Abstract
There is an important link between the upper and lower respiratory tracts whereby inflammation in one environment can influence the other. In acute rhinosinusitis, pathogen exposures are the primary driver for inflammation in the nose, which can exacerbate asthma. In chronic rhinosinusitis, a disease clinically associated with asthma, the inflammation observed is likely from a combination of an impaired epithelial barrier, dysregulated immune response, and potentially infection (or colonization) by specific pathogens. This review explores the associations between rhinosinusitis and asthma, with particular emphasis placed on the role of infections and inflammation.
Keywords: Acute rhinosinusitis, Chronic rhinosinusitis, Nasal polyp, Infection, Inflammation, Asthma, Microbiome
Key points
-
•
Rhinosinusitis is clinically defined as the presence of nasal drainage (anterior or posterior), nasal congestion, facial pain/pressure, and/or reduced sense of smell.
-
•
In acute rhinosinusitis, nasal symptoms last for less than 12 weeks and inflammation is often secondary to a viral or bacterial infection.
-
•
In chronic rhinosinusitis (CRS), nasal symptoms persist for longer than 12 weeks and the inflammation observed is secondary to impairments in the epithelial barrier, dysregulation of the host immune response, and potentially infections (or colonization) by pathogens.
-
•
CRS and asthma have a strong clinical association and share similar pathophysiologic mechanisms in support of the unified airway hypothesis.
Introduction
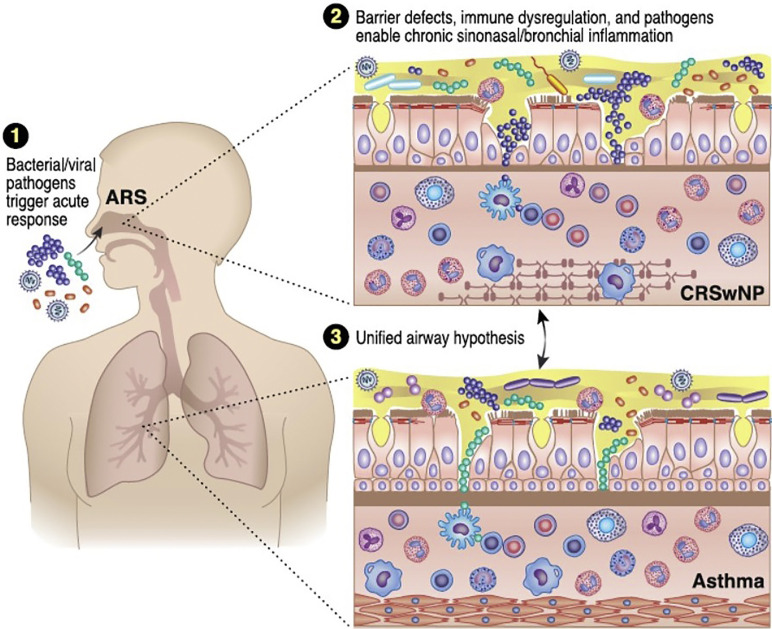
The unified airway hypothesis suggests that the nose and lungs are not separate organ systems but instead are part of the same continuum. Inflammation of the upper respiratory tract can affect the lower respiratory tract and vice versa. Viral and bacterial respiratory pathogens have long been known to induce acute inflammation in the airways and some have been implicated in the development of more chronic diseases. Rhinosinusitis and asthma are 2 common respiratory diseases that have been linked together on a clinical, as well as a pathophysiologic, basis (Fig. 1 ). In this review, associations between rhinosinusitis and asthma will be explored, with particular emphasis placed on the role of infections and inflammation.
Fig. 1.
Sinus infections, inflammation, and asthma. (1) Viral and bacterial respiratory pathogens are the most common cause of ARS, can exacerbate preexisting asthma, and potentially can lead to the development of asthma in certain populations. (2) In chronic rhinosinusitis with nasal polyp (CRSwNP) and asthma, impaired tight junctions, dysregulated immune responses, and possible infections (or colonization) by pathogens contribute to chronic airway inflammation. (3) The unified airway hypothesis suggests that upper airway inflammation can influence lower airway disease and vice versa further supporting the strong clinical association noted between CRSwNP and asthma.
(Courtesy of J. Schaffer, MAMS, Chicago, IL.)
Acute rhinosinusitis
Acute rhinosinusitis (ARS) is defined as the presence of nasal drainage (anterior or posterior), nasal congestion, facial pain/pressure, and/or reduced sense of smell. Depending on which guidelines are followed, ARS symptoms last either for less than 4 weeks1 or 12 weeks.2, 3 ARS is a clinical diagnosis, and objective confirmation by sinus computed tomography (CT) scan or nasal endoscopy is generally not indicated. Patients can have more than one episode of ARS each year but importantly, they are asymptomatic in the intervening periods.
Acute rhinosinusitis is extremely common. Studies specifying ARS found a disease prevalence of 6% to 15%,2, 4 with an estimated 0.035% of the population suffering from recurrent episodes.5 Between 2006 and 2010, there were an estimated 21.4 million ambulatory care visits with a primary diagnosis of ARS.6 Furthermore, in 2015 alone, acute upper respiratory infection (or presumed ARS) was one of the top 20 leading diagnoses for outpatient office visits.7
Pathogens and acute rhinosinusitis
Certain individuals may be predisposed to rhinosinusitis due to allergic rhinitis, allergy, smoking history, or a mechanical obstruction of the sinus ostium.2, 3 However, for most patients, upper respiratory tract infections are most often responsible. ARS is classically divided into 2 main subtypes based on the cause and duration of symptoms. Acute viral sinusitis lasts for less than 10 days with a rapid peak and then decline in nasal symptoms. The most common viruses isolated in ARS are rhinoviruses and coronaviruses, but respiratory syncytial virus (RSV), influenza virus, parainfluenza virus, enterovirus, and adenovirus can also be the causes.
