Highlights
Sudanese camel herd destination Egypt, a trip of over a month under the scorching sun of the desert using the same route, the same rest stops and drinking from the same wells that has been used for centuries.

-
•
H2S production extended the arsenal of factors implicated in M. arginini pathogenicity
-
•
Absence of the virulence genes vsp, uvrC and gapA
-
•
100% resistant to ciprofloxacin in the absence of the quinolone resistance genes parC and gyrA
Keywords: Camel, Mycoplasma arginini, Antibiotic resistance, Hydrogen sulphide production, Biofilm formation, Virulence genes, quinolones resistance genes, phylogenetic tree
Abstract
In the scientific literature, a small amount of information is found concerning mycoplasmosis in camel species. A variety of pathogens could be causative agents for pneumonia, but walking pneumonia is mostly caused by Mycoplasma with slow development and mild symptoms. The aim of this study was to identify mycoplasmas from camels (Camelus dromedarius) and extending the arsenal of factors implicated in pathogenicity of M. arginini to shed light on the current knowledge gap. 460 lung samples (pneumonic; n=210 and apparently healthy; n=250) were randomly collected from the one-humped camels (C. domedarius) that have been imported from Sudan and slaughtered at Cairo Slaughterhouse. 48 out of 210 isolates (22.9%) recovered from the pneumonic lungs were recorded as M. arginini. Positive PCR results were obtained for all 48 isolates. On the other hand, infection with the organism was not detected in the apparently healthy lungs. Hemolysis and hydrogen sulphide (H2S) production, a compound that has previously not been identified as a virulence factor in M. arginini, was evident in 100% of the isolates. The 48 M. arginini isolates were weak in their ability to form biofilm on polystyrene surfaces. All isolates were 100% susceptible to florfenicol and streptomycin and 100% resistant to ciprofloxacin. Resistance to lincomycin, spiromycin, tylosin, doxacyclin and erythromycin was observed at different frequencies. 13 different combinations of antibiotics representing one to four classes were evident with the Macrolide erythromycin being the most represented. It also should be noted that the ciprofloxacin, doxacyclin, lincomycin, erythromycin combination was the most noted in 21/48 isolates. Surprisingly, none of the virulence genes (vsp, uvrC and gapA) and quinolone resistance genes (parC and gyrA) were detected by PCR.
1. Introduction
The one-humped camel, dromedary (Camelus dromedarius), has a historical presence in civilization, though they were not used until more recent times. The camel was used primarily as means of transportation in the desert, though they are now also used for wool, milk, and farming. To date, the camels are widespread and are located anywhere from Egypt to Chad, Sudan, Ethopia, Eritria, Somalia and Libya (Roess et al., 2015; Napp et al., 2018).
Interestingly, dromedary camels are associated with various infectious diseases. One major disease is Middle East Respiratory Syndrome, which is a camel-to-human spread coronavirus that can originate in camel abattoirs, camel meat markets, camel farms and contribute to the virus spread (Roess et al., 2015; Napp et al., 2018). Unfortunately, there are other infectious diseases that are less well-understood, but also associated with camels. One such infection could be Mycoplasma species.
While most Mycoplasma species are host specific, there are reports of the presence of Mycoplasma in hosts that are not perceived as their normal habitat. In fact, since its first description in 1968 (Barile et al., 1968), M. arginini has been recovered from tissues and secretions of various mammals (Barile et al., 1968; Leach, 1970; Tan and Miles, 1974; al-Aubaidi et al., 1972; Hill, 1975; St George and Carmichael, 1975; Tan et al., 1977b; Goltz et al., 1986; Brogden et al., 1988; Hassan et al., 1997; Elfaki et al., 2002; Thomas et al., 2002; Navidmehr et al., 2009; Gonçalves et al., 2010; Navidmehr et al., 2011; Mederos-Iriarte et al., 2014; Alaa et al., 2018; Göçmen et al., 2020). Moreover, Silló et al. (2012) and Watanabe et al. (2012) wrote two separate reports that provided supportive evidence of a fatal cases of human infection with M. arginini. Each affected patient had an apparent history or possibility of exposure to a wild animal or animal products, thereby suggesting a zoonotic transmission of M. arginini to humans. That said, only three cases of M. arginini isolation occurred, though all people affected by the disease were exposed to various animals in different settings (e.g. slaughterhouse, lion attack, etc.) (Yechouron et al., 1992; Prayson et al., 2008; Silló et al., 2012).
Therefore, the aim of the study was to evaluate M. arginini isolated from the dromedary camel, which could act as a host of the disease and possibly contribute to disease perpetuation. This was accomplished by analyzing the hydrogen sulfide production by M. arginini as a potential virulence factor in addition to the hemolysis activity as well as its ability to produce biofilm and identification of two genes responsible for quinolone resistance (QRDR). This study also investigated the phylogenetic tree of the 16SRNA sequences in the M. arginini camel isolates.
2. Materials and Methods
2.1. Sample collection
There were 460 samples randomly recovered from pneumonic (n=210) and apparently healthy (n=250) lungs of imported one-humped camels between February to April 2018 from Sudan. The animals were submitted for routine slaughter. For the purposes of this study ‘pneumonic lungs’ was referred to those lungs that had gross lesions such as consolidation, fibrin deposition on the pleura, pleurisy, and/or adhesion; alternatively, ‘apparently healthy lungs’ was used to describe lungs without any gross lesions. Specimens were obtained aseptically using a sterile scalpel while taking precautions to prevent surface contamination. Following collection, the samples were transported to the microbiology laboratory in special ice-filled containers within 2 hours of sampling. Pieces of tissue from the border area between disease lesions and healthy lung were suspended by pounding in a mortar with sand and liquid growth medium. The suspension was inoculated into broth growth media with added Mycoplasma Supplement G. Dilutions of up to 10−5 of the liquid medium was prepared. The inoculated medium was incubated 7–10 days at 37°C in an incubator with 5 % CO2. The growth medium was checked daily for growth. A loopful of the broth cultures showing Mycoplasma growth or color change were inoculated onto Mycoplasma Agar Base media in a 95 % N2 and 5 % CO2 humidified atmosphere at 37°C; the petri dishes were examined in stereomicroscopy at the end of incubation. Colonies suspect for Mycoplasma were identified by routine methods.
Digitonin sensitivity test was carried out to differentiate between Mycoplasma and Acholeplasma genera using filter paper discs impregnated with 0.2 mL of 1.5% (W/V) ethanol solution of digitonin and dried overnight. Mycoplasma spp. show digitonin sensitivity while Acholeplasma spp. are resistant (Freundt et al., 1973). Biochemical identification was used for further testing of Mycoplasma sp. Glucose fermentation, arginine deamination and urea hydrolysis tests were also performed (Erno and Stipkovits, 1973; Howard et al., 1994). Serological confirmation of Mycoplasma spp. was conducted per methods of Clyde (1964), while the species-specific identification was performed with anti-M. bovis hyperimmune serum (Lauerman et al., 1994) by the growth inhibition test utilizing dried antiserum impregnated paper discs. Final identification of the isolates was achieved by PCR.
2.2. Phenotypic virulence traits
There were four assays used to demonstrate the phenotypic virulence potentiality of the 48 M. arginini isolates. This was conducted using the following: 1) the catalase enzyme activity was performed according to the procedure of Pritchard et al. (2014); 2) the hemolytic and hemoxidative activity of M. arginini was determined by the method adopted by Großhennig et al. (2016) using washed 2% sheep RBCs in PBS with or without supplements in a final volume of 1 ml; 3) the hydrogen sulfide (H2S) produced by the 48 M. arginini isolates was determined using lead acetate detection strips (Großhennig et al., 2016); and 4) biofilms grown on glass coverslips and in microtitre plates were quantified by measuring the absorbance (560 nm) of 100 ml of the solubilized crystal violet in a microtitre plate (McAuliffe et al., 2006).
2.3. Phenotypic susceptibility test
The 48 M. arginini isolates were tested for susceptibility to eight antimicrobial agents, which represented six classes; this was accomplished by the disc diffusion method pursuant to procedures described by Clinical and Laboratory Standards Institute (CLSI, 2012). The MARindexwas calculated by the equation a/(b x c), where ‘a’ was the aggregate antibiotic resistance score of all the isolates from the sample, ‘b’ was the number of antibiotics used (n=8 via this study) and ‘c’ was the number of isolates that originated from the sample (Krumpeman, 1983). The criteria was followed for standardized international terminology for defining multidrug-resistant (MDR), extensively drug-resistant (XDR) and pandrug-resistant (PDR), which was initially created through a joint initiative by the European Centre for Disease Prevention and Control and the Centers for Disease Control and Prevention (Magiorakos et al., 2012).
