Supplemental Digital Content is Available in the Text.
Keywords: children, COVID-19 pandemic, hospital outcomes, pediatric intensive care, public health preparedness, SARS-CoV-2
Abstract
Importance:
A surge in severe cases of COVID-19 (coronavirus disease 2019) in children would present unique challenges for hospitals and public health preparedness efforts in the United States.
Objective:
To provide evidence-based estimates of children infected with SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) and projected cumulative numbers of severely ill pediatric COVID-19 cases requiring hospitalization during the US 2020 pandemic.
Design:
Empirical case projection study.
Main Outcomes and Measures:
Adjusted pediatric severity proportions and adjusted pediatric criticality proportions were derived from clinical and spatiotemporal modeling studies of the COVID-19 epidemic in China for the period January-February 2020. Estimates of total children infected with SARS-CoV-2 in the United States through April 6, 2020, were calculated using US pediatric intensive care unit (PICU) cases and the adjusted pediatric criticality proportion. Projected numbers of severely and critically ill children with COVID-19 were derived by applying the adjusted severity and criticality proportions to US population data, under several scenarios of cumulative pediatric infection proportion (CPIP).
Results:
By April 6, 2020, there were 74 children who had been reported admitted to PICUs in 19 states, reflecting an estimated 176 190 children nationwide infected with SARS-CoV-2 (52 381 infants and toddlers younger than 2 years, 42 857 children aged 2-11 years, and 80 952 children aged 12-17 years). Under a CPIP scenario of 5%, there would be 3.7 million children infected with SARS-CoV-2, 9907 severely ill children requiring hospitalization, and 1086 critically ill children requiring PICU admission. Under a CPIP scenario of 50%, 10 865 children would require PICU admission, 99 073 would require hospitalization for severe pneumonia, and 37.0 million would be infected with SARS-CoV-2.
Conclusions and Relevance:
Because there are 74.0 million children 0 to 17 years old in the United States, the projected numbers of severe cases could overextend available pediatric hospital care resources under several moderate CPIP scenarios for 2020 despite lower severity of COVID-19 in children than in adults.
The early stages of the global COVID-19 (coronavirus disease 2019) pandemic in China, South Korea, and Italy revealed a strong age effect on disease severity, clinical outcomes, and case fatality.1–3 Relative risks for severe and fatal outcomes appear to be much higher among elderly patients than among children. Because the majority of children who are infected with the novel coronavirus SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) have experienced mild illness not requiring hospitalization, the virus-associated risks to children have been largely unrecognized by news media in the United States.4 Public messages have communicated that children can be infected with SARS-CoV-2 but that they will likely be healthy spreaders or at worst come down with a mild case of influenza-like illness requiring bed rest at home.5,6
A small proportion of children infected with SARS-CoV-2 develop severe cases of COVID-19 that require hospitalization.7–11 One of the earliest cases of COVID-19 in central Wuhan, China, was a previously healthy 3-year-old child who was admitted to the intensive care unit (ICU) in early January 2020 with ground glass opacities in both lungs, treated with pooled immunoglobulin, and discharged home after a hospital stay of 13 days.7 A case series of 171 confirmed SARS-CoV-2 pediatric patients who were tested and hospitalized at Wuhan Children's Hospital between January 28 and February 26 included 3 children who required intensive care, one of whom subsequently died 4 weeks after admission.8
In the largest (n = 2143) study of severity of COVID-19 in identified cases among children, Dong et al9 reported that infants were at highest risk of becoming severely or critically ill (10.6% of all infant cases), with severely ill characterized by pneumonia and central cyanosis (8.7% of infant cases) and critically ill defined as acute respiratory distress syndrome (ARDS) requiring mechanical ventilation (1.8% of infant cases). The proportion of cases that became severely or critically ill was 7.3% for those aged 1 to 5 years and 4.2% for those aged 6 to 15 years. There was 1 recorded fatality of a 14-year-old boy in Hubei Province.9
In China, strong mandatory quarantines and infection control efforts were effective in stopping the increase in incidence of pediatric COVID-19 cases by March 2020.9 Modeling studies predict that transmission chains can be interrupted with sustained social interventions.12,13 However, in geopolitical situations where widespread population infection has not been contained, community spread will include infections among the young. Despite a low probability of severe pediatric illness, the sizeable population of children in the United States could result in large numbers of children requiring acute or critical hospital care.
