Abstract
Pulmonary complications (PC) of hematologic malignancies and their treatments are common causes of morbidity and mortality. Early diagnosis is challenging due to host risk factors, clinical instability, and provider preference. Delayed diagnosis impairs targeted treatment and may contribute to poor outcomes. An integrated understanding of clinical risk and radiographic patterns informs a timely approach to diagnosis and treatment. There is little prospective evidence guiding optimal modality and timing of minimally invasive lung sampling; however, a low threshold for diagnostic bronchoscopy during the first 24 to 72 hours after presentation should be a guiding principle in high-risk patients.
Keywords: Pulmonary complications, Lung infiltrates, Hematopoietic cell transplant, Hematologic malignancy, Diagnosis, Pneumonia, Bronchoscopy
Key points
-
•
Patients with hematologic malignancies and recipients of hematopoietic cell transplantation are highly susceptible to pulmonary complications.
-
•
Early diagnosis of pulmonary complications is challenging. Delayed diagnosis limits opportunity for targeted treatment, and may contribute to poor outcomes, including mortality.
-
•
An integrated clinicoradiologic approach to diagnosing pulmonary complications provides some insight into their nature, and guides the risk/benefit assessment in pursuing lung sampling.
-
•
Diagnostic bronchoscopy should be considered promptly in these immunocompromised populations, especially in the presence of high-risk features, such as neutropenia and posttransplant status.
Introduction
Pulmonary complications (PC) of hematologic malignancies (HM) and their treatments, including hematopoietic cell transplantation (HCT), are common causes of morbidity and mortality.1, 2 Despite advances in management,3 these patients remain highly susceptible to lung injury involving one or more anatomic compartments of the lower respiratory tract (LRT), especially the lung parenchyma. Vulnerability to parenchymal PCs is multifactorial, determined largely by the type, magnitude, and duration of impaired immune defense.4 This risk is compounded further by treatment-related toxicities, complex comorbidities, and recurrent nosocomial exposures.
Patients at greatest risk for infectious PCs include those with prolonged neutropenia5 and recipients of HCT.6 Infectious and noninfectious parenchymal PCs occur in up to 70% of allogeneic HCT patients1 (25% after autologous HCT7), frequently in the acute setting,8 and represent the most common cause for admission to the intensive care unit.9 PCs significantly increase mortality, both during treatment (eg, during induction therapy for acute leukemias10) and in later periods, after HCT.1, 11 This predisposition requires clinical vigilance in the formulation of a differential diagnosis, in performing prompt diagnostic investigations, and in the initiation of treatment.
In practice, a specific cause of pulmonary disease is frequently undiagnosed ante mortem in this population.12, 13, 14 An elusive understanding of disease mechanisms, notably inflammatory HCT-related PCs, may contribute to this disparity. However, the lack of a diagnosis also reflects delayed, if not altogether deferred, diagnostic sampling of the LRT in the setting of excessive patient risk and/or provider preference. It has been suggested that diagnostic uncertainty regarding PCs may impact mortality after HCT.15, 16 Difficulty obtaining a timely diagnosis naturally interferes with the clinician’s ability to target treatment, leading to prolonged empirical management of many PCs. With the institution of these broad therapies come exposures to unnecessary toxicities, ripe conditions for the emergence of antibiotic resistance, and possibly the acceleration of poor outcomes.
Given the incidence of acute and often fatal PCs in this highly immunocompromised population, a comprehensive approach to the diagnostic evaluation of PCs in HM and HCT patients is essential. The integration of information regarding high-risk host features, abnormal chest imaging patterns, and noninvasive test results informs decisions to pursue lung sampling via minimally invasive techniques, such as fiberoptic bronchoscopy (FOB), or other modalities. The goal of this paper is to provide an overview of the considerations and practices in the diagnostic approach to the adult HM and HCT patient with respiratory signs and symptoms, with a focus on investigating PCs involving the lung parenchyma.
Diagnostic approach
Context
An initial survey of the clinical landscape is essential to ascertain PC risk and to determine subsequent diagnostic steps. Timing of presentation, host characteristics, immune deficits, treatment-related factors, and past exposures may each impact the risk/benefit equation for LRT sampling in an HM or HCT patient with new pulmonary infiltrates on chest imaging. The identification of high-risk features (eg, prolonged neutropenia or known mold exposure) may also raise suspicion of a specific disease entity (eg, invasive fungal infection), early enough to expedite lung sampling while initiating presumptive therapy.
Immune defects
Understanding the timing of respiratory symptom onset relative to immunosuppressive treatments17 can help to narrow the differential diagnosis of PCs. Defects in innate, cell-mediated, and humoral immunity, as well as splenic defects, each predispose to infection by specific organisms18 (Table 1 ). Neutropenia is the most common individual risk factor for cancer-related pneumonia, and a greater than 20% risk of febrile neutropenia (FN) can be expected with specific chemotherapy regimens for many types of HM.19 The underlying HM may also exacerbate treatment-related deficits in cell function,20 albeit less predictably.
Table 1.
Immune defects and associated pathogens in hematologic malignancies and HCT
| Immune Impairment | Potential Causes | Spectrum of Respiratory Infections |
|---|---|---|
| Neutrophil number/function | Leukemia Lymphoma Myelodysplastic syndrome Cytoreductive therapies Corticosteroids Hematopoietic stem cell transplant |
Gram-negative bacilli Gram-positive cocci Invasive molds (eg, Aspergillus spp, Mucorales, Fusarium, Scedosporium) |
| T lymphocytes |
|
Intracellular bacteria (eg, Nocardia, mycobacteria, legionella) Viruses (eg, respiratory viruses, latent Herpesviridae) Fungi (eg, Pneumocystis jirovecii, Cryptococcus spp, Histoplasma capsulatum, Coccidioides spp, Aspergillus spp, Micorales, Fusarium, Scedosporium) Parasites (eg, Strongyloides spp, Toxoplasma spp) |
| B lymphocytes and humoral immunity | Leukemia Multiple myeloma Anti–B-cell antibodies Splenectomy Plasmapheresis Drugs |
Encapsulated bacterial (eg, Pneumococcus, H influenza) Mycoplasma spp |
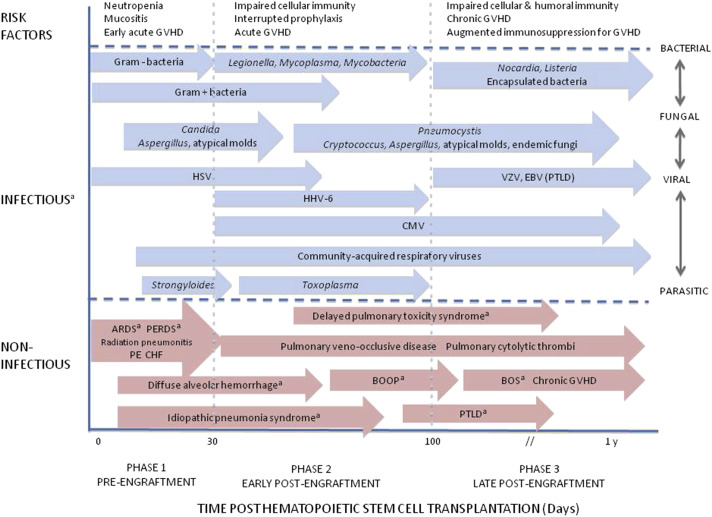
Recipients of HCTs have additional treatment-related risk factors for PCs, including intensity of the conditioning regimen, stem cell source, prolonged cytopenias, and intensified immunosuppression for graft-versus-host disease.1, 6 Pretransplant conditioning confers a shared susceptibility to PCs both before and after engraftment6 (Fig. 1 ). Preengraftment PCs are usually infectious and occur within 30 days of HCT. These commonly include Gram-negative bacterial pneumonias in the setting of neutropenia and/or mucositis. Early postengraftment PCs, which occur between days 30 and 100, typically include infectious processes associated with impaired cellular immunity. Late- postengraftment PCs tend to develop after day 100, typically after immune reconstitution. Atypical processes may occur outside of these expected windows based on additional host risk factors (eg, opportunistic infection late after engraftment in the setting of delayed antibody response21). PCs occurring before engraftment, which are predominantly infectious, are associated with significantly lower mortality compared with those that develop later.1
Fig. 1.
