Abstract
Background:
While Achilles tendon repairs are common, little data exist characterizing the cost drivers of this surgery.
Purpose:
To examine cases of primary Achilles tendon repair, primary repair with graft, and secondary repair to find patient characteristics and surgical variables that significantly drive costs.
Study Design:
Economic and decision analysis; Level of evidence, 3.
Methods:
A total of 5955 repairs from 6 states were pulled from the 2014 State Ambulatory Surgery and Services Database under the Current Procedural Terminology codes 27650, 27652, and 27654. Cases were analyzed under univariate analysis to select the key variables driving cost. Variables deemed close to significance (P < .10) were then examined under generalized linear models (GLMs) and evaluated for statistical significance (P < .05).
Results:
The average cost was $14,951 for primary repair, $23,861 for primary repair with graft, and $20,115 for secondary repair (P < .001). In the GLMs, high-volume ambulatory surgical centers (ASCs) showed a cost savings of $16,987 and $2854 in both the primary with graft and secondary repair groups, respectively (both P < .001). However, for primary repairs, high-volume ASCs had $2264 more in costs than low-volume ASCs (P < .001). In addition, privately owned ASCs showed cost savings compared with hospital-owned ASCs for both primary Achilles repair ($2450; P < .001) and primary repair with graft ($11,072; P = .019). Time in the operating room was also a significant cost, with each minute adding $36 of cost in primary repair and $31 in secondary repair (both P < .001).
Conclusion:
Private ASCs are associated with lower costs for patients undergoing primary Achilles repair, both with and without a graft. Patients undergoing the more complex secondary and primary with graft Achilles repairs had lower costs in facilities with greater caseload.
Keywords: Achilles tendon repair, cost drivers, economic analysis
Achilles tendon tears are becoming increasingly common in both athletes and the general population; 1 study10 cited an increase in incidence from 2.1 per 100,000 person-years in 1979 to 21.5 per 100,000 person-years in 2011. Multiple meta-analyses and recommendations suggest that these tears can be managed operatively or nonoperatively, depending on many complex variables such as patient demand, type of athlete, and time of season, all with relatively similar efficacy.9,14,16,21,23,25 While operative versus nonoperative treatment remains a personal provider-patient decision, understanding the economics at play may help both providers and patients with decision making. Therefore, understanding the characteristics and surgical factors associated with increased operative costs can aid both surgeons and patients.
Increased bundled care and set-price reimbursements have encouraged health care providers to find ways to efficiently reduce costs while maintaining quality. The data of the State Ambulatory Surgery and Services Databases (SASD) can be obtained to help characterize the patients undergoing Achilles tendon surgery. Two previous studies22,23 have shown that surgical management of Achilles tendon repair is more expensive than nonsurgical management. However, although the study by Westin et al23 analyzed the contributors to the overall cost of Achilles tendon injury, no study has been performed characterizing the patient- and surgeon-specific cost drivers of Achilles tendon repairs. In addition, a study about arthroscopic rotator cuff repair12 characterized high-volume surgeons as a key group reducing the costs; yet, similar trends have not been elucidated for Achilles tendon repair. In this study, we sought to characterize how factors such as patient and surgical characteristics were associated with costs in order to provide information on how cost savings may be achieved. We hypothesized that ambulatory surgical centers (ASCs) with a larger caseload would provide cost reductions over ASCs with fewer annual cases. We also hypothesized that private ASCs would provide cost reductions when compared with hospital-associated surgical centers.
Methods
Data Source
The data source for this study was the 2014 SASD, a part of the Healthcare Cost and Utilization Project. These databases, sponsored by the Agency for Healthcare Research and Quality, are a reliable encounter-level measure of outpatient procedures performed in ASCs. Data from 6 states representative of the diversity of the United States were used for this study: Florida, Kentucky, Iowa, Maryland, Nevada, and New York. This geographic selection has been previously validated in the cost analyses of other orthopaedic procedures.2,13
Data Collection
Cases with Current Procedural Terminology (CPT) codes 27650 (primary repair, open or percutaneous, and ruptured Achilles tendon), 27652 (primary repair with graft, open or percutaneous, and ruptured Achilles tendon), and 27654 (secondary repair, with or without graft, and ruptured Achilles tendon) were selected from the SASD. Primary repair was defined as repair completed within 2 weeks of an acute injury, whereas secondary repair involved repair of either a chronic condition or a recurrent acute injury or repair 2 weeks or more after injury. These definitions are up to provider discretion. Some providers may also use the secondary repair CPT code for debridement and repair of insertional tendinopathy.
Two categories of variables were analyzed: patient characteristics (patient sex, race, age, income quartile of patient’s zip code, presence of at least 1 medical comorbidity, and insurance) and surgical characteristics (type of anesthesia, postoperative admission to hospital, ASC ownership, surgeon volume, and ASC volume). Surgeon and ASC volumes were separated into high- and low-volume groups. The cutoffs for these groups were selected using the median caseload across the 3 surgical groups; median surgeon volume was 6 cases per year and median ASC volume was 15 cases per year. It should be noted that of the states studied, only New York includes data for operative time.
