1. Introduction
Across the world, pain treatment centres have closed their doors. Because of the COVID-19 pandemic, healthcare providers are abruptly changing their care delivery to protect patients and staff from infection and to reallocate resource towards the greatest acute needs. Elective, routine, and nonemergency casework has stopped in secondary and tertiary centres, while in primary care, patients are requested to stay away or “socially distance,” and in residential care facilities and hospices, strict isolation and separation protocols have been introduced.
Before the COVID-19 pandemic, telemedicine and eHealth approaches were being developed and tested in a gradual fashion with many studies focusing on lessons learned and barriers to using digital solutions.3,37,39,51 Overnight, however, treating or supporting people with non-urgent and long-term conditions at a distance from healthcare providers has become imperative. These immediate changes are happening across healthcare systems. Telemedicine is being used to demand-manage the flow of patients with respiratory distress accessing emergency departments25; video consultation is being introduced in multiple settings23; and using social media is being discussed positively for its potential to direct people to trusted resources, to counteract misinformation, and to provide psychological first aid.36
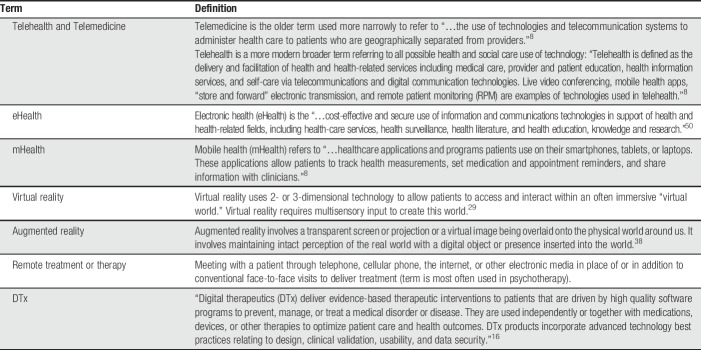
Pain management providers face the challenge of delivering face-to-face service through different modes. Fortunately, there is a rich stream of research and clinical experience in the use of different technological solutions. Table 1 provides a summary of the definitions and terminology in use.
Table 1.
Definitions and terminology used in remotely supported pain management.
We consider 4 related factors to help guide healthcare professionals caring for patients with chronic pain: (1) the public health consequences of COVID-19 for patients with pain; (2) the consequences of not treating these patients for the unknown duration of this pandemic; (3) options for remote assessment and management; and (4) clinical evidence supporting remote therapies. Finally, we provide guidance for those attempting to rapidly transition to remote care with technology and discuss the lessons for the future of the pain treatment centre.
2. Public health considerations
Pain prevention and control—particularly for chronic pain—will inevitably be disrupted by the COVID-19 pandemic. Diversion of resources will be planned (eg, cancelling elective surgery and outpatient procedures for chronic disease management) and unplanned (eg, medication shortages due to panic buying and inaccessibility of remaining healthcare options during movement restrictions). Longer-term, healthcare workers are likely to be at higher risk of lasting psychological morbidity based on evidence from the 2002 to 2003 SARS epidemic.33
The effect of the pandemic on pain burden will be differentially distributed across and within populations, depending on population characteristics emerging as determinants of the pandemic, including older age, population density, socioeconomic gradient, smoking prevalence, levels of chronic disease morbidity, availability of diagnostic testing, and access to health care. Some of these characteristics are also associated with higher levels of chronic pain prevalence and burden (eg, older age, socioeconomic status, smoking prevalence, chronic disease comorbidity, and access to health care).5 Therefore, populations with higher existing pain burden are more likely to experience higher incidence of COVID-19 infections, greater disruption to their usual healthcare access, and worse downstream consequences of abruptly altered health care. In addition, some at-risk population subgroups also have poor access to technologies used in remote care.48
Prevention of chronic pain within populations currently depends on best practice management of acute pain and early recognition of the risk of progression to chronic pain.6 Drivers of acute pain burden include injury-related pain and treatment-related pain (eg, after surgery). Social isolation measures will directly influence the number and type of injuries experienced within populations (eg, fewer road traffic and workplace accidents, increases in conflict/interpersonal violence, and domestic injuries). Changes in the overall volume and type of surgery (more emergency and high acuity elective surgery) are occurring as health systems pivot to respond to the pandemic. Preventing chronic pain is complex at the best of times, but in a global health pandemic, risk factors for pain morbidity and mortality will be magnified.
