Abstract
Objective
To describe and evaluate a risk-stratified triage pathway for inpatient urology consultations during the SARS-CoV-2 (COVID-19) pandemic. This pathway seeks to outline a urology patient care strategy that reduces the transmission risk to both healthcare providers and patients, reduces the healthcare burden, and maintains appropriate patient care.
Materials and Methods
Consultations to the urology service during a 3-week period (March 16 to April 2, 2020) were triaged and managed via one of 3 pathways: Standard, Telemedicine, or High-Risk. Standard consults were in-person consults with non COVID-19 patients, High-Risk consults were in-person consults with COVID-19 positive/suspected patients, and Telemedicine consults were telephonic consults for low-acuity urologic issues in either group of patients. Patient demographics, consultation parameters and consultation outcomes were compared to consultations from the month of March 2019. Categorical variables were compared using Chi-square test and continuous variables using Mann-Whitney U test. A P value <.05 was considered significant.
Results
Between March 16 and April 2, 2020, 53 inpatient consultations were performed. By following our triage pathway, a total of 19/53 consultations (35.8%) were performed via Telemedicine with no in-person exposure, 10/53 consultations (18.9%) were High-Risk, in which we strictly controlled the urology team member in-person contact, and the remainder, 24/53 consultations (45.2%), were performed as Standard in-person encounters. COVID-19 associated consultations represented 18/53 (34.0%) of all consultations during this period, and of these, 8/18 (44.4%) were managed successfully via Telemedicine alone. No team member developed COVID-19 infection.
Conclusion
During the COVID-19 pandemic, most urology consultations can be managed in a patient and physician safety-conscious manner, by implementing a novel triage pathway.
As of April 9, 2020, the World Health Organization reported nearly 400,000 cases of and 12,740 deaths attributed to COVID-19 in the United States (US) alone.1 In the state of Michigan, over 80% of cases and deaths are occurring in metropolitan Detroit, making it the third largest epicenter per population in the US,2 , 3 causing unprecedented changes to the healthcare environment. In the context of rapidly evolving guidelines for personal protective equipment and diagnostic testing for healthcare workers,4 as well as the internal reassignment of clinical team members to other patient care teams, implementation of new departmental protocols were needed. The present report details the efforts of the Urology Department (Henry Ford Hospital, Detroit, MI) to develop and implement an inpatient consultation triage pathway to minimize unnecessary exposure for providers and patients, while providing safe and effective care during the COVID-19 pandemic.
MATERIALS AND METHODS
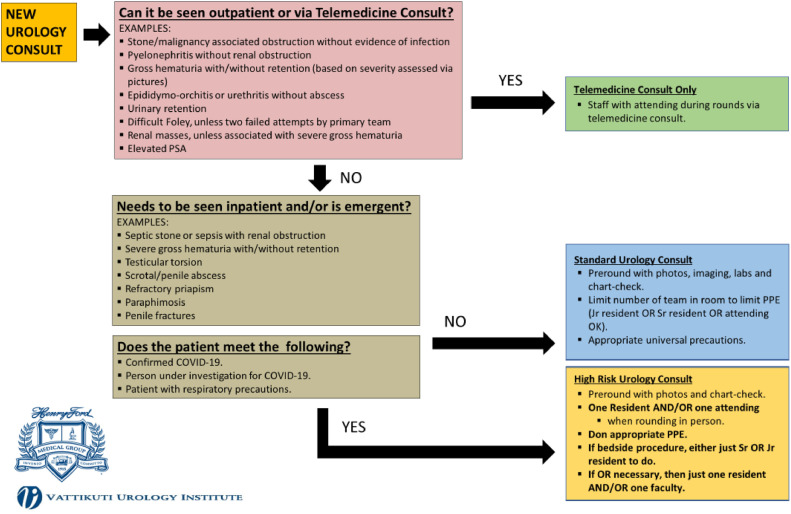
This study was conducted as a part of necessary transition of care delivery at a tertiary care institution. As the COVID-19 pandemic spread in the state of Michigan, there was a rapid increase in COVID-19 positive patients within the health system, with an accordant increase in COVID-19 suspected and positive inpatient and emergency department consultations. Thus, on March 16, 2020, the decision was made to implement a new Urology Consultation Triage Pathway (Fig. 1 ).
