Abstract
The pandemic of coronavirus SARS-CoV-2 disease affected Northern Italy, spreading from the Bergamo province to the entire country. During reorganization of our emergency department to support patients presenting with coronavirus SARS-CoV-2 disease, we aimed to evaluate whether children play a role in intrahospital spread of the infection.
Keywords: coronavirus, SARS-CoV-2, COVID-19, emergency department, healthcare workers, children
Abbreviations: COVID-19, SARS-CoV-2 disease; HCP, Healthcare personnel; NP/OP, Nasopharyngeal/oropharyngeal; PPE, Personal protective equipment
Beginning in February of 2020, an outbreak of the novel coronavirus SARS-CoV-2 disease (COVID-19) occurred in Northern Italy, and rapidly spread to the entire country.1 Owing to the impracticability of any containment measure, mitigation, and suppression policies to reduce self-sustaining community outbreak amplification were promulgated by the Italian government. This entailed 3 steps: (1) local confinement and regional social distancing (February 23 to March 7), a ban on leaving or accessing designated “red zones,” restricting gatherings, events, and meetings in Northern Italy, and suspending schools nationwide; (2) extensive lockdown (March 8-22), quarantine for most of Northern Italy, followed by expanded nationwide quarantine, with an all-event ban, travel restrictions, and the closure of all commercial and retail businesses, except those providing essential services; and (3) industrial shutdown (March 21), closure of all nonessential industries and businesses.
Despite these radical social interventions, as of March 27, Italian health authorities have reported 62 013 confirmed cases of COVID-19 and 8169 fatalities, of which 36% and 59%, respectively, were in the Lombardy region.2 , 3 The province of Bergamo became the most affected territory outside mainland China.
In Lombardy, the main outbreak of the infection was located in a community hospital in the Bergamo province, suggesting that the community spread of the infection probably arose from a large cohort of subjects who were in contact with patients with SARS-CoV-2 infection attending healthcare facilities, and who were probably unrecognized at that time. So far, pediatric services have not experienced the COVID-19 burden experienced in adults. The few known infected children seem to have a mild disease or are asymptomatic.4, 5, 6, 7 However, we do not know whether infected children play a substantial role as drivers of the epidemic. Children hospitalized for reasons other than lower respiratory tract infections could carry the virus and represent an occult threat for healthcare workers and other vulnerable patients. To address these issues, we developed a protocol addressing reception, risk management, and hospitalization of suspected SARS-CoV-2 cases at the pediatric emergency department and medical-surgical units aimed at containing intrahospital transmission of the infection, considering that currently our hospital is the largest referral site in the primary outbreak area in Italy.
Methods
A task force created the hospital pediatric COVID-19 protocol. Hospital Papa Giovanni XXIII is the referral hospital for the province of Bergamo, Lombardy (1 114 590 inhabitants), housing the national pediatric liver and solid organ transplant program (11 beds) and the provincial pediatric hematology/oncology treatment center (8 beds). A general pediatric medical unit accounts for 17 beds. The aim was to achieve effective case identification in children admitted through the pediatric emergency department. The specific aim was to decrease nosocomial transmission to patients and healthcare workers.
A literature review was performed with relevant terms (novel Coronavirus, nCoV, SARS-CoV-2, COVID-19) in PubMed and MEDLINE databases, and data regarding pediatric populations were extracted and summarized. Relevant updated epidemiologic data were collected.
Epidemiologic criteria for the definition of a suspected case according to the Italian Ministry of Health (ie, close contact with a confirmed or probable case of SARS-CoV-2 infection, OR having stayed in areas with presumed community transmission, OR having worked in a healthcare service providing care for SARS-CoV-2–infected patients) were not retained as applicable after March 6, 2020, for protocol purposes, owing to the widespread community transmission of COVID-19 all over Lombardy.6
Thus, case definition was defined as (1) suspected case (per protocol): patient with acute respiratory tract infection (sudden onset of ≥1 of the following: cough, fever, tachypnea) AND/OR who in the last 14 days has had close contact with a confirmed or probable case of SARS-CoV-2 infection; (2) probable case: a suspected case for whom testing for SARS-CoV-2 is inconclusive (according to the test results reported by the laboratory) or for whom testing was positive on a pan-coronavirus assay; and (3) confirmed case: a person with SARS-CoV-2 infection confirmed at Italian national reference laboratory, irrespective of clinical signs and symptoms.
Testing for SARS-CoV-2 was performed using real-time polymerase chain reaction for SARS-CoV-2 nucleic acids on nasopharyngeal/oropharyngeal swab (NP/OP swab).
