Abstract
Ischiofemoral space (IFS) is a radiological parameter employed for diagnosing ischiofemoral impingement (IFI). The mean IFS value measured with the leg in natural resting position has been reported as 23.0 mm in males and 18.6 mm in females in a patients-based Western population. The normal value of IFS for an Asian population is unknown. This study therefore aimed to investigate whether the IFS value in Japanese hip joints equals that of the Western population. We retrospectively examined 89 consecutive Japanese individuals (178 hips) (46 male subjects with 92 hips, 43 female subjects with 86 hips; mean age 58.7 ± 15.7 years, range 17–84 years) who had undergone computed tomography (CT) for conditions unrelated to hip disorders and ordered by other departments at our institution. All CT scans were performed in a standardized fashion: patient in a flat spine position, hips and knees in extension, and the leg in its natural resting position. IFS was evaluated on axial images as the shortest distance between the ischium and the lesser trochanter. The mean IFSs of this Japanese patient-based population were 20.5 ± 7.3 mm [95% confidence interval (CI) 19.0–22.0] in the male cohort and 13.9 ± 6.5 mm (95% CI 12.6–15.3) in the female cohort. The IFS value was significantly smaller in female subjects than in male subjects. Taking the lower limit of 95% CI into consideration, the IFSs measured in natural leg-resting position in the Japanese male and female groups were significantly smaller than those of the Western populations.
INTRODUCTION
Ischiofemoral impingement (IFI), first reported by Johnson [1], is a rare entity with groin and/or buttock pain that has been exacerbated by a combination of extension, abduction and external rotation of the hip joint [2]. IFI symptoms are thought to be due to a compressive injury to the quadratus femoris caused by narrowing of the space between the lesser trochanter and the ischial tuberosity [3–6]. Ischiofemoral space (IFS)—i.e. the shortest distance between the ischium and the lesser trochanter—is the most used radiological parameter for diagnosing IFI [3]. Torriani et al. [3] reported cutoff values for diagnosing IFI based on the results of their case–control studies: IFS ≤17 mm yielded a sensitivity of 83% and specificity of 82%.
In a patient-based Western population, the mean IFS value was 23.0 mm in men and 18.6 mm in women, according to Hujazi et al. [7]. These authors investigated 149 patients who underwent computed tomography (CT) at their institution for any pathology unrelated to the hip. Each CT scan was performed in a standardized fashion: the pelvis squared, hips and knees in extension, and the subject’s feet in their natural resting position with no external deforming force or supporting equipment. The normal IFS value for an Asian population was never reported and is still not known. Hence, the aim of this study was to identify the mean IFS value measured in the leg-resting position in Japanese unaffected hip joints and then to compare it with that of the reported Western population.
MATERIALS AND METHODS
Patients and measurements
The ethics committee of our institution approved the study protocol. We conducted the study on patients who had undergone CT imaging that included hip joints. Each CT scan had been requested by another department at our institution for a condition unrelated to a hip disorder. We retrospectively confirmed the clinical information with the patients’ medical records. We retrospectively reviewed the CT scans of 159 patients conducted during 1–31 July 2013. The exclusion criteria were as follows (Fig. 1): (i) age <17 years; (ii) patients with presumed inability to control the usual leg position (e.g. consciousness disorder, trauma); (iii) reconstructed axial slice thickness >2 mm (poor resolution); (iv) osteoarthritic change of the hip joint and previous hip surgery; (v) abnormal pelvic rotation and tilt, which did not meet the standard of each three planes described in the section ‘Radiological examination and standardization of CT images’; and (vi) history of hip pain.
Fig. 1.
Flow chart of the process of patient selection.
We retrospectively examined 89 consecutive Japanese individuals (46 male and 43 female subjects) who met the above criteria. Both hips were analysed in each patient. IFS was measured as the shortest distance (on an axial image) between the lateral ischial bone surface and the medial bone surface of the lesser trochanter (Fig. 2). We established the mean IFS value in this cohort and then compared it with that reported by Hujazi et al. [7], whose measurements were of a similar cohort using the same examination protocol.
Fig. 2.
Method for measuring ischiofemoral space (IFS). The IFS (*) was measured as the shortest distance between the lateral bone surface of the ischium and the medial bone surface of the lesser trochanter.
