Abstract
OBJECTIVE
To report U.S. national population-based rates and trends in diabetic ketoacidosis (DKA) and hyperglycemic hyperosmolar state (HHS) among adults, in both the emergency department (ED) and inpatient settings.
RESEARCH DESIGN AND METHODS
We analyzed data from 1 January 2006 through 30 September 2015 from the Nationwide Emergency Department Sample and National Inpatient Sample to characterize ED visits and inpatient admissions with DKA and HHS. We used corresponding year cross-sectional survey data from the National Health Interview Survey to estimate the number of adults ≥18 years with diagnosed diabetes to calculate population-based rates for DKA and HHS in both ED and inpatient settings. Linear trends from 2009 to 2015 were assessed using Joinpoint software.
RESULTS
In 2014, there were a total of 184,255 and 27,532 events for DKA and HHS, respectively. The majority of DKA events occurred in young adults aged 18–44 years (61.7%) and in adults with type 1 diabetes (70.6%), while HHS events were more prominent in middle-aged adults 45–64 years (47.5%) and in adults with type 2 diabetes (88.1%). Approximately 40% of the hyperglycemic events were in lower-income populations. Overall, event rates for DKA significantly increased from 2009 to 2015 in both ED (annual percentage change [APC] 13.5%) and inpatient settings (APC 8.3%). A similar trend was seen for HHS (APC 16.5% in ED and 6.3% in inpatient). The increase was in all age-groups and in both men and women.
CONCLUSIONS
Causes of increased rates of hyperglycemic events are unknown. More detailed data are needed to investigate the etiology and determine prevention strategies.
Introduction
Uncontrolled hyperglycemia leading to diabetic ketoacidosis (DKA) and hyperglycemic hyperosmolar state (HHS) are life-threatening, preventable metabolic complications of diabetes, a disease affecting more than 30 million people in the U.S. (1). DKA, characterized by the triad of hyperglycemia (>250 mg/dL), metabolic acidosis, and increased blood ketone concentration, is more common among people with type 1 diabetes, while HHS, defined by severe hyperglycemia (>600 mg/dL), hyperosmolarity, and dehydration, without ketoacidosis, is more common among older adults with type 2 diabetes (2). Either condition can lead to coma and/or death. Precipitating causes of DKA include newly presenting disease, infections, and inadequate treatment (2). Up to 20% of adults present at diabetes diagnosis in DKA (2). HHS is less likely to be found at diabetes diagnosis, and common precipitating conditions include urinary tract infections, pneumonia, and acute cardiovascular events (2). No U.S. national data exist for HHS incidence.
A recent study reported a 55% increase in the rate of DKA hospitalizations from 2009 to 2014, most notable in the <45-year-old age-group (3). However, questions remain about trends in HHS as well as DKA and HHS trends in emergency department (ED) settings. By evaluating ED and inpatient data simultaneously, we address the potential ascertainment bias associated with changes in hospital admission thresholds. We also present the numerator data by diabetes type, which have been lacking in the past. To our knowledge, this is the first comprehensive report to assess both DKA and HHS trends in both ED and inpatient settings.
Research Design and Methods
Data Sources
We analyzed 1 January 2006 through 30 September 2015 data from the Agency for Healthcare Research and Quality’s Nationwide Emergency Department Sample (NEDS) and National Inpatient Sample (NIS). NEDS and NIS, the largest all-payer ED and inpatient databases in the U.S., include ∼31 million and 7 million unweighted visits, respectively (4). Both data sets approximate a 20% stratified sample of discharges and can be weighted to provide estimates at the national level. Rehabilitation and long-term acute care hospitals are excluded from NIS. Both NEDS and NIS include International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM) codes as well as patient demographics, hospital characteristics, payment sources, patient disposition, and total charges. NEDS and NIS are event-based data, so we were not able to account for multiple admissions for an individual person within a single year. For 2015, we used data through 30 September because starting on 1 October, coding shifted from ICD-9-CM to ICD-10-CM.
We used 2006–2015 cross-sectional survey data from the National Center for Health Statistics’ National Health Interview Survey (NHIS) to estimate the number of adults with diagnosed diabetes among the noninstitutionalized U.S. civilian population aged ≥18 years. These estimates are used in the denominator for rate calculation, both overall and for specific characteristics. NHIS is a nationally representative, in-person household survey that relies on self-reported behaviors and medical conditions (5). Respondents are asked, other than during pregnancy, whether a health care professional had told them that they had diabetes. NHIS does not distinguish between diabetes type.
Definitions and Variables
DKA and HHS ED visits and inpatient admissions were defined by a first-listed ICD-9-CM diagnosis code of 250.1 (diabetes with ketoacidosis) and 250.2 (diabetes with hyperosmolarity), respectively. We reported patient characteristics by diabetes type, age-group, sex, race/ethnicity (available in NIS and NHIS but not NEDS), location (urban/rural), primary payer, poverty status, disposition, and U.S. region. Diabetes type was based on the ICD-9-CM fifth digit subclassification: a 1 or 3 was considered type 1 diabetes, and 0 and 2 were considered type 2 diabetes. If there was a discrepancy in diabetes type among multiple codes for the same patient, the type was considered unknown. ICD-9-CM coding in NEDS and NIS has not been validated against medical records for DKA, HHS, or type 1 or type 2 diabetes. Patient county locations with a population size of ≥50,000 were considered urban; not metropolitan or micropolitan counties were considered rural. Payers in NEDS and NIS are the expected primary payer, including Medicare, Medicaid, private insurance, and uninsured (4). In NHIS, if a participant had more than one kind of health insurance that included Medicare Part A coverage (e.g., Medicare and private insurance), we considered their age, retired status, and disabled status to determine the likely primary payer based on a 2018 Medicare user guide (6). In general, if the survey participant was retired, we assumed Medicare paid first. Otherwise, we assumed private insurance was the primary payer. We assumed the survey participant was working for a large employer when employer size was a factor in determining the primary payer. Poverty status was defined using the estimated median household income of the patient’s zip code, divided into quartiles. The lowest quartile was considered the poorest population.