If acute upper respiratory symptoms persist for greater than 10 days, or if symptoms initially improve but then worsen again, acute bacterial rhinosinusitis (ABRS) should be considered. In these patients, additional symptoms that are more likely to be observed include persistent purulent nasal drainage, severe facial pain, fever, and dental pain.1, 2, 3 ABRS generally develops following acute viral rhinosinusitis but overall is not a common occurrence, developing in only 0.5% to 2% of cases.8, 9
Pathogens most associated with acute bacterial rhinosinusitis include Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, Staphylococcus aureus, and Streptococcus pyogenes. Since the introduction of the Pneumococcal conjugate vaccine, the pathogen profile of ARS has changed with a declining incidence of S pneumoniae and increasing incidence of H influenzae, S pyogenes, and S aureus.10 Anaerobes such as Fusobacterium, Peptostreptococcus, and Bacteroides spp. account for a smaller percentage of ABRS cases.11, 12 Infections with gram-negative bacteria are unusual in community settings and the presence of Enterobacteriaceae or Pseudomonas spp. suggest a chronic underlying condition or a dental infection that has migrated to the sinuses.13, 14
Acute rhinosinusitis and asthma
It is well known that acute upper respiratory infections are capable of exacerbating preexisting asthma. However, one episode of ARS is not generally associated with having a higher risk of developing asthma per se. As discussed earlier and in the preceding chapters, there are specific pathogens associated with ARS that have also been associated with the development asthma. For example, RSV infections in infancy are a risk factor for developing allergic asthma in adolescence.15, 16, 17 Likewise, human rhinovirus in infants was also associated with higher incidence of having asthma as an adult.18, 19, 20, 21 Elucidating the key mechanistic links between specific viral (or bacterial) pathogens and development of new onset asthma is critical not only for better understanding of the link between the upper and lower respiratory tract but also for identifying potentially modifiable factors that could lead to disease prevention.
Chronic rhinosinusitis
In contrast to ARS, chronic rhinosinusitis (CRS) is characterized by chronic inflammation of the sinonasal mucosa. The diagnosis of CRS is made clinically in patients exhibiting anterior or posterior nasal drainage, nasal congestion, facial pain or pressure, and/or decreased sense of smell for greater than 12 weeks.2 Among patients reporting CRS symptoms, objective evidence of chronic inflammation should be confirmed either by direct visualization with nasal endoscopy or by sinus CT scan. A small subset of patients with CRS (∼20%) also has nasal polyps, which are benign inflammatory outgrowths of the sinonasal mucosa.2, 22 Such patients are aptly referred to as having CRS with nasal polyps (CRSwNP) leaving the remaining majority of patients with CRS as having CRS without nasal polyps (CRSsNP).
Using symptom-based criteria, the overall prevalence of CRS within a primary care US population was 11.9%.23 This is similar to earlier studies in Europe that reported the prevalence of CRS to be 10.9%.24 Among tertiary care populations, however, the prevalence of CRS is estimated to be even higher given a possible referral bias. In a longitudinal study of adults reporting CRS symptoms in a US general population, the lifetime prevalence of CRS was estimated to be 27.5% with an annual cumulative incidence of almost 2%.25 As a comparison, the lifetime prevalence of asthma in adults was 13.9% according to the 2016 National Health Interview Survey.7 The annual cost of these diseases has been estimated to be between $22 to $33 billion for CRS26, 27, 28 and $81.9 billion for asthma.29 Taken together, asthma and CRS are prevalent within the US population and can place large socioeconomic and financial burdens on affected patients and the health care system.
Chronic rhinosinusitis and asthma: clinical observations
The relationship between CRS and asthma remains of great interest from both a clinical as well as a pathophysiologic perspective. Although not every patient with CRS has asthma and vice versa, a strong and independent association between these conditions has been reported. In a large European study, asthma was more prevalent in patients with CRS than without (odds ratio [OR] 2.71).30 Furthermore, patients with CRSwNP were more likely to have asthma than those with CRSsNP,31 with one study reporting asthma in as many as 48.3% of patients with CRSwNP compared with only 16.5% with CRSsNP.32 A study from France also found that most of the asthmatics had abnormal sinus CT scans.33 Similarly, asthmatic patients with CRS were more likely to have nasal polyps than nonasthmatic patients with CRS.34
Exactly when (and why) patients develop CRS and asthma remains unclear. CRS is primarily a disease of adulthood, and given that the sinuses do not entirely form until late adolescence, other diseases, including cystic fibrosis, should first be considered in children presenting with nasal polyps.35 Although asthma can develop either in childhood or later in life, CRS is more significantly linked with adult-onset asthma.30 In particular, patients with CRS were more likely to develop nasal polyps if they had adult-onset versus childhood-onset disease.36 Asthma may precede the diagnosis of CRSwNP37 or develop following the diagnosis of CRSsNP.38 However, it is more likely that the time frame in which CRS and asthma develop is variable and depends on a variety of yet to be identified factors.
The association between CRS and asthma has important clinical implications. Among 250 patients with CRS at a tertiary care facility, those with asthma had significantly worse sinus CT and nasal endoscopic scores compared with patients with CRS without asthma.31, 39 Furthermore, the more severe the asthma, the greater the likelihood of having severe CRS.40 In the United States, the Severe Asthma Research Program identified distinct clinical phenotypes of severe asthma, with the cluster of asthmatics with the most severe airflow limitations at baseline being the same group with the highest percentage of reported sinus disease.41
Although asthma can influence sinonasal disease severity, CRS is also associated with more severe asthma. Patients with both CRS and asthma had lower lung function (percentage predicted forced expiratory volume in the first second of expiration and forced vital capacity) and quality of life when compared with patients with asthma alone.42 Furthermore, severe CRS is an independent risk factor for having frequent asthma exacerbations (OR 5.5),43 and patients with severe asthma were more likely to undergo sinus surgery for nasal polyps when compared with patients with mild asthma.44 Finally, when compared with patients with CRSwNP alone, those with both CRSwNP and asthma were significantly more likely to have enhanced sinonasal disease on sinus CT scan, to undergo more sinus surgeries and to be dependent on chronic oral corticosteroids for management of their disease.45 Taken together, these studies highlight the fact that CRS and asthma are frequently associated together in the clinical setting and the presence of one can significantly enhance the severity of the other. As such, it remains important to evaluate patients with CRS for asthma as well as asthmatic patients for CRS to optimize disease diagnosis and management.
Chronic rhinosinusitis and asthma: pathophysiologic observations
To better understand the mechanisms contributing to the clinical associations observed between CRS and asthma, nasal and pulmonary tissues would ideally be isolated at the same time from the same patient and then compared. Not surprisingly, such studies are exceedingly rare but in one such investigation a strong correlation in inflammatory profiles was observed between nasal polyp and bronchial biopsies.46 Larger mechanistic studies have also separately advanced the knowledge of the underlying cellular and molecular processes contributing to either asthma or CRS pathogenesis.47, 48, 49 Although an exhaustive summary of these findings is beyond the scope of the current review, focus will be placed on highlighting some of the key features of CRS especially in comparison to asthma.