Distribution of hips into seven groups according to hip rotation
Our cohort was then distributed into several groups taking hip rotation (femoral rotation associated with lower limb position) into consideration. We measured the width of the lesser trochanter using a three-dimensional (3D) scout view (Fig. 3) following the method reported by Zhang et al. [8]. Then, according to their proposed formula for relating the width of the lesser trochanter and hip rotation, we divided our cohort into seven groups according to the Zhang et al. formulas, as follows (with the internal rotation being ‘minus’ and the external rotation being ‘plus’).
Fig. 3.
Measuring the width of the lesser trochanter using a 3D scout view. A and B are ends of the base of the lesser trochanter base. A–B line represents the width of the lesser trochanter.
Formula for male subjects: width of the lesser trochanter =35.0 ±0.5 mm ×hip rotation angle.
Formula for female subjects: width of the lesser trochanter =30.1 ± 0.5 mm× hip rotation angle.
Excessive internal rotation (EIR) group: hip internally rotated >25°; i.e. width of lesser trochanter ≤22.5 mm in male subjects and ≤17.6 mm in female subjects.
Moderate internal rotation (MIR) group: hip internally rotated 15°–25°; i.e. width of lesser trochanter ranged from ≤27.5 to >22.5 mm in male subjects and from ≤22.6 to >17.6 mm in female subjects (Fig. 4).
Slight internal rotation (SIR) group: hip internally rotated 5°–15°; i.e. width of lesser trochanter ranged from ≤32.5 to >27.5 mm in male subjects and from ≤27.6 to >22.6 mm in female subjects.
Neutral rotation (NR) group: hip rotation was from 5° internal rotation to 5° external rotation; i.e. width of lesser trochanter ranged from ≤37.5 to >32.5 mm in male subjects and from ≤32.6 to >27.6 mm in female subjects (Fig. 5).
Slight external rotation (IER) group: hip externally rotated 5°–15°; i.e. width of lesser trochanter ranged from ≤42.5 to >37.5 mm in male subjects and from ≤37.6 to >32.6 mm in female subjects.
Moderate external rotation (MER) group: hip externally rotated 15°–25°; i.e. width of lesser trochanter ranged from ≤47.5 to >42.5 mm in male subjects and from ≤42.6 to >37.6 mm in female subjects.
Excessive external rotation (EER) group: hip externally rotated >25°; i.e. width of lesser trochanter was >47.5 mm in male subjects and >42.6 mm in female subjects.
Fig. 4.
Case presentation of moderate internal rotation. The width of the lesser trochanter was 20.8 mm. According to the formula of Zhang et al. [8], this hip was estimated to be internally rotated 18.6°.
Fig. 5.
Case presentation of neutral rotation. The width of the lesser trochanter was 28.8 mm. According to the formula of Zhang et al. [8], this hip was estimated to be internally rotated 2.6°.
Radiological examination and standardization of CT images
All CT scans had been performed in a standardized fashion—patient in flat spine position, hips and knees in extension, and the leg in its natural resting (relaxed) position with no external force (i.e. as reported by Hujazi et al. [7])—using a Toshiba Aquilion CX (Toshiba Medical Systems, Tokyo, Japan). The data were reconstructed under conditions suitable for bone evaluation using AquariusNET Viewer software (TeraRecon, San Francisco, CA, USA). This software allowed reconstruction of 3D CT views, which were used to confirm pelvic tilt and rotation: (i) rotation of the coronal plane (to subjectively investigate the symmetric appearance of the tear drop signs, the obturator foramina and the iliac wing) [9]; (ii) rotation of the axial plane (to subjectively determine whether the tip of the coccyx was above the pubic symphysis) [9] and (iii) tilt of the sagittal plane (to investigate the distance between the upper border of the symphysis and the mid-portion of the sacrococcygeal joint, as previously described) [9]. In the present study, we defined that pelvic tilts were considered neutral at 32 ± 10 mm in male subjects and 47 ± 10 mm in female subjects, based on the report of Ganz et al. [9].
Evaluation of the interobserver and intraobserver reliability in measuring the IFS
Interobserver reliability between the first (T.M.) and second (K.M.) observers and intraobserver reliability between the first and second assessments (T.M.) were evaluated for the first 20 consecutive cases.
