Abstract
In the last few years, the development of a plasmid-based reverse genetics system for mammalian reovirus has allowed the production and characterization of mutant viruses. This could be especially significant in the optimization of reovirus strains for virotherapeutic applications, either as gene vectors or oncolytic viruses. The genome of a mutant virus exhibiting increased sensitivity to interferon was completely sequenced and compared with its parental virus. Viruses corresponding to either the parental or mutant viruses were then rescued by reverse genetics and shown to exhibit the expected phenotypes. Systematic rescue of different viruses harboring either of the four parental genes in a mutant virus backbone, or reciprocally, indicated that a single amino acid substitution in one of λ2 methyltransferase domains is the major determinant of the difference in interferon sensitivity between these two viruses.
Keywords: Reovirus, Interferon, Reverse genetics, RNA capping, RNA methyltransferase
Highlights
-
•
An interferon sensitive reovirus harbors amino acids substitutions in four proteins.
-
•
Wild-type laboratory stock and mutant viruses were reconstructed by reverse genetics.
-
•
Each mutant gene was substituted by its wild-type counterpart and reciprocally.
-
•
Interferon sensitivity was assigned to a substitution in mRNA capping protein λ2.
Introduction
Mammalian reoviruses are among a plethora of viruses that are presently under investigation for their ability to preferentially infect and destroy transformed/cancer cells. This has led to recent progress in their clinical use against various forms of human cancers (briefly reviewed among others by Kelly et al., 2009, Black and Morris, 2012). In contrast to most other “oncolytic” viruses presently under consideration for clinical use, reoviruses are naturally oncolytic and have not been submitted to genetic manipulation for their clinical use. In fact, it was not possible until recently (Kobayashi et al., 2007) to easily manipulate the reovirus genome using a plasmid-based reverse genetics system.
The initial observations that led to the utilization of reovirus as an “oncolytic” virus suggested that a decreased activity of the interferon-inducible double-stranded RNA-dependent protein kinase (PKR), which occurs upon Ras-induced cell transformation, was responsible for the preferential infection and destruction of cancer cells by reovirus (Strong et al., 1998). Despite the fact that multiple steps of the reovirus replicative cycle are likely involved in preferential replication and virus-induced cancer cell death (Lemay et al., 2007, Marcato et al., 2007), further work has supported the idea that a lower induction of interferon in Ras-transformed cells favors viral propagation and could be of major importance to the virus׳ oncolytic activity (Shmulevitz et al., 2010).
To further support the idea that interferon-induced antiviral pathways are critical in the ability of reovirus to discriminate between parental and Ras-transformed cells, a mutant virus obtained by chemical mutagenesis was selected for its increased sensitivity to interferon and was actually shown to exhibit a more complete blockage than the wild-type virus in parental cells, even at extremely high multiplicity of infection (Rudd and Lemay, 2005).
Multiple reovirus genes are suspected to be involved in the control of the interferon innate immune response (Sherry, 2009, Sherry et al., 2009). The μ2 protein was shown to be the major determining factor in the control of interferon signaling induction by altering the subcellular localization of IRF-9 (Irvin et al., 2012, Zurney et al., 2009). The σ3 protein could rather affect interferon sensitivity due to its ability to sequester the dsRNA activator of the interferon-inducible protein kinase PKR; however, this property of σ3 could be modulated by μ1 since the σ3-μ1 heterohexamer does not appear to bind dsRNA (Schiff, 2008). Finally, at least in some cell types, the σ2 and λ2 protein were previously suspected to play a role in the control of either induction of interferon signaling or virus׳ sensitivity to interferon (Sherry et al., 1998).
In order to clarify which genetic determinants are involved in the large difference in interferon sensitivity between the parental and previously identified P4L-12 mutant virus (Rudd and Lemay, 2005), the complete sequence of the viral genome was determined. Both viruses were then reconstructed by site-directed mutagenesis and reverse genetics, since a number of differences were observed between the isolate used to construct the reverse genetics plasmids and the parental laboratory stock initially used to isolate the mutant virus. Each four genes exhibiting differences between the parental and mutant viruses were then individually substituted either to replace the mutant gene by its parental counterpart or replacing the parental gene by its mutant counterpart in the parental background. This clearly demonstrated that the single amino acid substitution in one of the two methyltransferase domains of λ2 is the major determinant of the difference in interferon sensitivity between these two viruses.
Results
Sequencing of the interferon-sensitive P4L-12 mutant
In order to determine the differences in sequence between the interferon-sensitive P4L-12 mutant (Rudd and Lemay, 2005) and the original wild-type type 3 Dearing (T3D) (T3/Human/Ohio/Dearing/55) from which it was derived, the whole coding sequence of the genome was analyzed by RT-PCR on the semi-purified viral genome from both the mutant and wild-type laboratory stocks, followed by direct sequencing of the PCR products, as described in Section Materials and Methods and previously used in the laboratory (Jabre et al., 2013).
Despite the fact that the P4L-12 mutant was obtained following treatment with a high dose of the chemical mutagen nitrosoguanidine (Rudd and Lemay, 2005), only 4 genes were found to exhibit nonsynonymous mutations compared to the wild-type resulting in a total of 6 amino acids substitutions ( Table 1 ). Of these, only the λ2 T636M, μ1 P315S and σ3 M221I are unique among currently available sequences of T3D ( Table 2 and data not shown) and were thus of special interest. Six additional silent nucleotide substitutions were also found between the wild-type and mutant virus (GeneBank accession numbers KP208804 to KP208813 for the wild-type and KP208814 to KP208823 for P4L-12 mutant).
Table 1.