2.4. Molecular Identification
2.4.1. DNA extraction
The bacterial lysates used as templates for the PCR were prepared. This was accomplished by gathering a loopful of bacteria from a fresh overnight culture on a tryptic soy agar plate, which was re-suspended homogeneously in 200 µl of sterile water. Then, the mixture was boiled at 100°C for five minutes to release the DNA and centrifuged. The supernatant was used as a template for PCR mixture. Isolates that only reacted with M.arginini antisera were selected.
2.4.2. 16S rRNA identification
Positive isolates were further confirmed for mycoplasmas by PCR amplification of the 16S rRNA gene using Mycoplasma specific primers (Table 1 ). PCR reaction was performed in a 50 μl volume for each isolate, consisting of 5 µl of 50 ng of Mycoplasma DNA, 10 µl of 10 x Taq buffer (10 mM tris- HCl [pH 8.8], 50 mM KCl), 1 µl of 50 pM of forward and reverse primers, 1.5 mM MgCl2, 1 µl of 2U of Taq polymerase, 1 µl of 50 uM of each dNTP, and 31µl of DNase- RNase- free, deionized water. The PCR reaction was performed in a thermal cycler (Biometra TRIO, Jena, Germany) with an intial denaturation at 94°C for 5 minutes, followed by 35 cycles of denaturation at 94°C for 1 minute, annealing at 55°C for 1 minute, and extension at 72°C for 1.5 minutes with a final extention at 72°C for 10 minutes.
Table 1.
Oligonucleotide primers used for detection of Mycoplasma spp., M. arginini, virulence genes, and fluoroquinolone resistance (QRDR) genes.
| Species | Sequence | Target | References |
|---|---|---|---|
| 16SrRNA. For Mycoplasma | 5⁄- AGA CTC CTA CGG GAG GCA GCA -3⁄ 5⁄- ACT AGC GAT TCC GAC TTC ATG -3⁄ |
1000bp | Alberto et al. (2006) |
| Mycoplasma group- specific | 5⁄-GGGAGCAAACAGGATAGATACCCT-3/ 5/-TGCACCATCTGTCACTCTGTTAACCTC-3/ |
280bp | VanKuppeved et al. (1994) |
| M. arginini | 5⁄- TGATCATTAGTCGGTGGAGAGTTC-3⁄ 5⁄- TATCTCTAGAGTCCTCGACATGACTC-3⁄ |
326bp | Vahid et al. (2009) |
| Virulence genes | |||
| uvrC | 5′-TTACGCAAGAGAATGCTTCA-3′ 5′-TAGGAAAGCACCCTATTGAT-3 |
1626 bp | Perez-Casal et al. (2007) |
| gapA | 5′-ATAGGAGGATCCAAAAGAGTCGCTATCAATGGTTTTGGACG-3′, 5′-GGAAATGGTACCTTACTTAGTTAGTTTAGCAAAGTATGTTAATG-3′ | 1007 bp | |
| vsp | 5/-CTTGGATCAGTGGCTTCATTAGC-3/ 5/-GTCATCATGCGGAATTCTTGGGT-3/ |
400bp | Alberto et al. (2006) |
| Fluoroquinolone resistance genes | |||
| gyrA | 5′-GACGAATCATCTAGCGAG-3′ 5′-GCCTTCTAGCATCAAAGTAGC-3′ |
531bp | Lysnyansky et al. (2009)__ |
| parC | 5′-GAGCAACAGTTAAACGATTTG-3′ 5′-GGCATAACAACTGGCTCTT-3′. |
488bp |
The same procedure for 16S rRNA PCR reaction as described above was used for Mycoplasma species identification, but with the following PCR modifications: 40 cycles in denaturation at 94°C for 60 seconds, annealing at 55°C for 1 minute and extension at 72°C for 2 minutes.
2.4.3. Mycoplasma arginini typing
Positive M. arginini isolates were further confirmed by PCR reaction. The PCR conditions for this reaction were denaturation 94°C for 45 seconds, primer annealing at 60°C for 1 minute, and extension at 72°C for 2 minutes. The reactions were performed for 30 or 35 cycles with a final extention at 72°C for 3 minutes.
2.4.4. Detection of virulence genes
PCR was performed to detect three virulence genes of M. arginini including the variable surface lipoprotein gene (vsp), cytadhesin (gapA) and the uvrC, which encodes a protein involved in DNA excision and repair.
2.4.4.1. Detection of vsp, uvrC and gapA genes
The detection of vsp, uvrC and gapA genes was performed (Table 1). PCR reactions were performed in a 20 µl volume for each isolate. The PCR condition for detection of the vsp gene was initial denaturation 94°C for 5 minutes, followed by 35 cycles of denaturation at 94°C for1 minute, annealing at 55°C for 1 minute, and extension at 72°C for 1.5 minutes with a final extension at 72°C for 10 minutes. The PCR condition for detection of the uvrC and gapA genes had an initial denaturation at 94°C for 2 minutes, followed by 35 cycles of denaturation at 94°C for 30 seconds, annealing at 56°C for 30 seconds for gapA and at 52C for 30 sec for uvrC, and extension at 72°C for 2min with a final extension 72°C for 5 min.
2.4.5. Detection of quinolones resistance (QRDR) genes
Detection of genes (gyrA and parC) encoding for quinolone resistance (QRDRs) was carried out by PCR. The PCR reactions were performed in 50 μl volume for each isolate, with 30 pmol/μl of each primer and 100 ng DNA. Conditions for the PCR were as follows: 95°C for 3 minutes, 30 cycles of denaturation for 30 seconds at 95°C, followed by annealing of 30 sec at 56°C and extension at 72°C for 45 seconds with a final extension at 72°C at 10 minutes.
2.5. Nucleotide sequencing and sequence analysis
Sequencing of the PCR amplified product was conducted by GATC Company using ABI 3730xl DNA sequencer and forward/reverse primers (Table 1). For M. arginini, the traditional Sanger technology was combined with the novel 454 technology for sequencing 326 bp PCR product of the specific gene. In order to establish sequence identity to GenBank accessions, a BLAST® analysis (Basic Local Alignment Search Tool) was initially performed. Published data of international reference strains from the GenBank were available from the National Center for Biotechnology Information (NCBI) (https://www.ncbi.nlm.nih.gov/nuccore/?term=infectious+bursal+disease+virus). The comparisons of obtained nucleotide 326 sequences and multiple alignments were performed using the BioEdit sequence alignment editor (7.1.5) for multiple sequence alignment.Sequences were then submitted to NCBI GenBank using BankIt [see: http://www.ncbi.nlm.nih.gov/WebSub/?tool=genbank] under the accession numbers:
MK271638 Mycoplasma arginini strain WA 1.Egypt, MK271639 Mycoplasma arginini strain WA 2.Egypt, MK271640 Mycoplasma arginini strain WA 4.Egypt, and MK271641 Mycoplasma arginini strain WA 5.Egypt.
2.6. Mycoplasma arginini specific gene phylogenetic tree
The 16S phylogenetic tree was inferred by the distance-based neighbor-joining (NJ) method using MEGA version 7.
3. Results
3.1. Prevalence of M. arginini in the samples recovered from lungs of camels
A total of 460 lung samples (pneumonic n=210; and apparently healthy n=250) samples were randomly collected from lungs of imported one humped camels that were slaughtered at Cairo Slaughter house. Of these, 48 out of the 210 pneumonic lung samples (22.9%) were recorded to be positive for putative mycoplasmas. All isolates that were identified as mycoplasmas formed typical ‘fried-egg’ and/or centerless granular colonies. They were all digitonin-sensitive, glucose-positive and arginine-negative. A positive PCR result for M. arginini was obtained for all 48 isolates. Alternatively, infection with the organism was not detected in the apparently healthy lungs.
3.2. The catalase enzyme activity of M. arginini
The catalase activity of M. arginini was examined and indicated by the generation of bubbles. There were nine M. arginini (19%) samples that tested catalase positive.
3.3. The hemolytic activity of M. arginini
The effect of M. arginini on RBCs was tested in a liquid environment. In this assay, the erythrocytes formed a loose pellet and the erythrocytes remained intact, though a red to brown color change of the blood cells for α-haemolysis did occur due to modification of hemoglobin. This confirms that all 48 isolates were phenotypically hemolytic.
3.4. Hydrogen sulfide production
To test whether sulfide ions caused hemolysis, RBCs were incubated in the presence of sodium sulfide (0.625% Na2S) and tested for the formation of H2S using lead acetate strips. The white strips changed to black when H2S was added, indicating production of lead sulfide.
