing Creases originated from Ear Hole; CC-EH – Crossing Creases originated from Ear Hole.
The results of logistic regression analysis of intermediate and high SYNTAX scores using different ear creases are presented in Table 3. The unadjusted model and 3 adjusted models adjusting for different confounding factors were established. VC-EF was associated with intermediate and high SYNTAX scores in all 4 models (OR=3.989–7.694, all P<0.05). Meanwhile, CC-NEH was also associated with intermediate and high SYNTAX scores in all 4 models (OR=2.913–4.654, all P<0.05). VC-F was not associated with intermediate and high SYNTAX scores, even in the unadjusted model. CC-EH was associated with intermediate and high SYNTAX scores in 3 models (OR=1.543–2.862, P<0.05); however, when left ventricle ejection fraction was enrolled as an adjusting factor in the logistic regression analysis, CC-EH was no longer associated with intermediate and high SYNTAX score (OR=1.095, P=829).
Table 3.
Logistic regression analysis of intermediate and high SYNTAX scores using different ear creases.
| Unadjusted | Model 1 | Model 2 | Model 3 | |||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | |
| LVC-F | 1.850 (0.625–5.477) | 0.267 | – | – | – | – | – | – |
| RVC-F | 0.000 (0.000––) | 0.998 | – | – | – | – | – | – |
| VC-F | 0.000 (0.000––) | 0.998 | – | – | – | – | – | – |
| LVC-EF | 3.198 (1.645–6.218) | 0.001 | 3.443 (1.733–6.839) | <0.001 | 2.233 (0.974–5.120) | 0.058 | 2.582 (1.073–6.215) | 0.034 |
| RVC-EF | 3.061 (1.500–6.246) | 0.002 | 3.391 (1.629–7.061) | 0.001 | 3.028 (1.102–8.314) | 0.031 | 1.762 (0.716–4.337) | 0.218 |
| VC-EF | 6.300 (2.220–17.877) | 0.001 | 7.694 (2.665–22.215) | <0.001 | 3.989 (1.198–13.280) | 0.024 | 4.625 (1.364–15.678) | 0.014 |
| LCC-NEH | 5.304 (2.878–9.775) | <0.001 | 4.431 (2.364–8.305) | <0.001 | 3.259 (1.409–8.007) | 0.006 | 3.236 (1.349–7.765) | 0.009 |
| RCC-NEH | 3.687 (1.957–6.947) | <0.001 | 3.308 (1.717–6.374) | <0.001 | 3.615 (1.558–8.389) | 0.003 | 2.563 (1.059–6.204) | 0.037 |
| CC-NEH | 4.654 (2.671–8.110) | <0.001 | 4.102 (2.317–7.264) | <0.001 | 3.350 (1.585–7.081) | 0.002 | 2.913 (1.311–6.471) | 0.009 |
| LCC-EH | 2.444 (1.446–4.132) | 0.001 | 2.457 (1.430–4.223) | 0.001 | 2.190 (1.057–4.534) | 0.035 | 1.038 (0.504–2.136) | 0.920 |
| RCC-EH | 1.641 (0.663–2.797) | 0.069 | – | – | – | – | – | – |
| CC-EH | 2.862 (1.566–5.230) | 0.001 | 2.593 (1.339–4.806) | 0.002 | 1.543 (1.011–2.357) | 0.045 | 1.095 (0.479–2.507) | 0.829 |
LVC-F – Left Vertical Creases on the Face side; RVC-F – Right Vertical Creases on the Face side; VC-F – Vertical Creases on the Face side; LVC-EF – Left Vertical Creases dividing Earlobe and Face; RVC-EF – Right Vertical Creases dividing Earlobe and Face; VC-EF – Vertical Creases dividing Earlobe and Face; LCC-NEH – Left Crossing Creases Not originated from Ear Hole; RCC-NEH – Left Crossing Creases Not originated from Ear Hole; CC-NEH – Crossing Creases Not originated from Ear Hole; LCC-EH – Left Crossing Creases originated from Ear Hole; RCC-EH – Right Crossing Creases originated from Ear Hole; CC-EH – Crossing Creases originated from Ear Hole; Model 1 – adjusted for age and sex; Model 2 – adjusted for age, sex, white blood cells count, neutrophile granulocytes percentage, hemoglobin, albumin, creatinine, high-density lipoprotein-cholesterol and type B natriuretic peptide; Model 3 – adjusted for age, sex, white blood cells count, neutrophile granulocytes percentage, hemoglobin, albumin, creatinine, high-density lipoprotein-cholesterol and left ventricle ejection fraction.