Figure 1.
New algorithm for triaging inpatient urology consultations during COVID-19 pandemic.“Color version available online.”
Briefly, all consultations for the Urology service were assessed based on clinical context (complexity and time-sensitivity of urological issue/s), resources available with the consulting teams to address minor urological issues, and the COVID-19 status of the patient (confirmed, suspected, not suspected) at time of consultation. Patients were then triaged into one of 3 pathways:
-
(1)
Telemedicine: Patients with nonurgent/nonemergent inpatient issues were managed with telemedicine consultation composed of chart review and discussion with primary team providers, with or without patient telephone interview (depending upon patient's clinical status). These patients could be COVID-19 positive, suspected or negative.
-
(2)
Standard: Patients with urgent/emergent inpatient needs but not proven/suspected COVID-19 positive had standard Urology consultation (though still minimizing the number of urology residents and/or attendings involved in direct patient care).
-
(3)
High-risk: Patients with urgent/emergent inpatient needs who were suspected/proven COVID-19 positive were deemed High-risk urology consultations (seen by only 1 urology resident and/or attending, especially if a bedside procedure or operative intervention was necessary). Personal protective equipment were donned, including N95 masks, per CDC and hospital policy.
A prospective database was maintained for this period, tracking the management of patients in each of the 3 triage pathways. Data were collected for a 3-week period (from March 16, 2020 to April 2, 2020), and analyzed between April 4 and April 7, 2020. Data points included age, sex, race, pertinent medical/surgical history, primary hospital diagnosis and consulting service. Management and treatment variables included reason for consultation, type of consultation performed, intervention performed, and COVID-19 status (at time of consultation and final). Interventions were defined as nonprocedural recommendations (medication and/or planned follow-up), operative procedure, bedside procedures (catheter placement or change, cystoscopy, incision and drainage, penile injections/aspiration/irrigation, etc.), or Interventional Radiology (IR) procedures.
In order to compare consultation workflow in the period preceding the implementation of the pathway, similar data points were extracted for all urology consultations for the month of March 2019 (March 1, 2019 to March 31, 2019). This latter cohort served as a control group, with no ongoing regional or national health care stressors.
Categorical variables were compared using Chi-square test (with Yates correction for n<5) or Fisher's exact test as appropriate, and continuous variables using Mann-Whitney U test. A P value <.05 was considered significant. Statistical analyses were done using MS Excel version 15 (Microsoft, Redmond, WA) and IBM SPSS version 21 (IBM, Armonk, NY). The study was approved by the International Review Board committee and exempted from informed consent under local institutional protocols.
RESULTS
Table 1 shows the demographics and consultation characteristics of urology consultations during the specified time periods. A total of 154 consultations were analyzed, 101 consultations from March 2019 and 53 from March 2020. The median age, sex, race and consulting service were similar between the groups. The most common reasons for consultation were hematuria, urinary retention and kidney stones and this was not significantly different between the 2019 and 2020 groups (P = .2). A greater proportion of patients were managed nonprocedurally in March 2020 compared to March 2019 (66% vs 51.5%), with fewer patients undergoing operative intervention (9.4% vs 21.7%) and more undergoing IR interventions (9.4% vs 0.9%) (P = .03). In March 2019, only Standard consultations were performed. In March 2020, following implementation of our triage pathway, a total of 19/53 consultations (35.8%) were performed via Telemedicine with no in-person exposure, 10/53 consultations (18.9%) were High-risk, and the remainder, 24/53 consultations (45.2%), were performed as Standard in-person encounters.
Table 1.
