Abstract
Background
There has been increasing interest in both suicide-specific diagnoses within the psychiatric nomenclature and related biomarkers. Because the Suicide Crisis Syndrome—an emotional crescendo of several interrelated symptoms—seems to be promising for the identification of individuals at risk of suicide, the aim of the present paper is to review the putative biological underpinnings of the Suicide Crisis Syndrome symptoms (entrapment, affective disturbance, loss of cognitive control, hyperarousal, social withdrawal).
Methods
A PubMed literature search was performed to identify studies reporting a link between each of the 5 Suicide Crisis Syndrome symptoms and biomarkers previously reported to be associated with suicidal outcomes.
Results
Disturbances in the hypothalamic-pituitary-adrenal axis, with dysregulated corticotropin-releasing hormone and cortisol levels, may be linked to a sense of entrapment. Affective disturbance is likely mediated by alterations in dopaminergic circuits involved in reward and antireward systems as well as endogenous opioids. Loss of cognitive control is linked to altered neurocognitive function in the areas of executive function, attention, and decision-making. Hyperarousal is linked to autonomic dysregulation, which may be characterized by a reduction in both heart rate variability and electrodermal activity. Social withdrawal has been associated with oxytocin availability. There is also evidence that inflammatory processes may contribute to individual Suicide Crisis Syndrome symptoms.
Conclusion
The Suicide Crisis Syndrome is a complex syndrome that is likely the consequence of distinct changes in interconnected neural, neuroendocrine, and autonomic systems. Available clinical and research data allow for development of empirically testable hypotheses and experimental paradigms to scrutinize the biological substrates of the Suicide Crisis Syndrome.
Keywords: acuity, biomarkers, review, suicide
Significance Statement.
The Suicide Crisis Syndrome (SCS)—an emotional crescendo of several interrelated symptoms—seems to be promising for the identification of individuals at risk of suicide. Hence, we reviewed the putative biological underpinnings of the SCS symptoms (entrapment [A], affective disturbance [B], loss of cognitive control [C], hyperarousal [D], social withdrawal [E]). Disturbances in the hypothalamic-pituitary-adrenal axis, with dysregulated corticotropin-releasing hormone and cortisol levels, may be linked to A. B is likely mediated by alterations in dopaminergic circuits involved in reward and anti-reward systems as well as endogenous opioids. C is linked to altered neurocognitive function in the areas of executive function, attention, and decision-making. D is linked to autonomic dysregulation, which may be characterized by a reduction in both heart rate variability and electrodermal activity. E has been associated with oxytocin availability. Available data allow for development of empirically testable hypotheses and experimental paradigms to scrutinize the SCS biological substrates.
Introduction
New diagnoses describing presuicidal mental states may facilitate research in mental processes that make suicide possible and may also help to correctly identify individuals at suicide risk to better target suicide prevention efforts. Three diagnoses have been proposed to date. The Suicidal Behavior Disorder (Oquendo and Baca-Garcia, 2014), focused on a suicide attempt (SA) within the past 2 years, was included among conditions needing further study in the Diagnostic and Statistical Manual of Mental Disorders—5th edition (DSM-5) (American Psychiatric Association, 2013). The Suicide Crisis Syndrome (SCS) (Galynker et al., 2017) and the Acute Suicidal Affective Disturbance (ASAD) (Rogers et al., 2017) describe an acute presuicidal mental state, are more recent, and are not present in the DSM-5. The 2 syndromes overlap symptomatically but are also quite different in that SCS does not include suicidal ideation (SI) while ASAD is based on rapidly escalating SI (Joiner et al., 2018; Rogers et al., 2019; Schuck et al., 2019).
In 2009 Galynker and Yaseen initiated research into the SCS based on the pioneering work of Fawcett and colleagues, who were among the first researchers to differentiate near-term risk factors for suicide from long-term risk factors (Fawcett et al., 1990). The term “suicide crisis” was introduced later by Hendin et al., who described “an emotional crescendo of several different but interrelated painful feelings” preceding suicide (Hendin et al., 2007). Galynker and Yaseen have coined the name SCS in homage to this early work of Hendin and others. For a detailed description of the intermediate steps between the first SCS concept and the subsequent delineation of the proposed DSM criteria for SCS, see (Yaseen et al., 2010, 2012, 2016, 2018; Galynker et al., 2017; Li et al., 2018).
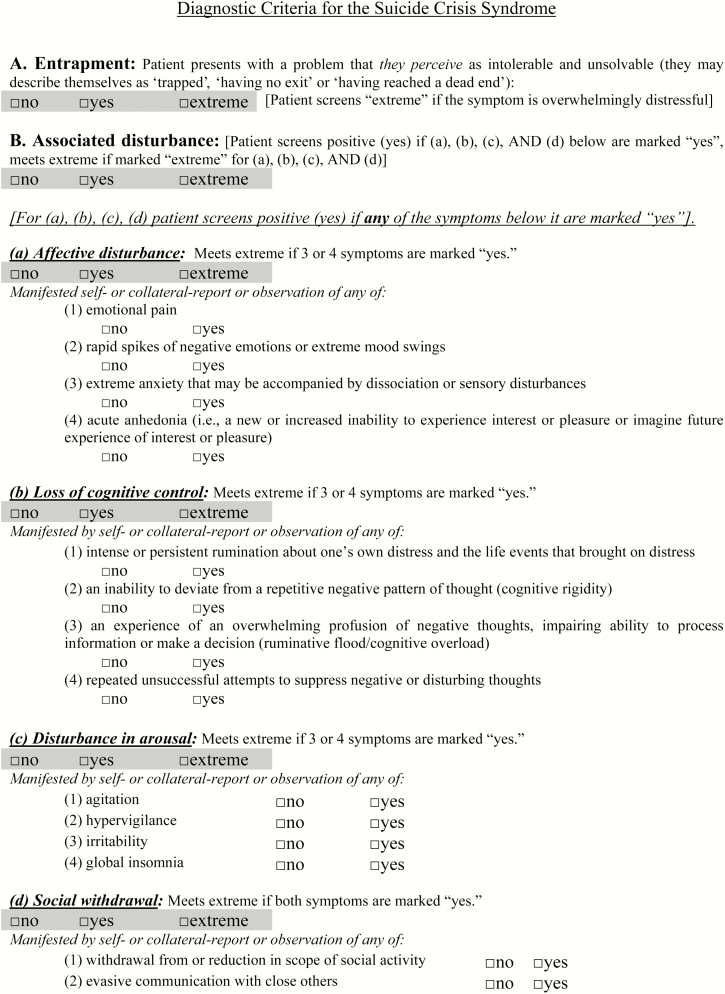
The current proposed DSM criteria for the SCS have 5 components, separated into 2 categories: Criterion A and Criterion B (see Appendix 1). Both Criterion A and all 4 categories of Criterion B must be met to receive a diagnosis. SI may or may not be present. The proposed DSM criteria are described below (Yaseen et al., 2018).
Criterion A is entrapment/frantic hopelessness, which is an urge to escape or avoid an unbearable life situation when escape is perceived as impossible; thus, death is perceived as the only solution. Typical situations are terminal illnesses, failure at work, or romantic rejection.
Criterion B has 4 categories, each enhancing the predictive validity of Criterion A. All 4 must be present for Criterion B to be met: (1) affective disturbance, (2) loss of cognitive control, (3) hyperarousal, and (4) recent social withdrawal.
Criteria A and B symptoms occur in the days and hours before the SA. Individuals meeting both Criterion A and Criterion B, compared with those meeting either alone, are at higher risk for a near-term SA (Yaseen et al., 2018). Therefore, both are needed to receive the SCS diagnosis.
In the early 1970s, 5 criteria, later known as the Feighner Criteria, were identified for the evaluation of the validity of diagnostic constructs (Robins and Guze, 1970; Feighner et al., 1972; Kendler et al., 2010): (1) clinical description, (2) laboratory studies, (3) delineation from other disorders, (4) follow-up studies, and (5) family studies. We have already obtained experimental evidence towards SCS meeting Feighner’s Criteria 1 and 4. For a detailed clinical description of the SCS (criterion 1) see (Schuck et al., 2019). In a preliminary follow-up study of acute psychiatric inpatients, the proposed SCS was found to confer a 7-fold increase in the risk of post-discharge SA (Yaseen et al., 2018) (criterion 4). A replication study in moderate-risk outpatients revealed a 6-fold increase of suicidal behavior over a 1-month period in those who fulfilled the criteria over those who did not (unpublished data). Criteria 2, 3, and 5 still need to be developed. Family studies on suicide, related to criterion 5 primarily, have focused on lifetime suicidal behavior rather than presuicidal mental states.
Past neuroimaging, genomic, and biochemical studies related to criterion 2 have sought to identify potential biomarkers (i.e., measurable biological parameters that increase the risk of a disease) that could help identify a biological risk profile of suicide. Much of the work was done prior to the clinical description of the SCS and ASAD and focused on biomarkers of suicidal behavior without a specific time frame. Exceptions include pioneering work on genetics, imaging, and short-term suicide risk (Colle et al., 2015; Consoloni et al., 2018; Deflesselle et al., 2018). Nevertheless, several biological risk factors contributing to suicide and nonfatal SA have been identified: alterations in key neurotransmitter systems (serotonergic, polyamine stress response, glutamatergic, and GABAergic systems), inflammatory changes, astroglial dysfunction, neuronal plasticity (brain-derived neurotrophic factor), and lipid alterations (Turecki, 2014; Almeida and Turecki, 2016; Chang et al., 2016; Sudol and Mann, 2017). Interestingly, (adolescent) suicide was recently described as a failure of systems implicated in acute stress responses: the autonomic nervous system, the hypothalamic–pituitary–adrenal (HPA) axis, the inflammatory response, and neural systems (Miller and Prinstein, 2019).
In the present study, we review literature on potential biomarkers previously associated with suicidal outcomes that are likely related to specific SCS criteria and individual symptoms. Our main goal is to formulate testable hypotheses for potential SCS biomarkers that may inform future research investigating a new suicide-specific DSM diagnosis.
Methods
A PubMed literature search was performed to identify studies reporting a link between each of the SCS symptoms and candidate biomarkers previously reported to be associated with suicidal outcomes. Additional details for the search strategy have been provided in supplementary Data 1.
Studies were included if they focused on any type of biomarker (brain imaging, genomics, biochemical) and if they focused on any suicidal outcomes. Since SCS is an acute state, we prioritized available studies examining biological parameters during acute states. The reference lists of the identified studies and reviews were checked as well for further relevant articles. Our aim was not to perform a systematic review but to provide a picture of current evidence. Because the proposed SCS criteria were derived from a former scale validated by our team, the Suicide Crisis Inventory (SCI) (Galynker et al., 2017), in the following description of the results we will refer, when possible, to both the SCI and SCS. The SCI leads to a continuous total score and 5 subscales (entrapment, emotional pain, frantic anxiety, fear of dying, and ruminative flooding). Every SCS criterion is dichotomous (presence vs absence).