The purpose of this study was to (1) report current surveillance counts of confirmed COVID-19 cases admitted to pediatric intensive care units (PICUs) in the United States; (2) provide empirically derived estimates of the total number of children infected with SARS-CoV-2 through April 6, 2020; (3) use possible scenarios of cumulative pediatric infection proportion (CPIP) to project cumulative numbers of severely and critically ill children with COVID-19 who will require hospitalization before the end of 2020.
Methods
Pediatric intensive care unit admissions in the United States
We obtained real-time data on the numbers of children with confirmed COVID-19 who were admitted to a hospital PICU in the United States from the online dashboard administered by Virtual PICU Systems (VPS) (myvps.org). Originally developed as a voluntary nationwide hospital registry to facilitate quality improvement in pediatric critical care,14 the VPS patient registry dashboard was retooled for COVID-19 on March 18, 2020, with the first registry-reported patient. The number of facilities contributing data to the VPS COVID-19 dashboard increased from 140 on March 18, 2020, to 166 on April 6, 2020.
Estimated number of children infected with SARS-CoV-2
We estimated the cumulative total number of children infected with SARS-CoV-2 in the United States for each day from March 18 to April 6 by dividing the PICU cumulative case count (described earlier) by an adjusted pediatric criticality proportion derived from an empirical study of COVID-19 in children in China. The pediatric criticality proportion is the number of critically ill children with COVID-19 divided by the total number of children who are infected with SARS-CoV-2 (including asymptomatic individuals); the derivation is explained in the next section.
Derivation of severity and criticality proportions
We searched for the most methodologically rigorous empirical published reports that describe clinical severity of COVID-19 in children in order to derive severity proportions and criticality proportions. Preliminary US surveillance data on severity of COVID-19 published by the Centers for Disease Control and Prevention (CDC)10,11 are important but suffer from high levels of missing information that precluded their utility for our analyses. In one MMWR report,10 hospitalization status was missing for 35.8% of cases and ICU admission was missing for 50.9% of cases. A second MMWR report11 on COVID-19 in children includes valuable descriptive data on symptoms and comorbidities for some patients but is missing hospitalization status for a majority of pediatric cases.
A peer-reviewed research report on the epidemiology and clinical outcomes of 2143 pediatric patients from across China,9 with high-quality data collected and verified by the Chinese Center for Disease Control and Prevention, was published online March 16, 2020. This study included cases detected between January 16 and February 8, the period of time both before and after initial quarantine efforts had been instituted by the government of China.15,16 The clinical case definitions for severe and critical COVID-19 are shown in Supplemental Digital Content Table 1 (available at http://links.lww.com/JPHMP/A659), along with the corresponding US treatment guidelines.17 Severe illness was characterized by pneumonia and central cyanosis, and critical illness was defined as ARDS requiring mechanical ventilation.
The observed proportion of children who developed severe or critical COVID-19 in the Dong et al9 study was 10.6% of infants, 7.3% of 1- to 5-year-olds, 4.3% of 6- to 15-year-olds, and 2.8% of 16- to 17-year-olds. These severity proportions are likely to be overestimates of the true proportion of severe illness for 2 reasons. First, the case definition included both laboratory-confirmed COVID-19 (n = 731) and suspected COVID-19 (n = 1412). For all ages combined, the severity proportion was 5.8% for all cases, but only 2.9% when restricted to confirmed cases. To be conservative, we restricted our subsequent derivation of severity and criticality proportions to laboratory-confirmed COVID-19 cases.
Second, the denominator for these proportions is detected cases. Detected cases were a fraction of all infected children in the population at risk.18,19 Consequently, because the observed denominator (detected cases) underestimates the desired denominator (all infected children), the observed severity proportions overestimate the true population severity proportions.
Therefore, we adjusted the rates of severe or critical illness reported by Dong et al9 to account for the large number of undetected cases present in the population at risk. An important assumption was that testing of children in China was not only limited but also highly selective—meaning that children with more symptoms were more likely to be tested. Therefore, we conservatively assumed that ALL of the undetected cases were asymptomatic, mild, or moderate cases.
