To the Editor,
Since the outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in Wuhan, a cumulative number of 80,754 confirmed cases were reported in China until March 9, 2020 [1]. To prevent and control the spread of the pandemic, effective measures of medical isolation and self-isolation were widely adopted. However, isolation may cause negative psychological effects [2], which in turn may impair sleep quality [3]. This study investigated the sleep status among the population in isolation.
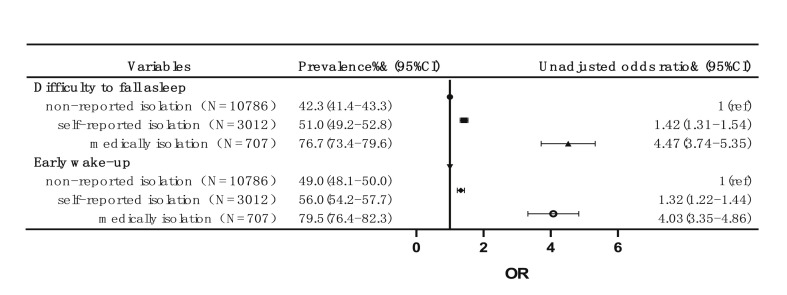
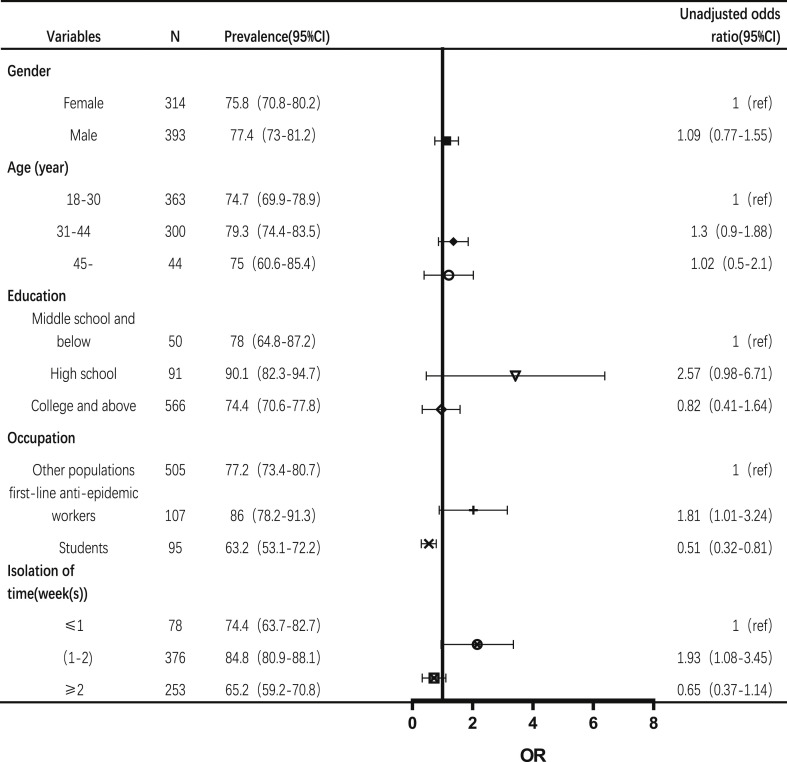
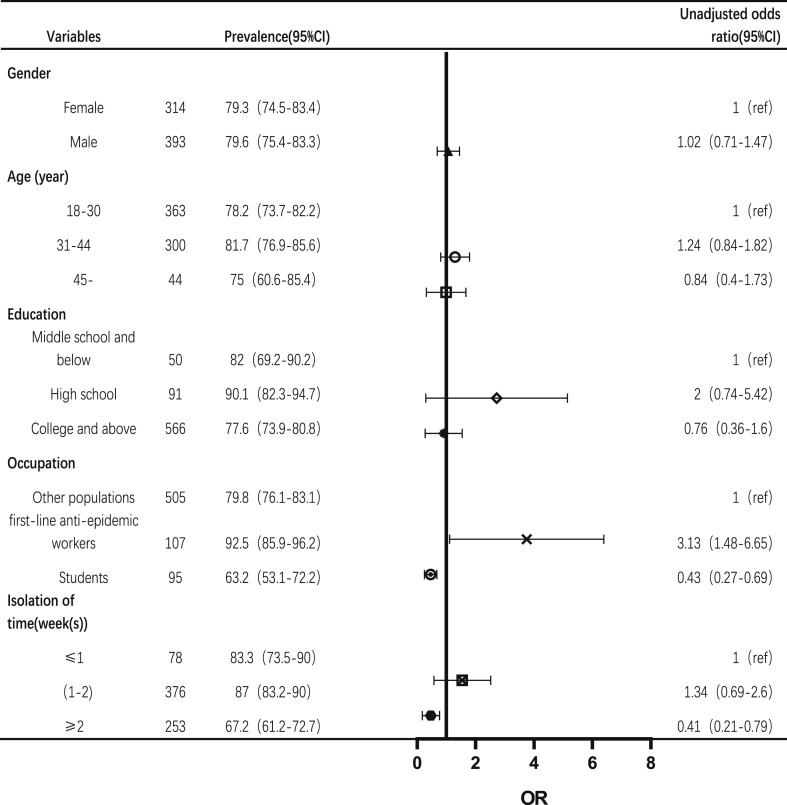
Demographic data, isolation status, and sleep status were collected via a nationwide online self-report questionnaire survey conducted in February 2020 in China, which collected 14,505 valid questionnaires. Medically isolated population was defined as people who were infected, suspected to be infected, had been exposed to infected or those suspected to be infected, or individuals who visited areas of high epidemic severity during the outbreak. Self-reported isolation population referred to people who reported self-isolation but did not meet the four conditions of medical isolation. A total of 76.7% of the medically isolated population reported difficulty falling asleep at least once over the week preceding the survey, while the corresponding rates among self-reported isolation (51.0%) and non-reported isolation groups (42.3%) were significantly lower. Likewise, the rate of early wake-up at least once over the week preceding the survey (79.5%) was highest among the medically isolated group (Fig. 1 ). Among the medically isolated population, front-line anti-epidemic workers were more likely to have difficulty falling asleep (odds ratio, OR: 1.81) and reported early wake-up (OR: 3.13) compared with the control group. The prevalence of sleep problems was high during the first two weeks of medical isolation and decreased thereafter (Fig. 2, Fig. 3 ). In conclusion, sleep problems were found to be prominent among the medically-isolated population, which may be due to fear of infection, suggesting that medically isolated individuals require appropriate psychological intervention.