Infectious and noninfectious pulmonary complications of hematopoietic cell transplantation. ARDS, acute respiratory distress syndrome; BOOP, bronchiolitis obliterans organizing pneumonia; BOS, bronchiolitis obliterans syndrome; CHF, congestive heart failure; CMV, cytomegalovirus; EBV, Epstein–Barr virus; GVHD, graft-versus-host disease; HHV-6, human herpes virus-6; HSV, herpes simplex virus; PE, pulmonary embolism; PERDS, periengraftment respiratory distress syndrome; PTLD, posttransplant lymphoproliferative disorder; VZV, varicella zoster virus. a Consider diagnostic bronchoscopy to (1) establish or rule out an infectious etiology, and/or (2) diagnose a noninfectious etiology for the pulmonary complication.
(Reproduced from Harris B, Lowy FD, Stover DE, et al. Diagnostic bronchoscopy in solid-organ and hematopoietic stem cell transplantation. Ann Am Thorac Soc 2013;10(1):41; with permission.)
It is more difficult to predict the timing of noninfectious PCs after HCT. A spectrum of acute lung injury syndromes may parallel endothelial damage that can occur at other organ sites (eg, the liver) early after HCT.2, 22 Preengraftment syndrome and diffuse alveolar hemorrhage develop soon after allogeneic or autologous HCT, whereas idiopathic pneumonia syndrome occurs somewhat later, albeit during the first 100 days after allogenic HCT. Although these processes are variably steroid responsive, both diffuse alveolar hemorrhage and idiopathic pneumonia syndrome are associated with high mortality,23, 24 and mortality after preengraftment syndrome tends to be significantly less.25 Of note, acute respiratory distress syndrome in HCT subjects is most often associated with an infectious etiology, and carries a very high mortality in the setting of invasive fungal disease.26 Thus, early recognition and appropriate intervention for both infectious and noninfectious transplant-related PCs is imperative to successful outcomes.
Risk factors
The medical histories of HM and HCT patients are among the most complex, representing unique disease chronologies, treatment courses/responses, and comorbidities. A history of tobacco smoking10, 27 and conditions such as chronic obstructive pulmonary disease predispose LRT colonization by bacterial pathogens,28 thereby increasing the risk of infectious PCs. The development of mucositis, a common complication of myeloablative chemotherapies, may impair airway clearance and nutritional intake, thereby increasing the risk of pneumonia and bacteremic events.29 Noninfectious causes of PCs may be suggested by a history of pneumotoxic chemotherapy (eg, bleomycin, alkylating agents, radiation therapy, non–cancer-related medications (eg, amiodarone), and transfusion of blood products. A history of pulmonary disease or cardiac dysfunction may increase risk of drug-related lung toxicities influence the acuity of their presentation.
Pretransplant pulmonary function should be considered in the assessment of PC risk after HCT, in particular. Reduced lung function, as measured by pulmonary function testing, has been associated with severe PCs occurring early after HCT.30 Abnormalities in the diffusing lung capacity for carbon monoxide and the forced expiratory volume in 1 second also contribute to the HCT-Co-morbidity Index, a validated prognostic indicator of posttransplant mortality.31, 32 Ongoing investigations of microbial biomarkers in allogeneic HCT recipients suggest that changes in gut flora, which commonly occur within days of initiating pretransplant conditioning and antimicrobial prophylaxis,33 may increase the likelihood of developing PCs.1 This may occur either via direct translocation of infectious agents, or indirectly via stimulation of an aberrant pulmonary inflammatory response. Importantly, gut microbiota changes and PCs may be significant and independent predictors of transplant-related mortality.1, 33, 34 This finding highlights a need for continued development of tools for identifying at-risk populations.
Exposures
Although many common respiratory tract infections arise from the patient’s own microbial flora, others are contracted through exposure to sick individuals or environmental sources. Eliciting such exposures is important in surveying the landscape for potential infections, both de novo (eg, multidrug-resistant organisms in the hospital setting) and with reactivation of latent infections. Patients should be questioned about travel or residence in areas with exposures to Mycobacterium tuberculosis and endemic fungal organisms, including Histoplasma capsulatum, Coccidioides immitis, Blastomyces dermatitidis, and others. Inquiry regarding exposures to house pets, birds, farm animals, aerosolized water sources, and disturbed soil dust can provide clues to infections caused by diverse organisms, such as Nocardia species (spp), Legionella spp, Toxoplasma gondii, and Cryptococcus neoformans. Immunologic evidence of the patient’s (and donor’s, in the case of allogeneic HCT) history of latent infection with cytomegalovirus, Epstein–Barr virus, T gondii, or M tuberculosis need to be reviewed carefully. These exposures should be kept in mind in considering additional noninvasive or invasive diagnostic investigations to pursue beyond routine testing.
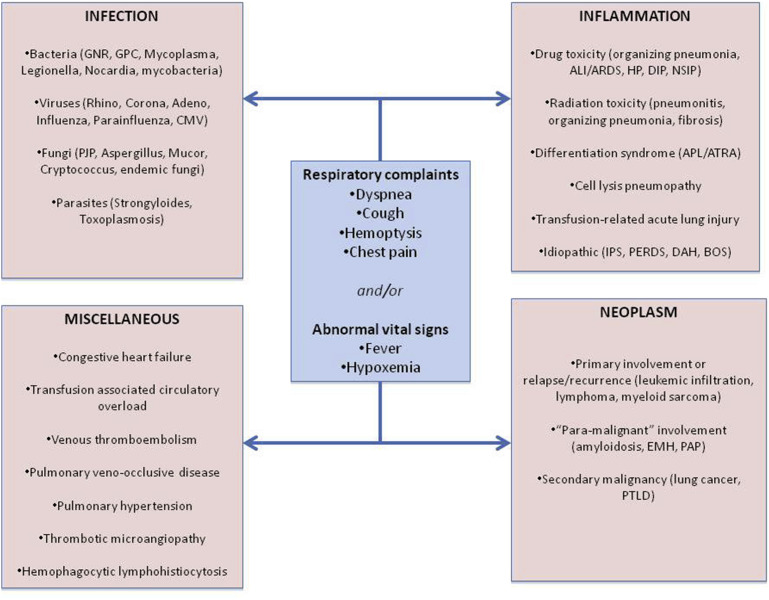
Presentation
PCs can broadly be categorized as infectious, inflammatory, malignant, or “other” (Fig. 2 ). Processes within each group share a common identity based on their predominant pathophysiology, although with some overlap, as in Epstein–Barr virus–related posttransplant lymphoproliferative disorder. The presence of abnormal vital signs (eg, fever, hypoxemia) and respiratory symptoms (eg, dyspnea, cough) does not readily distinguish between PC processes, whose presentations may vary further by underlying HM.35 For example, hemoptysis may suggest alveolar hemorrhage; however, its absence is common in diffuse alveolar hemorrhage. Hypoxemia with an elevated alveolar-arterial gradient may suggest Pneumocystis jirovecii pneumonia as the etiology of patchy ground glass opacities on chest imaging, but further investigation for an alternate explanation, such as pulmonary embolism, may be required if radiographic findings seem out of proportion to the gas exchange abnormality. The acuity of presentation may provide additional insight into the differential diagnosis in the appropriate context; for example, acute hypoxemia and new crackles in the setting of a blood product transfusion may suggest suggestive of transfusion-related acute lung injury or transfusion-associated circulation overload. However, further investigation into the PC cause is indicated more often than not.
Fig. 2.
Spectrum of pulmonary complications in patients with hematologic malignancies and in hematopoietic cell transplant recipients. ALI, acute lung injury; APL, acute promyelocytic leukemia; ARDS, acute respiratory distress syndrome; ATRA, all-trans retinoic acid; BOS, bronchiolitis obliterans syndrome; CMV, cytomegalovirus; DAH, diffuse alveolar hemorrhage; DIP, desquamative interstitial pneumonia; EMH, extramedullary hematopoiesis; GNR, gram-negative rods; GPC, gram-positive cocci; HP, hypersensitivity pneumonitis; IPS, idiopathic pneumonia syndrome; NSIP, nonspecific interstitial pneumonia; PAP, pulmonary alveolar proteinosis; PERDS, periengraftment respiratory distress syndrome; PJP, Pneumocystis jiroveci pneumonia; PTLD, posttransplant lymphoproliferative disease.