Frank score was correlated with SYNTAX score
The ear creases significantly associated with intermediate and high SYNTAX score – VC-EF and CC-NEH – were used to calculate the Frank’s sign scores. Each ear crease of LVC-EF, RVC-EF, LCC-NEH, and RCC-NEH was scored as 1 point, then the patients could have 0–4 points according to the ear creases, with the score constituting the Frank’s sign scores. The percentages of intermediate and high SYNTAX score in patients with different Frank’s sign scores are presented in Figure 2. Only 2.9% of patients with Frank’s sign scores=0 had intermediate and high SYNTAX scores, 16.0% and 19.3% of patients with Frank’s sign scores of 1 and 2 had intermediate and high SYNTAX scores, and 52.2% and 50.0% of patients with Frank score of 3 and 4 had intermediate and high SYNTAX scores. The SYNTAX scores in patients with different Frank’s sign scores are presented in Figure 3. The SYNTAX score was only 3.44±6.33 in patients with Frank’s sign scores of 0, the SYNTAX scores were 14.02±11.92 and 12.37±10.14 in patients with Frank’s sign scores of 1 and 2, respectively, and SYNTAX scores were 22.59±13.44 and 24.13±10.55 in patients with Frank’s sign scores of 3 and 4, respectively. Frank’s sign scores were significantly and positively correlated with SYNTAX scores (r=0.457, P<0.001).
Figure 2.
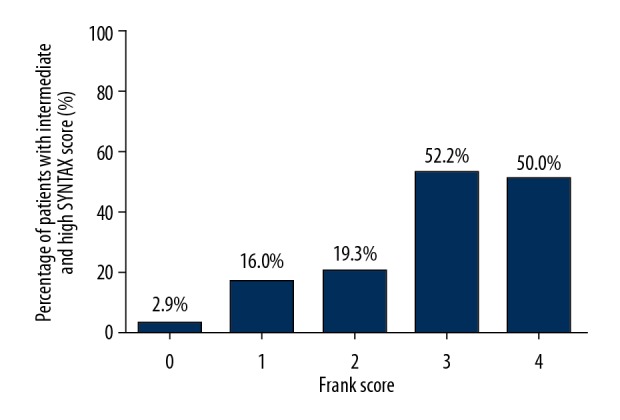
Percentages of intermediate and high SYNTAX score in patients with different Frank’s sign scores. The ear creases significantly associated with intermediate and high SYNTAX score, as VC-EF and CC-NEH were used to calculated the Frank’s sign scores. Each ear crease of LVC-EF, RVC-EF, LCC-NEH, RCC-NEH was scored as 1 point, then the patients could have 0–4 points according to the ear creases, and the total score was the Frank’s sign score.
Figure 3.

SYNTAX scores in patients with different Frank’s sign scores. The ear creases significantly associated with intermediate and high SYNTAX scores, as VC-EF and CC-NEH were used to calculated the Frank’s sign scores. Each ear crease of LVC-EF, RVC-EF, LCC-NEH, and RCC-NEH was scored as 1 point, then the patients could have 0–4 points according to the ear creases, with the total score constituting the Frank’s sign score.
Discussion
In this present study, the positive predictive values for intermediate and high SYNTAX scores ranged from 0.215 to 0.500 using different ear creases. LCC-NEH had the highest positive predictive value of only 0.500, which indicates that if 1 patient had CC-NEH on the left ear, the patient only had a 50% probability of having an intermediate or high SYNTAX score. However, the negative predictive values of the different ear creases for intermediate and high SYNTAX score were relatively higher, ranging from 0.800 to 1.000, which demonstrates that if 1 patient did not have the VC-F on both of the ears, the patient had 0% probability of having an intermediate or high SYNTAX score. Meanwhile, the negative likelihood ratio was 0.000, demonstrating the superior role in exclusion of certain diseases. Therefore, VC-F may be used as one exclusion criteria of intermediate and high SYNTAX scores, which may allow us prioritize patients with multiple diseases [23,24].
