Highlights
-
•
Commonly reported symptoms are headache, throat pain and lethargy.
-
•
A large number of healthcare workers report more than four symptoms.
-
•
Those with physical symptoms had higher rates of depression, anxiety, stress, PTSD.
-
•
Those with physical symptoms had higher mean scores in the IES-R, DASS subscales.
-
•
Association between physical symptoms and psychological outcomes may be bidirectional.
Keywords: COVID-19, Healthcare workers, Psychological impact, Anxiety, Depression, Stress, Pandemic, Physical symptoms
Abstract
Objective
Since the declaration of the coronavirus 2019 (COVID-19) outbreak as pandemic, there are reports on the increased prevalence of physical symptoms observed in the general population. We investigated the association between psychological outcomes and physical symptoms among healthcare workers.
Methods
Healthcare workers from 5 major hospitals, involved in the care for COVID-19 patients, in Singapore and India were invited to participate in a study by performing a self-administered questionnaire within the period of February 19 to April 17, 2020. Healthcare workers included doctors, nurses, allied healthcare workers, administrators, clerical staff and maintenance workers. This questionnaire collected information on demographics, medical history, symptom prevalence in the past month, Depression Anxiety Stress Scales (DASS-21) and the Impact of Events Scale-Revised (IES-R) instrument. The prevalence of physical symptoms displayed by healthcare workers and the associations between physical symptoms and psychological outcomes of depression, anxiety, stress, and post-traumatic stress disorder (PTSD) were evaluated.
Results
Out of the 906 healthcare workers who participated in the survey, 48 (5.3%) screened positive for moderate to very-severe depression, 79 (8.7%) for moderate to extremely-severe anxiety, 20 (2.2%) for moderate to extremely-severe stress, and 34 (3.8%) for moderate to severe levels of psychological distress. The commonest reported symptom was headache (32.3%), with a large number of participants (33.4%) reporting more than four symptoms. Participants who had experienced symptoms in the preceding month were more likely to be older, have pre-existing comorbidities and a positive screen for depression, anxiety, stress, and PTSD. After adjusting for age, gender and comorbidities, it was found that depression (OR 2.79, 95% CI 1.54–5.07, p = 0.001), anxiety (OR 2.18, 95% CI 1.36–3.48, p = 0.001), stress (OR 3.06, 95% CI 1.27–7.41, p = 0.13), and PTSD (OR 2.20, 95% CI 1.12–4.35, p = 0.023) remained significantly associated with the presence of physical symptoms experienced in the preceding month. Linear regression revealed that the presence of physical symptoms was associated with higher mean scores in the IES-R, DASS Anxiety, Stress and Depression subscales.
Conclusions
Our study demonstrates a significant association between the prevalence of physical symptoms and psychological outcomes among healthcare workers during the COVID-19 outbreak. We postulate that this association may be bi-directional, and that timely psychological interventions for healthcare workers with physical symptoms should be considered once an infection has been excluded.
1. Introduction
On December 31, 2019, the China office of World Health Organization (WHO) was notified regarding some cases of pneumonia of unknown etiology in Wuhan City of Hubei province. It was subsequently termed coronavirus disease 2019 (COVID-19) by the WHO. The rapid global spread of the disease led to the declaration of COVID-19 as a pandemic on March 11, 2020 (Organization, 2020). Being a global hub with high international traffic, Singapore observed an increasing spread of COVID-19. Accordingly, the Disease Outbreak Response System Condition (DORSCON) alert level was escalated to orange on February 7, 2020, which indicates that the outbreak is deemed to have moderate to high public health impact, necessitating additional measures like quarantine and temperature screening to minimize risk of further virus transmission in the community (S K. Singapore raises cornavirus outbreak alert to orange: What does it mean, 2020, SK CA-L, 2020). Similarly, being a densely populated country, the Indian authorities imposed a lockdown on March 24, 2020, which involved barring of all public transport and prohibiting opening of public spaces (The Times of India, 2020). Between February 19 to April 17, 2020, Singapore reported slightly over 5000 confirmed COVID-19 cases with 11 deaths, while India has reported >13,000 confirmed cases with >400 deaths (The Times of India, 2020, Ministry of Health Singapore, 2019). Much uncertainty revolved around the nature of spread of COVID-19, its severity, associated mortality and the availability of essential resources like facial masks, hand sanitizers and digital thermometers. Widespread fear of imposed quarantine and lockdown measures led to the unusual displays of panic in the form of frenzied buying of goods by the general public observed in many countries (Coronavirus: Hong Kong shoppers snap up rice and noodles as fears over outbreak mount, 2020, 'It's pandemonium': virus panic-buying hits Los Angeles, 2020, T A. Coronavirus: Politicians, supermarkets urge calm amid panic-buying of groceries, 2020).
Infectious disease outbreaks are known to have psychological impact on healthcare workers as well as the general population. A notable example would be the psychological sequelae observed during the Severe Acute Respiratory Syndrome (SARS) outbreak in 2003 (McAlonan et al., 2007, Ministry of Health S, 2004). Studies on the SARS outbreak revealed that healthcare workers experienced acute stress reactions (Tam et al., 2004, Grace et al., 2005).
In addition to the specific physical manifestations of various diseases, some symptoms may arise due to the psychological sequelae of these infection outbreaks. Such psychosomatic symptoms have been reported with increased prevalence during and after the outbreaks, such as the SARS and Ebola virus (Lam et al., 2009, Lee et al., 2005, Marco et al., 2015, Matua and Wal, 2015, Tucker, xxxx, Xiang et al., 2020). The commonly reported symptoms range from more specific symptoms like pain(Lam et al., 2009) to non-specific ones like fatigue, weakness and lethargy (Leow et al., 2005). In some cases, symptoms not perceived to be directly related to a particular infectious disease may be reported. For instance, some survivors of SARS outbreak developed chronic extra-pulmonary symptoms during outpatient clinical follow-up (Leow et al., 2005). It is important to understand the prevalence and patterns of such somatic manifestations since they can lead to undesirable overcrowding of hospital emergency departments (Farr, 2020, Abelson, 2020), causing additional workload to the already constrained healthcare systems. We investigate the association between various physical symptoms and psychological distress amongst healthcare workers in Singapore and India during the current COVID-19 outbreak.