Amino acids differences between wild-type reovirus type 3 Dearing laboratory stock (T3DS) and derived mutant P4L-12.
| Wild-type (T3DS) | Mutant (P4L-12) | Amino acid position | |
|---|---|---|---|
| λ2 | T | M | 636 |
| μ1 | P | S | 315 |
| T | A | 449 | |
| μNS | V | A | 705 |
| σ3 | G | E | 198 |
| M | I | 221 |
Table 2.
Amino acids differences between different reovirus type 3 Dearing.
| T3DKa | T3DSb | T3DWc | T3DHd | Reolysine | Amino acid position | |
|---|---|---|---|---|---|---|
| λ3 | M | L | 979 | |||
| S | R | 1045 | ||||
| N | S | S | S | 1048 | ||
| S | P | 1186 | ||||
| λ2 | G | E | E | E | 504 | |
| G | R | 509 | ||||
| I | M | M | 1165 | |||
| λ1 | A | T | 201 | |||
| I | S | S | S | 500 | ||
| A | T | 574 | ||||
| Q | H | 852 | ||||
| M | V | 982 | ||||
| G | D | 1017 | ||||
| μ2 | A | V | 122 | |||
| S | P | P | P | 208 | ||
| R | Q | Q | Q | Q | 342 | |
| A | S | 528 | ||||
| μ1 | E | D | 73 | |||
| T | I | 142 | ||||
| A | V | V | 305 | |||
| – | R | R | 439 | |||
| A | V | V | 440 | |||
| Q | M | M | 441 | |||
| A | T | 449 | ||||
| A | T | 529 | ||||
| μNS | K | E | E | E | 180 | |
| A | V | V | 705 | |||
| G | D | 707 | ||||
| σ1 | V | A | 22 | |||
| T | I | 249 | ||||
| Y | S | 253 | ||||
| T | A | A | A | 408 | ||
| σ3 | W | R | 133 | |||
| G | K | 198 | ||||
| E | D | D | D | 229 | ||
T3D-Kobayashi, wild-type virus from the reverse genetics system (Kobayashi et al., 2007).
T3D-Sandekian, original wild-type virus reported in this study
T3D-Wollenberg, wild-type virus (R124) used in van den Wollenberg et al. (2012).
T3D-Hosseini, wild-type unpublished virus sequence from NCBI database.
T3D-Reolysin®, wild-type virus used in clinical trials as described in Chakrabarty et al. (2014).
Sequence comparison of different stocks of wild-type reovirus type 3 Dearing
The complete sequences obtained were also compared with that of the wild-type virus encoded by the 10 plasmids of the reverse genetics system (Kobayashi et al., 2007) and at least one amino acid change between the two wild-type viruses was found in seven out of 11 proteins; the only completely identical proteins were σ2, σ3, σNS and σ1s. This is not the first time that such differences were observed between laboratory stocks of so-called reovirus type 3 Dearing (Coffey et al., 2006, Nygaard et al., 2013, Yin et al., 2004), this has even lead to the designation of subtypes such as T3DF (from Fields׳ laboratory), T3DN (from Nibert׳s laboratory) and T3DC (from Cashdollar׳s laboratory). Thus, for sake of simplicity, the laboratory virus stock used in the present study will be referred to as T3DS (Sandekian) while the wild-type virus rescued from the plasmids originally obtained from Kobayashi and Dermody will be referred to as T3DK (Kobayashi). In addition to the 12 amino acid substitutions, 11 silent nucleotide substitutions between the two viruses were also found (data not shown).
Comparative sequence analysis was also performed with the sequence of another complete T3D genome (referred to as T3DW) that was used in a recent study by another group (van den Wollenberg et al., 2012) and the sequence of another laboratory stock deposited in the NCBI database by one further group (referred to as T3DH); finally the sequence of the virus currently used in oncolytic virotherapy under the tradename “REOLYSIN®” was added to the comparison (Chakrabarty et al., 2014). Only complete sequences determined by direct sequencing of the viral genome were retained for this analysis since it is difficult to assume that sequences obtained earlier from cloned viral genes are necessarily representative and that they would actually generate a replication-competent virus when combined together.
The laboratory subtype, T3DS, did not display any more differences from T3DK when compared to other completely sequenced genomes. While some positions are clearly more variable, all stocks showed the presence of 8 to 19 differences including 2–8 unique substitutions compared to T3DK. It thus seems that each stock, or subtype, has its own sequence “signature” and that T3DS with 12 amino acid differences including only 3 unique substitutions is not more divergent from T3DK than other virus stocks currently in use in different laboratories.
Reverse genetics rescue of viruses harboring single-gene substitution
In order to determine which of the amino acids differences between T3DS and P4L-12 viruses are responsible for the difference in interferon sensitivity between the two viruses, site-directed mutagenesis was used to introduce the changes in the reverse genetics plasmids encoding the different proteins; when more than one change was found on the same protein, the corresponding nucleotide changes were all introduced on the same plasmid. Since the parental T3D (T3DS) used to isolate P4L-12 differs from the plasmid-encoded T3DK sequence, a complete set of plasmids encoding “wild-type” T3DS was first constructed and then further subjected to site-directed mutagenesis to obtain P4L-12 encoding sequences.
Both a parental T3DS and P4L-12 virus were rescued by transfection of the corresponding plasmid combination. Viruses were similarly obtained using one P4L-12 gene (L2, M2, M3 and S4) in a background of nine T3DS genes. All these viruses were rescued and propagated, as described in Materials and methods. Reciprocally, viruses harboring one T3DS gene in a background of nine P4L-12 genes were also rescued and propagated.
