Abstract
Objectives:
To examine associations of sociodemographic and clinical factors with cognitive, physical, and mental health among independent living older adults in a continuing care senior housing community (CCSHC).
Design:
Cross-sectional study.
Setting:
Independent living sector of a CCSHC in San Diego County in California.
Participants:
English-speaking adults age 65-95 years, two-thirds women. Of the 112 subjects recruited, 104 completed basic study assessments.
Measurements:
We computed composite measures of cognitive, physical, and mental health. We also assessed relevant clinical correlates including psychosocial factors such as resilience, loneliness, wisdom, and social support.
Results:
The CCSHC residents were similar to a randomly selected community-based sample of older adults on most standardized clinical measures. In the CCSHC, physical health correlated with both cognitive function and mental health, but there was no significant correlation between cognitive and mental health. Cognitive function was significantly associated with physical mobility, satisfaction with life, and wisdom, whereas physical health was associated with age, self-rated physical functioning, mental well-being, and resilience. Mental health was significantly associated with income, optimism, self-compassion, loneliness, and sleep disturbances.
Conclusions:
Different psychosocial factors are significantly associated with cognitive, physical, and mental health. Longitudinal studies of diverse samples of older adults are necessary to determine risk factors and protective factors for specific domains of health. With rapidly growing numbers of older adults who require healthcare as well as supportive housing, CCSHCs will become increasingly important sites for studying and promoting the health of older adults.
Keywords: Resilience, Social support, Loneliness, Wisdom, Retirement community, Lifestyle
Introduction
The US population over age 65 increased from 36 million in 2003 to 45 million in 2013, and is expected to total 84 million by 2050 (1, 2). Aging is a major risk factor for decline in cognitive and everyday functioning capacities and autonomy. Impairment in cognitive function is cited as the number one concern for older adults (3). Although most older adults would prefer to age in place, this goal becomes difficult to sustain as cognitive and physical disabilities increase, barriers to autonomy grow, and adequate caregiving becomes unavailable or unaffordable . Choosing between staying at home and moving to a more supportive housing is a complex decision impacted by a large number of “pushing factors” such as declining function, driving status, lack of assistance, and loneliness, and “pulling factors” like the need for replenishing social networks and a comfortable living environment .
Senior housing or retirement communities are a prime growth industry of the future (4). A popular model is a continuing-care senior housing community (CCSHC) which provides transitions along a continuum of care – independent living, assisted living, and memory care (5). It offers its residents stability of housing and healthcare when aging-associated cognitive and/or physical disabilities result in a move from independent to assisted living. As the ratio of older patients to younger caregivers increases (6), greater numbers of older adults may move into CCSHCs. For many CCSHCs, the monthly payment increases steeply when residents transition to assisted living. Delaying these transitions through facilitating longer independent living in a CCSHC should be an important healthcare goal.
As the World Health Organization has stated, the current healthcare system – focusing on acute treatment and disease cure – is too fragmented and inefficient (7). The future healthcare will involve more direct care within the community including the home (8). Promotion of lifestyle-based group interventions such as diet, physical activity, and cognitive stimulation is more feasible in CCSHCs than in the general community where older adults are geographically scattered. Characterization of the cognitive, physical, and mental health of the people living in CCSHCs is necessary for identifying treatment targets and planning effective interventions. Yet, we found few comprehensive studies of these different domains of health in residents of such retirement communities.
The main goals of this cross-sectional study were to describe a sample of older adults in the independent living sector of a representative CCSHC; assess their physical, cognitive, and mental health; and examine associations with potential risk factors and protective factors related to aging-related decline in health. Such data would help develop specific hypotheses for longitudinal studies of this population. To capture the broad phenomenon within each construct, we combined two or more related measures in each domain (e.g., physical health) and created composite scores by using principal component analysis, a dimension-reduction technique widely used to optimally summarize information from different outcomes. Risk factors are those reported in the literature as contributing to an increased risk of cognitive, physical, and mental disabilities and mortality. These include older age, smoking, substance use, sedentary behavior, loneliness, and worse health in other domains (e.g., poor cardiovascular health may increase the risk of cognitive decline). Protective factors are those that have been reported to promote positive health or delay decline in health; examples include resilience, optimism, social engagement, wisdom, and active lifestyle.
For the present study, we selected a CCSHC that was representative of CCSHCs in the US in terms of the sociodemographic characteristics of its residents. A typical CCSHC has residents with a mean age of 84 years, 68% being women, mostly white, 69% with college education, 41% married, and 72% with annual incomes of ≥ $50,000 (9).
We also sought to assess the generalizability of our findings to non-CCSHC older adults living in the community. For this purpose, we compared the CCSHC sample to randomly selected, age-and sex-comparable individuals from a separate ongoing study in the general community, called SAGE (Successful AGing Evaluation; (10, 11)). For the CCSHC cohort, we hypothesized that (1) cognitive, physical, and mental health composite measures would be related to each other; and (2) worse cognitive, physical, and mental health would be associated with older age, lower education and income, higher body mass index (BMI), loneliness, and sleep disturbances, and lower levels of positive psychosocial factors including resilience, optimism, wisdom, and self-compassion.
Research Design and Methods
Participants and Procedures
Senior Housing Residents:
Participants for this study were recruited from a senior housing community in San Diego County. This CCSHC has a total of 278 independent residential units and offers all three levels of care: independent living, assisted living, and memory care. All subjects came from the independent living sector and provided a written informed consent for study participation.
Selection criteria for enrollment were: i) English speaking individuals ≥ 65 years, ii) Ability to complete study assessments, and iii) no known diagnosis of dementia or any other disabling illness. This study protocol was approved by the University of California San Diego Human Research Protections Program (HRPP). Participants were recruited through short presentations using HRPP-approved script and flyers.
Comparison Group:
The comparison participants came from the SAGE study, which involves over 2,000 community-dwelling adults in San Diego County, aged 21 to 100 years, selected using random digit-dialing (10, 11). Participants were English-Speaking, able to provide informed consent, participate in a phone interview (mainly for cognitive assessment), and complete a survey questionnaire (online or mailed) that included a number of published rating scales for assessing physical and psychosocial functioning, but no in-person evaluations such as physical examinations (unlike CCSHC residents). We excluded participants residing in nursing homes or requiring daily, skilled nursing care, or with a diagnosis of dementia or a terminal illness. This study too had been approved by the university’s HRPP.