3. Not treating chronic pain
The high prevalence of chronic pain risks inuring us to suffering, one can easily mistake common for trivial. When people with chronic pain are denied assessment and treatment, their condition can worsen significantly; spontaneous recovery is rare. People living with chronic pain have the largest global morbidity, measured by years lived in disability.44 People waiting for assessment often report severe levels of pain that interfere with their ability to function, and reports of severe pain are associated with more severe levels of depression in 50% and suicidal thinking in 34.6%.10 Children and adolescents also report high symptom burden when awaiting evaluation.43 Furthermore, people waiting over 6 months for assessment experience deteriorating health-related quality of life, increased pain, and increased depression.30
The risks of harm from undertreatment can be exacerbated further by the risk of harm from inappropriate treatment. In many countries, most notably the United States and Canada, chronic pain management is practiced in the shadow of a crisis of the oversupply and overuse of opioids.47 Given that best practice for prevention of opioid harms is unclear, referral to pain professionals for pain medicine management is common.4 In the United States, few pain clinics can care for high volumes of patients, and referring everyone for opioid stewardship is unrealistic.11 In North America, we already see an increase in serious mental health problems as some turn to illicit sources of opioids, while others suffer in silence.24 Not treating chronic pain will have consequences for individuals, healthcare systems, and providers in the short- and long-term, increasing quantity, severity, and complexity of need.
4. Distance assessment and treatment with technology
To address the needs of people with chronic pain, one should look first to pervasive and inexpensive technology such as the telephone.40 Telemedicine, including telephone consultation, short message services, and video conferencing are used worldwide and are broadly analogous to traditional care, although the benefits and costs of telemedicine are still largely unknown.28,34 They are minimally disruptive and require a broadly similar healthcare resource.
Clinical assessment relying on patient-reported outcome measures can be undertaken remotely. Mobile telephones with camera technology allow for shareable images of paper assessments. In addition, many local electronic health record systems already allow for electronic administration of measures. Several web-based systems have been optimised for people with pain, such as the CHOIR system in the United States9 or the PAIN OUT system in Europe.41 Such systems allow clinicians to review measures before appointments. Interdisciplinary evaluations can be modified for distance use before the visit, supporting history and interview. Even aspects of the physical examination can be undertaken virtually, for example, in judging appearance, movement, or in self-examination under guidance. Although there are limitations to the lack of hands-on physical examination possible with telehealth, a modified virtual examination may allow an initial treatment plan to be started.
Pain self-management options are available using different technologies (eg, the internet, email, computers, and “smart” phones), which play a central role in health care provided to patients. Most studies have been concerned with remotely delivered self-management interventions for chronic pain, undertaken at one's convenience and without having to leave the home.12,14,15,42,45 These interventions aim to provide the same information and training in self-management skills as provided in face-to-face pain management programs but use technology in different ways. Interventions have been examined in controlled trials.20,46
The focus on technology promises increased access and scalability, although evaluations of their impact in reaching scale are scarce. Several of these interventions are already freely available in some parts of the world, and many others are commercially in development or are being offered.16 A caveat on commercially developed interventions, however, is the current lack of quality control over the content, security, and marketing claims. The burgeoning app market is a good example, and caution should be exercised.28
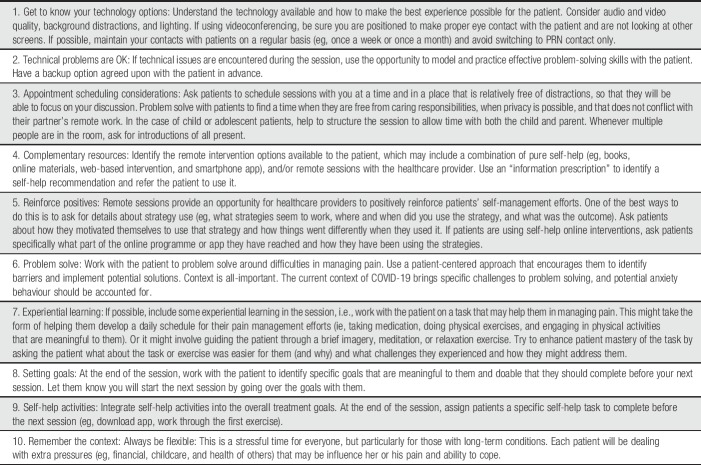
Table 2 summarises guidance for those unfamiliar with telemedicine and digital treatments who are tasked with their rapid deployment.