The primary outcome variable in this study was total charges billed for the case. This was used as a proxy measure for the cost of the procedure, an approach that has been validated in several recent studies of orthopaedic procedures.2,12,13 Total charges data reveal the cost-varying trends between different groups and surgical approaches. These trends may be useful in identifying the areas where cost savings can be achieved.
Statistical Analysis
Cases were first separated into 3 groups: primary repairs (CPT 27650), primary repairs with a graft (CPT 27652), and secondary repairs (CPT 27654). Univariate analysis of patient- and surgeon-specific cost drivers was performed to identify variables that were significantly associated with cost. Single linear regression, independent-samples t testing, and 1-way analysis of variance were used, where appropriate. These variables were then included in 3 generalized linear models (GLMs) to model the total cost of surgery while accounting for all significant factors. For the univariate analysis, a relaxed P value of .10 was used as the cutoff point for inclusion into the GLM. Values with P < .05 were considered statistically significant (SPSS Statistics v 25.0, IBM Corporation).
Results
A total of 4333 primary repairs, 549 primary repairs with graft, and 1073 secondary cases were included (total: 5955). Male patients comprised 63.3% of the sample. The average charge billed across all cases was $16,703 (Appendix Table A1). Primary surgeries averaged $14,951, surgeries with grafts averaged $23,861, and secondary surgeries averaged $20,115 (P < .001).
Univariate Analysis
Age and time in the operating room (OR) were often significant predictors of cost under univariate linear regression (Appendix Table A2). For age, each additional year added $116 for primary cases (P < .001), $167 for graft cases (P = .002), and $102 for secondary cases (P = .005). Each additional minute in the OR for primary surgeries was associated with an added $73 for primary surgeries (P < .001) and $37 for secondary surgeries (P < .001). Time in the OR was not statistically significant for primary surgeries with a graft (P = .097), although the P value met our relaxed cutoff for inclusion into the GLM.
Several patient-specific variables were associated with higher costs under univariate analysis (Appendix Table A3). In the primary repair group, female patients had 22% higher costs than male patients (P < .001). Patient sex was not significant for the graft repair or secondary repair group. Race was a significant factor in the primary repair and secondary repair groups but was not significant for patients undergoing repair with a graft. Hispanic patients had 14% higher costs than white patients in the primary repair group (P < .001) and 19% higher costs in the secondary repair group (P < .001). For the 3 groups under univariate analysis, patients living in 4th quartile (high-income) zip codes had lower costs than patients living in 1st quartile (low-income) zip codes. Costs for patients in high-income zip codes were 30% lower in the primary repair group (P < .001), 36% lower in the graft repair group (P < .001), and 34% lower in the secondary repair group (P < .001). In addition, the presence of at least 1 comorbidity significantly increased the costs across all 3 surgical groups. Comorbid patients had 23% higher costs in the primary repair group (P < .001), 26% higher costs in the graft repair group (P < .001), and 25% higher costs in the secondary repair group (P < .001). Finally, Medicare insurance was associated with higher costs for patients in the primary repair and secondary repair groups. Compared with patients with private insurance, patients with Medicare had 30% higher costs in the primary repair group (P < .001) and 16% higher costs in the secondary repair group (P < .001).
Several surgical variables were also associated with increased costs under univariate analysis (Appendix Table A4). For patients undergoing primary repair, general anesthesia plus a nerve block added 7% more cost than general anesthesia alone (P = .011). Anesthesia was not a significant factor for patients undergoing repair with a graft or for secondary repair. Postoperative admission to the hospital significantly increased the costs across all 3 groups. Patients admitted to the hospital had 46% higher costs for primary repairs (P < .001), 92% higher costs for repairs with a graft (P < .001), and 75% higher costs for secondary repairs (P < .001). Patients undergoing surgery at a privately owned ASC had lower costs in 2 of the 3 surgical groups. Private ASCs had 23% lower costs for primary repairs (P < .001) and 25% lower costs for repairs with a graft (P = .044). Costs were not significantly lower based on ASC ownership for secondary repairs (P = .059), but the P value met the relaxed cutoff for inclusion into the GLM. High-volume surgeons had 18% lower costs when performing a repair with a graft (P = .012). Surgeon volume did not affect costs in either the primary repair or secondary repair groups. High-volume ASCs had lower costs across the 3 surgical groups. Cases performed at a high-volume ASC had 14% lower costs for primary repairs (P < .001), 20% lower costs for repairs with a graft (P = .001), and 10% lower costs for secondary repairs (P = .021).