2. Methods
2.1. Study setting and population
From February 19 to April 17, 2020, we recruited healthcare workers from major tertiary healthcare institutions in Singapore and India. During the study period, the healthcare institutions were actively involved in the care of COVID-19 patients. Study participants included doctors, nurses, allied healthcare workers (pharmacists, physiotherapists, occupational therapists), technicians, administrators, clerical staff and maintenance workers. Written informed consent was obtained from all participants and the study was approved by the institutional review board, in accordance to the principles in the Declaration of Helsinki.
2.2. Screening questionnaire
The study questionnaire, written in English, comprised five main components- demographic characteristics, medical history, symptom prevalence in the previous month, Depression Anxiety Stress Scales (DASS-21) and the Impact of Events Scale-Revised (IES-R) instruments.
Baseline demographic characteristics such as gender, age, ethnicity, marital status, occupation and past medical history were recorded. Participants had to indicate if they experienced any of the 16 listed physical symptoms, general or respiratory-related symptoms, during the previous month and rated the severity of the reported symptoms (Supplementary Material 1). The study questionnaire was adopted from our previous study related to the psychological impact on healthcare workers in Singapore during the COVID-19 outbreak (Tay et al., 2020).
Depression, anxiety and stress were assessed using DASS-21 (LP, LS, 1995), which is a validated screening instrument for use among patients and general populations. It is a self-reported 21-item system developed by the University of New South Wales, Australia, which provides independent measures of depression, stress and anxiety with recommended severity thresholds for the depression, stress and anxiety subscales. The scores for each of the three components were calculated by summing up the scores for the relevant items, and multiplying by two to calculate the final score. Cut-off scores of > 9, >7 and > 14 represent a positive screen of depression, anxiety and stress, respectively. On the DASS-21 depression subscales, scores of 10–13 were deemed as “mild”, 14–20 as “moderate”, 21–27 as “severe”, and 28–42 as “extremely severe” depression. The DASS-21 anxiety subscale score was assessed as “mild” (8–9), “moderate” (10–14), “severe” (15–19), and extremely severe” (20–42). The DASS-21 stress subscale score was divided into “mild” (15–18), “moderate” (19–25), “severe” (26–33), and “extremely severe” stress (34–42) (Tay et al., 2020).
The psychological distress of the outbreak was assessed using the IES-R25, (Weiss, 2007), which is a validated 22-item self-report that measures the subjective distress caused by traumatic events. It has 3 subscales (Intrusion, Avoidance and Hyperarousal), which are closely affiliated with post-traumatic stress disorder (PTSD) symptoms. Participants were asked to rate the level of distress for each component during the previous seven days of their interview. The total IES-R score was graded for severity from normal (0–23), mild (24–32), moderate (33–36), and severe psychological impact (>37). A cut-off score of 24 was used to define PTSD of a clinical concern (Creamer et al., 2003, Weiss, 2007). Both DASS-21 and IES-R have been validated for use in a recent Chinese study investigating the psychological impact of COVID-19 on the general population (Wang et al., 2020a, Ho et al., 2014).
2.3. Study outcomes
We evaluated the prevalence of physical symptoms reported by the healthcare workers during previous one month before the survey administration period. Additionally, we investigated the association between the presence of various physical symptoms and psychological outcomes, namely the DASS-21 score and IES-R score.
2.4. Statistical analyses
Categorical variables are expressed as absolute values (percentage) and continuous variables were expressed as mean value ± (standard deviation). Student’s t-test was used to examine the association between continuous variables and Pearson’s chi-square test (or Fisher’s Exact Test, where appropriate) was used to evaluate categorical variables. Multivariable logistic regression was used to adjust for the effect of confounders when appropriate to determine independent associations of binary outcomes. Linear regression was employed to evaluate for associations between baseline characteristics, risk status, physical symptoms and the mean scores for DASS-21 and IES-R components. A p-value of<0.05 was deemed significant for this study. All statistical analyses were performed using IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY.
3. Results
3.1. Participants
Of the 1000 invited healthcare workers from the major hospitals in Singapore and India, 906 (90.6%) agreed to participate in this study. Of which, 480 respondents were from Singapore and 426 from India. Majority (583, 64.3%) were female and the median age was 29 (interquartile range: 25–35) years (Table 1 ). Most (55.1%) of the participants were Indian, followed by Chinese (33.7%) and Malay (4.8%) ethnicity. Being a relatively younger study population, 50.2% of the participants were unmarried. Two hundred and five (22.6%) participants had pre-existing comorbidities, migraine (9.6%) being the most prevalent followed by eczema (4.1%) and asthma (4.0%). Nurses comprised 39.2% of the study population, followed by physicians (29.6%) and allied healthcare professionals (10.6%) (Table 1).
Table 1.