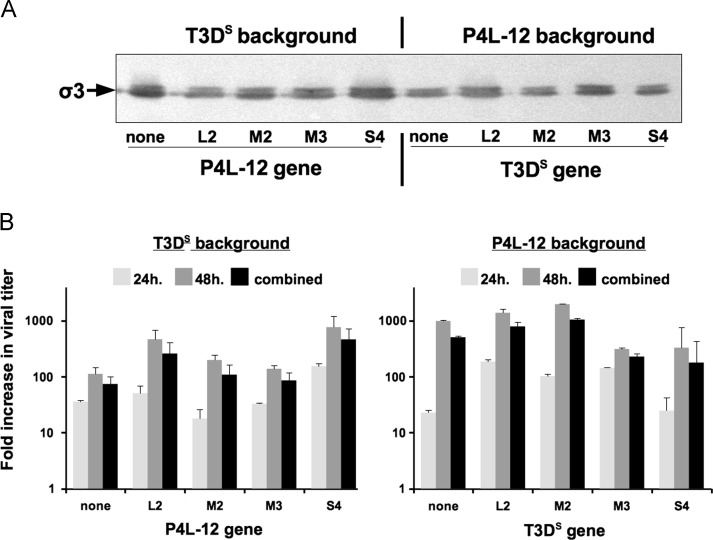
The infectivity and replicative ability of these different viruses was then examined. L929 cells were infected at a multiplity of infection of 2 TCID50 units per cell and viral proteins in infected cells were first examined by immunoblotting ( Fig. 1A); this was a first indication that all viruses were able to infect with a similar efficiency since there were no apparent differences in the amount of viral proteins produced. Production of infectious virus was next examined by infecting cells and measuring the fold-increase of infectious virus (Fig. 1B). In either the T3DS or P4L-12 background, all viruses harboring substitution of single genes from the other virus did not appear to be significantly different from their background virus. In the T3DS background a small increase (up to approximately sixfold for the S4 substitution) was observed while in the P4L-12 background a twofold increase was observed for M2 and twofold decrease for S4. Overall, there was thus no apparent significant defects when single genes were substituted in either background.
Fig. 1.
Infectivity and replication of the different rescued viruses. L929 cells were infected at a MOI of 2 TCID50 units/cell. Results for the different viruses harboring either none or single P4L-12 genes in a T3DS background or none or single T3DS genes in a P4L-12 background are presented. (A) Proteins were recovered from infected cells at 24 h and analyzed by immunoblotting using an anti-σ3 monoclonal antibody, as described in Section Material and methods. (B) Infected cells were recovered at either 24 or 48 h post-infection. Cells were disrupted by three cycles of freeze–thaw (−80 °C to room temperature) and virus titration was performed by TCID50 on L929 cells in 96-well microplates. Results, on a logarithmic scale with error bars representing standard error of the mean, are presented as the average fold-increase in two distinct experiments at 24 h, 48 h, and with all four data points combined, as indicated.
Interferon sensitivity of rescued viruses
Having established that the different rescued viruses can replicate to similar levels in the absence of interferon, their interferon sensitivity was then examined in comparison with their respective parental viruses.
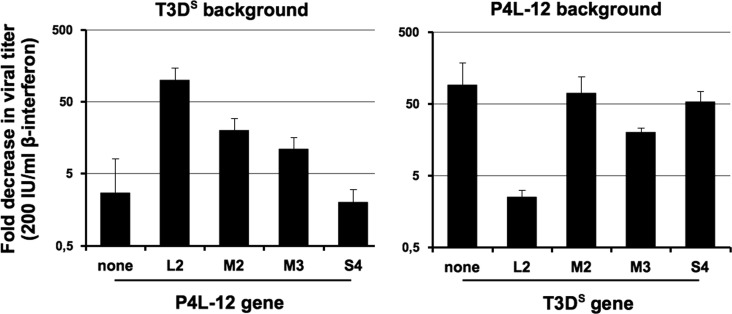
Interferon sensitivity was first examined by measuring the titer reduction on L929 cells treated at a fixed, near saturating, β-interferon concentration (200 international units/ml), as described in Materials and methods. As expected, rescued T3DS harboring none of the P4L-12 genes exhibited resistance to interferon, its titer being almost unaffected at 200 international units/ml of interferon while rescued P4L-12 showed close to a hundred-fold decrease of its titer ( Fig. 2). These values are comparable with those routinely obtained with the two parental viruses in previous experiments (data not shown).
Fig. 2.
Interferon sensitivity of the different rescued viruses. The different rescued viruses, as in Fig. 1, were titrated using a TCID50 assay in the absence or presence of 200 IU/ml of murine β-interferon, as described in Section Material and methods. Average fold-reduction in virus titers for independent experiments for each sample is presented on a logarithmic scale with error bars indicating the maximal value observed for each virus (n=5 for the parental viruses, n=3 for the two viruses harboring substitution of the L2 gene and n=2 for the other viruses). In both the T3DS and P4L-12 background, only L2 gene substitution statistically altered interferon sensitivity, at p=0.002 and p=0.05 respectively using unpaired Student׳s t-test.
Substitution of T3DS genes by those encoding either μNS or μ1 of P4L-12 only slightly increased sensitivity to interferon by less than tenfold while σ3 had no effect (Fig. 2). However, substitution of the L2 gene encoding λ2 significantly increased the interferon sensitivity rendering the virus as sensitive as the P4L-12 virus. The reciprocal experiment where single genes from T3DS were singly substituted in the P4L-12 background confirmed that λ2 by itself is sufficient to render the virus as resistant as T3DS while other proteins had only a slight (μNS) or essentially no effect (μ1 and σ3) on interferon sensitivity (Fig. 2).