We compared the CCSHC sample to 3 different (but overlapping) subsamples from the SAGE cohort: (1) all the SAGE subjects within the CCSHC age-range of 65-95 years (N=625), (2) one-to-one age (plus or minus 1 year) and sex-matched subsample of SAGE subjects (N=104), and (3) a subsample of SAGE participants matched by CCSHC age group percentages (N=119). For this last purpose, we divided the CCSHC sample into seven half-decade age groups (65-69, 70-74, etc.) to determine the percentage of participants within each group. Participants from the SAGE cohort were then randomly selected to create a subsample of subjects matched by half-decade age percentages (N=119). Results were largely similar across all the three sub-samples. Because of space constraints, we have presented results from the last subsample only.
Measures
Trained study staff conducted structured interviews with the CCSHC residents to obtain following data.
Socio-Demographics included age, sex, education, race/ethnicity, marital status, and personal income, all based on self-report.
Cognitive and Everyday functioning was measured with the Montreal Cognitive Assessment (MoCA) (12) and UCSD Performance Based Skills Assessment-Brief (UPSA-B) (13). Both MoCA and UPSA-B have been used internationally and validated as objective measures of cognitive status and everyday functioning, respectively, (14, 15). In the SAGE study, cognition had been assessed with the modified version of the Telephone Interview for Cognitive Status (TICS-m; 16).
Physical health was assessed primarily by using two objective measures: the Short Physical Performance Battery (SPPB) and Timed Up and Go (TUG) Test (17, 18), which have been widely used and validated as objective measures of lower extremity function and mobility (19) and as predictors of disability, global decline, and mortality (19). Other measures included the physical health component from the Medical Outcomes Study (MOS) 36-item Short Form (SF-36; 20), Patient-Reported Outcomes Measurement Information System (PROMIS) Sleep Disturbance measure (21), BMI (kg/m2), and Cumulative Illness Rating Scale for Geriatrics (CIRS-G) (22).
Mental health was primarily evaluated with the Satisfaction with Life Scale (23), Happiness Subscale (24) of the Center for Epidemiological Studies – Depression (CES-D) scale (25), mental health component score of the SF-36 (20), Brief Symptom Inventory or BSI Anxiety Scale (26), Patient Health Questionnaire – 9-item Depression Module (PHQ-9; 27), and Perceived Stress Scale (28). Additional measures of psychosocial factors included 10-item Connor-Davidson Resilience Scale or CDRS, (29), Life Orientation Test – Revised or LOTR for optimism (30), Neff Scale for Self-Compassion (31), UCLA-3 scale for loneliness (32), Social Support Inventory (33), and Brief Multi-Dimensional Measure of Religiousness/Spirituality (BMMRS) (34).
Analytic Procedures
Descriptive statistics (proportions for categorical variables, and means and standard deviations for continuous measures) were computed for the sample. Independent group t-test was used for continuous and chi-square test for categorical variables when comparing the CCSHC and SAGE groups. Spearman’s r (rs) was calculated to assess bivariate correlations.
Principal component analysis (PCA) was used to reduce dimensions of correlated outcomes and develop composite measures of the three main health domains: cognitive, physical, and mental health. The Cronbach’s alpha and omega statistics for internal consistency were calculated for each composite measure (35). The purpose of the regression analysis was to determine significant associations among those three principal domains of health, without any causal inferences. Each regression started with all relevant predictors plus covariates in the model. The least absolute shrinkage and selection operator (LASSO) was used to trim the model, and statistical significance was computed for the predictors/covariates that remained in the trimmed model (36). The variance inflation factor (VIF) was calculated to detect any potential multicollinearity (37). The backward elimination procedure ensured minimum bias in the final model (38).
Results
Participant Characteristics
We recruited 112 CCSHC subjects (76 women and 36 men), of whom 2 failed medical screening criteria for enrollment and 9 dropped out: 2 had surgical and medical procedures that made their participation difficult, 5 were no longer interested after signing the consent form, 1 moved out of the community, and 1 was lost to follow-up. All 9 drop-outs were white, between ages of 76 and 92 years, and 3 of them were women. Of the subjects being studied, 104 completed most assessments and were included in the analyses. These 104 subjects did not differ significantly from the 7 with incomplete assessments, on any sociodemographic measures.
The 104 study participants ranged in age from 65 to 95 years, and 67% of them were women (Table 1). Our CCSHC subjects were similar to the national CCSHC population in terms of mean age, gender and race/ethnicity distribution, education, marital status, and income (5). However, our CCSHC groups included fewer racial/ethnic minority subjects (specifically, Latinos and Asian Americans) and had more years of education than their age- and sex-comparable SAGE counterparts. Yet, the CCSHC and SAGE groups were similar on most of the self-reported sociodemographic, cognitive, physical, and mental health measures that were common to both groups. (The SAGE study had not included in-person cognitive or physical assessments.) The only exceptions were higher BMI, more cognitively stimulating activities, greater loneliness, and less optimism and self-compassion in the CCSHC group.