Statistical analysis
All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R software (The R Foundation for Statistical Computing, Vienna, Austria) [10]. More precisely, it is a modified version of R commander, which is designed to add statistical functions frequently used in biostatistics. An a priori power analysis was conducted on the difference in the IFS values in males and females reported by Hujazi et al. [7]. For a power of 0.8, we needed 46 cases of each sex for our study. The 95% confidence interval (CI), based on the score test for value, was estimated. Intraclass correlation coefficients (ICCs) were calculated to evaluate interobserver and intraobserver reliability. The significance of differences between men and women was evaluated using the Mann–Whitney U test. A one-way analysis of variance with the Tukey–Kramer post hoc test was used to determine significant differences among several groups. Values of P < 0.05 were considered to indicate statistical significance.
RESULTS
After excluding 70 patients according to the excrusion criteria, a total of 178 hips (92 male hips, 86 female hips) were evaluated (Fig. 1). The background characteristics of our cohort are shown in Table I. The height and weight of females were significantly less than those of males. The mean IFS measured in the natural leg-resting position of the Japanese patient-based population was overall 17.2 ± 7.7 mm (95% CI 16.1–18.3); male subjects 20.5 ± 7.3 mm (95% CI 19.0–22.0); female subjects 13.9 ± 6.5 mm (95% CI 12.6–15.3). The IFS value was significantly smaller in the female subjects than in the male subjects (P < 0.0001). Because the mean value of IFSs of the Western patient-based population were previously reported as 23.0 mm (male) and 18.6 mm (female) in the same examination protocol, taking the lower limit of 95% CI into consideration, the IFS of the Japanese patient-based population was significantly smaller than that of the Western population, especially in the female cohort.
Table I.
Background characteristics of the cohort
| Characteristic | Male (n = 92 hips) | Female (n = 86 hips) | P * |
|---|---|---|---|
| Age (years) | 60.4 ± 15.9 (21–83) | 56.4 ± 15.3 (17–84) | 0.0519 |
| Height (cm) | 165.4 ± 7.8 (152–183) | 156.0 ± 7.4 (139–172) | <0.0001 |
| Weight (kg) | 59.5 ± 11.9 (35–86) | 54.3 ± 11.7 (36–99) | 0.0002 |
| Body mass index (kg/m2) | 21.7 ± 3.5 (13.7–30.1) | 22.4 ± 5.0 (14.2–42.6) | 0.996 |
Results are given as the mean ± SD (range).
The significance of differences between the two groups was evaluated using the Mann–Whitney U test. P < 0.05 was considered to indicate statistical significance.
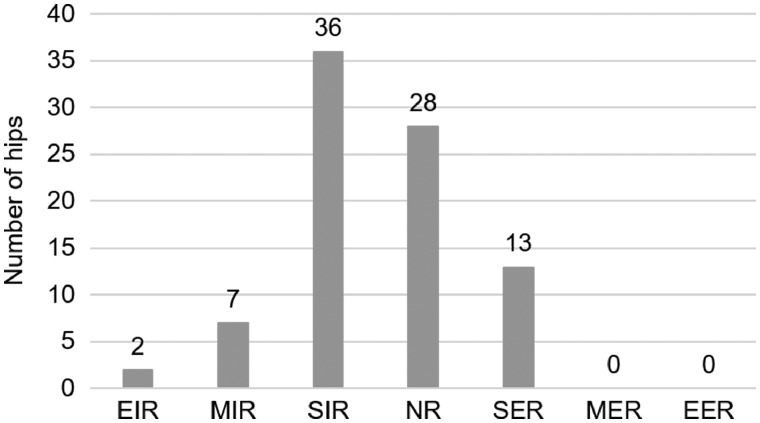
The distribution of the various hip joint designations (i.e. EIR, MIR, SIR, NR, SER, MER, EER) are shown in Fig. 6 (male subjects) and Fig. 7 (female subjects). The distributions (numbers of patients) of each group were similar between the sexes. The number was largest in the SIR group, followed by the NR group for both sexes. None of the patients met the criteria for the EER group, and no MER hip was detected in the female cohort.
Fig. 6.
Distribution of number of the hip joints of seven male groups, created according to the degree of hip rotation (estimated from the width of the lesser trochanter).
Fig. 7.
Distribution of the number of the hip joints of seven female groups, created according to the degree of hip rotation (estimated from the width of the lesser trochanter).
Table II shows the mean IFS values for the group formed according to hip rotation, which was estimated from the width of the lesser trochanter. The mean IFS value gradually decreased according to the hip rotation, from internal rotation to external rotation, for both sexes. We did not detect a significant difference among the designated hip rotation groups for the female subjects. In contrast, there was a significant difference among the hip groups for the male subjects (P = 0.00076). That significant difference, however, was detected only between the SER and EIR groups (P = 0.0178) and the SIR and SER groups (P = 0.0048).