It appears very unlikely that differences in residual interferon in the viral inocula could affect the results, given the freeze-thaw treatment, dilutions used, and the fact that there was no differences in interferon induction between T3DS and P4L-12 (data not shown). However, in order to further ruled out this possibility, infectious T3DS, P4L-12 and single L2 reassortant viruses were recovered from human HeLa cells before being titrated on murine L929 cells in the presence or absence of murine interferon; in these conditions any interferon from virus inoculum will be of human origins and will not act on murine cells used in the interferon assay. Identical results were obtained, correlating the presence of L2 from P4L-12 with interferon sensitivity (data not shown).
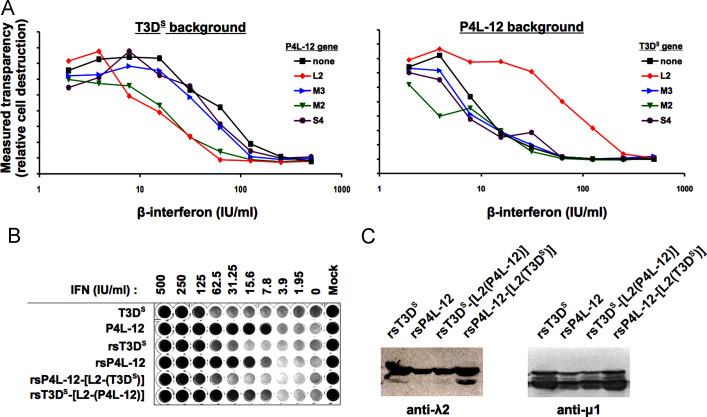
The interferon sensitivity of the same viruses was then further examined using serial binary dilutions of interferon in 96-multiwell plates that were then stained and quantitated ( Fig. 3A). When the rescued T3DS virus and viruses harboring a single P4L-12 gene in this background were examined (left panel), the effect of λ2 was again evident, especially at intermediate concentrations of interferon (approximately 10 to 50 IU/ml) while μNS and σ3 had no effect. In this assay, at lower interferon concentrations compared to Fig. 2, the μ1 protein of P4L-12 also increased interferon sensitivity.
Fig. 3.
Effect of different doses of interferon on the rescued viruses. (A) L929 cells were seeded in 96-well microplates and were infected 24 h later at a MOI of 0.05 TCID50 unit/cell with the different rescued viruses. Following the one-hour adsorption period at 4 °C, serial twofold dilutions of interferon were added to each well, as indicated. Cells were incubated 3 days before being fixed, stained with methylene blue, and quantified as described in Section Materials and methods. A representative experiment out of three independent experiments is presented. (B) Representative microwell plate comparing the two original T3DS and P4L-12 viruses with rescued viruses rsT3DS and rsP4L-12, as well as P4L-12 harboring λ2 from T3DS, rsP4L-12-[L2-(T3DS)], and reciprocally T3DS harboring λ2 from P4L-12, rsT3DS-[L2-(P4L-12)]. (C) Proteins were recovered 24 h post-infection from L929 cells infected at a MOI of 2 TCID50 unit/cell, as in panel B. Immunoblotting analysis was then performed using either anti-λ2 or anti-μ1 monoclonal antibody, as described in Section Materials and methods.
When viruses harboring single T3DS genes in a P4L-12 background were similarly analyzed (Fig. 3A, right panel), only λ2 clearly affected interferon sensitivity, rendering the virus as resistant to interferon as T3DS. The change in interferon sensitivity conferred by M2 of P4L-12 in the T3DS background was not reciprocal; therefore it was not further examined in the present study.
Altogether, the effect of λ2 was thus most striking and this gene appears to be the main and most likely the only determinant of the difference in interferon sensitivity between T3DS and P4L-12, its presence being clearly sufficient to reconstitute the respective phenotype of the two viruses. A representative multiwell plate is presented (Fig. 3B) comparing the original T3DS and P4L-12 virus with their corresponding rescued virus and those where the L2 gene was singly substituted.
Expression of the λ2 protein in infected cells
In order to rule out the possibility that there is a difference in the amount of λ2 present in the infected cells during infection by T3DS or P4L-12, immunoblotting was performed on the rescued viruses harboring all the genes of either viruses, as well as on the viruses harboring solely the λ2 protein of the other virus (T3DS background with λ2 of P4L-12 and reciprocally). The amount of λ2 protein in each case was compared with that of the major outer capsid protein μ1. There was no apparent difference between these four viruses (Fig. 3C) and a simple change in λ2 expression or stability is thus unlikely.
Discussion
The present study illustrates that the state-of-the-art plasmid-based reverse genetics approach can be successfully used to study and completely reconstruct virus mutants previously identified by the use of more classical genetic techniques such as chemical mutagenesis. This has allowed to identify polymorphic amino acids residues in the mammalian orthoreovirus genome as well as clearly pinpoint an amino acid substitution that can drastically affect the interferon sensitivity of viral strains. As previously mentioned, the λ2 protein was previously identified by classical reassortment studies as a possible molecular determinant of the control of interferon response in reovirus-infected cells; however, this is the first time that this has been firmly established using a completely defined genetic system. Interestingly, an immunoreceptor tyrosine-based activation motif (ITAM) that could affect interferon signaling pathways in some cell types, is observed in λ2, although there is currently no evidence that it is actually functional (Stebbing et al., 2014). The amino acid substitution in P4L-12 is not part of this ITAM motif.
