Abstract
This cohort study evaluates whether the incorporation of a pain tolerability question augments the information gathered from a numeric rating scale.
Introduction
The exclusive focus of the numeric rating scale (NRS) on pain intensity reduces the experience of chronic pain to a single dimension.1 This drawback minimizes the complex effects of chronic pain on patients’ lives and the trade-offs that are often involved in analgesic decision-making.2 Furthermore, continually asking patients to rate their pain on a scale that is anchored by a pain-free state (ie, 0) implies that being pain free is a readily attainable treatment goal, which may contribute to unrealistic expectations for complete relief.3 We hypothesized that the incorporation of a standardized pain tolerability question (PTQ) (ie, “is your pain tolerable?”) would efficiently augment the information gleaned from the NRS and help to align patients’ expectations with realistic treatment goals.
Methods
This cohort study was reviewed and approved by the University of Rochester Research Subjects Review Board with informed consent waived, given that the research presented no more than minimal risk and involved no procedures for which written consent is normally required outside the research context. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline. Participants were recruited electronically after a primary care encounter at 1 of 157 participating primary practices from December 2016 to March 2017. Eligible patients had an active prescription for an analgesic medication or an International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) visit diagnosis associated with chronic pain in their electronic health record, which was adapted using a previously validated ICD-9 chronic pain filter.4 Patients were asked the PTQ “is your pain tolerable?” (yes, no, or not in pain) and asked to rate average pain intensity during the past 24 hours, with 0 indicating no pain and 10 indicating the worst pain imaginable. To assess construct validity of the PTQ, responses to the question “is your pain tolerable?” were compared with responses on the NRS scale using logistic regression. Data analysis was conducted in February 2020 using JMP Pro version 14 (SAS Institute). Statistical significance was set at P < .05, and all tests were 2-tailed.
Results
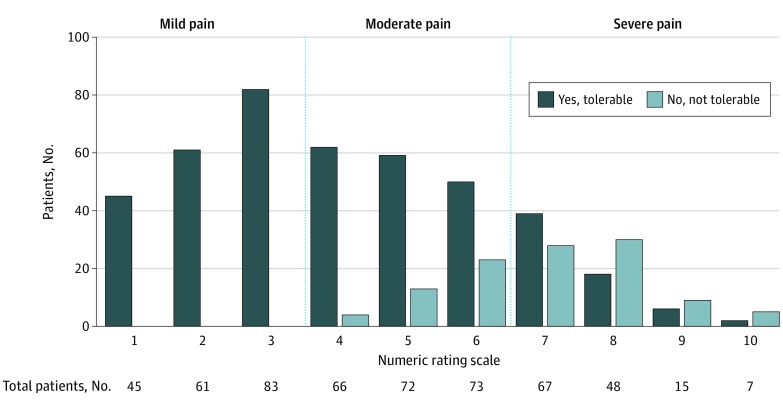
In total, 1384 patients were invited to participate in the survey including the NRS and PTQ; 663 patients (47.9%) responded. Of those, 124 reported a 0 on the NRS or responded not in pain to the PTQ and were excluded. Two additional participants failed to complete the NRS, leaving a final analytic sample of 537 patients, with a median (interquartile range) age of 62.2 (54.0-71.0) years and 206 (38.4%) men (Table). Of these, 202 patients (37.8%) had more than 1 chronic pain diagnosis; the leading diagnosis was musculoskeletal pain (eg, osteoarthritis or soft-tissue disorder), with 295 patients (54.9%). A pain rating of intolerable was associated with higher NRS scores (odds ratio per 1-point increase on NRS, 1.1; 95% CI, 1.02-1.2; P = .01) (Figure). In the moderate range of the NRS (ie, 4-6), 40 of 211 patients (19.0%) characterized their pain as intolerable, whereas in the severe range of the NRS (ie, 7-10), 72 of 137 patients (52.6%) considered it intolerable.
Table. Demographic Characteristics.
| Characteristic | No. (%) |
|---|---|
| Age, median (IQR), y | 62.2 (54.0-71.0) |
| Sex | |
| Women | 331 (61.6) |
| Men | 206 (38.4) |
| Diagnosis familya | |
| Diseases of the musculoskeletal system and connective tissue | 295 (54.9) |
| Diseases of the spine | 188 (35.0) |
| Diseases of the nervous system and diabetic neuropathy | 75 (14.0) |
| Migraine or headache | 80 (14.9) |
| Other chronic pain | 59 (11.0) |
| Pelvic or abdominal pain | 17 (3.2) |
Abbreviation: IQR, interquartile range.
International Statistical Classification of Diseases and Related Health Problems, Tenth Revision codes for each category were as follows: diseases of the musculoskeletal system and connective tissue, M15 to M19, M25, M70 to M79; diseases of the spine, M45 to M54, M96.1; diseases of the nervous system and diabetic neuropathy, G90.5, G50 to G63, E10.4, E11.4; migraine or headache, G43, G44, R51; other chronic pain, G89.2, G89.4, R52; and pelvic or abdominal pain, N94, R10.1 to 10.3.
Figure. Patient Ratings of Pain Tolerability and Pain Score.
Discussion
The overarching goal of chronic pain treatment is to make pain tolerable for the patient rather than to attain a targeted numeric rating. Our findings confirmed the intuitive assumption that most patients with low pain intensity (ie, NRS score, 1-3) find their pain tolerable. In contrast, the tolerability of pain rated between 4 and 6 varies substantially among patients. In this middle range, if a patient describes pain as tolerable, this might decrease the clinician’s inclination to initiate higher-risk treatments.5 A substantial subgroup of patients with severe pain reported their symptoms as tolerable.
Discordance between tolerability and pain intensity may be an opening for a clinician to explore mood, sleep disruption, or the curtailing of activities to control pain. Asking patients with chronic pain about pain tolerability directly addresses the main limitation of the NRS, which asks patients to rate a complex, highly subjective experience on a unidimensional intensity scale. A limitation of this study is that patients could have had flares of chronic pain or superimposed acute pain episodes at the time of assessment. Research related to the associations of using the PTQ with patient satisfaction regarding communication, treatment goal setting, and treatment effects could further characterize the value of the PTQ.
References
- 1.Ballantyne JC, Sullivan MD. Intensity of chronic pain—the wrong metric? N Engl J Med. 2015;373(22):-. doi: 10.1056/NEJMp1507136 [DOI] [PubMed] [Google Scholar]
- 2.Lucas CE, Vlahos AL, Ledgerwood AM. Kindness kills: the negative impact of pain as the fifth vital sign. J Am Coll Surg. 2007;205(1):101-107. doi: 10.1016/j.jamcollsurg.2007.01.062 [DOI] [PubMed] [Google Scholar]
- 3.Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27(1):117-126. doi: 10.1016/0304-3959(86)90228-9 [DOI] [PubMed] [Google Scholar]
- 4.Clark LL, Taubman SB. Brief report: incidence of diagnoses using ICD-9 codes specifying chronic pain (not neoplasm related) in the primary diagnostic position, active component, US Armed Forces, 2007-2014. MSMR. 2015;22(12):12-15. [PubMed] [Google Scholar]
- 5.Dartmouth Atlas Project. Preference-sensitive care. Accessed March 16, 2020. https://www.dartmouthatlas.org/downloads/reports/preference_sensitive.pdf