Abstract
The Coronavirus Disease 2019 (COVID-19) pandemic has thus far caused a total of 81,747 confirmed cases with 3283 deaths in China and more than 370,000 confirmed cases including over 16,000 deaths around the world by March 24, 2020. This issue has received extensive attention from the international community and has become a major public health priority. As the pandemic progresses, it is regrettable to know the health care workers, including anesthesiologists, are being infected constantly. Therefore, we would like to share our firsthand practical experience and perspective in China, focusing on the personal protection of health care workers and the risk factors related to their infection, based on the different stages of the COVID-19 epidemic in China.
As of this writing, it has been 2 weeks since the World Health Organization (WHO) officially announced the Coronavirus Disease 2019 (COVID-19) as a pandemic. The COVID-19 has spread rapidly, as it took only 30 days to expand from Wuhan, Hubei Province to the rest of thearea of Mainland China. The epidemic curve of onset of new cases in China peaked onJanuary 24–26, 2020 and began to decline afterFebruary 11, 2020.1 By March 24, 2020, a total of 81,747 confirmed cases hadbeen reported in China, with more than 370,000 confirmed cases, including over 16,000 deaths, had beenreported in 190 countries, areas, or territories all over the world.2 This pandemic has received widespread attention from the international community and has become a major public health priority that requires the collective efforts of people all around the world. Among the health care practitioners working against the COVID-19 pandemic, anesthesiologists are in a strategic position to assist their hospitals from a patient care perspective and through various leadership roles.
AN OVERVIEW OF COVID-19 AND THE ROLES OF HEALTH CARE WORKERS
COVID-19 is an infectious disease caused by a newly discovered coronavirus (Severe Acute Respiratory Syndrome Coronavirus 2 [SARS-CoV-2]).3 The outbreak started in December 2019, and then spread at an unprecedented rate throughout the world. The disease causes respiratory illness with symptoms including cough, fever, and, in more severe cases, difficulty breathing. Althoughmost people recover from the disease without needing special treatment, COVID-19 can be serious and even fatal. Older people and people with coexisting medical conditions could be more vulnerable to becoming severely ill. The outbreak of COVID-19 could be particularly risky for health care workers because of their ongoing professional exposure to the virus. Atpresent, health care practitioners are the most valuable resource for every country to combat the disease, and we believe that health care workers need to be well protected first, especially anesthesiologists who play a vital role in emergency airway management, intensive care, and perioperative medicine. Here, we review the different stages of COVID-19 development in China, focusing on the personal protection of health care workers and the risk factors related to their infection.
THE FIRST STAGE: UNKNOWN DISEASE, POORLY PROTECTED HEALTH CARE WORKERS
The initial cases of COVID-19 were identified from December 2019 to January 2020 in Wuhan, China, and were reported as “pneumonia of unknown etiology” when the disease was not yet officially named.3 During that period of time, the public, as well as the health care workers, knew little about such a new virus. Althougha few doctors in Wuhan noticed that the pneumonia transmitted unusually rapidly, pointing out its similarities with SARS (caused by SARS-CoV), unfortunately, they did not receive enough public attention.
By January 22, 2020, 571 confirmed cases (375 from Hubei Province) were reported to the National Health Commission of the People’s Republic of China covering 25 provinces (autonomous regions and municipalities) of country, including 95 severe cases and 17 deaths (all from Hubei Province).4 Outside China, a total of 10 confirmed cases from 7 countries, areas, or territories were reported.5
Due to the lack of understanding of this novel coronavirus and its highly contagious nature, at this stage, personal protection standards for medical workers were not established, and many health care workers with poor protection were infected and several even died as a result. At this time, the infection rate ranged from 3.5% to 29% among health care workers in different hospitals in the epicenter of Wuhan according to previous reports,6,7 when the initial source of the novel coronavirus still remained unknown. However, more and more evidence supported that the virus spread from humantohuman and also across generations of cases.3 Accordingly, WHO assessed the risk of this event to be very high in China.5
On January 23, 2020, the central government of China imposed a lockdown in Wuhan City, and other cities in Hubei province thereafter, in an effort to quarantine the epicenter of the COVID-19 outbreak and to stop the virus from spreading further across the nation. This took place a week before WHO declared the outbreak a Public Health Emergency of International Concern (PHEIC).8 At this stage, the general population had lack awareness of the disease, with barely any personal protection, when the number of patients was increasing sharply, leading to the frequent infection of health care workers.