There were 2 factors in our adjustment for case underascertainment. The first factor was an estimate of the overall SARS-CoV-2 reporting rate for China, derived from a peer-reviewed spatiotemporal infection dynamics modeling study recently published in Science.18 The authors modeled 3 time periods.20 The model for the period January 24 to February 8 (the period of time with the best overlap with the Dong et al9 case series) estimated that 69% (95% CI, 66-71) of SARS-CoV-2 cases were detected by laboratory testing (see page 42 of the Li et al20 online technical supplement for these modeling results).
The second adjustment factor in our analyses corrected for lower case ascertainment in children compared with adults. On the basis of the modeling study of Verity et al,19 which incorporated age-specific analyses, we estimated that child case detection was 15% of adult case detection. The calculation for the adjusted pediatric severity proportion (the number of severely ill children with COVID-19 divided by the total number of children who were infected with SARS-CoV-2) is shown in the following equation:
Using a similar equation (see Supplemental Digital Content Figure 1, available at http://links.lww.com/JPHMP/A659), we calculated an adjusted pediatric criticality proportion = 0.00042. Finally, using the same method, we calculated age-specific adjusted severity and criticality proportions for the following age groups: less than 1 year, 1 to 5 years, 6 to 15 years, and 16 to 17 years (see Supplemental Digital Content Table 2, available at http://links.lww.com/JPHMP/A659).
Cumulative case projections for the United States
There is currently (April 2020) considerable uncertainty among infectious disease epidemiology experts in forecasting the timing and extent of the COVID-19 pandemic in the United States.21 Uncertainty results from highly limited testing of suspected COVID-19 cases and government infection control measures that have varied widely in onset, duration, and enforcement. Given these uncertainties, we chose to calculate projected COVID-19 pediatric case counts for several different CPIP scenarios. The CPIP is the percentage of all children who have ever been infected with SARS-CoV-2 for a specified time period. The CPIP is independent of detection rates and patient outcomes. It is the “true” underlying infection rate of the pediatric population.
Cumulative numbers of children with a severe or critical case of COVID-19 were calculated in 3 steps. First, estimates of the total US child population for calendar year 2020 were obtained from the US Census Bureau.22 Single-year population estimates were summed into the following categories: less than 1 year, 1 to 5 years, 6 to 15 years, and 16to 17 years. Second, age-specific population totals were multiplied by CPIP scenario factors (eg, 10%) to obtain an estimate of the number of US children infected with SARS-CoV-2 under each scenario. Third, we multiplied the age-specific number of infected children by the age-specific adjusted pediatric severity proportions and adjusted pediatric criticality proportions (see Supplemental Digital Content Table 2, available at http://links.lww.com/JPHMP/A659) to obtain the projected numbers of severe and critical cases, respectively, under each CPIP scenario. Age-specific estimates were then summed to obtain the total for children aged 0 to 17 years.
Results
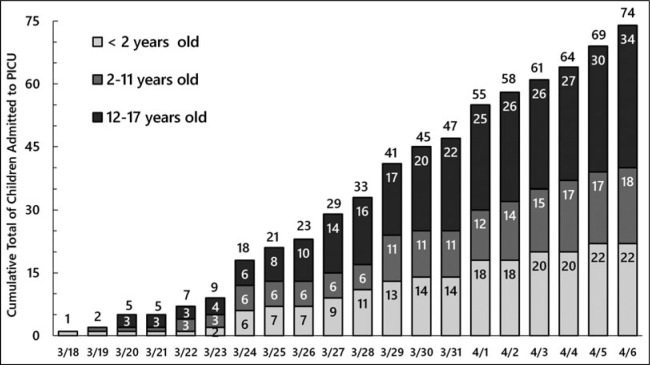
The cumulative numbers of children with confirmed COVID-19 who were admitted to a PICU in the United States from March 18 to April 6, 2020, are shown in Figure 1. By April 6, a total of 74 patients had been admitted to a PICU. These patient counts only encompass participating hospitals; the number of participating facilities increased from 140 on March 18 to 166 on April 6.
FIGURE 1.