Generalized Linear Models
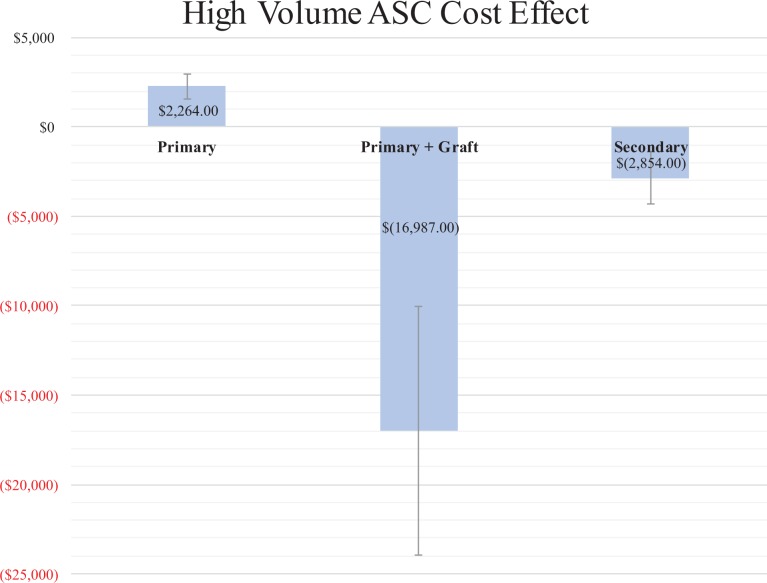
The GLMs revealed which variables that were significant under univariate analysis held significance when controlling for other factors. Several surgical variables were associated with cost. Across the 3 GLMs, surgical center volume significantly affected costs (Figure 1). For primary repairs (Table 1), high-volume ASCs had $2264 more in costs than low-volume ASCs (P < .001). This trend was reversed in repairs using grafts (Table 2) and in secondary repairs (Table 3), where high-volume ASCs had $16,987 and $2854 lower costs, respectively (both P < .001). Privately owned ASCs had lower costs for both primary repairs and repairs with grafts (Figure 2). In the primary repair group, privately owned ASCs had $2450 lower costs than hospital-owned ASCs (P < .001). In the graft repair group, private ownership conveyed a savings of $11,072 (P = .019). Increasing time in the OR also added cost in the primary repair and secondary repair groups. Each additional minute in the OR added $36 for primary repairs (P < .001) and $31 for secondary repairs (P < .001). Finally, postoperative hospital admission added $40,069 (P < .001) in costs for patients undergoing repairs with a graft.
Figure 1.
Cost reductions of high- versus low-facility volume ASCs (cutoff, n = 15 cases) in generalized linear models. For primary repairs using grafts and for secondary repairs, high-volume ASCs had lower costs than low-volume ASCs. ASC, ambulatory surgical center.
Table 1.
Generalized Linear Model—Primary Achilles Tendon Repaira
| Variable | Variable Group | β (2014 USD) | SE | 95% Wald CI | P | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Intercept | $3613 | $1243 | $1176 | $6050 | .004 | |
| Surgical center volume | High-volume ASC | $2264 | $371 | $1536 | $2991 | <.001 |
| Low-volume ASC | 0 | |||||
| Surgical center ownership | Privately owned ASC | $(2450) | $477 | $(3384) | $(1515) | <.001 |
| Hospital-owned ASC | 0 | |||||
| Comorbidity | Presence of comorbidity | $1194 | $398 | $413 | $1975 | .003 |
| No comorbidity | 0 | |||||
| Income quartile of patient’s zip code | 4th (Highest) | $2007 | $576 | $878 | $3135 | <.001 |
| 3rd | $(177) | $622 | $(1396) | $1042 | .776 | |
| 2nd | $(22) | $648 | $(1293) | $1248 | .973 | |
| 1st (Lowest) | 0 | |||||
| Race | Other | $1628 | $498 | $651 | $2604 | .001 |
| Native American | $(567) | $2304 | $(5082) | $3947 | .805 | |
| Asian | $1758 | $1031 | $(263) | $3778 | .088 | |
| Hispanic | $1669 | $723 | $251 | $3087 | .021 | |
| Black | $1382 | $490 | $422 | $2342 | .005 | |
| White | 0 | |||||
| Sex | Female | $934 | $387 | $175 | $1693 | .016 |
| Male | 0 | |||||
| Continuous variables | Age | $35 | $15 | $6 | $64 | .019 |
| Operative time | $36 | $4 | $29 | $43 | <.001 | |
aSignificant effects are bolded. Variables included but that were not significant: hospital readmission, insurance, and anesthesia. Parentheses indicate negative values. β corresponds to the cost added by the variable. ASC, ambulatory surgical center; USD, United States dollars.
Table 2.
Generalized Linear Model—Primary Achilles Tendon Repair With Grafta
| Variable | Variable Group | β (2014 USD) | SE | 95% Wald CI | P | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Intercept | $24,681 | $7036 | $10,890 | $38,471 | <.001 | |
| Admitted to hospital postoperatively | Admitted | $40,069 | $5264 | $29,752 | $50,387 | <.001 |
| Not admitted | 0 | |||||
| Surgical center ownership | Privately owned ASC | $(11,072) | $4726 | $(20,335) | $(1809) | .019 |
| Hospital-owned ASC | 0 | |||||
| Surgical center volume | High-volume ASC | $(16,987) | $3555 | $(23,954) | $(10,020) | <.001 |
| Low-volume ASC | 0 | |||||
| Age | $226 | $101 | $29 | $424 | .025 | |
aSignificant effects are bolded. Variables included but that were not significant: patient income, comorbidity, and surgeon volume. Parentheses indicate negative values. β corresponds to the cost added by the variable. ASC, ambulatory surgical center; USD, United States dollars.
Table 3.
