Abstract
An 8-year-old boy underwent a STING procedure for vesicoureteric reflux. 11 years later, at 19-years-old he presented with the passage of sediment per urethra every 7 weeks. CT scan demonstrated a lesion at the right VUJ. Cystoscopy revealed a 2cm suburothelial mass adjacent to the VUJ, with normal urothelium overlying it. Resection of the area revealed a white plastic-like substance, consistent with the bulking agent Deflux, which was scraped away. The patient made an uneventful recovery and at review, 3 months later, is symptom free. Our case demonstrates a rare and unusual complication of the STING procedure.
Section headings
Endourology, General Urology, Paediatrics.
Keywords: Vesicoureteric reflux, VUR, STING, Deflux
Introduction
Vesicoureteric reflux (VUR) is the backflow of urine from the bladder in to the ureter and kidneys. It is a common problem and affects 0.5–3% of the paediatric population. In patients with recurrent urinary tract infections (UTI), the incidence is as high as 30–40%.1 When VUR is associated with recurrent UTIs, this can lead to pyelonephritis, renal scarring and renal impairment. Voiding cystourethrography is the preferred investigation and allows grading from grade 1 → 5, according to classification by the International Reflux Study in Children.2 The treatment aim of VUR is to prevent recurrent febrile UTIs and prevent new renal parenchymal damage. Not all VUR requires treatment and this depends on the grade of VUR, symptoms, frequency of febrile UTIs and parental preference.1 Patients with higher grades of VUR are at greater risk of renal scarring, which can have a detrimental effect on kidney development and without treatment can lead to renal impairment.3 Treatment options include continuous antibiotics prophylaxis (CAP), endoscopic procedures and open surgery. The STING procedure (Subureteral Transurethral Injection) is an endoscopic technique involving the submucosal injection of bulking agent just below the intramural portion of the ureter. This results in elevation of the distal ureter and ureteric orifice, leading to narrowing of the ureteric orifice and decreased reflux of urine.3
Case
We describe a case of a 17-year-old boy who presented to the paediatric team with the passage of sediment in his urine every 7 weeks, associated with recurrent penile and urethral pain. Aged 8 years-old, he was investigated for recurrent UTIs and found to have right sided grade-4 VUR. This was treated with a ‘STING’ procedure using dextranomer/hyaluronic acid copolymer (Deflux). At 17 years-old, he started passing sediment per urethra and presented to the paediatric surgery team. Investigations including blood tests and urine were normal. Ultrasound scan (USS) showed normal kidneys and an echobright round focus at the level of the right vescioureteric junction (VUJ). This was felt to be a likely sequela of previous STING procedure. As his symptoms spontaneously resolved, no interventions were undertaken.
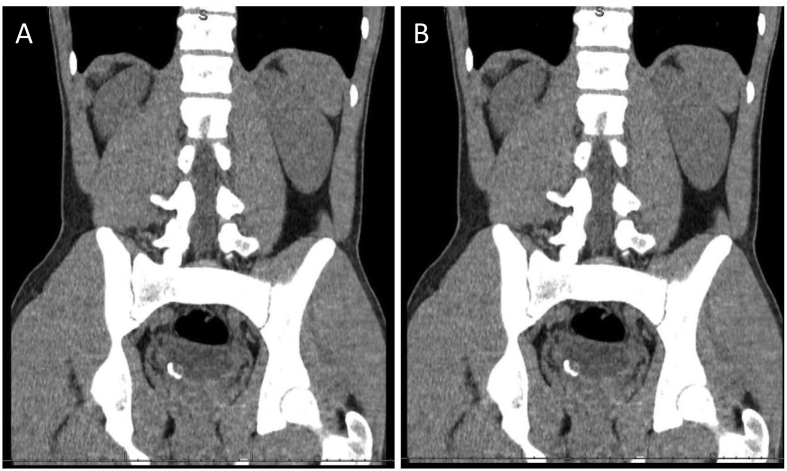
He subsequently presented to adult urology two years later aged 19, with recurrence of his symptoms. Again every 7 weeks, he passed grit and debris per urethra, with recurrent episodes of penile and urethral pain, in the absence of any UTI. A sample of the debris, sent for analysis, was inconclusive and no stone demonstrated. USS again demonstrated a bright area at the VUJ. Differential diagnosis included a stone in a ureterocoele or complication from previous anti-reflux procedure. A CT scan demonstrated a calcified lesion at the right VUJ Fig. 1. Uroradiology review excluded stone disease or ureterocoele, with calcification thought to be related to previous STING procedure. Given the patient's ongoing symptoms a decision was made to perform cystoscopy under general anaesthetic and possible resection of the area.
Fig. 1.
CT scans demonstrating calcified lesion at the right VUJ
A: Pre-operative CT scan non-contrast.
B: Pre-operative CT scan with contrast.