Table 2.
Practical recommendations for the rapid introduction of remotely supported pain management.
5. Evidence for efficacy and harm of telemedicine and DTx interventions
Although telephones are in common clinical use, full-scale telemedicine for people with chronic pain is rare. In general, the evidence is similar to that from primary care studies and is cautiously optimistic but recognizes barriers to implementation, unforeseen harm, and potential for inequity in access and use.17,21,31,39
Most innovation has been in the development of internet-delivered therapies for people with chronic pain. Many remotely delivered programs can be accessed directly and have minimal requirements. In children and adolescents with mixed chronic pain (eg, sickle cell disease, musculoskeletal pain, juvenile idiopathic arthritis, and headache), remote psychological therapies delivered through the internet or mobile applications show small beneficial effects for reducing pain intensity, including headache severity, after treatment, but not maintained at follow-up.20 The first Cochrane systematic review of technological interventions for chronic pain in adults found 15 studies with 2000 participants.18 Several systematic reviews have been published since.7,13,32,46 Reviews identify small to moderate reductions in pain, disability, and distress in intervention groups compared with any control (including active, standard care, or waitlist control).7,32 Unsurprisingly, when compared with only active control (eg, face-to-face therapies), no difference in treatment effect was found between remote and in-person therapies.32 Remotely delivered physical exercise interventions are also available, with benefits comparable with usual care for reducing pain and beneficial compared with no treatment.1
Although promising, there are concerns related to the evidence underlying remote therapies; relatively few studies assessed for harm, and dropout can be substantial. Access and engagement are important to track and report, particularly as disadvantaged groups use technology less (eg, older adults and disabled people).2 “Therapeutic alliance” is important but may be more challenging to establish, foster, and maintain remotely. That said, a large trial delivering psychological therapy through an online pain course showed improvement in pain, disability, and emotional functioning compared with waiting list but few differences between groups with varying amounts of therapist contact.15 Understanding who struggles to engage and use eHealth provision is crucial to maximise effectiveness, as are concerns about privacy, transparency (eg, therapist-generated vs automated messages), and training needs of staff accustomed to face-to-face working.
Virtual and augmented reality are rarely used with chronic pain but have potential for remote use, going beyond distraction, with a focus on improving function and reducing distress.18 Early studies are promising but small.22,26
6. Discussion
COVID-19 will have consequences for people with chronic pain, a large population with the greatest global burden of disease. The downstream consequences of disrupting treatments for chronic pain have yet to be modelled but are likely to be substantial. Many healthcare professionals specialising in pain have skills directly relevant to the acute response to the pandemic and so will be redeployed; others may be able to maintain some service delivery to affected individuals.
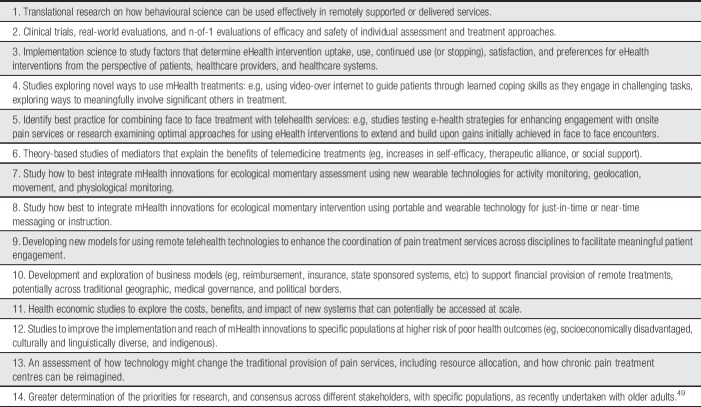
Telemedicine and eHealth interventions for service delivery will be attempted and will be novel for many. Ubiquitous communication technology is relatively inexpensive to access. It is practically possible to communicate with patients if the personnel and infrastructure are available. In some treatments, such as psychologically orientated self-management, investment in developing web-based or application-based platforms delivering pain self-management has produced some evidence of efficacy, and some products are freely available to download. Healthcare providers need to be aware that many of the behavioural components of eHealth self-management are not only potentially helpful for managing pain but also for emotional distress related to the COVID-19 pandemic. In Table 3, we suggest research priorities to improve the evidence for distance interventions and learn from this abrupt change in our practice.