Generalized Linear Model—Secondary Achilles Tendon Repairsa
| Variable | Variable Group | β (2014 USD) (SE) | SE | 95% Wald CI | P | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Intercept | $6136 | $2693 | $858 | $11,415 | .023 | |
| Race | Other | $(1423) | $944 | $(3274) | $427 | .132 |
| Native American | $(7279) | $3994 | $(15,107) | $548 | .068 | |
| Asian | $1308 | $3249 | $(5060) | $7675 | .687 | |
| Hispanic | $237 | $1398 | $(2503) | $2978 | .865 | |
| Black | $2720 | $1275 | $221 | $5219 | .033 | |
| White | 0 | |||||
| Income quartile of patient’s zip code | 4th (Highest) | $3370 | $1244 | $932 | $5807 | .007 |
| 3rd | $983 | $1351 | $(1666) | $3631 | .467 | |
| 2nd | $646 | $1414 | $(2126) | $3418 | .648 | |
| 1st (Lowest) | 0 | |||||
| Surgical center volume | High-volume ASC | $(2854) | $758 | $(4341) | $(1368) | <.001 |
| Low-volume ASC | 0 | |||||
| Time in OR | $31 | $7 | $18 | $45 | <.001 | |
aSignificant effects are bolded. Variables included but that were not significant: patient insurance, comorbidity, age, postoperative hospital admission, and surgical facility ownership. Parentheses indicate negative values. β corresponds to the cost added by the variable. ASC, ambulatory surgical center; OR, operating room; USD, United States dollars.
Figure 2.
Cost reductions of privately versus hospital-owned ASCs in generalized linear models. For primary repairs with or without a graft, privately owned ASCs had lower costs than hospital-owned ASCs. ASC, ambulatory surgical center.
Several patient characteristic variables were associated with increased cost in the GLMs. In the primary and secondary repair groups, black patients had $1382 (P = .005) and $2720 (P = .033) higher costs than white patients, respectively. Hispanic patients and patients of other race also had higher costs in the primary repair group. The trend of lower costs in higher income zip code groups reversed from univariate to GLM analysis. Multivariate analysis showed that patients living in the zip codes of the highest income quartile also had greater costs in the primary and secondary repair groups. Living in these zip codes added $2007 for primary repairs (P < .001) and $3370 for secondary repairs (P = .007). Older patients also tended to have higher costs; each additional year of age added $35 for patients undergoing primary repair (P = .019) and $226 for patients undergoing repair with a graft (P = .025). Female patients undergoing primary repair had $934 more in costs than male patients (P = .016). Finally, patients with 1 or more comorbidity had $1194 higher costs than noncomorbid patients in the primary repair group (P = .003).
Discussion
With health care costs receiving constant scrutiny in the public eye, health care providers and patients should both be aware of the costs of surgery. In this study, the cost drivers of the 3 types of Achilles tendon repair were compared using a large and geographically representative database. Univariate cost drivers were first analyzed, and significant variables were included in GLMs. These GLMs showed that for more complex surgical cases, high-volume ASCs had substantially lower costs than their lower volume counterparts. Privately owned ASCs also showed substantially lower costs in 2 of the 3 groups. In addition, several patient characteristic factors, including race, age, and sex, were significant cost drivers under the GLM, which matched results from similar studies.2,13
Our results demonstrate that high-volume ASCs deliver lower costs to patients undergoing the more complex repairs with a graft and secondary repairs. Primary repair with a graft requires experience in graft harvesting if an autograft is used or experience in graft preparation for allograft or synthetic graft repairs. In secondary repair of subacute or chronic injuries, the increased amount of scar tissue and degeneration of the tendon stumps may require additional surgical skills to repair effectively. There may also be more tendon retraction in chronic tendon tears. Additionally, repairs of insertional tendinopathy typically require the use of suture anchors and may require removal of a Haglund deformity.20 The results of this study suggest that the increased complexity of these repairs favors higher volume surgical centers that may be more experienced in these procedures. Even when controlling for operative time, comorbidity level, and hospital admission, high-volume ASCs delivered a savings of $16,987 (P < .001) for graft repairs and a savings of $2854 (P < .001) for secondary repairs when compared with their lower volume counterparts. Previous studies6,7,17 of similar orthopaedic procedures have also shown that high-volume facilities provide better outcomes and reduced risk of mortality. The data from this study suggest that directing more complicated graft repairs and secondary repairs to high-volume ASCs may provide cost benefits to both the facility and the patient.
In addition, it should be noted that high-volume ASCs delivered cost savings for all 3 procedure types in the univariate analysis, but in the GLM, costs were increased for patients undergoing primary repair at a high-volume ASC. It was unclear what factor is being controlled for in the GLM that caused this reversal. Nevertheless, these data demonstrate that straightforward primary repairs may not ultimately require treatment at a high-volume center. However, more complicated repairs can be performed at a lower cost in higher volume, more specialized settings. Directing patients with subacute or chronic Achilles tears to high-volume centers may provide a means for patients and payers to achieve cost reductions.
