Abstract
One of the most exciting developments in antiviral research has been the discovery of the direct-acting antivirals (DAAs) that effectively cure chronic hepatitis C virus (HCV) infections. Based on more than 100 clinical trials and real-world studies, we provide a comprehensive overview of FDA-approved therapies and newly discovered anti-HCV agents with a special focus on drug efficacy, mechanisms of action, and safety. We show that HCV drug development has advanced in multiple aspects: (i) interferon-based regimens were replaced by interferon-free regimens; (ii) genotype-specific drugs evolved to drugs for all HCV genotypes; (iii) therapies based upon multiple pills per day were simplified to a single pill per day; (iv) drug potency increased from moderate (∼60%) to high (>90%) levels of sustained virologic responses; (v) treatment durations were shortened from 48 to 12 or 8 weeks; and (vi) therapies could be administered orally regardless of prior treatment history and cirrhotic status. However, despite these remarkable achievements made in HCV drug discovery, challenges remain in the management of difficult-to-treat patients.
Keywords: Direct-acting antivirals, NS3/4A drugs, NS5A drugs, NS5B drugs
Abbreviations: BID, twice a day; CDC, Centers for Disease Control and Prevention; DAA, direct-acting antiviral; EC50, half maximal effective concentration; FDA, U S Food and Drug Administration; GT, genotype; HBV, hepatitis B virus; HCC, hepatocellular carcinoma; HCV, hepatitis C virus; HIV, human immunodeficiency virus; IC50, half maximal inhibitory concentration; PegIFNα, pegylated interferon alfa; QD, once a day; RBV, ribavirin; SVR12, sustained virologic response after the treatment for 12 weeks; SVR24, sustained virologic response after the treatment for 24 weeks; TID, three times a day; WHO, World Health Organization
Highlights
-
•
HCV genotype-specific drugs evolve to pan-genotypic drugs.
-
•
Drug potency increases from moderate (∼60%) to high (>90%) levels of sustained virologic response.
-
•
Treatment durations are shortened from a 48-week to 12-week or 8-week period.
-
•
HCV therapies based upon multiple pills per day are simplified to a single pill per day.
-
•
HCV therapies are administered orally regardless of prior treatment history and cirrhotic status.
1. Introduction
Over the past two decades, tremendous attempts have been made to discover antiviral drugs that effectively treat hepatitis C virus (HCV) infection (De Clercq, 2015, De Clercq, 2012, De Clercq, 2014, Welzel et al., 2014, De Clercq and Li, 2016). The first generation of FDA-approved HCV drugs includes: interferon alfacon-1 (approval year: 1997, discontinued in 2013 due to severe adverse events), ribavirin (1998), pegylated interferon alfa-2b (2001), and pegylated interferon alfa-2a (2002). These drugs had low cure rates and may cause severe adverse events (Manns et al., 2006); yet they have been the only standard-of-care treatments over a decade and are still popular in several countries. Subsequently, direct-acting antivirals (DAAs) represented a breakthrough in in vitro experiments and in clinical trials. In May 2011, telaprevir and boceprevir became the first FDA-approved drugs in the DAA class. The advent of DAAs marks a new era of anti-HCV drugs that directly target HCV proteins, offering promising cure rates and minimum adverse events. Similar to cocktail therapies against human immunodeficiency virus, combination therapies that target different stages of the HCV life cycle have been conceived to avoid cross-resistance. Importantly, their cure rates could attain more than 90% in clinical trials and real-world cohorts. Forthcoming therapies are endowed with higher cure rates, shorter treatment duration, lesser side effects, while being based upon all-oral regimens.
This review aims to summarize the latest trend of HCV drug development, focusing on FDA-approved therapies and newly discovered agents against HCV genotype 1 to 6 infections. We first provide a general overview of HCV infections. Subsequently, we summarize the approved HCV drugs and highlight their efficacy in clinical trials. Recent development of new agents is described. Challenges in HCV drug development are discussed at the end. To endorse this review, movies and teaching slides that highlight HCV drug actions are available from our online platform (http://www.virusface.com).