Table 1:
Comparison of Senior Housing Residents (N=104) with SAGE Subjects (N=119; Comparable in Age Group Percentages) on Sociodemographic, Lifestyle, Cognitive, Physical, and Mental Health Measures
| N | Mean or % |
SD | N | Mean or % |
SD |
t or x2 |
df | p | |
|---|---|---|---|---|---|---|---|---|---|
| Socio-demographics | |||||||||
| Female | 70 | 67% | 73 | 61% | 0.86 | 1 | .35 | ||
| Age | 104 | 83.6 | 6.6 | 119 | 83.4 | 6.5 | 0.31 | 221 | .76 |
| Education | |||||||||
| High School and Below | 13 | 12% | 23 | 19% | 7.10 | 2 | .03 | ||
| Some College to Bachelor Degree | 59 | 57% | 46 | 39% | |||||
| Post-Graduate Degree | 32 | 31% | 49 | 42% | |||||
| Race | |||||||||
| Caucasian | 97 | 93% | 95 | 80% | 8.37 | 1 | .004 | ||
| Non-Caucasian | 7 | 7% | 24 | 20% | |||||
| Marital Status | |||||||||
| Currently Married/Cohabitating | 40 | 39% | 55 | 46% | 1.37 | 1 | .24 | ||
| Currently Single | 64 | 61% | 64 | 54% | |||||
| Personal Income | |||||||||
| <$35,000 | 21 | 24% | 35 | 31% | 1.12 | 2 | .57 | ||
| $35,000 - $74,999 | 39 | 45% | 46 | 41% | |||||
| $75,000+ | 26 | 31% | 31 | 28% | |||||
| Lifestyle Factors | |||||||||
| Ever Smoker (% yes) | 43 | 45% | 48 | 43% | 0.11 | 1 | .74 | ||
| Current Smoker (% yes) | 0 | 0% | 5 | 5% | 4.78 | 1 | .06* | ||
| Alcohol Use | |||||||||
| Lifetime abstainer | 13 | 14% | 28 | 24% | 4.37 | 3 | .23 | ||
| Infrequent drinker (< once/day) | 41 | 43% | 46 | 40% | |||||
| Regular drinker (daily) | 23 | 24% | 26 | 23% | |||||
| Former infrequent drinker | 18 | 19% | 15 | 13% | |||||
| Cognitively Stimulating Activities | 87 | 3.3 | 0.6 | 111 | 3.1 | 0.7 | 2.48 | 196 | .01 |
| Social Engagement Activities | 83 | 2.2 | 0.6 | 97 | 2.1 | 0.7 | 0.62 | 178 | .54 |
| Cognitive and Everyday Functioning | |||||||||
| Cognitive Health Composite Score† | 97 | <0.01 | 1.25 | ||||||
| Global cognition (MoCA) | 101 | 23.5 | 3.6 | ||||||
| Everyday Functioning (UPSA-B) | 104 | 74.4 | 13.1 | ||||||
| Global Cognition (TICS-m) | 119 | 34.5 | 4.5 | ||||||
| Physical Health | |||||||||
| Physical Health Composite Score† | 97 | <0.01 | 1.33 | ||||||
| Physical Performance (SPPB) | 103 | 7.8 | 2.8 | ||||||
| Physical Mobility (TUG) | 96 | 11.3 | 3.5 | ||||||
| Physical Well-being (SF-36) | 95 | 40.5 | 11.1 | 117 | 41.5 | 11.9 | −0.64 | 210 | .53 |
| Sleep Disturbances (PROMIS) | 85 | 47.9 | 7.3 | 69 | 49.6 | 6.2 | −1.52 | 152 | .13 |
| BMI | 102 | 28.2 | 5.2 | 119 | 25.2 | 3.9 | 4.79 | 185.1 | <.001 |
| Comorbidities (CIRS-G) | 103 | 9.0 | 3.3 | ||||||
| Mental Health | |||||||||
| Mental Health Composite Score† | 97 | <0.01 | 1.00 | 119 | <0.01 | 1.00 | <0.01 | 205.3 | 1.0 |
| Satisfaction with Life Scale | 95 | 26.3 | 5.5 | 117 | 26.5 | 5.6 | −0.28 | 210 | .78 |
| Happiness (CESD) | 96 | 9.2 | 3.1 | 114 | 9.8 | 2.7 | −1.49 | 208 | .14 |
| Mental Well-being (SF-36) | 95 | 54.7 | 8.3 | 117 | 55.6 | 8.1 | −0.77 | 210 | .44 |
| Anxiety (BSI) | 97 | 1.9 | 3.4 | 118 | 1.4 | 2.1 | 1.41 | 154.7 | .16 |
| Depression (PHQ9) | 93 | 3.2 | 4.1 | 113 | 2.4 | 3.4 | 1.51 | 204 | .13 |
| Perceived Stress (PSS) | 92 | 12.3 | 5.1 | 115 | 11.4 | 5.4 | 1.27 | 205 | .20 |
| Resilience (CDRS) | 96 | 29.8 | 5.4 | 117 | 30.1 | 5.8 | −0.33 | 211 | .74 |
| Optimism (LOT-R) | 97 | 22.9 | 3.4 | 113 | 24.2 | 3.7 | −2.67 | 208 | .008 |
| Self-Compassion (Neff SCS) | 92 | 42.7 | 5.8 | 114 | 44.6 | 6.9 | −2.01 | 204 | .05 |
| Loneliness (UCLA-3) | 85 | 37.6 | 9.8 | 102 | 34.6 | 9.8 | 2.13 | 185 | .04 |
| Social Support Index | 87 | 51.0 | 7.5 | 113 | 51.2 | 7.6 | −0.17 | 198 | .86 |
| Overall Religiosity (BMMRS) | 92 | 5.0 | 1.7 | 115 | 4.8 | 1.7 | 0.98 | 205 | .33 |
| Life Events Scale | 94 | 3.7 | 4.6 | 109 | 3.0 | 2.8 | 1.26 | 148.7 | .21 |
| Self-Rated Successful Aging | 97 | 8.2 | 1.3 | 118 | 8.4 | 1.1 | −1.29 | 213 | .20 |
| San Diego Wisdom Scale | 85 | 3.8 | 0.3 | 114 | 3.8 | 0.4 | −0.91 | 197 | .37 |
| Personal Mastery Scale | 98 | 21.0 | 3.1 | 115 | 21.7 | 3.4 | −1.67 | 211 | .10 |
| Coping Self-Efficacy | 95 | 90.2 | 25.1 | 116 | 94.7 | 23.3 | −1.36 | 209 | .18 |
| Meaning of Life - Presence Scale | 97 | 25.6 | 5.7 | 114 | 27.1 | 5.3 | −1.90 | 209 | .06 |
| Meaning of Life - Search Scale | 96 | 19.6 | 6.9 | 113 | 18.2 | 7.5 | 1.32 | 207 | .19 |
Fisher’s exact test
Composite scores were based on normalized data
Abbreviations:
BMI = Body Mass Index
BMMRS = Brief Multi-Dimensional Measure of Religiousness/Spirituality
CCSHC = Continuing Care Senior Housing Community
BSI = Brief Symptom Inventory Anxiety Scale
CDRS = Connor-Davidson Resilience Scale
CES-D = Center for Epidemiological Studies – Depression scale
CIRS-G = Cumulative Illness Rating Scale - Geriatrics
LOT-R = Life Orientation Test – Revised
MoCA = Montreal Cognitive Assessment
PHQ-9 = Patient Health Questionnaire – 9-item Depression Module
PROMIS = Patient-Reported Outcomes Measurement Information System
PSS = Perceived Stress Scale
SAGE = Successful AGing Evaluation study
SCS = Self-Compassion Scale
SD = standard deviation
SD-WISE = San Diego Wisdom Scale
SF-36 = Short Form – 36-item scale
SPPB = Short Physical Performance Battery
SSI = Social Support Inventory
TICS-m = Telephone Interview for Cognitive Status
TUG = Timed Up and Go
UPSA-B = UCSD Performance-based Skills Assessment - Brief
UCLA-3 = UCLA-3 scale for loneliness
Computation of the Composite Domain Measures of Cognitive, Physical, and Mental Health:
Although missingness of values for most measures was low (20% or less), we performed multiple imputation to avoid listwise deletion in some regressions. The maximum number of computations was set at 20.