Results
Criterion A: Entrapment/Frantic Hopelessness
Entrapment/frantic hopelessness is the core feature of the SCS (Galynker, 2017). Neurobiological mechanisms underlying entrapment could be related to both a strong motivation to escape/flight and to the impossibility to do so (arrested escape/flight). Dixon et al. described “arrested flight” as a response of animals exposed to threatening situations (Dixon et al., 1989). According to the Cry of Pain/Arrested Flight Model (Williams, 2001) and the Integrated Motivational and Volitional Model (O’Connor, 2011; O’Connor and Portzky, 2018), experience of entrapment may be present in humans as an analogous reaction, and it may also be a core component of the psychological mechanisms underlying depression and SI and behaviors. Entrapment could be linked to HPA axis dysregulation. In fact, saliva cortisol levels were higher in patients having recently attempted suicide than in both patients who had attempted suicide more than a year before and healthy controls (Lewitzka et al., 2017). Moreover, depressed individuals with brief SI have a greater cortisol response to a social stressor compared with those with longer and continuous SI and healthy volunteers (Rizk et al., 2018). Again, inpatients admitted for SA showed lower hair cortisol concentrations compared with both inpatients admitted for SI but without prior SA history and healthy controls (Melhem et al., 2017). Thus, dysregulated HPA activity may not only distinguish suicidal individuals from controls but may also be a marker of acute vs chronic suicide risk.
Alternatively, a dysregulated HPA axis could be related to a hypothesized stress-responsive subtype of suicide, characterized by impulsive suicidal behavior in reaction to stressful life events and associated with high emotional reactivity and poor cognitive control (Bernanke et al., 2017). The second hypothetical phenotype would be influenced by serotonergic dysfunction and characterized by planned suicidal behavior, depressed mood, and good cognitive control (Rizk et al., 2018). The association between serotonin transporter low-expressing alleles (S and LG) and increased risk of violent SA (Purselle and Nemeroff, 2003; Serretti et al., 2006; Fanelli and Serretti, 2019) as well as the related gene-environment (G × E) interactions (Roy et al., 2009; Enoch et al., 2013) are also consistent with serotonergic dysfunction underlying mental processes making suicidal behavior possible.
Some of the discrepancies in the reported results could be due to inconsistencies in measured outcomes (e.g., resting cortisol level and cortisol response to stress) as well as from the timing differences in cortisol sampling. Moreover, age could be a potent confounder: in a recent meta-analysis including 27 studies, higher cortisol was associated with SA younger than 40 years and lower cortisol was associated with SA when the patients were ≥40 years old (O’Connor et al., 2016). In addition, the heterogeneity across studies in time elapsed post-SA should be taken into account.
The SCS is an acute state with greater lability than state anxiety (Galynker et al., 2017), and, like SI, may fluctuate rapidly and last days, hours, or minutes. Therefore, any experimental design to test the hypothesis that entrapment/frantic hopelessness of SCS is subserved by dysregulated HPA axis activity should measure cortisol levels in close temporal proximity to the assessment of Criterion A. If our hypothesis is correct, individuals with high SCS entrapment/frantic hopelessness subscale scores on the SCI will have more labile cortisol levels than those with low scores. Alternatively, in a binary analysis, those meeting criteria for entrapment/frantic hopelessness on the SCS checklist will have more dysregulated cortisol levels measured, for example, in saliva than those who do not meet such criteria. For example, similar to what has been done (Rizk et al., 2018), saliva samples could be collected at different time points. Entrapment/frantic hopelessness would be evaluated as well at each time point. A probe to elicit mild feeling of entrapment might be of considerable utility.
Criterion B
Affective Disturbance
Psychological or Emotional Pain
The concept of psychological pain is multifaceted and connected with depression and suicide (Conejero et al., 2018). Over the last 3 decades, several related concepts emerged, most notably emotional pain, psychic pain, and psychache (Meerwijk and Weiss, 2014).
Our research team reported that emotional pain was a significant predictor of suicidal behavior in high-risk psychiatric inpatients within a month following discharge (Galynker, 2017). Other experimental support for the role emotional pain may play in suicide was reviewed in a meta-analysis (k = 20) of the association between psychological pain and current or lifetime history of SI and SA (Ducasse et al., 2017). The intensity of psychological pain was found to be higher, even when controlling for depression in (1) participants with lifetime history of SI and participants with current SI compared with those without SI and (2) participants with a lifetime history of SA and participants with current SA compared with those without SA.
The intuitive link between psychological-social and physical pain (think about the expression “broken heart”) was confirmed in functional neuroimaging studies (Eisenberger, 2012). The neural network subserving psychological pain was shown to include the thalamus, anterior cingulate cortex (ACC), posterior cingulate cortex, prefrontal cortex (PFC), cerebellum, and parahippocampal gyrus (Eisenberger, 2012; Meerwijk et al., 2013). With the exception of the parahippocampal gyrus, all of these brain regions, together with the insula, were found to mediate physical pain (Eisenberger, 2012; Meerwijk et al., 2013).
Pertaining to the pain-suicidality link, Elman et al. focused on the pain-pleasure continuum according to a key theory delineating interfacing sensory and emotional pain components (Borsook et al., 2007; Elman et al., 2013). The pathophysiology of physical pain is extremely complex and has long been intimately linked with the reward system (Elman et al., 2013). As converging lines of recent evidence suggest, pain also involves allostatic neuroadaptations in reward- and stress-related brain circuits, resulting in a condition of anti-reward (Borsook et al., 2016). Anti-reward is defined as a neurophysiological state wherein interference with homeostatic functioning of the reward and reinforcement circuitry, through massive outpouring of stressogenic corticotropin-releasing factor, norepinephrine, and dynorphin, results in negative affective states, anhedonia, and motivational states that are rigidly and exclusively focused on the relief of pain (adapted from Borsook et al., 2016). In our opinion, this definition may be applicable to the concepts of psychache, entrapment/frantic hopelessness, and the Cry of Pain/Arrested Flight Model of suicide as an escape from pain.
Central to the reward system are dopaminergic neurons situated in the ventral tegmental area that project to the nucleus accumbens. The habenula is a central node in the anti-reward system. Elman et al. described 2 syndromes in the context of the pain-suicidality classification: the reward deficiency syndrome, and the enhanced anti-reward syndrome (Elman et al., 2013), mediated by the brain’s reward and anti-reward systems, respectively. Reward deficiency syndrome is related to decreased motivation and capacity to experience pleasure and the enhanced anti-reward syndrome is related to dysphoria or depression. Both syndromes could lead to suicidal acts.
Another prominent neurochemical substrate involved in both psychological pain and suicide is the endogenous opioid system (Lutz et al., 2018). It is comprised of opioid peptides known as β-endorphin, enkephalins, and dynorphins. These peptides typically activate 3 receptors: µ, δ, and κ opioid receptors (Kieffer and Evans, 2009). The µ and κ receptors critically contribute to the regulation of both social reward and social pain (Lutz et al., 2018). Because both depression and suicidality are characterized by a lower sensitivity to social reward in addition to a higher sensitivity to social pain, µ and κ receptors are promising candidate biomarkers and should be taken into account in the study of acute suicidal states as well.
In summary, neurochemical substrates subserving psychological and physical pain processes are mediated by the reward and anti-reward circuitry via dopaminergic and endogenous opioid neural pathways. We hypothesize that suicidal individuals with high SCI scores on the emotional pain subscale would have more pronounced abnormalities in the above systems than those with low scores and that these abnormalities would be related to acute suicidal outcomes. Moreover, we hypothesize that individuals with SCS emotional pain will differ from individuals without emotional pain in terms of density or activity of opioid µ and κ receptors. They can be assessed through plasma (peripheral sampling), cerebrospinal fluid (CSF), Positron Emission Tomography imaging, and perhaps functional magnetic resonance imaging (fMRI).
Depressive Turmoil, Rapid Spikes of Negative Emotions, or Extreme Mood Swings
Depressive turmoil is a form of emotional dysregulation characterized by rapid increases in mood swings in a matter of days or hours preceding suicidal behavior (Galynker, 2017). We found depressive turmoil to contribute to the predictive validity of SCS criteria in relation to SI and SA (Yaseen et al., 2018). Such mood cycling during an index episode (a change from a manic to depressive syndrome or vice versa) differentiated between those who died by suicide and those who did not (Fawcett et al., 1987). The depressive turmoil construct is similar to affective lability and depressive mixed symptoms; hence, in our biomarkers’ search, we have focused on these clinical entities.
Affective lability is characterized by shifts in affective states in response to either positive or negative environmental events (Verdolini et al., 2019). Affective lability predicted SI in bipolar patients (Ducasse et al., 2018b) and was associated with SA history in patients with borderline personality disorder (Sher et al., 2016). Mixed states/features are defined as co-occurrence of both depressive and manic symptoms, which could be present either in bipolar disorder or in unipolar depression (Koukopoulos and Koukopoulos, 1999; Benazzi et al., 2004). The higher risk of suicide among patients with mixed states is well established (Annear and Agius, 2016). Among patients with bipolar disorder, individuals with a history of mixed states compared with individuals without such a history are at higher risk of suicidal behavior (Persons et al., 2018). However, this finding was mainly driven by the greater proportion of time spent depressed rather than by mixed state itself.
To date, there have been very few studies of biomarkers of affective lability (Acuff et al., 2019). Similarly, relatively few studies have investigated differences in potential biomarkers between mixed and nonmixed episodes (Cassidy et al., 2008). In particular, cortisol levels were reported to be different in mixed manic patients compared with nonmixed, but the results on the direction of this association are conflicting. Interestingly, when the dexamethasone suppression test was administered to 10 bipolar patients, only the 7 patients with mixed symptoms failed to suppress cortisol; the 3 patients with manic type were normal suppressors (Evans and Nemeroff, 1983).
Two neurophysiological models have been proposed to better understand major depressive episodes (MDEs) with mixed features (Micoulaud Franchi et al., 2013). The emotional regulation model posits that patients with mixed features tend to be hyperreactive and to have unstable emotional responses (Henry et al., 2003). An alternative vigilance regulation model (vigilance in the sense of “brain arousal”) posits that patients with mixed features show dysregulation of vigilance. Such dysregulation, associated with rapid fluctuations on electroencephalography (EEG) (Hegerl and Hensch, 2014), may result in an acceleration of psychomotor behavior and the tendency to engage in very stimulating environments to stabilize vigilance level at a satisfactory level.
We can therefore hypothesize that depressive turmoil of the SCS will lead to dysregulation of vigilance, associated with rapid fluctuations on EEG. A specific algorithm may be used to assess EEG vigilance for the classification of stages from high alertness to sleep onset, for example, the VIGilance Algorithm Leipzig (Micoulaud Franchi et al., 2013).
Frantic Anxiety and Dissociative Symptoms
There exists substantial evidence that, overall, anxiety disorders are associated with higher levels of SI and SA (Bentley et al., 2016; De La Vega et al., 2018), and, even more importantly, they were found to predict the transition from SI to SA (May et al., 2012). Frantic anxiety of the SCS can be described as painful mental arousal and increased motor function (i.e., the urge to move or to do something). Fawcett et al. found that severe psychic anxiety, together with other features, was associated with suicide within 1 year in patients with a major affective disorder (Fawcett et al., 1990). We reported that past-year panic attacks were significantly associated with lifetime SI and SA (Katz et al., 2011). Specific panic symptoms, fear of dying and fear of losing control, were more strongly associated with SA (Katz et al., 2011). For a consensus statement concerning biological markers for anxiety disorders, see (Bandelow et al., 2016, 2017).
