Abstract
A killer pandemic is now more likely than ever. Where will it come from and how can we beat it, asks Debora MacKenzie
IN 1347, an epidemic of unimaginable ferocity struck Europe. People first experienced flu-like symptoms, but within days painful swellings developed, which turned black, split open and oozed pus and blood. The Great Pestilence, later dubbed the Black Death, swept across the continent within four years, killing up to half the population. The disease persisted in Europe until the 1700s, always circulating somewhere, killing people off.
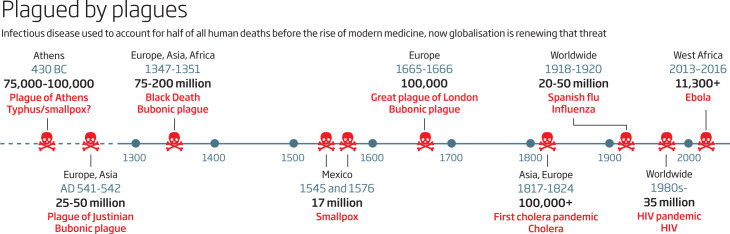
We speak of it nowadays as history. In fact, it is more like natural history: infectious disease is part of the ecology of our species. Until 1900, and despite considerable competition from violence and starvation, it was our biggest killer, causing half of all human deaths. Now, it accounts for fewer than a quarter of all deaths worldwide, most of them in poor, tropical regions. In rich countries it is only a few per cent. And the toll is falling.
But we shouldn't be complacent: plagues will return. The 1960s notion that infectious disease was on the way out ended when HIV appeared in the 1980s. Since then, many infections like bird flu, SARS and Zika have caused alarm. But it took a near-disaster – the worst ever outbreak of Ebola – to scare the inertia out of governments. As a result, we are at last preparing for the inevitable. A clutch of programmes being launched this year will improve our grip on microbial killers. And the world now has an emergency medical response team – which, astonishingly, it never had before. But we aren't there yet. If a novel virus struck now, we would still be in trouble.
For all our high-tech modernity, and in many ways, because of it, the risk that new infectious diseases will evolve is actually getting worse. Pathogens began circulating regularly among humans only after we started farming and settled in towns. One reason was that we caught infections from our livestock: flu from ducks, tuberculosis from cows. But crucially, there were enough of us in close proximity that a germ could always find a new host and keep spreading, persisting among people and adapting to us.
Now we are crowding into cities and travelling more, especially within the tropics where pathogen diversity is highest. That plus globalised trade, migration and climate change reshuffle wildlife, people and pathogens. Farms and towns invade the habitats of animals with viruses that can jump to us, or to our densely packed livestock, also booming as demand for animal protein soars.
Public health experts have been warning for years of “emerging” diseases, which can go from unknown to epidemic if the pathogen mutates or the ecology of its hosts changes to make its spread easier. And it is viruses that epidemiologists are most worried about. Bacteria can be deadly, and antibiotic resistance could mean diseases from gonorrhoea to ordinary bladder infections become incurable, but work has at least begun on new drugs. In contrast, viruses can evolve and spread faster, there are thousands we know nothing about, and we have few drugs against them. The worst emerging infections since 2000 have all been viruses.
None is more alarming than the 2014 outbreak of Ebola in West Africa. The virus infected 50 times more people than any previous outbreak, and reached big cities for the first time. As a bat virus still unaccustomed to humans, it spread fairly slowly, but an even slower international response allowed it to kill more than 11,000 people before old-fashioned methods, like isolating cases and quarantining their contacts, snuffed the outbreak out.
There was no other option. We were unable to produce a vaccine in time even though we already had experimental Ebola drugs and vaccines, and their deployment was accelerated, with regulation and manufacture taking months instead of the usual years. Researchers have since discovered that as it spread the Ebola virus was adapting to people, and getting better at transmitting. It almost spiralled out of control in Nigeria. “The world was close to an abyss,” says Tom Frieden, outgoing head of the US Centers for Disease Control and Prevention.
To combat the next plague, we will need vaccines, drugs and diagnostic tools – and just as importantly, some way to deploy them effectively. “We do not have that,” says Jeremy Farrar, head of UK medical research agency the Wellcome Trust. But we might if, in the wake of Ebola, we can build on momentum in three key areas: working out what the enemy is, arming ourselves against it and being ready to act forcefully and fast.
1 Know your enemy
First, what should we prepare for? “Spotting the next HIV or SARS before it strikes is virtually impossible,” says Ab Osterhaus, head of the new Research Center for Emerging Infections and Zoonoses in Hannover, Germany. “There are too many viruses in too many species, interacting with humans and evolving in unpredictable ways.” To narrow the field, he says, we need “a detailed understanding of when, where and how viruses are moving from wildlife to people”. Because, like the historical plagues, the next big disease is likely to be one that has made the leap from other animals to us.