Baseline characteristics of study participants (N = 906).
| Characteristic | N (%) |
|---|---|
| Sex, n (%) | |
| Female | 583 (64.3) |
| Male | 323 (35.7) |
| Median Age (IQR), y | 29 (25 – 35) |
| Ethnicity, n (%) | |
| Chinese | 305 (33.7) |
| Indian | 499 (55.1) |
| Malay | 44 (4.8) |
| Others | 58 (6.4) |
| Marital Status, n (%) | |
| Single | 455 (50.2) |
| Married | 434 (47.9) |
| Divorced, separated or widowed | 17 (1.9) |
| Occupation, n (%) | |
| Physician | 268 (29.6) |
| Nurse | 355 (39.2) |
| Allied health care professional | 96 (10.6) |
| Technician | 40 (4.4) |
| Clerical Staff | 56 (6.2) |
| Administrator | 39 (4.3) |
| Maintenance worker | 52 (5.7) |
| Medical History, n (%) | |
| Hypertension | 34 (3.8) |
| Hyperlipidemia | 29 (3.2) |
| Diabetes Mellitus | 14 (1.4) |
| Asthma | 36 (4.0) |
| Eczema | 37 (4.1) |
| Migraine | 87 (9.6) |
| Cigarette Smoking | 29 (3.2) |
| Ischemic Heart Disease | 4 (0.4) |
| Stroke | 1 (0.1) |
| Other comorbid conditions | 30 (3.3) |
3.2. Prevalence of physical symptoms
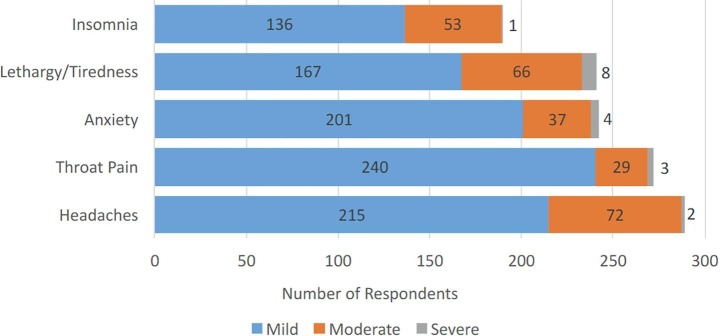
The commonest reported symptoms were headache (289, 31.9%), throat pain (304, 33.6%), anxiety (242, 26.7%), lethargy (241, 26.6%), and insomnia (190, 21.0%) (Fig. 1 ). While 302 (33.3%) respondents did not report any symptom within the preceding 1-month of the survey administration date, 115 (12.7%) reported one symptom, 113 (12.5%) reported two, 73 (8.1%) reported three, and 303 (33.4%) reported more than four symptoms. Importantly, the symptoms were generally mild in severity.
Fig. 1.
Five most common symptoms experienced during the past one month of the COVID-19 outbreak (N = 906).
3.3. Psychological outcomes
Using our predefined cut-offs for the DASS-21 scoring system to screen for depression, anxiety and stress, we found anxiety in 142 (15.7%), depression in 96 (10.6%) and stress in 47 (5.2%) study participants. There was no difference in psychological outcomes between study participants from the two countries (Table 2 ). The overall mean DASS-21 depression subscale score was 3.08 (SD 4.86). Of the 96 healthcare workers who screened positive for depression, 50% of them (48) were scored as moderate to very severe depression. The overall mean DASS-21 anxiety subscale score was 3.21 (SD 4.29). Of the 142 patients who screened positive for anxiety, 55.6% of them (79) showed moderate to very severe anxiety. In terms of the DASS-21 stress subscale, the overall mean score was 4.62 (SD 5.54). Stress was moderate-to-severe in 20 of the 47 participants (42.6%) who screened positive for it (Fig. 2 ).
Table 2.
Comparison of the prevalence of depression, anxiety, stress and post-traumatic stress disorder between the healthcare workers in Singapore and India (N = 906).
| Overall (N = 906) | Singapore (N = 480) | India (N = 426) | p-value | |
|---|---|---|---|---|
| Depression | 96 (10.6%) | 43 (9%) | 53 (12.4%) | 0.089 |
| Anxiety | 142 (15.7%) | 69 (14.4%) | 73 (17.1%) | 0.254 |
| Stress | 47 (5.2%) | 31 (6.5%) | 16 (3.8%) | 0.067 |
| Post-traumatic stress disorder | 67 (7.4%) | 36 (7.5%) | 31 (7.3%) | 0.898 |
Categorical variables displayed as n (%).
Fig. 2.
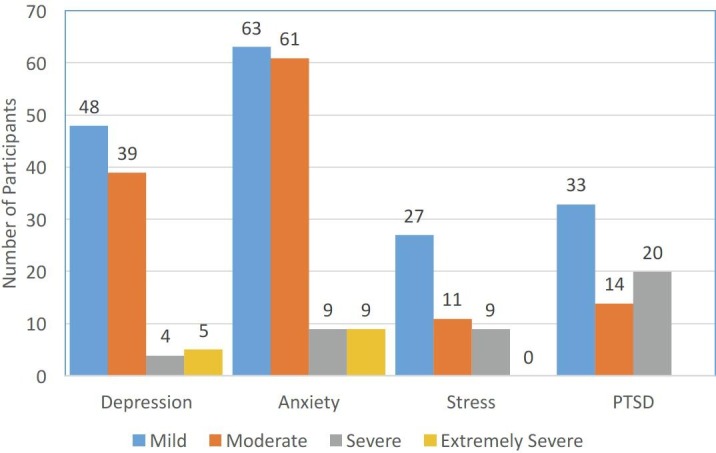
Number of participants experiencing adverse psychological impact, stratified by severity using DASS-21 (depression, anxiety and stress) and IES-R (post-traumatic stress disorder) (N = 906).
Healthcare workers rated their levels of psychological distress according to the IES-R during the preceding 7 days. The mean total IES-R score was 8.29 (SD 9.79) while the means (SD) for IES-R subsets for Intrusion, Avoidance and Hyperarousal were 0.39 (0.49), 0.38 (0.50) 0.36 (0.46), respectively. Of note, 67 (7.4%) of the study cohort screened positive for clinical concern of PTSD, of which 34 demonstrated moderate to severe levels of psychological distress.