With regard to the biomarkers linking acute suicidal behavior with anxiety states, recently interleukin-8 (IL-8) (plasma and CSF) levels were found to be significantly lower in inpatients admitted after a SA with acute anxiety compared with healthy controls (Janelidze et al., 2015). Moreover, suicide attempters carrying the T allele of rs4073 of the IL8 gene showed more severe anxiety. Also, the Spindle and Kinetochore Associated complex subunit 2 (SKA2), involved in stress response and cell cycle regulation, was found to significantly interact with anxiety to explain about 80% of suicidal behavior and progression from SI to SA in living cohorts (Guintivano et al., 2014). Moreover, in the same study, greater DNA methylation at SKA2 and less expression were found in suicide decedents compared with controls. Finally, SKA2 methylation was found to be associated not only with SI and SA but also with current and lifetime symptoms of internalizing disorders (Sadeh et al., 2016).
Concerning possible dissociative symptoms and the broader concept of dissociative experiences (absorption, disengagement, emotional constriction or numbing, memory disturbances), a recent meta-analysis (k = 216) focused on Dissociative Experiences Scale scores across different diagnoses and confirmed the presence of dissociative symptoms in nearly all psychiatric disorders (Lyssenko et al., 2018). Furthermore, in another recent meta-analysis, psychiatric patients with SA and NSSI reported higher Dissociative Experiences Scale scores compared with non-SA and non-NSSI patients (Calati et al., 2017).
For a recent review on dissociation and the dissociative disorders and a description of psychobiological aspects of dissociation, see (Loewenstein, 2018). Autonomic changes are present. Dissociation has been related to the animal “freeze” or “feigning death,” a protective response in the face of a danger where escape failed or would be more dangerous. Dissociation as a syndrome is tightly related to trauma, with reduction in hippocampal and amygdala volumes. Concerning genetic studies, single nucleotide polymorphisms implicated in dissociation in interaction with traumatic experiences (G × E) are linked to the HPA axis (FKBP5), serotonergic (5-HTTLPR), dopaminergic (catechol-O-methyltransferase), and BDNF systems (Loewenstein et al., 2017).
Hence, biomarkers associated with anxiety and dissociation, together with traumatic experiences, should be considered as well. We can hypothesize that individuals with SCS frantic anxiety may have lower SKA2 expression and higher methylation levels compared with patients without it. As recently suggested (Xie et al., 1995), SKA2 methylation can be assessed through peripheral blood testing.
Acute Anhedonia
Anhedonia refers to inability or reduced ability to experience pleasure. Researchers have distinguished several subtypes of anhedonia: anticipated, experienced/consummatory, remembered, and motivational anhedonia (incapacity/reduced capacity to expect pleasure from an experience, experience pleasure, recall experienced pleasure, and feel motivated to join in an activity to feel pleasure, respectively) (Rizvi et al., 2016). Moreover, acute anhedonia is distinct from chronic anhedonia.
In a number of clinical studies, anhedonia was found to be associated with indices of suicidality independent from depression severity. These data were recently reviewed in a meta-analysis (k = 15) (Ducasse et al., 2018a). Anhedonia was found to be higher among patients with current SI than in those without; after controlling for depression and psychiatric disorders, a medium effect size remained. Our recent study compared acutely anhedonic, chronically anhedonic, and nonanhedonic outpatients who were classified based on their responses to the Snaith-Hamilton Pleasure Scale (Hawes et al., 2018). Independent from anxiety and depression symptom severity, acutely anhedonic patients reported cross-sectionally and prospectively higher SI compared with nonanhedonic patients. Surprisingly, no difference in severity of SI was observed between the nonanhedonic and chronic anhedonic groups.
For a description of animal models of anhedonia, see (Goody et al., 2017). Brain structures involved in anhedonia overall are cortical (ventromedial and medial PFC, orbital frontal cortex, and ACC) and subcortical (basal ganglia and striatum—in particular the nucleus accumbens, ventral pallidum, ventral tegmental area, and substantia nigra—amygdala and hippocampus) (Treadway and Zald, 2011).
The already mentioned anti-reward system, and in particular the habenula, contributes to anhedonia in depression (Elman et al., 2013). With regard to anhedonia subtypes, deficits in the individual capacity of hedonic response after rewards (consummatory anhedonia) are different from the diminished motivation to pursue rewards (motivational anhedonia) (Treadway and Zald, 2011). Animal models suggested that the mesolimbic dopamine system (dopamine neurons innervating the ventral striatum) may be selectively involved in motivational anhedonia but not in consummatory anhedonia (Treadway and Zald, 2013). In particular, motivational anhedonia is associated with dopaminergic dysfunction in mesolimbic (Trainor, 2011) and mesocortical (Ventura et al., 2002) circuits. Consummatory anhedonia is modulated by the opioid system, amygdala, and ventromedial PFC (Treadway and Zald, 2011). Moreover, a role of inflammation has been hypothesized in anhedonia (Swardfager et al., 2016).
In summary, the identification of distinct neural circuits mapping the distinct anhedonia components is warranted, as recently suggested (Auerbach et al., 2019). To identify the substrate of SCS, these studies must include acute anhedonia. Moreover, because acute anhedonia could be associated with rapid changes in hedonic capacity, fMRI and ecological momentary assessment could be employed to capture these changes.
Loss of Cognitive Control
Ruminative Flooding
Ruminative flooding is defined as a particularly intense form of rumination distinguished by its association with head pain (distinct from a regular headache), head pressure, or, in extreme cases, by the sense that the head could explode from the pressure of ruminative thoughts (Yaseen et al., 2012, 2014, 2016). All individuals with ruminative flooding experience other aspects of loss of cognitive control to some degree but also experience distinct somatic symptoms and loss of control over their thoughts. We reported ruminative flooding to be associated with suicidal behavior in several prospective studies with different patient populations (Yaseen et al., 2010, 2012, 2014, 2016; Galynker et al., 2017).
Patients experiencing ruminative flooding describe that they cannot control their perseverative thoughts but rather they report feeling controlled and derailed by them, even though they may understand their lack of logic. In this respect, ruminative flooding overlaps with several aspects of thought disorder, which belongs in the psychotic spectrum. Similarly, the somatic symptoms of ruminative flooding overlap with somatic delusions present in psychosis. We hypothesize that ruminative flooding is an SCS subsyndrome that crosses into the realm of psychosis, similar to psychotic panic (Galynker et al., 1996). The fact that clozapine, together with lithium, possesses well-documented anti-suicidal properties (Bastiampillai et al., 2017) is concordant with this hypothesis.
The neurobiological substrates of thought disorder have been extensively described (Wensing et al., 2017; Cavelti et al., 2018; Sumner et al., 2018). Although the literature on this topic is vast and its thorough presentation is beyond the scope of this review, structural neuroimaging correlates implicated in thought disorder in schizophrenia include the left superior temporal gyrus, the orbitofrontal cortex, amygdala, hippocampus, nucleus accumbens, cerebellum, and corpus callosum (Sumner et al., 2018). Abnormal activation in brain regions specifically associated with language and speech processing (left hemisphere) was reported in thought disorder (Wensing et al., 2017). A potentially causative nucleotide deletion in the region 6q26–27 (164377205 AG > A) was found to affect formal thought disorder (Thygesen et al., 2015). The deletion is predicted to impair a regulatory site for the transcription factor Myocyte Enhancer Factor 2A involved in postsynaptic differentiation.
Besides thought disorder, ruminative flooding is phenomenologically similar to repetitive negative thinking seen in obsessive-compulsive disorder (OCD). In fact, repetitive negative thinking has been proposed to be transdiagnostic, prominent in major depressive disorder, generalized anxiety disorder, and OCD (Wahl et al., 2019). Moreover, metabolic, neuroinflammatory, and serotonergic abnormalities were found to play a role in OCD pathophysiology as well (Hellwig and Domschke, 2019), with the involvement of, among other structures, the caudate nucleus, putamen, and orbitofrontal cortex.
Therefore, we can hypothesize that individuals with SCS ruminative flooding would have functional abnormalities in brain areas associated with language processing compared with those without ruminative flooding (Wensing et al., 2017); moreover, they will have functional abnormalities in corticostriatal-thalamocortical circuits.
Intense and Persistent Ruminations
Rumination is the tendency to repetitively focus on the meaning, causes, and consequences of negative emotions, such as depressed mood (Nolen-Hoeksema, 1991). Two types of rumination have been described: brooding rumination (negative thinking about one’s own mental state) and reflective pondering or self-reflection (problem-solving–oriented intentional pondering) (Treynor et al., 2003). For a review focused on maladaptive brooding rumination as a trans-diagnostic factor in different psychiatric disorders, see Luca (Luca, 2019). Brooding rumination, compared with reflective pondering, was found to be more strongly associated with prospective SI (O’Connor and Noyce, 2008). Moreover, suicide-specific rumination was associated with a lifetime history of SA beyond other common risk factors such as general rumination (Rogers and Joiner, 2018).
The default-mode network (DMN) has been implicated in rumination (Hamilton et al., 2011, 2015). The DMN, including posterior cingulate and medial prefrontal cortices, has shown decreased activity during attention-demanding tasks and augmented activity during wakeful rest (Raichle et al., 2001). Increased activation in the DMN was associated with higher maladaptive, depressive rumination and lower adaptive, reflective rumination. Moreover, increased functional connectivity between the DMN and subgenual PFC has been suggested as a neural substrate of depressive rumination (Hamilton et al., 2015).
In addition, these midline cortical structures are also implicated in self-referential thinking (Northoff et al., 2006), which is likely related to the kinds of rumination that occur in the SCS. Hence, we hypothesize that individuals with SCS rumination will exhibit increased activation in the DMN in a resting-state fMRI study. Moreover, connectivity between the DMN and the subgenual PFC might be altered as well.
Cognitive Rigidity
Cognitive rigidity is a disposition to think in a rigid and inflexible manner (Neuringer, 1964). It has been linked to suicidality because this rigidity contributes to difficulty in developing new or alternative solutions to emotional problems (Giner et al., 2016). Moreover, cognitive rigidity seems to be associated with perfectionism (Buzzichelli et al., 2018), a trait often associated with SI and SA (Galynker, 2017; Limburg et al., 2017; Smith et al., 2018).
Cognitive rigidity is associated with deficits in executive function (EF). For a review of the existing literature on the relations between EF and suicidality, see (Bredemeier and Miller, 2015). Indirect evidence of the relation between EF deficits and suicide risk was found in structural and functional abnormalities in the PFC of suicide attempters (Jollant et al., 2011). Furthermore, cognitive rigidity may also be related to attentional bias/cognitive interferences that were shown to be present in neuropsychological tasks in suicide attempters (Cha et al., 2010; Glenn et al., 2017).
We hypothesize that individuals with SCS cognitive rigidity may exhibit abnormalities in the PFC.
Failure of Thought Suppression
The propensity to consciously suppress aversive thoughts is associated with suicidal thoughts and behaviors (Najmi et al., 2007; Cukrowicz et al., 2008; Pettit et al., 2009; Richard-Devantoy et al., 2015). Nock and his team proposed the following model in an attempt to describe the negative reinforcement function of thought suppression and self-injury (Najmi et al., 2007): high emotional reactivity leads to an intense experience of aversive thoughts and emotions, which triggers the suppression of these thoughts. Thought suppression, in turn, exacerbates the aversive thoughts/emotions: in fact, thought suppression is not always sustainable, particularly in the case of competing cognitive demands. When it fails, aversive thoughts and emotions may reoccur with higher frequency/intensity. The patient experiencing this exacerbation, in order to reduce it, may engage in suicidal thoughts and behaviors. The paradoxical or rebound effect of thought suppression has been reported (Abramowitz et al., 2001).
