Abstract
Background:
Palliative care is a specialized approach to symptom management that focuses on supporting patients’ physical and psychological quality of life throughout the disease course. In oncology, palliative care has been increasing in utilization. The evidence base for such care is also growing through the use of randomized controlled trials (RCTs). In this review, we aim to integrate the findings from 4 meta-analyses of palliative oncology care RCTs to examine the impact of palliative care on physical and psychological quality of life and survival.
Method:
We considered 4 meta-analyses of palliative oncology care RCTs, which each used slightly different methodologies and analyses. Two of the meta-analyses included both outpatient and inpatient populations, whereas the remaining meta-analyses focused specifically on outpatient palliative oncology care.
Results:
All 4 meta-analyses reported a robust quality of life advantage for patients randomized to receive palliative care. Two meta-analyses identified a survival advantage, whereas the other 2 detected no survival differences. In 1 meta-analysis that examined high-quality RCTs of outpatient palliative oncology care, it was found that an increased survival probability for palliative care, compared with standard of care, was confined to 6- to 18-month follow-up.
Conclusions:
There is a growing evidence base for palliative oncology care, as highlighted by the 4 meta-analyses considered. Such care successfully improves both physical and psychological quality of life for patients with serious illnesses, especially cancer. Clinicians should educate patients and their caregivers about the findings of these meta-analyses. Finally, governmental policies should focus on increasing palliative care access.
Keywords: Meta-analyses, palliative care, quality of life, randomized controlled trials
Invited Review
Palliative care is an interdisciplinary health care specialty for individuals with serious illnesses focused on attending to quality-of-life concerns throughout their disease course, rather than attempting to reverse or reduce the effects of the underlying cause of the disease.1 Palliative care visits include discussions of symptom management, coping, treatment decisions, and advance care planning (see Table 1).2 Reflecting the large emphasis of palliative care in oncology, the American Society of Clinical Oncology (ASCO) has recommended its early integration, along with routine treatment, for those with advanced cancer.3 The evidence base for palliative oncology care is growing through the use of randomized controlled trials (RCTs). Using PubMed, we searched for palliative care meta and identified 975 results. After conducting a title/abstract review, we identified 4 recent meta-analyses4-7 that have considered palliative oncology RCTs in the inpatient and/or outpatient setting. Each of these papers has their own unique strengths and weaknesses to consider. In this review, we integrate the findings from these 4 meta-analyses to present the evidence base for palliative oncology care for key patient outcomes, including physical and psychological quality of life as well as survival.
Table 1.
Key primary and secondary elements of palliative care.
| Element | Emphasis |
|---|---|
| Assessment and management of symptoms | Primary |
| Coping support | Primary |
| Rapport/therapeutic relationship | Primary |
| Patient education/illness understanding | Secondary |
| Decision-making | Secondary |
| Caregiver support | Secondary |
| Advance care planning | Secondary |
| End-of-life issues | Secondary |
Impact of Palliative Oncology Care on Quality of Life
Kavalieratos et al4 published the first meta-analysis of palliative care RCTs in which they highlighted key patient outcomes. In their comprehensive study, Kavalieratos et al aimed to determine the association between palliative care and patient quality of life, symptom burden, and survival. The review considered patients diagnosed with a wide range of life-limiting illnesses, including cancer, heart failure, HIV, and multiple sclerosis, who received either inpatient or outpatient palliative care. The study sample was derived from 43 RCTs and consisted of 12 731 patients and 2479 family caregivers. Twelve of the 24 trials (50%) that considered quality of life found palliative care to be associated with statistically significant improvements in quality of life. Limited studies included in this meta-analysis also showed a potential benefit of palliative care for caregivers. However, the combined meta-analytic results were inconclusive because most RCTs considered were patient-focused. There was considerable variability in the type and delivery of targeted caregiver interventions in the RCTs assessed. In addition, in all of the RCTs that included oncology patients, palliative care receipt was found not to be significantly associated with improved cancer survival. However, this finding should be interpreted with caution because the statistical tests used to make this assessment may have been too conservative and underpowered, an issue we review in more detail later.