Statistical Analysis
We reported the crude weighted number of patients with DKA and HHS for both 2006 and 2014, stratified by diabetes type, age-group, sex, race/ethnicity (inpatient only), location (urban/rural), primary payer, poverty status, disposition, and U.S. region for both the ED and inpatient settings. To avoid double counting, we excluded ED visits where the disposition was admission to the hospital because these hyperglycemic episodes were accounted for in the inpatient data. The weighted results estimate the number of ED visits and hospital admissions in the U.S. due to these conditions.
Event rates from 2006 to 2015 were calculated for each of the conditions in both ED and inpatient settings by using the number of adults with the specified condition from NEDS and NIS in the numerator divided by the adult population with diagnosed diabetes from NHIS. In 2015, the denominator from NHIS was adjusted to account for the partial year used in the numerator by multiplying by 0.75. We used the 2000 U.S. Census for age adjustment using age-groups 18–44, 45–64, and ≥65 years. We used SAS-callable SUDAAN (RTI International) to account for the complex sampling design in NEDS, NIS, and NHIS, and the Taylor series linearization was used to estimate the variance of the ratio of the numerator and denominator. Because previous studies have already identified an increase in DKA rates starting in 2009, we used Joinpoint Trend Analysis Software (version 4.5.0.1) to analyze event rate trends from 2009 to 2015, overall and by age-group, sex, primary payer, and U.S. region. With the exception of age-group, all rates were age-adjusted. We were not able to calculate rates by diabetes type because this question was not asked in NHIS during the study period. Location (urban/rural) and poverty status, although available in NHIS, were not categorized in the same way as in NEDS and NIS, so these factors were also excluded from rate calculations. In addition, the race/ethnicity variable in NIS was incomplete prior to 2012, so trends were not calculated by race/ethnicity.
Joinpoint Trend Analysis can identify statistically significant changes in linear trends (direction or magnitude) and calculates the annual percentage change (APC) for each identified time segment (7). To assess for a linear trend over the 7-year period from 2009 to 2015, we selected a maximum of zero joinpoints. We considered trends statistically significant if they had a two-sided P value <0.05.
Results
Diabetic Ketoacidosis
In 2014, there were an estimated 16,070 U.S. adult ED visits for DKA where the patient was not admitted to an inpatient unit (Table 1). In that same year, there were 168,185 adult admissions to inpatient settings in U.S. hospitals for DKA. Of all adults with DKA, in 2014, 70.6% of those admitted to the ED or inpatient setting for DKA had type 1 diabetes, and 61.7% were in the 18–44-year-old age-group. Over 80% of the patients with DKA were from urban settings. From 2006 to 2014, there was an increase in the proportion of adults with DKA having public health insurance (i.e., Medicare or Medicaid) as the primary payer from 41.9% in 2006 to 54.4% in 2014. In both years, almost 40% of patients with DKA had zip codes in the lowest household income quartile. Over 80% of inpatient admissions for DKA resulted in routine discharges to home. Less than 1% of patients died in the hospital. In both years, the Northeast region had the lowest number of DKA episodes, while the South had the highest (Table 1).
Table 1.
Characteristics of adults with DKA, NEDS and NIS 2006 and 2014
| Total | ED | Inpatient | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2006 | 2014 | 2006 | 2014 | 2006 | 2014 | |||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| Weighted total, N | 122,330 | 184,255 | 10,541 | 16,070 | 111,789 | 168,185 | ||||||
| Diabetes type | ||||||||||||
| 1 | 75,594 | 62.0 | 129,515 | 70.6 | 5,879 | 56.3 | 10,705 | 67.3 | 69,715 | 62.5 | 118,810 | 70.9 |
| 2 | 46,391 | 38.0 | 53,941 | 29.4 | 4,562 | 43.7 | 5,196 | 32.7 | 41,829 | 37.5 | 48,745 | 29.1 |
| Age-group, years | ||||||||||||
| 18–44 | 81,136 | 66.3 | 113,709 | 61.7 | 7,558 | 71.7 | 10,934 | 68.0 | 73,578 | 65.8 | 102,775 | 61.1 |
| 45–64 | 33,795 | 27.6 | 55,525 | 30.1 | 2,562 | 24.3 | 4,195 | 26.1 | 31,233 | 27.9 | 51,330 | 30.5 |
| 65–74 | 4,453 | 3.6 | 9,831 | 5.3 | 239 | 2.3 | 576 | 3.6 | 4,214 | 3.8 | 9,255 | 5.5 |
| 75+ | 2,946 | 2.4 | 5,190 | 2.8 | 182 | 1.7 | 365 | 2.3 | 2,764 | 2.5 | 4,825 | 2.9 |
| Women | 60,084 | 49.2 | 90,994 | 49.4 | 4,867 | 46.2 | 7,529 | 46.9 | 55,217 | 49.5 | 83,465 | 49.6 |
| Men | 62,109 | 50.8 | 93,231 | 50.6 | 5,674 | 53.8 | 8,541 | 53.1 | 56,435 | 50.5 | 84,690 | 50.4 |