As mentioned previously, the strongest association between asthma and CRS is observed among patients with CRSwNP. This is not surprising because, similar to what is observed in most of the asthmatics, nasal polyps in the United States and Europe are predominantly characterized by type 2 inflammation.50, 51, 52, 53 Eosinophils as well as their granule proteins (eg, eosinophil cationic protein, eosinophil peroxidase) are elevated in nasal polyps compared with healthy control sinonasal tissue.50, 54, 55 Other type 2 immune cells, including mast cells, basophils, and group 2 innate lymphoid cells, are also increased in nasal polyps.56, 57, 58, 59, 60, 61 This robust type 2 inflammatory response is orchestrated in part by elevated levels of prosurvival and chemotactic mediators such as interleukin 4 (IL-4), IL-5, IL-13, eotaxins, and thymic stromal lymphopoietin.55, 62, 63, 64
In contrast to CRSwNP, CRSsNP was originally characterized by type 1 inflammation due to elevated levels of interferon gamma (IFNγ) detected in this subtype.54, 63 However, subsequent studies have challenged this dichotomy and shown no differences in IFNγ levels observed between CRS subtypes.50, 55, 65 A more recent comprehensive analysis evaluating the expression of several inflammatory mediators in different sinonasal tissues in CRS suggested that CRSsNP is instead a heterogenous disease.66 In this work, 23% of patients with CRSsNP had a predominant type 1 phenotype as assessed by IFNγ gene expression levels above the 95th percentile of what was observed in healthy controls. Furthermore, 36% of patients with CRSsNP had increased gene expression of type 2 inflammatory mediators above the 95th percentile of what was measured in controls.66 The clinical relevance of these different endotypes, and why CRSsNP in general has a weaker association with asthma compared with CRSwNP, is unclear and remains the focus of ongoing investigations.
The adaptive immune response has also been characterized in CRS with both T and B cells thought to play important roles. T cells that produce type 2 inflammatory cytokines are increased in nasal polyps.50, 67 In addition, naïve B cells and plasma cells are elevated in nasal polyps when compared with healthy controls.68, 69, 70 Total levels of antibodies (including immunoglobulin E [IgE] and IgG) are significantly higher in nasal polyps when compared with peripheral blood of matched patients as well as healthy sinonasal tissue.69 The function of this local antibody production as well as the specificity of the antibodies generated is still largely unknown. However, IgG antibodies that are self-reactive71 and IgE antibodies against S aureus and its enterotoxins72 as well as other bacteria such as H influenzae 73 have been described.
Besides having an enhanced immunologic response, CRS is also characterized by a dysfunctional epithelial barrier with tight junctions, host defense proteins, and mucociliary clearance factors all found to be impaired.47, 74, 75 These findings, in most regard, are similar to what has been reported in the lower respiratory tract of asthma.76, 77 A weakened epithelial barrier can have profound consequences, because the upper and lower respiratory tracts are constantly exposed to millions of microbes daily. In a healthy host, these microbes are routinely cleared without inciting an inflammatory response, but in CRS such processes are impaired.78 It remains unknown if the impaired epithelial barrier leads to increased pathogen recognition by the host or if the exposure to pathogens in the respiratory tract leads to epithelial barrier damage. Either way, the endpoint could be the initiation and potentiation of a robust immunologic response.
Pathogens and chronic rhinosinusitis
S aureus is known to colonize the nasal mucosa,79 and it has been one of the most studied microbes in CRS. One hypothesis suggests that the bacteria itself is directly involved in driving CRS pathogenesis, damaging the epithelial barrier and activating the host immune response. Ex vivo studies of nasal polyp explants infected with S aureus showed reduced gene expression levels of various tight junction proteins when compared with similarly infected healthy nasal mucosa.80 In addition, in a separate study, S aureus was reported to bind to TLR2 and induce type 2 cytokine release from cultured epithelial cells.81 This in turn could potentially explain how colonization with S aureus in the nasal cavity could lead to the development of a chronic immunologic response. However, what is not addressed in these studies is why only some patients who are colonized with S aureus go on to develop CRS. Furthermore, in patients with CRSwNP, the presence of S aureus was associated with more severe sinus inflammation on CT scans but not sinonasal symptoms, suggesting this pathogen alone is not fully responsible for all aspects of disease.82
Another hypothesis is that the immune response to S aureus is important in CRS pathogenesis. In support of this, type 2 inflammatory mediators were significantly elevated in nasal polyps of patients with detectable levels of specific IgE antibodies to S aureus enterotoxins (SAE), but no correlation was found between these markers and the presence of S aureus in the tissue.83 Specific antibodies to SAEs can induce basophil degranulation72 and mast cell activation,84, 85 providing another possible mechanism by which S aureus could contribute to chronic type 2 inflammation. However, in a separate study, although patients with CRSwNP were more likely to have elevated serum levels of specific IgE to SAE compared with healthy controls, there was no association between these antibody levels and sinus disease severity as assessed by CT scan.86
It is important to note that not all patients with CRS are colonized with S aureus, with one study reporting colonization rates of 27.3% in CRS versus 33.3% in healthy controls.87 Likewise, only 27.8% of patients who were colonized with S aureus had detectable specific IgE to SAE.87 However, both colonization with S aureus and the presence of specific IgE to SAE were significantly higher in those patients who had both CRSwNP and asthma (66.7% and 53.8%, respectively).87 In a meta-analysis, nasal S aureus colonization was only modestly associated with asthma prevalence (OR 1.19) in the general population or, after adjusting for study bias, among a subset of patients with CRS (OR 1.21).88 However, patients with detectable specific IgE to SAE were more likely to have severe asthma89, 90, 91 as well as reduced lung function and increased airway reversibility to bronchodilation.92 Taken together, specific IgE to SAE and/or S aureus may be important in CRS pathogenesis and related to comorbid asthma in a select group of patients, but the exact mechanisms for these associations are still unclear.