Chest Imaging
Modality
Chest imaging is generally obtained for diagnosis of HMs with pulmonary manifestations, and for working up a suspicious sign or unexplained fever during management. The latter indication is common after HCT35 and in the setting of neutropenia, where 15% of patients with FN present with lung infiltrates.36 The distribution and morphology of infiltrates can help to refine the PC differential diagnosis, although a diminished inflammatory response may alter or delay the appearance of typical findings. There are significant limitations to the sensitivity of chest radiographs for diagnosing PCs in HM and HCT patients, even when combined with clinical data.37, 38 In 1 study of febrile immunocompromised patients, one-half of those with a negative chest radiograph had parenchymal abnormalities detected on computed tomography (CT) imaging of the chest.37 Thus, a reliance on CT imaging of the chest as the initial diagnostic imaging modality is commonplace in the management of the compromised host with respiratory complaints.39 Chest CT is also performed routinely for disease surveillance during treatment of certain HMs (eg, lymphoma) and may be useful for comparison when diagnostic chest radiographs suggest a new PC. The special role of high-resolution CT has been considered useful in HM and HCT subgroups; however, their interpretation is not considered “unambiguous.”39, 40, 41 PET scanning may be useful for the evaluation of a solitary pulmonary nodule,42 and MRI may be required when a subject cannot receive iodinated contrast for a CT study, although a noncontrast CT is generally sufficient for the evaluation of parenchymal infiltrates.
Abnormal parenchymal patterns
Table 2 shows differential diagnoses to consider in the HM or HCT patient presenting with common parenchymal patterns on chest CT, including airspace consolidation, ground glass opacities, nodules, and reticular changes. Radiographic findings may be typical of certain clinical scenarios, for example, symmetric ground glass opacities with sharp margins in prior radiation fields suggest radiation pneumonitis, and diffuse reticular markings during a leukemic blast crisis may support pulmonary leukostasis. The differential may be justifiably narrowed quickly enough to warrant empiric treatment without more thorough investigation in select cases. However, radiographic abnormalities frequently overlap or are ill-defined, and their management may present conflict. For example, bacterial and fungal pneumonias often present as focal or multifocal airspace consolidation, as does noninfectious organizing pneumonia. Given that organizing pneumonia would require steroids for treatment, and that steroids would likely exacerbate an infectious process, further investigation is paramount. Along with the integration of information regarding underlying patient risk factors, clinical presentation, and abnormal imaging, results of noninvasive testing help to determine the next steps in management.
Table 2.
Abnormal parenchymal findings in hematologic malignancies and hematopoietic cell transplantation patients warranting consideration of lung sampling for diagnosis
| Radiographic Abnormalitiesa | Onset | Distribution/Sign |
|---|---|---|
| Airspace consolidation | Acute: Infection (bacteria) Subacute/chronic: Infection (fungi, Nocardia or Actinomyces spp, mycobacteria), drug toxicity, COP/BOOP, malignancy |
Focal: Infection (bacteria), malignancy Multi-focal/diffuse: Infection (bacteria, fungi/mold), COP/BOOP, drug toxicity, malignancy Air-bronchogram: Infection (bacteria) |
| Ground-glass attenuation | Acute: Infection (early PJP, CMV, HHV-6, CARV, atypical bacteria), alveolar hemorrhage, IPS,b acute radiation pneumonitis, eosinophilic pneumonia, pulmonary edema, ARDS, TRALI Subacute/chronic: Infection (CMV, atypicals), drug/radiation toxicity, malignancy, PAP, PVODb |
Multi-focal/diffuse: Infection (PJP, CMV, CARV, HHV-6), drug/radiation toxicity, DAH, IPS,b PERDS,b COP/BOOP, ARDS, TRALI Mosaic attenuation & air trapping: BOSb/chronic GVHD |
| Nodules & mass lesions | Acute: Infection (necrotizing bacteria, eg, Pseudomonas, Staphylococcus aureus, Klebsiella spp; Aspergillus spp) Subacute/chronic: Infection (fungi, Nocardia, mycobacteria), malignancy |
Halo-sign: Aspergillus infection Reversed Halo-sign: COP Tree-in-bud: Infection (atypical bacteria, mycobacteria, fungi), mucoid impaction Diffuse centrilobular nodules: viral bronchiolitis, late BOSb |
| Interstitial infiltrates | Acute: Infection (late PJP, viruses, atypical bacteria), pulmonary edema, ARDS, TRALI Subacute/chronic: Infection (mycobacteria), drug/radiation toxicity, malignancy (leukemic infiltration), PAP, PVODb |
Multi-focal/diffuse: Infection (PJP, viruses,atypical bacteria), pulmonary edema, ARDS, TRALI, malignancy (leukemic infiltration), PAP Crazy-paving: PAP, pulmonary edema, DAH |
Abbreviations: ARDS, acute respiratory distress syndrome; BOOP, bronchiolitis obliterans organizing pneumonia; BOS, bronchiolitis obliterans syndrome; CARV, community-acquired respiratory virus; CMV, cytomegalovirus; COP, cryptogenic organizing pneumonia; DAH, diffuse alveolar hemorrhage; GVHD, graft-versus-host disease; HHV-6, human herpes virus 6; IPS, idiopathic pneumonia syndrome; PAP, pulmonary alveolar proteinosis; PERDS, periengraftment respiratory distress syndrome; PJP, Pneumocystis jirovecii pneumonia; PVOD, pulmonary veno-occlusive disease; TRALI, transfusion-related acute lung injury.
In some cases, findings may be apparent on chest radiography, but chest computed tomography scans, especially when performed at high resolution, allow for earlier detection. Common radiologic patterns include airspace consolidation, ground-glass attenuation, interstitial infiltrates, and nodular/mass lesions.
Unique to hematopoietic cell transplant recipients.
Noninvasive Testing
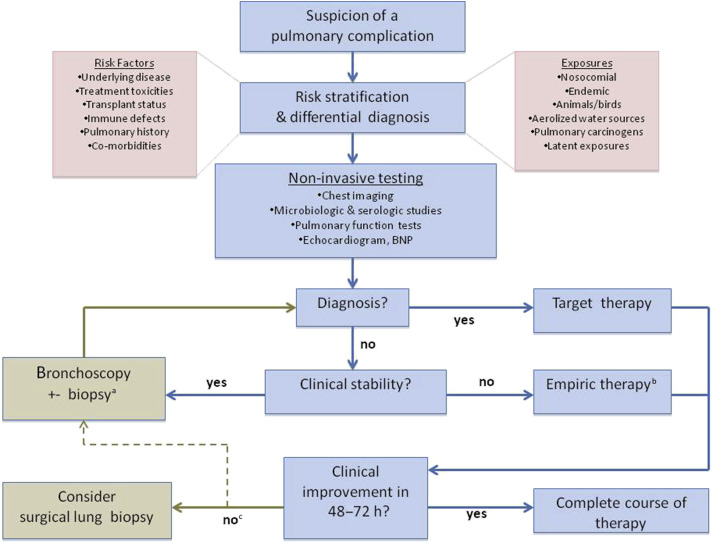
Infectious workup
Together with chest imaging, the results of noninvasive diagnostic testing narrow the differential diagnosis for an infectious PC (Fig. 3 ). Routine microbiological and serologic investigations of serum, urine, and respiratory specimens (nasopharyngeal swabs, sputum, tracheal aspirates) are usually obtained at the time of clinical presentation. Additional assays are requested based on risk features of the patient, for example, endemic fungal exposures; and chest CT patterns, for example, nodule infiltrates, which may heighten suspicion for atypical processes. In recent years, culture-based methods of pathogen isolation from respiratory secretions or blood have been supplemented or supplanted by molecular testing techniques, such as polymerase chain reaction, for diagnosis of infectious PCs (Table 3 ). At our institution, polymerase chain reaction for the identification of P jirovecii, M tuberculosis, and community-acquired respiratory viruses is performed routinely on respiratory samples of appropriate HM and HCT patients. Antigen testing in serum (eg, Aspergillus galactomannan, beta-D glucan, cryptococcal and histoplasma antigens), and in urine (eg, Streptococcus pneumoniae and Legionella pneumophila antigens), are obtained in appropriate patients. In some cases, the negative predictive value may be most valuable, as with beta-D glucan, where only moderate diagnostic value is mitigated by its high negative predictive value in critically ill HM patients.43 As with any test results, preexisting clinical suspicion is essential for their interpretation, to avoid overdiagnosis or underdiagnosis, and to ensure appropriate treatment decisions.
Fig. 3.
Approach to the diagnostic evaluation of pulmonary infiltrates in patients with hematologic malignancies and in hematopoietic cell transplant recipients. a Transbronchial lung biopsy is generally reserved for suspicion of invasive viral, fungal or mycobacterial disease. b The unstable transplant patient who becomes clinically stable may benefit from early diagnostic bronchoscopy within 48 to 72 hours of initiating therapy (dashed line). c Diagnostic bronchoscopy should be considered before surgical lung biopsy in cases refractory to empiric therapy (dotted line). BNP, B-natriuretic peptide.