Table 3.
Research priorities for remotely supported (eHealth) pain management services.
Changing practice in such an unplanned way will have positive and negative consequences, many unforeseen. Systems can establish protocols that can enable them to oversee, monitor, and capture important patient and provider outcomes and perspectives. When we come to redesign services after the pandemic, we will need to share that experience and use it to learn what works, to modify what does not work, and to build new models of care for people living with chronic pain.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Acknowledgements
No funding was provided for any author on this article, and there are no known conflicts of interest for any author. The authors are grateful for the PAIN Editorial Office, for the peer reviewers, and for the publishers for working quickly on this article.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
References
- [1].Adamse C, Dekker-Van Weering MG, van Etten-Jamaludin FS, Stuiver MM. The effectiveness of exercise-based telemedicine on pain, physical activity and quality of life in the treatment of chronic pain: a systematic review. J Telemed Telecare 2018;24:511–26. [DOI] [PubMed] [Google Scholar]
- [2].Arnberg FK, Linton SJ, Hultcrantz M, Heintz E, Jonsson U. Internet-delivered psychological treatments for mood and anxiety disorders: a systematic review of their efficacy, safety, and cost-effectiveness. PLoS One 2014;9:e98118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Badalato GM, Kaag M, Lee R, Vora A, Burnett A; the Workgroup AUA Telemedicine. Role of telemedicine in urology: contemporary practice patterns and future directions. Urol Pract 2020;7:122–6. [DOI] [PubMed] [Google Scholar]
- [4].Barnett ML. Opioid prescribing in the midst of crisis—myths and realities. NEJM 2020;382:1086–8. [DOI] [PubMed] [Google Scholar]
- [5].Blyth FM. The demography of chronic pain: an overview. In: Croft P, Blyth FM, van der Windt D, editors. Chronic pain epidemiology: from aetiology to public health. New York: Oxford University Press, 2010. ISBN 9780199235766. [Google Scholar]
- [6].Blyth FM, Van Der Windt DA, Croft PR. Chronic disabling pain: a significant public health problem. Am J Prev Med 2015;49:98–101. [DOI] [PubMed] [Google Scholar]
- [7].Buhrman M, Gordh T, Andersson G. Internet interventions for chronic pain including headache: a systematic review. Internet Interv 2016;l4:17–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Catalyst NE. What is telehealth? NEJM Catalyst 2018;4:1. [Google Scholar]
- [9].CHOIR. Available at: https://choir.stanford.edu/. Accessed March 2020.
- [10].Choiniere MD, Dion P, Peng R, Banner P, Barton A, Boulanger AJ, Clark A, Gordon D, Guerriere MC, Geurtin HM, Intrater S, LeFort SM, Lynch ME, Moulin DE, Ong-Lam M, Racine M, Rashiq S, Shir Y, Taenzer P, Ware M. The Canadian STOP-PAIN Project-part 1: who are the patients on the waitlists of multidisciplinary pain treatment facilities? Can J Anesth 2010;57:539–48. [DOI] [PubMed] [Google Scholar]
- [11].Comerci GJ, Katzman J, Duhigg DO. Controlling the swing of the pendulum. NEJM 2018;378:691–3. [DOI] [PubMed] [Google Scholar]
- [12].Connelly M, Schanberg LE, Ardoin S, Blakley M, Carrasco R, Chira P, Hayward K, Ibarra M, Kimura Y, Kingsbury DJ, Klein-Gitelman MS, Lawson E, Stinson J. Multisite randomized clinical trial evaluating an online self-management program for adolescents with juvenile idiopathic arthritis. J Pediatr Psychol 2019;44:363–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Dario AB, Cabral AM, Almeida L, Ferreira ML, Refshauge K, Simic M, Pappas E, Ferreira PH. Effectiveness of telehealth-based interventions in the management of non-specific low back pain: a systematic review with meta-analysis. Spine J 2017;17:1342–51. [DOI] [PubMed] [Google Scholar]
- [14].Dear BF, Titov N, Perry KN, Johnston L, Wootton BM, Terides MD, Rapee RM, Hudson JL. The Pain Course: a randomised controlled trial of a clinician-guided Internet-delivered cognitive behaviour therapy program for managing chronic pain and emotional well-being. PAIN 2013;154:942–50. [DOI] [PubMed] [Google Scholar]