In addition to S aureus, other bacteria including coagulase-negative staphylococci, H influenzae, S pneumoniae, Moraxella catarrhalis, Corynebacterium spp., and Propionibacterium acnes have been detected in sinonasal samples of patients with CRS either by nasal culture or by measuring bacteria-specific 16S ribosomal DNA.93, 94, 95, 96, 97 Total bacterial counts did not correlate with sinus disease severity98 but, when compared with healthy controls, one study found patients with CRS to have significantly lower Actinobacteria levels (and lower Corynebacterium spp.) as well as reduced relative abundance of the genus Peptoniphilus.99
Differences have also been reported in the nasal microbiome in patients with CRS with or without asthma. In one study, those with asthma had increased abundance of the phylum Proteobacteria, M catarrhalis, and Staphylococcus xylosus and decreased abundance of genus Corynebacterium, Geobacter anodireducens/sulfurreducens, and Pelomonas puraquae.100 In a separate study of 111 CRS cases, no significant difference in the diversity of bacterial species was noted between patients with CRS with and without asthma.101 Although, the relative abundance of Streptococcus spp. was significantly higher in patients with CRS with asthma as compared with without.101 Furthermore, asthmatic patients with CRS with emergency room (ER) visits for asthma had significantly higher relative abundance of Proteobacteria phylum (likely due to increased Burkholderia spp.) than patients who did not visit the ER for symptoms.101 These findings are interesting given that Streptococcus has been linked to asthma development in children102 and Burkholderia is associated with decreased lung function in patients with cystic fibrosis.103 However, how these bacteria are specifically involved in CRS pathogenesis is not known.
By comparing the frequency, abundance, and diversity of bacteria in patients with CRS with that observed in healthy controls, the ideal goal would be to identify particular bacteria that could be protective against or predispose toward developing the disease. Unfortunately, most studies to date have been descriptive without causality shown. In addition, there are significant variations between studies with differences in the patient demographics, where within the sinonasal cavity samples were collected, how the data were generated, and the methods by which the data were analyzed. To date, no one particular pathogen has been implicated in CRS, but an overall increased abundance and decreased diversity of the microbiome has been observed.104, 105 It is thus likely that differences in the microbiome are important in CRS pathogenesis and in the link between CRS and asthma. However, further studies are needed to investigate what these key factors could be.
Future considerations/summary
There is a strong and important relationship between the upper and lower respiratory tracts whereby inflammation in one environment can influence the other. In acute rhinosinusitis, exposures to viral and bacterial pathogens are the primary driver for acute inflammation in the nose, which can then lead to exacerbations of asthma. In contrast, it remains unclear what precise role infections (or colonization) in the airways play in the development of CRS, but other factors, including the presence of an impaired epithelial barrier and dysregulated immune responses, can promote the chronic inflammation that is observed in CRS. Clinically, CRS is strongly associated with asthma with both diseases sharing similar underlying inflammatory processes. In conclusion, significant advancements have been made in identifying sinus infections and inflammation as important in asthma pathogenesis, but additional work is needed to further define the specific mechanisms responsible for connecting the nose with the lungs.
Footnotes
Disclosure Statements: A.G. Staudacher and W.W. Stevens have no financial disclosures.
References
- 1.Rosenfeld R.M., Piccirillo J.F., Chandrasekhar S.S., et al. Clinical practice guideline (update): adult sinusitis executive summary. Otolaryngol Head Neck Surg. 2015;152:598–609. doi: 10.1177/0194599815574247. [DOI] [PubMed] [Google Scholar]
- 2.Fokkens WJ, Lund VJ, Mullol J, et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2012. Rhinol Suppl 2012; 23:p. 3. preceding table of contents, 1-298. [PubMed]
- 3.Peters A.T., Spector S., Hsu J., et al. Diagnosis and management of rhinosinusitis: a practice parameter update. Ann Allergy Asthma Immunol. 2014;113:347–385. doi: 10.1016/j.anai.2014.07.025. [DOI] [PubMed] [Google Scholar]
- 4.Bhattacharyya N. Contemporary assessment of the disease burden of sinusitis. Am J Rhinol Allergy. 2009;23:392–395. doi: 10.2500/ajra.2009.23.3355. [DOI] [PubMed] [Google Scholar]
- 5.Bhattacharyya N., Grebner J., Martinson N.G. Recurrent acute rhinosinusitis: epidemiology and health care cost burden. Otolaryngol Head Neck Surg. 2012;146:307–312. doi: 10.1177/0194599811426089. [DOI] [PubMed] [Google Scholar]
- 6.Smith S.S., Evans C.T., Tan B.K., et al. National burden of antibiotic use for adult rhinosinusitis. J Allergy Clin Immunol. 2013;132:1230–1232. doi: 10.1016/j.jaci.2013.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.NCHS. National Ambulatory Medical Care Survey. 2015 https://www.cdc.gov/nchs/data/ahcd/namcs_summary/2015_namcs_web_tables.pdf Available at: Accessed April 11, 2019. [Google Scholar]
- 8.Gwaltney J.M., Jr. Acute community-acquired sinusitis. Clin Infect Dis. 1996;23:1209–1223. doi: 10.1093/clinids/23.6.1209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Piccirillo J.F. Clinical practice. Acute bacterial sinusitis. N Engl J Med. 2004;351:902–910. doi: 10.1056/NEJMcp035553. [DOI] [PubMed] [Google Scholar]