In December, Mark Woolhouse and his colleagues at the University of Edinburgh, UK, reviewed what we know about such viruses. They identified 37 already able to spread from human to human, though poorly, that could become more contagious. These range from virtual unknowns like o'nyong-nyong, an African virus that causes debilitating joint pain, to Rift Valley fever, a common livestock illness.
That's just the viruses we know. A project called PREDICT, funded by the US Agency for International Development, is looking for others. In places, mostly tropical, where humans and wild mammals interact, the project screens people, their food and their rodent, bat and primate neighbours, looking for genetic sequences of viruses in families known to spawn human pathogens. They have found 984 viruses, 815 of them new to science. In the process, they have mapped hotspots of viral diversity and trained and equipped local labs to test for viruses and watch for disease.
Predicting risk
But which of these viruses should we focus on? Some are obvious, such as a Chinese virus closely related to SARS but different enough that prototype SARS vaccines won't work against it. Others might be identified using a clue discovered by Kevin Olival of the EcoHealth Alliance, who works with PREDICT.
He has statistically analysed all the available data on the flavivirus family, a troublesome lot carried by mosquitoes and ticks that includes yellow fever, Zika, dengue and West Nile. Last November, he reported that the more species a flavivirus regularly infects, the more likely it is to infect humans as well. That makes the riskiest flaviviruses a clutch of virtual unknowns: Usutu – a bird-borne virus invading Europe – Ilheus, louping ill, Wesselsbron and Tyuleniy.
The Global Virome Project wants to go further in learning about the enemy, genetically sequencing and mapping most of the estimated half-million so-far undiscovered viruses in families we know can infect humans. It reckons it will need $3.4 billion to do that over the next decade, and this year it will start canvassing for funds. The hope is that knowing what viral diversity exists and where could provide unexpected insights and spur investment in disease control.
2 Arm yourself
Once we know what we are fighting, we have to arm ourselves. Finding weapons won't be easy, though. The vaccines that defeated so many infectious diseases in the 20th century were mostly made by government-owned firms that didn't have to turn a profit and produced what was needed as a “public good”. In the 1980s, everything was privatised. That was good for spurring profitable medicines for chronic conditions. But much medical innovation is now done by small, start-up biotech firms, which can't afford to shepherd their products through the “valley of death” – the long, expensive process of testing for safety and efficacy, and establishing manufacturing processes and formulations for licensing. Only big pharma companies have the know-how and the $1 billion or so needed to bring a new vaccine to market. But vaccines for common diseases offer little profit; those against a virus that might or might not go epidemic are a commercial non-starter.
There have been efforts to bring public good back in. Since the 1990s, new treatments for diseases of poverty, like the meningococcal vaccine for Africa, were developed by public-private partnerships between big pharma, governments and large philanthropies like the Bill & Melinda Gates Foundation. “But the momentum fell,” says Farrar. In 2013, government and private research on “neglected” emerging diseases amounted to only 1.6 per cent of the $195 billion spent on health R&D. Of that, only a fifth was private.
Now, because of Ebola, the momentum may be back. Last May, the World Health Organization set out an “R&D blueprint for action to prevent epidemics“, which aims to bring all parties together to develop responses before the next plague strikes. Committees are being set up to look for solutions to problems that emerged during the Ebola outbreak, from agreed protocols for quickly testing and licensing experimental drugs and vaccines, to liability insurance for using experimental products, to contracts ensuring information and biological samples are shared.
But the most important goal is to accelerate R&D on nine priority pathogens (see “The nine viruses of the apocalypse ”). Using an approach pioneered for malaria vaccines, the WHO will find out what research is being done, get participants talking and push progress towards vaccines, drugs and diagnostic tests. Any products must be affordable. That means their prices will be “delinked” from the cost of developing them, by making sure companies are recompensed in other ways. So far no one knows how that will work, but it is already being discussed for new antibiotics.
The nine viruses of the apocalypse.
These are the diseases the World Health Organization thinks we should find remedies for, fast. The first six are its highest priority.
Lassa fever
This West African virus, carried by the common Natal multimammate rat, infects 300,000 people a year. Most have no symptoms, but it can cause diarrhoea and vomiting, then internal fluid accumulation, bleeding from orifices, shock, seizure and coma. It kills some 5000 people annually. Initial symptoms resemble other local diseases, making diagnosis tricky – one reason West Africa was slow to spot Ebola.
Nipah
This bat virus started killing people in 1999 in Malaysia after pig farms were built near fruit bats, which dropped half-eaten fruit into pigsties. People get it from pigs and bats, but it can also spread between humans. Nipah breaks out sporadically in and around densely populated Bangladesh, causes inflammation of the brain and has a high fatality rate.