| Race/ethnicity | ||||||||||||
| Non-Hispanic white | NA | NA | NA | NA | NA | 93,720 | 58.3 | |||||
| Non-Hispanic black | NA | NA | NA | NA | NA | 41,740 | 26.0 | |||||
| Non-Hispanic Asian* | NA | NA | NA | NA | NA | 1,800 | 1.1 | |||||
| Non-Hispanic other | NA | NA | NA | NA | NA | 5,500 | 3.4 | |||||
| Hispanic | NA | NA | NA | NA | NA | 17,940 | 11.2 | |||||
| Location | ||||||||||||
| Urban | 99,786 | 82.0 | 151,039 | 82.4 | 8,372 | 80.0 | 12,094 | 75.9 | 91,414 | 82.2 | 138,945 | 83.0 |
| Micropolitan | 13,496 | 11.1 | 18,832 | 10.3 | 1,120 | 10.7 | 1,957 | 12.3 | 12,376 | 11.1 | 16,875 | 10.1 |
| Rural | 8,356 | 6.9 | 13,386 | 7.3 | 973 | 9.3 | 1,891 | 11.9 | 7,383 | 6.6 | 11,495 | 6.9 |
| Payer | ||||||||||||
| Medicare | 21,140 | 17.3 | 39,960 | 21.7 | 1,327 | 12.6 | 2,500 | 15.6 | 19,813 | 17.8 | 37,460 | 22.3 |
| Medicaid | 30,071 | 24.6 | 60,102 | 32.7 | 2,697 | 25.7 | 5,687 | 35.5 | 27,374 | 24.5 | 54,415 | 32.4 |
| Private | 36,071 | 29.6 | 50,035 | 27.2 | 3,142 | 29.9 | 4,585 | 28.6 | 32,929 | 29.5 | 45,450 | 27.1 |
| Uninsured | 24,666 | 20.2 | 25,982 | 14.1 | 2,531 | 24.1 | 2,442 | 15.3 | 22,135 | 19.8 | 23,540 | 14.0 |
| Other | 10,118 | 8.3 | 7,702 | 4.2 | 802 | 7.7 | 797 | 5.0 | 9,316 | 8.4 | 6,905 | 4.1 |
| Household income† | ||||||||||||
| First quartile (poorest) | 44,034 | 37.2 | 69,798 | 38.8 | 4,152 | 40.6 | 6,183 | 39.2 | 39,882 | 36.8 | 63,615 | 38.7 |
| Second quartile | 32,225 | 27.2 | 51,642 | 28.7 | 2,684 | 26.2 | 4,782 | 30.4 | 29,541 | 27.3 | 46,860 | 28.5 |
| Third quartile | 25,479 | 21.5 | 36,262 | 20.1 | 2,150 | 21.0 | 3,012 | 19.1 | 23,329 | 21.5 | 33,250 | 20.2 |
| Fourth quartile (wealthiest) | 16,789 | 14.1 | 22,374 | 12.4 | 1,247 | 12.2 | 1,779 | 11.3 | 15,542 | 14.4 | 20,595 | 12.5 |
| Disposition | ||||||||||||
| Routine (home) | 100,418 | 82.1 | 151,065 | 82.0 | 7,385 | 70.1 | 13,115 | 81.6 | 93,033 | 83.2 | 137,950 | 82.1 |
| SNF or home health‡ | 13,135 | 10.7 | 21,622 | 11.7 | 565 | 5.3 | 857 | 5.4 | 12,570 | 11.2 | 20,765 | 12.3 |
| AMA | 6,623 | 5.4 | 10,641 | 5.8 | 1,002 | 9.5 | 1,881 | 11.7 | 5,621 | 5.0 | 8,760 | 5.2 |
| Died | 582 | 0.5 | 727 | 0.4 | 46 | 0.4 | 107 | 0.7 | 536 | 0.5 | 620 | 0.4 |
| Unknown§ | 1,547 | 1.3 | 140 | 0.1 | 1,543 | 14.6 | 110 | 0.7 | 4 | 0.0 | 30 | 0.0 |
| U.S. region‖ | ||||||||||||
| Northeast | 20,725 | 16.9 | 26,730 | 14.5 | 1,234 | 11.7 | 1,980 | 12.3 | 19,491 | 17.4 | 24,750 | 14.7 |
| Midwest | 26,443 | 21.6 | 42,654 | 23.1 | 2,601 | 24.7 | 5,084 | 31.6 | 23,842 | 21.3 | 37,570 | 22.3 |
| South | 52,137 | 42.6 | 79,086 | 42.9 | 4,736 | 44.9 | 5,831 | 36.3 | 47,401 | 42.4 | 73,255 | 43.6 |
| West | 23,025 | 18.8 | 35,785 | 19.4 | 1,970 | 18.7 | 3,175 | 19.8 | 21,055 | 18.8 | 32,610 | 19.4 |
Percentages were based on nonmissing data, which were <5% for all stratifying variables. AMA, left against medical advice; NA, not available; SNF, skilled nursing facility.
Includes Pacific Islanders.
Median household income for patient’s zip code.
For inpatient, also includes transfer to other short-term hospital.
For ED, not admitted to the inpatient setting; for inpatient, did not die.
As defined by the U.S. Census Bureau.
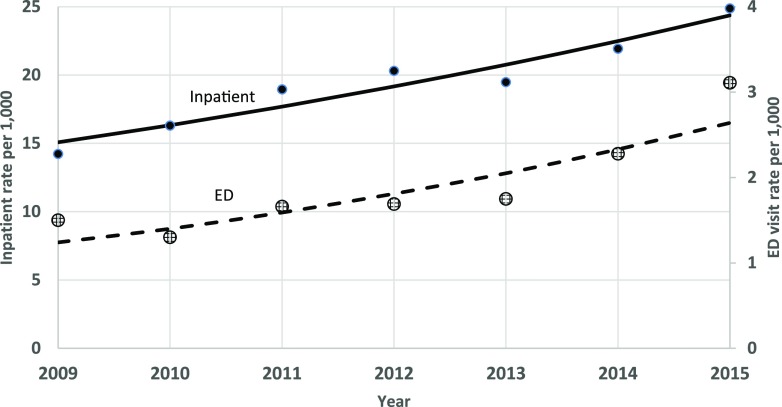
Overall, U.S. adult nonadmitted ED visit rates for DKA doubled from 2009 to 2015 from 1.5 to 3.1 per 1,000 adults with diabetes (APC 13.5% [95% CI 5.9%, 21.6%], P ≤ 0.01) (Fig. 1 and Supplementary Table 1). In the inpatient setting, DKA rates increased 75.4% from 14.2 to 24.9 per 1,000 adults with diabetes (APC 8.3% [95% CI 5.2%, 11.6%], P ≤ 0.01) (Fig. 1 and Supplementary Table 2). The increasing trend was seen in both ED and inpatient settings for both men and women, with men having ∼1.7 times the APC as women (Supplementary Tables 1 and 2). In the inpatient setting, all age-groups experienced a significant increase in DKA rates from 2009 to 2015. However, the 18–44-year-old age-group had the highest rates (24.4 to 43.5 per 1,000 with diabetes versus 1.1 to 1.6 per 1,000 with diabetes in the ≥65-year-old age-group). Patients with Medicare or Medicaid as the primary payer had the highest DKA event rates in both the ED and inpatient settings. An increasing trend in DKA rates in the ED setting was seen for all but the uninsured. In the inpatient setting, Medicaid and private insurance had increasing DKA trends. DKA rates increased in the ED setting in the Midwest and West, and in the inpatient setting, rates increased in the Midwest, South, and West. In 2015, DKA rates were highest in the South (26.4 per 1,000 adults with diabetes) and Midwest (26.2 per 1,000 adults with diabetes) (Supplementary Table 2).