- 10.Brook I., Gober A.E. Frequency of recovery of pathogens from the nasopharynx of children with acute maxillary sinusitis before and after the introduction of vaccination with the 7-valent pneumococcal vaccine. Int J Pediatr Otorhinolaryngol. 2007;71:575–579. doi: 10.1016/j.ijporl.2006.10.025. [DOI] [PubMed] [Google Scholar]
- 11.Brook I. Bacteriology of acute and chronic frontal sinusitis. Arch Otolaryngol Head Neck Surg. 2002;128:583–585. doi: 10.1001/archotol.128.5.583. [DOI] [PubMed] [Google Scholar]
- 12.Brook I. The role of anaerobic bacteria in sinusitis. Anaerobe. 2006;12:5–12. doi: 10.1016/j.anaerobe.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 13.Brook I. Microbiology of intracranial abscesses associated with sinusitis of odontogenic origin. Ann Otol Rhinol Laryngol. 2006;115:917–920. doi: 10.1177/000348940611501211. [DOI] [PubMed] [Google Scholar]
- 14.Brook I. Sinusitis of odontogenic origin. Otolaryngol Head Neck Surg. 2006;135:349–355. doi: 10.1016/j.otohns.2005.10.059. [DOI] [PubMed] [Google Scholar]
- 15.Wu P., Dupont W.D., Griffin M.R., et al. Evidence of a causal role of winter virus infection during infancy in early childhood asthma. Am J Respir Crit Care Med. 2008;178:1123–1129. doi: 10.1164/rccm.200804-579OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sigurs N., Gustafsson P.M., Bjarnason R., et al. Severe respiratory syncytial virus bronchiolitis in infancy and asthma and allergy at age 13. Am J Respir Crit Care Med. 2005;171:137–141. doi: 10.1164/rccm.200406-730OC. [DOI] [PubMed] [Google Scholar]
- 17.Feldman A.S., He Y., Moore M.L., et al. Toward primary prevention of asthma. Reviewing the evidence for early-life respiratory viral infections as modifiable risk factors to prevent childhood asthma. Am J Respir Crit Care Med. 2015;191:34–44. doi: 10.1164/rccm.201405-0901PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jackson D.J., Gangnon R.E., Evans M.D., et al. Wheezing rhinovirus illnesses in early life predict asthma development in high-risk children. Am J Respir Crit Care Med. 2008;178:667–672. doi: 10.1164/rccm.200802-309OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lemanske R.F., Jr., Jackson D.J., Gangnon R.E., et al. Rhinovirus illnesses during infancy predict subsequent childhood wheezing. J Allergy Clin Immunol. 2005;116:571–577. doi: 10.1016/j.jaci.2005.06.024. [DOI] [PubMed] [Google Scholar]
- 20.Busse W.W., Lemanske R.F., Jr., Gern J.E. Role of viral respiratory infections in asthma and asthma exacerbations. Lancet. 2010;376:826–834. doi: 10.1016/S0140-6736(10)61380-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Soto-Quiros M., Avila L., Platts-Mills T.A., et al. High titers of IgE antibody to dust mite allergen and risk for wheezing among asthmatic children infected with rhinovirus. J Allergy Clin Immunol. 2012;129:1499–1505. doi: 10.1016/j.jaci.2012.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Orlandi R.R., Kingdom T.T., Hwang P.H. International consensus statement on allergy and rhinology: rhinosinusitis executive summary. Int Forum Allergy Rhinol. 2016;6(Suppl 1):S3–S21. doi: 10.1002/alr.21694. [DOI] [PubMed] [Google Scholar]
- 23.Hirsch A.G., Stewart W.F., Sundaresan A.S., et al. Nasal and sinus symptoms and chronic rhinosinusitis in a population-based sample. Allergy. 2017;72:274–281. doi: 10.1111/all.13042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hastan D., Fokkens W.J., Bachert C., et al. Chronic rhinosinusitis in Europe–an underestimated disease. A GA(2)LEN study. Allergy. 2011;66:1216–1223. doi: 10.1111/j.1398-9995.2011.02646.x. [DOI] [PubMed] [Google Scholar]
- 25.Sundaresan A.S., Hirsch A.G., Young A.J., et al. Longitudinal evaluation of chronic rhinosinusitis symptoms in a population-based sample. J Allergy Clin Immunol Pract. 2018;6:1327–1335. doi: 10.1016/j.jaip.2017.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bhattacharyya N., Orlandi R.R., Grebner J., et al. Cost burden of chronic rhinosinusitis: a claims-based study. Otolaryngol Head Neck Surg. 2011;144:440–445. doi: 10.1177/0194599810391852. [DOI] [PubMed] [Google Scholar]
- 27.Rudmik L. Economics of chronic rhinosinusitis. Curr Allergy Asthma Rep. 2017;17:20. doi: 10.1007/s11882-017-0690-5. [DOI] [PubMed] [Google Scholar]
- 28.Smith K.A., Orlandi R.R., Rudmik L. Cost of adult chronic rhinosinusitis: a systematic review. Laryngoscope. 2015;125:1547–1556. doi: 10.1002/lary.25180. [DOI] [PubMed] [Google Scholar]
- 29.Nurmagambetov T., Kuwahara R., Garbe P. The economic burden of asthma in the United States, 2008-2013. Ann Am Thorac Soc. 2018;15:348–356. doi: 10.1513/AnnalsATS.201703-259OC. [DOI] [PubMed] [Google Scholar]
- 30.Jarvis D., Newson R., Lotvall J., et al. Asthma in adults and its association with chronic rhinosinusitis: the GA2LEN survey in Europe. Allergy. 2012;67:91–98. doi: 10.1111/j.1398-9995.2011.02709.x. [DOI] [PubMed] [Google Scholar]
- 31.Batra P.S., Tong L., Citardi M.J. Analysis of comorbidities and objective parameters in refractory chronic rhinosinusitis. Laryngoscope. 2013;123(Suppl 7):S1–S11. doi: 10.1002/lary.24418. [DOI] [PubMed] [Google Scholar]
- 32.Promsopa C., Kansara S., Citardi M.J., et al. Prevalence of confirmed asthma varies in chronic rhinosinusitis subtypes. Int Forum Allergy Rhinol. 2016;6:373–377. doi: 10.1002/alr.21674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bresciani M., Paradis L., Des Roches A., et al. Rhinosinusitis in severe asthma. J Allergy Clin Immunol. 2001;107:73–80. doi: 10.1067/mai.2001.111593. [DOI] [PubMed] [Google Scholar]
- 34.Pearlman A.N., Chandra R.K., Chang D., et al. Relationships between severity of chronic rhinosinusitis and nasal polyposis, asthma, and atopy. Am J Rhinol Allergy. 2009;23:145–148. doi: 10.2500/ajra.2009.23.3284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hamilos D.L. Chronic rhinosinusitis in patients with cystic fibrosis. J Allergy Clin Immunol Pract. 2016;4:605–612. doi: 10.1016/j.jaip.2016.04.013. [DOI] [PubMed] [Google Scholar]