Fig. 1.
Prevalence of self-reported sleep problems at least once during the week preceding the survey among individuals in different states of isolation.
Fig. 2.
Prevalence and distribution of difficulty to fall asleep at least once during the week preceding the survey among individuals in medical isolation.
Fig. 3.
Prevalence and distribution of early wake-up at least once during the week preceding the survey among individuals in medical isolation.
Funding
This work was supported by the China Postdoctoral Science Foundation (2019M650358), the Medical Scientific Research Foundation of Guangdong Province (A2019155), and the Sanming Project of Medicine in Shenzhen (SZSM201612079).
Footnotes
The authors declare no conflicts of interest.
The ICMJE Uniform Disclosure Form for Potential Conflicts of Interest associated with this article can be viewed by clicking on the following link: https://doi.org/10.1016/j.sleep.2020.04.014.
Contributor Information
Jianbo Liu, Email: liujianbo@csu.edu.cn.
Jianping Lu, Email: szlujianping@126.com.
Conflict of interest
The following is the supplementary data related to this article:
Multimedia component 1
References
- 1.National Health Commission of the People’s Republic of China . 2020. Update on novel coronavirus pneumonia at 24:00 as at 9 March.2020.http://www.nhc.gov.cn/yjb/s7860/202003/948a03ad76f54d3583a018785efd7be9.shtml [Google Scholar]
- 2.Abad C., Fearday A., Safdar N. Adverse effects of isolation in hospitalised patients: a systematic review. J Hosp Infect. 2010;76(2) doi: 10.1016/j.jhin.2010.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yu B., Steptoe A., Niu K. Prospective associations of social isolation and loneliness with poor sleep quality in older adults. Qual Life Res. 2018;27(3):683–691. doi: 10.1007/s11136-017-1752-9. https://link.springer.com/article/10.1007%2Fs11136-017-1752-9 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Multimedia component 1