(Adapted from Harris B, Lowy FD, Stover DE, et al. Diagnostic bronchoscopy in solid-organ and hematopoietic stem cell transplantation. Ann Am Thorac Soc 2013;10(1):44; with permission.)
Table 3.
Diagnostic evaluation of bronchoscopic specimens for specific infectious pulmonary complications of hematologic malignancies and HCT
| Infectious Etiology | Microbiology (BAL, PSB, TBLB) | Pathology (BAL, EBB, TBLB) | Additional Studies (BAL, Other) | Comments |
|---|---|---|---|---|
|
|
|
|
|
|
Stain (KOH, Giemsa, Silver, Calcofluor white) and culturea PCRb |
Cytology (BAL)c Tissue invasion (TBLB) Airway infection (EBB) II |
Pneumocystis IFA/DFA/PCR (BAL) A Galactomannan (BAL, serum) Urine and serum antigens, serologyd |
|
|
Stain (Papanicolaou) and culturea PCRb |
Cytology (BAL)c Tissue invasion (TBLB)e |
CMV DFA (BAL) Serum antigen and viral loadd Nasal swab PCRb |
|
|
PCR | Immunostain (BAL) Larvae (BAL) |
Serology, peripheral cell count, stool studiesd |
|
Abbreviations: BAL, bronchoalveolar lavage; CARV, community-acquired respiratory virus; CFU, colony forming unit; CMV, cytomegalovirus; DFA, direct fluorescent antibody; EBB, endobronchial biopsy; EBV, Epstein–Barr virus; ESBL, extended spectrum beta lactam; HCT, hematopoietic cell transplantation; HHV-6, human herpes virus-6; HSV, herpes simplex virus; IFA, indirect fluorescent antibody; KOH, potassium hydroxide stain; MRSA, methicillin-resistant S aureus; PCR, polymerase chain reaction; PSB, protected specimen brushing; spp, species; TBLB, transbronchial lung biopsy; VRE, vancomycin-resistant Enterococcus; VZV, varicella zoster virus.
Direct stains are lacking for atypical organisms such as M pneumoniae and C pneumonia, and special media is required for culture of L pneumophila. Culture is unavailable for P jirovecii, and most fungi are difficult to cultivate in the clinical laboratory. Viral staining and culture is predominantly done for CMV. Culture is uncommonly performed for the identification of T gondii or S stercoralis.
Multiplex PCR is available for a comprehensive panel of respiratory viruses and atypical bacteria, including L pneumoniae, C pneumoniae, M pneumoniae, and B pertussis. PCR for M tuberculosis is routinely performed on samples with a positive acid-fast stain or in smear-negative specimens from a high-risk patient.
Cytology with special stains is generally performed for the identification of organisms that are difficult to cultivate in the laboratory, including acid-fast bacteria, fungi (including Pneumocystis) and CMV.
Other tests that may assist in microbiologic diagnosis include complement fixation and cold agglutinins for Mycoplasma in serum and urine antigen testing for S pneumonia and L pneumophilia serotype 1. Non-BAL antigen testing may also be done for C neoformans (serum), H capsulatum (serum, urine), and B dermatitidis (serum, urine), as well as HSV, RSV, influenza A and B, and adenovirus 40/41 (all serum). Viral load provides information pertaining to CMV activity. Nasopharyngeal swab for PCR of CARV may be useful before bronchoscopy. Serology, peripheral cell count (eg, eosinophilia) and stool studies may be useful adjunctive tests for parasitic causes of infection, notably Strongyloides.
Tissue invasion is commonly caused by fungi (Aspergillus and atypical molds) and CMV. EBB may be useful to establish airway infection caused by Aspergillus.
Reprinted from Harris B, Lowy FD, Stover DE, et al. Diagnostic bronchoscopy in solid-organ and hematopoietic stem cell transplantation. Ann Am Thorac Soc 2013;10(1):45; with permission.
Biomarkers
There is limited usefulness to nonspecific inflammatory biomarkers, such as C-reactive protein, in diagnosing PCs in HM and HCT patients. This lack is likely due to both test and patient characteristics, including highly varied and aberrant responses to inflammation. Serum procalcitonin may be useful in distinguishing bacterial from viral or fungal infection in the immunocompromised host, and may be considered for its negative predictive value in the neutropenic patient with persistent fever.44 It generally has limited specificity in the critically ill HM patient,45 or at the time of FN onset,46 when it might be of greatest practical use. Furthermore, limited study in HCT recipients suggests that procalcitonin cannot distinguish between infectious and noninfectious pulmonary processes, but may indicate severity.47 Few empiric treatment decisions are likely to be made or altered in the absence of more reliable, supportive data.
Other tests
Lung function testing is not indicated commonly in the evaluation of new pulmonary infiltrates. Pulmonary function tests may be valuable when there is suspicion of airways disease, such as bronchiolitis obliterans syndrome, which is a late complication, as well as monitoring response to therapy of the more common problems, such as chemotherapy toxicity. Last, echocardiography and measurement of serum B-natriuretic peptide may help to distinguish cardiogenic pulmonary edema from other causes of diffuse lung infiltrates.
Invasive Testing
Results of noninvasive testing may support a specific diagnosis, such as invasive aspergillosis in a patient with FN who presents with a halo sign on chest CT and elevated serum Aspergillus galactomannan antigen.48 These results may be acceptable drivers of therapy in the high-risk or unstable patient who cannot safely undergo further diagnostic workup. However, for the clinically stable patient with a paucity of data supporting probable cause, diagnostic FOB is an important tool to consider early in PC management. The purpose of prompt lung sampling is as much to identify an infectious etiology on which to base or modify antimicrobial therapy, as it is to rule out an infectious process before empiric augmentation of immunosuppression for alternative causes.
Overview of fiberoptic bronchoscopy
Minimally invasive lung sampling via FOB is more likely to capture a snapshot of pulmonary process than expectorated sputum and tracheal aspirates, which are specimens highly contaminated by colonizing flora,49 and may provide additional diagnostic information in more than one-half of patients.50 Visual inspection of the airways may identify areas of focal hemorrhage, fungal plaques, purulence, and tumor. Specimens may be collected from the entire LRT via FOB, and most commonly include proximal and distal airway secretions collected via bronchial washing and bronchoalveolar lavage (BAL), and lung tissue via transbronchial lung biopsy (TBLB). Microbiologic, cytologic, and histopathologic studies of BAL and TBLB, when performed, are the primary sources of diagnostic information obtained via FOB.
Signs and symptoms warranting consideration of diagnostic FOB include fever, leukocytosis, hypoxemia, hemoptysis, and unexplained dyspnea, usually in association with new parenchymal opacities (see Table 2). The immediate period after recognition of symptoms may be a critical window for lung sampling in high-risk patients, including those with FN or early post-HCT, and for those who present acutely with multifocal or diffuse infiltrates. Once etiologies such as pulmonary embolism, cardiac abnormalities, and nonparenchymal infectious sources have been ruled out appropriately, FOB should be considered promptly. Empiric therapy may be warranted in the unstable patient (or in the stable but high-risk patient) in whom bronchoscopy cannot be performed urgently; however, the initiation of treatment should not preclude continued risk assessment to proceed with FOB in a timely manner (see Fig. 3).
Complications associated with FOB in HM and HCT patients are similar to those in the general population, and include hypoxemia, bleeding, bronchospasm, pneumothorax, and cardiac events.51 Accordingly, contraindications to the procedure include severe hypoxemia, myocardial ischemia, hemodynamic instability, severe thrombocytopenia, or coagulopathy.51 Bleeding is a common complication in HM and HCT subjects in the setting of prevalent cytopenias, and has been reported in up to 15% of HCT subjects who undergo diagnostic FOB.52 A lower platelet threshold for BAL, for example, 20,000/μL, has been associated with only mild bleeding episodes,53 and is a commonly used cutoff for performing BAL at our institution. Hypoxemia is another major concern in these patients, many of whom have diminished pulmonary reserve before FOB. In single-center retrospective studies of HCT recipients, the procedure has been associated with respiratory decline54 and mortality.55 Given that the likelihood of intubation after FOB in HCT recipients with acute respiratory failure may is greater, clinicians may favor a purely noninvasive diagnostic approach to PC diagnosis. However, data from a large cohort of HCT patients showed hypoxemia associated with FOB to occur in a small minority (1.8%), and led to mechanical ventilation in only 2% of that group.52 The overall low rate of intubation in the HCT and neutropenic patients suggests that a low incidence of procedure-related hypoxemia may be an acceptable risk.52, 56, 57, 58
In practice, myriad challenges face providers in determining the appropriate timing of FOB in HM and HCT patients, many of whom are too sick to undergo conscious sedation or general anesthesia for a diagnostic procedure. Provider preference has also been shown to be a barrier to FOB independent of clinical status,59, 60 and delay in diagnosis may have less to do with respiratory status than with physician choice.61 Based on autopsy studies, PC diagnoses remain elusive before death in many HCT subjects,12, 13, 14 suggesting that a ‘wait and see’ approach to empiric therapy is used commonly. As a result of these differences, rigorous study is difficult and there is limited prospective evidence on which to base decisions regarding optimal timing, modality, yield or impact of FOB on outcomes in these populations. The available literature regarding the role of diagnostic bronchoscopy in transplant recipients has been reviewed in detail previously6 and is summarized briefly herein.