THE SECOND STAGE: DISEASE GRADUALLY RECOGNIZED; INADEQUATELY PROTECTED HEALTH CARE WORKERS DUE TO LACK OF SUPPLIES
After the recognition of efficient human-to-human transmission of the disease, Wuhan went into lockdown as a critical step in national antiepidemic effort. At this point, infection-control regulations were established, health care workers were extensively educated,and appropriate personal protective equipment was required. Correspondingly, different levels of precautions were set up according to the patient care settings and situations in hospitals.
However, the Wuhan lockdown took place right before the Chinese New Year’s Eve, which is the most important traditional Chinese holiday, with a 7-day-long legal vacation. Particularly in the year 2020, this vacation was extended to 14 days to keep citizens at home to reduce the risk of spreading the novel coronavirus. By extending the holiday, the downtime of factories was correspondingly extended, which resulted in significantly reduced production of personal protective equipment that failed to meet the clinical demands.
During this period of time, the number of confirmed cases in China was still increasing rapidly. We were deeply distressed to see that by February 11, 2020, a total of 1716 health care workers were confirmed with COVID-19, including 5 deaths.1 When the vacation ended by February 13, 2020, the total confirmed cases surpassed 50,000, with cases reported from all 31 provinces (autonomous regions and municipalities) in China.9 At this point, the disease was being gradually appreciated, and the importance of wearing personal protective equipment being realized, but this was still not enough. We knew that stronger measures were urgently needed to control the spread of the epidemic and to better protect medical workers when they provide medical services for the rapidly increasing number ofpatients.
THE THIRD STAGE: THE SEVERITY OF THE DISEASE ACKNOWLEDGED; FULLY PROTECTED HEALTH CARE WORKERS
With confirmed cases doubling every 4 days, China launched house-to-house visits in Wuhan on February 7, 2020, making every effort to hospitalize every confirmed patient. For this purpose, 2 brand new emergency specialty field hospitals, Huoshenshan and Leishenshan, specialized for COVID-19 patients, had been built within 10 days, accommodating 2600 beds in total. These field hospitals began to receive patients on February 2 and 8, 2020. To meet the need of the dramatically increased number ofpatients, 16 exhibition centers and stadiums in Wuhan were transformed into makeshift hospitals successively, with a total capacity of more than 10,000 beds, focusing on treating mild cases of COVID-19 patients. On average, every 1 in 4 confirmed cases in Wuhan wastreated in these makeshift hospitals.
At the same time, hundreds of medical teams from all over China arrived in Wuhan and other cities in Hubei Province to manage COVID-19 alongside local medical staff on the frontline. In total, more than 42,600 health care workers, including 790 anesthesiologists, from different regions of the country made up 346 medical teams that shifted and joined the frontline.
The National Health Commission of the People’s Republic of China and the professional committees of the Chinese Medical Association have also quickly established corresponding standards, guidelines, and recommendations in this unprecedented period to better inform and guide the health care workers.
For example, the Joint Task Force of the Chinese Society of Anesthesiology and the Chinese Association of Anesthesiologists established their recommendations regarding the perioperative management of patients infected with the novel coronavirus, emphasizing the importance of appropriate personal protection for health care workers.10 The highest level of precaution, so-called full precaution, is mandatory for high-risk exposure, a disposable surgical cap, test-fit N95 masks or respirators, gloves, goggles or face shield, gown, and fluid-resistant shoe covers. We would like to point out that the key element of full precaution is the complete coverage of the head and facial skin, which does not necessarily mean a conjoined hood or even powered air-purifying respirator system as previously reported.11 Based on our experience, a surgical mask in addition to the N95 mask to cover the remaining bare skin on face, together with goggles and face shield, have worked well (Figure 1).
Figure 1.