Cognitive function:
The MoCA and UPSA-B scores were positively correlated (rs = 0.54, p<0.001), thus PCA could be used to reduce the number of dimensions from 2 to 1. Higher scores on these two scales indicate better functioning. The first principal component (PC1) explained 76.1% of the information on MoCA and UPSA-B, and it had high loadings from both with the same directional effects. The second factor representing the contributions from the MoCA and UPSA-B contained 23.9% of the total information. The cognitive composite measure was a linear combination of MoCA and UPSA-B scores.
Physical health:
The SPPB and TUG scores were negatively correlated (rs = −0.76, p <0.001), thus PCA could be used to reduce the number of dimensions from 2 to 1. (Higher scores on SPPB and lower scores on TUG reflect better physical functioning.) The first principal component (PC1) explained 85.2% of the information on SPPB and TUG, indicating that PC1 mainly represented the difference in the effects of SPPB and TUG. The second PC mainly represented additive effects of SPPB and TUG; it contained 14.8% of the total information. The physical composite score was a linear combination of SPPB and TUG scores.
Mental health:
As reported previously for the SAGE study, the mental health composite score was computed by standardizing total scores of three positive and three negative psychological attributes, calculating the average value (with negative attributes weighted by −1), and then standardizing the outcome (11). The three measures reflecting positive attributes included the Satisfaction with Life Scale (23), Happiness Subscale of CES-D (24), and SF-36 mental health component (20). The three negative attributes included the BSI Anxiety Scale (26), PHQ-9 depression scale (27), and the Perceived Stress Scale (28). The internal consistency of the mental health composite score has been shown to be high (α=0.78), with variance being dominated by a general factor (ωh=0.87).
We examined correlations among the three composite domain measures (Figure 1). There were significant positive correlations between cognitive and physical health (rs = 0.26, p =0.01), and between physical and mental health composite scores (rs = 0.34, p <0.001). There was, however, no significant correlation between the cognitive and mental health composite scores (rs = 0.13, p = 0.22).
Figure 1: Relationship Among the Three Composite Measures of Health: Components and Putative Predictive Factors.
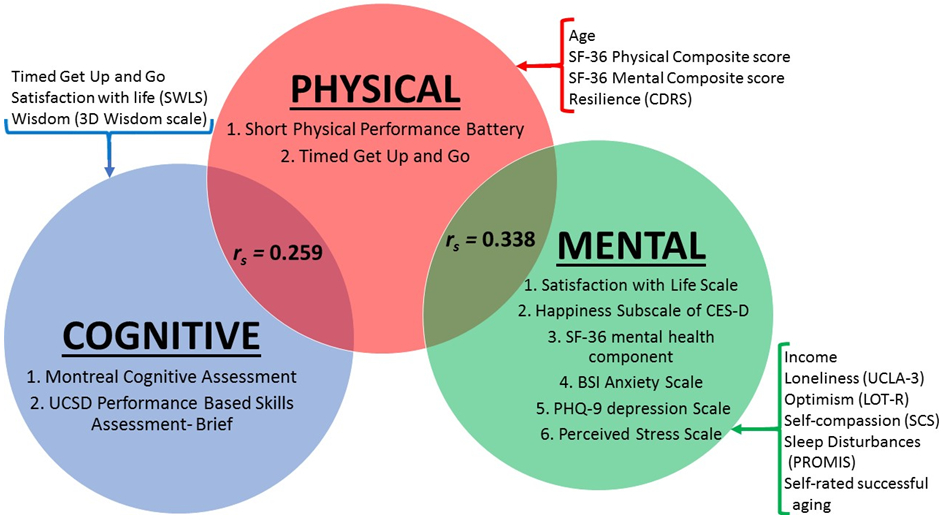
Note: Please see the text for the computation of the three composite measures. Components of each composite measure are shown inside the circles.
Putative predictors of each component are shown outside the circles.
Abbreviations:
BSI = Brief Symptom Inventory Anxiety Scale
CDRS = Connor-Davidson Resilience Scale
CES-D = Center for Epidemiological Studies – Depression scale
PHQ-9 = Patient Health Questionnaire – 9-item Depression Module
PROMIS = Patient-Reported Outcomes Measurement Information System
rs = Spearman’s r
SCS = Self-rated Compassion Scale (Neff)
SF-36 = Short-Form 36 item scale
SWLS = Satisfaction with Life Scale
UCLA-3 = UCLA-3 scale for loneliness
Results of Linear Regression Analysis on the Association of the 3 Composite Domain Measures with Putative Risk or Protective Factors:
Cognitive function:
Higher cognitive composite scores were significantly associated with better lower extremity function and mobility (TUG test), lower satisfaction with life and greater levels of wisdom, and VIF value was less than 1.1, suggesting that collinearity was minimal (Table 2).
Table 2:
: Linear Regression Analysis (Backward Selection): Significant Correlates of Cognitive Composite score (df = 93)
| B | SE | t | p | η2 | |
|---|---|---|---|---|---|
| Intercept | −1.01 | 1.50 | −0.73 | ||
| Mobility (TUG) | −0.10 | 0.03 | −2.95 | 0.004 | 0.88 |
| Satisfaction with life (SWLS) | −0.06 | 0.02 | −2.47 | 0.02 | 0.003 |
| Wisdom (SD-WISE) | 0.98 | 0.36 | 2.74 | 0.007 | <0.001 |
Cronbach’s alpha of Cognitive Composite Score = 0.46 with 95% CI [0.37 ,0.56]
Omega of Cognitive Composite Score =0.73
Spearman’s r between MoCA & UPSA: 0.5369 with p-value < 0.0001.