The threonine at position 636, substituted for a methionine in P4L-12, is a conserved residue in the λ2 protein sequence of different virus strain (Table 2) (Breun et al., 2001) and is located in one of the two methyltransferase domains (Reinisch et al., 2000, Breun et al., 2001, Bujnicki and Rychlewski, 2001). It is still not firmly established if this first methyltransferase domain is responsible for N-7 or the subsequent 2′-O methylation of the cap structure. However, sequence comparisons suggest the latter possibility (Bujnicki and Rychlewski, 2001) and is also consistent with the relative order of the two methyltransferase domains in Cypovirus (Zhu et al., 2014), another double-stranded RNA virus of the Reoviridae family. Methylation of the RNA cap structure, especially at the 2′-O position could be of importance to avoid recognition of viral RNA as nonself. It could thus affect either induction of interferon signaling or sensitivity to interferon-induced antiviral proteins, such as IFIT1 (recently reviewed by: Hyde and Diamond, 2015). This aspect has been especially well studied in members of the Flaviviridae family but has also been noticed in such different viruses as coronaviruses, vesicular stomatitis virus and metapneumovirus (Daffis et al., 2011, Zust et al., 2011, Habjan et al., 2013, Kimura et al., 2013, Dong et al., 2014, Kindler and Thiel, 2014, Ma et al., 2014, Menachery et al., 2014). An altered 2′-O methyltransferase activity of λ2 could thus potentially explain the altered interferon resistance of P4L-12 compared to the parental virus. Interestingly, in rotavirus, another member of the Reoviridae family, the capping enzyme VP3 was shown to act as an antagonist of innate immunity (Zhang et al., 2013) and it was proposed that variations in the efficiency of the capping reaction, more specifically that of methyltransferase activity, should be examined to determine if it could affect the ability of the virus to control the innate immune reaction (Arnold et al., 2013, Ogden et al., 2014). It will be of interest to perform similar studies with the λ2 protein of reovirus.
Previous work has established the μ2 protein as the major determinant of the extent of interferon signaling following reovirus infection (Zurney et al., 2009, Irvin et al., 2012 ; Stebbing et al., 2014). When interferon induction by T3DS and P4L-12 was compared by recovering supernatant from L929-infected cells (data not shown), both of these supernatants were able to similarly protect cells against the unrelated murine encephalomyocarditis virus (EMCV), as used in previous studies (Sandekian et al., 2013). This is well in accordance with the fact that there is no difference in the μ2 protein of the two viruses and thus probably no significant differences in induction of either interferon or interferon-induced genes. Furthermore, it should be stressed that the presence of a proline at position 208 indicates that these viruses are relatively, although not completely, efficient at repressing interferon signaling (Irvin et al., 2012, Stebbing et al., 2014) suggesting that their difference could rather resides in differences of sensitivity to interferon-induced antiviral mechanisms although this remains to be firmly established.
The results presented herein thus further support the idea that multiple reovirus proteins are involved as determinants of reovirus׳ sensitivity to interferon either by differences in the modulation of interferon signaling or differences in the sensitivity of the interferon-induced antiviral effectors. In this study the λ2-encoding gene, L2, appears as the major determinant of the difference between T3DS and P4L-12. The importance of multiple regulatory mechanisms directed against the interferon innate immune response has also been demonstrated in rotavirus (Arnold et al., 2013), another member of the Reoviridae, and in other unrelated viruses such as the large DNA virus vaccinia (Perdiguero and Esteban, 2009) as well as important human RNA viruses such as hepatitis C (Qashqari et al., 2013) and influenza virus (Garcia-Sastre, 2011).
There are numerous evidence suggesting induction of interferon antiviral response or virus׳ sensitivity to this response is critical in the differential ability of a virus to replicate in, and kill, different cell types. As described in the introduction, this is also likely critical in reovirus׳ oncolytic ability. The possibility of modulating both the level of interferon signaling and sensitivity of reovirus strains to antiviral interferon-induced genes, by a combination of various mutations in either σ3, μ2 and λ2, could certainly contribute to further optimization of viral strains for infection and killing of different cancer cell types.
Materials and methods
Cell lines and viruses
L929 mouse fibroblasts were originally obtained from the American type culture collection (ATCC® CCL-1™). The baby hamster kidney cell line (BHK) stably expressing the T7 RNA polymerase has been described (Buchholz et al., 1999) and was a generous gift from the laboratory of Dr John Hiscott (Lady Davis Research Institute, Montréal, Canada). Both cell lines were grown in minimal Eagle medium (MEM) with 5% fetal bovine serum.
Wild-type reovirus type 3 Dearing (T3/Human/Ohio/Dearing/55) was originally obtained from the American Type Culture Collection (Reovirus 3, ATCC® VR824™). The laboratory stock was derived from a pure plaque after one passage of the original stock on L929 cells. This laboratory virus stock was thereafter used between passage 3 and 5 at a low multiplicity of infection.
Sequencing of the whole viral genomes
Viral genomic RNA was prepared and fragments for sequencing were generated by RT-PCR, as previously described (Brochu-Lafontaine and Lemay, 2012), except that Vertrel was used to prepare reovirus virions (Mendez et al., 2000). The sequences corresponding to all 10 genes of the wild-type laboratory stock were deposited under accession numbers KP208804 to KP208813 in GenBank. The sequences corresponding to all 10 genes of the reovirus interferon-sensitive P4L-12 mutant are accessible under numbers KP208814 to KP208823.
Accession numbers for sequences used for comparisons are EF494435 to EF494444 in the nucleotide database for T3DK; ADJ00316 to ADJ00325 in the protein database for T3DH; and GU991659 to GU991668 for T3DW in the nucleotide database. The sequence of REOLYSIN® was deduced from the differences noticed between each of the genes and its reference sequence as described (Chakrabarty et al., 2014).