Close contact was defined according to European Centre for Disease Control (ECDC)/World Health Organization (WHO) definition (www.ecdc.europa.eu/sites/default/files/documents/nove-coronavirus-infection-prevention-control-patients-healthcare-settings.pdf). Three meetings, which took place on February 27, February 28, and March 6, 2020, finalized the protocol, included a representative member from the hospital executive board.
Protocol
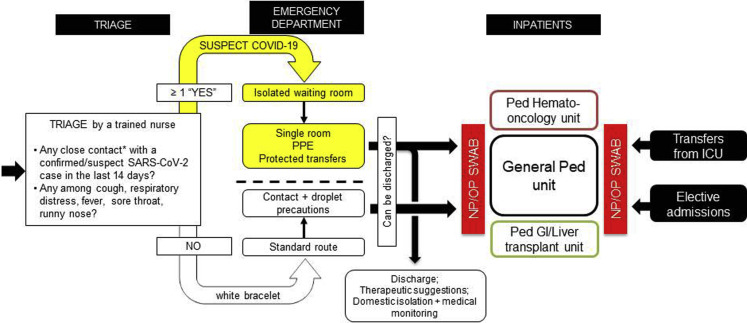
The protocol was adopted on March 6, 2020, and consisted of 3 parts: triage optimization, risk assessment and management in the emergency room, and patient management on the pediatric unit. Spatial reorganization of the emergency department with the creation of separate routes access for suspected COVID-19 and standard patients was completed on March 13, 2020 (Figure 1 ).
Figure 1.
Daily numbers of referrals to the pediatric emergency department (white bars) comprehensive of numbers of COVID-19 suspected cases (light grey) as per protocol definition, and cumulative COVID-19-confirmed cases among hospitalized children (dark grey bars) and suspect and confirmed cases among child care personnel (dashed bars) at our Institution. cum, cumulative. Ped ED, pediatric emergency department; Susp COVID-19, suspected COVID-19.
Triage and Emergency Department
Children and caretakers with acute respiratory tract infection with or without fever are approached with a FFP2/N95 masked staff member and receive a 2-item questionnaire, addressing the risk of community or intrafamilial transmission. Answering “yes” to ≥1 of the questions (with symptoms of respiratory tract infection AND/OR previous contact with a confirmed or probable case of SARS-CoV-2 infection), marks the case as suspect. Patients triaged as suspected cases receive a yellow identification bracelet, are accepted into the department via a separate route, have a separate waiting room, and undergo protected transfers (Figure 1).
Suspected COVID-19 Route (Yellow Bracelet)
Patients enter the emergency department through a separate path, are evaluated by healthcare personnel protected according to the COVID-19 World Health Organization recommendations (FFP2/N95 respirator + eye protection goggles or face shield + isolation gown + face mask + gloves).8 Physical examination takes place in isolated single rooms. The pediatrician assesses additional elements of suspicion (eg, presence of a household contact with history of a lower respiratory tract infection within the last 14 days; presence of a lower respiratory tract infection/community-acquired pneumonia not responding to standard antibiotic therapy in children >14 years of age).
Patients requiring oxygen receive nonhumidified gas through a nasal cannula or Venturi mask to decrease aerosol formation. Those requiring chest imaging reach the emergency radiology department through a dedicated hallway. All transfers are operated with the patient wearing a surgical mask, including transfer to the pediatric unit for children requiring hospitalization.
Patients not requiring hospitalization are discharged to domestic isolation, and undergo medical monitoring by the local health services handling the clinical aspects and the infectious risk (Figure 1).
Standard Route (White Bracelet)
Patients accessing the emergency department for nonrespiratory problems and without a history of contact with a patient with COVID-19 are accepted into a separate area and managed according to the standard procedure, with contact and droplet precautions.
Management on the Pediatric Unit
Patients suspected of having COVID-19 requiring hospitalization are managed by healthcare personnel (HCP) using personal protective equipment (PPE) (FFP2/N95 respirator + eye protection goggles or face shield + isolation gowns + face mask + gloves), who perform the acquisition of an NP/OP swab for SARS-CoV-2 real-time polymerase chain reaction testing. The beds for patients with suspected COVID-19 are located in an isolated, clearly marked area.
Blood samples are collected according to HCP recommendations, and patients undergo evaluation for other etiologies according to HCP clinical judgment. If SARS-CoV-2 testing yields a negative result, standard protective precautions are adopted. If COVID-19 is confirmed, subsequent management takes place with HCP using PPE in tight cooperation with infectious diseases specialists.
Patients admitted for nonrespiratory problems and without history of contact with patients with COVID-19 also undergo diagnostic NP/OP swab for SARS-CoV-2, to detect asymptomatic carriers, and are managed with COVID-19 precautions until the swab result is available. Therefore, universal NP/OP screening is carried out in all admitted patients on the first day of admission (Figure 1).