2. Literature selection
Here, our procedure for literature selection is described. We searched literature in PubMed using the keywords of HCV drugs within the publication period from 2013/01/01 to 2016/10/01. To search the most recent publications that are unavailable in PubMed, similar queries were also performed by visiting the websites of eleven journals (NEJM, JAMA, Lancet, Lancet infectious diseases, Gut, Clinical Infectious Diseases, Gastroenterology, Hepatology, Journal of hepatology, The American Journal of Gastroenterology, Annals of Internal Medicine). Only clinical trials in the phase 2, 3 and 4 stages were considered, while case reports were excluded from our literature review because of their small samples and rare subjects. We also extracted information about clinical trials from ClinicalTrials.gov (http://www.clinicaltrials.gov/) or the European Clinical Trials Database (EudraCT, https://eudract.ema.europa.eu/index.html). Clinical studies in the drug labeling of the FDA (https://www.accessdata.fda.gov) were also included in our literature search. Three exclusion criteria were undertaken. First, data from the meta-analysis or reports that summarized clinical trials in other publications were not considered so as to avoid duplicates. Second, publications (e.g. HCV-TARGET (Terrault et al., 2016), real-world study (Backus et al., 2016)) that reported the coinfections with HCV and other infectious diseases (e.g. HIV, HBV) were not collected because coinfections were beyond the focus of our review. Third, in order to highlight the SVR rates of antiviral drugs in each HCV genotype, only publications that clearly addressed SVR rates of HCV therapies in individual genotypes were summarized. Moreover, we communicated with every corresponding author if SVR rates in certain patient groups were not addressed in a publication. By doing so, we managed to obtain SVR data from most publications except for a phase 2 study (Osinusi et al., 2013), the ANRS C023 CUPILT study (Coilly et al., 2016), the A1444040 study (Sulkowski et al., 2014a), the C-EDGE Head-2-Head study (Sperl et al., 2016), and the C-EDGE treatment-experienced study (Kwo et al., 2017).
3. Overview of hepatitis C virus
3.1. HCV origin, epidemiology, and diversity
Hepatitis C virus is a hepacivirus in the Flaviviridae family, and it was first discovered from the serum of a person with non-A, non-B hepatitis in 1989 (Choo et al., 1989, Kuo et al., 1989). Now, HCV can be found in worldwide populations (Shepard et al., 2005), while the immediate sources of HCV associated with its pandemic spread have been traced to the circulation in Central and West sub-Saharan Africa and South and Southeast Asia over hundreds of years (Simmonds, 2013). Although its origin remains unclear, HCV might have originated from zoonotic sources such as non-human primates (e.g. monkeys, apes) and mammals (e.g. dogs, horses) (Simmonds, 2013). As of today, HCV has been recognized as one of the most lethal infectious diseases next to measles, influenza, respiratory syncytial virus, rotavirus, hepatitis B, and human immunodeficiency virus (Mortality, 2016, Disease et al., 2016). According to the WHO global health survey, 130 to 150 million people are currently living with HCV, causing approximately 700,000 deaths every year. Importantly, more than 95% of HCV-infected patients are unaware of their status in worldwide populations (Cox, 2015).
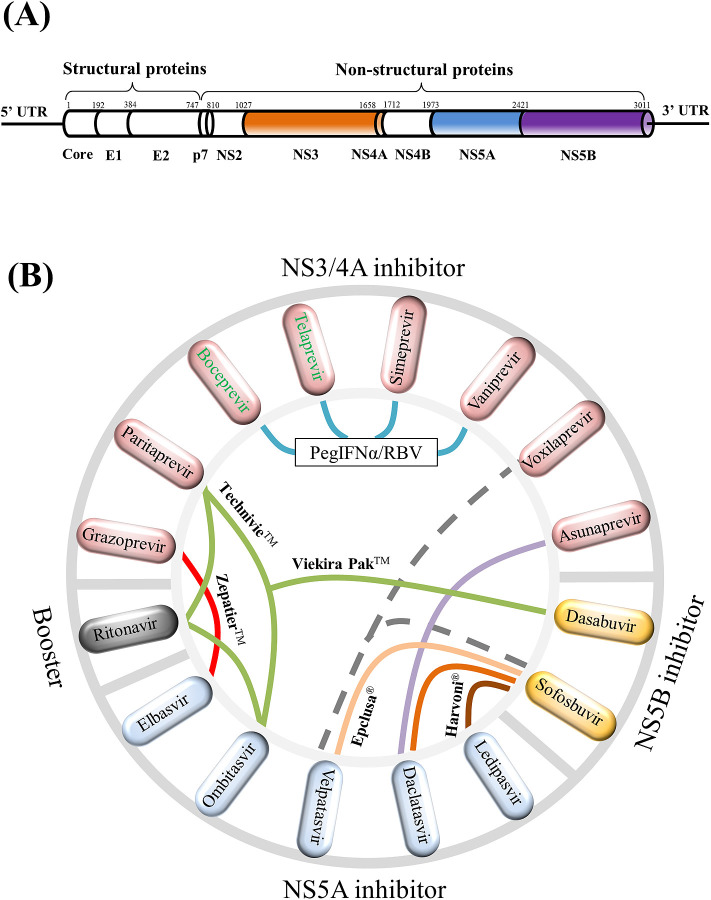