Reverse genetics
The plasmids separately harboring each of the cDNA corresponding to the 10 genes of reovirus serotype 3 Dearing, under the transcriptional control of the T7 promoter, as previously described (Kobayashi et al., 2007), were obtained from the laboratory of Dr Terence Dermody (Vanderbilt University, Nashville, Tennessee). To obtain virus mutants in specific genes, the corresponding plasmid was directly submitted to site-directed mutagenesis and used to recover infectious virus by transfection in BHK cells expressing the T7 RNA polymerase and rescued viruses were propagated. Kinetics of viral replication and viral titers were assessed as previously described (Brochu-Lafontaine and Lemay, 2012).
Immunoblotting
Infected cells were recovered by scraping in a small volume of medium and processed for immunoblotting, as previously described (Brochu-Lafontaine and Lemay, 2012). Immunoblotting was performed using monoclonal antibodies directed against either σ3 (4F2), λ2 (7F4) or μ1 (10F6) (Virgin et al., 1991). Images were obtained using either autoradiography on Kodak BioMax Light films or on a Typhoon Trio™ imager (GE Healthcare Life Sciences).
Determination of interferon sensitivity
Interferon sensitivity was determined by two different approaches. The reduction of titer assay was first used as previously described (Danis et al., 1997). Briefly, L929 cells were seeded in 96-well plates and were either left untreated or pre-treated with 200 international units (IU)/ml of mouse β-interferon (PBL InterferonSource) for 24 h before being used in virus titration by TCID50. Following virus adsorption, interferon was added back to the pre-treated plate and the reduction in virus titer in interferon-treated cells compared to untreated cells was determined 7 days post-infection.
To measure sensitivity of viruses to different concentrations of interferon, serial twofold dilution of interferon in 96-well plates was done followed by infection with the different virus strains at the same multiplicity of infection. Plates were stained with methylene blue as previously described (Sandekian et al., 2013); images were obtained and quantitated using an AlphaImager HP image analyzer.
Acknowledgments
We thank Stéphanie Côté for technical assistance in viral titrations and Dr George Szatmari for helpful suggestions to improve the manuscript.
We thank Dr. Takeshi Kobayashi and Dr. Terence Dermody (Vanderbilt University, Nashville, Tennessee) for their generous gift of the plasmids used for reverse genetics. We thank Simon Léveillé and Dr. John Hiscott (Lady Davis Research Institute, Montreal, Canada) for the original stock of BHK cells expressing the T7 RNA polymerase.
This work was supported by an operating grant number 155580 from the Natural Sciences and Engineering Research Council of Canada (NSERC) to G.L. We also thank the “Faculté des études supérieures” of “Université de Montréal” for partial financial support to V.S.
References
- Arnold M.M., Sen A., Greenberg H.B., Patton J.T. The battle between rotavirus and its host for control of the interferon signaling pathway. PLoS Pathog. 2013;9(1):e1003064. doi: 10.1371/journal.ppat.1003064.g002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black A.J., Morris D.G. Clinical trials involving the oncolytic virus, reovirus: ready for prime time? Expert Rev. Clin. Pharmacol. 2012;5(5):517–520. doi: 10.1586/ecp.12.53. [DOI] [PubMed] [Google Scholar]
- Breun L.A., Broering T.J., McCutcheon A.M., Harrison S.J., Luongo C.L., Nibert M.L. Mammalian reovirus L2 gene and λ2 core spike protein sequences and whole-genome comparisons of reoviruses type 1 Lang, type 2 Jones, and type 3 Dearing. Virology. 2001;287(2):333–348. doi: 10.1006/viro.2001.1052. [DOI] [PubMed] [Google Scholar]
- Brochu-Lafontaine V., Lemay G. Addition of exogenous polypeptides on the mammalian reovirus outer capsid using reverse genetics. J. Virol. Methods. 2012;179(2):342–350. doi: 10.1016/j.jviromet.2011.11.021. [DOI] [PubMed] [Google Scholar]
- Buchholz U.J., Finke S., Conzelmann K.K. Generation of bovine respiratory syncytial virus (BRSV) from cDNA: BRSV NS2 is not essential for virus replication in tissue culture, and the human RSV leader region acts as a functional BRSV genome promoter. J. Virol. 1999;73(1):251–259. doi: 10.1128/jvi.73.1.251-259.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bujnicki J.M., Rychlewski L. Reassignment of specificities of two cap methyltransferase domains in the reovirus lambda 2 protein. Genome Biol. 2001;2(9) doi: 10.1186/gb-2001-2-9-research0038. research0038.1–0038.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakrabarty R., Tran H., Fortin Y., Yu Z., Shen S.-H., Kolman J., Onions D., Voyer R., Hagerman A., Serl S., Kamen A., Thompson B., Coffey M. Evaluation of homogeneity and genetic stability of REOLYSIN® (pelareorep) by complete genome sequencing of reovirus after large scale production. Appl. Microbiol. Biotechnol. 2014;98(4):1763–1770. doi: 10.1007/s00253-013-5499-0. [DOI] [PubMed] [Google Scholar]