Yield and timing of fiberoptic bronchoscopy
Diagnostic yield commonly refers to the identification of a causative organism or other etiology in BAL, protected brush specimens (not routinely used in HM and HCT patients), and/or TBLB specimens. Using mostly retrospective data, the overall range for yield of FOB in HM and HCT is wide, from 30% to 67%.15, 56, 57, 58, 62, 63, 64, 65 Diagnostic yield may correlate with anatomic location and with radiographic patterns. For example, BAL return in the setting of reticular/nodular infiltrates is generally lower as compared with BAL performed in regions with hazy ground glass or consolidation.42, 66 FOB yield may be highest for multifocal infections, such as P jirovecii pneumonia, and lowest for mycobacterial or fungal etiologies.67 Diagnostic yield may also be higher in febrile or symptomatic patients as compared with those who are asymptomatic.57, 66 In a retrospective review of 501 nonintubated allogeneic HCT recipients with new pulmonary infiltrates during the first 100 days after HCT, the diagnostic yield of FOB more than doubled during the first 4 days after symptom onset.57 This same study showed a diagnostic yield of 75% if performed within 24 hours before the initiation of antimicrobials, and other studies suggest that optimal yield can still be achieved if FOB is performed within 1 to 3 days of the initiation of therapy.58, 68, 69 Empirical antimicrobial therapy before lung sampling is an unavoidable reality in many high-risk patients and may reduce diagnostic yield for invasive fungal disease, in particular.70 Accordingly, the yield of diagnostic FOB may be least in patients who would most greatly benefit from early treatment guidance, including critically ill HCT recipients54 and those who have acute graft-versus-host disease.71
The importance of diagnostic yield lies in its direct impact on management, and on its indirect impact on PC-related outcomes, such as mortality. Although few studies have rigorously evaluated the impact of FOB on patient management or mortality using prospective methods, available data suggest that early FOB is more likely to provide a diagnosis (especially bacterial) upon which changes in management can be made.72 FOB-guided changes in antimicrobial therapy have been reported in 20% to 70% of HM and HCT recipients,52, 54, 57, 58, 62, 65, 73, 74 including withdrawal of antimicrobial agents in nearly one-half of HCT subjects.52, 58 FOB results may also provide critical insight into the management of resistant pathogens. In 1 study, pathogens detected in BAL alone demonstrated antimicrobial resistance profiles integral to management, thus rendering inappropriate the choice of empiric therapy based on antimicrobial profiles identified in upper respiratory or peripheral specimens.64 However, diagnostic yield may not always correlate with a change in management, as demonstrated in neutropenic intensive care unit patients, where a 50% diagnostic yield had little impact on treatment changes.65
The impact of diagnostic FOB on PC-related survival is also unclear. Several retrospective, single-center studies suggest that FOB has no discernible influence on mortality.56, 65, 75 Although a prospective multicenter study of critically ill cancer patients, including a subset of HCT recipients, did not find FOB to influence mortality, FOB performed within 4 days of symptom onset was associated with a significant survival advantage at 30 days compared with subjects who underwent late FOB-associated antibiotic changes.57 Another study showed FOB-driven changes in antimicrobial management within 7 days of presentation to be associated with lower mortality compared with patients in whom change was instituted beyond 1 week.58 Thus, an inability to target treatment expediently may contribute to poor outcomes. Diagnostic delay or a lack of diagnosis has been shown to independently predict death in immunosuppressed hosts with pulmonary infiltrates, highest in critically ill HCT recipients and those with FN.15, 76 This finding highlights the importance of obtaining a correct microbiological diagnosis in the compromised patient, when possible.77
Recommended approach to diagnostic fiberoptic bronchoscopy
As a guiding principle, diagnostic FOB should be considered in the HM or HCT subject upon presentation with a new infiltrate on diagnostic chest imaging, and/or in the absence of clinical or radiographic response to at least 48 to 72 hours of empiric antimicrobial therapy (see Fig. 3). In the event that empiric therapy is instituted before sampling, whether based on the acuity of patient illness or high suspicion for opportunistic illness, timely investigation is critical to optimize yield and avoid masking a partially treated infection. If the clinical decision is to observe the effects of empiric therapy before lung sampling, this period should be limited to just a few days. The use of systematic institutional protocols for FOB in compromised hosts may be considered.78
Consideration of lung biopsy
There is controversy regarding the usefulness of lung biopsy in HM and HCT subjects. For some providers, BAL has historically been considered sufficient for diagnosis65, 79; for others, the improved yield of combined BAL and TBLB as compared with BAL alone can also be justified by low reported complication rates.80, 81 In a more recent metaanalysis, similar rates of diagnosis were found in studies of BAL and lung biopsy from HCT recipients, although infection was identified more commonly from BAL and noninfectious etiologies were picked up on biopsy.60 Upon suspicion of invasive fungal or viral infection, however, TBLB may improve diagnostic yield over BAL alone.81 Overall, however, the impact of TBLB on management remains unclear.82
As an alternative to TBLB, CT-guided transthoracic lung biopsy may be preferred for sampling peripheral lung lesions (unless BAL would be contributory) and can be high yield in the HM or HCT patient.42 A specificity of 100% for diagnosis of invasive fungal disease using CT-guided sampling has been reported.83 There is an increased risk of pneumothorax using this approach as compared with TBLB; thus, it is important to choose a large enough nodule for improved sampling yield in the face of elevated procedural risk.42
Surgical lung biopsy (SLB), whether open or video assisted, is generally kept as a last resort owing to increased procedural risk. Although TBLB, transthoracic lung biopsy, and SLB have not be compared head to head, the decision to proceed to SLB generally follows a nondiagnostic TBLB or an unrelenting course despite empiric therapy.67 In a retrospective study from our institution, open lung biopsy in HM subjects demonstrated a specific diagnosis in 62%, led to a change in management in 69%, and correlated with an improved overall survival.84 Although the diagnostic yield of SLB can be high,85 its impact on management is difficult to ascertain, and associated mortality limits SLB as a first-line diagnostic modality in transplant recipients. Furthermore, SLB has been on the decrease in recent years as diagnostics for invasive fungal disease improve.86
Diagnostic testing of lung specimens
Table 3 summarizes the applications of assays to lung specimens for the diagnosis of infectious PCs. Culture-dependent and -independent methods for identifying common respiratory pathogens and opportunistic organisms in bronchoscopic specimens are similar to those applied to upper respiratory specimens; however, their interpretation requires caution. Contamination of LRT specimens by oral and upper airway flora or colonizers needs to be considered when interpreting the results of microbiological investigations in BAL. Furthermore, the identification of a potential pathogen, such as cytomegalovirus or methicillin-resistant Staphylococcus aureus, or fungal antigen, such as beta-D glucan, in BAL, does not always imply causation, emphasizing the importance of clinical context in the interpretation of results. BAL cytology continues to be useful to suggest processes involving tissue invasion (such as P jirovecii pneumonia and cytomegalovirus disease) in the absence of biopsy specimens, and may also identify malignant cells (eg, lymphoma), hemorrhage, and alveolar proteinosis. BAL cell count is generally nonspecific, although it may be useful in diffuse alveolar hemorrhage or organizing pneumonia. Lung tissue histopathology is important not only for definitive diagnosis of invasive fungal or viral infections, but also malignancy, organizing pneumonia, and interstitial diseases associated with drug toxicity.