Demographics and consultation parameters for inpatient consultations from March 1-31, 2019 and March 16-April 2, 2020
| March 2019 | March 2020 | P Value | |
|---|---|---|---|
| Total patients | 101 | 53 | |
| Consults/day (Median, IQR) | 3.2 (1.5-4) | 2.8 (1-4) | .6 |
| Age (Median, IQR) years | 63 (43-73) | 59 (44-72) | .8 |
| Sex, n (%) | .7 | ||
| Male | 68 (67.3) | 37 (69.8) | |
| Female | 33 (23.7) | 16 (30.2) | |
| Race, n (%) | .2 | ||
| African American | 42 (37.1) | 27 (50.9) | |
| Caucasian | 40 (35.4) | 11 (20.8) | |
| Hispanic | 3 (2.6) | 1 (1.9) | |
| Unrecorded | 16 (14.2) | 14 (26.4) | |
| Primary hospital diagnosis, n (%) | .02 | ||
| Pulmonary | 5 (4.9) | 10 (19.2) | |
| Cardiac | 5 (4.9) | 0 (0) | |
| Genitourinary | 72 (71.3) | 27 (51.9) | |
| Other | 19 (18.8) | 15 (28.8) | |
| Consulting service, n (%) | .4 | ||
| Emergency department | 57 (56.4) | 27 (50.9) | |
| Medicine | 33 (32.7) | 15 (28.3) | |
| Surgery | 1 (0.9) | 4 (7.5) | |
| Intensive care unit | 10 (9.9) | 7 (13.2) | |
| Reason for consult, n (%) | .2 | ||
| Hematuria | 21 (20.8) | 11 (20.8) | |
| Urinary retention | 11 (10.9) | 15 (28.3) | |
| Abscess/GU infection | 12 (11.9) | 4 (7.5) | |
| Kidney stone | 17 (16.8) | 9 (17.0) | |
| Hydronephrosis | 14 (13.9) | 4 (7.5) | |
| Nephrostomy tube malfunction | 1 (0.9) | 2 (3.8) | |
| Scrotal pain | 3 (2.9) | 3 (5.6) | |
| Other | 22 (21.7) | 5 (9.4) | |
| Consult type, n (%) | <.01 | ||
| Standard | 101 (100) | 24 (45.2) | |
| Telemedicine | - | 19 (35.8) | |
| High-risk | - | 10 (18.9) | |
| Intervention, n (%) | .03 | ||
| Nonprocedural recommendations | 52 (51.5) | 35 (66.0) | |
| Operating room | 22 (21.7) | 5 (9.4) | |
| Bedside procedure/catheter placement | 26 (25.7) | 8 (15.1) | |
| Interventional radiology | 1 (0.9) | 5 (9.4) |
Table 2 shows consultation characteristics for March 2020.
Table 2.
Consult parameters and COVID-19 status, by consult type for March 16-April 2, 2020
| Standard (n = 24) | Telemedicine (n = 19) | High-Risk (n = 10) | |
|---|---|---|---|
| Reason for consultation, n (%) | |||
| Hematuria | 7 (29.2) | 3 (15.8) | 1 (10) |
| Urinary retention | 2 (8.3) | 6 (31.6) | 7 (70) |
| Abscess/GU infection | 3 (12.5) | 1 (5.2) | 0 |
| Kidney stone | 4 (16.7) | 4 (21.1) | 1 (10) |
| Hydronephrosis | 2 (8.3) | 1 (5.2) | 1 (10) |
| Nephrostomy tube malfunction | 0 | 2 (10.5) | 0 |
| Scrotal pain | 3 (12.5) | 0 | 0 |
| Other | 3 (12.5) | 2 (10.5) | 0 |
| Intervention performed, n (%) | |||
| Nonprocedural recommendations | 15 (62.5) | 16 (84.2) | 4 (40) |
| Operating room | 5 (20.9) | 0 | 0 |
| Bedside procedure/catheter placement | 3 (12.5) | 0 | 5 (50) |
| Interventional radiology | 1 | 3 (15.8) | 1 (10) |
| COVID-19 status at time of consultation, n (%) | |||
| Positive | 0 | 2 (10.5) | 4 (40) |
| Pending | 0 | 6 (31.6) | 6 (60) |
| Not tested | 24 (100) | 11 (57.9) | 0 |
| COVID-19 final status, n (%) | |||
| Positive | - | 4 (21.1) | 4 (40) |
| Negative | - | 4 (21.1) | 6 (60) |
| Not tested | 24 (100) | 11 (57.9) | 0 |
Consultations managed by Telemedicine were most commonly for urinary retention 6/16 (31.6%), kidney stones 4/19 (21.1%) and hematuria 3/19 (15.8%), compared to the High-risk consultations, where the vast majority were for urinary retention 7/10 (70%). Of the Telemedicine consultations, nearly 85% (16/19) were managed nonprocedurally (neither an intervention from urology or IR was required).