Table II.
Ischiofemoral space in each group a
| Participants | EIR group | MIR group | SIR group | NR group | SER group | MER group | P |
|---|---|---|---|---|---|---|---|
| Men (n=92 hips) | 32.2 ± 10.2 | 23.3 ± 3.8 | 23.1 ± 6.3 | 19.7 ± 7.0 | 15.8 ± 6.1 | 14.6 ± 3.1 | 0.0178*, |
| (22.0–42.4) | (17.4–29.0) | (10.8–35.8) | (8.3–33.4) | (5.8–26.2) | (10.9–18.5) | ||
| (n=2) | (n=5) | (n=33 | (n=31) | (n=18) | (n=3) | 0.0048** | |
| Women (n=86 hips) | 20.2 ± 4.9 | 16.2 ± 7.9 | 15.1 ± 7.2 | 12.2 ± 5.1 | 12.1± 4.4 | – | ns |
| (15.3–25.1) | (7.1–28.5) | (4.8–35.0) | (3.7–26.2) | (3.2–18.0) | – | ||
| (n=2) | (n=7) | (n=36) | (n=28) | (n=13) |
Results are given as the mean±SD (range). None of the participants exhibited excessive external rotation. One-way analysis of variance (ANOVA) with the Tukey–Kramer post hoc test was used to determine the significant difference between groups, except for EER in men and MER and EER in women. Values of P < 0.05 were considered to indicate statistical significance.
The groups were created according to hip rotation, which was estimated from the width of the lesser trochanter.
Significant difference between EIR and SER.
Significant difference between SIR and SER.
EIR, excessive internal rotation; MIR, moderate internal rotation; SIR, slight internal rotation; NR, neutral rotation; SER, slight external rotation; MER, moderate external rotation; ns, not significant.
The ICC values for intraobserver and interobserver reliability was 0.85 and 0.83, respectively.
DISCUSSION
Previous reports describing the normal value or cutoff value of IFI radiological parameters were all from regions that did not include Asian populations. In the present study, we intended to report the IFS value measured with the leg in resting position for a Japanese population. During our efforts, we revealed that the IFS value measured in this position was significantly smaller than that for Western populations and that it was significantly smaller for female Japanese than for their male counterparts. We therefore believe that we should pay more attention to IFI when we are confronted with groin and/or buttock pain in Japan, especially in the female population.
Hujazi et al. [7] reported the normal IFS value for patients in an English-language population using CT with the leg in a natural resting (relaxed) position. They reviewed 149 patients (298 hips) who had a CT scan of their pelvis for non-orthopedic (abdominopelvic) pathology. They reported that the mean male and female IFS values were 23.0 ± 7.0 mm and 18.6 ± 8.0 mm, respectively, and the female value was significantly smaller than the male value. In the present study, we evaluated the IFS in a similar (but Japanese) population using the same investigative manners as in their report and then compared our values with their results. We showed that the Japanese IFS was significantly smaller than that of the Western IFS value and that the IFS value was significantly smaller for the female subjects than for the male subjects. We surmised that the differences could be explained by the smaller physique of the Japanese population compared with that of the Western population. In addition, the fact that the IFS in our female Japanese subjects was smaller than that in the male Japanese subjects is understandable given the dimensions of each physical feature (Table I) and in line with previous reports from Western countries [3, 7, 11].
The most suitable hip rotation (leg rotation) for examining patients for IFS remains controversial. Torriani et al. [3] reported cutoff values of IFS with the patient in an internally rotated position, but they provided no description of the degree of internal rotation used. Tosun et al. [12] and Ohnishi et al. [13] employed neutral rotation. Tosun et al. [12] positioned the subject’s hip relative to the position of the patella and maintained the foot facing directly upward by adhesive-taping the subject’s feet. Ohnishi et al. [13] did not define ‘neutral rotation’ of the hip. In contrast, Hujazi et al. [7] employed a natural resting rotation with no external deforming force or supporting equipment. They advocated that the leg-resting position was suitable for measuring the radiological parameter because it was difficult and unreasonable to judge hip rotation based on knee and foot positions [7]. We agree. We also think that control of foot rotation cannot always directly control hip rotation (femoral rotation) because of the joint flexibility of the knee and ankle joints if the foot rotation is set at an objective angle.