A single HCV particle is approximately 68 nm (range: 45–86 nm) in diameter (Catanese et al., 2013), and it contains a linear positive-sense single-stranded RNA genome encoding 10 viral proteins (Moradpour and Penin, 2013) (Fig. 1 A). Due to the sequence variation of different HCV strains, 7 genotypes (genotypes 1 to 7) have been recognized and their global prevalence is unequally distributed. Among 7 HCV genotypes, genotype 1 (46.2%) and 3 (30.1%) dominate the global infections; genotypes 2, 4, and 6 circulate in approximately 22.8% of HCV infections; genotype 5 accounts for the remaining less than 1% (Messina et al., 2015); genotype 7 has been identified so far in very few patients originating from Central Africa (Murphy et al., 2015). It is worth mentioning that the nucleotide diversity of HCV genomes is approximately 32.4% between HCV genotypes, and 14.6% within HCV genotypes (Cuypers et al., 2015). An average of 1.3 × 1012 virions are produced per day in each HCV-infected patient (Neumann et al., 1998). Moreover, HCV evolves so fast that the HCV mutation rate is approximately 1.92 × 10−3 nucleotide substitutions per genomic site per year (Ogata et al., 1991).
Fig. 1.
HCV genome structure and schematic view of HCV combination drugs. (A) HCV genome structure. In the length of approximately 3011 amino acids, the HCV genome codes for three structural proteins (core, E1, E2) and seven non-structural proteins (p7, NS2, NS3, NS4A, NS4B, NS5A, NS5B) whose amino acid positions are mapped accordingly. The 5′ untranslated region (5′ UTR) and the 3′ untranslated region (3′ UTR) are also indicated. Approved antiviral agents directly target to NS3/4A, NS5A, and NS5B for effective inhibition of HCV replications. (B) A total of 15 NS3/4A, NS5A, NS5B compounds plus ritonavir are displayed in the circle. Colored links in the center visualize 13 drug combinations: (i) boceprevir (Victrelis®) + PegIFNα/RBV, (ii) telaprevir (Incivek®) + PegIFNα/RBV, (iii) sofosbuvir (Sovaldi®) + PegIFNα/RBV, (iv) simeprevir (Olysio®) + PegIFNα/RBV, (v) ledipasvir + sofosbuvir (Harvoni®), (vi) ombitasvir + paritaprevir + ritonavir + dasabuvir (Viekira Pak™), (vii) ombitasvir + paritaprevir + ritonavir (Technivie™), (viii) daclatasvir (Daklinza™) + sofosbuvir (Sovaldi®), (ix) elbasvir + grazoprevir (Zepatier™), (x) sofosbuvir + velpatasvir (Epclusa®), (xi) vaniprevir (Vanihep®) + PegIFNα/RBV, (xii) asunaprevir (Sunvepra®) + daclatasvir (Daklinza®), (xiii) voxilaprevir + velpatasvir + sofosbuvir. Notably, (i) to (x) were approved by the FDA and could be used with or without ribavirin; (xi) and (xii) were approved in Japan; and (xiii) is currently under assessment by the FDA. Two discontinued drugs boceprevir and telaprevir are indicated by green texts. This figure shows that HCV combination drugs are composed of anti-HCV inhibitors from different drug classes.
3.2. HCV clinical syndrome and pathogenesis
As a blood-borne virus, HCV can be transmitted by blood transfusions, needle sharing, sexual contacts, or maternal transmissions. Although HCV can circulate in many human organs, it infects predominately hepatocytes in the liver and evades the host innate and adaptive immune system (Rehermann, 2009). With an incubation period of 2–12 weeks, HCV infection begins with an acute phase that usually goes undiagnosed, during which symptomatic infections (10%–15%) and asymptomatic infections (85%–90%) are observed (Maheshwari et al., 2008). Approximately, 25%–52% of symptomatic infections and 10%–15% of asymptomatic infections undertake spontaneous viral clearance, indicating that HCV is cleared from HCV-infected patients by specific immune responses (Maheshwari et al., 2008). If not cleared, acute HCV evolves into chronic HCV. Without proper treatment, patients with chronic HCV are threatened by serious complications such as cirrhosis, liver cancer, and liver failure (Thrift et al., 2017). Of note, liver damage is the consequence of long-lasting inflammation when host immune responses are activated to fight HCV infections (Antonelli et al., 2008).