- [15].Dear BF, Gandy M, Karin E, Staples LG, Johnston L, Fogliati VJ, Wooton BM, Terides MD, Kayrouz R, Perry KN, Sharpe L, Nicholas MK, Titov N. The Pain Course: a randomised controlled trial examining an internet-delivered pain management program when provided with different levels of clinician support. PAIN 2015;156:1920–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].DTxAlliance. Available at: https://dtxalliance.org/. Accessed March 26, 2020. [Google Scholar]
- [17].Eaton LH, Godfrey DS, Langford DJ, Rue T, Tauben DJ, Doorenbos AZ. Telementoring for improving primary care provider knowledge and competence in managing chronic pain: a randomised controlled trial. J Telemed Telecare 2020;26:21–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Eccleston C, Fisher E, Brown R, Craig L, Duggan GB, Rosser BA, Keogh E. Psychological therapies (Internet‐delivered) for the management of chronic pain in adults. Cochrane Database Syst Rev 2014;2:CD010152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Eccleston C, Tabor A, Keogh E. Using advanced technologies to improve access to treatment, to improve treatment, and to directly alter experience. In: Turk DC, Gatchel RJ, editors. Psychological approaches to pain management. 3rd ed. New York: Guilford Press, 2018. p. 289–301. ISBN 9781462528530. [Google Scholar]
- [20].Fisher E, Law E, Dudeney J, Eccleston C, Palermo TM. Psychological therapies (remotely delivered) for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev 2019;4:CD011118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Furlan AD, Zhao J, Voth J, Hassan S, Dubin R, Stinson JN, Jaglal S, Fabico R, Smith AJ, Taenzer P, Flannery JF. Evaluation of an innovative tele-education intervention in chronic pain management for primary care clinicians practicing in underserved areas. J Telemed Telecare 2019;25:484–92. [DOI] [PubMed] [Google Scholar]
- [22].Garrett B, Taverner T, McDade P. Virtual reality as an adjunct home therapy in chronic pain management: an exploratory study. JMIR Med Inform 2017;5:e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Geenhalgh T, Wherton J, Shaw S, Morrison C. Video consultations for covid-19: an opportunity in a crisis?. BMJ 2020;368:m998. [DOI] [PubMed] [Google Scholar]
- [24].Glod S. The other victims of the opioid epidemic. N Engl J Med 2017;376:2101–2. [DOI] [PubMed] [Google Scholar]
- [25].Hollander JE, Carr BG. Virutally perfect? Telemedicine for covid-19. N Engl J Med 2020. 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- [26].Jones T, Moore T, Choo J. The impact of virtual reality on chronic pain. PLoS One 2016;11:e0167523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Kroenke K, Theobald D, Wu J, Norton K, Morrison G, Carpenter J, Tu W. Effect of telecare management on pain and depression in patients with cancer: a randomised controlled trial. JAMA 2010;304:163–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Lalloo C, Shah U, Birnie KA, Davies-Chalmers C, Rivera J, Stinson J, Campbell F. Commercially available smartphone apps to support postoperative pain self-management: scoping review. JMIR Mhealth Uhealth 2017;5:e162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Li A, Montaño Z, Chen VJ, Gold JI. Virtual reality and pain management: current trends and future directions. Pain Man 2011;1:147–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Lynch ME, Campbell FA, Clark AJ, Dunbar MJ, Goldstein D, Peng P, Stinson J, Tupper H. A systematic review of the effect of waiting for treatment for chronic pain. PAIN 2008;136:97–116. [DOI] [PubMed] [Google Scholar]
- [31].Mariano TY, Wan L, Edwards RR, Jamison RN. Online teletherapy for chronic pain: a systematic review. J Telemed Telecare 2019:1357633X19871746. [DOI] [PubMed] [Google Scholar]
- [32].Martorella G, Boitor M, Berube M, Fredericks S, Le May S, Gélinas C. Tailored web-based interventions for pain: systematic review and meta-analysis. JIMR 2017;19:e385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Maunder RG, Lancee WJ, Balderson KE, Bennett JP, Borgundvaag B, Evans S, Fernandes CM, Goldbloom DS, Gupta M, Hunter JJ, McGillis Hall L, Nagle LM, Pain C, Peczeniuk SS, Raymond G, Read N, Rourke SB, Steinberg RJ, Stewart TE, Van De Velde-Coke S, Veldhorst GG, Wasylenki DA. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis 2006;12:1924–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].McGeary DD, McGear CA, Gatchel RJ. A comprehensive review of telehealth for pain management: where are we and the way ahead. Pain Pract 2012;12:570–7. [DOI] [PubMed] [Google Scholar]