Soon afterward, Gaertner et al5 published another meta-analysis which examined 10 RCTs, both in the outpatient and inpatient setting, with 2454 total patients (n = 1766 or 72% with cancer). The findings of this investigation were consistent with those published in the first meta-analysis4 and suggested a health-related quality of life benefit of palliative care. Importantly, Gaertner et al also noted that palliative care may be particularly useful for oncology patients.
Impact of Palliative Oncology Care on Survival
Although the meta-analyses conducted by Kavalieratos et al4 and Gaertner et al5 were comprehensive and informative, neither study conducted analyses specific to outpatient palliative oncology care. Outpatient palliative care has seen tremendous growth over the past decade, especially in oncology, and affords greater potential benefits to patients given that it is provided much earlier in the disease course. Hoerger et al6 conducted the first meta-analysis targeting outpatient oncology RCTs. This study considered 8 RCTs with a total of 2092 patients with advanced cancer. However, the study’s main analyses focused on 1491 patients from 5 high-quality RCTs, assessed as such by meeting 2 prespecified quality criteria. These quality criteria included that the RCT contained (1) a cancer sample or subsample of ⩾100 patients and (2) randomization procedures that avoided excessive potential for confounding variables.8 The latter criterion was set in response to 2 previous studies9,10 in which unsatisfactory randomization practices resulted in patients with more aggressive cancer diagnoses being disproportionately assigned to the palliative care group.8
In that meta-analysis, Hoerger et al reported that, in the outpatient oncology setting, those patients randomly assigned to receive palliative care had better survival outcomes than those who received standard of care (SOC; see Figure 1). By the prespecified 1-year survival endpoint, 56% of palliative care patients were alive compared with only 42% of control patients (P < .001). Subsequent sensitivity analyses considered survival differences between 3 and 24 months, in quarterly intervals, and differences in survival were constrained to 6- to 18-month follow-up (see Figure 1). Presumably, during the early phases of follow-up, palliative care has not yet provided a substantial “dose” to affect survival odds, and beyond 18 months, most patients succumb to their illness regardless of the care received. In contrast to the 2 previous meta-analyses, Hoerger et al6 also conducted sensitivity analyses using Guyot et al’s11 method to develop composite Kaplan-Meier curves to assess survival differences across all the RCTs considered. From this statistical method, it was found that the median survival advantage of outpatient palliative oncology care was 4.56 months. This was derived from the palliative care group’s 14.55 months of median survival versus the control group’s 9.99 months (P = .0026).
Figure 1.
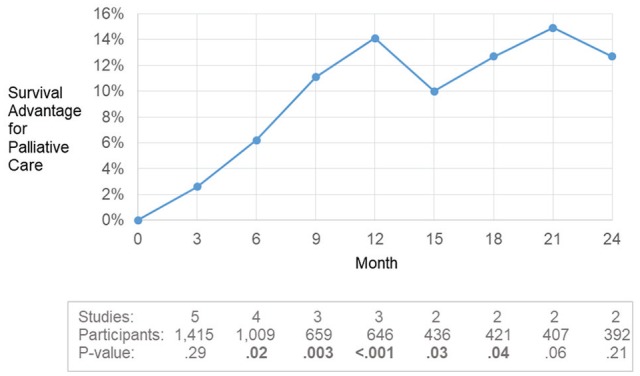
Increased survival probability for palliative care compared with usual care in the Hoerger et al6 meta-analysis of high-quality RCTs of outpatient palliative oncology care. The survival advantages were statistically significant from 6 to 18 months, including at the prespecified primary endpoint of 12 months (1 year). At earlier time points, the “dose” of palliative care may be insufficient to affect survival. At later follow-up, sample sizes were insufficient for discerning differences, and differences in survival would be expected to diminish as patients succumb to their illness regardless of care received. Clinicians are advised to note that although palliative care may extend survival duration for some patients, the primary mission of such care is to improve quality of life, and any impact on survival is in duration only, not chances of a cure.