3.5. Biofilm formation capability
M. arginini isolates (n=48) were found to be weak in their ability to adhere to polystyrene multiwall plates. A very low spectrophotometric values (A560 (0.0440-0.1)) were detected for these isolates that had poor adhesion and biofilm formation abilities.
3.6. Antimicrobial resistance among the M. arginini isolates
The antimicrobial resistance profiles of M. arginini isolates obtained in this study were tested (Table 2 ). All isolates were 100% susceptible to florfenicol and streptomycin and 100% resistant to ciprofloxacin. Resistance to lincomycin, tylosin, doxacyclin and erythromycin was observed at different frequencies. On the other hand, there were13 different combinations of antibiotics representing one to four classes, with the Macrolide erythromycin being the most obviously seen in 10 out of the 13 combinations (Table 3 ). It also should be noted that the Ciprofloxacin, Doxacyclin, Lincomycin, Erythromycin combination was the most noted in 21/48 isolates; moreover, the multidrug-resistant (MDR), and extensively drug-resistant (XDR) isolates were obvious in 31/48 (64.59%) and 8/48 (16.67%) isolates respectively.
Table 2.
Investigation of phenotypic antibacterial resistance, phenotypic virulence traits, virulence and Fluoroquinolone Resistance genes in M. arginini species isolated from camel pneumonic lungs.
| Antibiotics | Phenotypic Virulence Traits | Virulence genes | Fluoroquinolone Resistance genes | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ciprofloxacin (5 ug) | Doxacyclin (30 ug) | Lincomycin (2 ug) | Florafenicol (30 ug) | Spiromycin (100 ug) | Tylosin (30 ug) | Erythromycin (15 ug) | Streptomycin (10ug) | MARindex | Hemolysis | Catalase | H2S | Biofilm | vsp | parC | uvrC | gyrA | gapA | ||
| R | R | R | S | S | S | R | S | MDR | 0.5 | + | - | + | 0.051 | - | - | - | - | - | |
| R | R | R | S | S | S | R | S | MDR | 0.5 | + | - | + | 0.050 | - | - | - | - | - | |
| R | R | R | S | S | S | R | S | MDR | 0.5 | + | - | + | 0.048 | - | - | - | - | - | |
| R | S | I | S | I | I | R | S | MDR | 0.625 | + | + | + | 0.049 | - | - | - | - | - | |
| R | R | S | S | S | S | R | S | XDR | 0.375 | + | - | + | 0.050 | - | - | - | - | - | |
| R | R | R | S | S | S | R | S | MDR | 0.5 | + | - | + | 0.051 | - | - | - | - | - | |
| R | S | R | S | I | I | R | S | MDR | 0.625 | + | - | + | 0.064 | - | - | - | - | - | |
| R | R | R | S | S | S | R | S | MDR | 0.5 | + | + | + | 0.069 | - | - | - | - | - | |
| R | R | S | S | S | S | R | S | XDR | 0.375 | + | - | + | 0.063 | - | - | - | - | - | |
| R | S | S | S | S | S | R | S | XDR | 0.25 | + | + | + | 0.066 | - | - | - | - | - | |
| I | R | R | S | I | I | R | S | MDR | 0.75 | + | - | + | 0.078 | - | - | - | - | - | |
| R | R | R | S | S | S | S | S | XDR | 0.375 | + | - | + | 0.095 | - | - | - | - | - | |
| R | S | S | S | S | S | S | S | - | 0.125 | + | - | + | 0.046 | - | - | - | - | - | |
| R | R | R | S | S | S | R | S | MDR | 0.5 | + | - | + | 0.060 | - | - | - | - | - | |
| R | S | S | S | S | S | S | S | - | 0.125 | + | - | + | 0.047 | - | - | - | - | - | |
| R | R | R | S | S | S | R | S | MDR | 0.5 | + | + | + | 0.050 | - | - | - | - | - | |
| R | R | R | S | S | S | R | S | MDR | 0.5 | + | - | + | 0.083 | - | - | - | - | - | |
| R | R | R | S | S | S | R | S | MDR | 0.5 | + | - | + | 0.069 | - | - | - | - | - | |
| R | S | S | S | S | S | S | S | - | 0.125 | + | - | + | 0.061 | - | - | - | - | - | |
| I | S | S | S | I | I | R | S | XDR | 0.5 | + | - | + | 0.049 | - | - | - | - | - | |
| R | R | I | S | I | S | R | S | MDR | 0.625 | + | + | + | 0.097 | - | - | - | - | - | |
| R | R | R | S | S | S | R | S | MDR | 0.5 | + | - | + | 0.081 | - | - | - | - | - | |
| R | S | S | S | S | S | S | S | - | 0.125 | + | + | + | 0.066 | - | - | - | - | - | |
| R | R | R | S | S | S | R | S | MDR | 0.5 | + | - | + | 0.079 | - | - | - | - | - | |
| R | R | R | S | S | S | R | S | MDR | 0.5 | + | - | + | 0.058 | - | - | - | - | - | |
| R | S | S | S | S | S | S | S | - | 0.125 | + | - | + | 0.066 | - | - | - | - | - | |
| R | R | R | S | S | S | R | S | MDR | 0.5 | + | - | + | 0.057 | - | - | - | - | - | |
| S | S | S | S | S | S | S | S | - | 0 | + | - | + | 0.060 | - | - | - | - | - | |
| R | R | R | S | S | S | R | S | MDR | 0.5 | + | - | + | 0.053 | - | - | - | - | - | |
| R | S | S | S | S | S | S | S | - | 0.125 | + | + | + | 0.068 | - | - | - | - | - | |
| R | R | R | S | S | S | R | S | MDR | 0.5 | + | - | + | 0.059 | - | - | - | - | - | |
| I | S | S | S | I | I | S | S | XDR | 0.375 | + | + | + | 0.067 | - | - | - | - | - | |
| R | R | R | S | S | S | R | S | MDR | 0.5 | + | - | + | 0.055 | - | - | - | - | - | |
| R | R | R | S | S | S | R | S | MDR | 0.5 | + | - | + | 0.060 | - | - | - | - | - | |
| R | S | S | S | S | S | S | S | - | 0.125 | + | - | + | 0.095 | - | - | - | - | - | |
| R | R | R | S | S | S | R | S | MDR | 0.5 | + | - | + | 0.100 | - | - | - | - | - | |
| I | S | I | S | I | S | R | S | MDR | 0.5 | + | - | + | 0.046 | - | - | - | - | - | |
| R | R | R | S | S | S | R | S | MDR | 0.5 | + | + | + | 0.073 | - | - | - | - | - | |
| R | S | R | S | S | S | R | S | MDR | 0.375 | + | - | + | 0.057 | - | - | - | - | - | |
| R | R | S | S | S | S | R | S | XDR | 0.375 | + | - | + | 0.051 | - | - | - | - | - | |
| S | R | R | S | S | I | R | S | MDR | 0.5 | + | - | + | 0.044 | - | - | - | - | - | |
| R | R | R | S | S | I | R | S | MDR | 0.625 | + | - | + | 0.055 | - | - | - | - | - | |
| R | S | S | S | S | S | S | S | - | 0.125 | + | - | + | 0.065 | - | - | - | - | - | |
| R | R | R | S | S | S | R | S | MDR | 0.5 | + | - | + | 0.057 | - | - | - | - | - | |
| I | R | S | S | S | S | R | S | XDR | 0.375 | + | - | + | 0.071 | - | - | - | - | - | |
| R | S | R | S | I | S | R | S | MDR | 0.5 | + | - | + | 0.062 | - | - | - | - | - | |
| R | R | I | S | I | S | R | S | MDR | 0.625 | + | - | + | 0.055 | - | - | - | - | - | |
| S | R | R | S | S | I | R | S | MDR | 0.5 | + | - | + | 0.045 | - | - | - | - | - | |
R, resistant; I, intermediate; S, susceptible
MDR, non-susceptibility to at least one agent in three or more antimicrobial categories; XDR non-susceptibility to at least one agent in all but two or fewer antimicrobial categories (non-susceptible to ≥1 agent in all but ≤2 categories).
Table 3.