F(df =3,93) = 6.99, p < 0.001. Adjusted R2 of model = 0.16
Abbreviations:
SD-WISE = San Diego Wisdom Scale
SWLS = Satisfaction with Life Scale
TUG = Timed Up and Go
Physical Health:
Higher physical composite scores were significantly associated with older age, higher self-rated physical functioning, higher mental well-being, and greater resilience; VIF values were all less than 1.2, suggesting that collinearity was minimal (Table 3).
Table 3:
Linear Regression Analysis (Backward Selection): Significant Correlates of Physical Composite score (df = 92)
| B | SE | t | p | η2 | |
|---|---|---|---|---|---|
| Intercept | −1.33 | 1.93 | −0.69 | ||
| Age | 0.04 | 0.02 | −2.46 | 0.02 | 0.10 |
| Physical well-being (SF-36) | 0.04 | 0.01 | 3.70 | <0.001 | 0.11 |
| Mental well-being (SF-36) | 0.03 | 0.01 | 2.36 | 0.02 | 0.07 |
| Resilience (CDRS) | 0.05 | 0.02 | 2.20 | 0.03 | 0.04 |
Cronbach’s alpha of Physical Composite Score = 0.85 with 95% CI [0.8 ,0.91]
Omega of Physical Composite Score =0.87
Spearman’s r between SPPB & TUG: −0.7559 with p-value < 0.0001.
F(df = 4,92) = 10.9, p < 0.001. Adjusted R2 of model = 0.29
Abbreviations:
CDRS = Connor-Davidson resilience scale
SF-36 = Short Form – 36-item scale
Mental Health:
Higher mental health composite scores were significantly associated with higher personal income, higher optimism and self-compassion, lower levels of loneliness and sleep disturbances, and better self-rated successful aging; VIF values were all below 1.3, suggesting that collinearity was minimal (Table 4.)
Table 4:
Linear Regression Analysis (Backward Selection): Significant Correlates of Mental Health Composite Score (df = 89)
| B | SE | t | p | η2 | |
|---|---|---|---|---|---|
| Intercept | −3.00 | 1.07 | −2.82 | ||
| Income* | 0.55 | 0.16 | 3.40 | 0.001 | 0.099† |
| Income** | 0.33 | 0.18 | 1.85 | 0.07 | |
| Sleep Disturbances (PROMIS) | −0.03 | 0.01 | −3.13 | 0.002 | 0.04 |
| Optimism (LOTR) | 0.09 | 0.02 | 4.38 | <0.001 | 0.04 |
| Self-Compassion (Neff SCS) | 0.03 | 0.01 | 2.54 | 0.01 | 0.006 |
| Loneliness (UCLA-3) | −0.02 | 0.01 | −2.61 | 0.01 | 0.005 |
| Self-rated successful aging | 0.17 | 0.05 | 3.07 | 0.002 | 0.04 |
Comparison of middle tier of income with lowest tier
Comparison of highest tier of income with lowest tier
For income variable as a whole
Cronbach’s alpha of Mental Health Composite Score = 0.78 with 95% CI [0.73 ,0.84]
Omega of Mental Health Composite Score =0.87
F(df = 7, 89) = 22.4, p < 0.001. Adjusted R2 of model = 0.61
Abbreviations:
CDRS = Connor-Davidson resilience scale
LOTR = Life Orientation Test – Revised
PROMIS = Patient-Reported Outcomes Measurement Information System
SCS = Self-Compassion Scale
UCLA-3 = UCLA-3 scale for loneliness
Discussion and Implications
The CCSHC group had fewer racial/ethnic minority participants and higher level of education than a randomly selected and age- and sex-comparable sample of older adults from the same metropolitan area (SAGE study); yet, the two groups did not differ significantly from each other on most of the other self-reported health measures, with just a few exceptions. The CCSHC sample had higher BMI, lower optimism and self-compassion, and greater loneliness - factors that might be associated with the decision to move into the supporting environment of a CCSHC, although the cross-sectional nature of our data does not permit us to make causal interpretations. The greater number of cognitively stimulating activities in the CCSHC likely reflect on the various social activities common that setting. The lack of significant differences between the two groups on most of the other self-reported health measures suggests that our results may be generalizable to the diverse community at large.
Of the three composite health domains (cognitive, physical, and mental), the physical health measure was significantly related to the other two. Absence of a significant relationship between cognitive function and mental health needs further exploration. Several studies have reported that depression, anxiety, and stress are associated with impaired cognitive functioning (39). Nonetheless, it is worth noting that the effect sizes of the significant associations between physical health and cognitive or mental health were small (rs ~0.3), suggesting that these three principal domains of health are partially independent from one another and require separate evaluations.
In terms of statistical “predictors” of these components, psychosocial factors were associated with all the health domains (satisfaction with life and wisdom with cognitive health; mental well-being and resilience with physical health; and optimism, self-compassion, loneliness and self-rated successful aging with mental health.) Additionally, physical mobility (TUG) was associated with cognitive health, age and subjective physical well-being with physical health, and personal income and sleep quality with mental health.
There has been growing literature reporting on a positive impact of resilience and adverse effects of loneliness on health (40). Resilience has been linked with positive health-related behaviors (e.g., adherence to self-care routines, psychiatric treatment, and exercise) as well as better mental and physical health outcomes. We and others have shown that resilience may buffer some of the adverse health effects of negative influences like childhood trauma (41). Conversely, loneliness has been associated with negative mental and physical health outcomes including depression, hopelessness, substance use, cognitive impairment, malnutrition, hypertension, disrupted sleep, and frailty (42). Distinct from objective social network size, loneliness describes the distress stemming from a discrepancy between perceived and desired social relationships (42). The Irish Longitudinal Study on Ageing (TILDA) reported a longitudinal association between experiencing loneliness and a higher risk of developing depressive and anxiety disorders two years later (43). Attention to loneliness in the United Kingdom has extended to the government-level, including the creation of a Ministry of Loneliness.
Correlated with cognitive health, wisdom is a complex human trait with several components- i.e., emotional regulation, self-reflection, pro-social behaviors such as empathy and compassion, decisiveness, social advising, tolerance of divergent values, and spirituality (44, 45). Wisdom may increase with age (46), and has been linked to enhanced physical (47) and mental health (48). Interestingly, our study found wisdom to be associated significantly with cognitive health, which may be related to cognitive aspects of wisdom (decisiveness, knowledge) and the importance of well-being to cognitive health.