- Coffey C.M., Sheh A., Kim I.S., Chandran K., Nibert M.L., Parker J.S.L. Reovirus outer capsid protein micro1 induces apoptosis and associates with lipid droplets, endoplasmic reticulum, and mitochondria. J. Virol. 2006;80(17):8422–8438. doi: 10.1128/JVI.02601-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daffis S., Szretter K.J., Schriewer J., Li J., Youn S., Errett J., Lin T.-Y., Schneller S., Zust R., Dong H., Thiel V., Sen G.C., Fensterl V., Klimstra W.B., Pierson T.C., Buller R.M., Gale M., Shi P.-Y., Diamond M.S. 2′-O methylation of the viral mRNA cap evades host restriction by IFIT family members. Nature. 2011;468(7322):452–456. doi: 10.1038/nature09489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danis C., Mabrouk T., Faure M., Lemay G. Interferon has no protective effect during acute or persistent reovirus infection of mouse SC1 fibroblasts. Virus Res. 1997;51(2):139–149. doi: 10.1016/s0168-1702(97)00088-9. [DOI] [PubMed] [Google Scholar]
- Dong H., Fink K., Zust R., Lim S.P., Qin C.F., Shi P.Y. Flavivirus RNA methylation. J. Gen.Virol. 2014;95(4):763–778. doi: 10.1099/vir.0.062208-0. [DOI] [PubMed] [Google Scholar]
- Garcia-Sastre A. Induction and evasion of type I interferon responses by influenza viruses. Virus Res. 2011;162(1–2):12–18. doi: 10.1016/j.virusres.2011.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habjan M., Hubel P., Lacerda L., Benda C., Holze C., Eberl C.H., Mann A., Kindler E., Gil-Cruz C., Ziebuhr J., Thiel V., Pichlmair A. Sequestration by IFIT1 impairs translation of 2′O-unmethylated capped RNA. PLoS Pathog. 2013;9:e1003663. doi: 10.1371/journal.ppat.1003663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyde J.L., Diamond M.S. Innate immune restriction and antagonism of viral RNA lacking 2′-O methylation. Virology. 2015:479–480. doi: 10.1016/j.virol.2015.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irvin S.C., Zurney J., Ooms L.S., Chappell J.D., Dermody T.S., Sherry B. A single-amino-acid polymorphism in reovirus protein μ2 determines repression of interferon signaling and modulates myocarditis. J. Virol. 2012;86(4):2302–2311. doi: 10.1128/JVI.06236-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jabre R., Sandekian V., Lemay G. Amino acid substitutions in σ1 and μ1 outer capsid proteins are selected during mammalian reovirus adaptation to Vero cells. Virus Res. 2013;176(1–2):188–198. doi: 10.1016/j.virusres.2013.06.007. [DOI] [PubMed] [Google Scholar]
- Kelly K., Nawrocki S., Mita A., Coffey M., Giles F.J., Mita M. Reovirus-based therapy for cancer. Expert Opin. Biol. Ther. 2009;9(7):817–830. doi: 10.1517/14712590903002039. [DOI] [PubMed] [Google Scholar]
- Kimura T., Katoh H., Kayama H., Saiga H., Okuyama M., Okamoto T., Umemoto E., Matsuura Y., Yamamoto M., Takeda K. Ifit1 inhibits Japanese encephalitis virus replication through binding to 5′ capped 2′-O unmethylated RNA. J. Virol. 2013;87(18):9997–10003. doi: 10.1128/JVI.00883-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kindler E., Thiel V. To sense or not to sense viral RNA – essentials of coronavirus innate immune evasion. Curr. Opin. Microbiol. 2014;20:69–75. doi: 10.1016/j.mib.2014.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi T., Antar A., Boehme K., Danthi P., Eby E., Guglielmi K., Holm G., Johnson E., Maginnis M., Naik S. A plasmid-based reverse genetics system for animal double-stranded RNA viruses. Cell Host Microbe. 2007;1(2):147–157. doi: 10.1016/j.chom.2007.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemay G., Tumilasci V., Hiscott J. Uncoating reo: uncovering the steps critical for oncolysis. Mol. Ther. 2007;15(8):1406–1407. doi: 10.1038/sj.mt.6300242. [DOI] [PubMed] [Google Scholar]
- Ma Y., Wei Y., Zhang X., Zhang Y., Cai H., Zhu Y., Shilo K., Oglesbee M., Krakowka S., Whelan S.P.J., Li J., Lyles D.S. mRNA cap methylation influences pathogenesis of vesicular stomatitis virus in vivo. J. Virol. 2014;88(5):2913–2926. doi: 10.1128/JVI.03420-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcato P., Shmulevitz M., Pan D., Stoltz D., Lee P.W. Ras transformation mediates reovirus oncolysis by enhancing virus uncoating, particle infectivity, and apoptosis-dependent release. Mol. Ther. 2007;15(8):1522–1530. doi: 10.1038/sj.mt.6300179. [DOI] [PubMed] [Google Scholar]
- Mendez I.I., Hermann L.L., Hazelton P.R., Coombs K.M. A comparative analysis of freon substitutes in the purification of reovirus and calicivirus. J. Virol. Methods. 2000;90(1):59–67. doi: 10.1016/s0166-0934(00)00217-2. [DOI] [PubMed] [Google Scholar]
- Menachery V.D., Yount B.L., Josset L., Gralinski L.E., Scobey T., Agnihothram S., Katze M.G., Baric R.S. Attenuation and restoration of severe acute respiratory syndrome coronavirus mutant lacking 2′-O-methyltransferase activity. J. Virol. 2014;88(8):4251–4264. doi: 10.1128/JVI.03571-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nygaard R.M., Lahti L., Boehme K.W., Ikizler M., Doyle J.D., Dermody T.S., Schiff L.A. Genetic determinants of reovirus pathogenesis in a murine model of respiratory infection. J. Virol. 2013;87(16):9279–9289. doi: 10.1128/JVI.00182-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden K.M., Snyder M.J., Dennis A.F., Patton J.T. Predicted structure and domain organization of rotavirus capping enzyme and innate immune antagonist VP3. J. Virol. 2014;88(16):9072–9085. doi: 10.1128/JVI.00923-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perdiguero B., Esteban M. The interferon system and vaccinia virus evasion mechanisms. J. Interf. Cytokine Res. 2009;29(9):581–598. doi: 10.1089/jir.2009.0073. [DOI] [PubMed] [Google Scholar]