The antimicrobial resistance combinations of Mycoplasma arginini to various antibiotics.
| Antibiotics | n= resistant antibiotics | n= antibiotic classes | n= of isolates |
|---|---|---|---|
| Ciprofloxacin | 1 | 1 | 8 |
| Ciprofloxacin, Erythromycin | 2 | 2 | 1 |
| Ciprofloxacin, Doxacyclin, Erythromycin | 3 | 3 | 4 |
| Ciprofloxacin, Doxacyclin, Lincomycin | 3 | 3 | 1 |
| Ciprofloxacin, Spiromycin, Tylosin | 3 | 2 | 1 |
| Ciprofloxacin, Lincomycin, Erythromycin | 3 | 3 | 1 |
| Ciprofloxacin, Doxacyclin, Lincomycin, Erythromycin | 4 | 4 | 21 |
| Ciprofloxacin, Spiromycin, Tylosin, Erythromycin | 4 | 2 | 1 |
| Ciprofloxacin, Lincomycin, Spiromycin, Erythromycin | 4 | 3 | 1 |
| Doxacyclin, Lincomycin, Tylosin, Erythromycin | 4 | 3 | 2 |
| Ciprofloxacin, Lincomycin, Spiromycin, Tylosin, Erythromycin | 5 | 3 | 2 |
| Ciprofloxacin, Doxacyclin, Lincomycin, Tylosin, Erythromycin | 5 | 3 | 1 |
| Ciprofloxacin, Doxacyclin, Lincomycin, Spiromycin, Tylosin, Erythromycin | 6 | 3 | 1 |
3.7. Distribution of the virulence and QRDR genes in the M. arginini isolates
Interestedly and unexpectable, the vsp, uvrC, parC virulence genes and the gyrA and gapA QRDR genes were not detected by PCR in the 48 M. arginini isolates (Table 1).
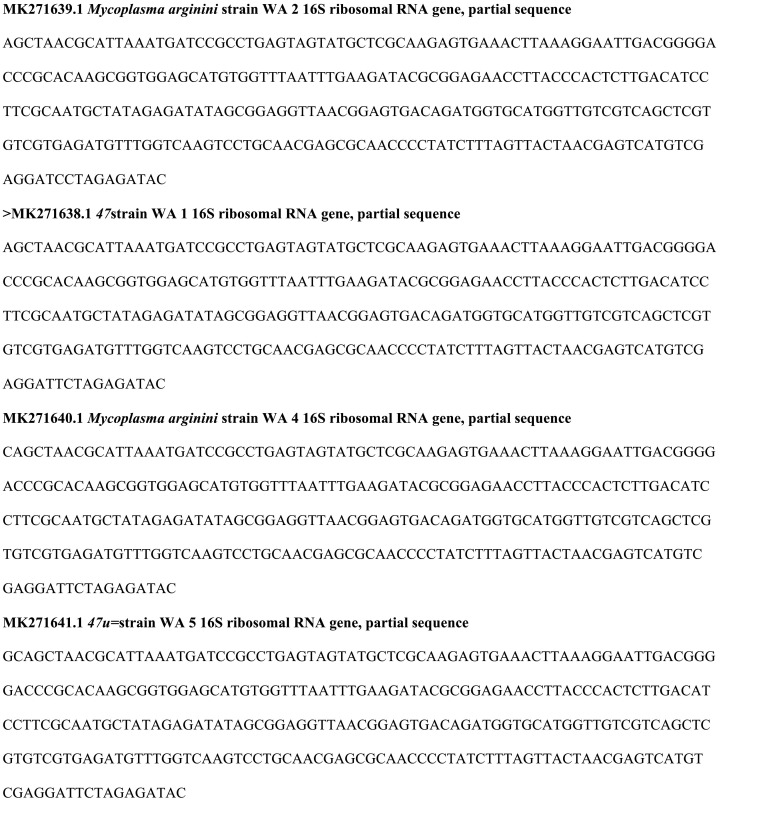
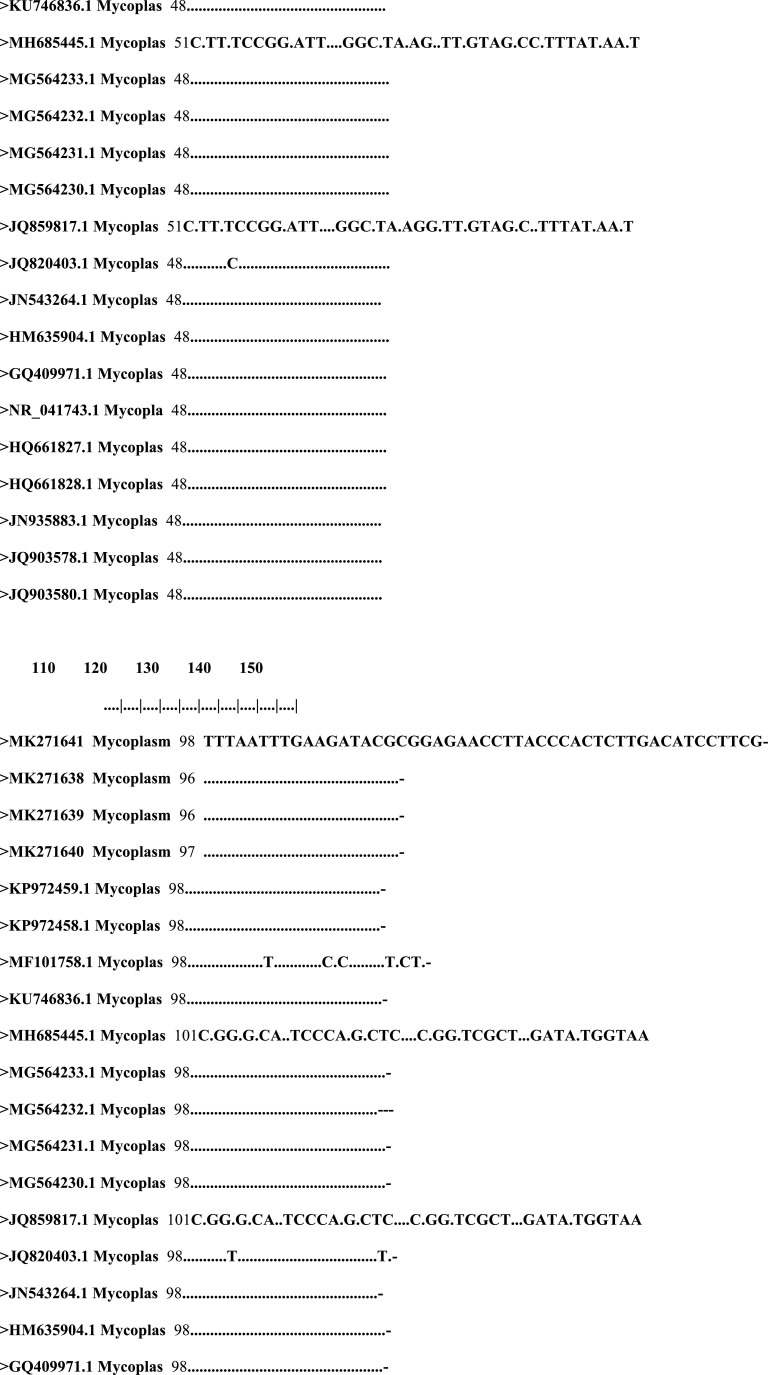
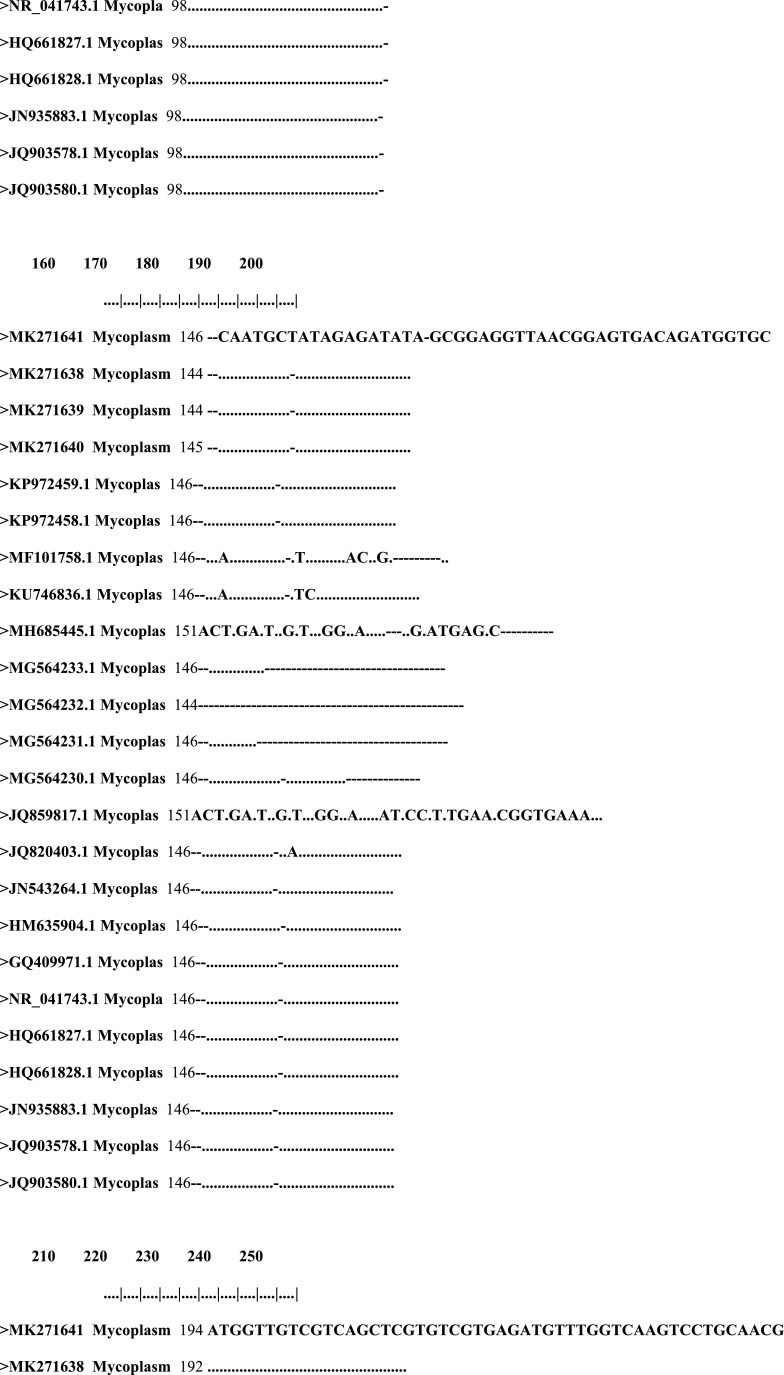
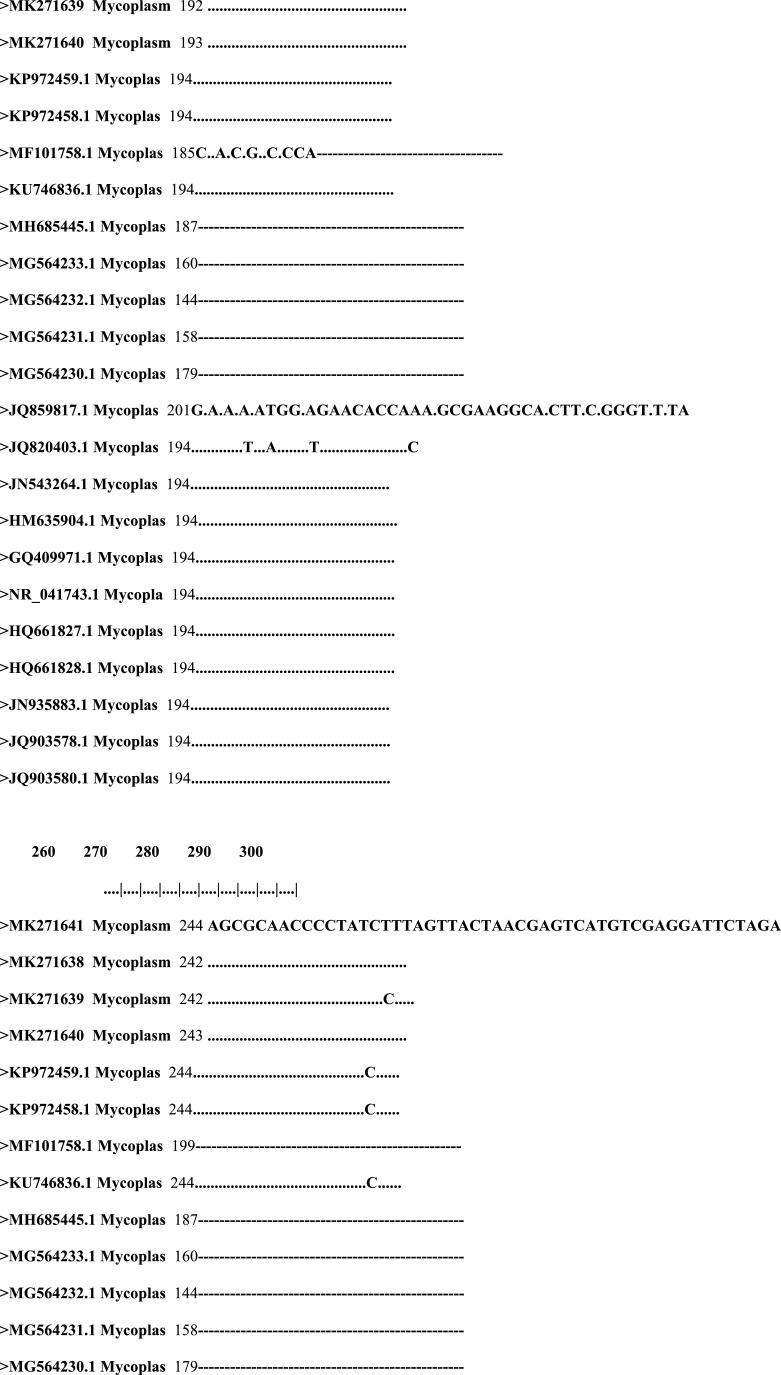
3.8. Sequence analysis of M. arginini specific gene
From the sequence of M. arginini specific gene (Figs. 1 & 2 ), this study isolated MK271639.1, MK271638.1, MK271640.1 and MK271641.1. These had high nucleotide identity of 100%, with 99% occurring in other Egyptian isolates including: JN543264.1 and HM635904.1, European isolates GQ409971.1 (England), NR_041743.1 (Sweden), African isolatesHQ661827.1, HQ661828 (South Africa), and American isolates JN935883.1, JQ903578.1 and JQ903580.1 (USA). Some had low nucleotide identity at 24%, 31% and 48% with Egyptian isolates MH685445.1, MG564232.1 and JQ859817.1, respectively (Figs. 3 & 4 ).
Fig. 1.
DNA sequence of M. arginini isolates.
Fig. 2.
Alignment of nucleotides of 16s rRNA gene of M. arginini.
Fig. 3.
Identity % of 16s rRNA gene of M. arginini isolates.
Fig. 4.
Phylogenetic tree of 16s rRNA gene of M. arginini isolates.
4. Discussion