Cumulative Number of Confirmed COVID-19 Pediatric Intensive Care Patients, United States, March 18, 2020, to April 6, 2020
The estimated numbers of children in the United States infected with SARS-CoV-2 are shown in Figure 2. Our analyses predict 2381 children in the community infected with SARS-CoV-2 for each single child who is admitted to the PICU, based on the adjusted pediatric criticality rate of 0.00042. The estimated number of infants and toddlers younger than 2 years who were infected with SARS-CoV-2 increased over the course of 19 days from 2381 on March 18 to 52 381 on April 6. Overall, there were an estimated 176 190 children aged 0 to 17 years infected with SARS-CoV-2 by April 6.
FIGURE 2.
Cumulative Estimated Number of Children Infected With SARS-CoV-2 in the United States, March 18, 2020, to April 6, 2020
The projected cumulative numbers of severely and critically ill infants and children with COVID-19, for scenarios of CPIP ranging from 0.5% (1 out of every 200 children) infected to 60% (3 out of every 5 children) infected, are shown in the Table and Figure 3. Under the lowest CPIP considered (that 1 in 200 children will become infected with SARS-CoV-2 nationwide), 991 children would become severely ill and require hospitalization. Of those, 109 would become critically ill and require PICU care. Under the highest CPIP scenario considered (3 out of 5 children infected nationwide), 118 887 children would become severely ill and 13 038 of those would become critically ill.
FIGURE 3.
Projected Numbers of Children Aged 0 to 17 Years in the United States Who Will Require Hospitalization for COVID-19 During 2020
TABLE. Projected Numbers of Children (0-17 Years) in the United States Who Will Require Hospitalization for COVID-19 During 2020, for Several Scenarios of Cumulative Pediatric Infection Proportion.
| Scenario: Percentage of All Children Infected | Projected Number of Infected Children | Projected Number of Severely Ill Children | Projected Number of Critically Ill Children | Projected Number of Severely + Critically Ill Children |
|---|---|---|---|---|
| 0.5 | 369 833 | 882 | 109 | 991 |
| 1.0 | 739 666 | 1 764 | 217 | 1 981 |
| 5.0 | 3 698 331 | 8 821 | 1 086 | 9 907 |
| 10.0 | 7 396 662 | 17 642 | 2 173 | 19 815 |
| 15.0 | 11 094 993 | 26 462 | 3 259 | 29 722 |
| 20.0 | 14 793 324 | 35 283 | 4 346 | 39 629 |
| 25.0 | 18 491 655 | 44 104 | 5 432 | 49 536 |
| 30.0 | 22 189 986 | 52 925 | 6 519 | 59 444 |
| 35.0 | 25 888 317 | 61 746 | 7 605 | 69 351 |
| 40.0 | 29 586 648 | 70 566 | 8 692 | 79 258 |
| 45.0 | 33 284 979 | 79 387 | 9 778 | 89 165 |
| 50.0 | 36 983 310 | 88 208 | 10 865 | 99 073 |
| 55.0 | 40 681 640 | 97 029 | 11 951 | 108 980 |
| 60.0 | 44 379 971 | 105 849 | 13 038 | 118 887 |
Discussion
During early 2020, SARS-CoV-2 spread throughout the United States for at least 2 months mostly unchecked, and COVID-19 cases were subsequently detected in every state. Severity and case fatality are much lower for children than for elderly persons, and this truth has created a sense of complacency that “COVID-19 is not a major concern for children's health.”23 But the devil is in the denominator. There are 74.0 million children younger than 18 years in the United States in 2020. Every 1% increase in the proportion of the US population infected with SARS-CoV-2 includes an additional 740 000 children who become infected. Even under moderate cumulative infection proportion scenarios, it is projected that there would be millions of children infected with SARS-CoV-2 and thousands of severely ill pediatric COVID-19 patients as the epidemic peaks across the nation.
The Pediatric Infectious Diseases Society and the Infectious Diseases Society of America strongly recommend hospitalization for children with severe community-acquired pneumonia, defined by the presence of respiratory distress and hypoxemia (oxygen saturation <90%).17 Children who are critically ill require PICU-level care, with continuous cardiorespiratory monitoring, mechanical ventilation, and possibly dialysis and other comorbidity supportive care. The COVID-19 PICU surveillance data from the VPS dashboard14 reported in our study show that there were already 74 critically ill children who required PICU admission by April 6, 2020.