- 36.Staniorski C.J., Price C.P.E., Weibman A.R., et al. Asthma onset pattern and patient outcomes in a chronic rhinosinusitis population. Int Forum Allergy Rhinol. 2018;8:495–503. doi: 10.1002/alr.22064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tan B.K., Chandra R.K., Pollak J., et al. Incidence and associated premorbid diagnoses of patients with chronic rhinosinusitis. J Allergy Clin Immunol. 2013;131:1350–1360. doi: 10.1016/j.jaci.2013.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hirsch A.G., Yan X.S., Sundaresan A.S., et al. Five-year risk of incident disease following a diagnosis of chronic rhinosinusitis. Allergy. 2015;70:1613–1621. doi: 10.1111/all.12759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.ten Brinke A., Grootendorst D.C., Schmidt J.T., et al. Chronic sinusitis in severe asthma is related to sputum eosinophilia. J Allergy Clin Immunol. 2002;109:621–626. doi: 10.1067/mai.2002.122458. [DOI] [PubMed] [Google Scholar]
- 40.Lin D.C., Chandra R.K., Tan B.K., et al. Association between severity of asthma and degree of chronic rhinosinusitis. Am J Rhinol Allergy. 2011;25:205–208. doi: 10.2500/ajra.2011.25.3613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Moore W.C., Meyers D.A., Wenzel S.E., et al. Identification of asthma phenotypes using cluster analysis in the Severe Asthma Research Program. Am J Respir Crit Care Med. 2010;181:315–323. doi: 10.1164/rccm.200906-0896OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ek A., Middelveld R.J., Bertilsson H., et al. Chronic rhinosinusitis in asthma is a negative predictor of quality of life: results from the Swedish GA(2)LEN survey. Allergy. 2013;68:1314–1321. doi: 10.1111/all.12222. [DOI] [PubMed] [Google Scholar]
- 43.ten Brinke A., Sterk P.J., Masclee A.A., et al. Risk factors of frequent exacerbations in difficult-to-treat asthma. Eur Respir J. 2005;26:812–818. doi: 10.1183/09031936.05.00037905. [DOI] [PubMed] [Google Scholar]
- 44.Wu W., Bleecker E., Moore W., et al. Unsupervised phenotyping of Severe Asthma Research Program participants using expanded lung data. J Allergy Clin Immunol. 2014;133:1280–1288. doi: 10.1016/j.jaci.2013.11.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stevens W.W., Peters A.T., Hirsch A.G., et al. Clinical characteristics of patients with chronic rhinosinusitis with nasal polyps, asthma, and aspirin-exacerbated respiratory disease. J Allergy Clin Immunol Pract. 2017;5:1061–1070. doi: 10.1016/j.jaip.2016.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hakansson K., Bachert C., Konge L., et al. Airway inflammation in chronic rhinosinusitis with nasal polyps and asthma: the united airways concept further supported. PLoS One. 2015;10:e0127228. doi: 10.1371/journal.pone.0127228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schleimer R.P. Immunopathogenesis of chronic rhinosinusitis and nasal polyposis. Annu Rev Pathol. 2017;12:331–357. doi: 10.1146/annurev-pathol-052016-100401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Holgate S.T., Wenzel S., Postma D.S., et al. Asthma. Nat Rev Dis Primers. 2015;1:15025. doi: 10.1038/nrdp.2015.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ray A., Raundhal M., Oriss T.B., et al. Current concepts of severe asthma. J Clin Invest. 2016;126:2394–2403. doi: 10.1172/JCI84144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhang N., Van Zele T., Perez-Novo C., et al. Different types of T-effector cells orchestrate mucosal inflammation in chronic sinus disease. J Allergy Clin Immunol. 2008;122:961–968. doi: 10.1016/j.jaci.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 51.Wang X., Zhang N., Bo M., et al. Diversity of TH cytokine profiles in patients with chronic rhinosinusitis: a multicenter study in Europe, Asia, and Oceania. J Allergy Clin Immunol. 2016;138:1344–1353. doi: 10.1016/j.jaci.2016.05.041. [DOI] [PubMed] [Google Scholar]
- 52.Caminati M., Pham D.L., Bagnasco D., et al. Type 2 immunity in asthma. World Allergy Organ J. 2018;11:13. doi: 10.1186/s40413-018-0192-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kubo M. Innate and adaptive type 2 immunity in lung allergic inflammation. Immunol Rev. 2017;278:162–172. doi: 10.1111/imr.12557. [DOI] [PubMed] [Google Scholar]
- 54.Van Zele T., Claeys S., Gevaert P., et al. Differentiation of chronic sinus diseases by measurement of inflammatory mediators. Allergy. 2006;61:1280–1289. doi: 10.1111/j.1398-9995.2006.01225.x. [DOI] [PubMed] [Google Scholar]
- 55.Stevens W.W., Ocampo C.J., Berdnikovs S., et al. Cytokines in chronic rhinosinusitis. role in eosinophilia and aspirin-exacerbated respiratory disease. Am J Respir Crit Care Med. 2015;192:682–694. doi: 10.1164/rccm.201412-2278OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shaw J.L., Ashoori F., Fakhri S., et al. Increased percentage of mast cells within sinonasal mucosa of chronic rhinosinusitis with nasal polyp patients independent of atopy. Int Forum Allergy Rhinol. 2012;2:233–240. doi: 10.1002/alr.21021. [DOI] [PubMed] [Google Scholar]