Pneumonia can be caused by bacteria, virus or fungi; that said, walking pneumonia is mostly caused by the bacteria Mycoplasma, which slowly progresses with mild symptoms that can evolve into more severe symptoms (Stamm and Stankewicz, 2020). In humans, walking pneumonia usually is caused more specifically by M. pneumoniae (CDC, 2018). Other forms of bacteria can cause pneumonia, though, and should not be dismissed as irrelevant. For example, M. arginini can modulate inflammatory response and energy metabolism on the transcription level in B-lymphoid cells with HTT mutation (Krzysztoń-Russjan et al., 2016). Additionally, M. arginini is particularly incriminated to be involved in oncogenesis and infections in different human cell lines (e.g. fibroblast, embryonic kidney, breast cancer, colorectal carcinoma) and mouse fibroblasts (Zellaa et al., 2018).
Mycoplasmas are commensal bacteria found widely in association with mucous membranes of all mammalian species (Sykes, 2014) and can be isolated from normal human and animal respiratory mucosa (Thomas and Smith, 1972; Koshimizu and Ogata, 1974; Aroch et al., 2008; Gabinaitiene et al., 2011; Zhou and Li, 2014; Ericsson et al., 2016; Peek and Divers, 2017; Jambhekar et al., 2019; Maboni et al., 2019; Mead et al., 2019; Thomas et al., 2019). Several non-M. bovis species are of interest in cattle with varying degrees of clinical significance of which M. arginini comes to our interest (Parker et al., 2018). There is debate on whether these are truly new emerging pathogens or pre-existing pathogens that are now easier to detect due to the advent of sophisticated molecular diagnostic tools and more frequent diagnostic testing. For decades, the role of other bacterial agents such as M. arginini has been questioned (Yechouron et al., 1992; Watanabe et al., 2012). It is unknown whether certain Mycoplasma species such as M. arginini act as a medical hazard. It is of significance to emphasize that, the 48 M. arginini isolates were from the pneumonic lungs and not from the healthy lungs. This was also encountered in other animals reflecting that most mycoplasmas are normal inhabitants of the upper respiratory tract but do not appear in the lungs of healthy animals (Thomas and Smith, 1972; Tan et al., 1977a; Thomas et al., 2002; Aroch et al., 2008; Mohamed et al., 2018).