None of the residents or faculty caring for urology consultation patients during the March 2020 period developed symptoms suggestive of COVID-19 and/or tested positive for it.
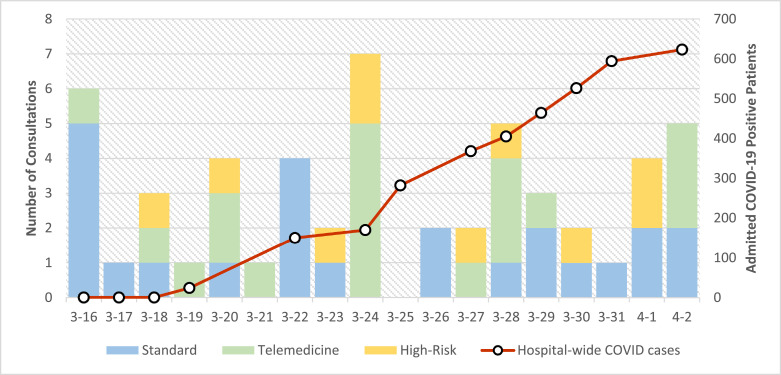
Figure 2 depicts the number of COVID positive patients admitted to our hospital over the study period, as well as, the number of Standard, Telemedicine, and High-risk consultations performed on each day after the triage pathway was implemented.
Figure 2.
Consultation type, and COVID-19 cases, by day, from March 16-April 2, 2020. “Color version available online."
COMMENT
In response to the COVID-19 pandemic, all aspects of medical and surgical patient care have been transformed. Because a significant proportion of COVID-19 infections are caused by undocumented exposure,5 decreasing in-person contact with emergency department and hospitalized patients is of utmost importance. The described consultation triage pathway allows for necessary urgent and emergent urologic care, while minimizing exposure that would be associated with standard urology consultations.
During the March 2020 study period, we managed over half of all consultations (54.7%) using a modified consultation type (Telemedicine or High-risk), and for some days, the majority of consultations were managed using Telemedicine alone.
Importantly, demographics and consultation characteristics, with the exception of primary hospital diagnosis, were not significantly different in March 2019 and March 2020, suggesting that March 2020 (other than the presence of the COVID-19 pandemic), represented a typical month of urologic consultations. More consults during 2020 had a primary pulmonary diagnosis, likely reflecting the presence of the COVID-19 pandemic.
Notably, fewer consults in March 2020, 5/53 (9.4%), resulted in operative intervention compared to 22/101 (21.7%) consults in March 2019. This can, in part, be attributed to the Henry Ford Health System policy enacted on March 15 2020, which postponed all nontime sensitive surgeries. Unsurprisingly, more patients were managed with nonprocedural recommendations and IR procedures in March 2020, which likely reflects both departmental and hospital-wide efforts to preserve operating room space and all associated resources.
Of note, while 34.0% of consultations in the 2020 study period were for COVID-19 status positive or COVID-19 status pending patients, our hospital has quickly become a majority COVID-19 facility, and we expect the majority of urology consultations moving forward during this pandemic to be classified as either Telemedicine or High-risk, and managed accordingly.
Contemporaneously, and in conjunction with development of this pathway, we restructured our urology service into 2 teams to optimize patient care and minimize unnecessary exposures, described similarly at other institutions.6 Each week, “Team A” covers urologic care across our covered hospitals, including additional satellite facilities, while “Team B” covers COVID-19 and non-COVID-19 units as needed. These teams switch responsibilities each week. This system has allowed us to help in other hospital departments and units, while ensuring adequate coverage for any needed urologic care.
Limitations of the study include the following. There are a relatively small number of consultations tracked over a short period of time. The control group, while it appeared well-matched in our analysis, may represent a different cohort of consultations than our study group. The pathway we utilized is nonvalidated. Lastly, we have no follow-up to identify outcomes associated with the consultations performed during the study.