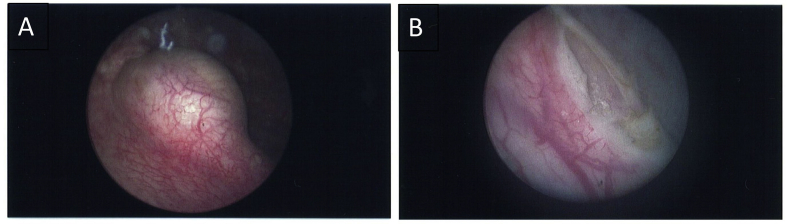
Cystoscopy revealed a 2cm suburothelial mass adjacent to the right VUJ, with normal urothelium overlying it. The ureteric orifice was seen and appeared uninvolved. Resection of the area revealed a white plastic-like substance, consistent with the bulking agent Deflux, which was scraped away leaving a small cavity Fig. 2. The patient made an uneventful recovery and at review, 3 months later, is symptom free.
Fig. 2.
Intraoperative cystoscopy images.
A: Pre-resection demonstrating 2 cm suburothelial mass.
B: Post-resection revealing a small cavity with white plastic-like substance.
Discussion
Vesicoureteric reflux (VUR) is a common paediatric problem, with significant clinical implications including recurrent UTIs and deteriorating renal function. Treatment options include no intervention, CAP, endoscopic procedures and open surgery. There is a limited body of high-level evidence looking at different treatment options for VUR with limited consensus in the correct approach. The European Association of Urology published the most recent guidelines on the management of VUR in children in 2012.3 They concluded that this is a topic that would need re-visiting in years to come due to the lack of high-level evidence. They divided patients with VUR into three risk groups, low, moderate and high, depending on symptoms and grade of reflux. The recommendations for the low and high-risk groups were clear. In the low-risk group, either no treatment or CAP. In the high-risk group, they recommend early intervention and open surgery, which they advised has better results than endoscopic surgery. However, in the moderate-risk group although they recommend early intervention, the choice of intervention between endoscopic and open surgery is controversial and often comes down to surgeon's preference. Citamak et al. carried out a retrospective analysis of 686 patients with VUR, their management consistent with EAU guidelines.4 They found patients treated with open surgery (open reimplantation of the ureter) had a statistically significant greater chance of success compared with endoscopic management, 86–92% compared with 73–75%. Few patients in their high-risk group were treated with STING procedure, so this is most applicable to the low and moderate-risk groups.
Endoscopic management has gained popularity due to its minimal invasiveness. The STING procedure originally used Teflon, however as a result of local and distant migration; Teflon has been replaced with Deflux. VUJ obstruction is a documented complication of the STING procedure, both early and late, with one case describing obstruction 21 years after initial surgery.5
Apart from VUJ obstruction there are few cases of long-term complications from STING procedures. This is the first documented case of debris passed per urethra as a result of previous STING procedure. The rarity of this complication led to delayed diagnosis and thus delays to eventual treatment and symptom resolution. Thankfully due to the nature of the complication, the patient suffered no long-term effects and a simple operation left him symptom free.
Conclusion
Endoscopic management with STING procedure using Deflux has been shown to be a minimally invasive and safe treatment option for VUR. Our case demonstrates a rare and unusual complication of the STING procedure occurring several years after initial operation. Highlighting the need for adult urologists to be mindful that complications may occur several years post treatment and to be aware of the appearance of sub-ureteric mounds that may persist for many years. There is ongoing demand for high-level evidence in this area looking at long term outcomes and complications following VUR treatment.
Contributor Information
Joseph Santiapillai, Email: joseph.santiapillai@nhs.net.
Andrew Symes, Email: andrew.symes@nhs.net.
References
- 1.Starmer B., McAndrew F., Corbett H. A review of novel STING bulking agents. J Pediatr Urol. 2019;15(5):484–490. doi: 10.1016/j.jpurol.2019.08.018. [DOI] [PubMed] [Google Scholar]
- 2.Lebowitz R.L., Olbing H., Parkkulainen K.V., Smellie J.M., Tamminen-Mobius T.E. International system of radiographic grading of vesicoureteric reflux. International Reflux Study in Children. Pediatr Radiol. 1985;15(2):105–109. doi: 10.1007/bf02388714. [DOI] [PubMed] [Google Scholar]
- 3.Tekgul S., Riedmiller H., Hoebeke P. EAU guidelines on vesicoureteral reflux in children. Eur Urol. 2012;62(3):534–542. doi: 10.1016/j.eururo.2012.05.059. [DOI] [PubMed] [Google Scholar]
- 4.Citamak B., Bozaci A.C., Altan M. Surgical outcome of patients with vesicoureteral reflux from a single institution in reference to the ESPU guidelines: a retrospective analysis. J Pediatr Urol. 2019;15(1):73.e1–73.e6. doi: 10.1016/j.jpurol.2018.10.017. [DOI] [PubMed] [Google Scholar]
- 5.Crozier J., Aw I., Tan P.H.M., Clarke D. Taking the STING out of ureteral obstruction. J Endourol Case Rep. 2016;2(1):166–168. doi: 10.1089/cren.2016.0092. [DOI] [PMC free article] [PubMed] [Google Scholar]