Figure 1.
Age-adjusted DKA ED and hospitalization rates per 1,000 adults with diagnosed diabetes, 2009–2015. Numerator data are from the NEDS and NIS. Denominator data are from National Center for Health Statistics’ NHIS. Dots are observed annual values. The lines are modeled using Joinpoint Trend Analysis Software. The 2000 U.S. Census was used for age-adjustment using age-groups 18–44, 45–64, and ≥65 years.
Hyperglycemic Hyperosmolar State
In 2014, there were an estimated 2,557 U.S. adult ED visits for HHS where the patient was not admitted to an inpatient unit (Table 2). In that same year, there were 24,975 adult admissions to inpatient settings in U.S. hospitals for HHS. Overall, in 2014, 88.1% of the adults admitted to the ED or inpatient setting with HHS had type 2 diabetes, 47.5% were in the 45–64-year-old age-group, and 56.5% were men. Over 80% of the patients were from urban settings. Similar to DKA, from 2006 to 2014, there was an increase in the proportion of adults with HHS having public health insurance (i.e., Medicare or Medicaid) as the primary payer from 57.9% in 2006 to 67.1% in 2014. In 2014, 42.7% of patients with HHS events had zip codes in the lowest household income quartile. In both years, ∼70% of inpatient admissions for HHS resulted in routine discharges to home. Approximately a quarter were discharged to skilled nursing facilities, other short-term hospitals, or with home care. From 2006 to 2014, the proportion dying in the hospital setting declined from 1.7% to 0.8%. The West region had the lowest number of HHS episodes, while the South had the highest (Table 2).
Table 2.
Characteristics of adults with HHS, NEDS and NIS 2006 and 2014
| Total | ED | Inpatient | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2006 | 2014 | 2006 | 2014 | 2006 | 2014 | |||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| Weighted total, N | 15,400 | 27,532 | 682 | 2,557 | 14,718 | 24,975 | ||||||
| Diabetes type | ||||||||||||
| 1 | 1,563 | 10.2 | 3,279 | 11.9 | 80 | 11.8 | 279 | 10.9 | 1,483 | 10.1 | 3,000 | 12.0 |
| 2 | 13,822 | 89.8 | 24,223 | 88.1 | 596 | 88.2 | 2,278 | 89.1 | 13,226 | 89.9 | 21,945 | 88.0 |
| Age-group, years | ||||||||||||
| 18–44 | 4,010 | 26.0 | 6,539 | 23.8 | 288 | 42.2 | 934 | 36.5 | 3,722 | 25.3 | 5,605 | 22.4 |
| 45–64 | 6,808 | 44.2 | 13,081 | 47.5 | 247 | 36.2 | 1,126 | 44.0 | 6,561 | 44.6 | 11,955 | 47.9 |
| 65–74 | 2,282 | 14.8 | 4,238 | 15.4 | 88 | 12.9 | 273 | 10.7 | 2,194 | 14.9 | 3,965 | 15.9 |
| 75+ | 2,300 | 14.9 | 3,674 | 13.3 | 59 | 8.7 | 224 | 8.8 | 2,241 | 15.2 | 3,450 | 13.8 |
| Women | 6,852 | 46.1 | 11,973 | 43.5 | 335 | 49.1 | 1,098 | 42.9 | 6,517 | 44.3 | 10,875 | 43.6 |
| Men | 8,549 | 53.9 | 15,554 | 56.5 | 347 | 50.9 | 1,459 | 57.1 | 8,202 | 55.7 | 14,095 | 56.4 |
| Race/ethnicity | ||||||||||||
| Non-Hispanic white | NA | NA | NA | NA | NA | 10,795 | 45.1 | |||||
| Non-Hispanic black | NA | NA | NA | NA | NA | 9,135 | 38.2 | |||||
| Non-Hispanic Asian* | NA | NA | NA | NA | NA | 350 | 1.4 | |||||
| Non-Hispanic other | NA | NA | NA | NA | NA | 865 | 3.6 | |||||
| Hispanic | NA | NA | NA | NA | NA | 2,775 | 11.6 | |||||
| Location | ||||||||||||
| Urban | 12,771 | 83.3 | 23,011 | 84.2 | 498 | 73.3 | 1,941 | 76.1 | 12,273 | 83.8 | 21,070 | 85.0 |
| Micropolitan | 1,573 | 10.3 | 2,634 | 9.6 | 96 | 14.1 | 319 | 12.5 | 1,477 | 10.1 | 2,315 | 9.3 |
| Rural | 986 | 6.4 | 1,689 | 6.2 | 85 | 12.5 | 289 | 11.3 | 901 | 6.1 | 1,400 | 5.6 |
| Payer | ||||||||||||
| Medicare | 6,077 | 39.5 | 11,759 | 42.8 | 177 | 26.1 | 794 | 31.2 | 5,900 | 40.2 | 10,965 | 44.0 |
| Medicaid | 2,825 | 18.4 | 6,673 | 24.3 | 131 | 19.3 | 708 | 27.8 | 2,694 | 18.3 | 5,965 | 23.9 |
| Private | 3,754 | 24.4 | 5,214 | 19.0 | 183 | 27.0 | 504 | 19.8 | 3,571 | 24.3 | 4,710 | 18.9 |
| Uninsured | 2,002 | 13.0 | 2,755 | 10.0 | 164 | 24.2 | 415 | 16.3 | 1,838 | 12.5 | 2,340 | 9.4 |
| Other | 711 | 4.6 | 1,057 | 3.8 | 24 | 3.5 | 127 | 5.0 | 687 | 4.7 | 930 | 3.7 |
| Household income† | ||||||||||||
| First quartile (poorest) | 5,922 | 39.8 | 11,419 | 42.7 | 284 | 42.1 | 1,114 | 44.0 | 5,638 | 39.7 | 10,305 | 42.5 |