There are only 5100 PICU beds in the entire United States, 94% of which are concentrated in major metropolitan areas.24 Federal Emergency Management Areas (FEMA) zones 8 (Mountain West), 10 (Pacific Northwest), and 1 (New England) have the lowest numbers of PICU beds per capita, at 5.6, 5.8, and 6.8 per 100 000 children, respectively.24 Hospitals will need to plan, based on their circumstances and geographic location, for the volume of pediatric-sized equipment and supplies that will be needed and for enhanced staff complements to manage a possible surge in pediatric patients who require critical care.25 Furthermore, clinical reports indicate that pediatric hospital length of stay for COVID-19 can range from 10 to 20 days, with mean hospitalization of 14 days (SD = 3).26 Under a high cumulative infection scenario of 50%, 1.4 million hospital bed-days could be required for children within the span of a few months. This demand would occur during the same period that bed-day demands for adult patients would be many times higher.
US hospitals have been advised to implement social distancing and quarantine protocols that include limiting or prohibiting visitors for adult COVID-19 patients.27 In New York, special considerations have been given to children for whom the visitor is a needed advocate and caregiver.28 However, child hospital companions may also be infected with COVID-19 themselves and will require both logistical and infection control accommodations that place an additional strain on hospital resources. To add further complexity, hospital discharge instructions must be clear and detailed for those same caregivers, as infants and young children will be unable to independently comply with home infection control and self-isolation recommendations.
The SARS-CoV-2 virus persists in fecal samples for an average of 27 days, which is 10 days longer than its persistence in respiratory tract samples.29 A separate preliminary examination of environmental contamination of hospital room air, equipment, personal objects, and toilets at the University of Nebraska Medical Center found widespread contamination even among low-acuity patients without active cough.30 These research results have grave implications for household protection measures upon discharge for children not yet toilet trained and for parent education, home infection protocols, and postepidemic school preparedness.
Underlying Factors Impacting Risk of Infection and Severity of COVID-19 in Children
To date, the majority of primary transmission of COVID-19 for children has been observed to occur within family clusters.31 Infants and young children will be at an elevated risk when they reside in environments that facilitate viral spread. Census data for 201932,33 reveal the social environmental34 vulnerability of children to an easily transmitted infectious disease. The majority (70.1%) of all children live with both parents, and 10.0% of children younger than 18 years live with at least 1 grandparent in their immediate household.32 Furthermore, only 20.1% of child households in the United States are single-child households. Most children live with other children—38.7% in 2-child households, 24.9% in 3-child households, and 16.3% in households with 4 or more children present.32 A large minority of children (38%) live in households with incomes below 200% of the federal poverty level.33 Infection risk will likely be higher for children in low-income families, with parents in blue-collar and service jobs that preclude the option of working from home. Almost one-third of all US resident children are younger than 5 years. Children 0 to 5 years of age comprise 12% of the residents of low-income public housing projects.35 Urban public housing projects typically have high population densities, with close proximity of housing units, small communal recreation and commons areas, and lack of daily preventive sanitation measures in communal areas.
Children who are medically vulnerable to both risk of infection and severity of disease include those with developmental disabilities, those with congenital birth defects, those with underlying medical conditions such as type I diabetes and cancer, and those with chronic lung diseases such as asthma that impair pulmonary function. Among 345 confirmed COVID-19 pediatric cases for whom data on underlying conditions were not missing, the CDC reported that the most common underlying conditions were chronic lung disease (11.6%), cardiovascular disease (7.2%), and immunosuppression (2.9%).11
In summary, the social environment will catalyze risk of infection and adverse COVID-19 outcomes for the most vulnerable children: the medically vulnerable, the poor, those living in large families or crowded housing, the homeless, those in uninsured and undocumented families, those living in polluted environments or in areas without reliable access to clean water, and those confined in institutions such as psychiatric hospitals, long-term care facilities, jails, prisons, and detention camps. Furthermore, consideration of the social environmental context of transmission of SARS-CoV-2 suggests that cumulative infection proportions for children will vary widely by family socioeconomic position and geographic area.