Our results also show that private ownership of the surgical center conveys cost savings. In the GLM, privately owned ASCs conferred a cost reduction for primary repairs of $2450 compared with their hospital-owned counterparts (P < .001). For primary repairs with a graft, private ownership was associated with a cost savings of $11,072 (P = .019). We hypothesize that private ASCs may be better equipped to provide orthopaedic-specific teams with greater knowledge of the tools and techniques being used. A previous study of anterior cruciate ligament reconstruction (ACLR)18 found greater procedural efficiency at private ASCs compared with their hospital counterparts. A study of supracondylar humeral fractures19 found that surgeries performed at a physician-owned ASC were more efficient and more cost-effective than surgeries performed at a hospital outpatient department. Similarly, in a study of posterior lumbar fusion,15 it was found that private ownership of the hospital not only provided lower costs, but also reduced risk of postoperative complications. As with high-volume ASCs, privately owned ASCs can be more specialized and orthopaedic specific compared with hospital-owned ASCs. Achilles tendon repairs directed to privately owned ASCs may provide an avenue to reduce costs for patients and surgeons.
In both primary and secondary tendon repairs, operative time was a significant cost driver. Each additional minute added $36 for primary repairs (P < .001) and $31 for secondary repairs (P < .001). These numbers are on par with the results of a study that found an OR cost of $36 per minute for ambulatory surgeries.3 Clearly, reducing time in the OR has the potential to significantly reduce costs. Surgeons ought to be aware of their time efficiency when performing primary and secondary Achilles tendon repairs.
Several characteristic factors were associated with increased costs in the GLMs. Patients with comorbidities face $1194 higher costs for primary repairs (P < .001). Surgery and postoperative management on these patients may be more complicated. Dombrowski et al5 recently demonstrated that comorbid patients are at greater risk of surgical site infection, a factor that can increase costs.
The GLMs also showed that for both primary and secondary repairs, black patients had higher costs than white patients. Hispanic patients and patients of other race also had higher costs in the primary repair group. Hispanic patients have previously been reported to experience higher costs for ACLR.2 Black patients have been shown to experience higher rates of Achilles tendon rupture.11 It is unclear why these groups are subject to higher costs of repair. This study did not include data on mechanism of injury or injury severity, both of which may play a role. Older patients also had higher costs for primary repairs and primary repairs with grafts. Although we did not have data on perioperative time, it is possible that older individuals require greater preoperative preparation or more time in the postanesthesia care unit. This finding is significant, as the mean age of patients who experience Achilles tendon rupture has been increasing8; this may be one contributor to increasing costs. Finally, there was an association between high income and higher costs in multivariate analysis. Patients living in high-income zip codes had significantly higher costs than any other income quartile for primary and secondary repairs, the opposite of the trend shown in univariate analysis. This is likely because of confounding variables being controlled in the GLM. Patient insurance was included in both analyses and was found to be nonsignificant, so it is unclear what other confounding factor high-income patients may have that leads to increased costs.
Limitations
This study used GLMs to help mitigate the influence of confounding variables. However, there are still several inherent limitations. The smaller sample size and larger standard deviation in the cost of the primary-with-graft group led to large confidence intervals in the GLM; the model thus may be more useful for showing directionality in trends rather than a truly accurate cost model. The SASD is a claims-based database; so there may be misclassified cases or miscoding of collected data elements. This may be especially apparent because of the confusion between primary and secondary repairs, which may lead to misclassified repairs. We also were unable to determine which cases coded as secondary repair were for repair of insertional tendinopathy versus subacute ruptures. There may also be factors that significantly affect the cost of surgery that are not captured in the SASD, both surgical and characteristic. In addition, there may also be a gap in coding versus clinical practice; for example, some surgeons may not bill for every medication administered during and after each case. The total charge billed was used as a proxy for the true cost, but charges may vary, as reimbursement depends on contracts between providers and insurers. To mitigate the effects of contract variation, we included patient insurance in the GLMs when it was significant under univariate analysis. In addition, we used a large and geographically diverse sample to reduce the effects of different billing practices. The total charges also did not include ancillary costs such as physical therapy or out-of-work status.
Despite these limitations, the methodology used in this study has been demonstrated to be useful in several previous orthopaedic studies.1,2,4,12,13,24 The goal of this study was to analyze how surgeon- and patient-specific factors are associated with cost, and further studies may aim to delve deeper into the trends identified. Although there are limitations inherent in this analysis, the trends identified can prove useful to surgeons and patients alike.
Conclusion
Privately owned surgery centers deliver cost savings to patients undergoing both primary Achilles tendon repair and primary repair with a graft. For the more complex primary repair with a graft and for secondary repairs, high-volume surgery centers provide lower costs. Increasing age and longer operative times both increase costs. Additionally, both black race and high income are associated with higher costs for primary and secondary repairs. To achieve a cost savings to the health care system, patients requiring more complex operative treatment of an Achilles tendon rupture may be directed to surgical centers with higher caseloads.
Appendix
Table A1.
Average Cost by Case Type
| Procedure | N | Mean Cost (SD) | P |
|---|---|---|---|
| Primary surgery | 4333 | $14,951 ($11,408) | <.001 |
| Surgery with graft | 549 | $23,861 ($17,832) | |
| Secondary surgery | 1073 | $20,115 ($15,107) | |
| Total | 5955 | $16,703 ($13,195) |
Table A2.