The authors recognize that by using this pathway, there may be a suggestion of decreased value associated with some urology consultations. In addition to urologic procedures and recommendations, urologists provide reassurance about and explanations for urologic problems, while facilitating and encouraging outpatient follow-up.7 , 8 Additionally, the reimbursement pattern for Telemedicine consultations was evolving during the study period. As of March 30, 2020, the Accreditation Council for Graduate Medical Education Program requirements VI.A.2.(1).(b) and revised Centers for Medicare and Medicaid rules now permit faculty members to provide direct supervision through telecommunications technology. These changes allow residents to perform Telehealth consultations, while being staffed remotely, as billable encounters.9, 10, 11
By utilizing Telemedicine during consultation with patients with nonurgent urologic problems, we have been able to provide appropriate care and counseling, while mitigating the surge of future outpatient urologic visits and care following the COVID-19 crisis.9
CONCLUSION
Implementing a urology consultation triage pathway allowed for appropriate inpatient urologic consultation management while minimizing the risk of exposure for both patients and urology team members during the COVID-19 pandemic. Given the fluidity of the current circumstances, we acknowledge the need to continue to adapt to any new and unforeseen circumstances, but we hope that this pathway may provide a useful framework for other urology departments.
Footnotes
Funding:None.
Disclosure:None of the authors have any relevant disclosures, and none of the authors have any financial or non-financial interests that may be relevant to the submitted work.
References
- 1.World Health Organization . Published 2020. Coronavirus disease 19 (COVID-19)- Situation Report 80.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200409-sitrep-80-covid-19.pdf?sfvrsn=1b685d64_4 [Google Scholar]
- 2.Michigan.gov. Governor Whitmer Signs Executive Order Expanding COVID-19 Emergency Declaration and Declaring State of Disaster.https://www.michigan.gov/coronavirus/0,9753,7-406-98158-523989–,00.html. Accessed April 7, 2020
- 3.Mack J. Mlive; Published 2020. Michigan Has Become a U.S. Epicenter for Coronavirus. Why?https://www.mlive.com/public-interest/2020/03/michigan-has-become-a-us-epicenter-for-coronavirus-why.html [Google Scholar]
- 4.Gooch K. Becker's Hospital Review; Published 2020. 'We Are Not Immune': Henry Ford Health Says 734 Employees Positive for COVID-19. More than 700 Employees of Detroit-Based Henry Ford Health System Have Tested Positive for COVID-19.https://www.beckershospitalreview.com/workforce/we-are-not-immune-henry-ford-health-says-734-employees-positive-for-covid-19.html [Google Scholar]
- 5.Li R, Pei S, Chen B. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2) Science. 2020 doi: 10.1126/science.abb3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vargo E, Ali M, Henry F, Kmetz D, Krishnan J, Bologna R. Cleveland clinic akron general urology residency program's COVID-19 experience. Urology. 2020 doi: 10.1016/j.urology.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhao H, Quach A, Cohen T, Anger J. “Characteristics, burden, and necessity of inpatient consults for academic and private practice urologists. Urology. 2020 doi: 10.1016/j.urology.2020.02.016. [DOI] [PubMed] [Google Scholar]
- 8.Ellison JS. The value of a urology consultation. J Urol. 2018;200:46–47. doi: 10.1016/j.juro.2018.04.017. [DOI] [PubMed] [Google Scholar]
- 9.Dowling RA. Urology Times; Published 2020. Business of Urology.https://www.urologytimes.com/business-urology [Google Scholar]
- 10.ACGME Response to COVID-19 . Published 2020. Clarification Regarding Telemedicine and ACGME Surveys.https://www.acgme.org/Newsroom/Blog/Details/ArticleID/10125/ACGME-Response-to-COVID-19-Clarification-regarding-Telemedicine-and-ACGME-Surveys [Google Scholar]
- 11.Coronavirus update: CMS releases waivers for COVID-19: AHA. Am Hosp Assoc. 2020 https://www.aha.org/advisory/2020-03-31-coronavirus-update-cms-releases-waivers-covid-19 [Google Scholar]