Dr Kaicheng Song with the precaution of personal protective equipment. Dr Song is an attending anesthesiologist in Department of Anesthesiology, PUMCH, Beijing, China. He voluntarily joined the national medical team for Wuhan on February 7, 2020, since then he has worked in the intensive care unit of Zhongfaxincheng campus of Tongji Hospital affiliated to Huazhong University of Science and Technology. At the time of this writing, Dr Song, together with 10 other anesthesiologists and operating room nurses from PUMCH, are still fighting COVID-19 at the frontlines in Wuhan. (Photograph by Dr Kaicheng Song.) COVID-19 indicates Coronavirus Disease 2019; PUMCH, Peking Union Medical College Hospital.
It was also gratifying to see that, with the steady progress of resumption of work and production, the shortage of personal protective equipment was then greatly relieved. Every health care worker caring for COVID-19 patients was able to be adequately protected at this moment.
With all these efforts, we are very grateful to see that the transmission of the novel coronavirus has been greatly controlled, and the number of new COVID-19 cases has significantly declined in China. No confirmed cases were reported in 10 provinces (autonomous regions and municipalities) by March 24, 2020, and the total number of confirmed new cases has decreased to <5000 in China.12
All the makeshift hospitals in Wuhan were closed by March 10, 2020, and more than one-third of the medical staffs temporarily assisting in Hubei Province returned to their hometown after their mission in Hubei. It is reassuring that none of these health care workers were infected with the novel coronavirus through their providing medical care. Although,up to now, there areno data available showing the best way for protection, no health care workers became infected once appropriate personal protective equipment was used. We believe that the right attitude may seem like a little thing, but it makes abig difference. The strategies of consistently using strong precautions have worked well and were also acceptable in such a battle.
When most of the hospitals in China are fighting the COVID-19 epidemic, life still needs to go on. For health care practitioners in the majority of Chinese hospitals, many patients had other diseases that required care. In this situation, appropriate clinical recommendations have been gradually established and become available in most hospitals to alleviate public anxiety. Accordingly, we have also set up our own standard precautions at Peking Union Medical College Hospital during COVID-19 epidemic, hoping to help our staff members to use the proper personal precautions in different clinical settings, trying to reduce the consumption of disposable personal protective equipment in daily clinical practice (Figure 2).
Figure 2.
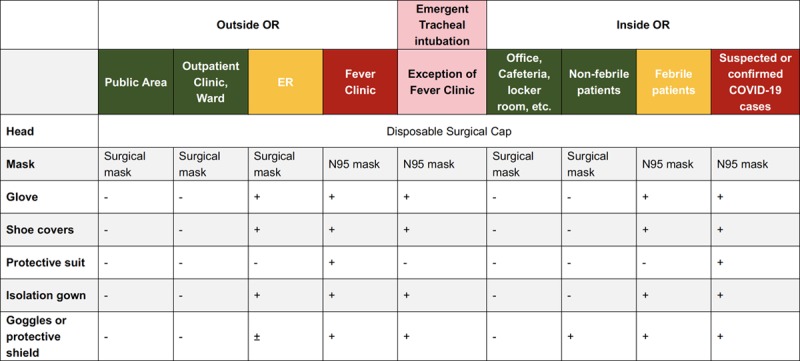
Standardized precautions at Peking Union Medical College Hospital for anesthesiologists in different clinical settings. (1) Green cells: clean or relatively clean area (hospital public area, office, outpatient clinic, ward, etc) or low-risk procedure; yellow cells: possibly contaminated area or medium-risk procedure (ER, elective operations with febrile patients, etc); red cells: contaminated area or high-risk medical procedure (emergent intubation outside OR, fever clinic, suspected or confirmed COVID-19 cases, etc). (2) Hand hygiene is mandatory. (3) The disposable protective materials and other medical wastes should be handled according to ER or ward regulations to avoid cross-contamination. COVID-19 indicates Coronavirus Disease 2019; ER, emergency room; OR, operating room.