The influence of psychosocial factors on mental health has been well established. Optimism has been shown to be an important inverse predictor of depression (49). Self-compassion is protective against development of mental health problems in older adults (50). Self-rated successful aging has been associated with better mental well-being (SF-36) (51). Interestingly, higher satisfaction with life was associated with lower cognitive health, which may seem counterintuitive. However, Ihle et al. showed in a study of over 3,000 older adults that the link between poor cognitive abilities and lower well-being were moderated by greater cognitive reserve and social support (52). The sample in the current study was highly educated and it is possible that social supports buffered the cognition-well-being link. In addition, Wilson et al. have shown that lower cognition has differential impact on various aspects of well-being, e.g., purpose versus self-acceptance (53).
The linkage between cognitive and physical functioning in older adults has long been recognized (54). Cognitive and physical decline may go hand in hand, representing a global decline in health status; it is also possible that decline in one domain may be a leading indicator of more global decline. Interventions to improve physical activity have salutary effects on cognition in multiple populations (55); it is not known if cognitive interventions could also improve physical health.
Throughout the lifespan, and in particular among older adults, sleep disturbances are linked with worse mental health including anxiety, depression, and suicidal behaviors (56). Furthermore, aging itself is associated with increased sleep disturbances. Older individuals have higher rates of insomnia and other sleep disorders, as well as more frequent sleep disturbances (e.g., lower sleep efficiency) and shorter overall sleep time (57). Thus, sleep is an important component of health in older adults.
Aging is a well-established risk factor for physical and cognitive decline. However, our study did not find a significant relationship between age and cognitive health composite scores, after controlling for other variables. The age range among the study participants was restricted to 65-95 years. Furthermore, all the participants were living independently in a CCSHC. Due to the demands of living independently, these participants may be more similar in their levels of cognitive functioning in this cross-sectional assessment, despite the variations in age. It is possible that the individual participants’ trajectories of cognitive functioning will vary widely, if they are followed longitudinally.
This study has several strengths, including comprehensive cognitive, physical, and mental health evaluations using standardized and validated rating scales, specific assessment of psychosocial factors such as resilience, social support, and loneliness, and comparison with an age- and sex-matched group of community-dwelling subjects selected using random digit dialling (the SAGE cohort). We developed composite measures for all three main health outcomes, which are likely to be more reliable and valid than single tests or scales. Furthermore, we employed objective measures of cognitive (MoCA and UPSA-B) and physical (SPPB and TUG) health to compute composite measures of those two health domains. (Mental health is, by definition, subjective.) We adjusted for age and sex in all regression models exploring the effects of other potential risk and protective factors. Finally, this is one of the few studies of senior housing residents from a geriatric psychiatry perspective that focuses on health in a broad sense and not only on putative risk factors that need to be mitigated but also on potential protective factors that need to be enhanced.
There are also several limitations to this investigation. The cross-sectional nature of these data precludes demonstration of causal relationships among specific variables. We are planning to follow our study participants longitudinally to assess health outcomes along with risk and protective factors over time. The study sample consisted predominately of well-educated White participants from middle and upper socioeconomic strata, and the results may not apply to socioeconomically disadvantaged or racial/ethnic minority groups. Although we compared our sample to the ethnically diverse SAGE sample, the latter did not have in-person assessment measures such as UPSA-B, SPPB, and TUG. Another limitation was that the cognitive measure was broad and might have missed more subtle impairments, compared to a comprehensive neuropsychological test battery. We did not include neuroimaging, blood-based biomarkers of aging, or anticholinergic burden from medications. Our findings may not apply to people with disabilities or those in assisted living settings. Finally, any study of older adults inevitably involves healthy survivor bias as well as birth cohort bias, meaning that the results may not generalize to younger or middle-aged adults.
Clinical Implications
This cross-sectional study suggests that some psychosocial factors are related to every domain of health, i.e., cognitive, physical, and mental. Larger and longitudinal studies in diverse samples of older adults are necessary to determine if these variables constitute potential risk or protective factors related to cognitive, physical, or mental disabilities. Such data would pave the way for developing new interventions. A growing body of research already supports the use of mind-body therapies (e.g., tai-chi, yoga, walking meditation) as minimally invasive and effective approaches for the management of late-life mood and cognitive disorders (58).
With the national healthcare system in flux, especially for older adults, new models of healthcare will be tested. We propose that CCSHCs may be a good model for future clinical research, allowing for assessment of individuals and their environment as well as their response to interventions. The number of senior housing or retirement communities is likely to continue its rapid growth. Partnerships between senior housing communities and academic/industry researchers will foster pragmatic trials with appropriate study designs and meaningful outcome measures, including healthcare economics. Future CCSHCs will be expected to implement evidence-based strategies that facilitate healthy aging, including healthy diet, physical and cognitive activity, social engagement, stress reduction, sleep hygiene, and regular healthcare. Technology-enabled solutions in senior housing may be needed for addressing residents’ healthcare coordination and promoting healthy lifestyle (59).
Highlights.
1. What is the primary question addressed by this study?
This study examined sociodemographic and clinical associations of cognitive, physical, and mental health in a sample of older adults in the independent living sector of a continuing care senior housing community.
2. What is the main finding of this study?
Physical health was correlated with both cognitive and mental health, but there was no significant correlation between cognitive and mental health. Psychosocial factors (satisfaction with life, wisdom, mental well-being, resilience, optimism, self-compassion, and loneliness) were associated with one of the three health domains. Additionally, physical mobility was associated with cognitive health, age and self-rated physical functioning were associated with physical health, and income and sleep disturbances were associated with mental health.
3. What is the meaning of the finding?
Longitudinal studies in diverse samples of older adults are necessary to determine if the above-mentioned psychosocial and other variables are potential risk or protective factors related to cognitive, physical, or mental health and diseases. The eventual goal would be to develop new health-focused interventions. Continuing care senior housing communities are important sites for studying and promoting health in older adults.
Acknowledgments
FUNDING
This study was supported, in part, by the IBM Research AI through the AI Horizons Network, the National Institutes of Health (grant R01MH094151-01 to DVJ [PI]), the National Institute of Mental Health T32 Geriatric Mental Health Program (grant MH019934 to DVJ [PI]), the National Institutes of Health (grant UL1TR001442 of CTSA funding; PI: Gary Firestein), and the Sam and Rose Stein Institute for Research on Aging at the University of California San Diego. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
CONFLICT OF INTEREST STATEMENT
The authors report no conflict of interest regarding this study.