The differences in survival between palliative care and control patients noted in the Hoerger et al article conflict with the meta-analytic findings of Kavalieratos et al. These divergent findings could be a result of the studies’ different foci. Although Kavalieratos et al conducted a broader, more comprehensive meta-analysis, which contained both inpatient and outpatient setting RCTs and patients with a variety of serious illnesses, Hoerger et al specifically targeted high-quality outpatient palliative oncology care RCTs. This is salient because it has been noted that inpatient palliative care populations tend to have a short average survival duration.12 Therefore, to document a discernable survival advantage in an inpatient RCT, it would require thousands of oncology patients and the effect would likely be small.
As noted previously, the Kavalieratos et al study was potentially too analytically conservative as the statistical procedures they used violated analytical assumptions, weakening observed effects. That study relied on the hazard ratio statistic, which assumes that relative differences in survival are comparable across the follow-up period. For example, if the relative risk of death is 10% more favorable at 3 months, it should be 10% more favorable at 6, 9, 12 months, and so forth. Such an assumption is often met in pharmaceutical trials, where the pharmacokinetics or biologic impact of treatment is felt almost immediately. No such assumption can be made regarding palliative care, as even in care settings with the most resources, patients only receive palliative care visits on an approximately monthly basis,2,6 meaning it could take several months to have any plausible biologic impact on survival. Moreover, although palliative care could delay death in some cases, no palliative care clinician could argue that it is curative, and the long-term convergence in survival (at 18-21 months of follow-up) mitigates the power of the hazard ratio to test survival differences. In such circumstances, where the hazard ratio is inappropriate, researchers should compare differences at prespecified time points (eg, 1 year) or examine differences in survival duration.
An additional reason for the lack of finding in the Kavalieratos et al meta-analysis was that they also gave the greatest statistical weight to larger studies, a common practice, but failed to exclude the largest study,9 which had fatal randomization issues. This large study was eliminated in the Hoerger et al analysis based on prespecified quality standards. Hoerger et al also used time-based parameters, including median and overall survival at 1 year, which are more powerful than the hazard ratios used in the Kavalieratos et al meta-analysis.
In their investigation, Hoerger et al also affirmed the Kavalieratos et al and Gaertner et al meta-analytic findings of a quality of life benefit associated with palliative care receipt (P < .001). Building off these findings, Hoerger et al conducted secondary analyses of physical (P = .006) and psychological (P = .001) outcomes and determined separate palliative care advantages for both.
Finally, Fulton et al7 published their meta-analysis of outpatient palliative oncology care RCTs which replicated the findings of Hoerger et al. This study considered 9 RCTs and thus 1 additional study that was not analyzed in the Hoerger et al article because the palliative care clinician did not provide care using an interdisciplinary team in accordance with the clinical practice guidelines set by the National Consensus Project for Quality Palliative Care. Importantly, Fulton et al, using a different research methodology and analytic approach, reiterated the findings of an outpatient palliative oncology care survival benefit first noted by Hoerger et al. Interestingly, the study did use hazard ratios to examine survival differences, and although we criticized this approach previously, it is noteworthy that they replicated the survival advantage even when using an approach that was statistically conservative. The findings of the 4 aforementioned meta-analyses4-7 are summarized in Table 2.
Table 2.
Summary of meta-analyses of palliative oncology care RCTs.
| Meta-analysis | Total number of patients | No. of RCTs | PC setting | PC quality of life advantage? | PC survival advantage? |
|---|---|---|---|---|---|
| Kavalieratos et al4 | 12 731 | 43 | Inpatient and outpatient | Yes | No |
| Gaertner et al5 | 2454 | 10 | Inpatient and outpatient | Yes | No |
| Hoerger et al6 | 2092 | 8 | Outpatient | Yes | Yes |
| Fulton et al7 | 1487 | 9 | Outpatient | Yes | Yes |
Abbreviations: PC, palliative care; RCTs, randomized controlled trials.