To evaluate the validity of measuring the IFS in resting position, we investigated the distribution of hip rotation (the tendency of femoral rotation) under the natural leg-resting position. Although Gollwitzer et al. [14] stated that the relaxed position meant ‘most likely external rotated’, the hip rotation itself (estimated based on the width of the lesser trochanter) in our cohort unexpectedly showed a tendency toward internal rotation, rather than external rotation. Surprisingly, none of the male cohort in our study showed EER, and none of the female subjects were found to have MER or ERR. Furthermore, ∼89% of both male and female cohorts were in the SIR, NR and SER categories (from 15° internal rotation to 15° external rotation). As a result, the method for measuring IFS in the natural leg-resting position, with hips and knees in extension, might be expected to be transferable as a position for measuring radiological parameters of IFI. Our results, however, showed that there was some variation in hip rotation in the natural leg-resting position to some extent. Therefore, we do not wholly recommend the neutral leg-resting position as suitable for measuring the IFS.
In the present study, the mean IFS value changed with the degree of hip rotation (estimated from the width of the lesser trochanter). It gradually decreased in both genders according to the hip rotation, from internal rotation to external rotation. These results were compatible with those from previous reports [7, 15, 16]. Hujazi et al. [7] compared the IFS in 40° internal rotation and 50° external rotation. Kivlan et al. [15] directly measured the IFS using calipers and compared the results between 40° internal rotation and 60° external rotation. Finnoff et al. [16] compared the IFS in 30° internal rotation and 30° external rotation. In the present study, a significant difference was detected in the male cohort. Surprisingly, there was no significant difference in the female cohort. We consider this finding as new knowledge because no previous report has shown the variations in IFS according to the detailed consecutive hip rotation positions as in the current study. Additional detailed research considering the distinction of sex is warranted to assess how the degree hip rotation influences the significant changes seen in the radiological parameters of IFI.
Finnoff et al. [16] compared the IFS in 15° abduction, neutral position and 15° adduction. The IFS in hip abduction was significantly larger than in the neutral or adducted position. Shoji et al. [17] stated that posterior pelvic tilt is a risk factor for posterior impingement after total hip arthroplasty. To evaluate the IFS more exactly, in this study we contorted pelvic alignment. We employed only individuals in whom pelvic alignment was considered normal. We believe that IFS value is affected not only by the lower limb position (femoral position) but also pelvic alignment, although previous reports measuring radiological IFI parameters did not mention this important concern. We suggest that pelvic alignment should be taken into consideration when measuring radiological IFI parameters. As a future prospect, we strongly suggest that a worldwide, unified, standard measurement method for radiological IFI parameters should be established not only for lower limb control (internal–external rotation and abduction–adduction) but also pelvic alignment. Although the problem of radiation exposure, we consider that CT examination, which can verify the alignment of pelvis and lower limb, is desirable for accurate measurement of IFI parameters. To this end, we should take CT images of the knee joint (and thereby, e.g. check the patella position and/or the alignment of the posterior condyle line of the femur). We believe that examining the subject in this manner will help put an end to the discussion regarding accurate posture during radiological examination for IFI. If CT examination is employed for evaluation of IFI in future studies, we hope that suitable and satisfactory discussion will aim to fulfill the measurement approach described herein. Furthermore, we strongly believe that we should distinguish the sex, when we talk about cutoff values of radiological parameters for diagnosing IFI because the differences in IFS values in men and women is significant. Additionally, we emphasize that the actual diagnosis of IFI should be arrived at through the several physical examinations specific to IFI [18, 19].
This study has some limitations. First, we could not confirm that the leg positions in the two studies (our study and that of Hujazi et al.) were exactly the same because both studies were retrospective. Second, the rotation angle of the hip joint was an indirect angle that was estimated based on the formula for the width of the lesser trochanter. We understand that the position, size, and shape of the lesser trochanter is different to some extent in each individual. Furthermore, the formula for the width of the lesser trochanter and hip rotation reported by Zhang et al. [8] was based on plain radiography, although we used their formula for the 3D scout view. Nevertheless, we believed that we could assess the tendency of hip rotation in the natural leg-resting position by using this formula. Third, the numbers of patients in the EIR and MER groups were small. If more individuals had been investigated, the statistical results might be different.