With the work presented in this study, an arsenal of factors were implicated in the pathogenicity of M. arginini. The overlapping, but distinct effects of H2S, indicated that the bacteria possess a set of virulence determinants that synthesize and allow the bacteria getting efficient access to the host's resources. Großhennig et al. (2016) shared results confirming H2S production and hemolysis were correlated in M. pneumonia. This was the first time that correlation was recorded for M. arginini isolated from camels, where H2S was not previously identified as a virulence factor in lung pathogens in camels. This study also concluded that H2O2 was the responsible agent for the oxidation of heme, but not for lysis of RBCs (Großhennig et al., 2016).
Contrary to the assumptions based on the effects of catalase and catalase inhibitors on erythrocyte hemolysis by M. pneumoniae, Großhennig et al. (2016) also found that a mutant of M. pneumoniae, which was unable to produce H2O2, could still lyse erythrocytes in a blood agar overlay via β-hemolysis. The research conducted in this study concluded that catalase played only a minor role in hemolysis by M. arginini, similar to the property found in M. pneumoniae and that the discoloration of hemoglobin was specifically attributed to cysteine-dependent formation of H2S2 ions. This data was also in accordance to the findings of Großhennig et al. (2016). On the other hand, the induced weak biofilm formation by M. arginini in this study could be attributed as a reflection to the weak production of catalase, which is considered as an enhancement factor for biofilm growth and formation (Simmons et al., 2015).
The MARindexes of the M. arginini isolates were decided based on eight different antibiotics. M. arginini demonstrated MARindex ranging from 0.0 and 0.625. Those isolates with a MARindexes above 0.2 suggested that the bacteria isolates were from a high-risk source, where antibiotics were frequently used. Drug resistance in isolates originating from wildlife, which are not influenced by selective pressures of antimicrobial drugs, are believed to be low (Gufe et al., 2019). The values for all the strains between 0 and 0.625 suggested a diverse origin from a high-risk source of contamination where antibiotics are often used or encountered during transport from native countries (e.g. Sudan, Ethiopia and Chad) to Egypt.
The 16S rRNA gene is one of the most common genes targeted for bacterial identification because of its presence in all bacteria and unchanged function over time (Janda et al., 2007). The specificity of these PCR assays targeting the16S rDNA PCR/DGGE and16S-23S rRNA spacer region appeared to be adequate against most Mycoplasma species and Acholeplasma spp. (Tang et al., 2000; McAuliffe, et al., 2005; Jozefova, et al., 2014). This approach enabled us to identify and differentiate the 48 M. arginini species that were isolated from the pneumonic lungs of the camel. We also followed the steps of Gioia et al. (2016) by sequence analysis,which allowed identification and discrimination of several Mycoplasma and Acholeplasma spp., including M. arginini, M. alkalescens, M. bovigenitalium, M. canadense, M. bovirhinis, M. californicum, A. laidlawii, and Acholeplasma oculi, when the Mycoplasma 16-23S rDNA and Acholeplasma 16-23S rDNA were targeted.
Compared to other bacterial pathogens, the current knowledge of the molecular basis of pathogenicity of mycoplasmas is limited, and disruption at the molecular and cellular level remain to be elucidated. Several studies in the past years have shown that pathogenic mycoplasmas are equipped with sophisticated genetic systems, which allow these agents to spontaneously change their surface antigenic make-up (Jeqchlinger et al., 2004; Chopra-Dewasthaly et al., 2017). It is implicated that these variable surface components provide the wall-less mycoplasmas with a means to avoid the host immune response and promote host colonization (Jeqchlinger et al., 2004). The uvrC gene is well conserved and an enzyme that is essential for replication, as it is involved with DNA repair, making it a highly stable gene (Thomas et al., 2004) and a much more specific target gene than 16S rRNA (Subramaniam et al., 1998). In our investigation this was not the case and the uvrC gene failed to be evident in addition to the other two virulence genes, vsp and gapA. There were 16 genes found to be essential in previous studies on other mycoplasma species that were found to be dispensable (Sharma et al., 2014). Of these, five genes have previously been predicted to be part of the core set of 153 essential genes in mycoplasmas (Sharma et al., 2014).
The absence of these three virulence genes was also reflected to the two gyrA and parC genes encoding for quinolone resistance. A strange and unexpected situation occurred, which raises the question of the dispensability of these genes in M. arginini isolated from camel. Moreover, this study could extend the list of non-essential genes of mycoplasmas that were previously generated by studies in other species (Sharma et al., 2014).
This study also has some limitations with substantial outputs. First, the number of isolates included in the study was relatively small. Second, isolates were selected from imported camels, thereby suggesting a further analysis conducted with domestic camel isolates. Third, the potential of whole genome sequencing (WGS) must be implemented to provide more detailed information than traditional molecular typing methods. This further exploration of genomic diversity among M. arginini isolates can advance the epidemiological information specific to at-risk populations for an important, yet often underestimated, respiratory pathogen. This information can highlight biological risks from a public health perspective as well as identify the emergence of new variants or genetic features that may impact transmission or virulence.
5. Conclusion
The live camel trade is a major industry in Egypt, which is also a source of pathogens dissemination and transmission of infectious diseases. Because of this significant presence and risks associated with it, this study was conducted to detect, isolate, and identify mycoplasmas from camels (C. dromedarius). To date, several non-M. bovis species are of interest in cattle with varying degrees of clinical significance, which was another factor reaffirming the importance of studying pathogens in M. arginini.
This study employed an arsenal of factors implicated in pathogenicity of M. arginini to shed light on current knowledge gaps. By better understanding H2S and investigating other potential virulence factors found in this organism, more can be understood about M. arginini. Ultimately, the goal of this research and future research is to fully understand pathogens in possible hosts; this type of information can lead to novel, more effective treatment, control, and preventive measures and improve vaccine development.
CRediT authorship contribution statement
Walaa Mohammed Abdelazeem: Data curation, Investigation. Tara Rava Zolnikov: Writing - review & editing. Zeinab Roshdy Mohammed: Supervision. Alaa Saad: Data curation, Investigation. Kamelia M Osman: Supervision, Data curation, Writing - original draft, Writing - review & editing.
Declaration of Competing Interest
The authors declare that they have no conflict of interest
References
- al-Aubaidi J.M., Taylor W.D., Bubash G.R., Dardiri A.H. Identification and characterization of Mycoplasma arginini from bighorn sheep (Ovis canadensis) and goats. Am. J. Vet. Res. 1972;33:87–90. [PubMed] [Google Scholar]
- Alberto A., Addis M.F., Chessa B., Cubaddu T., Profiti M., Rosati S., Ruiu A., Pittau M. Molecular and antigenic characterization of a Mycoplasma bovis strain causing an outbreak of infectious kerato-conjunctivitis. J. Vet. Diagn. Invest. 2006;18:41–51. doi: 10.1177/104063870601800106. [DOI] [PubMed] [Google Scholar]
- Aroch I., Ofri R., Sutton G.A. Chapter 18 - Ocular Manifestations of Systemic Diseases. In: Maggs D.J., Miller P.E., Ofri R., editors. Slatter's Fundamentals of Veterinary Ophthalmology. Fourth Edition. Elsevier Inc; 2008. pp. 374–418. Edited by. Edited byCopyright © 2008. [DOI] [Google Scholar]
- Barile M.F., DelGiudice R.A., Carski T.R., Gibbs C.J., Morris J.A. Isolation and characterization of Mycoplasma arginini: spec. nov. Proc. Soc. Exp. Biol. Med. 1968;129:489–494. doi: 10.3181/00379727-129-33351. [DOI] [PubMed] [Google Scholar]
- Brogden K.A., Rose D., Cutlip R.C., Lehmkuhl H.D., Tully J.G. Isolation and identification of mycoplasmas from the nasal cavity of sheep. Am. J. Vet. Res. 1988;49:1669–1672. [PubMed] [Google Scholar]
- CDC, Centers for Disease Control and Prevention2018. National Center for Immunization and Respiratory Diseases, Division of Bacterial Diseases. Mycoplasma pneumoniae Infections. Page last reviewed: April 13, 2018.
- Chopra-Dewasthaly R., Spergser J., Zimmermann M., Citti C., Jechlinger W., Rosengarten R. Vpma phase variation is important for survival and persistence of Mycoplasma agalactiae in the immunocompetent host. PLoSPathog. 2017;13(9) doi: 10.1371/journal.ppat.1006656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CLSI, Clinical and Laboratory Standards Institute, 2012. Performance standards for antimicrobial susceptibility testing; twenty-second informational supplement. M100-S21. Wayne; CLSI.