Rift Valley fever
Widespread across Africa, this virus invaded the Arabian Peninsula in 2000, and could go further. It mainly infects cattle and is spread by mosquitoes; people can get it from mosquito bites or by eating infected beef. Symptoms are usually mild but it can cause haemorrhagic fever, which kills in half of cases.
SARS, MERS and emerging coronaviruses
These related bat viruses infect a range of mammals and have already emerged in humans twice, resulting in severe pneumonia: SARS in 2003 and MERS in 2014. Both spread from human to human.
Crimean-Congo haemorrhagic fever
Found across Africa, Asia and south-east Europe, the virus is invading new territory as its tick hosts capitalise on global warming. It appeared in western Europe in 2010. Infected people generally have a mild fever but some strains cause severe haemorrhagic disease, with bleeding internally and from orifices, from which 30 per cent of people die.
Chikungunya
A virus spread by Aedes mosquitoes between monkeys and small mammals in East Africa, Chikungunya started causing large epidemics around 2000 and exploded into Asia in 2005, after mutations made it better adapted to a new mosquito host. In 2014, it invaded the Americas and has occurred in Europe. It rarely kills but causes debilitating joint pains, which can persist for months.
Zika
A monkey virus that has infected humans in Africa and Asia for decades, Zika suddenly entered the Americas in 2013. In 2015, it was linked to a wave of severe birth defects including microcephaly. Companies are already working on vaccines but the WHO wants extra research into the virus's effects on fetal brains.
Severe fever with thrombocytopenia syndrome
Flies under the radar – possibly because of its name. The virus, discovered in 2011, can cause fever and multi-organ failure, killing 12 per cent of people it infects. It has been found in east Asia, seems to be carried by farm animals, and is spread by ticks. A nearly identical virus, called heartland, has turned up in the US.
Novel agent
Given the rate at which previously unknown or obscure infections have suddenly emerged in humans and other animals, the WHO is leaving a slot on its list for a germ we don't yet know. Research here may include looking for agents that might explode.
Money matters.
As global economies become more interconnected, contagious diseases and their knock-on effects spread more rapidly. “Nowadays the biggest risk from epidemics is economic,” says Ramanan Laxminarayan of Princeton University. The 2003 SARS epidemic killed 800 people, for example, but cost the world $54 billion in quarantine measures and lost trade and travel. The World Bank estimates that a flu pandemic as bad as the one in 1918 would lop 5 per cent off world GDP and cause an $8 trillion recession. The faster we respond to an epidemic, the less expensive it will be. So we must be prepared – and that costs. Who will pay?
One answer may be novel funding mechanisms. Last May, the World Bank launched something new: plague insurance. Rich countries are at risk from epidemics that start in poor countries. So under the Pandemic Emergency Financing Facility they can buy insurance against severe flu, coronaviruses like SARS or MERS, filoviruses like Ebola, and diseases that pass between animals and humans like Lassa. Premiums are based on risk, calculated for the bank by the epidemiological modelling company Metabiota. If one of these diseases strikes a poor country, money to contain it can be released quickly from the insurance pot. The bank also sells “catastrophe” bonds to fund response to a wider range of epidemics.
The WHO is not alone in trying to encourage the forging of weapons. In January, the Coalition for Epidemic Preparedness Innovations (CEPI) was launched at the World Economic Forum in Davos, Switzerland, to help get experimental vaccines through the “valley of death”. CEPI, which is backed by Norway, India, the Gates Foundation and the Wellcome Trust, has commitments of $540 million and, say organisers, is “on track” to get $1 billion for the next five years. By then it hopes to have vaccines against Nipah, MERS and Lassa viruses tested for safety and effectiveness in phase II trials. It even wants to have small stockpiles of the promising vaccines for fast response to outbreaks.
However, no one can afford phase III trials on larger numbers of people. And no one can test whether a vaccine works until there is an outbreak. Those tests may have to be done in a hurry once an epidemic starts.
3 Be ready to act – fast
With potential mass killers identified, and drugs in hand, we will be on the right track. But we must also be ready to act fast on a large scale. Paradoxically, that means getting more familiar with what is normal, so we can spot ominous changes.
One problem is that contagion is exponential: case numbers rise very slowly at first, then sky-rocket. “First people complain that you are putting too much effort into a small problem. Later they say you were too slow,” says Sylvie Briand, head of the pandemics department at the WHO. To better predict which outbreaks might take off, the WHO now has teams looking at the use of “big data”, such as combining existing data sets on climate, vaccination and population immunity. It is also setting up networks of social scientists and anthropologists to explore ways to improve communications among people swept up in plagues – a major roadblock to rapid response during the Ebola outbreak. The first and fundamental problem there, however, was surveillance: no one spotted the first few cases of Ebola before it spread widely.