Summary
Early diagnosis of PCs is challenging owing to heterogeneous patient, clinical, and provider factors. A delay in PC diagnosis limits the opportunity for targeted treatment, which may contribute to poor outcomes. Thus, an integrated clinicoradiologic approach can provide crucial insight into the nature of PCs, and provide guidance for further diagnostic testing in HM and HCT patients. Although controversy persists, available data suggest an advantage to early FOB in terms of diagnostic yield, targeted management, and mortality for high-risk HM and HCT recipients, perhaps with exception in the critically ill population. A low threshold for minimally invasive lung sampling should therefore be a guiding principle in high-risk patients, including those with FN and recipients of HCT. This practice may become especially important as advances are made in the sensitivity and specificity of next-generation sequencing applications for infectious disease diagnosis. Empirical treatment is important for the neutropenic or febrile patient presenting with signs or symptoms of pneumonia, however FOB within 72 hours of intubation and empiric treatment is nonetheless encouraged. After careful assessment of risk, lung biopsy via TBLB or transthoracic lung biopsy should be considered when there is concern for invasive fungal or viral disease and in the absence of supportive data from noninvasive sources. SLB should be reserved for cases where diagnoses remain elusive despite investigations of BAL or lung tissue obtain via minimally invasive modalities, and where increased procedural risk is warranted in favor of diagnostic results that would impact key aspects of management. Although prospective study is needed to determine optimal the strategy for lung sampling, close attention to individual risk/benefit profiles will always remain integral to management.
Footnotes
Disclosure Statement: The authors have nothing to disclose.
References
- 1.Harris B., Morjaria S.M., Littmann E.R. Gut microbiota predict pulmonary infiltrates after allogeneic hematopoietic cell transplantation. Am J Respir Crit Care Med. 2016;194(4):450–463. doi: 10.1164/rccm.201507-1491OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Choi M.H., Jung J.I., Chung W.D. Acute pulmonary complications in patients with hematologic malignancies. Radiographics. 2014;34(6):1755–1768. doi: 10.1148/rg.346130107. [DOI] [PubMed] [Google Scholar]
- 3.Gooley T.A., Chien J.W., Pergam S.A. Reduced mortality after allogeneic hematopoietic-cell transplantation. N Engl J Med. 2010;363(22):2091–2101. doi: 10.1056/NEJMoa1004383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Joos L., Tamm M. Breakdown of pulmonary host defense in the immunocompromised host: cancer chemotherapy. Proc Am Thorac Soc. 2005;2(5):445–448. doi: 10.1513/pats.200508-097JS. [DOI] [PubMed] [Google Scholar]
- 5.Evans S.E., Ost D.E. Pneumonia in the neutropenic cancer patient. Curr Opin Pulm Med. 2015;21(3):260–271. doi: 10.1097/MCP.0000000000000156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harris B., Lowy F.D., Stover D.E. Diagnostic bronchoscopy in solid-organ and hematopoietic stem cell transplantation. Ann Am Thorac Soc. 2013;10(1):39–49. doi: 10.1513/AnnalsATS.201212-114FR. [DOI] [PubMed] [Google Scholar]
- 7.Afessa B., Abdulai R.M., Kremers W.K. Risk factors and outcome of pulmonary complications after autologous hematopoietic stem cell transplant. Chest. 2012;141(2):442–450. doi: 10.1378/chest.10-2889. [DOI] [PubMed] [Google Scholar]
- 8.Peters S.G., Afessa B. Acute lung injury after hematopoietic stem cell transplantation. Clin Chest Med. 2005;26:561–569. doi: 10.1016/j.ccm.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 9.Benz R., Schanz U., Maggiorini M. Risk factors for ICU admission and ICU survival after allogeneic hematopoietic SCT. Bone Marrow Transplant. 2014;49(1):62–65. doi: 10.1038/bmt.2013.141. [DOI] [PubMed] [Google Scholar]
- 10.Garcia J.B., Lei X., Wierda W. Pneumonia during remission induction chemotherapy in patients with acute leukemia. Ann Am Thorac Soc. 2013;10(5):432–440. doi: 10.1513/AnnalsATS.201304-097OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mayer S., Pastores S.M., Riedel E. Short- and long-term outcomes of adult allogeneic hematopoietic stem cell transplant patients admitted to the intensive care unit in the peritransplant period. Leuk Lymphoma. 2017;58(2):382–390. doi: 10.1080/10428194.2016.1195499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sharma S., Nadrous H.F., Peters S.G. Pulmonary complications in adult blood and marrow transplant recipients: autopsy Findings. Chest. 2005;128(3):1385–1392. doi: 10.1378/chest.128.3.1385. [DOI] [PubMed] [Google Scholar]
- 13.Roychowdhury M., Pambuccian S.E., Aslan D.L. Pulmonary complications after bone marrow transplantation: an autopsy study from a large transplantation center. Arch Pathol Lab Med. 2005;129(3):366–371. doi: 10.5858/2005-129-366-PCABMT. [DOI] [PubMed] [Google Scholar]
- 14.Pastores S.M., Dulu A., Voigt L. Premortem clinical diagnoses and postmortem autopsy findings: discrepancies in critically ill cancer patients. Crit Care. 2007;11(2):R48. doi: 10.1186/cc5782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gruson D., Hilbert G., valentine R. Utility of fiberoptic bronchoscopy in neutropenic patients admitted to the intensive care unit with pulmonary infiltrates. Crit Care Med. 2000;28(7):2224–2230. doi: 10.1097/00003246-200007000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Rano A., Agusti C., Natividada B. Prognostic factors of non-HIV immunocompromised patients with pulmonary infiltrates. Chest. 2002;122(1):253–261. doi: 10.1378/chest.122.1.253. [DOI] [PubMed] [Google Scholar]
- 17.White D.A. Drug-induced pulmonary infection. Clin Chest Med. 2004;25(1):179–187. doi: 10.1016/S0272-5231(03)00134-5. [DOI] [PubMed] [Google Scholar]
- 18.Safdar A., Armstrong D. Infections in patients with hematologic neoplasms and hematopoietic stem cell transplantation: neutropenia, humoral, and splenic defects. Clin Infect Dis. 2011;53(8):798–806. doi: 10.1093/cid/cir492. [DOI] [PubMed] [Google Scholar]
- 19.Bennett C.L., Djulbegovic B., Norris L.B. Colony-stimulating factors for febrile neutropenia during cancer therapy. N Engl J Med. 2013;368(12):1131–1139. doi: 10.1056/NEJMct1210890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Neuberger S., Maschmeyer G. Update on management of infections in cancer and stem cell transplant patients. Ann Hematol. 2006;85:346–356. doi: 10.1007/s00277-005-0048-2. [DOI] [PubMed] [Google Scholar]
- 21.Marr K.A. Delayed opportunistic infections in hematopoietic stem cell transplantation patients: a surmountable challenge. Hematology Am Soc Hematol Educ Program. 2012;2012:265–270. doi: 10.1182/asheducation-2012.1.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carreras E., Diaz-Ricart M. The role of the endothelium in the short-term complications of hematopoietic SCT. Bone Marrow Transplant. 2011;46(12):1495–1502. doi: 10.1038/bmt.2011.65. [DOI] [PubMed] [Google Scholar]
- 23.Spira D., Wirths S., Skowronski F. Diffuse alveolar hemorrhage in patients with hematological malignancies: HRCT patterns of pulmonary involvement and disease course. Clin Imaging. 2013;37(4):680–686. doi: 10.1016/j.clinimag.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 24.Panoskaltsis-Mortari A., Griese M., Madtes D.K., on behalf of the American Thoracic Society Committee on Idiopathic Pneumonia Syndrome An official American Thoracic Society research statement: noninfectious lung injury after hematopoietic stem cell transplantation: idiopathic pneumonia syndrome. Am J Respir Crit Care Med. 2011;183:1262–1279. doi: 10.1164/rccm.2007-413ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pene F., Aubron C., Azoulay E. Outcome of critically ill allogeneic hematopoietic stem cell transplantation recipients: a reappraisal of indications for organ failure supports. J Clin Oncol. 2006;24(4):643–649. doi: 10.1200/JCO.2005.03.9073. [DOI] [PubMed] [Google Scholar]