- 57.Takabayashi T., Kato A., Peters A.T., et al. Glandular mast cells with distinct phenotype are highly elevated in chronic rhinosinusitis with nasal polyps. J Allergy Clin Immunol. 2012;130:410–420. doi: 10.1016/j.jaci.2012.02.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kagoya R., Kondo K., Baba S., et al. Correlation of basophil infiltration in nasal polyps with the severity of chronic rhinosinusitis. Ann Allergy Asthma Immunol. 2015;114:30–35. doi: 10.1016/j.anai.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 59.Mahdavinia M., Carter R.G., Ocampo C.J., et al. Basophils are elevated in nasal polyps of patients with chronic rhinosinusitis without aspirin sensitivity. J Allergy Clin Immunol. 2014;133:1759–1763. doi: 10.1016/j.jaci.2013.12.1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Poposki J.A., Klingler A.I., Tan B.K., et al. Group 2 innate lymphoid cells are elevated and activated in chronic rhinosinusitis with nasal polyps. Immun Inflamm Dis. 2017;5:233–243. doi: 10.1002/iid3.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Shaw J.L., Fakhri S., Citardi M.J., et al. IL-33-responsive innate lymphoid cells are an important source of IL-13 in chronic rhinosinusitis with nasal polyps. Am J Respir Crit Care Med. 2013;188:432–439. doi: 10.1164/rccm.201212-2227OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hulse K.E., Stevens W.W., Tan B.K., et al. Pathogenesis of nasal polyposis. Clin Exp Allergy. 2015;45:328–346. doi: 10.1111/cea.12472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Van Bruaene N., Perez-Novo C.A., Basinski T.M., et al. T-cell regulation in chronic paranasal sinus disease. J Allergy Clin Immunol. 2008;121:1435–1441. doi: 10.1016/j.jaci.2008.02.018. 41. [DOI] [PubMed] [Google Scholar]
- 64.Nagarkar D.R., Poposki J.A., Tan B.K., et al. Thymic stromal lymphopoietin activity is increased in nasal polyps of patients with chronic rhinosinusitis. J Allergy Clin Immunol. 2013;132:593–600. doi: 10.1016/j.jaci.2013.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Van Bruaene N., C P.N., Van Crombruggen K., et al. Inflammation and remodelling patterns in early stage chronic rhinosinusitis. Clin Exp Allergy. 2012;42:883–890. doi: 10.1111/j.1365-2222.2011.03898.x. [DOI] [PubMed] [Google Scholar]
- 66.Tan B.K., Klingler A.I., Poposki J.A., et al. Heterogeneous inflammatory patterns in chronic rhinosinusitis without nasal polyps in Chicago, Illinois. J Allergy Clin Immunol. 2017;139:699–703.e7. doi: 10.1016/j.jaci.2016.06.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Derycke L., Eyerich S., Van Crombruggen K., et al. Mixed T helper cell signatures in chronic rhinosinusitis with and without polyps. PLoS One. 2014;9:e97581. doi: 10.1371/journal.pone.0097581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gevaert P., Holtappels G., Johansson S.G., et al. Organization of secondary lymphoid tissue and local IgE formation to Staphylococcus aureus enterotoxins in nasal polyp tissue. Allergy. 2005;60:71–79. doi: 10.1111/j.1398-9995.2004.00621.x. [DOI] [PubMed] [Google Scholar]
- 69.Hulse K.E., Norton J.E., Suh L., et al. Chronic rhinosinusitis with nasal polyps is characterized by B-cell inflammation and EBV-induced protein 2 expression. J Allergy Clin Immunol. 2013;131:1075–1083. doi: 10.1016/j.jaci.2013.01.043. 83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gevaert P., Nouri-Aria K.T., Wu H., et al. Local receptor revision and class switching to IgE in chronic rhinosinusitis with nasal polyps. Allergy. 2013;68:55–63. doi: 10.1111/all.12054. [DOI] [PubMed] [Google Scholar]
- 71.Tan B.K., Li Q.Z., Suh L., et al. Evidence for intranasal antinuclear autoantibodies in patients with chronic rhinosinusitis with nasal polyps. J Allergy Clin Immunol. 2011;128:1198–1206. doi: 10.1016/j.jaci.2011.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chen J.B., James L.K., Davies A.M., et al. Antibodies and superantibodies in patients with chronic rhinosinusitis with nasal polyps. J Allergy Clin Immunol. 2017;139:1195–1204. doi: 10.1016/j.jaci.2016.06.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Takeda K., Sakakibara S., Yamashita K., et al. Allergic conversion of protective mucosal immunity against nasal bacteria in patients with chronic rhinosinusitis with nasal polyposis. J Allergy Clin Immunol. 2018;143(3):1163–1175.e15. doi: 10.1016/j.jaci.2018.07.006. [DOI] [PubMed] [Google Scholar]
- 74.Steelant B., Seys S.F., Boeckxstaens G., et al. Restoring airway epithelial barrier dysfunction: a new therapeutic challenge in allergic airway disease. Rhinology. 2016;54:195–205. doi: 10.4193/Rhino15.376. [DOI] [PubMed] [Google Scholar]
- 75.Zhang N., Van Crombruggen K., Gevaert E., et al. Barrier function of the nasal mucosa in health and type-2 biased airway diseases. Allergy. 2016;71:295–307. doi: 10.1111/all.12809. [DOI] [PubMed] [Google Scholar]
- 76.Gon Y., Hashimoto S. Role of airway epithelial barrier dysfunction in pathogenesis of asthma. Allergol Int. 2018;67:12–17. doi: 10.1016/j.alit.2017.08.011. [DOI] [PubMed] [Google Scholar]
- 77.Holgate S.T. The sentinel role of the airway epithelium in asthma pathogenesis. Immunol Rev. 2011;242:205–219. doi: 10.1111/j.1600-065X.2011.01030.x. [DOI] [PubMed] [Google Scholar]
- 78.Hamilos D.L. Drivers of chronic rhinosinusitis: inflammation versus infection. J Allergy Clin Immunol. 2015;136:1454–1459. doi: 10.1016/j.jaci.2015.10.011. [DOI] [PubMed] [Google Scholar]
- 79.von Eiff C., Becker K., Machka K., et al. Nasal carriage as a source of Staphylococcus aureus bacteremia. Study Group. N Engl J Med. 2001;344:11–16. doi: 10.1056/NEJM200101043440102. [DOI] [PubMed] [Google Scholar]
- 80.Altunbulakli C., Costa R., Lan F., et al. Staphylococcus aureus enhances the tight junction barrier integrity in healthy nasal tissue, but not in nasal polyps. J Allergy Clin Immunol. 2018;142:665–668. doi: 10.1016/j.jaci.2018.01.046. [DOI] [PubMed] [Google Scholar]
- 81.Lan F., Zhang N., Holtappels G., et al. Staphylococcus aureus induces a mucosal type 2 immune response via epithelial cell-derived cytokines. Am J Respir Crit Care Med. 2018;198:452–463. doi: 10.1164/rccm.201710-2112OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Clark D.W., Wenaas A., Citardi M.J., et al. Chronic rhinosinusitis with nasal polyps: elevated serum immunoglobulin E is associated with Staphylococcus aureus on culture. Int Forum Allergy Rhinol. 2011;1:445–450. doi: 10.1002/alr.20079. [DOI] [PubMed] [Google Scholar]