Activation in dorsolateral PFC (DLPFC) and ACC during thought suppression was lower in depressed patients compared with an at-risk group defined as having a first-degree relative with depression and healthy controls (Carew et al., 2013).
Resting heart rate variability (HRV), defined as the standard deviation of the RR intervals (the distance between each heartbeat) on the electrocardiogram, is a measure of how the heart responds to physiological demand (Thayer and Lane, 2009). HRV was reported to be associated with physiological, emotional, cognitive, and behavioral processes involved in self-regulation. Low HRV is a risk factor for pathophysiology (dysfunctions involving physiological, affective, and cognitive regulation) and psychopathology (Thayer and Lane, 2009). Moreover, HRV has been reported in multiple studies to be reduced in depressed patients (Sgoifo et al., 2015; Schiweck et al., 2019). Individuals with higher resting HRV, compared with those with lower levels, produce context-appropriate emotional responses and perform better on tasks requiring EF. Hence, higher resting HRV seems to be related to the capacity to flexibly adjust one’s feelings, thoughts, and behaviors to adapt to situational demands.
Higher resting HRV was also found to be associated with the ability to control unwanted thoughts with thought suppression (Gillie et al., 2015). Gillie et al. interpreted this finding considering thought suppression as likely to be effective only when it is one among other self-regulatory strategies that can be flexibly applied in response to environmental challenges.
We hypothesize that individuals with SCS thought suppression may differ from patients without it in terms of a lower resting HRV. Thought suppression task can be readily studied during electrocardiogram (Gillie et al., 2015) when participants are asked to record occurrences of a personally relevant intrusive thought over monitored periods (Gillie et al., 2015).
Hyperarousal
Agitation and Irritability
Agitation is a state of increased psychological and physical arousal during which the individual may feel restless or tense. From a chart review study, 1 week prior to death by suicide, 50% of patients reported severe or extreme agitation (Busch et al., 2003). In a recent meta-analysis (k = 13), the association between agitation (severe psychic anxiety) and suicidal behavior was found to be moderately strong (Rogers et al., 2016). Irritability was also reported to be associated with both SI and SA (Orri et al., 2018). As discussed in the section on depressive turmoil, both psychomotor agitation and irritability (inner psychic tension) are symptoms of agitated (mixed) depression with/without racing/crowded thoughts (Koukopoulos and Koukopoulos, 1999; Benazzi et al., 2004). These 2 subsyndromal manic symptoms were found to be highly prevalent in bipolar MDEs and were found to be associated with more SI and SA (Judd et al., 2012).
The psychological constructs of agitation/irritability are linked to physical arousal. Together with HRV, already described, electrodermal activity (EDA), or skin conductance, is a basic indicator of the state of the autonomic nervous system (Sarchiapone et al., 2018). Heart rate is modulated by both the sympathetic and parasympathetic arms of the autonomic nervous system. EDA is modulated solely by the sympathetic nervous system. EDA uses the quantity of sweat secreted by eccrine sweat glands in the hypodermis to measure changes in the electrical conductance of the skin. EDA is thought to be an indicator of emotional states such as agitation/irritability. EDA is measured by passing direct current through the epidermis of 2 fingers attached to 2 electrodes while a moderately strong tone plays through headphones at specific intervals (Sarchiapone et al., 2017). Sensors located within the electrodes then register the EDA to the tones. Individuals can show high EDA and slow habituation to specific stimuli (labile individuals), or low EDA and more rapid habituation (stable individuals). In terms of personality, EDA-labile individuals are described as internalizing, overcontrolled, and agreeable, whereas EDA-stable individuals tend to be externalizing, emotionally expressive, more irritable, and more antagonistic (Crider, 2008; Sarchiapone et al., 2018).
A reduction in HRV (Wilson et al., 2016) was observed in suicide attempters. Moreover, in a systematic review, low EDA was found in both depression and suicidal behavior, and EDA has been hypothesized to be a good indicator of acute suicide risk, even if further studies are needed (Sarchiapone et al., 2018). Furthermore, Sarchiapone et al. suggested that EDA could help in the future to distinguish between depressive subtypes; patients with psychomotor retardation found in endogenous and psychotic depression were found to have lower EDA than patients with agitation, found in nonendogenous and nonpsychotic depression (Sarchiapone et al., 2018).
Hence, low HRV and low EDA might be present in SCS as well and deserve further investigation. We hypothesize that individuals with SCS agitation and/or irritability may differ from patients without these symptoms in terms of lower HRV/EDA.
Hypervigilance
Hypervigilance is defined as a behavioral, cognitive, and physiological state of sustained alertness and hyperarousal in the absence of a specific threat. Our research team reported hypervigilance as contributing to the predictive validity of SCS diagnosis (Yaseen et al., 2018). Increased fear-potentiated startle has been reported in depressed patients with a history of SA compared with those without SA (Ballard et al., 2014). Impaired fear-potentiated startle was found in patients with focal bilateral basolateral amygdala damage (Klumpers et al., 2015). Further, the amygdala has been extensively implicated in the hyper-reactivity of patients at risk for suicidal behavior (Hariri et al., 2002). Indeed, the amygdala has been implicated in suicide in several postmortem studies (Hrdina et al., 1993; Anisman et al., 2008; Maheu et al., 2013; Pérez-Ortiz et al., 2013). Hence, the role of the amygdala should be investigated in the context of SCS; for example, in a shock paradigm comparing SCS patients with and without hypervigilance. Moreover, because we already described in the depression discussion the vigilance regulation model, we can hypothesize that, similarly, individuals with SCS hypervigilance will differ from patients without in terms of unstable regulation of the vigilance.
Insomnia
The association between insomnia and suicidal behavior is well established (Porras-Segovia et al., 2019). Sleep disturbances across different psychiatric diagnoses are significantly associated with suicidal behaviors; these include depression, posttraumatic stress disorder, panic disorder, and schizophrenia (Malik et al., 2014). Higher risk was conferred by insomnia, parasomnias, and sleep-related breathing disorders but not by hypersomnias. Recently, insomnia, together with other factors, was found to predict SA in a 6-year longitudinal study (Eikelenboom et al., 2019). Furthermore, not only sleep disturbances but also being awake at night were found to confer greater risk for suicide than being awake at other times of the day (Perlis et al., 2016), and evening and night work shifts were associated with increased SI compared with day work shifts (Kim et al., 2019).
Some factors that modulate the association between sleep problems and suicidal behavior include sleep deprivation-induced neurocognitive deficits, emotional dysregulation, alterations in circadian rhythms, and negative feelings (Porras-Segovia et al., 2019). In a recent study, in 50 of 4847 university undergraduate participants with SA history and recent SI, both objective and subjective measurements of sleep disturbances predicted acute SI increases independently of depression (Bernert et al., 2017). More specifically, self-reported insomnia, nightmares (subjective parameters), and sleep variability measured with actigraphy were found to be acute warning signs of SI.
Clearly, sleep quality and quantity can be measured, and one possible research design suggested by Bernert et al. (Bernert et al., 2017) is of interest in which patients with and without SCS would wear an actigraph that measures various sleep parameters on the wrist for 21 consecutive days while completing a sleep diary.
Recent Social Withdrawal
The term social withdrawal is used to indicate deficits in social functioning present in many neuropsychiatric disorders (Porcelli et al., 2019). When different social-relatedness constructs (marital status and living alone, social isolation, loneliness, alienation, and belongingness) were reviewed in their association with suicidal outcomes, both the objective conditions (e.g., living alone) and the subjective feeling of being alone (i.e., loneliness or perceived social isolation) were strongly associated with suicidal outcomes, in particular with SA and SI (Calati et al., 2019). Our research team used a Visual Analogue Scale to assess feelings of connectedness to a support network (Yaseen et al., 2018). Social withdrawal, alone and in combination with entrapment, contributed to the predictive validity of SCS for postdischarge SA.
The pathophysiology of social isolation was studied from the viewpoint of stress. According to animal models, exposure to social isolation stress produces a variety of pathophysiological changes (Mumtaz et al., 2018). These include hormonal changes, such as HPA axis activation, culminating in the release of glucocorticoids; activation of the sympatho-adrenomedullary system and the release of oxytocin and vasopressin; changes in neurotransmitter systems, such as dopamine, serotonin, gamma-aminobutyric acid and glutamate; alterations in endogenous opioid and cannabinoid systems; and, finally, changes in inflammatory and neuroplasticity-related signaling pathways.
The anti-reward system may be linked to social isolation and withdrawal while reward has evolved in the direction of emotional attachment and affiliation (Elman et al., 2013). For a review focused on neurobiological substrates of social withdrawal, considered as a trans-diagnostic domain in schizophrenia, Alzheimer’s disease, and major depressive disorder, see (Porcelli et al., 2019).
Alternatively, social isolation can be conceptualized in terms of a social threat hypothesis of anxiety, inflammation, and depression (Slavich and Irwin, 2014). Elevated levels of actual or perceived social threat (among others, social isolation) were posited to increase anxiety and activate social signal transduction pathways that upregulate inflammatory activity. Prolonged experiences of social threat may lead to both high inflammation and inflated perceptions of social threat. Within this framework, social anxiety-related disorders (Gadassi et al., 2014; Danneel et al., 2019) and social isolation/loneliness are linked in a mutually reinforcing vicious cycle.
Among other modulating factors, oxytocin was hypothesized to be involved in the complex link between social sensitivity and suicide through increasing the salience of social stimuli. Because oxytocin is essentially a hormone of social bonding and attachment, its lack likely leads to social withdrawal. Indeed, low CSF and plasma oxytocin levels were found in suicide attempters compared with controls, with low oxytocin levels in patients with strong intent to die (Jokinen et al., 2012).
The genetics of loneliness have been extensively reviewed (Goossens et al., 2015). Among others, a specific genetic variant that controls oxytocin release (CD38, Cluster of Differentiation 38) was reported to be associated with higher social sensitivity and with both depression and SI among university students (McQuaid et al., 2016).
Thus, in addition to reward/anti-reward system abnormalities previously described in the discussion of other SCS components, oxytocin may play a prominent role in linking SCS with social withdrawal. Future studies of this link may include plasma and CSF oxytocin assays. In parallel with acute anhedonia, we hypothesize the SCS syndrome will be associated with acute social withdrawal while chronic social isolation may be related to long-term suicide risk.
Discussion
The focus of this review was on the identification of potential biomarkers for SCS, an acute presuicidal syndrome characterized by a negative affective state combining an overwhelming sense of entrapment/frantic hopelessness with cognitive and emotional dysregulation. The results could form the basis for the development of empirically testable hypotheses to refine the structure and boundaries of the SCS as a whole.
In the most general terms, we can hypothesize that individuals affected by the SCS exhibit dysregulation in the brain circuits described in the results. More specifically, abnormalities in the HPA axis, with dysregulated cortisol levels, could be linked to entrapment. Both psychological pain and anhedonia are likely to be mediated by alterations in brain dopaminergic circuits involved in reward and anti-reward as well as changes in endogenous opioid systems. The loss of cognitive control is linked to altered neural processing in the brain areas underlying thought disorder and involved in executive function, attention, and decision-making. Hyperarousal is linked to autonomic dysregulation manifesting both as reduced HRV and altered EDA. Finally, social withdrawal appears to be modulated in part by oxytocin availability.