REFERENCES
- 1.Ortman JM, Velkoff VA,Hogan H: An aging nation: the older population in the United States, United States Census Bureau, Economics and Statistics Administration, US Department of Commerce, 2014 [Google Scholar]
- 2.Administration on Aging: Projected future growth of the older population. A profile of older Americans, 2015
- 3.Cooper C, Bebbington P, Lindesay J, et al. : The meaning of reporting forgetfulness: a cross-sectional study of adults in the English 2007 Adult Psychiatric Morbidity Survey. Age Ageing 2011; 40:711–717 [DOI] [PubMed] [Google Scholar]
- 4.Jeste D,Childers J: Strategic Planning for Transformative Senior Living: Developing Tomorrow’s Leadership and Workforce. Seniors Housing & Care Journal 2017; 25:113–126 [Google Scholar]
- 5.Zarem JE: Today’s Continuing Care Retirement Community (CCRC), CCRC Task Force, Am Seniors Hous Assoc, 2010 [Google Scholar]
- 6.Bragg BE,Hansen JC: A Revelation of Numbers : Will America’s Eldercare Workforce be Ready to Care for an Aging America? Generations 2011; 34:11–20 [Google Scholar]
- 7.World Health Organization: Health systems that meet the needs of older people, World Health Organization, 2019 [Google Scholar]
- 8.Jeste DV, Blazer DG 2nd, Buckwalter KC, et al. : Age-Friendly Communities Initiative: Public Health Approach to Promoting Successful Aging. Am J Geriatr Psychiatry 2016; 24:1158–1170 [DOI] [PubMed] [Google Scholar]
- 9.American Seniors Housing Association: Residents of Independent Living: How Today’s Residents Compare to Residents of 2001, American Seniors Housing Association, 2013 [Google Scholar]
- 10.Jeste DV, Savla GN, Thompson WK, et al. : Association between older age and more successful aging: Critical role of resilience and depression. American Journal of Psychiatry 2013; 170:188–196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thomas M, Kaufmann C, Palmer B, et al. : Paradoxical trend for improvement in mental health with aging: A community-based study of 1,546 adults aged 21-99 years. Journal Clinical Psychiatry 2016; In Press: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nasreddine ZS, Phillips NA, Bedirian V, et al. : The Montreal Cognitive Assessment, MoCA: A Brief Screening Tool For Mild Cognitive Impairment. Journal of the American Geriatrics Society 2005; 53:695–699 [DOI] [PubMed] [Google Scholar]
- 13.Mausbach BT, Harvey PD, Goldman SR, et al. : Development of a brief scale of everyday functioning in persons with serious mental illness. Schizophr Bull 2007; 33:1364–1372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sweet L, Van Adel M, Metcalf V, et al. : The Montreal Cognitive Assessment (MoCA) in geriatric rehabilitation: psychometric properties and association with rehabilitation outcomes. International Psychogeriatrics 2011; 23:1582–1591 [DOI] [PubMed] [Google Scholar]
- 15.Mausbach BT, Harvey PD, Pulver AE, et al. : Relationship of the Brief UCSD Performance-based Skills Assessment (UPSA-B) to multiple indicators of functioning in people with schizophrenia and bipolar disorder. Bipolar Disorders 2010; 12:45–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.de Jager CA, Budge MM,Clarke R: Utility of TICS-M for the assessment of cognitive function in older adults. International Journal of Geriatric Psychiatry 2003; 18:318–324 [DOI] [PubMed] [Google Scholar]
- 17.Guralnik JM, Simonsick EM, Ferrucci L, et al. : A Short Physical Performance Battery Assessing Lower Extremity Function: Association With Self-Reported Disability and Prediction of Mortality and Nursing Home Admission. J. Gerontol 1994; 49:M85–M94 [DOI] [PubMed] [Google Scholar]
- 18.Podsiadlo D,Richardson S: The Timed “Up & Go”: A Test of Basic Functional Mobility for Frail Elderly Persons. Journal of the American Geriatrics Society 1991; 39:142–148 [DOI] [PubMed] [Google Scholar]
- 19.Guralnik JM, Ferrucci L, Pieper CF, et al. : Lower Extremity Function and Subsequent Disability: Consistency Across Studies, Predictive Models, and Value of Gait Speed Alone Compared With the Short Physical Performance Battery. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 2000; 55:M221–M231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ware JE,Sherbourne CD: The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992; 30:473–483 [PubMed] [Google Scholar]
- 21.Yu L, Buysse DJ, Germain A, et al. : Development of short forms from the PROMIS sleep disturbance and Sleep-Related Impairment item banks. Behavioral sleep medicine 2011; 10:6–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Parmelee PA, Thuras PD, Katz IR, et al. : Validation of the Cumulative Illness Rating Scale in a Geriatric Residential Population. Journal of the American Geriatrics Society 1995; 43:130–137 [DOI] [PubMed] [Google Scholar]
- 23.Diener E, Emmons RA, Larsen RJ, et al. : The satisfaction with life scale. Journal of Personality Assessment 1985; 49:71–75 [DOI] [PubMed] [Google Scholar]
- 24.Fowler JH,Christakis NA: Dynamic spread of happiness in a large social network: longitudinal analysis over 20 years in the Framingham Heart Study. BMJ (Clinical Research Ed.) 2008; 337:a2338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Andresen EM, Malmgren JA, Carter WB, et al. : Screening for depression in well older adults: evaluation of. Prev Med 1994; 10:77–84 [PubMed] [Google Scholar]
- 26.Derogatis LR,Spencer P: Brief symptom inventory: BSI, Pearson; Upper Saddle River, NJ:, 1993 [Google Scholar]
- 27.Kroenke K, Spitzer RL,Williams JB: The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16:606–613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cohen S, Kamarck T,Mermelstein R: A global measure of perceived stress. Journal of Health and Social Behavior 1983; 385–396 [PubMed] [Google Scholar]
- 29.Campbell-Sills L,Stein MB: Psychometric analysis and refinement of the connor-davidson resilience scale (CD-RISC): Validation of a 10-item measure of resilience. Journal of Traumatic Stress 2007; 20:1019–1028 [DOI] [PubMed] [Google Scholar]