- Clyde W.A. Mycoplasma species identification based upon growth inhibition by specific antisera. J. Immunol. 1964;92:958–965. [PubMed] [Google Scholar]
- Elfaki M.G., Abbas B., Mahmoud O.M., Kleven S.H. Isolation and characterization of Mycoplasma arginini from camels (Camelus dromedaries) with pneumonia. Comp. Immunol. Microbiol. Infect. Dis. 2002;25:49–57. doi: 10.1016/s0147-9571(01)00021-2. [DOI] [PubMed] [Google Scholar]
- Ericsson A.C., Personett A.R., Grobman M.E., Rindt H., Reinero C.R. Composition and predicted metabolic capacity of upper and lower airway microbiota of healthy dogs in relation to the fecal microbiota. PLoS One. 2016;11 doi: 10.1371/journal.pone.0154646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erno H., Stipkovits L. Bovine Mycoplasma cultural and biochemical studies. Acta. Vet. Scand. 1973;14:450–463. doi: 10.1186/BF03547432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freundt E.A. Principles of Mycoplasma classification. Ann. N.Y. Acad. Sci. 1973;225:713. [Google Scholar]
- Gabinaitiene A., Siugzdaite J., Zilinskas H., Siugzda R., Petkevicius S. Mycoplasma bovis and bacterial pathogens in the bovine respiratory tract. Veterinarni Medicina. 2011;56:29–35. [Google Scholar]
- Gioia G., Werner B., Nydam D.V., Moroni P. Validation of a mycoplasma molecular diagnostic test and distribution of mycoplasma species in bovine milk among New York State dairy farms. J. Dairy Sci. 2016;99:4668–4677. doi: 10.3168/jds.2015-10724. [DOI] [PubMed] [Google Scholar]
- Göçmen H., Alçay S., Rosales R.S., Ridley A. Characterisation of genital Mycoplasma species from preputial swabs of bucks and rams. Kafkas Univ. Vet. Fak. Derg. 2020;26:305–308. [Google Scholar]
- Goltz J.P., Rosendal S., McCraw B.M., Ruhnke H.L. Experimental studies the pathogenicity of Mycoplasma ovipneumoniae and Mycoplasma arginini for the respiratory tract of goats. Can. J. Vet. Res. 1986;50:59–67. [PMC free article] [PubMed] [Google Scholar]
- Gonçalves R, Mariano I., Núñez A., Branco S., Fairfoul G., Nicholas R. Atypical non-progressive pneumonia in goats. Vet. J. 2010;183:219–221. doi: 10.1016/j.tvjl.2008.10.005. [DOI] [PubMed] [Google Scholar]
- Großhennig S., Ischebeck T., Gibhardt J., Busse J., Feussner I., Stulke J. Hydrogen sulfide is a novel potential virulence factor of M y c o p l a s m a p n e u m o nia e: characterization of the unusual cysteine desulfurase/desulfhydraseHapE. Mol. Microbiol. 2016;100:42–54. doi: 10.1111/mmi.13300. [DOI] [PubMed] [Google Scholar]
- Gufe C., Hodobo T.C., Mbonjani B., Majonga O., Marumure J., Musari S., Jongi G., Makaya P.V., Machakwa J. Antimicrobial Profiling of Bacteria Isolated from Fish Sold at Informal Market in Mufakose, Zimbabwe. Int. J. Microbiol. 2019:7. doi: 10.1155/2019/8759636. 2019, Article ID 8759636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassan N.I., Ahmed T. Mycoplasma and Ureaplasma of the genital tract of camels in Egypt. Assiut Vet. Med. J. 1997;38:104–118. [Google Scholar]
- Hill A. Comparison of mycoplasmas isolated from captive wild felines. Res. Vet. Sci. 1975;18:139–143. [PubMed] [Google Scholar]
- Howard, W.W., Ricardo, F.C., Lioyd, H.L., 1994. Textbook of Mycoplasmosis in Animals, Laboratory Diagnosis, AVLD, 1st edition.
- Jambhekar A., Robin E., Le Boedec K. A systematic review and meta-analyses of the association between 4 Mycoplasma species and lower respiratory tract disease in dogs. J. Vet. Intern. Med. 2019;33:1880–1891. doi: 10.1111/jvim.15568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janda J.M., Abbott S.L. 16S rRNA gene sequencing for bacterial identification in the diagnostic laboratory: Pluses, perils, and pitfalls. J. Clin. Microbiol. 2007;45:2761–2764. doi: 10.1128/JCM.01228-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jechlinger W., Chopra-Dewasthaly R., Glew M., Citti C., Rosengarten R. Molekulare Grundlage der Pathogenität von Mycoplasma agalactiae [Molecular basis of Mycoplasma agalactiae pathogenicity]. Berl. Munch. Tierarztl. Wochenschr. 2004;117:472–479. [PubMed] [Google Scholar]
- Jozefova J., Ayling R.D., Zendulkova D. Report on investigations into the Mycoplasma species present in some clinically sick cattle in the Czech Republic. Med. Weter. 2014;70:413–416. [Google Scholar]
- Koshimizu K, Ogata M. Characterization and differentiation of mycoplasmas of canine origin. Nippon JuigakuZasshi. 1974;36:391–406. doi: 10.1292/jvms1939.36.391. [DOI] [PubMed] [Google Scholar]
- Krumpeman P.H. Multiple antibiotic resistance indexing Escherichia coli to identify the risk sources of faecal contamination of foods. Appl. Environ. Microbiol. 4. 1983;165:170. doi: 10.1128/aem.46.1.165-170.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krzysztoń-Russjan J., Bubko I., Drozd E., Gruber-Bzura B.M., Anuszewska E.A. B23 Influence of Mycoplasma arginini on inflammatory response and energy metabolism in human cells with and without HTT gene mutation. JNNP. 2016;87(Suppl 1) [Google Scholar]
- Lauerman L.H. Mycoplasmas of the Bovine Respiratory Tract. In: Whitford H.W., Rosenbusch R.F., Lauerman L.H., editors. Mycoplasmosis in Animals: Laboratory Diagnosis. Iowa State University Press; Ames, Iowa: 1994. pp. 50–56. [Google Scholar]
- Leach R.H. The occurrence of Mycoplasma arginini in several animal hosts. Vet. Rec. 1970;87:319–320. doi: 10.1136/vr.87.11.319. [DOI] [PubMed] [Google Scholar]
- Lysnyansky I., Mikula I., Gerchman I., Levisohn S. Rapid Detection of a Point Mutation in the parC Gene Associated with Decreased Susceptibility to Fluoroquinolones in Mycoplasma bovis. Antimicrob. Agents Chemother. 2009;53:4911–4914. doi: 10.1128/AAC.00703-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maboni G., Seguel M., Lorton A., Berghaus R, Sanchez S. Canine infectious respiratory disease: New insights into the etiology and epidemiology of associated pathogens. PLoS ONE. 2019;14(4) doi: 10.1371/journal.pone.0215817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magiorakos A.P., Srinivasan A., Carey R.B., Carmeli Y., Falagas M.E., Giske C.G., Harbarth S., Hindler J.F., Kahlmeter G., Olsson-Liljequist B., Paterson D.L., Rice L.B., Stelling J., Struelens M.J., Vatopoulos A., Weber J.T., Monnet D.L. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012;18(3):268–281. doi: 10.1111/j.1469-0691.2011.03570.x. [DOI] [PubMed] [Google Scholar]
- McAuliffe L., Ellis R.J., Lawes J.R., Ayling R.D., Nicholas R.A. 16S rDNA PCR and denaturing gradient gel electrophoresis; a single generic test for detecting and differentiating Mycoplasma species. J. Med. Microbiol. 2005;54:731–739. doi: 10.1099/jmm.0.46058-0. [DOI] [PubMed] [Google Scholar]
- McAuliffe L., Ellis R.J., Miles K., Ayling R.D., Nicholas R.A.J. Biofilm formation by Mycoplasma species and its role in environment persistence and survival. Microbiology. 2006;152:913–922. doi: 10.1099/mic.0.28604-0. [DOI] [PubMed] [Google Scholar]
- Mederos-Iriarte L.E., Poveda J.B., Poveda C.G., Vega-Orellana O.M., Gutiérrez C., Corbera J.A., Ramírez A.S. Mycoplasma detection and isolation from one-humped camels (Camelus dromedarius) Trop. Anim Health Prod. 2014;46:1317–1320. doi: 10.1007/s11250-014-0639-9. [DOI] [PubMed] [Google Scholar]