Future research directions should examine these potential biomarkers in relation to rapid symptomatologic changes in the SCS intensity. The ideal study design would include the assessment of SCS criteria and the putative biomarkers before, during, and after the suicidal crisis using ecological momentary assessment or another methodology with similar temporal resolution in real time. In addition to capturing putative psychopathological changes at their peak, longitudinal studies, or studies similar to those by Bagge’s group (timeline follow-back methodology) (Bagge et al., 2013, 2014), would be very informative. In this review, we have suggested specific testable hypotheses for SCS symptoms.
Considering that the SCS is an acute state, careful attention should be given to the role of (early) stressful life events in triggering this state. To detect clinically relevant effects, initially, high-risk populations should be studied, such as acute psychiatric inpatients. Although paradigms such as the Trier Social Stress Test could be used to examine the induction of SCS, provocative experimental paradigms would present significant ethical challenges. One alternative would be the use of virtual reality to reduce the burden of these challenges.
The SCS and suicidal behavior are trans-diagnostic. Nevertheless, SCS structure may vary across different established diagnoses, as is the case for other trans-diagnostic symptoms (Milak et al., 2007; Eisenberg et al., 2009). We can hypothesize that psychological pain would be present specifically in individuals with impaired affect regulation such as patients with depression or borderline personality disorder. In contrast, ruminative flooding may be overrepresented in the psychotic spectrum disorders.
The suggested possible biomarkers and future research directions should be considered within the limitations of this review, which is the first attempt to our knowledge to draft a biological description of the SCS. Because no biological correlates of the SCS have been described, much of the supporting evidence was gathered from the studies of long-term suicidal risk. This is a simplified picture of the evidence; hence, our proposition of specific biomarkers related to every SCS criterion is a necessary schematization and an oversimplification. To provide more detail at this stage of SCS research would be premature, but such experiments could and will be delineated in subsequent phases of scientific inquiry. Clearly obtaining the supporting genetic and epigenetic evidence is of critical importance.
Finally, several possible other biomarkers were not mentioned here for several reasons: the lack of a direct or plausible link with the specific SCS symptoms, the lack of evidence of their modulation of suicidal risk, and brevity. Nonetheless, they might prove to be relevant or even extremely relevant. Two examples can be identified. First, neuropeptides, specifically neuropeptide Y (NPY), might play a role in SA. Lower CSF NPY, in fact, was found in euthymic bipolar patients with a history of SA compared with patients with no such history (Sandberga et al., 2014). Moreover, CSF NPY was markedly lower in patients who attempted suicide in the year after the examination (prospectively examined) compared with nonattempters (n = 8 vs n = 90). Second, the role of gut microbiota (microbiota-gut-brain axis), discovered not only for depression (da Cruz Pereira et al., 2020) but also for complex aspects of social behaviors (Sherwin et al., 2019), should be taken into account together with the biomarkers here listed.
Conclusion
Compelling clinical evidence exists in support of a new suicide-specific phenomenological and diagnostic entity, the SCS. Including SCS in diagnostic manuals, in a new section dedicated to suicide, will reflect the clinical reality of the suicidal state and behavior comprising a mental illness with potentially fatal outcome. The present review identifies neural, neuroendocrine, genetic, and physiological mechanisms that could be targets in experimental paradigms for examination of biological substrates of the SCS. If successful, the results of the proposed scientific inquiry would add to the clinical evidence supporting the validity of the SCS as a new suicide-specific diagnosis and would instill clinicians with confidence in identifying and treating patients at risk for imminent suicide.
Supplementary Material
Acknowledgments
We thank Dr Courtnie Beaubian and Lauren Lloveras for the linguistic suggestions.
This study was supported by the American Foundation for Suicide Prevention (AFSP) focus grant #RFA-1-015-14.
Appendix
Statement of Interest
The content is solely the responsibility of the authors and does not necessarily represent the official AFSP views. The funders had no role in the decision to publish or in the preparation of the manuscript. Prof. Charles B. Nemeroff served as consultant for Xhale, Takeda, Taisho Pharmaceutical Inc., Bracket (Clintara), Sunovion Pharmaceuticals Inc., Janssen Research & Development LLC, Magstim Inc., Navitor Pharmaceuticals Inc., TC MSO Inc., Intra-Cellular Therapies Inc., EMA Wellness, Gerson Lehrman Group (GLG), and Acadia Pharmaceuticals. Prof. Charles B. Nemeroff is stockholder for Xhale, Celgene, Seattle Genetics, Abbvie, OPKO Health Inc., Antares, BI Gen Holdings Inc., Corcept Therapeutics Pharmaceuticals Company, TC MSO Inc., Trends in Pharma Development, LLC, and EMA Wellness.
Contributors
Dr Raffaella Calati conceived the idea, performed the literature search, wrote the manuscript, and added suggestions from the other authors. Prof. Charles Nemeroff, Prof. Jorge Lopez-Castroman, and Prof. Lisa J. Cohen critically revised the manuscript. Prof. Igor Galynker conceived and structured the manuscript and supervised the manuscript writing.
References
- Abramowitz JS, Tolin DF, Street GP (2001) Paradoxical effects of thought suppression: a meta-analysis of controlled studies. Clin Psychol Rev 21:683–703. [DOI] [PubMed] [Google Scholar]
- Acuff HE, Versace A, Bertocci MA, Hanford LC, Ladouceur CD, Manelis A, Monk K, Bonar L, McCaffrey A, Goldstein BI, Goldstein TR, Sakolsky D, Axelson D, Birmaher B, Phillips ML; LAMS Consortium (2019) White matter - emotion processing activity relationships in youth offspring of bipolar parents. J Affect Disord 243:153–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almeida D, Turecki G (2016) A slice of the suicidal brain: what have postmortem molecular studies taught us? Curr Psychiatry Rep 18:98. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th ed Washington DC: American Psychiatric Association. [Google Scholar]
- Anisman H, Du L, Palkovits M, Faludi G, Kovacs GG, Szontagh-Kishazi P, Merali Z, Poulter MO (2008) Serotonin receptor subtype and p11 mRNA expression in stress-relevant brain regions of suicide and control subjects. J Psychiatry Neurosci 33:131–141. [PMC free article] [PubMed] [Google Scholar]
- Annear D, Agius M (2016) Should assessment for bipolar disorder and mixed affective state be a standard part of assessment for suicide risk? Psychiatr Danub 28:18–20. [PubMed] [Google Scholar]
- Auerbach RP, Pagliaccio D, Pizzagalli DA (2019) Toward an improved understanding of anhedonia. JAMA Psychiatry 76:571–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagge CL, Glenn CR, Lee HJ (2013) Quantifying the impact of recent negative life events on suicide attempts. J Abnorm Psychol 122:359–368. [DOI] [PubMed] [Google Scholar]
- Bagge CL, Littlefield AK, Conner KR, Schumacher JA, Lee HJ (2014) Near-term predictors of the intensity of suicidal ideation: an examination of the 24 h prior to a recent suicide attempt. J Affect Disord 165:53–58. [DOI] [PubMed] [Google Scholar]
- Ballard ED, Ionescu DF, Vande Voort JL, Slonena EE, Franco-Chaves JA, Zarate CA Jr, Grillon C (2014) Increased fear-potentiated startle in major depressive disorder patients with lifetime history of suicide attempt. J Affect Disord 162:34–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandelow B, Baldwin D, Abelli M, Altamura C, Dell’Osso B, Domschke K, Fineberg NA, Grünblatt E, Jarema M, Maron E, Nutt D, Pini S, Vaghi MM, Wichniak A, Zai G, Riederer P (2016) Biological markers for anxiety disorders, OCD and PTSD - a consensus statement. Part I: neuroimaging and genetics. World J Biol Psychiatry 17:321–365. [DOI] [PubMed] [Google Scholar]
- Bandelow B, et al. (2017) Biological markers for anxiety disorders, OCD and PTSD: a consensus statement. Part II: neurochemistry, neurophysiology and neurocognition. World J Biol Psychiatry 18:162–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastiampillai T, Sharfstein SS, Allison S (2017) Increasing the use of lithium and clozapine in US suicide prevention. JAMA Psychiatry 74:423. [DOI] [PubMed] [Google Scholar]
- Benazzi F, Koukopoulos A, Akiskal HS (2004) Toward a validation of a new definition of agitated depression as a bipolar mixed state (mixed depression). Eur Psychiatry 19:85–90. [DOI] [PubMed] [Google Scholar]
- Bentley KH, Franklin JC, Ribeiro JD, Kleiman EM, Fox KR, Nock MK (2016) Anxiety and its disorders as risk factors for suicidal thoughts and behaviors: a meta-analytic review. Clin Psychol Rev 43:30–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernanke JA, Stanley BH, Oquendo MA (2017) Toward fine-grained phenotyping of suicidal behavior: the role of suicidal subtypes. Mol Psychiatry 22:1080–1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernert RA, Hom MA, Iwata NG, Joiner TE (2017) Objectively assessed sleep variability as an acute warning sign of suicidal ideation in a longitudinal evaluation of young adults at high suicide risk. J Clin Psychiatry 78:e678–e687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsook D, Becerra L, Carlezon WA Jr, Shaw M, Renshaw P, Elman I, Levine J (2007) Reward-aversion circuitry in analgesia and pain: implications for psychiatric disorders. Eur J Pain 11:7–20. [DOI] [PubMed] [Google Scholar]
- Borsook D, Linnman C, Faria V, Strassman AM, Becerra L, Elman I (2016) Reward deficiency and anti-reward in pain chronification. Neurosci Biobehav Rev 68:282–297. [DOI] [PubMed] [Google Scholar]
- Bredemeier K, Miller IW (2015) Executive function and suicidality: a systematic qualitative review. Clin Psychol Rev 40:170–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busch KA, Fawcett J, Jacobs DG (2003) Clinical correlates of inpatient suicide. J Clin Psychiatry 64:14–19. [DOI] [PubMed] [Google Scholar]
- Buzzichelli S, Marzola E, Amianto F, Fassino S, Abbate-Daga G (2018) Perfectionism and cognitive rigidity in anorexia nervosa: is there an association? Eur Eat Disord Rev 26:360–366. [DOI] [PubMed] [Google Scholar]
- Calati R, Bensassi I, Courtet P (2017) The link between dissociation and both suicide attempts and non-suicidal self-injury: meta-analyses. Psychiatry Res 251:103–114. [DOI] [PubMed] [Google Scholar]