Study Strengths and Limitations
We derived adjusted pediatric severity proportions and adjusted pediatric criticality proportions from the largest clinical study of COVID-19 in children and spatiotemporal modeling studies of the COVID-19 epidemic in China. We used the adjusted pediatric criticality proportion to provide empirically derived estimates of the total number of children infected with SARS-CoV-2 through April 6, 2020, based on documented US PICU admissions of children with confirmed COVID-19. We projected cumulative numbers of severely and critically ill children with COVID-19 who will require hospitalization before the end of 2020, under several possible scenarios of the proportion of the pediatric population who will become infected with SARS-CoV-2.
Our projections estimate that 11.0% of children who require hospitalization for COVID-19 will become critically ill and require PICU admission. These projections are consistent with the findings from a preliminary US surveillance study from the CDC, which reported that among 147 children known to be hospitalized with COVID-19, 10.2% (n = 15) were admitted to a PICU. This CDC report relied on case reporting from state health departments and did not include data from the VPS PICU dashboard.11
It is possible that the conservative criticality proportions we derived from the Chinese empirical data are an underestimate of the true pediatric criticality proportion experienced in China. This is due to the fact that we excluded all cases of pediatric COVID-19 that were clinically diagnosed but not confirmed by laboratory testing in the Dong et al9 study. To the extent that any of those suspected cases were true cases, the criticality proportion estimates used in our study are underestimates.
Implications for Policy & Practice
We undertook these analyses to alert government officials, policy makers, and the pediatric intensive care community that there is a likelihood of capacity challenges to hospitals and health care providers over the next few months of the COVID-19 pandemic in the United States.
A key point is that for every documented admission of a single child with COVID-19 to a PICU in the United States, our analyses conservatively estimate that there are 2381 children in the community infected with SARS-CoV-2. As of April 6, 2020, there were an estimated 176 190 SARS-CoV-2–infected children nationwide.
One well-regarded epidemic modeling study found that population infection rates could rise as high as 80% in the United States in the absence of effective and persistent nationwide infection control measures (eg, school, retail, and restaurant closures, event cancellations, and stay-at-home orders).13
Under the highest CPIP scenario included in our study (60%), we projected that 118 887 children would require hospitalization with severe COVID-19, and 13 038 of those hospitalized children would become critically ill and require PICU admission.
In interpreting our findings from a health care system capacity perspective, it is important to underscore that the rate at which the population becomes infected is critical, underscoring the importance of effective mitigation strategies.
Our recommendations are as follows:
Hospitals, PICUs, emergency medical services systems, pediatricians, local health departments, and other stakeholders should rush to completion county- and city-specific plans to care for severe pediatric cases of COVID-19, including transportation and regionalization plans.
National pediatric medicine and maternal and child health organizations should consider the precautionary principle36 when updating their official recommendations to parents about the protection of infants and very young children from COVID-19.
Public health leaders should rapidly develop and disseminate detailed parent education materials on household infection control practices, specifically for multichild and multigenerational families.
Plans for early detection, treatment, and isolation of children with COVID-19 should ensure timely testing of children and their household contacts, recognizing the wide variability in COVID-19 symptoms in children.11 Testing to identify confirmed cases can greatly aid in epidemiologic case-containment efforts, minimizing household and child-to-child spread. A larger denominator of tested children will also permit better US-based estimates of case severity and case fatality.37
Current real-time surveillance data on confirmed COVID-19 cases for the United States as whole are inadequate. All state health departments and the CDC should begin reporting confirmed COVID-19 cases in age-specific tables, using the standard 5-year age groups for health surveillance. These data should be publicly available and updated daily. The Florida Department of Health COVID-19 Dashboard is one of several exemplary models, with detailed demographic data provided for cases at both the state and county levels.38
Supplementary Material
Footnotes
The authors express their gratitude to 4 anonymous peer reviewers whose thoughtful suggestions helped them greatly improve the final version of this article. Any errors that remain are the sole responsibility of the authors.
Conflict of Interests: None.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (http://www.JPHMP.com).