- 26.Azoulay E., Lemiale V., Mokart D. Acute respiratory distress syndrome in patients with malignancies. Intensive Care Med. 2014;40(8):1106–1114. doi: 10.1007/s00134-014-3354-0. [DOI] [PubMed] [Google Scholar]
- 27.Hanajiri R., Kakihana K., Kobayashi T. Tobacco smoking is associated with infectious pulmonary complications after allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant. 2015;50(8):1141–1143. doi: 10.1038/bmt.2015.116. [DOI] [PubMed] [Google Scholar]
- 28.Sethi S., Maloney J., Grove L. Airway inflammation and bronchial bacterial colonization in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2006;173:991–998. doi: 10.1164/rccm.200509-1525OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Van Vliet M.J., Harmsen H.J., de Bont E.S. The role of intestinal microbiota in the development and severity of chemotherapy-induced mucositis. PLoS Pathog. 2010;6(5):e1000879. doi: 10.1371/journal.ppat.1000879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ho V.T., Weller E., Lee S.J. Prognostic factors for early severe pulmonary complications after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2001;7(4):223–229. doi: 10.1053/bbmt.2001.v7.pm11349809. [DOI] [PubMed] [Google Scholar]
- 31.Sorror M.L. Comorbidities and hematopoietic cell transplantation outcomes. Hematology Am Soc Hematol Educ Program. 2010;2010:237–247. doi: 10.1182/asheducation-2010.1.237. [DOI] [PubMed] [Google Scholar]
- 32.Bayraktar U.D., Shpall E.J., Liu P. Hematopoietic cell transplantation-specific comorbidity index predicts inpatient mortality and survival in patients who received allogeneic transplantation admitted to the intensive care unit. J Clin Oncol. 2013;31(33):4207–4214. doi: 10.1200/JCO.2013.50.5867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Taur Y., Xavier J.B., Lipuma L. Intestinal domination and the risk of bacteremia in patients undergoing allogeneic hematopoietic stem cell transplantation. Clin Infect Dis. 2012;55(7):905–914. doi: 10.1093/cid/cis580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Taur Y., Jenq R., Perales M. The effects of intestinal tract bacterial diversity on mortality following allogeneic hematopoietic stem cell transplantation. Blood. 2014;124(7):1174–1182. doi: 10.1182/blood-2014-02-554725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bergeron A. The pulmonologist's point of view on lung infiltrates in haematological malignancies. Diagn Interv Imaging. 2013;94(2):216–220. doi: 10.1016/j.diii.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 36.Maschmeyer G., Donnelly J.P. How to manage lung infiltrates in adults suffering from haematological malignancies outside allogeneic haematopoietic stem cell transplantation. Br J Haematol. 2016;173(2):179–189. doi: 10.1111/bjh.13934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Heussel C.P., Kauczor H.U., Heussel G.E. Pneumonia in febrile neutropenic patients and in bone marrow and blood stem-cell transplant recipients: use of high-resolution computed tomography. J Clin Oncol. 1999;17(3):796–805. doi: 10.1200/JCO.1999.17.3.796. [DOI] [PubMed] [Google Scholar]
- 38.Cereser L., Zuiani C., Graziani G. Impact of clinical data on chest radiography sensitivity in detecting pulmonary abnormalities in immunocompromised patients with suspected pneumonia. Radiol Med. 2010;115(2):205–214. doi: 10.1007/s11547-009-0433-3. [DOI] [PubMed] [Google Scholar]
- 39.Wijers S.C., Boelens J.J., Raphael M.F. Does high-resolution CT has diagnostic value in patients presenting with respiratory symptoms after hematopoietic stem cell transplantation? Eur J Radiol. 2011;80(3):e536–e543. doi: 10.1016/j.ejrad.2011.01.037. [DOI] [PubMed] [Google Scholar]
- 40.Tanaka N., Kunihiro Y., Yujiri T. High-resolution computed tomography of chest complications in patients treated with hematopoietic stem cell transplantation. Jpn J Radiol. 2011;29(4):229–235. doi: 10.1007/s11604-010-0544-8. [DOI] [PubMed] [Google Scholar]
- 41.Brodoefel H., Faul C., Salih H. Therapy-related noninfectious complications in patients with hematologic malignancies: high-resolution computed tomography findings. J Thorac Imaging. 2013;28(1):W5–W11. doi: 10.1097/RTI.0b013e31822031f0. [DOI] [PubMed] [Google Scholar]
- 42.Wingard J.R., Hiemenz J.W., Jantz M.A. How I manage pulmonary nodular lesions and nodular infiltrates in patients with hematologic malignancies or undergoing hematopoietic cell transplantation. Blood. 2012;120(9):1791–1800. doi: 10.1182/blood-2012-02-378976. [DOI] [PubMed] [Google Scholar]
- 43.Azoulay E., Guigue N., Darmon M. (1, 3)-β-D-glucan assay for diagnosing invasive fungal infections in critically ill patients with hematological malignancies. Oncotarget. 2016;7(16):21484–21495. doi: 10.18632/oncotarget.7471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Koya J., Nannya Y., Ichikawa M. The clinical role of procalcitonin in hematopoietic SCT. Bone Marrow Transplant. 2012;47(10):1326–1331. doi: 10.1038/bmt.2012.18. [DOI] [PubMed] [Google Scholar]
- 45.Bele N., Darmon M., Coquet I. Diagnostic accuracy of procalcitonin in critically ill immunocompromised patients. BMC Infect Dis. 2011;11:224. doi: 10.1186/1471-2334-11-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Robinson J.O., Lamoth F., Bally F. Monitoring procalcitonin in febrile neutropenia: what is its utility for initial diagnosis of infection and reassessment in persistent fever? PLoS One. 2011;6(4):e18886. doi: 10.1371/journal.pone.0018886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lucena C.M., Rovira M., Gabarrús A. The clinical value of biomarkers in respiratory complications in hematopoietic SCT. Bone Marrow Transplant. 2016 doi: 10.1038/bmt.2016.280. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Marom E.M., Kontoyiannis D.P. Imaging studies for diagnosing invasive fungal pneumonia in immunocompromised patients. Curr Opin Infect Dis. 2011;24(4):309–314. doi: 10.1097/QCO.0b013e328348b2e1. [DOI] [PubMed] [Google Scholar]
- 49.Lentino J.R., Lucks D.A. Nonvalue of sputum culture in the management of lower respiratory tract infections. J Clin Microbiol. 1987;25(5):758–762. doi: 10.1128/jcm.25.5.758-762.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Habtes I, Shah P, Harris B, et al. Bronchoalveolar lavage among hematopoietic stem cell transplant recipients: diagnostic yield and change in management. Poster presented at the ATS International Conference. San Francisco (CA), May 15, 2016.
- 51.British Thoracic Society Bronchoscopy Guidelines Committee, a Subcommittee of the Standards of Care Committee of the British Thoracic Society British Thoracic Society guidelines on diagnostic flexible bronchoscopy. Thorax. 2001;56(Suppl 1):i1–i21. doi: 10.1136/thorax.56.suppl_1.i1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yanik G.A., Ho V.T., Levine J.E. The impact of soluble tumor necrosis factor receptor etanercept on the treatment of idiopathic pneumonia syndrome after allogenic hematopoietic stem cell transplantation. Blood. 2008;112(8):3073–3081. doi: 10.1182/blood-2008-03-143412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Carr I.M., Koefelenberg C.F., von Groote-Bidlingmaier F. Blood loss during flexible bronchoscopy: a prospective observational study. Respiration. 2012;84(4):312–318. doi: 10.1159/000339507. [DOI] [PubMed] [Google Scholar]
- 54.Azoulay E., Mokart D., Rabbat A. Diagnostic bronchoscopy in hematology and oncology patients with acute respiratory failure: prospective multi-center data. Crit Care Med. 2008;1(36):100–107. doi: 10.1097/01.CCM.0000295590.33145.C4. [DOI] [PubMed] [Google Scholar]
- 55.Burger C.D. Utility of positive bronchoalveolar lavage in predicting respiratory failure after hematopoietic stem cell transplantation: a retrospective analysis. Transplant Proc. 2007;39:1623–1625. doi: 10.1016/j.transproceed.2007.02.065. [DOI] [PubMed] [Google Scholar]
- 56.Kuehnhardt D., Hannemann M., Schmidt B. Therapeutic implication of BAL in patients with neutropenia. Ann Hematol. 2009;88:1249–1256. doi: 10.1007/s00277-009-0747-1. [DOI] [PubMed] [Google Scholar]
- 57.Shannon V.R., Andersson B.S., Lei X. Utility of early versus late fiberoptic bronchoscopy in the evaluation of new pulmonary infiltrates following hematopoietic stem cell transplantation. Bone Marrow Transplant. 2010;45:647–665. doi: 10.1038/bmt.2009.203. [DOI] [PubMed] [Google Scholar]