In conclusion, the mean value of IFS measured in natural leg-resting position in a Japanese population was 20.5 ± 7.3 mm in male subjects and 13.9 ± 6.5 mm in female subjects. The female value was significantly smaller than the male value. Taking the lower limit of 95% CI into consideration, the overall IFS measured in the natural leg-resting position in the Japanese population was significantly smaller than that of Western populations.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Johnson KA. Impingement of lesser trochanter on the ischial ramus after total hip arthroplasty: report of three cases. J Bone Joint Surg Am 1977; 59: 268–9. [PubMed] [Google Scholar]
- 2. Stafford GH, Villar RN.. Ischiofemoral impingement. J Bone Joint Surg Br 2011; 93:1300–2. [DOI] [PubMed] [Google Scholar]
- 3. Torriani M, Souto SC, Thomas BJ. et al. Ischiofemoral impingement syndrome: an entity with hip pain and abnormalities of the quadratus femoris muscle. AJR Am J Roentogenol 2009; 193: 186–90. [DOI] [PubMed] [Google Scholar]
- 4. de Sa D, Alradwan H, Cargnelli S. et al. Extra-articular hip impingement: a systematic review examining operative treatment of psoas, subspine, ischiofemoral, and greater trochanteric/pelvic impingement. Arthroscopy 2014; 30: 1026–41. [DOI] [PubMed] [Google Scholar]
- 5. Wilson MD, Keene JS.. Treatment of ischiofemoral impingement: results of diagnostic injection and arthroscopic resection of the lesser trochanter. J Hip Preserv Surg 2016; 26: 146–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cheatham SW. Extra-articular impingement: a narrative review of the literature. J Can Chiropr Assoc 2016; 60: 47–56. [PMC free article] [PubMed] [Google Scholar]
- 7. Hujazi I, Jones T, Johal S. et al. The normal ischofemoral distance and its variations. J Hip Preserv Surg 2016; 3: 197–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zhang Q, Liu H, Chen W. et al. Radiologic measurement of lesser trochanter and its clinical significance in Chinese. Skeletal Radiol 2009; 38: 1175–81. [DOI] [PubMed] [Google Scholar]
- 9. Siebenrock KA, Kalbermatten DF, Ganz R.. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res 2003; 407: 241–28. [DOI] [PubMed] [Google Scholar]
- 10. Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 2013; 48: 452–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tanaja AK, Bredella MA, Torriani M.. Ischiofemoral impingement. Magn Reson Imaging Clin N Am 2013; 21: 65–73. [DOI] [PubMed] [Google Scholar]
- 12. Tosun O, Algin O, Yalcin N. et al. Ischiofemoral impingement: evaluation with new MRI parameters and assessment of their reliability. Skeletal Radiol 2012; 41: 575–87. [DOI] [PubMed] [Google Scholar]
- 13. Ohnishi Y, Suzuki H, Nakashima H. et al. Radiologic correlation between the ischiofemoral space and morphologic characteristics of the hips in hips with symptoms of dysplasia. Am J Roentgenol 2018; 210: 608–14. [DOI] [PubMed] [Google Scholar]
- 14. Gollwitzer H, Banke IJ, Schauwecker J. et al. How to address ischiofemoral impingement? Treatment algorism and review of the literature. J Hip Presev Surg 2017; 4: 289–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kivlan BR, Martin RL, Martin HD.. Ischifemoral impingement: defining the lesser trochanter-ischial space. Knee Surg Sports Traumatol Arthrosc 2017; 25: 72–6. [DOI] [PubMed] [Google Scholar]
- 16. Finnoff JT, Bond JR, Collins MS. et al. Variability of the ischiofemoral space relative to femur position: an ultrasound study. Pm R 2015; 7: 930–7. [DOI] [PubMed] [Google Scholar]
- 17. Shoji T, Yamasaki T, Izumi S. et al. Factors affecting the potential for bony impingement after total hip arthroplasty. Bone Joint J 2017; 99-B: 1140–6. [DOI] [PubMed] [Google Scholar]
- 18. Gómez-Hoyos J, Martin RL, Schröder R. et al. Accuracy of 2 clinical tests for ischiofemoral impingement in patients with posterior hip pain and endoscopically confirmed diagnosis. Arthroscopy 2016; 32: 1279–84. [DOI] [PubMed] [Google Scholar]
- 19. Martin HD, Reddy M, Gómez-Hoyos J.. Deep gluteal syndrome. J Hip Preserv Surg 2015; 2: 99–107. [DOI] [PMC free article] [PubMed] [Google Scholar]