References
- 1.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. [DOI] [PubMed] [Google Scholar]
- 2.Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy [published online ahead of print March 23, 2020]. JAMA. 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 3.Korean Society of Infectious Diseases; Korean Society of Pediatric Infectious Diseases; Korean Society of Epidemiology; Korean Society for Antimicrobial Therapy; Korean Society for Healthcare-associated Infection Control and Prevention; Korea Centers for Disease Control and Prevention. Report on the epidemiological features of coronavirus disease 2019 (COVID-19) outbreak in the Republic of Korea from January 19 to March 2, 2020. J Korean Med Sci. 2020;35(10):e112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hein A. Is coronavirus a threat to children? How to keep them safe. https://www.foxnews.com/health/are-children-at-risk-for-coronavirus. Published March 13, 2020. Accessed March 25, 2020.
- 5.Centers for Disease Control and Prevention. Coronavirus COVID-19 frequently asked questions: COVID-19 and children. https://www.cdc.gov/coronavirus/2019-ncov/faq.html. Published 2020. Accessed March 25, 2020.
- 6.Intermountain Healthcare. COVID-19 and children: what you should know. https://intermountainhealthcare.org/blogs/topics/live-well/2020/03/covid-19-and-children-what-you-should-know/. Published 2020. Accessed March 25, 2020.
- 7.Liu W, Zhang Q, Chen J, et al. Detection of Covid-19 in children in early January 2020 in Wuhan, China. N Engl J Med. 2020;382(14):1370–1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lu X, Zhang L, Du H, et al. SARS-CoV-2 infection in children [published online ahead of print March 18, 2020]. N Engl J Med. 10.1056/NEJMc2005073. [Google Scholar]
- 9.Dong Y, Mo X, Hu Y, et al. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China [published online ahead of print March 16, 2020]. Pediatrics. 10.1542/peds.2020-0702. [Google Scholar]
- 10.CDC COVID-19 Response Team. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12-March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(12):343–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.CDC COVID-19 Response Team. Coronavirus disease 2019 in children—United States, February 12-April 2, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(14):422–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Prem K, Liu Y, Russell TW, et al. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study [published online ahead of print March 25, 2020]. Lancet Public Health. 10.1016/S2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ferguson NM, Laydon D, Nedjati-Gilani G, et al. Report 9: Impact of Non-pharmaceutical Interventions (NPIs) to Reduce COVID-19 Mortality and Healthcare Demand. London, England: Imperial College London; 2020:1–20. [Google Scholar]
- 14.Virtual Pediatric Systems (VPS). COVID-19 Data Dashboard: North American pediatric ICUs. https://covid19.myvps.org. Published 2020. Accessed April 6, 2020.
- 15.@chinadaily. Public #transportation such as bus, subway, ferry and long-distance bus in Wuhan will be temporarily closed since 10am Thursday. All flights and trains departed from #Wuhan will be temporarily cancelled to reduce risk of spread of the new. virus, local govt says. #coronavirus. https://twitter.com/ChinaDaily/status/1220052882596286465/photo/1. Posted January 22, 2020.
- 16.Qin A, Wang V. Wuhan, Center of coronavirus outbreak, is being cut off by Chinese authorities. New York Times. January 22, 2020. https://www.nytimes.com/2020/01/22/world/asia/china-coronavirus-travel.html. Accessed March 25, 2020.
- 17.Bradley JS, Byington CL, Shah SS, et al. The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53(7):e25–e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li R, Pei S, Chen B, et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2) [published online ahead of print March 16, 2020]. Science. 10.1126/science.abb3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Verity R, Okell LC, Dorigatti I, et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis [published online ahead of print March 30, 2020]. Lancet Infect Dis. 10.1016/S1473-3099(20)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li R, Pei S, Chen B, et al. Supplementary materials for substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2). Science. https://science.sciencemag.org/content/sci/suppl/2020/03/13/science.abb3221.DC1/abb3221_Li_SM_rev.pdf. Published March 16, 2020. Accessed March 25, 2020. [DOI] [PMC free article] [PubMed]
- 21.Wan W, Johnson C. America's most influential coronavirus model just revised its estimates downward. But not every model agrees. Washington Post. April 7, 2020. https://www.washingtonpost.com/health/2020/04/06/americas-most-influential-coronavirus-model-just-revised-its-estimates-downward-not-every-model-agrees/. Accessed April 7, 2020. [Google Scholar]
- 22.US Census Bureau. Mid-year five year age groups and sex. https://www.census.gov/programs-surveys/international-programs/data.html. Published 2020. Accessed March 25, 2020.