All of the patients with intermediate and high SYNTAX scores had the VC-F on 1 ear, but the vast majority of patients (up to 99%) who did not have an intermediate or high SYNTAX score also had the VC-F crease. We found that 83.1% of patients with low SYNTAX scores did not have CC-NEH on both ears, but only 48.6% of patients with intermediate or high SYNTAX scores had CC-NEH on 1 or both ears. According to a previous study [25], when the positive likelihood ratio is >10 or the negative likelihood ratio is <0.1, the probability of diagnosing or excluding a certain disease significantly increases. Therefore, the ear creases documented in this study may not have enough power to predict intermediate and high SYNTAX scores alone, but the VC-F may be used as the exclusion criterion of intermediate and high SYNTAX scores since it has the negative likelihood ratio of 0.000.
To investigate the association between different ear creases and intermediate and high SYNTAX scores, we performed logistic regression analysis using 4 models (Unadjusted and Model 1–3). We assessed associations between the LCC-NEH, RCC-NEH, and CC-NEH on at least 1 ear and intermediate and high SYNTAX scores in all 4 model (all P<0.05). The OR values ranged from to 2.563 to 5.304, indicating the patients with CC-NEH may have up to 5 times greater probability of having intermediate and high SYNTAX scores compared with patients with no CC-NEH. Having VC-EF on at least 1 ear was also significantly associated with intermediate and high SYNTAX scores in all 4 logistic regression models (all P<0.05), the OR values ranged from 3.989 to 7.694, indicating that patients with VC-EF on at least 1 ear have up to 7 times higher probability of having intermediate and high SYNTAX scores compared with patients with no VC-EF in both ears. Interestingly, the traditional typical Frank’s sign, CC-EH, was not associated with intermediate and high SYNTAX scores when the LVEF was entered into the logistic regression analysis (OR=1.095, P=829). The reason for this is unclear, but the strong association between LVEF and intermediate and high SYNTAX scores may remove the Frank’s sign out of the regression analysis [26,27].
To clarify the association between the number of ear creases and intermediate and high SYNTAX scores, we enrolled the intermediate and high SYNTAX score-associated ear creases, VC-EF and CC-NEH, to establish the “Frank’s sign score”. For example, no VC-EF in both ears was marked as “0” points, VC-EF in only 1 ear was marked as “1” point, VC-EF in both ears was marked as “2” points. The same methods were used in the scoring for CC-NEH, and the accumulated score of both ear creases were calculated as the Frank’s sign score (0–4 points). The percentage of intermediate and high SYNTAX scores displayed a staircase trend, only 2.9% of patients with the Frank’s sign score=0 had intermediate and high SYNTAX scores, the incidence reached 16–19.3% when patients had the Frank’s sign scores=1 or 2, and 50–52.2% of patients had intermediate and high SYNTAX scores when the Frank’s sign scores=3 or 4. Meanwhile, the SYNTAX score was only 3.44 points when the Frank’s sign scores were=0, then SYNTAX scores increased to 12.37 to 14.02 points when the Frank’s sign scores were=1 or 2, and the SYNTAX scores reached 22.59 to 24.13 when the Frank’s sign scores were=3 or 4. Pearson correlation analysis showed that the SYNTAX scores were significantly correlated with Frank’s sign scores (r=0.457, P<0.001). Therefore, the Frank’s sign score=0 may be used as the exclusion criteria for intermediate and high SYNTAX score, while the Frank’s sign scores=3 or 4 should receive much more attention since up to 50% of these patients have very complicated and potentially lethal coronary lesions.
This study has several strengths. First, it expanded the traditional Frank’s sign, which we named as CC-EH, and we also innovatively enrolled 3 common ear crease, VC-F, VC-EF, and CC-NEH, and found VC-EF and CC-NEH were associated with intermediate and high-risk of coronary lesions. Second, we used the SYNTAX score-based intermediate and high-risk coronary lesions rather than the coronary artery disease as the grouping method; allowing us to exclude patients with stable coronary artery disease and mild coronary lesions to focus more attention on patients with very complicated and potentially lethal coronary lesions. Third, we innovatively selected the intermediate and high SYNTAX score-associated ear creases, VC-EF and CC-NEH, to establish the “Frank’s sign score”, which made the evaluation of coronary lesions via ear creases easy and precise. This present study also has several limitations, in that it was a cross-sectional study, and we could not determine the causal relationship between the ear creases and intermediate and high SYNTAX scores. LVC-EF and RCC-EH had marginal significance in some logistic regression models, but these ear creases might be significant if the sample size is enlarged [28].