“To get ready for the big one, we need health workers close to the entire population, everywhere, who know where to go if something funny is going on – then labs to test samples, and response teams,” says Seth Berkley, head of GAVI, a global alliance that helps poor countries get routine vaccines. Under a 2005 treaty called the International Health Regulations, all 192 WHO member states must set up enough surveillance to tell the WHO about any outbreak that is serious, unusual or could trigger international travel or trade restrictions. However, not one world region, even Europe, has done everything the treaty requires. Africa, home of many worrying viruses, has done least.
An international collaboration called the Global Health Security Agenda is trying to help countries fill the gaps – and Ebola has scared many into listening. “There has been a change of mindset,” says Briand: watching existing health risks more closely will help countries spot new ones.
Emergency responders
In addition, the WHO, which has always been a technical agency, setting policies by slow consensus, has reinvented itself to respond faster in an emergency. Instead of independent offices in different countries spotting emergencies – or not – according to their own criteria, the WHO now has dedicated staff worldwide who can do standardised assessments of unusual events, deploy emergency teams within 72 hours and scale up quickly. To aid coordination, they are answerable to the head office in Geneva, a first for the WHO.
The agency is also working with the World Food Programme to set up global supply chains for equipment such as masks and syringes. This year it will launch an online course to train emergency responders. And it is working with the Inter-Agency Standing Committee, a Geneva-based body that coordinates the world's emergency responses to war and natural disasters, which last year expanded its remit to epidemics.
Plagued by plagues
But, no matter how fast you detect outbreaks, or how many drugs or vaccines you invent, you still face the problem of producing and deploying enough of them to make a difference. “You can't build a vaccine factory and only switch it on in an emergency,” says Martin Friede at the WHO. Like standing armies, production lines and staff need honing and updating.
A possible solution for limited manufacturing capacity comes from ongoing efforts to control flu – one pandemic we know for sure will come. The flu vaccine is made of a standard, benign flu virus with two new proteins from whatever strain is circulating that year stuck onto it to induce immunity to that strain. The vaccine changes every year, but doesn't need new plants or regulatory approval as the package is well tested. “We can produce safety-tested vectors at scale, then drop in antigens of interest if a new disease emerges,” says Berkley. “That way, you can build vaccine capacity for a pathogen you don't even know.”
That isn't happening yet. Nor is it clear if the WHO will get enough funds to continue any of this work, especially with a new US president who has opposed UN funding. “The really big problem is appreciating what is at stake,” says Berkley. He says a pandemic is an “evolutionary certainty”. “If people understood the risk, they would want to be sure systems are in place to deal with it. The costs of doing that are trivial compared to the cost of ignoring it.”
We have been jolted out of our complacency, but there's still a lot to be done. “With Ebola the world recognised that the largest unmanaged risk to the global economy and security is infectious hazards,” says Bruce Aylward, assistant director-general at the WHO. “Are we prepared for pandemics? Definitely not! Are we more prepared? Definitely.”
This article appeared in print under the headline “The coming plague”
How you can reduce the risk of a pandemic.
In our increasingly crowded, urban, globalised world, a virus will eventually get out of control. There are things we can all do to reduce the risks.
Bear witness: Inform yourself and do what you can to spread awareness of the risks, and of the responses being devised that desperately need support. Politicians control purses, so get tweeting.
Stand up to denialists: Some will say warnings about pandemics are a hoax, because SARS/bird flu/swine flu was supposed to kill us all and didn't. Here's your riposte: a lot of people worked hard to keep SARS contained; bird flu hasn't gone rogue yet but it's a few mutations away; swine flu did kill and the next flu could kill far more.
Prepare: You needn't be a survivalist to prepare for the panic and disorder likely to attend a pandemic. Most countries have guidelines that recommend stocking a few weeks' worth of water, food, medicines, flashlight batteries and such. Learn about the best ways to avoid people who might be contagious. If you run a business, have a continuity plan. If you are a public official, check whether your administration has a pandemic plan. If not, check out the WHO's guidelines. If you speak for a health body or organisation, learn about communications in a pandemic because mistakes can be deadly. Hint: trust people with the truth.
Keep watch: Countries don't like to admit they have infectious diseases: it's bad for business. The ProMed global reporting site revealed SARS and MERS before the governments involved did. Now it has helped launch Epicore. Medical and veterinary workers sign up to it, then when ProMed gets wind of something it asks them what's happening. Replies appear on a web platform that can be set to partial or total confidentiality. Wherever you are, if you meet the criteria, sign up to Epicore. You could be the first to spot something amiss.