According to Centers for Disease Control and Prevention (CDC), HCV-related cirrhosis is often observed in 5%–20% of patients with chronic infections over a period of 20–30 years. Advanced cirrhosis eventually causes end-stage liver disease and liver failure with debilitating symptoms such as hepatic encephalopathy, portal hypertension, hepatorenal syndrome, and hepatocellular carcinoma (Ge and Runyon, 2016). As the most common type of liver cancer, hepatocellular carcinoma can be found in 1%–3% of HCV-infected patients over three decades (El-Serag, 2012). Nevertheless, successful anti-HCV treatments can reduce the overall mortality and the risk of death among HCV patients with compensated cirrhosis (Nahon et al., 2016).
3.3. HCV proteins and drug targets
HCV genome encodes 3 structural proteins (core, E1, E2) and 7 nonstructural proteins (p7, NS2, NS3, NS4A, NS4B, NS5A, NS5B) (Fig. 1A). Similar to genome-wide protein interactions in human immunodeficiency virus (Li and De Clercq, 2016), HCV proteins cooperatively play multiple functions that take part in different stages of the viral life cycle (Dubuisson and Cosset, 2014, Bartenschlager et al., 2013). Major functions of HCV proteins are briefly described herein. (i) The core protein is the key element to form viral nucleocapsid that encapsulates HCV RNA genome inside viral particles. (ii) Envelope glycoproteins E1 and E2 constitute a non-covalent complex that takes part in receptor binding and fusion processes during the viral entry. (iii) The non-structural protein p7 in the form of hexamers has a cation channel activity and plays multiple roles in viral particle maturation and release (Scull et al., 2015). (iv) The NS2-NS3 autoprotease cleaves the link between NS2 and NS3 in the same polyprotein during the HCV polyprotein processing. (v) NS3 protease with its cofactor NS4A in a structural complex cleaves four links (NS3-NS4A, NS4A-NS4B, NS4B-NS5A, NS5A-NS5B) in the polyprotein to release NS3, NS4A, NS4B, NS5A and NS5B for their maturation. (vi) NS4B induces the formation of the membranous web which serves as the principle site of viral replication and assembly (Egger et al., 2002, Gosert et al., 2003). (vii) The NS5A phosphoprotein is a replicase factor that interacts with many other viral and host proteins to regulate HCV replication (Bartenschlager et al., 2013). (viii) The NS5B polymerase is the key enzyme that synthesizes viral RNA to produce new viral particles. Overall, ten HCV proteins play important roles in the viral life cycle, making them potential drug targets to inhibit HCV replication and infection. More details about HCV life cycle can be found in other reviews (Bartenschlager et al., 2013, Moradpour et al., 2007, Scheel and Rice, 2013, Lindenbach and Rice, 2005, Bartenschlager et al., 2011).
Discovery of the multifunctional aspects of HCV proteins has shed light on the novel mechanisms of anti-HCV drugs. Known drug targets include one non-structural protein (NS5A) and two HCV enzymes (NS3/4A, NS5B) (De Clercq, 2014). Three drug targets therefore offer ideal drug binding pockets for the design of HCV combination therapies, leading to the tremendous success of pan-genotypic therapies (e.g. Epclusa®) with more than 90% of sustained virologic response. Approved DAA combination therapies are commonly composed of two or three compounds that inhibit either NS3/4A, NS5A, or NS5B with different mechanism of drug action (Fig. 1). In comparison to individual compounds, combination therapies offer much higher efficacy to inhibit HCV infections.