- Calati R, Ferrari C, Brittner M, Oasi O, Olié E, Carvalho AF, Courtet P (2019) Suicidal thoughts and behaviors and social isolation: a narrative review of the literature. J Affect Disord 245:653–667. [DOI] [PubMed] [Google Scholar]
- Carew CL, Milne AM, Tatham EL, MacQueen GM, Hall GB (2013) Neural systems underlying thought suppression in young women with, and at-risk, for depression. Behav Brain Res 257:13–24. [DOI] [PubMed] [Google Scholar]
- Cassidy F, Yatham LN, Berk M, Grof P (2008) Pure and mixed manic subtypes: a review of diagnostic classification and validation. Bipolar Disord 10:131–143. [DOI] [PubMed] [Google Scholar]
- Cavelti M, Kircher T, Nagels A, Strik W, Homan P (2018) Is formal thought disorder in schizophrenia related to structural and functional aberrations in the language network? A systematic review of neuroimaging findings. Schizophr Res 199:2–16. [DOI] [PubMed] [Google Scholar]
- Cha CB, Najmi S, Park JM, Finn CT, Nock MK (2010) Attentional bias toward suicide-related stimuli predicts suicidal behavior. J Abnorm Psychol 119:616–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang BP, Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Nock MK (2016) Biological risk factors for suicidal behaviors: a meta-analysis. Transl Psychiatry 6:e887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colle R, Chupin M, Cury C, Vandendrie C, Gressier F, Hardy P, Falissard B, Colliot O, Ducreux D, Corruble E (2015) Depressed suicide attempters have smaller hippocampus than depressed patients without suicide attempts. J Psychiatr Res 61:13–18. [DOI] [PubMed] [Google Scholar]
- Conejero I, Olié E, Calati R, Ducasse D, Courtet P (2018) Psychological pain, depression, and suicide: recent evidences and future directions. Curr Psychiatry Rep 20:33. [DOI] [PubMed] [Google Scholar]
- Consoloni JL, Ibrahim EC, Lefebvre MN, Zendjidjian X, Olié E, Mazzola-Pomietto P, Desmidt T, Samalin L, Llorca PM, Abbar M, Lopez-Castroman J, Haffen E, Baumstarck K, Naudin J, Azorin JM, El-Hage W, Courtet P, Belzeaux R (2018) Serotonin transporter gene expression predicts the worsening of suicidal ideation and suicide attempts along a long-term follow-up of a Major Depressive Episode. Eur Neuropsychopharmacol 28:401–414. [DOI] [PubMed] [Google Scholar]
- Crider A. (2008) Personality and electrodermal response lability: an interpretation. Appl Psychophysiol Biofeedback 33:141–148. [DOI] [PubMed] [Google Scholar]
- Cukrowicz KC, Ekblad AG, Cheavens JS, Rosenthal MZ, Lynch TR (2008) Coping and thought suppression as predictors of suicidal ideation in depressed older adults with personality disorders. Aging Ment Health 12:149–157. [DOI] [PubMed] [Google Scholar]
- da Cruz Pereira J, Rea K, Nolan YM, O’Leary OF, Dinan TG, Cryan JF (2020) Depression’s unholy trinity: dysregulated stress, immunity, and the microbiome. Annu Rev Psychol 17:1–21, 30. [DOI] [PubMed] [Google Scholar]
- Danneel S, Nelemans S, Spithoven A, Bastin M, Bijttebier P, Colpin H, Van Den Noortgate W, Van Leeuwen K, Verschueren K, Goossens L (2019) Internalizing problems in adolescence: linking loneliness, social anxiety symptoms, and depressive symptoms over time. J Abnorm Child Psychol 47:1691–1705. [DOI] [PubMed] [Google Scholar]
- Deflesselle E, Colle R, Rigal L, David DJ, Vievard A, Martin S, Becquemont L, Verstuyft C, Corruble E (2018) The TRKB rs2289656 genetic polymorphism is associated with acute suicide attempts in depressed patients: a transversal case control study. PLoS One 13:e0205648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De La Vega D, Giner L, Courtet P (2018) Suicidality in subjects with anxiety or obsessive-compulsive and related disorders: recent advances. Curr Psychiatry Rep 20:26. [DOI] [PubMed] [Google Scholar]
- Dixon AK, Fisch HU, Huber C, Walser A (1989) Ethological studies in animals and man, their use in psychiatry. Pharmacopsychiatry 22(Suppl 1):44–50. [DOI] [PubMed] [Google Scholar]
- Ducasse D, Holden R, Boyer L, Artero S, Calati R, Guillaume S, Courtet P, Olie E (2018a) Psychological pain in suicidality: a meta-analysis. J Clin Psychiatry 79. [DOI] [PubMed] [Google Scholar]
- Ducasse D, Jaussent I, Guillaume S, Azorin JM, Bellivier F, Belzeaux R, Bougerol T, Etain B, Gard S, Henry C, Kahn JP, Leboyer M, Loftus J, Passerieux C, Olié E, Courtet P; FondaMental Advanced Centers of Expertise in Bipolar Disorders (FACE-BD) Collaborators (2017) Affect lability predicts occurrence of suicidal ideation in bipolar patients: a two-year prospective study. Acta Psychiatr Scand 135:460–469. [DOI] [PubMed] [Google Scholar]
- Ducasse D, Loas G, Dassa D, Gramaglia C, Zeppegno P, Guillaume S, Olié E, Courtet P (2018b) Anhedonia is associated with suicidal ideation independently of depression: a meta-analysis. Depress Anxiety 35:382–392. [DOI] [PubMed] [Google Scholar]
- Eikelenboom M, Beekman ATF, Penninx BWJH, Smit JH (2019) A 6-year longitudinal study of predictors for suicide attempts in major depressive disorder. Psychol Med 49:911–921. [DOI] [PubMed] [Google Scholar]
- Eisenberg DP, Aniskin DB, White L, Stein JA, Harvey PD, Galynker II (2009) Structural differences within negative and depressive syndrome dimensions in schizophrenia, organic brain disease, and major depression: a confirmatory factor analysis of the positive and negative syndrome scale. Psychopathology 42:242–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberger NI. (2012) The pain of social disconnection: examining the shared neural underpinnings of physical and social pain. Nat Rev Neurosci 13:421–434. [DOI] [PubMed] [Google Scholar]
- Elman I, Borsook D, Volkow ND (2013) Pain and suicidality: insights from reward and addiction neuroscience. Prog Neurobiol 109:1–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enoch MA, Hodgkinson CA, Gorodetsky E, Goldman D, Roy A (2013) Independent effects of 5’ and 3’ functional variants in the serotonin transporter gene on suicidal behavior in the context of childhood trauma. J Psychiatr Res 47:900–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans DL, Nemeroff CB (1983) The dexamethasone suppression test in mixed bipolar disorder. Am J Psychiatry 140:615–617. [DOI] [PubMed] [Google Scholar]
- Fanelli G, Serretti A (2019) The influence of the serotonin transporter gene 5-HTTLPR polymorphism on suicidal behaviors: a meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry 88:375–387. [DOI] [PubMed] [Google Scholar]
- Fawcett J, Scheftner W, Clark D, Hedeker D, Gibbons R, Coryell W (1987) Clinical predictors of suicide in patients with major affective disorders: a controlled prospective study. Am J Psychiatry 144:35–40. [DOI] [PubMed] [Google Scholar]
- Fawcett J, Scheftner WA, Fogg L, Clark DC, Young MA, Hedeker D, Gibbons R (1990) Time-related predictors of suicide in major affective disorder. Am J Psychiatry 147:1189–1194. [DOI] [PubMed] [Google Scholar]
- Feighner JP, Robins E, Guze SB, Woodruff RA Jr, Winokur G, Munoz R (1972) Diagnostic criteria for use in psychiatric research. Arch Gen Psychiatry 26:57–63. [DOI] [PubMed] [Google Scholar]
- Gadassi R, Snir A, Berenson K, Downey G, Rafaeli E (2014) Out of the frying pan, into the fire: mixed affective reactions to social proximity in borderline and avoidant personality disorders in daily life. J Abnorm Psychol 123:613–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galynker I. (2017) The suicidal crisis: clinical guide to the assessment of imminent suicide risk. Oxford, UK: Oxford University Press. [Google Scholar]
- Galynker I, Ieronimo C, Perez-Acquino A, Lee Y, Winston A (1996) Panic attacks with psychotic features. J Clin Psychiatry 57:402–406. [PubMed] [Google Scholar]
- Galynker I, Yaseen ZS, Cohen A, Benhamou O, Hawes M, Briggs J (2017) Prediction of suicidal behavior in high risk psychiatric patients using an assessment of acute suicidal state: the suicide crisis inventory. Depress Anxiety 34:147–158. [DOI] [PubMed] [Google Scholar]
- Gillie BL, Vasey MW, Thayer JF (2015) Individual differences in resting heart rate variability moderate thought suppression success. Psychophysiology 52:1149–1160. [DOI] [PubMed] [Google Scholar]
- Giner L, Blasco-Fontecilla H, De La Vega D, Courtet P (2016) Cognitive, emotional, temperament, and personality trait correlates of suicidal behavior. Curr Psychiatry Rep 18:102. [DOI] [PubMed] [Google Scholar]
- Glenn JJ, Werntz AJ, Slama SJ, Steinman SA, Teachman BA, Nock MK (2017) Suicide and self-injury-related implicit cognition: a large-scale examination and replication. J Abnorm Psychol 126:199–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goody SMG, Cannon KE, Liu M, Kallman MJ, Martinolle JP, Mazelin-Winum L, Giarola A, Ardayfio P, Moyer JA, Teuns G, Hudzik TJ (2017) Considerations on nonclinical approaches to modeling risk factors of suicidal ideation and behavior. Regul Toxicol Pharmacol 89:288–301. [DOI] [PubMed] [Google Scholar]
- Goossens L, van Roekel E, Verhagen M, Cacioppo JT, Cacioppo S, Maes M, Boomsma DI (2015) The genetics of loneliness: linking evolutionary theory to genome-wide genetics, epigenetics, and social science. Perspect Psychol Sci 10:213–226. [DOI] [PubMed] [Google Scholar]
- Guintivano J, Brown T, Newcomer A, Jones M, Cox O, Maher BS, Eaton WW, Payne JL, Wilcox HC, Kaminsky ZA (2014) Identification and replication of a combined epigenetic and genetic biomarker predicting suicide and suicidal behaviors. Am J Psychiatry 171:1287–1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton JP, Furman DJ, Chang C, Thomason ME, Dennis E, Gotlib IH (2011) Default-mode and task-positive network activity in major depressive disorder: implications for adaptive and maladaptive rumination. Biol Psychiatry 70:327–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton JP, Farmer M, Fogelman P, Gotlib IH (2015) Depressive rumination, the default-mode network, and the dark matter of clinical neuroscience. Biol Psychiatry 78:224–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hariri AR, Mattay VS, Tessitore A, Kolachana B, Fera F, Goldman D, Egan MF, Weinberger DR (2002) Serotonin transporter genetic variation and the response of the human amygdala. Science 297:400–403. [DOI] [PubMed] [Google Scholar]
- Hawes M, Galynker I, Barzilay S, Yaseen ZS (2018) Anhedonia and suicidal thoughts and behaviors in psychiatric outpatients: the role of acuity. Depress Anxiety 35:1218–1227. [DOI] [PubMed] [Google Scholar]
- Hegerl U, Hensch T (2014) The vigilance regulation model of affective disorders and ADHD. Neurosci Biobehav Rev 44:45–57. [DOI] [PubMed] [Google Scholar]
- Hellwig S, Domschke K (2019) Update on PET imaging biomarkers in the diagnosis of neuropsychiatric disorders. Curr Opin Neurol 32:539–547. [DOI] [PubMed] [Google Scholar]
