Supplemental digital content is available in the text.
Keywords: COVID-19, coronavirus, critical care, innovation, intensive care, knowledge dissemination, nursing, pandemic, personal protective equipment, PPE, preparedness
ABSTRACT
INTRODUCTION
This reflections article provides insight toward nursing innovations to reduce the overuse of personal protective equipment while maintaining a safe environment for staff taking care of COVID-19 patients. The secondary aim of this article to capitalize on recent advances in mass electronic communication through social media to encourage nurses across the globe to share their knowledge and expertise during this pandemic.
INNOVATIONS
The many innovations that have been implemented fall into 3 categories of reducing unnecessary use of personal protective equipment, promoting staff safety and readiness, and reducing foot traffic.
SUMMARY
These strategies are being shared to promote dissemination of innovative nursing interventions that will save lives during the COVID-19 pandemic.
This reflections article has 2 aims. The first aim is to share recent tips, tricks, modifications, and techniques that we have found useful during the COVID-19 pandemic. The second and perhaps more important aim is to facilitate the nursing communication network that is sharing the wealth of nursing knowledge and experience. During the COVID-19 pandemic, the World Health Organization (WHO)1 has outlined a 4-pronged strategy to (1) prepare and be ready; (2) detect, prevent, and treat; (3) reduce and suppress; and (4) innovate and improve. Registered nurses (RNs) on the front lines have been working for weeks with limited resources, and they have been instrumental in all 4 prongs outlined by the WHO.
Nurses are innovative out of necessity; the phrase “where there's a nurse around—there's a work-around…” embodies that we find ways to improve the process of care at every opportunity.2,3 Florence Nightingale was born in 1820, and during her lifetime, she revolutionized care by sharing nursing knowledge during a war.4 Through information dissemination and nursing actions, the spread of disease was reduced and lives were saved. Two hundred years later, during a pandemic, nurses are once again tasked to reduce contamination. A vital key to Nightingale's success was her ability to disseminate her observations. Clearly, one truth is that there is no single intervention, modification, or tip that only 1 hospital in the world has discovered. Unique to 2020 is the rapidity through which these ideas can be shared.5
Innovations
The nursing response to COVID-19 can be summarized as strategies that are aimed to reduce the use of personal protective equipment (PPE), reduce transmission of the disease, and promote readiness while maintaining a safe environment (Table 1). A short description of various innovations is provided in Table 2.
TABLE 1.
Early Innovations and Actions Implemented During the COVID-19 Pandemic

TABLE 2.
Brief Description of Innovations
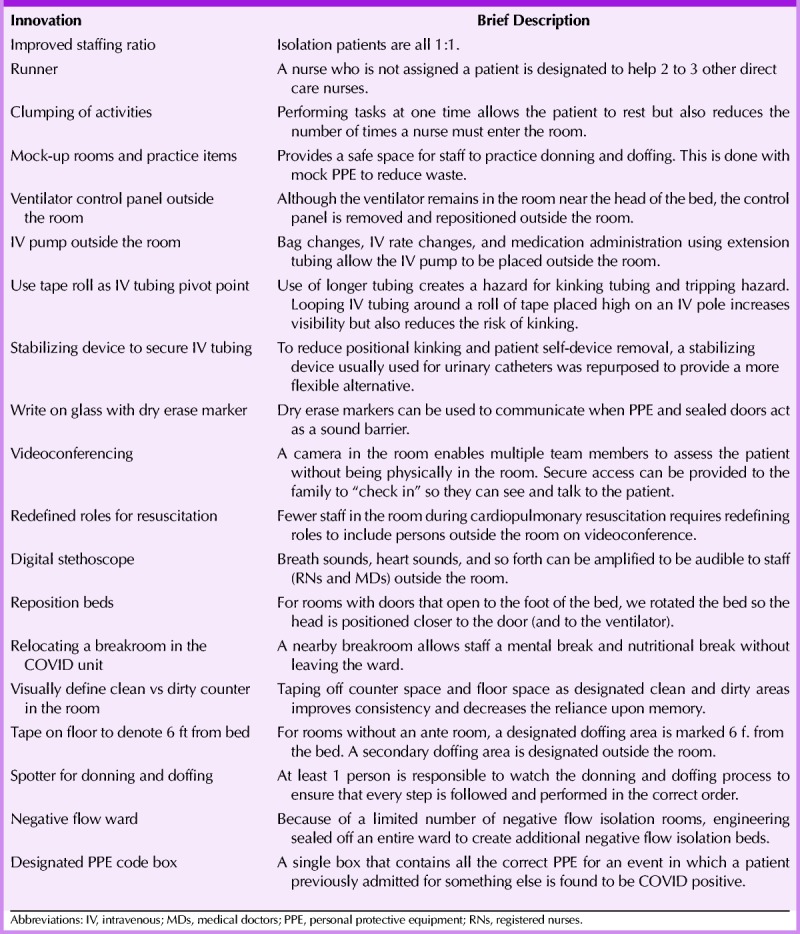
The COVID-10 pandemic has created a shortage of PPE, and nurse-driven strategies aimed to reduce use of PPE address the WHO need for preparedness, prevention, and innovation. Only by judicious use of resources can we extend the window of protection for frontline staff. Improved staffing ratios have already been shown to reduce cost and outcomes.6–10 Increasing the staffing ratio, clumping activities, and designating an RN to be a “runner” and not be in an isolation room enable that a nurse can stay in a COVID-19 room without the need to doff PPE to retrieve supplies or medications, nor overstock/oversupply the room. Videoconferencing and digital stethoscopes allow staff to assess the patient without being in the room (this is functionally similar to an RN in the room performing the NIHSS while the neurology team observes). In some cases, the video link (secure) can be shared with family to further reduce foot traffic while facilitating family virtual presence.