3.4. Comparing healthcare workers with and without physical symptoms
The group which displayed presence of symptoms in the preceding month had less female participants compared to the group without symptoms (odds ratio (OR) 0.68, 95% confidence interval (CI) 0.50–0.91, P = 0.010). On the other hand, participants with physical symptoms were more likely to have pre-existing comorbidities (OR 2.87, 95% CI 1.94–4.24, p < 0.001) and older in age (mean difference 2.22, 95% CI 0.88–3.55, p = 0.001). In terms of study outcomes, those with physical symptoms were more likely to have a positive screening for depression (OR 3.23, 95% CI 1.80–5.80, p < 0.001), anxiety (OR 2.66, 95% CI 1.69–4.20, p < 0.001), stress (OR 3.59, 95% CI 1.51–8.56, p = 0.002), and PTSD (OR 2.70, 95% CI 1.40–5.24, p = 0.002) (Table 2).
3.5. Physical symptoms and psychological outcomes
In the multivariable logistic regression model, after adjustment for age, gender and presence of comorbidities, the psychological outcomes depression (OR 2.79, 95% CI 1.54–5.07, p = 0.001), anxiety (OR 2.18, 95% CI 1.36–3.48, p = 0.001), stress (OR 3.06, 95% CI 1.27–7.41, p = 0.13), and PTSD (OR 2.20, 95% CI 1.12–4.35, p = 0.023) remained significantly associated with the presence of physical symptoms experienced in the preceding month (Table 3 ).
Table 3.
Univariate analysis of participants presenting with any symptoms and no symptoms experienced in the study population (N = 906).
| Any symptoms experiences(n = 604) | No symptoms experiences(n = 302) | P-value | |
|---|---|---|---|
| Demographic | |||
| Female Gender | 371 (61.4%) | 212 (70.2%) | 0.009 |
| Married | 301 (49.8%) | 133 (44.0%) | 0.100 |
| Presence of comorbidities | 169 (28.0%) | 36 (12.0%) | <0.001 |
| Age | 31.40 (±9.4) | 29.2 (±9.4) | 0.001 |
| Outcomes | |||
| Depression | 82 (13.6%) | 14 (4.6%) | <0.001* |
| Anxiety | 117 (19.4%) | 25 (8.3%) | <0.001* |
| Stress | 41 (6.8%) | 6 (2.0%) | 0.002* |
| Post-traumatic stress disorder | 56 (9.3%) | 11 (3.6%) | 0.002* |
* Psychological outcome remains statistically significant after adjusting for age, gender and presence of comorbidities.
Categorical variables displayed as n (%), continuous variables displayed as mean (±standard deviation)
Linear regression revealed that the presence of physical symptoms was associated with higher mean scores in the IES-R, DASS-21 Anxiety, Stress and Depression subscales. This association was present across the three respiratory-related symptoms (sore throat, breathlessness and cough) as well as constitutional symptoms like lethargy, myalgia, poor appetite. However, there was no statistical significance between the association of coryza and psychological distress (Table 4 ).
Table 4.
Linear regression of physical symptoms in the past one month associated with the psychological impact of the COVID-19 outbreak (N = 906).
| Variables | Impact of event scale | DASS-21 Stress | DASS-Anxiety | DASS-Depression | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N (%) | R-Squared(R2) | Adjusted R-Squared (AR2) | β (95% CI) | R2 | AR2 | β (95% CI) | R2 | AR2 | β (95% CI) | R2 | AR2 | β (95% CI) | |
| Throat pain | 272 (30%) | 0.026 | 0.025 | 0.292* (0.176, 0.408) | 0.054 | 0.053 | 0.418** (0.304, 0.533) | 0.080 | 0.079 | 0.508** (0.396, 0.621) | 0.038 | 0.037 | 0.351* (0.235, 0.466) |
| Nausea/vomiting | 96 (10.6%) | 0.037 | 0.036 | 0.548** (0.366, 0.729) | 0.017 | 0.016 | 0.373** (0.190, 0.556) | 0.060 | 0.059 | 0.696** (0.517, 875) | 0.017 | 0.016 | 0.374** (0.190, 0.557) |
| Anxiety | 242 (26.7%) | 0.137 | 0.136 | 0.649** (0.543, 0.755) | 0.161 | 0.160 | 0.704** (0.599, 0.809) | 0.133 | 0.133 | 0.641** (0.534, 0.747) | 0.112 | 0.111 | 0.587** (0.479, 0.695) |
| Insomnia | 190 (21.0%) | 0.092 | 0.091 | 0.535** (0.426, 0.645) | 0.082 | 0.081 | 0.506** (0.396, 0.616) | 0.082 | 0.081 | 0.505**(0.394, 0.615) | 0.080 | 0.079 | 0.500** (0.389, 0.610) |
| Poor appetite | 128 (14.1%) | 0.043 | 0.042 | 0.450** (0.312, 0.589) | 0.025 | 0.024 | 0.342** (0.202, 0.482) | 0.077 | 0.076 | 0.602** (0.466, 0.738) | 0.047 | 0.046 | 0.472** (0.334, 0.611) |
| Headache | 289 (31.9%) | 0.044 | 0.043 | 0.328** (0.229, 0.427) | 0.040 | 0.039 | 0.310** (0.211, 0.410) | 0.066 | 0.065 | 0.400** (0.302, 0.498) | 0.020 | 0.019 | 0.219** (0.119, 0.320) |
| Neck stiffness | 149 (16.4%) | 0.036 | 0.035 | 0.370** (0.245, 0.494) | 0.046 | 0.045 | 0.417** (0.293, 0.541) | 0.046 | 0.045 | 0.415** (0.292, 0.539) | 0.030 | 0.029 | 0.337** (0.212, 0.462) |
| Cough | 153 (16.9%) | 0.012 | 0.011 | 0.231* (0.095, 0.367) | 0.023 | 0.022 | 0.314** (0.179, 0.449) | 0.032 | 0.031 | 0.375** (0.241, 0.510) | 0.013 | 0.012 | 0.238* (0.102, 0.373) |
| Sputum | 102 (11.3%) | 0.031 | 0.030 | 0.440** (0.279, 0.601) | 0.043 | 0.042 | 0.519** (0.359, 0.679) | 0.052 | 0.051 | 0.571** (0.411, 0.730) | 0.014 | 0.013 | 0.292** (0.130, 0.455) |