| Second quartile | 3,775 | 25.4 | 7,308 | 27.3 | 201 | 29.8 | 738 | 29.1 | 3,574 | 25.2 | 6,570 | 27.1 |
| Third quartile | 3,040 | 20.5 | 4,922 | 18.4 | 126 | 18.7 | 397 | 15.7 | 2,914 | 20.5 | 4,525 | 18.7 |
| Fourth quartile (wealthiest) | 2,127 | 14.3 | 3,124 | 11.6 | 63 | 9.3 | 284 | 11.2 | 2,064 | 14.5 | 2,840 | 11.7 |
| Disposition | ||||||||||||
| Routine (home) | 10,800 | 70.1 | 19,236 | 69.9 | 574 | 84.2 | 2,221 | 86.9 | 10,226 | 69.5 | 17,015 | 68.1 |
| SNF or home health‡ | 3,894 | 25.3 | 7,091 | 25.8 | 29 | 4.2 | 126 | 4.9 | 3,865 | 26.2 | 6,965 | 27.9 |
| AMA | 410 | 2.7 | 951 | 3.5 | 31 | 4.5 | 161 | 6.3 | 379 | 2.6 | 790 | 3.2 |
| Died | 249 | 1.6 | 208 | 0.8 | 5 | 0.7 | 18 | 0.7 | 244 | 1.7 | 190 | 0.8 |
| Unknown§ | 47 | 0.3 | 41 | 0.1 | 43 | 6.3 | 31 | 1.2 | 4 | 0.0 | 10 | 0.0 |
| U.S. region‖ | ||||||||||||
| Northeast | 3,509 | 22.8 | 5,485 | 19.9 | 115 | 16.9 | 395 | 15.4 | 3,394 | 23.1 | 5,090 | 20.4 |
| Midwest | 2,761 | 17.9 | 5,669 | 20.6 | 117 | 17.2 | 604 | 23.6 | 2,644 | 18.0 | 5,065 | 20.3 |
| South | 6,793 | 44.1 | 11,974 | 43.5 | 392 | 57.5 | 1,099 | 43.0 | 6,401 | 43.5 | 10,875 | 43.5 |
| West | 2,337 | 15.2 | 4,404 | 16.0 | 58 | 8.5 | 459 | 18.0 | 2,279 | 15.5 | 3,945 | 15.8 |
Percentages were based on nonmissing data, which were <5% for all stratifying variables. AMA, left against medical advice; NA, not available; SNF, skilled nursing facility.
Includes Pacific Islanders.
Median household income for patient’s zip code.
For inpatient, also includes transfer to other short-term hospital.
For ED, not admitted to the inpatient setting; for inpatient, did not die.
As defined by the U.S. Census Bureau.
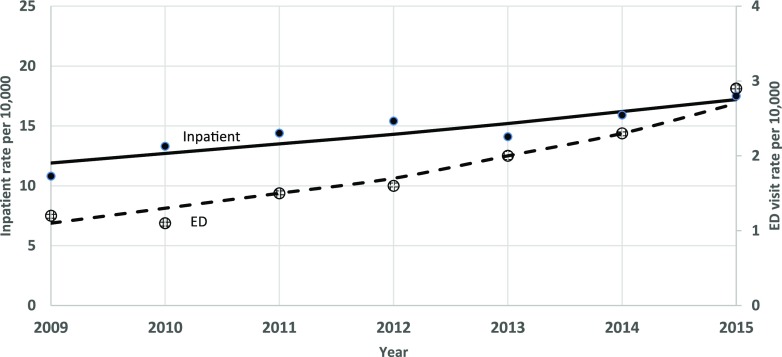
Overall, U.S. adult nonadmitted ED visit rates for HHS more than doubled from 2009 to 2015 from 1.2 to 2.9 per 10,000 adults with diabetes (APC 16.5% [95% CI 11.7%, 21.5%], P ≤ 0.01) (Fig. 2 and Supplementary Table 3). In the inpatient setting, HHS rates increased 62.0% from 10.8 (n = 18,193) to 17.5 per 10,000 adults with diabetes (n = 24,975 in 2014; APC 6.3% [95% CI 2.3%, 10.4%], P ≤ 0.01) (Fig. 2 and Supplementary Table 4). The significantly increasing trend was seen in both ED and inpatient settings for both men and women and for all age-groups (Supplementary Tables 3 and 4). Patients with Medicare or Medicaid as the primary payer had the highest HHS event rates in the inpatient setting but varied in the ED setting. The privately insured had consistently lower HHS rates in both settings. An increasing trend in HHS rates in the ED setting was seen for patients with public sponsored programs but not for privately insured or uninsured patients. Only the population with private insurance as the primary payer had a significant increase in HHS events in the inpatient setting. HHS rates increased in the ED setting in all regions of the country, and in the inpatient setting, rates increased in all but the Northeast region. In 2015, inpatient HHS rates were highest in the South (20.2 per 10,000 adults with diabetes) and Northeast (19.6 per 10,000 adults with diabetes) (Supplementary Table 4).
Figure 2.
Age-adjusted HHS ED and hospitalization rates per 10,000 adults with diagnosed diabetes, 2009–2015. Numerator data are from the NEDS and NIS. Denominator data are from National Center for Health Statistics’ NHIS. Dots are observed annual values. The lines are modeled using Joinpoint Trend Analysis Software. The 2000 U.S. Census was used for age-adjustment using age-groups 18–44, 45–64, and ≥65 years.
Hyperglycemic Crises
The contribution of each complication (DKA and HHS) across patient care settings (ED and inpatient) and diabetes type (type 1 and type 2) is important to assess. DKA, treated in the inpatient setting, made up ∼80% of cases of hyperglycemic crises for both 2006 and 2014, with over half of patients having type 1 diabetes (Supplementary Fig. 1). HHS, treated in the inpatient setting, contributed ∼11% of the hyperglycemic cases, and almost 90% of those patients had type 2 diabetes. Nonadmitted DKA and HHS cases in the ED setting comprised the remaining cases of hyperglycemic crises.