- 83.Corriveau M.N., Zhang N., Holtappels G., et al. Detection of Staphylococcus aureus in nasal tissue with peptide nucleic acid-fluorescence in situ hybridization. Am J Rhinol Allergy. 2009;23:461–465. doi: 10.2500/ajra.2009.23.3367. [DOI] [PubMed] [Google Scholar]
- 84.Patou J., Gevaert P., Van Zele T., et al. Staphylococcus aureus enterotoxin B, protein A, and lipoteichoic acid stimulations in nasal polyps. J Allergy Clin Immunol. 2008;121:110–115. doi: 10.1016/j.jaci.2007.08.059. [DOI] [PubMed] [Google Scholar]
- 85.Zhang N., Holtappels G., Gevaert P., et al. Mucosal tissue polyclonal IgE is functional in response to allergen and SEB. Allergy. 2011;66:141–148. doi: 10.1111/j.1398-9995.2010.02448.x. [DOI] [PubMed] [Google Scholar]
- 86.Tripathi A., Conley D.B., Grammer L.C., et al. Immunoglobulin E to staphylococcal and streptococcal toxins in patients with chronic sinusitis/nasal polyposis. Laryngoscope. 2004;114:1822–1826. doi: 10.1097/00005537-200410000-00027. [DOI] [PubMed] [Google Scholar]
- 87.Van Zele T., Gevaert P., Watelet J.B., et al. Staphylococcus aureus colonization and IgE antibody formation to enterotoxins is increased in nasal polyposis. J Allergy Clin Immunol. 2004;114:981–983. doi: 10.1016/j.jaci.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 88.Kim Y.C., Won H.K., Lee J.W., et al. Staphylococcus aureus nasal colonization and asthma in adults: systematic review and meta-Analysis. J Allergy Clin Immunol Pract. 2018;7(2):606–615.e9. doi: 10.1016/j.jaip.2018.08.020. [DOI] [PubMed] [Google Scholar]
- 89.Bachert C., Gevaert P., Howarth P., et al. IgE to Staphylococcus aureus enterotoxins in serum is related to severity of asthma. J Allergy Clin Immunol. 2003;111:1131–1132. [PubMed] [Google Scholar]
- 90.Tanaka A., Suzuki S., Ohta S., et al. Association between specific IgE to Staphylococcus aureus enterotoxins A and B and asthma control. Ann Allergy Asthma Immunol. 2015;115:191–197. doi: 10.1016/j.anai.2015.06.017. [DOI] [PubMed] [Google Scholar]
- 91.Bachert C., van Steen K., Zhang N., et al. Specific IgE against Staphylococcus aureus enterotoxins: an independent risk factor for asthma. J Allergy Clin Immunol. 2012;130:376–381. doi: 10.1016/j.jaci.2012.05.012. [DOI] [PubMed] [Google Scholar]
- 92.Kowalski M.L., Cieslak M., Pérez-Novo C.A., et al. Clinical and immunological determinants of severe/refractory asthma (SRA): association with Staphylococcal superantigen-specific IgE antibodies. Allergy. 2011;66:32–38. doi: 10.1111/j.1398-9995.2010.02379.x. [DOI] [PubMed] [Google Scholar]
- 93.Biel M.A., Brown C.A., Levinson R.M., et al. Evaluation of the microbiology of chronic maxillary sinusitis. Ann Otol Rhinol Laryngol. 1998;107:942–945. doi: 10.1177/000348949810701107. [DOI] [PubMed] [Google Scholar]
- 94.Chan J., Hadley J. The microbiology of chronic rhinosinusitis: results of a community surveillance study. Ear Nose Throat J. 2001;80:143–145. [PubMed] [Google Scholar]
- 95.Boase S., Foreman A., Cleland E., et al. The microbiome of chronic rhinosinusitis: culture, molecular diagnostics and biofilm detection. BMC Infect Dis. 2013;13:210. doi: 10.1186/1471-2334-13-210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Cope E.K., Goldberg A.N., Pletcher S.D., et al. Compositionally and functionally distinct sinus microbiota in chronic rhinosinusitis patients have immunological and clinically divergent consequences. Microbiome. 2017;5:53. doi: 10.1186/s40168-017-0266-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Feazel L.M., Robertson C.E., Ramakrishnan V.R., et al. Microbiome complexity and Staphylococcus aureus in chronic rhinosinusitis. Laryngoscope. 2012;122:467–472. doi: 10.1002/lary.22398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ramakrishnan V.R., Feazel L.M., Abrass L.J., et al. Prevalence and abundance of Staphylococcus aureus in the middle meatus of patients with chronic rhinosinusitis, nasal polyps, and asthma. Int Forum Allergy Rhinol. 2013;3:267–271. doi: 10.1002/alr.21101. [DOI] [PubMed] [Google Scholar]
- 99.Mahdavinia M., Engen P.A., LoSavio P.S., et al. The nasal microbiome in patients with chronic rhinosinusitis: Analyzing the effects of atopy and bacterial functional pathways in 111 patients. J Allergy Clin Immunol. 2018;142:287–290. doi: 10.1016/j.jaci.2018.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Chalermwatanachai T., Vilchez-Vargas R., Holtappels G., et al. Chronic rhinosinusitis with nasal polyps is characterized by dysbacteriosis of the nasal microbiota. Sci Rep. 2018;8:7926. doi: 10.1038/s41598-018-26327-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Yang H.J., LoSavio P.S., Holtappels G., et al. Association of nasal microbiome and asthma control in patients with chronic rhinosinusitis. Clin Exp Allergy. 2018;48(12):1744–1747. doi: 10.1111/cea.13255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Teo S.M., Mok D., Pham K., et al. The infant nasopharyngeal microbiome impacts severity of lower respiratory infection and risk of asthma development. Cell Host Microbe. 2015;17:704–715. doi: 10.1016/j.chom.2015.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Navarro J., Rainisio M., Harms H.K., et al. Factors associated with poor pulmonary function: cross-sectional analysis of data from the ERCF. European Epidemiologic Registry of Cystic Fibrosis. Eur Respir J. 2001;18:298–305. doi: 10.1183/09031936.01.00068901. [DOI] [PubMed] [Google Scholar]
- 104.Mahdavinia M., Keshavarzian A., Tobin M.C., et al. A comprehensive review of the nasal microbiome in chronic rhinosinusitis (CRS) Clin Exp Allergy. 2016;46:21–41. doi: 10.1111/cea.12666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Chalermwatanachai T., Velasquez L.C., Bachert C. The microbiome of the upper airways: focus on chronic rhinosinusitis. World Allergy Organ J. 2015;8:3. doi: 10.1186/s40413-014-0048-6. [DOI] [PMC free article] [PubMed] [Google Scholar]