Conclusions
We identified the correlation between Frank’s sign and SYNTAX score. We found that 4 specific ear creases were predictors for SYNTAX score. Moreover, we introduced Frank’s sign score based on observation of specific ear creases. Frank’s sign score was significantly and positively correlated with SYNTAX score. Our results from this study provide a quick, easy, and effective assessment of complicated coronary artery disease when performing physical examinations.
Acknowledgements
We thank Mr. Haitian Qiu for his work during collecting clinical data.
Footnotes
Ethics, consent, and permissions
The protocol of this study was reviewed and approved by the Research Ethics Committee of Shaanxi Provincial People’s Hospital.
Conflict of interests
None.
Source of support: The study was supported by the National Natural Science Foundation of China (81600646), the Health Research Foundation of Shaanxi Province (2018E011), and the Innovative Talents Promotion Project of Shaanxi Province (2019KJXX-019)
References
- 1.Arnson Y, Rozanski A, Gransar H, et al. Comparison of the coronary artery calcium score and number of calcified coronary plaques for predicting patient mortality risk. Am J Cardiol. 2017;120:2154–59. doi: 10.1016/j.amjcard.2017.09.001. [DOI] [PubMed] [Google Scholar]
- 2.Marso SP, McGuire DK. Coronary revascularization strategies in patients with diabetes and multivessel coronary artery disease: Has the final chapter been written? J Am Coll Cardiol. 2014;64:1198–201. doi: 10.1016/j.jacc.2014.07.022. [DOI] [PubMed] [Google Scholar]
- 3.Sianos G, Morel MA, Kappetein AP, et al. The SYNTAX Score: An angiographic tool grading the complexity of coronary artery disease. EuroIntervention. 2005;1:219–27. [PubMed] [Google Scholar]
- 4.Serruys PW, Onuma Y, Garg S, et al. Assessment of the SYNTAX score in the Syntax study. EuroIntervention. 2009;5:50–56. doi: 10.4244/eijv5i1a9. [DOI] [PubMed] [Google Scholar]
- 5.Valgimigli M, Serruys PW, Tsuchida K, et al. Cyphering the complexity of coronary artery disease using the syntax score to predict clinical outcome in patients with three-vessel lumen obstruction undergoing percutaneous coronary intervention. Am J Cardiol. 2007;99:1072–81. doi: 10.1016/j.amjcard.2006.11.062. [DOI] [PubMed] [Google Scholar]
- 6.Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360:961–72. doi: 10.1056/NEJMoa0804626. [DOI] [PubMed] [Google Scholar]
- 7.Serruys PW, Onuma Y, Garg S, et al. 5-year clinical outcomes of the ARTS II (Arterial Revascularization Therapies Study II) of the sirolimus-eluting stent in the treatment of patients with multivessel de novo coronary artery lesions. J Am Coll Cardiol. 2010;55:1093–101. doi: 10.1016/j.jacc.2009.11.049. [DOI] [PubMed] [Google Scholar]
- 8.Capodanno D, Di Salvo ME, Cincotta G, et al. Usefulness of the SYNTAX score for predicting clinical outcome after percutaneous coronary intervention of unprotected left main coronary artery disease. Circ Cardiovasc Interv. 2009;2:302–8. doi: 10.1161/CIRCINTERVENTIONS.108.847137. [DOI] [PubMed] [Google Scholar]
- 9.van Gaal WJ, Ponnuthurai FA, Selvanayagam J, et al. The Syntax score predicts peri-procedural myocardial necrosis during percutaneous coronary intervention. Int J Cardiol. 2009;135:60–65. doi: 10.1016/j.ijcard.2008.03.033. [DOI] [PubMed] [Google Scholar]
- 10.Ikeno F, Brooks MM, Nakagawa K, et al. SYNTAX score and long-term outcomes: The BARI-2D trial. J Am Coll Cardiol. 2017;69:395–403. doi: 10.1016/j.jacc.2016.10.067. [DOI] [PubMed] [Google Scholar]
- 11.Wykrzykowska JJ, Garg S, Girasis C, et al. Value of the SYNTAX score for risk assessment in the all-comers population of the randomized multicenter LEADERS (Limus Eluted from A Durable versus ERodable Stent coating) trial. J Am Coll Cardiol. 2010;56:272–77. doi: 10.1016/j.jacc.2010.03.044. [DOI] [PubMed] [Google Scholar]