Analysis of Age and Time in ORa
| Age | |||
|---|---|---|---|
| Group | Constant (SE) | β Value (SE) | P |
| Primary | $9545 ($585) | $116 ($12) | <.001 |
| With graft | $15,636 ($2769) | $167 ($53) | .002 |
| Secondary | $14,761 ($1945) | $102 ($36) | .005 |
| Time in OR | |||
| Group | Constant (SE) | β Value (SE) | P |
| Primary | $7800 ($592) | $73 ($5) | <.001 |
| With graft | $12,285 ($1712) | $20 ($12) | .097 |
| Secondary | $8168 ($798) | $37 ($7) | <.001 |
aOR, operating room.
Table A3.
Univariate Analysis of Patient Characteristic Factors
| Sex | ||||
|---|---|---|---|---|
| Group | Variable | N | Mean (SD) | P |
| Primary | Male | 2925 | $13,967 ($10,726) | <.001 |
| Female | 1415 | $17,013 ($12,453) | ||
| With graft | Male | 351 | $23,696 ($19,176) | .574 |
| Female | 200 | $24,598 ($15,943) | ||
| Secondary | Male | 496 | $20,137 ($15,539) | .964 |
| Female | 577 | $20,095 ($14,739) | ||
| Race | ||||
| Group | Variable | N | Mean (SD) | P |
| Primary | White | 2699 | $15,786 ($12,039) | <.001a |
| Black | 751 | $13,455 ($10,023) | ||
| Hispanic | 291 | $17,987 ($11,588) | ||
| Asian | 74 | $13,798 ($8500) | ||
| Native American | 22 | $11,120 ($4466) | ||
| Other | 323 | $12,416 ($9331) | ||
| With graft | White | 342 | $24,620 ($18,372) | .184 |
| Black | 98 | $22,401 ($17,626) | ||
| Hispanic | 58 | $28,057 ($18,638) | ||
| Asian | 13 | $16,705 ($11,161) | ||
| Other | 21 | $22,069 ($19,498) | ||
| Secondary | White | 773 | $20,513 ($15,077) | <.001a |
| Black | 107 | $19,107 ($14,629) | ||
| Hispanic | 82 | $24,406 ($17,273) | ||
| Asian | 8 | $28,996 ($21,279) | ||
| Native American | 3 | $9550 ($5456) | ||
| Other | 57 | $12,829 ($13,399) | ||
| Income quartile of patient’s zip code | ||||
| Group | Variable | N | Mean (SD) | P |
| Primary | 1 | 766 | $17,451 ($13,232) | <.001b |
| 2 | 1036 | $17,180 ($13,298) | ||
| 3 | 1078 | $14,399 ($10,709) | ||
| 4 | 1401 | $12,285 ($8347) | ||
| With graft | 1 | 104 | $26,145 ($17,320) | <.001b |
| 2 | 163 | $28,832 ($17,930) | ||
| 3 | 128 | $24,593 ($19,662) | ||
| 4 | 150 | $16,827 ($14,914) | ||
| Secondary | 1 | 224 | $23,345 ($16,444) | <.001b |
| 2 | 270 | $22,896 ($15,778) | ||
| 3 | 274 | $19,466 ($15,128) | ||
| 4 | 285 | $15,349 ($10,756) | ||
| Presence of comorbidity | ||||
| Group | Variable | N | Mean (SD) | P |
| Primary | No comorbidity | 2633 | $13,382 ($9824) | <.001 |
| ≥1 comorbidity | 1708 | $17,390 ($13,121) | ||
| With graft | No comorbidity | 293 | $20,623 ($16,136) | <.001 |
| ≥1 comorbidity | 258 | $27,886 ($19,340) | ||
| Secondary | No comorbidity | 510 | $17,770 ($13,621) | <.001 |
| ≥1 comorbidity | 563 | $22,239 ($16,056) | ||
| Patient insurance | ||||
| Group | Variable | N | Mean (SD) | P |
| Primary | Medicare | 540 | $18,817 ($13,567) | <.001c |
| Medicaid | 301 | $13,610 ($10,428) | ||
| Private insurance | 2966 | $14,508 ($10,887) | ||
| Self-pay | 194 | $13,767 ($12,021) | ||
| Other | 340 | $14,635 ($11,380) | ||
| With graft | Medicare | 106 | $27,541 ($16,731) | .183 |
| Medicaid | 40 | $23,244 ($18,756) | ||
| Private insurance | 341 | $23,390 ($17,849) | ||
| Self-pay | 14 | $17,900 ($14,166) | ||
| Other | 50 | $23,228 ($21,814) | ||
| Secondary | Medicare | 215 | $23,298 ($16,285) | <.001c |
| Medicaid | 53 | $16,693 ($10,250) | ||
| Private insurance | 694 | $20,043 ($15,219) | ||
| Self-pay | 23 | $14,698 ($10,265) | ||
| Other | 88 | $16,378 ($13,089) | ||
aSignificant difference compared with Hispanic patients.
bSignificant difference compared with 4th quartile zip codes.
cSignificant difference compared with private insurance.