| Breathless-ness | 56 (6.2%) | 0.036 | 0.035 | 0.699**(0.463,0.934) | 0.020 | 0.019 | 0.525**(0.287, 0.762) | 0.077 | 0.076 | 1.018** (0.787, 1.249) | 0.028 | 0.027 | 0.616** (0.380, 0.853) |
| Coryza | 127 (14.0%) | 0.003 | 0.002 | 0.126(-0.026, 0.278) | 0.013 | 0.012 | 0.262*(0.111, 0.413) | 0.016 | 0.014 | 0.290** (0.139, 0.441) | 0.009 | 0.008 | 0.218*(0.067, 0.370) |
| Joint/muscle pain | 187 (20.6%) | 0.101 | 0.099 | 0.497** (0.362, 0.632) | 0.087 | 0.085 | 0.463** (0.327, 0.600) | 0.062 | 0.060 | 0.389** (0.251, 0.527) | 0.072 | 0.070 | 0.420** (0.282, 0.557) |
| Rashes | 33 (3.6%) | 0.087 | 0.086 | 0.511** (0.403, 0.619) | 0.096 | 0.095 | 0.536** (0.429, 0.643) | 0.073 | 0.072 | 0.469** (0.361, 0.578) | 0.071 | 0.070 | 0.462** (0.354, 0.571) |
| Lethargy/tiredness | 241 (26.6%) | 0.066 | 0.065 | 0.391** (0.295, 0.488) | 0.128 | 0.127 | 0.547** (0.454, 0.640) | 0.099 | 0.098 | 0.481** (0.387, 0.576) | 0.095 | 0.094 | 0.470** (0.375, 0.565) |
| Itching | 53 (5.8%) | 0.011 | 0.010 | 0.351* (0.133, 0.568) | 0.012 | 0.011 | 0.361* (0.143, 0.578) | 0.019 | 0.018 | 0.468** (0.251, 0.684) | 0.019 | 0.018 | 0.465** (0.247, 0.682) |
| Watery eyes | 50 (5.5%) | 0.016 | 0.015 | 0.463** (0.229, 0.697) | 0.015 | 0.014 | 0.444** (0.210, 0.678) | 0.026 | 0.025 | 0.588** (0.355, 0.820) | 0.015 | 0.014 | 0.447** (0.213, 0.680) |
* p-value < 0.05; ** p-value < 0.001.
4. Discussion
This multinational, multicenter study found significant association between adverse psychological outcomes and physical symptoms displayed by healthcare workers during the current COVID-19 pandemic. Our findings mirror the trend in recent studies on the psychological impact of the COVID-19 epidemic among the general population in China during its initial stages (Wang et al., 2020a, Li et al., 2020, Kang et al., 2019). We have previously reported that the psychological impact (specifically anxiety) of COVID-19 was more common among non-medically trained healthcare workers when compared to the medically trained personnel (Tay et al., 2020).
Symptoms of COVID-19 infection are wide-ranging, and may be non-specific and similar to other viral infections (Guan et al., 2019). Therefore, when healthcare workers develop any such symptoms, they often faced the dilemma of whether to apply for medical leave of absence, or to continue working alongside their over-worked colleagues during this critical period. Even though healthcare workers are entitled to take paid sick leave for a given number of days, little is known about the employment risks posed, especially to the low-paid non-medically trained healthcare contract workers in the event of a prolonged absence. Psychological distress levels may also be exacerbated by the fear of being a carrier of the virus, causing transmission amongst fellow healthcare workers and their own families if they choose to continue to work. The fear of transmission is especially high due to the reports of asymptomatic transmission of COVID-19, including high transmission rates amongst healthcare workers during in China where as many as 3000 healthcare workers contracted the infection and 22 of them succumbed (Adams and Walls, 2020). Such prevailing and overwhelming thoughts in the current pandemic atmosphere often have adverse psychological sequelae and may lead to various somatic symptoms (Joob and Wiwanitkit, 2020).
Moderate to severe psychological symptoms were reported amongst the general population in a recent Chinese study during the COVID-19 outbreak (Wang et al., 2020a, Wang et al., 2020b). This is in sharp contrast to a low prevalence of moderate to severe psychological impact in our study (3.8% compared to 58% reported in the Chinese study). Furthermore, compared to the Chinese study population, our cohort had lower prevalence rates of moderate to severe depression (5.3% versus 16.5%), anxiety (8.7% versus 28.8%) and stress levels (2.2% versus 8.1%). However, despite our lower prevalence rates of emotional distress, our study population displayed higher prevalence rates of physical symptoms such as headache (32.3% versus 9.7%) and sore throat (33.6% versus 11.5%) when compared to the Chinese cohort. The true association of physical symptoms and psychological stress is indeed challenging to determine, especially in the current climate where the active infection needs to be urgently excluded in every suspected case before giving much importance to the ‘non-specific’ symptoms. Nevertheless, somatic symptoms may be more prevalent during periods of stress and these are hypothesized to represent a way of communicating emotions (Basant et al., 2014). We hypothesize that the increased prevalence of self-reported physical symptoms is likely to have been contributed by the psychological impact of the outbreak. Another possible contributing factor could be the social stigma associated with mental health issues, which may have resulted in individuals having a higher tendency to express their psychological distress via physical symptoms instead (Yl, 2007).