- Hendin H, Maltsberger JT, Szanto K (2007) The role of intense affective states in signaling a suicide crisis. J Nerv Ment Dis 195:363–368. [DOI] [PubMed] [Google Scholar]
- Henry C, Swendsen J, Van den Bulke D, Sorbara F, Demotes-Mainard J, Leboyer M (2003) Emotional hyper-reactivity as a fundamental mood characteristic of manic and mixed states. Eur Psychiatry 18:124–128. [DOI] [PubMed] [Google Scholar]
- Hrdina PD, Demeter E, Vu TB, Sótónyi P, Palkovits M (1993) 5-HT uptake sites and 5-HT2 receptors in brain of antidepressant-free suicide victims/depressives: increase in 5-HT2 sites in cortex and amygdala. Brain Res 614:37–44. [DOI] [PubMed] [Google Scholar]
- Janelidze S, Suchankova P, Ekman A, Erhardt S, Sellgren C, Samuelsson M, Westrin A, Minthon L, Hansson O, Träskman-Bendz L, Brundin L (2015) Low IL-8 is associated with anxiety in suicidal patients: genetic variation and decreased protein levels. Acta Psychiatr Scand 131:269–278. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Simpson S, Rogers ML, Stanley IH, Galynker II (2018) Whether called acute suicidal affective disturbance or suicide crisis syndrome, a suicide-specific diagnosis would enhance clinical care, increase patient safety, and mitigate clinician liability. J Psychiatr Pract 24:274–278. [DOI] [PubMed] [Google Scholar]
- Jokinen J, Chatzittofis A, Hellström C, Nordström P, Uvnäs-Moberg K, Asberg M (2012) Low CSF oxytocin reflects high intent in suicide attempters. Psychoneuroendocrinology 37:482–490. [DOI] [PubMed] [Google Scholar]
- Jollant F, Lawrence NL, Olié E, Guillaume S, Courtet P (2011) The suicidal mind and brain: a review of neuropsychological and neuroimaging studies. World J Biol Psychiatry 12:319–339. [DOI] [PubMed] [Google Scholar]
- Judd LL, Schettler PJ, Akiskal H, Coryell W, Fawcett J, Fiedorowicz JG, Solomon DA, Keller MB (2012) Prevalence and clinical significance of subsyndromal manic symptoms, including irritability and psychomotor agitation, during bipolar major depressive episodes. J Affect Disord 138:440–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz C, Yaseen ZS, Mojtabai R, Cohen LJ, Galynker II (2011) Panic as an independent risk factor for suicide attempt in depressive illness: findings from the National Epidemiological Survey on Alcohol and Related Conditions (NESARC). J Clin Psychiatry 72:1628–1635. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Muñoz RA, Murphy G (2010) The development of the Feighner criteria: a historical perspective. Am J Psychiatry 167:134–142. [DOI] [PubMed] [Google Scholar]
- Kieffer BL, Evans CJ (2009) Opioid receptors: from binding sites to visible molecules in vivo. Neuropharmacology 56(Suppl 1):205–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim KK, Lee KR, Suh HS, Ko KD, Hwang IC (2019) Association between shift work and suicidal ideation: data from the Korea National Health and Nutrition Examination Survey (2008–2016). Scand J Work Environ Health 45:458–464. [DOI] [PubMed] [Google Scholar]
- Klumpers F, Morgan B, Terburg D, Stein DJ, van Honk J (2015) Impaired acquisition of classically conditioned fear-potentiated startle reflexes in humans with focal bilateral basolateral amygdala damage. Soc Cogn Affect Neurosci 10:1161–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koukopoulos A, Koukopoulos A (1999) Agitated depression as a mixed state and the problem of melancholia. Psychiatr Clin North Am 22:547–564. [DOI] [PubMed] [Google Scholar]
- Lewitzka U, Bauer M, Ripke B, Bronisch T, Günther L (2017) Impulsivity and saliva cortisol in patients with suicide attempt and controls. Neuropsychobiology 75:162–168. [DOI] [PubMed] [Google Scholar]
- Li S, Yaseen ZS, Kim HJ, Briggs J, Duffy M, Frechette-Hagan A, Cohen LJ, Galynker II (2018) Entrapment as a mediator of suicide crises. BMC Psychiatry 18:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Limburg K, Watson HJ, Hagger MS, Egan SJ (2017) The relationship between perfectionism and psychopathology: a meta-analysis. J Clin Psychol 73:1301–1326. [DOI] [PubMed] [Google Scholar]
- Loewenstein RJ. (2018) Dissociation debates: everything you know is wrong. Dialogues Clin Neurosci 20:229–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loewenstein RJ, Frewen PA, Lewis-Fernández R (2017) Dissociative disorders. In: Kaplan & Sadock’s comprehensive textbook of psychiatry (Sadock BJ, Sadock VA, Ruiz P, eds.), pp 1866–1952. Philadelphia, PA: Wolters Kluwer/Lippincott Williams & Wilkens. [Google Scholar]
- Luca M. (2019) Maladaptive rumination as a transdiagnostic mediator of vulnerability and outcome in psychopathology. J Clin Med 8: 314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutz PE, Courtet P, Calati R (2018) The opioid system and the social brain: implications for depression and suicide. J Neurosci Res. doi: 10.1002/jnr.24269. In press. [DOI] [PubMed] [Google Scholar]
- Lyssenko L, Schmahl C, Bockhacker L, Vonderlin R, Bohus M, Kleindienst N (2018) Dissociation in psychiatric disorders: a meta-analysis of studies using the dissociative experiences scale. Am J Psychiatry 175:37–46. [DOI] [PubMed] [Google Scholar]
- Maheu ME, Davoli MA, Turecki G, Mechawar N (2013) Amygdalar expression of proteins associated with neuroplasticity in major depression and suicide. J Psychiatr Res 47:384–390. [DOI] [PubMed] [Google Scholar]
- Malik S, Kanwar A, Sim LA, Prokop LJ, Wang Z, Benkhadra K, Murad MH (2014) The association between sleep disturbances and suicidal behaviors in patients with psychiatric diagnoses: a systematic review and meta-analysis. Syst Rev 3:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May AM, Klonsky ED, Klein DN (2012) Predicting future suicide attempts among depressed suicide ideators: a 10-year longitudinal study. J Psychiatr Res 46:946–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQuaid RJ, McInnis OA, Matheson K, Anisman H (2016) Oxytocin and social sensitivity: gene polymorphisms in relation to depressive symptoms and suicidal ideation. Front Hum Neurosci 10:358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meerwijk EL, Ford JM, Weiss SJ (2013) Brain regions associated with psychological pain: implications for a neural network and its relationship to physical pain. Brain Imaging Behav 7:1–14. [DOI] [PubMed] [Google Scholar]
- Meerwijk EL, Weiss SJ (2014) Toward a unifying definition: response to ‘The concept of mental pain’. Psychother Psychosom 83:62–63. [DOI] [PubMed] [Google Scholar]
- Melhem NM, Munroe S, Marsland A, Gray K, Brent D, Porta G, Douaihy A, Laudenslager ML, DePietro F, Diler R, Driscoll H, Gopalan P (2017) Blunted HPA axis activity prior to suicide attempt and increased inflammation in attempters. Psychoneuroendocrinology 77:284–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Micoulaud Franchi JA, Geoffroy PA, Vion-Dury J, Balzani C, Belzeaux R, Maurel M, Cermolacce M, Fakra E, Azorin JM (2013) Mixed depressions: clinical and neurophysiological biomarkers. Encephale 39(Suppl 3):S149–S156. [DOI] [PubMed] [Google Scholar]
- Milak MS, Aniskin DB, Eisenberg DP, Prikhojan A, Cohen LJ, Yard SS, Galynker II (2007) The negative syndrome as a dimension: factor analyses of PANSS in major depressive disorder and organic brain disease compared with negative syndrome structures found in the schizophrenia literature. Cogn Behav Neurol 20:113–120. [DOI] [PubMed] [Google Scholar]
- Miller AB, Prinstein MJ (2019) Adolescent suicide as a failure of acute stress-response systems. Annu Rev Clin Psychol 15:425–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mumtaz F, Khan MI, Zubair M, Dehpour AR (2018) Neurobiology and consequences of social isolation stress in animal model-A comprehensive review. Biomed Pharmacother 105:1205–1222. [DOI] [PubMed] [Google Scholar]
- Najmi S, Wegner DM, Nock MK (2007) Thought suppression and self-injurious thoughts and behaviors. Behav Res Ther 45:1957–1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuringer C. (1964) Rigid thinking in suicidal individuals. J Consult Psychol 28:54–58. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. (1991) Responses to depression and their effects on the duration of depressive episodes. J Abnorm Psychol 100:569–582. [DOI] [PubMed] [Google Scholar]
- Northoff G, Heinzel A, de Greck M, Bermpohl F, Dobrowolny H, Panksepp J (2006) Self-referential processing in our brain–a meta-analysis of imaging studies on the self. Neuroimage 31:440–457. [DOI] [PubMed] [Google Scholar]
- O’Connor DB, Ferguson E, Green JA, O’Carroll RE, O’Connor RC (2016) Cortisol levels and suicidal behavior: a meta-analysis. Psychoneuroendocrinology 63:370–379. [DOI] [PubMed] [Google Scholar]
- O’Connor RC. (2011) The integrated motivational-volitional model of suicidal behavior. Crisis 32:295–298. [DOI] [PubMed] [Google Scholar]
- O’Connor RC, Noyce R (2008) Personality and cognitive processes: self-criticism and different types of rumination as predictors of suicidal ideation. Behav Res Ther 46:392–401. [DOI] [PubMed] [Google Scholar]
- O’Connor RC, Portzky G (2018) The relationship between entrapment and suicidal behavior through the lens of the integrated motivational-volitional model of suicidal behavior. Curr Opin Psychol 22:12–17. [DOI] [PubMed] [Google Scholar]
- Oquendo MA, Baca-Garcia E (2014) Suicidal behavior disorder as a diagnostic entity in the DSM-5 classification system: advantages outweigh limitations. World Psychiatry 13:128–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orri M, Perret LC, Turecki G, Geoffroy MC (2018) Association between irritability and suicide-related outcomes across the life-course. Systematic review of both community and clinical studies. J Affect Disord 239:220–233. [DOI] [PubMed] [Google Scholar]
- Pérez-Ortiz JM, García-Gutiérrez MS, Navarrete F, Giner S, Manzanares J (2013) Gene and protein alterations of FKBP5 and glucocorticoid receptor in the amygdala of suicide victims. Psychoneuroendocrinology 38:1251–1258. [DOI] [PubMed] [Google Scholar]
- Perlis ML, Grandner MA, Brown GK, Basner M, Chakravorty S, Morales KH, Gehrman PR, Chaudhary NS, Thase ME, Dinges DF (2016) Nocturnal wakefulness as a previously unrecognized risk factor for suicide. J Clin Psychiatry 77:e726–e733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persons JE, Coryell WH, Solomon DA, Keller MB, Endicott J, Fiedorowicz JG (2018) Mixed state and suicide: is the effect of mixed state on suicidal behavior more than the sum of its parts? Bipolar Disord 20:35–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettit JW, Temple SR, Norton PJ, Yaroslavsky I, Grover KE, Morgan ST, Schatte DJ (2009) Thought suppression and suicidal ideation: preliminary evidence in support of a robust association. Depress Anxiety 26:758–763. [DOI] [PubMed] [Google Scholar]