Table A4.
Univariate Analysis of Surgical Variablesa
| Anesthesia | ||||
|---|---|---|---|---|
| Group | Variable | N | Mean (SD) | P |
| Primary | General | 986 | $12,103 ($7386) | .011b |
| General with regional block | 460 | $12,995 ($6867) | ||
| Other | 104 | $10,928 ($5431) | ||
| With graft | General anesthesia | 80 | $15,171 ($8948) | .96 |
| General anesthesia + regional block | 15 | $14,636 ($6938) | ||
| Other | 11 | $14,496 ($13,863) | ||
| Secondary | General anesthesia | 169 | $12,860 ($6338) | .352 |
| General anesthesia + regional block | 64 | $12,832 ($5711) | ||
| Other | 16 | $10,550 ($5798) | ||
| Hospital admission | ||||
| Group | Variable | Admission rate, % | Mean (SD) | P |
| Primary | Not admitted | 94.4 | $14,548 ($10,776) | <.001 |
| Admitted postoperatively | 5.6 | $21,270 ($17,606) | ||
| With graft | Not admitted | 89.8 | $21,984 ($16,139) | <.001 |
| Admitted postoperatively | 10.2 | $42,208 ($23,465) | ||
| Secondary | Not admitted | 94.0 | $19,233 ($14,203) | <.001 |
| Admitted postoperatively | 6.0 | $33,610 ($21,402) | ||
| Surgical center ownership | ||||
| Group | Variable | N | Mean (SD) | P |
| Primary | Hospital-owned ASC | 2228 | $12,112 ($8353) | <.001 |
| Privately owned ASC | 482 | $9353 ($7170) | ||
| With graft | Hospital-owned ASC | 229 | $17,794 ($13,672) | .044 |
| Privately owned ASC | 37 | $13,045 ($10,246) | ||
| Secondary | Hospital-owned ASC | 424 | $14,429 ($10,223) | .059 |
| Privately owned ASC | 135 | $12,645 ($6960) | ||
| Surgeon volume—6 case cutoff | ||||
| Group | Variable | N | Mean (SD) | P |
| Primary | Low-volume surgeon | 1244 | $17,146 ($14,212) | .4 |
| High-volume surgeon | 1034 | $17,631 ($13,040) | ||
| With graft | Low-volume surgeon | 197 | $29,589 ($20,416) | .012 |
| High-volume surgeon | 176 | $24,352 ($19,575) | ||
| Secondary | Low-volume surgeon | 215 | $22,527 ($16,369) | .137 |
| High-volume surgeon | 462 | $24,630 ($17,472) | ||
| Surgical facility volume—15 case cutoff | ||||
| Group | Variable | N | Mean (SD) | P |
| Primary | Low-volume ASC | 2069 | $16,194 ($12,726) | <.001 |
| High-volume ASC | 2049 | $13,846 ($10,299) | ||
| With graft | Low-volume ASC | 299 | $26,617 ($20,126) | .001 |
| High-volume ASC | 227 | $21,318 ($15,277) | ||
| Secondary | Low-volume ASC | 393 | $21,711 ($15,635) | .021 |
| High-volume ASC | 642 | $19,450 ($15,031) | ||
aASC, ambulatory surgical center.
bSignificant difference compared with anesthesia + nerve block.
Footnotes
Final revision submitted December 10, 2019; accepted December 23, 2019.
One or more of the authors has declared the following potential conflict of interest or source of funding: S.L.B. has received educational support from Stryker and hospitality payments from Smith & Nephew and Stryker. R.Y.H. has received hospitality payments from Smith & Nephew and Stryker. B.D.B. has received hospitality payments from Wright Medical. B.D.O. has received consulting fees from DePuy, Linvatec, the Musculoskeletal Transplant Foundation, and Vericel and is a paid associate editor for The American Journal of Sports Medicine. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Bekelis K, Missios S, Kakoulides G, Rahmani R, Simmons N. Selection of patients for ambulatory lumbar discectomy: results from four US states. Spine J. 2014;14(9):1944–1950. [DOI] [PubMed] [Google Scholar]
- 2. Bokshan SL, Mehta S, DeFroda SF, Owens BD. What are the primary cost drivers of anterior cruciate ligament reconstruction in the United States? A cost-minimization analysis of 14,713 patients. Arthroscopy. 2019;35(5):1576–1581. [DOI] [PubMed] [Google Scholar]
- 3. Childers CP, Maggard-Gibbons M. Understanding costs of care in the operating room. JAMA Surg. 2018;153(4):e176233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Churchill RS, Ghorai JK. Total cost and operating room time comparison of rotator cuff repair techniques at low, intermediate, and high volume centers: mini-open versus all-arthroscopic. J Shoulder Elbow Surg. 2010;19(5):716–721. [DOI] [PubMed] [Google Scholar]
- 5. Dombrowski M, Murawski CD, Yasui Y, et al. Medical comorbidities increase the rate of surgical site infection in primary Achilles tendon repair. Knee Surg Sports Traumatol Arthrosc. 2019;27(9):2840–2851. [DOI] [PubMed] [Google Scholar]
- 6. Farjoodi P, Skolasky RL, Riley LH. The effects of hospital and surgeon volume on postoperative complications after lumbar spine surgery. Spine (Phila Pa 1976). 2011;36(24):2069–2075. [DOI] [PubMed] [Google Scholar]