Conclusions
For DKA, the burden was highest among young adults 18–44 years of age and for adults with type 1 diabetes. For HHS, close to 90% of episodes were among adults with type 2 diabetes, and although most episodes were in people 45–64 years of age, rates were highest in younger adults. Trends varied by subpopulations, but overall, DKA and HHS rates increased from 2009 to 2015 overall and for all age-groups, in both men and women, in both ED and inpatient settings, and in most regions of the country. The APCs were similar and higher in the ED setting for both conditions, but the burden was higher in the inpatient setting.
This comprehensive report adds to the growing literature on the resurgence of diabetes complications in the U.S. (8,9). We show that both DKA and HHS are increasing overall and in all age categories and both sexes. By including the ED setting in our analysis, we also refute the hypothesis that a change in the threshold for hyperglycemic crises warranting hospital admissions may be contributing to this finding (3). In fact, we also saw an increase in ED visit rates for DKA and HHS in patients who were treated and not admitted to hospitals.
In England, a different trend in DKA hospitalizations was described for people with type 1 diabetes. Zhong et al. (10) found an increase in incidence from 1998 to 2007 and then a flattening, whereas for type 2 diabetes, incidence gradually increased at 4.2% annually from 1998 to 2013. Although we are not able to differentiate trends by diabetes type, we see a rapid increase in DKA starting in 2009 in the U.S. (3). The demographic characteristics of patients with hyperglycemic crises in this analysis were similar to those in other studies. For example, although often perceived as a complication of type 1 diabetes, we found that roughly one-third of DKA cases were patients with type 2 diabetes and that DKA was predominantly a problem among young adults (11,12). We also found HHS occurring mostly in patients with type 2 diabetes who were older (13). However, HHS event rates were highest in the youngest age category. HHS is recognized as an emerging issue in children and young adults (14). Other studies using NIS have found similar increases in hyperglycemic crisis events but use different denominators (15,16). Our study is unique in that we report rates by the population with diagnosed diabetes, which accounts for changes in diabetes epidemiology over time. In addition, we report estimates for HHS, which does not appear in the literature.
The etiology of the resurgence of DKA and HHS is unknown, but numerous causes are possible. Infections are a precipitating cause of both DKA and HHS (2), with urinary tract infections and pneumonia being specifically associated with HHS (17). Overall, infections requiring hospitalization among adults with diabetes did not increase from 2000 to 2015 (18). The incidence of skin and soft tissue infections, including cellulitis, foot infections, and osteomyelitis, increased among adults with diabetes from 2009 to 2015, but pneumonia rates remained flat over time (18). Noninfectious acute events, such myocardial infarction and stroke, are also precipitating causes of HHS (19). During the same time period that DKA and HHS rates increased, myocardial infarction and stroke increased among adults with diabetes in younger age-groups (8). It is possible that these acute events led to increased rates of HHS in the younger population, but again, it does not explain the increases in both conditions in all age-groups.
The frequency of alcohol and drug abuse is high among patients presenting with DKA (20,21). A recent meta-analysis of survey data reported on the increased prevalence of alcohol use and binge drinking over the past 10–15 years (20). Middle-aged and older adults were most affected. This would not explain the sharp increase in DKA event rates in young adults nor the increase in HHS event rates. However, cannabis use has also been found to increase the risk of DKA among patients with type 1 diabetes (22). These patients were younger with a mean age of 31 years and were more likely to be male. Data from the Substance Abuse and Mental Health Services Administration’s National Survey on Drug Use and Health shows an increase in cannabis use from 2007 to 2013 (23). It cannot be determined with these data whether and to what degree alcohol and drug abuse are contributing to the increase in hyperglycemic events.
Sodium–glucose cotransporter 2 inhibitors, approved for treatment of type 2 diabetes, have been found to increase the risk of DKA. In May 2015, the U.S. Food and Drug Administration issued a drug safety communication about this risk (24) and subsequently added a warning to the drug label (25). The U.S. Food and Drug Administration has not approved the use of sodium–glucose cotransporter 2 inhibitors in patients with type 1 diabetes. Although this drug class was first approved in March 2013 and therefore was not responsible for the initial increase in DKA episodes, it is worthy of further monitoring.
Insulin omission is the most common cause of DKA in young patients with type 1 diabetes (2). Causes of poor adherence to insulin are varied and include eating disorders, fear of weight gain, psychological distress, and fear of hypoglycemia (26). Insulin prices tripled from 2002 to 2013 in the U.S. (27), and evidence has shown that increasing insulin prices often lead patients to ration their insulin (28). How much these changes have contributed to the upward trend in hyperglycemic crises is unknown. However, since ∼40% of these acute events are occurring in patients who live in poorer zip codes, one hypothesis may be that the cost of insulin may be a factor leading to adverse events. The data on primary payers, however, do not consistently support this theory. Uninsured patients accounted for only a small proportion of the total cases of hyperglycemic crisis events and their event rates were flat from 2009 to 2015. The majority of the hyperglycemic crisis events and the highest event rates occurred in the population with Medicare or Medicaid as the primary payer, with increasing rates from 2009 to 2015 in the Medicaid population for both DKA and HHS (except for hospitalizations for HHS).
Medicaid beneficiaries with diabetes generally self-report having poorer health and more comorbidities than other insured populations (29). Despite the fact that Medicaid either pays for most medications or requires a nominal copayment, out-of-pocket costs for medications and medical care are still a concern and, in some cases, may lead to insulin rationing (29,30). Medicare beneficiaries with prescription drug coverage (i.e., those enrolled in Medicare Part D or Medicare Advantage plans) and privately insured populations generally have deductibles and copayments for medications, which can lead to high out-of-pocket costs (28). We found that hyperglycemic crisis event rates increased in the Medicare population in the ED setting and increased in the inpatient setting for the privately insured, albeit at rates much lower than the Medicare or Medicaid insured population.
Ketosis-prone diabetes has been described since the 1980s and has an atypical presentation, including severe hyperglycemia and ketoacidosis with no precipitating cause (31,32). These patients usually have obesity with a strong family history of type 2 diabetes and often recover after treatment without the need of further insulin treatment. Though these patients may be contributing to the overall numbers of patients classified in the ED and inpatient settings as having DKA, we did not find evidence in the literature that this disease variant is increasing in the population, and thus it is unlikely to explain the increasing trend of hyperglycemic crises.