Relocating equipment, such as intravenous (IV) pumps, ventilator control panel, and the bed to facilitate the safe removal of equipment outside the room, all have the benefit of reducing the number of times an RN needs to go into the room (see Supplemental Digital Content 1, available at http://links.lww.com/JNN/A252). This reduces the unnecessary use of PPE and increases staff safety. We found that relocating equipment had the downstream effect of creating a tripping hazard (IV tubing) and also a risk that the tubing would kink and obstruct flow. An innovation and simple solution was to repurpose a urinary catheter stabilizing device (StatLock, CRBard Inc) to secure the tubing to the patient and to an IV pole. This was further enhanced by a roll of tape (see Supplemental Digital Content 2, available at http://links.lww.com/JNN/A253) that prevents the IV tubing from occluding. This also ensures the IV extension tubing used does not touch the floor, reducing the risk of contamination.
Nurse-Driven Strategies Aimed to Promote Staff Safety and Readiness
Readiness can be interpreted in many ways.11 One can be ready (prepared) mentally and physically, or one can be willing (ready) to take action. Both are vital for successful response.12 Having a designated space for staff to eat, drink, and relax (even if only for a few minutes) is vital to preparedness. By creating a makeshift breakroom, we further reduce foot traffic while simultaneously promoting staff wellness. Staff ingenuity such as clumping activities and moving IV pumps outside the room helps decrease the risk of exposure. The use of a dedicated person to observe doffing (spotter) is vital; this person not only helps ensure the proper steps are followed in the proper order but also can act as a set of eyes to monitor for accidental exposure risk (eg, the outside of the gown touches the RN's skin).
Additional visual cues are provided using dressing tape. Because rooms are being repurposed during high census, there are often rooms without ante room. Tape is placed to mark an area inside the room and 6 ft from the bed where the initial doffing (mask and face shield) takes place before the RN exits the room to another area outside the room (also marked by tape) to finish the doffing procedure (see Supplemental Digital Content 3, available at http://links.lww.com/JNN/A254).
Nurse-Driven Strategies Aimed to Reduce Foot Traffic
Foot traffic refers both to the number of people who are entering an isolation room or an isolation ward and to the number of times the area is entered. This can be operationalized as the number of times any door is opened for passage and thereby increases the risk of contamination. As described earlier, adequate staffing to support a 1:1 or 2:1 ratio decreases the number of times a nurse needs to go in and out of a room. After engineering adjustments, the entire nurses' station ventilation was adjusted to increase positive pressure while each patient room in the ward became negative flow. Designating a break area within the ward decreased the need for staff to leave the ward and further reduced door opening.