- Porcelli S, Van Der Wee N, van der Werff S, Aghajani M, Glennon JC, van Heukelum S, Mogavero F, Lobo A, Olivera FJ, Lobo E, Posadas M, Dukart J, Kozak R, Arce E, Ikram A, Vorstman J, Bilderbeck A, Saris I, Kas MJ, Serretti A (2019) Social brain, social dysfunction and social withdrawal. Neurosci Biobehav Rev 97:10–33. [DOI] [PubMed] [Google Scholar]
- Porras-Segovia A, Pérez-Rodríguez MM, López-Esteban P, Courtet P, Barrigón M ML, López-Castromán J, Cervilla JA, Baca-García E (2019) Contribution of sleep deprivation to suicidal behaviour: a systematic review. Sleep Med Rev 44:37–47. [DOI] [PubMed] [Google Scholar]
- Purselle DC, Nemeroff CB (2003) Serotonin transporter: a potential substrate in the biology of suicide. Neuropsychopharmacology 28:613–619. [DOI] [PubMed] [Google Scholar]
- Raichle ME, MacLeod AM, Snyder AZ, Powers WJ, Gusnard DA, Shulman GL (2001) A default mode of brain function. Proc Natl Acad Sci U S A 98:676–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richard-Devantoy S, Szanto K, Butters MA, Kalkus J, Dombrovski AY (2015) Cognitive inhibition in older high-lethality suicide attempters. Int J Geriatr Psychiatry 30:274–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizk MM, Galfalvy H, Singh T, Keilp JG, Sublette ME, Oquendo MA, Mann JJ, Stanley B (2018) Toward subtyping of suicidality: brief suicidal ideation is associated with greater stress response. J Affect Disord 230:87–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizvi SJ, Pizzagalli DA, Sproule BA, Kennedy SH (2016) Assessing anhedonia in depression: potentials and pitfalls. Neurosci Biobehav Rev 65:21–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robins E, Guze SB (1970) Establishment of diagnostic validity in psychiatric illness: its application to schizophrenia. Am J Psychiatry 126:983–987. [DOI] [PubMed] [Google Scholar]
- Rogers ML, Chiurliza B, Hagan CR, Tzoneva M, Hames JL, Michaels MS, Hitschfeld MJ, Palmer BA, Lineberry TW, Jobes DA, Joiner TE (2017) Acute suicidal affective disturbance: factorial structure and initial validation across psychiatric outpatient and inpatient samples. J Affect Disord 211:1–11. [DOI] [PubMed] [Google Scholar]
- Rogers ML, Chu C, Joiner T (2019) The necessity, validity, and clinical utility of a new diagnostic entity: acute suicidal affective disturbance. J Clin Psychol 75:999–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers ML, Joiner TE (2018) Suicide-specific rumination relates to lifetime suicide attempts above and beyond a variety of other suicide risk factors. J Psychiatr Res 98:78–86. [DOI] [PubMed] [Google Scholar]
- Rogers ML, Ringer FB, Joiner TE (2016) A meta-analytic review of the association between agitation and suicide attempts. Clin Psychol Rev 48:1–6. [DOI] [PubMed] [Google Scholar]
- Roy A, Sarchiopone M, Carli V (2009) Gene-environment interaction and suicidal behavior. J Psychiatr Pract 15:282–288. [DOI] [PubMed] [Google Scholar]
- Sadeh N, Wolf EJ, Logue MW, Hayes JP, Stone A, Griffin LM, Schichman SA, Miller MW (2016) Epigenetic variation at SKA2 predicts suicide phenotypes and internalizing psychopathology. Depress Anxiety 33:308–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandberg JV, Jakobsson J, Pålsson E, Landén M, Mathé AA (2014) Low neuropeptide Y in cerebrospinal fluid in bipolar patients is associated with previous and prospective suicide attempts. Eur Neuropsychopharmacol 24:1907–1915. [DOI] [PubMed] [Google Scholar]
- Sarchiapone M, Iosue M, Carli V, Amore M, Baca-Garcia E, Batra A, Cosman D, Courtet P, Di Sciascio G, Gusmao R, Parnowski T, Pestality P, Saiz P, Thome J, Tingström A, Wojnar M, Zeppegno P, Thorell LH (2017) EUDOR-A multi-centre research program: a naturalistic, European Multi-centre Clinical Study of EDOR Test in adult patients with primary depression. BMC Psychiatry 17:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarchiapone M, Gramaglia C, Iosue M, Carli V, Mandelli L, Serretti A, Marangon D, Zeppegno P (2018) The association between electrodermal activity (EDA), depression and suicidal behaviour: a systematic review and narrative synthesis. BMC Psychiatry 18:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiweck C, Piette D, Berckmans D, Claes S, Vrieze E (2019) Heart rate and high frequency heart rate variability during stress as biomarker for clinical depression. A systematic review. Psychol Med 49:200–211. [DOI] [PubMed] [Google Scholar]
- Schuck A, Calati R, Barzilay S, Bloch-Elkouby S, Galynker I (2019) Suicide crisis syndrome: a review of supporting evidence for a new suicide-specific diagnosis. Behav Sci Law 37:223–239. [DOI] [PubMed] [Google Scholar]
- Serretti A, Calati R, Mandelli L, De Ronchi D (2006) Serotonin transporter gene variants and behavior: a comprehensive review. Curr Drug Targets 7:1659–1669. [DOI] [PubMed] [Google Scholar]
- Sgoifo A, Carnevali L, Alfonso Mde L, Amore M (2015) Autonomic dysfunction and heart rate variability in depression. Stress 18:343–352. [DOI] [PubMed] [Google Scholar]
- Sher L, Fisher AM, Kelliher CH, Penner JD, Goodman M, Koenigsberg HW, New AS, Siever LJ, Hazlett EA (2016) Clinical features and psychiatric comorbidities of borderline personality disorder patients with versus without a history of suicide attempt. Psychiatry Res 246:261–266. [DOI] [PubMed] [Google Scholar]
- Sherwin E, Bordenstein SR, Quinn JL, Dinan TG, Cryan JF (2019) Microbiota and the social brain. Science 366. doi: 10.1126/science.aar2016. Review. [DOI] [PubMed] [Google Scholar]
- Slavich GM, Irwin MR (2014) From stress to inflammation and major depressive disorder: a social signal transduction theory of depression. Psychol Bull 140:774–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith MM, Sherry SB, Chen S, Saklofske DH, Mushquash C, Flett GL, Hewitt PL (2018) The perniciousness of perfectionism: a meta-analytic review of the perfectionism-suicide relationship. J Pers 86:522–542. [DOI] [PubMed] [Google Scholar]
- Sudol K, Mann JJ (2017) Biomarkers of suicide attempt behavior: towards a biological model of risk. Curr Psychiatry Rep 19:31. [DOI] [PubMed] [Google Scholar]
- Sumner PJ, Bell IH, Rossell SL (2018) A systematic review of the structural neuroimaging correlates of thought disorder. Neurosci Biobehav Rev 84:299–315. [DOI] [PubMed] [Google Scholar]
- Swardfager W, Rosenblat JD, Benlamri M, McIntyre RS (2016) Mapping inflammation onto mood: Inflammatory mediators of anhedonia. Neurosci Biobehav Rev 64:148–166. [DOI] [PubMed] [Google Scholar]
- Thayer JF, Lane RD (2009) Claude Bernard and the heart-brain connection: further elaboration of a model of neurovisceral integration. Neurosci Biobehav Rev 33:81–88. [DOI] [PubMed] [Google Scholar]
- Thygesen JH, Zambach SK, Ingason A, Lundin P, Hansen T, Bertalan M, Rosengren A, Bjerre D, Ferrero-Miliani L, Rasmussen HB, Parnas J, Werge T (2015) Linkage and whole genome sequencing identify a locus on 6q25-26 for formal thought disorder and implicate MEF2A regulation. Schizophr Res 169:441–446. [DOI] [PubMed] [Google Scholar]
- Trainor BC. (2011) Stress responses and the mesolimbic dopamine system: social contexts and sex differences. Horm Behav 60:457–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treadway MT, Zald DH (2011) Reconsidering anhedonia in depression: lessons from translational neuroscience. Neurosci Biobehav Rev 35:537–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treadway MT, Zald DH (2013) Parsing anhedonia: translational models of reward-processing deficits in psychopathology. Curr Dir Psychol Sci 22:244–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treynor W, Gonzalez R, Nolen-Hoeksema S (2003) Rumination reconsidered: a psychometric analysis. Cognit Ther Res 27:247–259. [Google Scholar]
- Turecki G. (2014) The molecular bases of the suicidal brain. Nat Rev Neurosci 15:802–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventura R, Cabib S, Puglisi-Allegra S (2002) Genetic susceptibility of mesocortical dopamine to stress determines liability to inhibition of mesoaccumbens dopamine and to behavioral ‘despair’ in a mouse model of depression. Neuroscience 115:999–1007. [DOI] [PubMed] [Google Scholar]
- Verdolini N, Menculini G, Perugi G, Murru A, Samalin L, Angst J, Azorin JM, Bowden CL, Mosolov S, Young AH, Barbuti M, Popovic D, Vieta E, Pacchiarotti I (2019) Sultans of swing: a reappraisal of the intertwined association between affective lability and mood reactivity in a post hoc analysis of the BRIDGE-II-MIX study. J Clin Psychiatry 80. [DOI] [PubMed] [Google Scholar]
- Wahl K, Ehring T, Kley H, Lieb R, Meyer A, Kordon A, Heinzel CV, Mazanec M, Schönfeld S (2019) Is repetitive negative thinking a transdiagnostic process? A comparison of key processes of RNT in depression, generalized anxiety disorder, obsessive-compulsive disorder, and community controls. J Behav Ther Exp Psychiatry 64:45–53. [DOI] [PubMed] [Google Scholar]
- Wensing T, Cieslik EC, Müller VI, Hoffstaedter F, Eickhoff SB, Nickl-Jockschat T (2017) Neural correlates of formal thought disorder: an activation likelihood estimation meta-analysis. Hum Brain Mapp 38:4946–4965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams JMG. (2001) Suicide and attempted suicide. Understanding the cry of pain. London: Penguin. [Google Scholar]
- Wilson ST, Chesin M, Fertuck E, Keilp J, Brodsky B, Mann JJ, Sönmez CC, Benjamin-Phillips C, Stanley B (2016) Heart rate variability and suicidal behavior. Psychiatry Res 240:241–247. [DOI] [PubMed] [Google Scholar]
- Xie DW, Deng ZL, Ishigaki T, Nakamura Y, Suzuki Y, Miyasato K, Ohara K, Ohara K (1995) The gene encoding the 5-HT1A receptor is intact in mood disorders. Neuropsychopharmacology 12:263–268. [DOI] [PubMed] [Google Scholar]
- Yaseen Z, Katz C, Johnson MS, Eisenberg D, Cohen LJ, Galynker II (2010) Construct development: the suicide trigger scale (STS-2), a measure of a hypothesized suicide trigger state. BMC Psychiatry 10:110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaseen ZS, Gilmer E, Modi J, Cohen LJ, Galynker II (2012) Emergency room validation of the revised suicide trigger scale (STS-3): a measure of a hypothesized suicide trigger state. PLoS One 7:e45157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaseen ZS, Kopeykina I, Gutkovich Z, Bassirnia A, Cohen LJ, Galynker II (2014) Predictive validity of the suicide trigger scale (STS-3) for post-discharge suicide attempt in high-risk psychiatric inpatients. PLoS One 9:e86768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaseen ZS, Galynker II, Briggs J, Freed RD, Gabbay V (2016) Functional domains as correlates of suicidality among psychiatric inpatients. J Affect Disord 203:77–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaseen ZS, Hawes M, Barzilay S, Galynker I (2018) Predictive validity of proposed diagnostic criteria for the suicide crisis syndrome: an acute presuicidal state. Suicide Life Threat Behav 49:1124–1135. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.