This study had a number of limitations. First, because of the inability to differentiate diabetes type in the NHIS survey data, we were not able to report trends in DKA and HHS rates by diabetes type. Although consistent with the literature, even the hyperglycemic crisis event numbers by diabetes type were subject to misclassification based on coding errors. Second, NEDS and NIS are event-level data, not patient-level data. We do not know how many of these events were readmissions versus new events, which would falsely increase population-based rates, especially in certain subpopulations at higher risk for recurrence (33,34). Third, the case definitions of DKA and HHS were based on first-listed ICD-9-CM codes. Events may have been misclassified by coding errors or missed if the hyperglycemic code was not selected as the primary diagnosis (35). Application of strict diagnostic criteria may also be lacking, as evidenced by the low mortality disposition of those admissions with HHS, which is inconsistent with case studies (36). However, these potential misclassifications and missed events were not likely to affect trends in rates over time. Fourth, we did not consider the comorbid diagnoses of DKA and HHS. Pasquel et al. (37) found this unique subset of patients to have a higher in-hospital mortality rate. Fifth, the duration of diabetes is unknown using these data sets, so we were not able to stratify the analysis by newly diagnosed versus established disease. Sixth, from 2009 to 2014, there was a decline in the total number of hospital admissions with the primary code of 250.3 (diabetes with other coma) from 3,820 to 2,135. This code does not differentiate hyper- from hypoglycemic coma, which may be the reason for the decreased use. If these cases were instead classified as DKA or HHS, this coding change would boost DKA and HHS rates but not enough to fully explain the increasing trend. Finally, although NEDS and NIS are the largest administrative data sets for U.S. ED visits and inpatient admissions and are nationally representative, federal hospitals are not included in the sample, which excludes a small segment of the U.S. population.
In summary, we report an overall increase in DKA and HHS event rates among adults in both the ED and inpatient settings in the U.S. from 2009 to 2015. The increase is occurring in all age-groups, in both sexes, and in all regions of the country, suggesting that widespread societal factors may be influencing this trend. Although these data do not provide a definitive etiology, we do see some subpopulations at high risk of acute diabetic complications such as young adults, people with lower income, and people with public insurance as the primary payer. A deeper dive into data with more clinical, economic, and community characteristics may help determine the specific factors leading to these trends, which may, in turn, help determine preventive measures for these life-threatening, yet avoidable, complications of diabetes.
Supplementary Material
Article Information
Funding. F.J.P. is partially supported by a National Institutes of Health grant from the National Institute of General Medical Sciences (1K23-GM-128221-01A1).
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. S.R.B. developed the study concept, performed analysis and interpretation of the data, and drafted the manuscript. I.H. analyzed the data. F.J.P., E.W.G, A.L.A., and G.I. participated in the study design and interpretation of the data and critically revised the manuscript. S.R.B. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
This article contains Supplementary Data online at https://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc19-2449/-/DC1.
References
- 1.Centers for Disease Control and Prevention National Diabetes Statistics Report, 2017. Atlanta, GA, Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services, 2017 [Google Scholar]
- 2.Fayfman M, Pasquel FJ, Umpierrez GE. Management of hyperglycemic crises: diabetic ketoacidosis and hyperglycemic hyperosmolar state. Med Clin North Am 2017;101:587–606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benoit SR, Zhang Y, Geiss LS, Gregg EW, Albright A. Trends in diabetic ketoacidosis hospitalizations and in-hospital mortality - United States, 2000-2014. MMWR Morb Mortal Wkly Rep 2018;67:362–365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project. [Internet], 2019. Available from https://www.hcup-us.ahrq.gov. Accessed 18 June 2019.
- 5.Parsons VL, Moriarity C, Jonas K, Moore TF, Davis KE, Tompkins L. Design and estimation for the national health interview survey, 2006-2015. Vital Health Stat 2 2014;165:1–53 [PubMed] [Google Scholar]
- 6. Centers for Medicare & Medicaid Services. Medicare & Other Health Benefits: Your Guide to Who Pays First [Internet], 2018. Available from https://www.medicare.gov/Pubs/pdf/02179-medicare-coordination-benefits-payer.pdf. Accessed 14 August 2019.
- 7.National Cancer Institute Joinpoint Trend Analysis Software. [Internet], 2019. Available from https://surveillance.cancer.gov/joinpoint/. Accessed 18 June 2019.