- [35].Melville KM, Casey LM, Kavanagh DJ. Dropout from Internet‐based treatment for psychological disorders. Br J Clin Psychol 2010;49:455–71. [DOI] [PubMed] [Google Scholar]
- [36].Merchant RM, Lurie N. Social media and emergency preparedness in response to novel coronavirus. JAMA 2020. 10.1001/jama.2020.4469. [DOI] [PubMed] [Google Scholar]
- [37].Moo LR, Gately ME, Jafri Z, Shirk SD. Home-based video telemedicine for dementia management. Clin Gerontol 2020;43:193–203. [DOI] [PubMed] [Google Scholar]
- [38].Mott J, Bucolo S, Cuttle L, Mill J, Hilder M, Miller K, Kimble RM. The efficacy of an augmented virtual reality system to alleviate pain in children undergoing burns dressing changes: a randomised controlled trial. Burns 2008;34:803–8. [DOI] [PubMed] [Google Scholar]
- [39].O'Brien KM, Hodder RK, Wiggers J, Williams A, Campbell E, Wolfenden L, Yoong SL, Tzelepis F, Kamper SJ, Williams CM. Effectiveness of telephone-based interventions for managing osteoarthritis and spinal pain: a systematic review and meta-analysis. PeerJ 2018;6:e5846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Our World in Data. Availble at: https://ourworldindata.org/technology-adoption#mobile-phone-adoption. Accessed March 26, 2020. [Google Scholar]
- [41].PAINOUT. Availble at: http://pain-out.med.uni-jena.de. Accessed March 2020. [Google Scholar]
- [42].Palermo TM, Law EF, Fales J, Bromberg MH, Jessen-Fiddick T, Tai G. Internet-delivered cognitive-behavioral treatment for adolescents with chronic pain and their parents: a randomized controlled multicenter trial. PAIN 2016;157:174–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Palermo TM, Slack M, Zhou C, Aaron R, Fisher E, Rodriguez S. Waiting for a pediatric chronic pain clinic evaluation: a prospective study characterizing waiting times and symptom trajectories. J Pain 2019;20:339–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Rice AS, Smith BH, Blyth FM. Pain and the global burden of disease. PAIN 2016;157:791–6. [DOI] [PubMed] [Google Scholar]
- [45].Rini C, Porter LS, Somers TJ, McKee DC, DeVellis RF, Smith M, Winkel G, Ahern DK, Goldman R, Stiller JL, Mariani C, Patterson C, Jordan JM, Caldwell DS, Keefe FJ. Automated Internet-based pain coping skills training to manage osteoarthritis pain: a randomized controlled trial. PAIN 2015;156:837–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Slattery BW, Haugh S, O'Connor L, Francis K, Dwyer CP, O'Higgins S, Egan J, McGuire BE. An evaluation of the effectiveness of the modalities used to deliver electronic health interventions for chronic pain: systematic review with network meta-analysis. J Med Internet Res 2019;21:e11086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Stannard C. Opioids for pain in Europe: differing problems and differing solutions. In: Eccleston C, Wells C, Morlion B, editors. European pain management. Oxford: Oxford University Press, 2018. pp. 225–42. [Google Scholar]
- [48].Struminger BB, Arora S. Leveraging telehealth to improve health care access in rural America: it takes more than bandwidth. Ann Intern Med 2019;171:376–7. [DOI] [PubMed] [Google Scholar]
- [49].Wetherington E, Eccleston C, Gay G, Gooberman-Hill R, Schofield P, Bacon E, Dombrowski W, Jamison R, Rothman M, Meador L, Kenien C, Pillemer K, Lockenhoff C, Reid MC. Establishing a research agenda on mobile health technologies and later-life pain using an evidence-based consensus conference approach. Clin J Pain 2018;12:1416–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].World Health Organisation. eHealth. Available at: http://www.emro.who.int/health-topics/ehealth/. Accessed March 2020. [Google Scholar]
- [51].Zachrison KS, Boggs KM, Hayden EM, Espinola JA, Camargo CA., Jr Understanding barriers to telemedicine implementation in rural emergency departments. Ann Emerg Med 2020;75:392–9. [DOI] [PubMed] [Google Scholar]