- Qashqari H., Al-Mars A., Chaudhary A., Abuzenadah A., Damanhouri G., Alqahtani M., Mahmoud M., Sayed Zaki, El. M., Fatima K., Qadri I. Understanding the molecular mechanism(s) of hepatitis C virus (HCV) induced interferon resistance. Infect. Genet. Evol. 2013;19:113–119. doi: 10.1016/j.meegid.2013.06.025. [DOI] [PubMed] [Google Scholar]
- Reinisch K.M., Nibert M.L., Harrison S.C. Structure of the reovirus core at 3.6 A resolution. Nature. 2000;404(6781):960–967. doi: 10.1038/35010041. [DOI] [PubMed] [Google Scholar]
- Rudd P., Lemay G. Correlation between interferon sensitivity of reovirus isolates and ability to discriminate between normal and Ras-transformed cells. J. Gen. Virol. 2005;86(5):1489–1497. doi: 10.1099/vir.0.80628-0. [DOI] [PubMed] [Google Scholar]
- Sandekian V., Lim D., Prud’homme P., Lemay G. Transient high level mammalian reovirus replication in a bat epithelial cell line occurs without cytopathic effect. Virus Res. 2013;173(2):327–335. doi: 10.1016/j.virusres.2013.01.010. [DOI] [PubMed] [Google Scholar]
- Schiff L.A. Structure and functions of the orthoreovirus σ3 protein. In: Patton J.T., editor. Segmented Double-stranded RNA Viruses: Structure and Molecular Biology. Caister Academic Press; Norfolk, U.K.: 2008. pp. 173–188. [Google Scholar]
- Sherry B., Torres J., Blum M.A. Reovirus induction of and sensitivity to beta interferon in cardiac myocyte cultures correlate with induction of myocarditis and are determined by viral core proteins. J. Virol. 1998;72(2):1314–1323. doi: 10.1128/jvi.72.2.1314-1323.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherry B. Rotavirus and reovirus modulation of the interferon response. J. Interf. Cytokine Res. 2009;29(9):559–567. doi: 10.1089/jir.2009.0072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherry B., Patton J.T., Dermody T.S. Innate immune responses elicited by reovirus and rotavirus. In: Brasier A.R., Garcia-Sastre A., Lemon S.M., editors. Cellular Signaling and Innate Immune Responses to RNA Virus Infections. ASM Press; Washington, D.C: 2009. pp. 403–422. [Google Scholar]
- Shmulevitz M., Pan L.-Z., Garant K., Pan D., Lee P.W.K. Oncogenic Ras promotes reovirus spread by suppressing IFN-β production through negative regulation of RIG-I signaling. Cancer Res. 2010;70(12):4912–4921. doi: 10.1158/0008-5472.CAN-09-4676. [DOI] [PubMed] [Google Scholar]
- Stebbing R.E., Irvin S.C., Rivera-Serrano E.E., Boehme K.W., Ikizler M., Yoder J.A., Dermody T.S., Sherry B., Lyles D.S. An ITAM in a nonenveloped virus regulates activation of NF-κB, induction of beta interferon, and viral spread. J. Virol. 2014;88(5):2572–2583. doi: 10.1128/JVI.02573-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strong J.E., Coffey M.C., Tang D., Sabinin P., Lee P.W. The molecular basis of viral oncolysis: usurpation of the Ras signaling pathway by reovirus. EMBO J. 1998;17(12):3351–3362. doi: 10.1093/emboj/17.12.3351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Wollenberg D.J.M., Dautzenberg I.J.C., van den Hengel S.K., Cramer S.J., de Groot R.J., Hoeben R.C. Isolation of reovirus T3D mutants capable of infecting human tumor cells independent of junction adhesion molecule-A. PLoS ONE. 2012;7(10):e48064. doi: 10.1371/journal.pone.0048064.t001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virgin H.W., Mann M.A., Fields B.N., Tyler K.L. Monoclonal antibodies to reovirus reveal structure/function relationships between capsid proteins and genetics of susceptibility to antibody action. J. Virol. 1991;65(12):6772–6781. doi: 10.1128/jvi.65.12.6772-6781.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin P., Keirstead N.D., Broering T.J., Arnold M.M., Parker J.S., Nibert M.L., Coombs K.M. Comparisons of the M1 genome segments and encoded μ2 proteins of different reovirus isolates. Virol. J. 2004;1(1):6. doi: 10.1186/1743-422X-1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang R., Jha B.K., Ogden K.M., Dong B., Zhao L., Elliott R., Patton J.T., Silverman R.H., Weiss S.R. Homologous 2′,5′-phosphodiesterases from disparate RNA viruses antagonize antiviral innate immunity. Proc. Natl. Acad. Sci. USA. 2013;110(32):13114–13119. doi: 10.1073/pnas.1306917110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu B., Yang C., Liu H., Cheng L., Song F., Zeng S., Huang X., Ji G., Zhu P. Identification of the active sites in the methyltransferases of a transcribing dsRNA virus. J. Mol. Biol. 2014;426(11):2167–2174. doi: 10.1016/j.jmb.2014.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zurney J., Kobayashi T., Holm G.H., Dermody T.S., Sherry B. Reovirus μ2 protein inhibits interferon signaling through a novel mechanism involving nuclear accumulation of interferon regulatory factor 9. J. Virol. 2009;83(5):2178–2187. doi: 10.1128/JVI.01787-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zust R., Cervantes-Barragan L., Habjan M., Maier R., Neuman B.W., Ziebuhr J., Szretter K.J., Baker S.C., Barchet W., Diamond M.S., Siddell S.G., Ludewig B., Thiel V. Ribose 2′-O-methylation provides a molecular signature for the distinction of self and non-self mRNA dependent on the RNA sensor Mda5. Nat. Immunol. 2011;12(2):137–143. doi: 10.1038/ni.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]