- 8.Gregg EW, Hora I, Benoit SR. Resurgence in diabetes-related complications. JAMA 2019;321:1867–1868 [DOI] [PubMed] [Google Scholar]
- 9.Geiss LS, Li Y, Hora I, Albright A, Rolka D, Gregg EW. Resurgence of diabetes-related nontraumatic lower-extremity amputation in the young and middle-aged adult U.S. population. Diabetes Care 2019;42:50–54 [DOI] [PubMed] [Google Scholar]
- 10.Zhong VW, Juhaeri J, Mayer-Davis EJ. Trends in hospital admission for diabetic ketoacidosis in adults with type 1 and type 2 diabetes in England, 1998-2013: a retrospective cohort study. Diabetes Care 2018;41:1870–1877 [DOI] [PubMed] [Google Scholar]
- 11.Wang ZH, Kihl-Selstam E, Eriksson JW. Ketoacidosis occurs in both type 1 and type 2 diabetes--a population-based study from Northern Sweden. Diabet Med 2008;25:867–870 [DOI] [PubMed] [Google Scholar]
- 12.Miller KM, Foster NC, Beck RW, et al.; T1D Exchange Clinic Network . Current state of type 1 diabetes treatment in the U.S.: updated data from the T1D Exchange clinic registry. Diabetes Care 2015;38:971–978 [DOI] [PubMed] [Google Scholar]
- 13.Pasquel FJ, Umpierrez GE. Hyperosmolar hyperglycemic state: a historic review of the clinical presentation, diagnosis, and treatment. Diabetes Care 2014;37:3124–3131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rosenbloom AL. Hyperglycemic hyperosmolar state: an emerging pediatric problem. J Pediatr 2010;156:180–184 [DOI] [PubMed] [Google Scholar]
- 15.Desai D, Mehta D, Mathias P, Menon G, Schubart UK. Health care utilization and burden of diabetic ketoacidosis in the U.S. over the past decade: a nationwide analysis. Diabetes Care 2018;41:1631–1638 [DOI] [PubMed] [Google Scholar]
- 16.Desai R, Singh S, Syed MH, et al. Temporal trends in the prevalence of diabetes decompensation (diabetic ketoacidosis and hyperosmolar hyperglycemic state) among adult patients hospitalized with diabetes mellitus: a nationwide analysis stratified by age, gender, and race. Cureus 2019;11:e4353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wachtel TJ, Tetu-Mouradjian LM, Goldman DL, Ellis SE, O’Sullivan PS. Hyperosmolarity and acidosis in diabetes mellitus: a three-year experience in Rhode Island. J Gen Intern Med 1991;6:495–502 [DOI] [PubMed] [Google Scholar]
- 18.Harding JL, Benoit SR, Gregg EW, Pavkov ME, Perreault L. Trends in rates of infections requiring hospitalization among adults with versus without diabetes in the U.S., 2000-2015. Diabetes Care 2020;43:106–116 [DOI] [PubMed] [Google Scholar]
- 19.Karslioglu French E, Donihi AC, Korytkowski MT. Diabetic ketoacidosis and hyperosmolar hyperglycemic syndrome: review of acute decompensated diabetes in adult patients. BMJ 2019;365:l1114. [DOI] [PubMed] [Google Scholar]
- 20.Grucza RA, Sher KJ, Kerr WC, et al. Trends in adult alcohol use and binge drinking in the early 21st-century United States: a meta-analysis of 6 national survey series. Alcohol Clin Exp Res 2018;42:1939–1950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Isidro ML, Jorge S. Recreational drug abuse in patients hospitalized for diabetic ketosis or diabetic ketoacidosis. Acta Diabetol 2013;50:183–187 [DOI] [PubMed] [Google Scholar]
- 22.Kinney GL, Akturk HK, Taylor DD, Foster NC, Shah VN. Cannabis use is associated with increased risk for diabetic ketoacidosis in adults with type 1 diabetes: findings from the T1D Exchange clinic registry. Diabetes Care 2020;43:247–249 [DOI] [PubMed] [Google Scholar]
- 23.National Institute on Drug Abuse Nationwide Trends. [Internet], 2015. Available from https://www.drugabuse.gov/publications/drugfacts/nationwide-trends. Accessed 4 February 2020.
- 24.U.S. FDA Drug Safety Communication FDA warns that SGLT2 inhibitors for diabetes may result in a serious condition of too much acid in the blood. [Internet], 2015. Available from https://wayback.archive-it.org/7993/20170112031553/https://www.fda.gov/Drugs/DrugSafety/ucm446845.htm. Accessed 13 August 2019.
- 25.U.S. FDA Drug Safety Communication FDA revises labels of SGLT2 inhibitors for diabetes to include warnings about too much acid in the blood and serious urinary tract infections. [Internet], 2015. Available from https://wayback.archive-it.org/7993/20170112031533/https://www.fda.gov/Drugs/DrugSafety/ucm475463.htm. Accessed 13 August 2019.
- 26.Lohiya S, Kreisberg R, Lohiya V. Recurrent diabetic ketoacidosis in two community teaching hospitals. Endocr Pract 2013;19:829–833 [DOI] [PubMed] [Google Scholar]
- 27.Hua X, Carvalho N, Tew M, Huang ES, Herman WH, Clarke P. Expenditures and prices of antihyperglycemic medications in the United States: 2002-2013. JAMA 2016;315:1400–1402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cefalu WT, Dawes DE, Gavlak G, et al.; Insulin Access and Affordability Working Group . Insulin Access and Affordability Working Group: conclusions and recommendations [published correction appears in Diabetes Care 2018;41:1831] Diabetes Care 2018;41:1299–1311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Garfield SS, Xenakis JJ, Bastian A, McBride M. Experiences of people with diabetes by payer type: an analysis of the Roper Diabetes Data Set. Diabetes Ther 2015;6:113–125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Centers for Medicare & Medicaid Services. Keeping America Healthy: Cost Sharing Out of Pocket Costs [Internet], 2018. Available from https://www.medicaid.gov/medicaid/cost-sharing/out-of-pocket-costs/index.html. Accessed 14 November 2019.
- 31.Umpierrez GE. Ketosis-prone type 2 diabetes: time to revise the classification of diabetes. Diabetes Care 2006;29:2755–2757 [DOI] [PubMed] [Google Scholar]
- 32.Lebovitz HE, Banerji MA. Ketosis-prone diabetes (Flatbush diabetes): an emerging worldwide clinically important entity. Curr Diab Rep 2018;18:120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Randall L, Begovic J, Hudson M, et al. Recurrent diabetic ketoacidosis in inner-city minority patients: behavioral, socioeconomic, and psychosocial factors. Diabetes Care 2011;34:1891–1896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bradford AL, Crider CC, Xu X, Naqvi SH. Predictors of recurrent hospital admission for patients presenting with diabetic ketoacidosis and hyperglycemic hyperosmolar state. J Clin Med Res 2017;9:35–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.VanderWeele J, Pollack T, Oakes DJ, et al. Validation of data from electronic data warehouse in diabetic ketoacidosis: caution is needed. J Diabetes Complications 2018;32:650–654 [DOI] [PubMed] [Google Scholar]
- 36.Fadini GP, de Kreutzenberg SV, Rigato M, et al. Characteristics and outcomes of the hyperglycemic hyperosmolar non-ketotic syndrome in a cohort of 51 consecutive cases at a single center. Diabetes Res Clin Pract 2011;94:172–179 [DOI] [PubMed] [Google Scholar]
- 37.Pasquel FJ, Tsegka K, Wang H, et al. Clinical outcomes in patients with isolated or combined diabetic ketoacidosis and hyperosmolar hyperglycemic state: a retrospective, hospital-based cohort study. Diabetes Care 2020;43:349–357 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.