Discussion
Implications for outpatient palliative oncology care
The finding of an outpatient palliative oncology care survival benefit noted in the Hoerger et al and Fulton et al studies provides an important area for additional investigation. It will be critical to determine how, mechanistically, certain palliative care aspects improve patient outcomes, including quality of life and overall survival. Two recent studies provide 1 potential mechanism for the palliative care associated survival benefit. Basch et al13 and Denis et al14 found that symptom monitoring in cancer was associated with increased survival time. Basch et al13 compared members of a patient-reported outcomes (PRO) group with those in SOC and found a survival difference of 5 months (P = .03). The PRO group’s median overall survival was 31.2 months (95% confidence interval [CI] = 24.5-39.6), whereas the SOC group’s median overall survival was only 26.0 months (95% CI = 22.1-30.9). In the latter study, Denis et al14 used a web-mediated follow-up algorithm that considered patient-reported symptoms. The authors noted improved overall survival in the experimental arm compared with the control arm. Future studies should focus on other key elements of palliative care (see Table 1) that may affect survival. These may include reductions in high grade toxicities, improved pulmonary functioning, reduced substance use, improved medicinal management and exercise frequency, or changes in the timing of chemotherapy administration.
Disseminating critical findings, expanding palliative care programs, and training future palliative care specialists
After considering the 4 meta-analyses on palliative oncology care,4-7 the benefits for patient quality of life and survival are clear. Moving forward, disseminating these research findings will be critical to improve the lives of cancer patients and, more generally, public health. The Hoerger et al group developed a nonproprietary meta-analysis dissemination website (www.pallonc.com) to improve public awareness of palliative care’s efficacy. It is important to note, however, that the findings of these 4 studies must be generalized with caution. Overgeneralizing the quality of life and survival advantages of palliative oncology care to other forms of care, such as hospice, and patient populations, such as noncancer patients, may potentially be misguided. Patients must be made aware of the various strengths and limitations of germane clinical research. Importantly, since palliative care is focused on symptom management, patients should not be misled with unrealistic notions of any curative ability of such care.
As studies and reviews continue to highlight the importance of symptom management and discussing coping and decision-making to improve patient outcomes, palliative care programs are growing and expanding throughout the United States, Canada, Europe, and Australia. The aforementioned meta-analytic findings are contributing to this expansion of palliative care.15 Research has also generated evidence-based recommendations to advocate for palliative care in states that have been considered “low-access” by the Center to Advance Palliative Care (CAPC).16 Some of the key methods that have been outlined to do so are based on personality theory and include (1) explaining the research evidence base of palliative care; (2) relating palliative care to traditional services, such as pain and symptom management; and (3) describing the key elements of palliative care in concrete terms.
As the evidence-based nature of palliative care continues to grow rapidly and the approach gains public popularity, there is also a need to address the shortage of specialized palliative care clinicians. Innovative training programs have been developed to increase the number of physicians and nurses in the specialty/subspecialty. Efforts should also be made to expose undergraduate and graduate students to the specialty early in their career development. In addition, there is a considerable shortage of specialized palliative care professionals in other disciplines, such as pharmacy, respiratory therapy, physical therapy, and psychology. Paradoxically, most psychology trainees do not gain exposure to palliative care until late in their training, despite the clear benefit they could provide in patient and caregiver coping, symptom assessment and management, care planning, and advancing high-quality palliative care research.
Conclusions
Hypothesis-driven research and high-quality RCTs have provided a growing evidence base for palliative oncology care. The 4 meta-analyses that were considered in this review4-7 provide evidence that palliative care successfully improves both physical and psychological quality of life for patients with serious illnesses, including cancer. Two of the meta-analyses that focused specifically on outpatient palliative oncology care provided congruent accounts that implicate palliative care with a small, but noteworthy, benefit for survival duration. These preliminary findings must be refined via mechanistic studies. Importantly, clinicians should educate their patients and their caregivers about the findings of these meta-analyses. Administrators and policymakers should also work to improve access to palliative care programs.
Footnotes
Funding:The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institute of General Medical Sciences (U54GM104940) and the Louisiana Board of Regents (LEQSF(2016-19)-RD-A-18).