Headache was the most commonly reported symptom in this study. A recent study on headache associated with personal protective equipment (PPE) among healthcare workers during the COVID-19 pandemic demonstrated that 81% of respondents reported PPE associated headaches, with a pre-existing primary headache diagnosis reported as an independent predictor for PPE associated headaches (Ong et al., 2020). Similarly, migraine was the most commonly reported comorbidity in our study. Hence, the common presenting complaint of headache may be related to the increased adverse psychological impact or an exacerbation of their pre-existing condition. Notably in prior studies, fatigue was the most commonly reported symptom among SARS survivors in both healthcare workers and the general public.(Lam et al., 2009) Interestingly, even in our study, lethargy was one of the most commonly reported symptom amongst healthcare workers. In a previous study from Hong Kong, Lam et al demonstrated that the prevalence of chronic fatigue was significantly higher among SARS survivors which persisted through the acute phase of infection till one month after the disease outbreak (Lam et al., 2009). Interestingly, healthcare workers infected by SARS were more likely to give up their employment, and the occupational risks faced by the healthcare workers during an epidemic may potentially lead to psychiatric morbidity, physical symptoms such as fatigue, and eventually burnout. Although fatigue and headache may be vague and often unsubstantiated, it is crucial not to neglect such physical symptoms as they may be a reflection of underlying psychological distress (Lam et al., 2009).
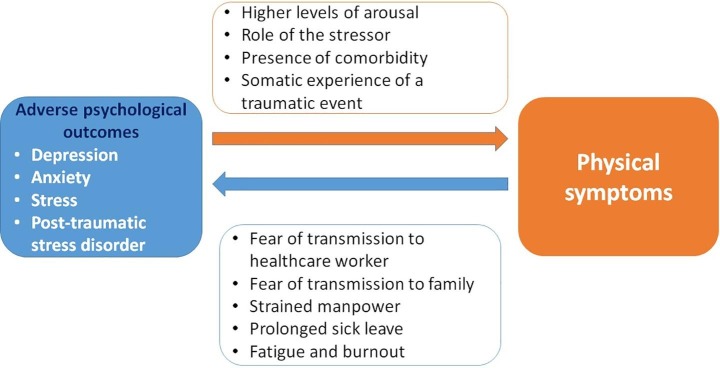
The association of psychological distress and physical symptoms is poorly understood. In addition to the fear of transmitting the infection to colleagues and family members coupled with the dilemma of applying for sick leave in an already strained healthcare sector, many healthcare workers develop burnout and may experience a sense of intense fear, stigmatization and ostracism when displaying physical symptoms suggestive of the virus infection, which often leads to negative psychological pain (Nezlek et al., 2012, Troyer et al., 2020). This phenomenon has already been described in the studies during the current COVID-19 outbreak (Wang et al., 2020a) as well as previous Ebola crisis (Matua and Van Der, 2015). We postulate a bi-directional complex relationship between psychological distress and physical symptoms, where an inadvertent psychological distress exacerbates physical symptoms and vice versa (Fig. 3 ). Accordingly, the physical symptoms related to high levels of arousal in a stressful environment of a disease outbreak may lead to over-reporting of cardiovascular, respiratory, neurological or gastrointestinal symptoms (McFarlane et al., 1994). Furthermore, a known stressor may precipitate or worsen specific physical symptoms. For example, a previous study has reported increased prevalence of respiratory symptoms seen in fire-fighters suffering from PTSD as a result of the psychological stress of smoke inhalation (McFarlane et al., 1994). We believe that various symptoms of throat pain, cough and myalgia during the current COVID-19 outbreak may be over-represented as a result of the psychological stress, and further exacerbated by the presence of various comorbidities (McFarlane et al., 1994). This observation is also commonly evident in patients with depression, with the somatization of back pain and headache (von Knorring et al., 1983). This is in line with our finding of the significant association of the presence of comorbidities and physical symptoms amongst healthcare workers.
Fig. 3.
Proposed bi-directional association between adverse psychological outcomes and physical symptoms amongst healthcare workers in the COVID-19 outbreak.
Targeted multidisciplinary interventions are needed to support healthcare workers by addressing both the psychological manifestations and physical symptoms. All efforts should be made to offer psychological support and interventions once an acute infection has been excluded. Dedicated counselling may be arranged to allay their fear of transmitting the infection to their family members (Wang et al., 2020a) as well as to boost the confidence and morale of our healthcare workers.
5. Limitations
Given that this is a multinational, multicentre study, with similar prevalence of psychological outcomes in both countries, the observed psychological and physical symptoms findings are more likely generalizable. However, our study has its limitations. Firstly, the cross-sectional nature of the study does not allow interpretation for causality. Whilst we found a strong association between presence of physical symptoms and prevalence of psychological distress, we are unable to conclude that psychological distress had resulted in the manifestation of these physical symptoms. Secondly, we did not assess if study participants had taken medical leave of absence, or if they sought the testing for COVID-19 during the manifestation of physical symptoms. Thirdly, owing to the stringent hospital infection control protocols to minimize contact between healthcare workers, the questionnaire had to be self-administered and information provided on symptoms was not verified by a medical professional. Fourthly, we did not record socioeconomic status and education level, which could have influenced our results. We intend to re-evaluate our study participants if the current COVID-19 outbreak escalates further in the region, as well as after it subsides to obtain much reliable explanations about the association of psychological sequelae and various physical symptoms.
6. Conclusion
This study describes an expansive range of physical symptoms experience by healthcare workers during the ongoing COVID-19 outbreak. There is a significant association between the prevalence of physical symptoms and psychological distress, which is probably bi-directional. We recommend the provision for timely psychological support and interventions for healthcare workers who present with physical symptoms once an infection has been excluded.