The Screening Policy of the Healthcare Personnel
Owing to the shortage of virologic diagnostic reagents and laboratory consumables, the following hospital policy for management of HCP was used for personnel with mild respiratory symptoms without fever: continuation of regular activity, continuous donning of a surgical masks, and, for personnel with symptoms preventing work activity (fever, cough, evidence of lower respiratory tract infection, gastrointestinal symptoms, malaise), domestic isolation until 14 days from the disappearance of symptoms, before returning to work. The routine use of diagnostic NP/OP swabs for SARS-CoV-2 testing in asymptomatic or mildly symptomatic HCP was not adopted.
Results
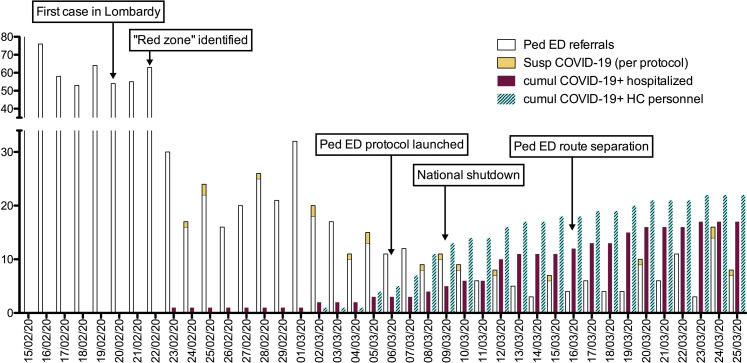
Remarkably, during the SARS-CoV-2 epidemic, the number of pediatric patients presenting to the emergency department decreased from a mean of 62 per day to a mean of 8 per day (Figure 2 ). At the time of writing (March 27), 17 confirmed pediatric COVID-19 cases were identified at our institution (median age, 6.6 years; IQR, 2 months to 11.3 years). During the period of time of the study protocol we performed 58 NP/OP swabs. Among patients admitted from the emergency department and classified as suspected cases, 9 of 15 (69%) had a positive NP/OP swab, vs only 1 of 13 (7%) of the nonsuspect cases (a child with appendicitis). Remarkably, among the patients admitted electively to the hemato-oncology unit, 3 or 15 (20%) tested positive (2 with hepatoblastoma and 1 with rhabdoid tumor, all with fever and neutropenia after chemotherapy).
Figure 2.
Daily numbers of referrals to the pediatric emergency department (white bars) comprehensive of numbers of COVID-19 suspected cases (yellow bars) as per protocol definition, and cumulative COVID-19-confirmed cases among hospitalized children (purple bars) and suspect and confirmed cases among child care personnel (dashed bars) at our Institution. cum, cumulative. Ped ED, pediatric emergency department; Susp COVID-19, suspected COVID-19.
In the hepatology, gastroenterology, and transplantation unit, none of the 15 tested children had a positive NP/OP swab (9 of the 15 had a liver transplant, 1 had an intestinal transplant, 1 had Coombs' positive anemia with giant cell hepatitis, and 4 had chronic liver disease and no immunosuppressive treatment). The mother of 1 child who was admitted for a biliary stricture after liver transplantation had a positive test for SARS-CoV-2.
Only 2 children were admitted for respiratory problems (uncomplicated pneumonia), and 6 children had no or very mild respiratory symptoms. Six newborns/infants had fever without signs of localization.
Unfortunately, before the adoption of a dedicated protective protocol, 6 confirmed and 16 suspected COVID-19 cases occurred among HCP employed in our pediatric care services. Eight of 33 pediatricians (24%) and 14 of 45 nurses (31%) were infected in 22 days, with 6 exhibiting radiographically confirmed pneumonia (requiring hospitalization in 2); the others had mild upper respiratory tract symptoms and/or fever requiring home isolation. However, only 4 cases occurred after (≥48 hours) the adoption of the spatial reorganization of the emergency department and of the ward, and the adoption of the final COVID-19 protocol (Figure 2).