- 7. Genuario J, Koval KJ, Cantu RV, Spratt KF. Does hospital surgical volume affect in-hospital outcomes in surgically treated pelvic and acetabular fractures? Bull NYU Hosp Jt Dis. 2008;66(4):282–289. [PubMed] [Google Scholar]
- 8. Ho G, Tantigate D, Kirschenbaum J, Greisberg JK, Vosseller JT. Increasing age in Achilles rupture patients over time. Injury. 2017;48(7):1701–1709. [DOI] [PubMed] [Google Scholar]
- 9. Krueger H, David S. The effectiveness of open repair versus percutaneous repair for an acute Achilles tendon rupture. J Sport Rehabil. 2016;25(4):404–410. [DOI] [PubMed] [Google Scholar]
- 10. Lantto I, Heikkinen J, Flinkkila T, Ohtonen P, Leppilahti J. Epidemiology of Achilles tendon ruptures: increasing incidence over a 33-year period. Scand J Med Sci Sports. 2015;25(1):e133–e138. [DOI] [PubMed] [Google Scholar]
- 11. Lemme NJ, Li NY, DeFroda SF, Kleiner J, Owens BD. Epidemiology of Achilles tendon ruptures in the United States: athletic and nonathletic injuries from 2012 to 2016. Orthop J Sports Med. 2018;6(11):2325967118808238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Li L, Bokshan SL, Mehta SR, Owens BD. Disparities in cost and access by caseload for arthroscopic rotator cuff repair: an analysis of 18,616 cases. Orthop J Sports Med. 2019;7(6):2325967119850503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Li L, Bokshan SL, Ready LV, Owens BD. The primary cost drivers of arthroscopic rotator cuff repair surgery: a cost-minimization analysis of 40,618 cases. J Shoulder Elbow Surg. 2019;28(10):1977–1982. [DOI] [PubMed] [Google Scholar]
- 14. Liles J, Adams SB. Management of complications of Achilles tendon surgery. Foot Ankle Clin. 2019;24(3):447–457. [DOI] [PubMed] [Google Scholar]
- 15. Malik AT, Phillips FM, Kim J, Yu E, Khan SN. Posterior lumbar fusions at physician-owned hospitals—is it time to reconsider the restrictions of the Affordable Care Act? Spine J. 2019;19(9):1566–1572. [DOI] [PubMed] [Google Scholar]
- 16. Ochen Y, Beks RB, van Heijl M, et al. Operative treatment versus nonoperative treatment of Achilles tendon ruptures: systematic review and meta-analysis. BMJ. 2019;364:K5120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pamilo KJ, Peltola M, Paloneva J, Makela K, Hakkinen U, Remes V. Hospital volume affects outcome after total knee arthroplasty. Acta Orthop. 2015;86(1):41–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Patrick NC, Kowalski CA, Hennrikus WL. Surgical efficiency of anterior cruciate ligament reconstruction in outpatient surgical center versus hospital operating room. Orthopedics. 2017;40(5):297–302. [DOI] [PubMed] [Google Scholar]
- 19. Rider CM, Hong VY, Westbrooks TJ, et al. Surgical treatment of supracondylar humeral fractures in a freestanding ambulatory surgery center is as safe as and faster and more cost-effective than in a children’s hospital. J Pediatr Orthop. 2018;38(6):e343–e348. [DOI] [PubMed] [Google Scholar]
- 20. Shakked RJ, Raikin SM. Insertional tendinopathy of the Achilles: debridement, primary repair, and when to augment. Foot Ankle Clin. 2017;22(4):761–780. [DOI] [PubMed] [Google Scholar]
- 21. Soroceanu A, Sidhwa F, Aarabi S, Kaufman A, Glazebrook M. Surgical versus nonsurgical treatment of acute Achilles tendon rupture: a meta-analysis of randomized trials. J Bone Joint Surg Am. 2012;94(23):2136–2143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Truntzer JN, Triana B, Harris AHS, Baker L, Chou L, Kamal RN. Cost-minimization analysis of the management of acute Achilles tendon rupture. J Am Acad Orthop Surg. 2017;25(6):449–457. [DOI] [PubMed] [Google Scholar]
- 23. Westin O, Svensson M, Nilsson Helander K, et al. Cost-effectiveness analysis of surgical versus non-surgical management of acute Achilles tendon ruptures. Knee Surg Sports Traumatol Arthrosc. 2018;26(10):3074–3082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Williamson ERC, Vasquez Montes D, Melamed E. Multistate comparison of cost, trends, and complications in open versus endoscopic carpal tunnel release [published online March 29, 2019]. Hand (N Y). doi: 10.1177/1558944719837020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Willits K, Amendola A, Bryant D, et al. Operative versus nonoperative treatment of acute Achilles tendon ruptures: a multicenter randomized trial using accelerated functional rehabilitation. J Bone Joint Surg Am. 2010;92(17):2767–2775. [DOI] [PubMed] [Google Scholar]