Considerable clinical experience has been accumulated through the above 3 stages in the past two and ahalf months. First, once a novel disease is discovered, it should receive enough attention at the earliest stage to realize its characteristics and to formulate the corresponding countermeasures as soon as possible. Second, organizational arrangements and relevant support through the joint efforts of all stakeholders are vital in combating the epidemic. Third, as medical professionals, especially as anesthesiologists, it is also important that the academic societies, associations, and scientific journals are supposed to play their professional leading role in this battle against COVID-19. Moreover, all individuals have their own responsibility to the public. We recommend that everyone maintain social distancing, make sure to practice hand hygiene, and wear a facemask in public, especially in crowded areas during the COVID-19 pandemic.
The public and personal health situation in China has been very much improved at the writing of this article. However, the rest of the world is now experiencing a critical and extremely difficult time. We are sad to learn that there are nearly 5000 health care workers infected in Italy and more than 3000 medical staff infected in Spain. We pay the highest respect to every health care worker’s dedication in this war against the novel coronavirus. We appreciate having this opportunity to share our firsthand and practical experience with you all to finallywin the antivirus war, hoping sincerely that every health care worker can be well protected. Together, we are stronger. With the joint efforts from people all around the world, this pandemic will eventually be overcome. We look forward to this day.
DISCLOSURES
Name: Weiyun Chen, MD.
Contribution: This author helped draft the manuscript.
Name: Yuguang Huang, MD.
Contribution: This author helped review and revise the manuscript.
This manuscript was handled by: Thomas R. Vetter, MD, MPH.
FOOTNOTES
GLOSSARY
- COVID-19
- Coronavirus Disease 2019
- ER
- emergency room
- OR
- operating room
- PHEIC
- Public Health Emergency of International Concern
- PUMCH
- Peking Union Medical College Hospital
- SARS
- Severe Acute Respiratory Syndrome
- SARS-Cov-2
- Severe Acute Respiratory Syndrome Coronavirus 2
- WHO
- World Health Organization
Funding: None.
The authors declare no conflicts of interest.
Reprints will not be available from the authors.
REFERENCES
- 1.Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Chinese J Epidemiol. 2020;41:145–151(in Chinese). [Google Scholar]
- 2.Coronavirus disease 2019 (COVID-19) Situation Report - 64. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200324-sitrep-64-covid-19.pdf?sfvrsn=703b2c40_2. Accessed March 25, 2020.
- 3.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020;382:1199–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Situation report of COVID-19 (Jan 22) from the National Health Commission of the People’s Republic of China. Available at: http://www.nhc.gov.cn/xcs/yqtb/202001/5d19a4f6d3154b9fae328918ed2e3c8a.shtml. Accessed March 25, 2020. [DOI] [PMC free article] [PubMed]
- 5.Novel Coronavirus (2019-nCoV) Situation Report - 3 23 January 2020. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200123-sitrep-3-2019-ncov.pdf?sfvrsn=d6d23643_8. Accessed March 25, 2020.
- 6.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020 February 28 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020 February 7 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Novel Coronavirus (2019-nCoV) Situation Report - 11. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200131-sitrep-11-ncov.pdf?sfvrsn=de7c0f7_4. Accessed March 25, 2020.
- 9.Situation report of COVID-19 (Feb 13) from the National Health Commission of the People’s Republic of China. Available at: http://www.nhc.gov.cn/xcs/yqtb/202002/553ff43ca29d4fe88f3837d49d6b6ef1.shtml. Accessed March 25, 2020. [DOI] [PMC free article] [PubMed]
- 10.Chen X, Liu Y, Gong Y, et al. Perioperative management of patients infected with the novel coronavirus: recommendation from the Joint Task Force of the Chinese Society of Anesthesiology and the Chinese Association of Anesthesiologists. Anesthesiology. 2020 March 19 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meng L, Qiu H, Wan L, et al. Intubation and ventilation amid the COVID-19 outbreak: Wuhan’s experience. Anesthesiology. 2020 March 19 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Situation report of COVID-19 (Mar 24) from the National Health Commission of the People’s Republic of China. Available at: http://www.nhc.gov.cn/xcs/yqtb/202003/e6c12d0c2cf04474944187f4088dc021.shtml. Accessed March 25, 2020. [DOI] [PMC free article] [PubMed]