Discussion
The SARS-CoV-2 outbreak represents a hazard of unknown proportion to national healthcare systems. It is now clear that, in the absence of population-wide mitigation policies aimed at containment, the number of patients presenting to the emergency department with suspected COVID-19 is large. This sudden and overwhelming burden of patients has rapidly saturated the general and intensive care bed capacity, and shifted the human and medical resources to the care of patients who occupy most of the beds in all healthcare facilities. Infection of a large proportion of HCP has been recorded, and the role of healthcare facilities as sources of spread of the epidemic has emerged. The high rate of infections among HCP in Wuhan, China, and in our experience in Bergamo suggests that hospitals may play a substantial role in SARS-CoV-2 dispersion to the community. For their own health and for protection of others, HCP PPE should be a priority. Although children are relatively spared as far as morbidity and mortality from COVID-19, they also can spread the infection. The mission of a pediatric department is to cocoon hospitalized patients carrying the virus. As the tertiary pediatric care facility in the “eye of the cyclone”—a pediatric oncology hub and pediatric liver transplant center—we aimed to create safe reception routes to the emergency department by the identification of patients at risk of COVID-19 at the point of entry to detect infections among children admitted to the hospital units and to protect HCP. Because children infected with COVID-19 have mild or no symptoms, we chose to obtain a NP/OP swab from all children requiring hospitalization, regardless of presenting symptoms, to separate the cohorts of patients effectively.5 , 6
Despite risk assessment beginning at triage, the proportion of infected physicians and nurses was high before the implementation of strict protocols. Remarkably, only 4 cases of COVID-19 occurred among HCP after spatial separation of a dedicated area for suspect cases, which allowed timely adoption of PPE. We believe it is likely that the infection of these 4 persons may have occurred outside the hospital. It is likely that a proportion of infected HCP, if insufficiently protected, acquire infection in the hospital environment, and others can be infected through community contacts. If this hypothesis is correct, the only way to prevent intrahospital transmission of infection (and possible spread to the community during an epidemic) is to perform consistent hand hygiene and implement universal use of PPE, and to perform wide NP/OP screening of the admitted patients and possibly the HCP, regardless of symptoms.9
It is noteworthy that we did not experience severe forms of COVID-19 in our pediatric patients, including children with malignancies and pediatric solid organ transplant recipients (3 patients under chemotherapy were SARS-CoV-2 positive when admitted for fever and neutropenia, but had no respiratory symptomatology). This supports data gathered from previous coronavirus outbreaks (SARS, MERS), suggesting that immunosuppression per se does not seem to be an additional risk factor for COVID-19.10 A major limitation of our study is the small number of children tested and cases detected.
Intrahospital spread of SARS-CoV-2 seems to be a major threat during this pandemic and should not be overlooked. We propose the use of a strict surveillance and management protocol during outbreaks of highly virulent viruses such as SARS-CoV-2, through dedicated patient pathways, adoption of PPE for HCP, and use of NP/OP screening of all admitted children and possibly all HCP.
Footnotes
The authors declare no conflicts of interest.
References
- 1.European Centre for Disease Prevention and Control . ECDC; Stockholm: 2020. Outbreak of novel coronavirus disease 2019 (COVID- 19): situation in Italy. 23 February 2020. [Google Scholar]
- 2.Ministry of Health Novel Coronavirus. www.salute.gov.it/portale/nuovocoronavirus/ Accessed March 29, 2020.
- 3.Official Gazette of the Republic of Italy Collection of documents containing urgent measures regarding the containment and management of the epidemiological emergency from COVID-19. www.gazzettaufficiale.it/attiAssociati/1/?areaNode=13 Accessed March 29, 2020.
- 4.Chen Z.M., Fu J.F., Shu Q., Chen Y.H., Hua C.Z., Li F.B. Diagnosis and treatment recommendations for pediatric respiratory infection caused by the 2019 novel coronavirus. World J Pediatr. 2020 doi: 10.1007/s12519-020-00345-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wei M., Yuan J., Liu Y., Fu T., Yu X., Zhang Z. Novel Coronavirus infection in hospitalized infants under 1 year of age in China. JAMA. 2020 doi: 10.1001/jama.2020.2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu Z., McGoogan J.M. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1313–1314. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 7.Dong Y., Mo X., Hu Y., Qi X., Jiang F., Jiang Z. Epidemiological characteristics of 2143 pediatric patients with 2019 Coronavirus disease in China. Pediatrics. 2020 [Google Scholar]
- 8.World Health Organization . Interim Guidance; Geneva: 2020. Infection prevention and control during healthcare when novel coronavirus (nCoV) infection is suspected.www.who.int/publications-detail/infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected WHO/2019-nCoV/IPC/v2020.1. Accessed March 29, 2020. [Google Scholar]
- 9.Ong J., Cross G.B., Dan Y.Y. Prevention of nosocomial SARS-CoV-2 transmission in endoscopy: international recommendations and the need for a gold standard. Gut. 2020 doi: 10.1136/gutjnl-2020-321154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.D'Antiga L. Coronaviruses and immunosuppressed patients. The facts during the third epidemic. Liver Transpl. 2020 doi: 10.1002/lt.25756. [DOI] [PubMed] [Google Scholar]