- Mohamed A.A., Yassin M.H., Hassan M.M., Sabry A.M., Ibrahim A.M. Molecular and Bacteriological Diagnosis of Mycoplasma Species Infection in Camels at Taif Governorate. Saudi Arabia. Ann. Res. Rev. Biol. 2018;23:1–6. Article no.ARRB.39063. [Google Scholar]
- Napp S., Chevalier V., Busquets N., Calistri P., Casal J., Attia M., Elbassal R., Hosni H., Farrag H., Hassan N., Tawfik R., Abd Elkader S., Bayomy S. Understanding the legal trade of cattle and camels and the derived risk of Rift Valley Fever introduction into and transmission within Egypt. PLoSNegl. Trop. Dis. 2018;12(1) doi: 10.1371/journal.pntd.0006143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navidmehr J., Zibaei M., Afshariyan M., Fathinajafi M. 2009. Identification of Mycoplasma from camels with Pneumonia slaughtered in Mashhad industrial abattoir by Nested-PCR. AGRIS, Agricultural Scientific Information and Documentation Centre, Agricultural Research and Education OrganizationPublisher: Razi Vaccine and Serum Research Institute 101 page. [Google Scholar]
- Parker A.M., Sheehy P.A., Hazelton M.S., Bosward K.L., House J.K. A review of mycoplasma diagnostics in cattle. J. Vet. Intern. Med. 2018;32:1241–1252. doi: 10.1111/jvim.15135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez-Casal J., Prysliak T. Detection of antibodies against the <pe-bold>Mycoplasma bovis glyceraldehyde-3-phosphate dehydrogenase protein in beef cattle. Microb. Pathog. 2007;43:189–197. doi: 10.1016/j.micpath.2007.05.009. [DOI] [PubMed] [Google Scholar]
- Prayson M.J., Venkatarayappa I., Srivastava M., Northern I., Burdette S.D. Deep infection with Mycoplasma arginini in an open femur fracture secondary to an African lion bite: a case report. Injury Extra. 2008;39:243–246. [Google Scholar]
- Pritchard R.E., Prassinos A.J., Osborne J.D., Raviv Z., Balish M.F. Reduction of Hydrogen Peroxide Accumulation and Toxicity by a Catalase from Mycoplasma iowae. PLoS ONE. 2014;9(8) doi: 10.1371/journal.pone.0105188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roess A., Carruth L., Mann M., Kabbash I., Melaku S., Atia M., Mohamed M., Bansal S., Lahm S., Terefe Y., Salman M. Livestock movement and emerging zoonotic disease outbreaks: applying ecological, network, and sociocultural theories to assess the risk of Middle East respiratory syndrome from camel trade in Ethiopia and Egypt. The Lancet Global Health. 2015;3(Supplement 1):S26. [Google Scholar]
- Sharma S., Markham P.F., Browning G.F. Genes Found Essential in Other Mycoplasmas Are Dispensable in Mycoplasma bovis. PLoS ONE. 2014;9(6):e97100. doi: 10.1371/journal.pone.0097100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silló P., Pintér D., Ostorházi E., Mazán M., Wikonkál N., Pónyai K., Volokhov D.V., Chizhikov V.E., Szathmary S., Stipkovits L., Kárpáti S. Eosinophilic fasciitis associated with Mycoplasma arginini infection. J. Clin. Microbiol. 2012;50:1113–1117. doi: 10.1128/JCM.05568-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmons W.L., Dybvig K. Catalase Enhances Growth and Biofilm Production of Mycoplasma pneumoniae. Curr. Microbiol. 2015;71:190–194. doi: 10.1007/s00284-015-0822-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- St George T.D., Carmichael L.E. Isolation of Mycoplasma ovipneumoniae from sheep with chronic pneumonia. Vet. Rec. 1975;97:205–206. doi: 10.1136/vr.97.11.205. [DOI] [PubMed] [Google Scholar]
- Stamm D.R., Stankewicz H.A. StatPearls [Internet] StatPearls Publishing; Treasure IslandFL: 2020. Atypical Bacterial Pneumonia. [Updated 2019 Nov 6].https://www.ncbi.nlm.nih.gov/books/NBK532239/ 2020 Jan-. Available from. [PubMed] [Google Scholar]
- Subramaniam S, Bergonier D, Poumarat F, Capaul S., Schlatter Y., Nicolet J., Frey J. Species identification of Mycoplasma bovis and Mycoplasma agalactiae based on the uvrC genes by PCR. Mol. Cell Probe. 1998;12:161–169. doi: 10.1006/mcpr.1998.0160. [DOI] [PubMed] [Google Scholar]
- Sykes J.E. Copyright © 2013 Elsevier Inc.; 2014. Mycoplasma Infectionsin Canine and Feline Infectious Diseases. [DOI] [Google Scholar]
- Tan R.J.S., Lim E.W., Ishak B. Ecology of mycoplasmas in clinically healthy cats. Aust. Vet. J. 1977 a;53:515–518. doi: 10.1111/j.1751-0813.1977.tb07934.x. [DOI] [PubMed] [Google Scholar]
- Tan R.J.S., Lim E.W., Ishak B. Significance and pathogenic role of Mycoplasma arginini in cat diseases. Can. J. Comp. Med. 1977 b;41:349–354. [PMC free article] [PubMed] [Google Scholar]
- Tan R.J.S., Miles J.A.R. Incidence and significance of mycoplasmas in sick cats. Res. Vet. Sci. 1974;16:27–34. [PubMed] [Google Scholar]
- Tang J., Hu M., Lee S., Roblin R. A polymerase chain reaction based method for detecting Mycoplama/Acholeplasma contaminants in cell culture. J. Microbiol. Methods. 2000;39:121–126. doi: 10.1016/s0167-7012(99)00107-4. [DOI] [PubMed] [Google Scholar]
- Thomas A., Dizier I., Linden A., Mainil J., Frey J., Vilei E.M. Conservation of the uvrC gene sequence in Mycoplasma bovis and its use in routine PCR diagnosis. Vet. J. 2004;168:100–102. doi: 10.1016/j.tvjl.2003.10.006. [DOI] [PubMed] [Google Scholar]
- Thomas A., Dizier I., Trolin A., Mainil J., Linden A., Ball H., Bell C. Isolation of Mycoplasma species from the lower respiratory tract of healthy cattle and cattle with respiratory disease in Belgium. Vet. Rec. 2002;151:472–476. doi: 10.1136/vr.151.16.472. [DOI] [PubMed] [Google Scholar]
- Thomas A.C., Bailey M., Lee M.R.F., Mead A., Morales-Aza B., Reynolds R., Vipond B., Finn A., Eisler M.C. Insights into Pasteurellaceae carriage dynamics in the nasal passages of healthy beef calves. Sci Rep. 2019;9:11943. doi: 10.1038/s41598-019-48007-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas L.H., Smith G.S. Distribution of mycoplasmas in the non-pneumonic bovine respiratory tract. J. Comp. Pathol. 1972;82:1–4. doi: 10.1016/0021-9975(72)90019-9. [DOI] [PubMed] [Google Scholar]
- Van Kuppeveld F.J.M., Johansson K.E., Galama J.M.D., Kissing J.G., Bolske G., Van Der Logt J.T.M., Melchers W.J.G. Detection of Mycoplasma contamination in cell cultures by a Mycoplasma Group-Specific PCR. Appl. Environ. Microbiol. 1994;60:149–152. doi: 10.1128/aem.60.1.149-152.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanabe M., Hitomi S., Goto M., Hasegawa Y. Blood stream Infection Due to Mycoplasma arginini in an Immunocompromised Patient. J. Clin. Microbiol. 2012;50:3133–3135. doi: 10.1128/JCM.00736-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yechouron A., Lefebvre J., Robson H.G., Rose D.L., Tully J.G. Fatal septicemia due to Mycoplasma arginini: a new human zoonosis. Clin. Infect. Dis. 1992;15:434–438. doi: 10.1093/clind/15.3.434. [DOI] [PubMed] [Google Scholar]
- Zella D., Curreli S., Benedetti F., Krishnan S., Cocchi F., Latinovic O.S., Denaro F., Romerio F., Djavani M., Charurat M.E., Bryant J.L., Tettelin H., Gallo R.C. Mycoplasma promotes malignant transformation in vivo, and its DnaK, a bacterial chaperone protein, has broad oncogenic properties. PNAS. 2018;115:E12005–E12014. doi: 10.1073/pnas.1815660115. [DOI] [PMC free article] [PubMed] [Google Scholar]