As a result of the Coronavirus Disease 2019 (COVID-19) outbreak and the projected financial and workforce burden it will place on most health care systems, we intend to outline basic guidelines that may help hospital systems and specifically spine departments. Our aim is to provide a fluid framework with which surgeons and hospital staff can triage spinal surgical candidates. While most spine procedures are theoretically “elective” in that the patient was evaluated in an office setting and later provided an operative appointment date—many cases are not truly elective. For many spine patients, a significant delay in care may result in a progression of extremity weakness and pain with possibly less predictable improvements after surgery. Furthermore, in many conditions, such as myelopathy, delaying surgical decompression may allow for neurological deterioration and irreversible patient harm. In this current era of uncertainty, there is not a reliable timeline for the normalization of elective surgical scheduling, which might take months or years.
Although there is little debate regarding the need to perform spine surgery for acute trauma, epidural abscess, or tumors, there is a need to clarify and set initial guidelines for spinal conditions with associated myelopathy, radiculopathy, and motor deficits. We acknowledge that the dissemination of the COVID-19 and management and utilization of hospital resources are of the utmost importance and recognize that postoperative complications in the form of respiratory distress from COVID-19 infection should also be a concern for all patients. Respiratory issues are only one medical risk that should be considered during the preoperative patient optimization and weighed against the risks of continued nonsurgical management of progressive conditions. To this end, we provide a framework for institutions and spine departments that may help guide practices to provide a strategy to continue essential surgical spine care. Below are some key points of consideration that should be considered with the understanding that modifications may be necessary given the dynamic nature of the pandemic:
Real-time and evolving assessments regarding the current state of the hospital and the COVID-19 census. There should be daily updates of the hospital’s ability to rapidly transition care toward increasing respiratory support capacity and directing operative staff to support these endeavors including floor/ward nurse support.
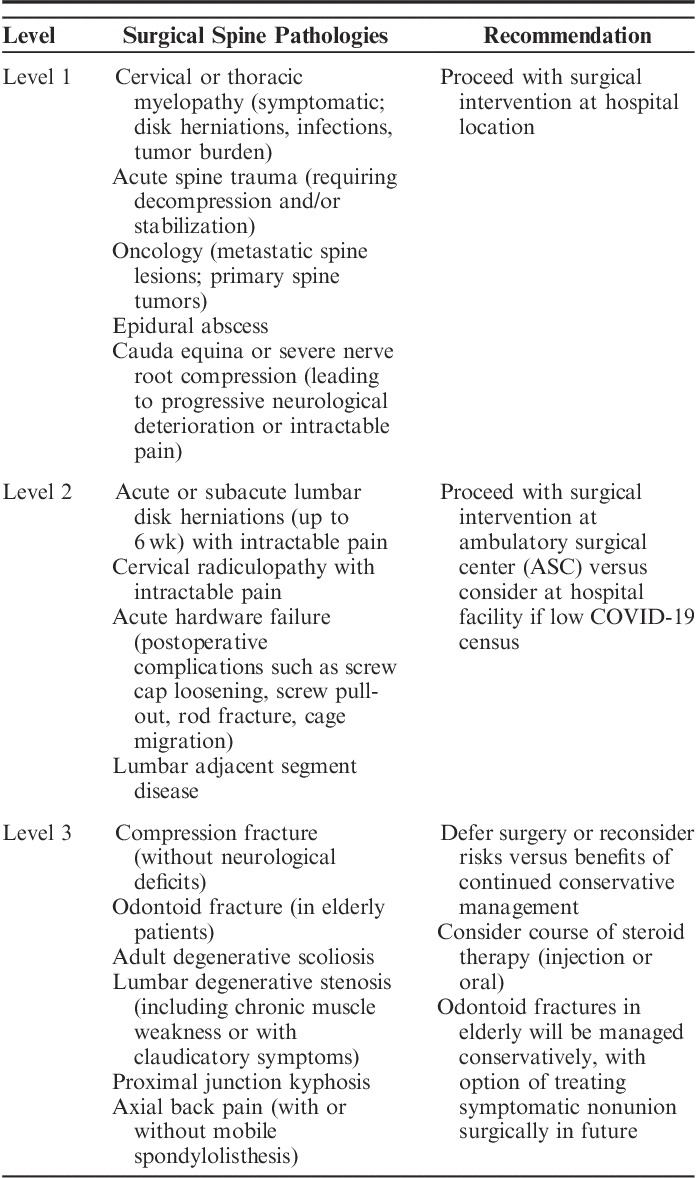
The urgency of surgical intervention for each patient should be agreed upon by members of the spine department. We encourage a department meeting or to review the urgency of cases for the proceeding 2 weeks initially and then subsequently on a weekly basis. The included guidelines can be used to supplement a discussion (Table 1). This will allow an assessment of the current surgical necessity and provide a sense of cohesiveness and uniformity of surgical urgency to the hospital staff about on-going spine cases.
It should not be assumed surgical delays will be for a short time period. The risk of postponing a spine surgery should be assessed, understanding the eventual surgery may occur in 3–4 months from the present. Patient quality of life and the risk of neurological deterioration should be considered over this time frame with frequent follow-up utilizing telemedicine if necessary.
For spine surgeries that cannot be postponed, alternative surgical plans and less invasive options may be considered depending on hospital bed availability. Surgeons and nursing staff should emphasize minimizing postoperative length of stay through measures such as early rehabilitation, intraoperative technique, and pain management.
TABLE 1.
Rothman Institute Guidelines for Spine Surgery in the COVID-19 Era
Footnotes
Dr Schroeder has received funds to travel from AO Spine and Medtronic. Dr Vaccaro has consulted or has done independent contracting for DePuy, Medtronic, Stryker Spine, Globus, Stout Medical, Gerson Lehrman Group, Guidepoint Global, Medacorp, Innovative Surgical Design, Orthobullets, Ellipse, and Vertex. He has also served on the scientific advisory board/board of directors/committees for Flagship Surgical, AO Spine, Innovative Surgical Design, and Association of Collaborative Spine Research. Dr Vaccaro has received royalty payments from Medtronic, Stryker Spine, Globus, Aesculap, Thieme, Jaypee, Elsevier, and Taylor Francis/Hodder and Stoughton. He has stock/stock option ownership interests in Replication Medica, Globus, Paradigm Spine, Stout Medical, Progressive Spinal Technologies, Advanced Spinal Intellectual Properties, Spine Medica, Computational Biodynamics, Spinology, In Vivo, Flagship Surgical, Cytonics, Bonovo Orthopaedics, Electrocore, Gamma Spine, Location Based Intelligence, FlowPharma, R.S.I., Rothman Institute and Related Properties, Innovative Surgical Design, and Avaz Surgical. He has also served as deputy editor/editor of Spine. In addition, Dr Vaccaro has also provided expert testimony. The remaining authors declare no conflict of interest.