- 30.Scheier MF, Carver CS,Bridges MW: Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. Journal of personality and social psychology 1994; 67:1063–1078 [DOI] [PubMed] [Google Scholar]
- 31.Neff KD: The development and validation of a scale to measure self-compassion. Self and Identity 2003; 2:223–250 [Google Scholar]
- 32.Russell DW: UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J Pers Assess 1996; 66:20–40 [DOI] [PubMed] [Google Scholar]
- 33.McCubbin HI, Patterson J,Glynn T: Social Support Index (SSI), in Family Assessment Resiliency, Coping and Adaptation Inventories for Research and Practice. Edited by McCubbin HI, Thompson AI,McCubbin MA. Madison, WI, University of Wisconsin, 1996, pp 357–389 [Google Scholar]
- 34.Fetzer Institute: Multidimensional measurement of religiousness/ spirituality for use in health research, Bethesda, MD, Fetzer Institute, 1999 [Google Scholar]
- 35.Revelle W,Zinbarg RE: Coefficients alpha, beta, omega, and the glb: Comments on Sijtsma. Psychometrika 2009; 74:145–154 [Google Scholar]
- 36.Chen T, Wu P, Tang W, et al. : Variable selection for distribution-free models for longitudinal zero-inflated count responses. Stat Med 2016; 35:2770–2785 [DOI] [PubMed] [Google Scholar]
- 37.Seber G,Lee A: Linear Regression Analysis, 2nd Hoboken, NJ, John Wiley & Sons, Inc., 2003 [Google Scholar]
- 38.Wang H, Peng J, Wang B, et al. : Inconsistency between univariate and multiple logistic regressions. Shanghai Arch Psychiatry 2017; 29:124–128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kassem AM, Ganguli M, Yaffe K, et al. : Anxiety symptoms and risk of cognitive decline in older community-dwelling men. International Psychogeriatrics 2017; 29:1137–1145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee EE, Depp C, Palmer BW, et al. : High prevalence and adverse health effects of loneliness in community-dwelling adults across the lifespan: role of wisdom as a protective factor. Int Psychogeriatr 2018; 1–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lee EE, Martin AS, Tu X, et al. : Childhood Adversity and Schizophrenia: The Protective Role of Resilience in Mental and Physical Health and Metabolic Markers. J Clin Psychiatry 2018; 79: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cacioppo JT, Hawkley LC, Crawford LE, et al. : Loneliness and health: potential mechanisms. Psychosom Med 2002; 64:407–417 [DOI] [PubMed] [Google Scholar]
- 43.Domenech-Abella J, Mundo J, Haro JM, et al. : Anxiety, depression, loneliness and social network in the elderly: Longitudinal associations from The Irish Longitudinal Study on Ageing (TILDA). J Affect Disord 2019; 246:82–88 [DOI] [PubMed] [Google Scholar]
- 44.Meeks TW,Jeste DV: Neurobiology of wisdom: a literature overview. Arch Gen Psychiatry 2009; 66:355–365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jeste D,Lee EE: Emerging Empirical Science of Wisdom: Definition, Measurement, Neurobiology, Longevity, and Interventions. Harvard Review of Psychiatry 2018; In Press: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Happé FGE, Winner E,Brownell H: The getting of wisdom: Theory of mind in old age. Developmental Psychology 1998; 34:358–362 [DOI] [PubMed] [Google Scholar]
- 47.Ardelt M: Antecedents and Effects of Wisdom in Old Age. Research on Aging 2000; 22:360–394 [Google Scholar]
- 48.Thomas ML, Bangen KJ, Palmer BW, et al. : A new scale for assessing wisdom based on common domains and a neurobiological model: The San Diego Wisdom Scale (SD-WISE). Journal of Psychiatric Research 2019; 108:40–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Giltay EJ, Zitman FG,Kromhout D: Dispositional optimism and the risk of depressive symptoms during 15 years of follow-up: the Zutphen Elderly Study. J Affect Disord 2006; 91:45–52 [DOI] [PubMed] [Google Scholar]
- 50.Kim C,Ko H: The impact of self-compassion on mental health, sleep, quality of life and life satisfaction among older adults. Geriatric nursing (New York, N.Y.) 2018; 39:623–628 [DOI] [PubMed] [Google Scholar]
- 51.Montross LP, Depp C, Daly J, et al. : Correlates of self-rated successful aging among community-dwelling older adults. Am J Geriatr Psychiatry 2006; 14:43–51 [DOI] [PubMed] [Google Scholar]
- 52.Ihle A, Oris M, Sauter J, et al. : The relation of low cognitive abilities to low well-being in old age is attenuated in individuals with greater cognitive reserve and greater social capital accumulated over the life course. Aging Ment Health 2018; 1–8 [DOI] [PubMed] [Google Scholar]
- 53.Wilson RS, Boyle PA, Segawa E, et al. : The influence of cognitive decline on well-being in old age. Psychol Aging 2013; 28:304–313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Verghese J, Wang C, Lipton RB, et al. : Quantitative gait dysfunction and risk of cognitive decline and dementia. Journal of Neurology, Neurosurgery & Psychiatry 2007; 78:929–935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Groot C, Hooghiemstra AM, Raijmakers PG, et al. : The effect of physical activity on cognitive function in patients with dementia: A meta-analysis of randomized control trials. Ageing research reviews 2016; 25:13–23 [DOI] [PubMed] [Google Scholar]
- 56.Nadorff MR, Drapeau CW,Pigeon WR: Psychiatric Illness and Sleep in Older Adults: Comorbidity and Opportunities for Intervention. Sleep medicine clinics 2018; 13:81–91 [DOI] [PubMed] [Google Scholar]
- 57.Reynolds CF 3rd,O’Hara R: DSM-5 sleep-wake disorders classification: overview for use in clinical practice. Am J Psychiatry 2013; 170:1099–1101 [DOI] [PubMed] [Google Scholar]
- 58.Laird KT, Paholpak P, Roman M, et al. : Mind-Body Therapies for Late-Life Mental and Cognitive Health. Curr Psychiatry Rep 2018; 20:2. [DOI] [PubMed] [Google Scholar]
- 59.Rosenberg D, Depp CA, Vahia IV, et al. : Exergames for subsyndromal depression in older adults: a pilot study of a novel intervention. Am J Geriatr Psychiatry 2010; 18:221–226 [DOI] [PMC free article] [PubMed] [Google Scholar]