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: JLR was responsible for data analyses, interpretation of results, manuscript preparation, and approval of the final manuscript. LMP was responsible for interpretation of results, manuscript preparation, and approval of the final manuscript. MH was responsible for conception, design, data analyses, interpretation of results, manuscript preparation, and approval of the final manuscript.
ORCID iD: Michael Hoerger  https://orcid.org/0000-0002-4398-2820
https://orcid.org/0000-0002-4398-2820
References
- 1. Shalev A, Phongtankuel V, Kozlov E, Shen MJ, Adelman RD, Reid M. Awareness and misperceptions of hospice and palliative care: a population-based survey study. Am J Hosp Palliat Care. 2018;35:431-439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hoerger M, Greer JA, Jackson VA, et al. Defining the elements of early palliative care that are associated with patient-reported outcomes and the delivery of end-of-life care. J Clin Oncol. 2018;36:1096-1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ferrell BR, Temel JS, Temin S, et al. Integration of palliative care into standard oncology care: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2017;35:96-112. [DOI] [PubMed] [Google Scholar]
- 4. Kavalieratos D, Corbelli J, Zhang D, et al. Association between palliative care and patient and caregiver outcomes: a systematic review and meta-analysis. JAMA. 2016;316:2104-2114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gaertner J, Siemens W, Meerpohl JJ, et al. Effect of specialist palliative care services on quality of life in adults with advanced incurable illness in hospital, hospice, or community settings: systematic review and meta-analysis. BMJ. 2017;357:j2925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hoerger M, Wayser GR, Schwing G, Suzuki A, Perry LM. Impact of interdisciplinary outpatient specialty palliative care on survival and quality of life in adults with advanced cancer: a meta-analysis of randomized controlled trials. Ann Behav Med. 2019;53:674-685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fulton JJ, LeBlanc TW, Cutson TM, et al. Integrated outpatient palliative care for patients with advanced cancer: a systematic review and meta-analysis. Palliat Med. 2019;33:123-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hoerger M. Randomization failure in palliative care RCTs. Palliat Med. 2018;32:533-534. [DOI] [PubMed] [Google Scholar]
- 9. Jordhøy MS, Fayers P, Loge JH, Ahlner-Elmqvist M, Kaasa S. Quality of life in palliative cancer care: results from a cluster randomized trial. J Clin Oncol. 2001;19:3884-3894. [DOI] [PubMed] [Google Scholar]
- 10. McCorkle R, Jeon S, Ercolano E, et al. An advanced practice nurse coordinated multidisciplinary intervention for patients with late-stage cancer: a cluster randomized trial. J Palliat Med. 2015;18:962-969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Guyot P, Ades A, Ouwens MJ, Welton NJ. Enhanced secondary analysis of survival data: reconstructing the data from published Kaplan-Meier survival curves. BMC Med Res Methodol. 2012;12:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hui D, Elsayem A, Palla S, et al. Discharge outcomes and survival of patients with advanced cancer admitted to an acute palliative care unit at a comprehensive cancer center. J Palliat Med. 2010;13:49-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Basch E, Deal AM, Dueck AC, et al. Overall survival results of a trial assessing patient-reported outcomes for symptom monitoring during routine cancer treatment. JAMA. 2017;318:197-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Denis F, Lethrosne C, Pourel N, et al. Randomized trial comparing a web-mediated follow-up with routine surveillance in lung cancer patients. J Natl Cancer I. 2017;109:436-448. [DOI] [PubMed] [Google Scholar]
- 15. Center to Advance Palliative Care and the National Palliative Care Research Center. America’s Care of Serious Illness: A State-by-State Report Card on Access to Palliative Care in Our Nation’s Hospitals. New York, NY: Center to Advance Palliative Care and the National Palliative Care Research Center; 2019. [Google Scholar]
- 16. Hoerger M, Perry LM, Korotkin BD, et al. Statewide differences in personality associated with geographic disparities in access to palliative care: findings on openness. J Palliat Med. 2019;22:628-634. [DOI] [PMC free article] [PubMed] [Google Scholar]