Author contribution
Nicholas W.S. Chew: Data curation, Formal analysis, Methodology, Resources, Writing. Grace K.H. Lee: Data curation, Formal analysis, Methodology, Resources, Writing. Benjamin Y.Q. Tan: Data curation, Formal analysis, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing. Mingxue Jing: Data curation. Yihui Goh: Data curation. Leonard L.L. Yeo: Data curation. Aftab Ahmad: Data curation. Faheem Ahmed Khan: Data curation. Arvind K. Sharma: Data curation. R.N. Komalkumar: Data curation. P.V. Meenakshi: Data curation. Kenam Shah: Data curation. Bhargesh Patel: Data curation. Bernard P.L. Chan: Data curation. Sibi Sunny: Data curation. Bharatendu Chandra: Data curation. Jonathan J.Y. Ong: Data curation. Prakash R. Paliwal: Data curation. Lily Y.H. Wong: Project administration. Renarebecca Sagayanathan: Project administration. Jin Tao Chen: Project administration. Alison Ying Ying Ng: Project administration. Hock Luen Teoh: Project administration. Georgios Tsivgoulis: Writing. Cyrus S. Ho: Conceptualization, Supervision, Validation, Visualization, Writing. Roger C. Ho: Conceptualization, Supervision, Validation, Visualization, Writing. Vijay K. Sharma: Conceptualization, Formal analysis, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Disclosures
VKS is the current recipient of Senior Clinician Scientist Award from National Medical Research Council, Ministry of Health, Singapore. Other authors have no financial disclosures.
Acknowledgement
No funding reported.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bbi.2020.04.049.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Abelson R. Doctors and Patients Turn to Telemedicine in the Coronavirus Outbreak. 2020. https://www.nytimes.com/2020/03/11/health/telemedicine-coronavirus.html. Published 11 March 2020. Accessed 03 April 2020.
- Adams JG, Walls RM. 2020. Supporting the Health Care Workforce During the COVID-19 Global Epidemic [published online ahead of print, 2020 Mar 12]. JAMA. doi:10.1001/jama.2020.3972. [DOI] [PubMed]
- Basant K., Puri A.H., Ho Roger. 3rd. United States of America: CRC Press, Taylor & Francis Group; 2014. Revision Notes In Psychiatry. [Google Scholar]
- Coronavirus: Hong Kong shoppers snap up rice and noodles as fears over outbreak mount. 2020. https://www.straitstimes.com/asia/east-asia/hong-kong-shoppers-snap-up-rice-and-noodles-as-coronavirus-fears-mount. Published 07 Feb 2020. Accessed 09 March 2020.
- Creamer M., Bell R., Failla S. Psychometric properties of the Impact of Event Scale - Revised. Behav. Res. Ther. 2003;41(12):1489–1496. doi: 10.1016/j.brat.2003.07.010. [DOI] [PubMed] [Google Scholar]
- Farr C. How hospitals hope to keep “worried well” from flooding emergency rooms during coronavirus outbreak. 2020. https://www.cnbc.com/2020/03/13/hospitals-using-digital-tools-to-reduce-coronavirus-crowding.html. Published 13 March 2020. Accessed 03 April 2020.
- Grace S.L., Hershenfield K., Robertson E., Stewart D.E. The occupational and psychosocial impact of SARS on academic physicians in three affected hospitals. Psychosomatics. 2005;46(5):385–391. doi: 10.1176/appi.psy.46.5.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan W-j, Ni Z-y, Hu Y, et al. 2019. Clinical Characteristics of Coronavirus Disease 2019 in China [published online ahead of print, 2020 Feb 28]. New Engl. J. Med. doi:10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed]
- Ho R.C., Zhang M.W., Ho C.S., Pan F., Lu Y., Sharma V.K. Impact of 2013 south Asian haze crisis: study of physical and psychological symptoms and perceived dangerousness of pollution level. BMC Psychiatry. 2014;14:81. doi: 10.1186/1471-244X-14-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 'It's pandemonium': virus panic-buying hits Los Angeles. 2020. https://www.straitstimes.com/world/united-states/its-pandemonium-virus-panic-buying-hits-los-angeles. Published 07 March 2020. Accessed 09 March 2020.
- Joob B, Wiwanitkit V. 2020. Traumatization in medical staff helping with COVID-19 control [published online ahead of print, 2020 Mar 20]. Brain, behavior, and immunity. doi:10.1016/j.bbi.2020.03.020. [DOI] [PMC free article] [PubMed]
- Kang L, Ma S, Chen M, et al. 2019. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study [published online ahead of print, 2020 Mar 30]. Brain Behav. Immun. doi:10.1016/j.bbi.2020.03.028. [DOI] [PMC free article] [PubMed]
- Lam M.H.-B., Wing Y.-K., Yu M.W.-M. Mental Morbidities and Chronic Fatigue in Severe Acute Respiratory Syndrome Survivors: Long-term Follow-up. Archiv. Int. Med. 2009;169(22):2142–2147. doi: 10.1001/archinternmed.2009.384. [DOI] [PubMed] [Google Scholar]
- Lee S., Chan L.Y., Chau A.M., Kwok K.P., Kleinman A. The experience of SARS-related stigma at Amoy Gardens. Soc. Sci. Med. 2005;61(9):2038–2046. doi: 10.1016/j.socscimed.2005.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leow M.K., Kwek D.S., Ng A.W., Ong K.C., Kaw G.J., Lee L.S. Hypocortisolism in survivors of severe acute respiratory syndrome (SARS) Clin. Endocrinol. (Oxf). 2005;63(2):197–202. doi: 10.1111/j.1365-2265.2005.02325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z, Ge J, Yang M, 2020. et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control [published online ahead of print, 2020 Mar 10]. Brain Behav. Immun. doi:10.1016/j.bbi.2020.03.007. [DOI] [PMC free article] [PubMed]
- LP LS. 1995. Manual for the Depression Anxiety Stress Scales. 2nd ed ed: Sydney (AU): Psychology Foundation of Australia.