- 58.Rano A., Agusti C., Jiminez P. Pulmonary infiltrates in non-HIV immunocompromised patients: a diagnostic approach using non-invasive and bronchoscopic procedures. Thorax. 2001;56:379–387. doi: 10.1136/thorax.56.5.379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wahidi M.M., Rocha A.T., Hollingsworth J.W. Contraindications and safety of transbronchial lung biopsy via flexible bronchoscopy. A survey of pulmonologists and review of the literature. Respiration. 2005;72:285–295. doi: 10.1159/000085370. [DOI] [PubMed] [Google Scholar]
- 60.Chellapandian D., Lehrnbecher T., Phillips B. Bronchoalveolar lavage and lung biopsy in patients with cancer and hematopoietic stem-cell transplantation recipients: a systematic review and meta-analysis. J Clin Oncol. 2015;33(5):501–509. doi: 10.1200/JCO.2014.58.0480. [DOI] [PubMed] [Google Scholar]
- 61.Wahla A.S., Chatterjee A., Khan I.I. Survey of academic pulmonologists, oncologists, and infectious disease physicians on the role of bronchoscopy in managing hematopoietic stem cell transplantation patients with pulmonary infiltrates. J Bronchology Interv Pulmonol. 2014;21(1):32–39. doi: 10.1097/LBR.0000000000000042. [DOI] [PubMed] [Google Scholar]
- 62.Kim S.W., Rhee C.K., Kang H.S. Diagnostic value of bronchoscopy in patients with hematologic malignancy and pulmonary infiltrates. Ann Hematol. 2015;94(1):153–159. doi: 10.1007/s00277-014-2172-3. [DOI] [PubMed] [Google Scholar]
- 63.Hummel M., Rudert S., Hof H. Diagnostic yield of bronchoscopy with bronchoalveolar lavage in febrile patients with hematologic malignancies and pulmonary infiltrates. Ann Hematol. 2008;87(4):291–297. doi: 10.1007/s00277-007-0391-6. [DOI] [PubMed] [Google Scholar]
- 64.Hohenadel I.A., Kiworr M., Genitsariotis R. Role of bronchoalveolar lavage in immunocompromised patients with pneumonia treated with a broad spectrum antibiotic and antifungal regimen. Thorax. 2001;56:115–120. doi: 10.1136/thorax.56.2.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hofmeister C.C., Czerlanis C., Forsythe S. Retrospective utility of bronchoscopy after hematopoietic stem cell transplant. Bone Marrow Transplant. 2006;38:693–698. doi: 10.1038/sj.bmt.1705505. [DOI] [PubMed] [Google Scholar]
- 66.Brownback K.R., Simpson S.Q. Association of bronchoalveolar lavage yield with chest computed tomography findings and symptoms in immunocompromised patients. Ann Thorac Med. 2013;8(3):153–159. doi: 10.4103/1817-1737.114302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Baughman R.P., Lower E.E. Diagnosis of pneumonia in immunocompromised patient. In: Agusti C., Torres A., editors. Pulmonary infection in the immunocompromised patient: strategies for management. Wiley-Blackwell; West Sussex, United Kingdom: 2009. pp. 53–93. [Google Scholar]
- 68.Pereira Gomes J.C., Pedreira J.W., Jr., Araujo E.M. Impact of BAL in the management of pneumonia with treatment failure: positivity of BAL culture under antibiotic therapy. Chest. 2000;118(6):1739–1746. doi: 10.1378/chest.118.6.1739. [DOI] [PubMed] [Google Scholar]
- 69.Yacoub A.T., Thomas D., Yuan C. Diagnostic value of bronchoalveolar lavage in leukemic and bone marrow transplant patients: the impact of antimicrobial therapy. Mediterr J Hematol Infect Dis. 2015;7(1):e2015002. doi: 10.4084/MJHID.2015.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Reinwald M., Hummel M., Kovalevskaya E. Therapy with antifungals decreases the diagnostic performance of PCR for diagnosing invasive aspergillosis in bronchoalveolar lavage samples of patients with haematological malignancies. J Antimicrob Chemother. 2012;67:2260–2267. doi: 10.1093/jac/dks208. [DOI] [PubMed] [Google Scholar]
- 71.Kasow K.A., King E., Rochester R. Diagnostic yield of bronchoalveolar lavage is low in allogeneic hematopoietic stem cell recipients receiving immunosuppressive therapy or with acute-graft-versus-host disease: the St. Jude experience. Biol Blood Marrow Transplant. 2007;13:831–837. doi: 10.1016/j.bbmt.2007.03.008. [DOI] [PubMed] [Google Scholar]
- 72.Lucena C.M., Torres A., Rovira M. Pulmonary complications in hematopoietic SCT: a prospective study. Bone Marrow Transplant. 2014;49(10):1293–1299. doi: 10.1038/bmt.2014.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gilbert C.R., Lerner A., Baram M. Utility of flexible bronchoscopy in the evaluation of pulmonary infiltrates in the hematopoietic stem cell transplant population – a single center fourteen year experience. Arch Bronconeumol. 2013;49(5):189–195. doi: 10.1016/j.arbres.2012.11.012. [DOI] [PubMed] [Google Scholar]
- 74.Gupta S., Sultenfuss M., Romaguera J.E. CT-guided percutaneous lung biopsies in patients with haematologic malignancies and undiagnosed pulmonary lesions. Hematol Oncol. 2010;28(2):75–81. doi: 10.1002/hon.923. [DOI] [PubMed] [Google Scholar]
- 75.Dunagan D.P., Baker A.M., Hurd D.D. Bronchoscopic evaluation of pulmonary infiltrates following bone marrow transplantation. Chest. 1997;111(1):135–141. doi: 10.1378/chest.111.1.135. [DOI] [PubMed] [Google Scholar]
- 76.Azoulay E., Mokart D., Lambert J. Diagnostic strategy for hematology and oncology patients with acute respiratory failure: randomized controlled trial. Am J Respir Crit Care Med. 2010;182(8):1038–1046. doi: 10.1164/rccm.201001-0018OC. [DOI] [PubMed] [Google Scholar]
- 77.Kontoyiannis D.P. Rational approach to pulmonary infiltrates in leukemia and transplantation. Best Pract Res Clin Haematol. 2013;26(3):301–306. doi: 10.1016/j.beha.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 78.Sampsonas F., Kontoyiannis D.P., Dickey B.F. Performance of a standardized bronchoalveolar lavage protocol in a comprehensive cancer center: a prospective 2-year study. Cancer. 2011;117(15):3424–3433. doi: 10.1002/cncr.25905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.White P., Bonacum J.T., Miller C.B. Utility of fiberoptic bronchoscopy in bone marrow transplant patients. Bone Marrow Transplant. 1997;20(8):681–687. doi: 10.1038/sj.bmt.1700957. [DOI] [PubMed] [Google Scholar]
- 80.Jain P., Sandur S., Meli Y. Role of flexible bronchoscopy in immunocompromised patients with lung infiltrates. Chest. 2004;125(2):712–722. doi: 10.1378/chest.125.2.712. [DOI] [PubMed] [Google Scholar]
- 81.Cazzadori A., DiPerri G., Todeschini G. Transbronchial biopsy in the diagnosis of pulmonary infiltrates in immunosuppressed patients. Chest. 1995;197:101–106. doi: 10.1378/chest.107.1.101. [DOI] [PubMed] [Google Scholar]
- 82.Peikert T., Rana S., Edell E.S. Safety, diagnostic yield, and therapeutic implications of flexible bronchoscopy in patients with febrile neutropenia and pulmonary infiltrates. Mayo Clin Proc. 2005;80(11):1414–1420. doi: 10.4065/80.11.1414. [DOI] [PubMed] [Google Scholar]
- 83.Carrafiello G., Laganà D., Nosari A.M. Utility of computed tomography (CT) and of fine needle aspiration biopsy (FNAB) in early diagnosis of fungal pulmonary infections. Study of infections from filamentous fungi in haematologically immunodeficient patients. Radiol Med. 2006;111(1):33–41. doi: 10.1007/s11547-006-0004-9. [DOI] [PubMed] [Google Scholar]
- 84.White D.A., Wong P.W., Downey R. The utility of open lung biopsy in patients with hematologic malignancies. Am J Respir Crit Care Med. 2000;161(3 Pt 1):723–729. doi: 10.1164/ajrccm.161.3.9904016. [DOI] [PubMed] [Google Scholar]
- 85.Zihlif M., Khanchandani G., Ahmed H.P. Surgical lung biopsy in patients with hematological malignancy or hematopoietic stem cell transplantation and unexplained pulmonary infiltrates: improved outcome with specific diagnosis. Am J Hematol. 2005;78(2):94–99. doi: 10.1002/ajh.20258. [DOI] [PubMed] [Google Scholar]
- 86.Cheng G.S., Stednick Z.J., Madtes D.K. Decline in the use of surgical biopsy for diagnosis of pulmonary disease in hematopoietic cell transplantation recipients in an era of improved diagnostics and empirical therapy. Biol Blood Marrow Transplant. 2016;22(12):2243–2249. doi: 10.1016/j.bbmt.2016.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]