The COVID-19 pandemic has rapidly changed how physicians assess and interact with patients. Many providers have appropriately cancelled nonemergent surgical procedures and converted ambulatory in-person appointments to remote video visits or phone calls. As hospitals throughout the United States begin to fill with patients afflicted with COVID-19 and other acute illnesses, the need to preserve personal protective equipment (PPE) and to reduce the risk of nosocomial COVID-19 transmission to patients and providers is critical. Likewise, it is imperative to rapidly triage, diagnose, and provide disposition for nonCOVID-19-related urgent and emergent hospital visits.
In order to support this objective, we developed a process to utilize inpatient telemedicine video visits and electronic consultation (eConsults) to assess patients with non-procedural urological needs presenting to the emergency department (ED) or admitted to the hospital. We aim to describe these types of remote consultation, medical documentation and billing requirements, and demonstrate a process for rapid implementation. Our hope is that other consulting specialists can implement similar programs, contribute to PPE preservation, and minimize unnecessary physical exposure without compromising medical care.
VIDEO VISITS FOR HOSPITALIZED AND EMERGENCY ROOM PATIENTS
Video visits are a real-time, simultaneous audio and visual interaction with patients via a video conferencing platform.1 During the COVID-19 emergency, prior restrictions on patient location during video visits have been waived by the Centers for Medicare and Medicaid Services as well as by most state Medicaid programs and private insurers.2 , 3 Nearly all Americans can now participate in a video visit with a healthcare provider from any location. As a result, clinicians across the United States have rapidly adopted the use of video visits to replace in-person outpatient visits during the COVID-19 emergency.4
Many of these regulatory changes are directly applicable to physician consultation in both the ED and inpatient settings. Video visits can be used to evaluate patients without a procedural need or for conditions where physical exam is not a major contributor to clinical decision making.5 During the COVID-19 emergency, this will facilitate rapid assessment and disposition from the ED and promote essential goals: preserving PPE, limiting potential exposures and the possible spread of disease in the ED and inpatient settings. Although this method of consultation may be new for many providers, video visits have been used for years to assess patients presenting with stroke symptoms to facilitate rapid decisions on tissue plasminogen activator use.6 , 7
The appropriate documentation and consenting process for ED and inpatient video visit consultation are identical to outpatient video visit requirements. In addition to standard evaluation and management components of a consultation note, providers should document (1) consent of the patient to a video visit, (2) the location of the patient and the provider at time of the encounter, (3) the time spent for the consultation. We also encourage providers to document a statement that the visit was conducted via video to preserve PPE and limit exposures during the COVID-19 emergency. The specific CPT codes for initial and follow-up video visit consultations are provided for reference (Table 1 ).
Table 1.
Video visit and eConsult codes
| CPT® Code | Description | Time Spent | CY2020 RVU |
|---|---|---|---|
| Video Visits | |||
| G0425-7 | Telehealth consultation, emergency department or initial inpatient | 30, 50, 70 min | 1.92, 2.61, 3.86 |
| G0406-8 | Telehealth consultation, follow-up | 15, 25, 35 min | 0.76, 1.39, 2.00 |
| eConsults | |||
| 99446-9 | Interprofessional telephone/internet/electronic health record assessment and management service provided by a consultative physician, including a verbal and written report to the patient's treating/requesting physician or other qualified healthcare professional. | 5-10, 11-20, 31-30, >30 min | 0.35, 0.75, 1.05, 1.40 |
| 99451 | Interprofessional telephone/internet/electronic health record assessment and management service provided by a consultative physician, including a written report to the patient's treating/requesting physician or other qualified healthcare professional. | 5+ min | 0.70 |
eCONSULTS
An eConsult, or interprofessional consultation, is defined as a diagnosis or management service provided by a consulting physician to a requesting physician or other qualified healthcare professional via verbal and written report.8 This service takes place without face-to-face or video evaluation of the patient by the consultant. This method of consultation allows for rapid, direct, and documented communication of recommendations from the consultant to the treating provider.9 , 10 It is important to note that the consultant must be a physician. Like video visits, the use of eConsults has typically been reserved for outpatient care; however, there are no restrictions for its application to inpatient and ED consultation.11
There are important billing and documentation requirements for eConsults. First, the requesting provider needs to briefly obtain and document verbal consent from the patient for the use of eConsults. Second, the consulting physician should document (1) the reason for consultation, (2) findings from the medical records, (3) further evaluation and/or treatment recommendations, and (4) the time spent reviewing the record and speaking with the requesting physician (if applicable). Lastly, if upon reviewing the clinical record, the consultant determines that a formal video or in-person consultation is recommended (either immediately or as an outpatient), or if an in-person consultation occurs within 14 days, then the eConsult is no longer a billable event. The appropriate billing codes are listed in Table 1. One important nuance is that code 99451 is used when there is no verbal report given to the requesting provider after the recommendations are documented in the eConsult note. This is more often utilized in the outpatient setting but may also be appropriate for inpatient use.
CONSULTATION WORKFLOW
Implementing video visits and/or eConsults in the ED and inpatient settings requires careful planning for safe and effective implementation. These methods of consultation will likely be new for many providers who request a consultation. Thus, engaging with the leadership of services that are frequently requesting consultation (eg, ED, internal medicine, and general surgery) will help to address workflow impediments when recommending a video or eConsult during COVID-19.