- 23.Newkirk V. The kids aren't all right. The Atlantic. March 24, 2020. https://www.theatlantic.com/health/archive/2020/03/what-coronavirus-will-do-kids/608608. Accessed March 25, 2020.
- 24.Horak RV, Griffin JF, Brown AM, et al. Growth and changing characteristics of pediatric intensive care 2001-2016. Crit Care Med. 2019;47(8):1135–1142. [DOI] [PubMed] [Google Scholar]
- 25.Halpern NA, Tan KS. United States ICU resource availability for COVID-19. https://www.sccm.org/getattachment/Blog/March-2020/United-States-Resource-Availability-for-COVID-19/United-States-Resource-Availability-for-COVID-19.pdf?lang=en-US. Published March 25, 2020. Accessed March 25, 2020.
- 26.Qiu H, Wu J, Hong L, Luo Y, Song Q, Chen D. Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID-19) in Zhejiang, China: an observational cohort study [published online ahead of print March 25, 2020]. Lancet Infect Dis. 10.1016/S1473-3099(20)30198-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention. Interim guidance for healthcare facilities: preparing for community transmission of COVID-19 in the United States. https://www.cdc.gov/coronavirus/2019-ncov/healthcare-facilities/guidance-hcf.html. Published 2020. Accessed March 25, 2020.
- 28.New York State Health Department. Health advisory: COVID-19 guidance for hospital operators regarding visitation. Updated guidance regarding obstetrical and pediatric settings. https://coronavirus.health.ny.gov/system/files/documents/2020/03/doh_covid19_obpedsvisitation_032720.pdf. Published 2020. Accessed March 21, 2020.
- 29.Wu Y, Guo C, Tang L, et al. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples [published online ahead of print March 19, 2020]. Lancet Gastroenterol Hepatol. 10.1016/S2468-1253(20)30083-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Santarpia JL, Rivera DN, Herrera V, et al. Transmission potential of SARS-CoV-2 in viral shedding observed at the University of Nebraska Medical Center. medRxiv. March 26, 2020. 10.1101/2020.03.23.20039446. [Google Scholar]
- 31.Qian G, Yang N, Ma AHY, et al. A COVID-19 transmission within a family cluster by presymptomatic infectors in China [published online ahead of print March 23, 2020]. Clin Infect Dis. 10.1093/cid/ciaa316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.US Census Bureau. America's families and living arrangements. Table C2. Household relationship and living arrangements of children under 18 years, by age and sex. https://www.census.gov/data/tables/2019/demo/families/cps-2019.html. Published 2019. Accessed March 25, 2020.
- 33.US Census Bureau. America's families and living arrangements. Table C8. Poverty status, food stamp receipt, and public assistance for children under 18 years by selected characteristics. https://www.census.gov/data/tables/2019/demo/families/cps-2019.html. Published 2019. Accessed March 24, 2020.
- 34.Barnett E, Casper M. A definition of “social environment. Am J Public Health. 2001;91(3):465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.US Department of Housing and Urban Development. Resident characteristics report, public housing, national level. https://pic.hud.gov/pic/RCRPublic/rcrmain.asp. Published 2020. Accessed April 4, 2020.
- 36.Richter ED, Laster R. The Precautionary principle, epidemiology and the ethics of delay. Int J Occup Med Environ Health. 2004;17(1):9–16. [PubMed] [Google Scholar]
- 37.Lipsitch M, Swerdlow DL, Finelli L. Defining the epidemiology of Covid-19—Studies Needed. N Engl J Med. 2020;382(13):1194–1196. [DOI] [PubMed] [Google Scholar]
- 38.Florida Department of Health. Florida's COVID-19 Data and Surveillance Dashboard. https://experience.arcgis.com/experience/96dd742462124fa0b38ddedb9b25e429. Published 2020. Accessed March 27, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.