- 12.Akturk E, Askin L, Tasolar H, et al. Comparison of the predictive roles of risk scores of in-hospital major adverse cardiovascular events in patients with non-ST elevation myocardial infarction undergoing percutaneous coronary intervention. Med Princ Pract. 2018;27:459–65. doi: 10.1159/000489399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stone GW, Sabik JF, Serruys PW, et al. Everolimus-eluting stents or bypass surgery for left main coronary artery disease. N Engl J Med. 2016;375:2223–35. doi: 10.1056/NEJMoa1610227. [DOI] [PubMed] [Google Scholar]
- 14.Frank ST. Ear-crease sign of coronary disease. N Engl J Med. 1977;297:282. doi: 10.1056/NEJM197708042970516. [DOI] [PubMed] [Google Scholar]
- 15.Frank ST. Aural sign of coronary-artery disease. N Engl J Med. 1973;289:327–28. doi: 10.1056/nejm197308092890622. [DOI] [PubMed] [Google Scholar]
- 16.Lin AN, Lin K, Kyaw H, Abboud J. A myth still needs to be clarified: A case report of the Frank’s sign. Cureus. 2018;10:e2080. doi: 10.7759/cureus.2080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Del Brutto OH, Mera RM, Zambrano M, Costa AF. The association between earlobe crease (Frank’s sign) and cognitive performance is related to age. Results from the Atahualpa Project. Arch Gerontol Geriatr. 2018;79:104–7. doi: 10.1016/j.archger.2018.08.008. [DOI] [PubMed] [Google Scholar]
- 18.Davis TM, Balme M, Jackson D, et al. The diagonal ear lobe crease (Frank’s sign) is not associated with coronary artery disease or retinopathy in type 2 diabetes: the Fremantle Diabetes Study. Aust NZ J Med. 2000;30:573–77. doi: 10.1111/j.1445-5994.2000.tb00858.x. [DOI] [PubMed] [Google Scholar]
- 19.Pan S, Liu ZW, Lv Y, et al. Association between neutrophilic granulocyte percentage and depression in hospitalized patients with heart failure. BMC Psychiatry. 2016;16:446. doi: 10.1186/s12888-016-1161-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pan S, Liu ZW, Shi S, et al. Hamilton rating scale for depression-24 (HAM-D24) as a novel predictor for diabetic microvascular complications in type 2 diabetes mellitus patients. Psychiatry Res. 2017;258:177–83. doi: 10.1016/j.psychres.2017.07.050. [DOI] [PubMed] [Google Scholar]
- 21.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–115. doi: 10.1161/HYP.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 22.American Diabetes Association. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes – 2018. Diabetes Care. 2018;41:S13–27. doi: 10.2337/dc18-S002. [DOI] [PubMed] [Google Scholar]
- 23.Wakasugi M, Kazama JJ, Kawamura K, et al. Prevalence of earlobe creases and their association with history of cardiovascular disease in patients undergoing hemodialysis: A cross-sectional study. Ther Apher Dial. 2017;21:478–84. doi: 10.1111/1744-9987.12567. [DOI] [PubMed] [Google Scholar]
- 24.Honma M, Shibuya T, Iwasaki T, et al. Prevalence of coronary artery calcification in Japanese patients with psoriasis: A close correlation with bilateral diagonal earlobe creases. J Dermatol. 2017;44:1122–28. doi: 10.1111/1346-8138.13895. [DOI] [PubMed] [Google Scholar]
- 25.Bohning D. Youden’s Index and the likelihood ratio positive in diagnostic testing. Methods Inf Med. 2015;54:382–83. doi: 10.3414/ME15-04-0004. [DOI] [PubMed] [Google Scholar]
- 26.Pathmarajah P, Rowland Payne C. Paired ear creases of the helix (PECH): A possible physical sign. Cureus. 2017;9:e1884. doi: 10.7759/cureus.1884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ramos PM, Gumieiro JH, Miot HA. Association between ear creases and peripheral arterial disease. Clinics (Sao Paulo) 2010;65:1325–27. doi: 10.1590/S1807-59322010001200016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang Y, Mao LH, Jia EZ, et al. Relationship between diagonal earlobe creases and coronary artery disease as determined via angiography. BMJ Open. 2016;6:e008558. doi: 10.1136/bmjopen-2015-008558. [DOI] [PMC free article] [PubMed] [Google Scholar]