One of the greatest challenges for consultants is determining which patients are ideal candidates for video or eConsult. For consults requiring a procedure or assessment for emergent surgery, an in-person evaluation is required. Otherwise, there are no clear guidelines for which clinical questions require in-person evaluation. The consultant and requesting provider should discuss patient acuity, physical exam needs, and provider comfort with remote assessment.
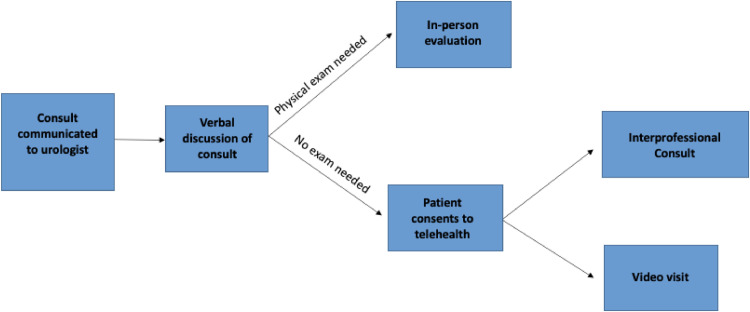
Lastly, technological workflows for video visits should be established. Not all patients, hospital rooms, or ED units, have a device capable of video conferencing. Thus, inpatient wards and EDs may consider repurposing mobile computers and/or tablets used for research or translator services to be used for video visits. The consultation workflow at our institutions is displayed in Figure 1 . At present, some institutions have implemented this for all patients. Others are using this workflow only for patients admitted to COVID-19 wards. Each institution will need to determine its individualized workflow and its criteria for which patients would benefit from remote evaluation. This will also depend on the state of each institution's technological capabilities, hospital PPE supplies, and the estimated trajectory of patients with COVID-19.
Figure 1.
Remote consultation workflow. (Color version available online.)
Importantly, the use of remote ED and inpatient consultation could harness a centralized team of providers that could manage remote consultations across multiple hospitals. This may become particularly important at institutions experiencing a surge of COVID-19 patients where specialists are being redeployed to provide care in intensive care units, EDs, and inpatient wards. As fewer specialists are available to serve as consultants for their trained specialty, more facilities will likely need to be serviced by a smaller team of specialist providers.
CONCLUSION
The COVID-19 pandemic has necessitated dramatic changes in the practice of medicine. The utilization of telemedicine video visits and eConsults for certain patients requiring specialist evaluation in the ED and inpatient ward setting will help to conserve PPE, limit exposures bidirectionally, could allow for a centralized consult workforce to service multiple hospitals, and facilitate rapid triage and disposition of non-COVID-19 emergencies during this crisis.
Footnotes
Disclosures: Dr. Anobel Odisho had a prior consulting relationship with VSee, Inc.
References
- 1.Gadzinski AJ, Ellimoottil Chad, Odisho Anobel Y, Watts KL, Gore JL. Telemedicine in urology: a crash course during the COVID-19 pandemic.https://www.urologytimes.com/business-urology/telemedicine-urology-crash-course-during-covid-19-pandemic. Published2020. Accessed 31 March 2020.
- 2.Centers for Medicare & Medicaid Services. Medicare Telemedicine Health Care Provider Fact Sheet; 2020. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. Accessed 7 April 2020.
- 3.Center for Connected Health Policy. COVID-19 RELATED STATE ACTIONS. CCHP Telehealth Policy. https://www.cchpca.org/resources/covid-19-related-state-actions. Published 2020. Accessed 5 April 2020.
- 4.Mehrotra A, Ray K, Brockmeyer DM, Barnett ML, Bender JA. Rapidly Converting to “Virtual Practices”: Outpatient Care in the Era of COVID 19. NEJM Catal. 2020 doi: 10.1056/CAT.20.0091. [DOI] [Google Scholar]
- 5.Zhao H, Quach A, Cohen T, Anger JT. Characteristics, burden, and necessity of inpatient consults for academic and private practice urologists. Urology. 2020 doi: 10.1016/j.urology.2020.02.016. [DOI] [PubMed] [Google Scholar]
- 6.Wechsler LR, Demaerschalk BM, Schwamm LH. Telemedicine quality and outcomes in stroke: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2017;48 doi: 10.1161/STR.0000000000000114. [DOI] [PubMed] [Google Scholar]
- 7.Witrick B, Zhang D, Switzer JA, Hess DC, Shi L. The association between stroke mortality and time of admission and participation in a telestroke network. J Stroke Cerebrovasc Dis. 2020;29 doi: 10.1016/j.jstrokecerebrovasdis.2019.104480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blue P. Revenue Cycle Advisor; 2019. Q&A: 2019 CPT Codes for Interprofessional Consultations.https://revenuecycleadvisor.com/news-analysis/qa-2019-cpt-codes-interprofessional-consultations PublishedAccessed 1 April 2020. [Google Scholar]
- 9.Vimalananda VG, Gupte G, Seraj SM. Electronic consultations (e-consults) to improve access to specialty care: a systematic review and narrative synthesis. J Telemed Telecare. 2015;21:323–330. doi: 10.1177/1357633X15582108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Castaneda P, Ellimoottil C. Current use of telehealth in urology: a review. World J Urol. 2019 doi: 10.1007/s00345-019-02882-9. [DOI] [PubMed] [Google Scholar]
- 11.Tande AJ, Berbari EF, Ramar P. Association of a remotely offered infectious diseases eConsult service with improved clinical outcomes. Open Forum Infect Dis. 2020;7 doi: 10.1093/ofid/ofaa003. [DOI] [PMC free article] [PubMed] [Google Scholar]