- Marco L., Christian A.B., Bernd L. Ebola and Psychological Stress of Health Care Professionals. Emerg. Infect. Diseas. J. 2015;21(5):913. doi: 10.3201/eid2105.141988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matua G.A., Van Der Wal DM. Living under the constant threat of ebola: A phenomenological study of survivors and family caregivers during an ebola outbreak. J. Nurs. Res. 2015;23(13):217–224. doi: 10.1097/jnr.0000000000000116. [DOI] [PubMed] [Google Scholar]
- Matua G.A., Wal D.M. Living under the constant threat of Ebola: a phenomenological study of survivors and family caregivers during an ebola outbreak. J. Nurs. Res. 2015;23(3):217–224. doi: 10.1097/jnr.0000000000000116. [DOI] [PubMed] [Google Scholar]
- McAlonan G.M., Lee A.M., Cheung V. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J. Psychiat. 2007;52(4):241–247. doi: 10.1177/070674370705200406. [DOI] [PubMed] [Google Scholar]
- McFarlane A.C., Atchison M., Rafalowicz E., Papay P. Physical symptoms in post-traumatic stress disorder. J. Psychosom. Res. 1994;38(7):715–726. doi: 10.1016/0022-3999(94)90024-8. [DOI] [PubMed] [Google Scholar]
- Ministry of Health S. 2004. Communicable Diseases Surveillance in Singapore. In. Singapore: Ministry of Health, Singapore.
- Ministry of Health Singapore. Updates on COVID-19 (Coronavirus disease 2019) local situation. https://www.moh.gov.sg/covid-19. Published 17 Apr 2020. Accessed 17 Apr 2020.
- Nezlek J.B., Wesselmann E.D., Wheeler L., Williams K.D. Ostracism in everyday life. Group Dynamics: Theory, Research & Practice. 2012;16(2):91–104. [Google Scholar]
- Ong, J.J., Bharatendu, C., Goh, Y., et al. 2020. Headaches associated with personal protective equipment – A cross‐sectional study among frontline healthcare workers during COVID‐19 [published online ahead of print, 2020 Mar 30]. Headache. doi:10.1111/head.13811. [DOI] [PubMed]
- Organization WH. 2020. WHO characterizes COVID-19 as a pandemic. World Heatlh Organization https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen. Published 2020. Accessed 13 March 2020.
- S K. Singapore raises cornavirus outbreak alert to orange: What does it mean?. 2020. https://www.straitstimes.com/singapore/health/coronavirus-new-measures-to-kick-in-as-singapore-moves-to-code-orange. Published 07 Feb 2020. Accessed 16 March 2020.
- SK CA-L. Coronavirus: Singapore ups outbreak alert to orange as more cases surface with no known links; more measures in force. 2020. https://www.straitstimes.com/singapore/coronavirus-outbreak-alert-upped-to-orange-as-more-cases-surface-with-no-known-links-more. Published 07 Feb 2020. Accessed 09 March 2020.
- T A. Coronavirus: Politicians, supermarkets urge calm amid panic-buying of groceries. 2020. https://www.straitstimes.com/singapore/health/coronavirus-fairprice-chief-urges-calm-amid-panic-buying-of-groceries-singapores. Published 07 Feb 2020. Accessed 09 March 2020.
- Tam C.W., Pang E.P., Lam L.C., Chiu H.F. Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: stress and psychological impact among frontline healthcare workers. Psychol. Med. 2004;34(7):1197–1204. doi: 10.1017/s0033291704002247. [DOI] [PubMed] [Google Scholar]
- Tay BYQ, Chew NWS, Lee GKH et al. 2020. Psychological impact of the COVID-19 pandemic on health care workers in Singapore [published online ahead of print, 2020 Apr 6]. Ann. Intern. Med. doi: 10.7326/M20-1083. [DOI] [PMC free article] [PubMed]
- The Times of India. Coronavirus. https://timesofindia.indiatimes.com/coronavirus. Published 17 Apr 2020. Accessed 17 Apr 2020.
- The Times of India. Govt fresh guidelines for lockdown 2.0. https://timesofindia.indiatimes.com/india/govt-fresh-guidelines-for-lockdown-2-0-whats-shut-whats-open-from-april-20/articleshow/75152832.cms. Published 15 Apr 2020. Accessed 15 Apr 2020.
- Troyer EA, Kohn JN, Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms [published online ahead of print, 2020 Apr 13]. Brain Behav. Immun. doi:10.1016/j.bbi.2020.04.027. [DOI] [PMC free article] [PubMed]
- Tucker ME. Psychiatric Disorders Seen in SARS Patients. In. Clinical Psychiatry News. Vol 322004.
- von Knorring L., Perris C., Eisemann M., Eriksson U., Perris H. Pain as a symptom in depressive disorders. II. Relationship to personality traits as assessed by means of KSP. Pain. 1983;17(4):377–384. doi: 10.1016/0304-3959(83)90169-0. [DOI] [PubMed] [Google Scholar]
- Wang C, Pan R, Wan X, et al. 2020 A longitudinal study on the mental health of general population during the COVID-19 epidemic in China [published online ahead of print, 2020 Apr 13]. Brain, behavior, and immunity. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed]
- Wang C., Pan R., Wan X. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss DS. The Impact of Event Scale: Revised. In: Cross-cultural assessment of psychological trauma and PTSD. New York, NY, US: Springer Science + Business Media; 2007:219-238.
- Xiang Y.-T., Yang Y., Li W. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiat. 2020;7(3):228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yl H. Application of mental illness stigma theory to Chinese societies: synthesis and new directions. Singapore Med. J. 2007;48(11):977. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.