Protecting the environment of care does not end at the bedside, and staff have tapped into their gaming skills to design new intrahospital transport routes. In our hospital, there is 1 floor that has zero patients and wider-than-average hallways. Although this is a less direct route, patients with known or suspected COVID-19 are transported through this area to reduce the risk of exposure to other patients.
Summary
Nightingale was very likely not the first person to consider hand hygiene. Furthermore, her innovations, in themselves, were not revolutionary: do not put too many people in 1 room, clean and change dressings, circulate fresh air, and so forth. What Nightingale did that was revolutionary was to share her ideas. Basing their work in large part on Nightingale's founding principles, Pope et al13 described that, as nurses, we should become part of a cadre of professionals who are responsible for the dissemination of knowledge. We believe that, if Florence had a Facebook or Twitter account, she would have been posting daily from the Crimean battlefield. During this worldwide event, we share our knowledge in the hopes that this will encourage other nurses to share their tips, their innovations, and their ingenuity.
Supplementary Material
Footnotes
Dr Olson declares that he is the editor of the Journal of Neuroscience Nursing. The remaining authors declare no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.jnnonline.com).
References
- 1.World Health Organization WHO Director-General's Opening Remarks at the Mission Briefing on COVID-19—12 March 2020. World Health Organization; 2020. [Google Scholar]
- 2.Gray A. Advanced or advancing nursing practice: what is the future direction for nursing? Br J Nurs. 2016;25(1):8, 10, 12–8, 10, 13. [DOI] [PubMed] [Google Scholar]
- 3.Carroll VS. Executive summary: the Zika virus. J Neurosci Nurs. 2017;49(1):2–4. [DOI] [PubMed] [Google Scholar]
- 4.Nightingale F, Skretkowicz V. Florence Nightingale's Notes on Nursing. London, England: Scutari Press; 1992. [Google Scholar]
- 5.Ross P, Cross R. Rise of the e-nurse: the power of social media in nursing. Contemp Nurse. 2019;55(2–3):211–220. [DOI] [PubMed] [Google Scholar]
- 6.Carlisle B, Perera A, Stutzman SE, Brown-Cleere S, Parwaiz A, Olson DM. Efficacy of using available data to examine nurse staffing ratios and quality of care metrics. J Neurosci Nurs. 2020;52(2):78–83. [DOI] [PubMed] [Google Scholar]
- 7.Wynendaele H, Willems R, Trybou J. Systematic review: association between the patient-nurse ratio and nurse outcomes in acute care hospitals. J Nurs Manag. 2019;27(5):896–917. [DOI] [PubMed] [Google Scholar]
- 8.Nadolski C, Britt P, Ramos LC. Improving staffing and nurse engagement in a neuroscience intermediate unit. J Neurosci Nurs. 2017;49(3):169–173. [DOI] [PubMed] [Google Scholar]
- 9.Lee A, Cheung YSL, Joynt GM, Leung CCH, Wong WT, Gomersall CD. Are high nurse workload/staffing ratios associated with decreased survival in critically ill patients? A cohort study. Ann Intensive Care. 2017;7(1):46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aiken LH, Sloane DM, Bruyneel L, et al. Nurse staffing and education and hospital mortality in nine European countries: a retrospective observational study. Lancet. 2014;383(9931):1824–1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jester B, Uyeki T, Jernigan D. Readiness for responding to a severe pandemic 100 years after 1918. Am J Epidemiol. 2018;187(12):2596–2602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nicholson A, Shah CM, Ogawa VA, eds. Forum on microbial threats. Board on Global Health, Health and Medicine Division, National Academies of Sciences, Engineering, and Medicine. In: Exploring Lessons Learned from a Century of Outbreaks: Readiness for 2030: Proceedings of a Workshop. Washington, DC: National Academies Press (US); 2019. [PubMed] [Google Scholar]
- 13.Pope AMSM, Mood LH. Ch. 5. Nursing research. In: Pope AM, Snyder MA, Mood LH, eds. Nursing Health, & Environment: Strengthening the Relationship to Improve the Public's Health. Washinton, DC: National Academies Press (US); 1995. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