Four classes of drug actions have been discovered. First, NS3/4A inhibitors (e.g. asunaprevir, boceprevir, telaprevir, paritaprevir, grazoprevir, simeprevir, vaniprevir, voxilaprevir) can inhibit the enzymatic activity of NS3/4A. Second, NS5A inhibitors (e.g. daclatasvir, ledipasvir, ombitasvir, elbasvir, velpatasvir) might inhibit replication complex formation at the endoplasmic reticulum and sequester NS5A in lipid droplets to inhibit virus formation and release (Nettles et al., 2014). Without affecting the stability and dimerization of NS5A, NS5A inhibitors not only block HCV RNA synthesis at the stage of membranous web biogenesis (Berger et al., 2014), but also impair viral assembly by inhibiting the delivery of HCV genomes to assembly sites (Boson et al., 2017). In spite of their high potency, NS5A inhibitors slowly inhibit HCV RNA synthesis in comparison to HCV protease or polymerase inhibitors (McGivern et al., 2014). It is also worth mentioning that the cooperation interaction between pairs of NS5A inhibitors may enhance drug resistance barrier and restore antiviral activity against NS5A resistance variants (Sun et al., 2015). Third, nucleotide inhibitors (e.g. sofosbuvir triphosphate) bind to the catalytic site of NS5B and compete with incoming nucleoside triphosphates to interrupt the RNA synthesis. Fourth, non-nucleotide inhibitors (e.g. dasabuvir) bind to the allosteric binding pockets outside the NS5B catalytic site based on the non-competitive mechanisms of action that inhibit the RNA synthesis (Gotte and Feld, 2016). In addition to these known drug binding sites, alternative drug targets in other viral and host proteins have been explored by experimental drugs. The following sections provide more details about the approved and experimental drugs.
4. Approved antiviral therapies
Interferon alfacon-1 (Infergen®) was the first FDA-approved drug against HCV infections. Later, ribavirin (Copegus®, Rebetol®, Virazole®), pegylated interferon alfa 2b (PegIntron®, Intron®-A), and pegylated interferon alfa 2a (Pegasys®, Roferon®-A) joined to combat HCV infections. Before 2011, interferon and ribavirin were the standard of care therapies, whereas they offered rather low clinical effectiveness and caused serious side effects (see reviews elsewhere (Selzner et al., 2011, Aghemo et al., 2010, Webster et al., 2009)). The advent of DAAs opened an era to potentially cure HCV in most patients (De Clercq, 2015, De Clercq, 2012, De Clercq, 2014). Between January 2011 and November 2016, there were ten therapies approved by the FDA (Table 1 ), as well as two approved drugs (asunaprevir + daclatasvir, vaniprevir + ribavirin + PegIFNα) in Japan. Due to severe side effects and commercial reasons, telaprevir and boceprevir have been discontinued.
Table 1.
FDA-approved HCV therapies with their recommended use.
| Drug name | FDA-approved HCV therapy | Genotype | Date approved |
|---|---|---|---|
| Victrelis® | PegIFNα/RBV for 4w + 200 mg boceprevir TID plus PegIFNα/RBV for 44 weeks. | GT-1 | May 2011 |
| Incivek® | 1125 mg telaprevir BID plus PegIFNα/RBV for 12w + PegIFNα/RBV for 12w or 36w. | GT-1 | May 2011 |
| Sovaldi® | 400 mg sofosbuvir QD + ribavirin for 12w or 24w; or 400 mg sofosbuvir QD + PegIFNα/RBV for 12w. | GT-1, GT-2, GT-3, GT-4 | Dec. 2013 |
| Olysio® | 150 mg simeprevir + 400 mg sofosbuvir QD for 12w or 24w; 150 mg simeprevir QD for 12w + PegIFNα/RBV for 24w or 48w. | GT-1, GT-4 | Nov. 2013 |
| Harvoni® | A fixed-dose combination tablet of 90 mg ledipasvir + 400 mg sofosbuvir, QD with or without ribavirin for 12 or 24 weeks. | GT-1, GT-4, GT-5, GT-6 | Oct. 2014 |
| Viekira Pak™ | Two fixed-dose combination tablets of 12.5 mg ombitasvir + 75 mg paritaprevir + 50 mg ritonavir QD plus 250 mg dasabuvir BID with or without ribavirin for 12 or 24 weeks. | GT-1 | Dec. 2014 |
| Technivie™ | Two fixed-dose combination tablets of 12.5 mg ombitasvir + 75 mg paritaprevir + 50 mg ritonavir with or without ribavirin, QD for 12 weeks. | GT-4 | July 2015 |
| Daklinza™ + Sovaldi® | 60 mg daclatasvir QD + 400 mg sofosbuvir QD with or without ribavirin for 12 weeks. | GT-1, GT-3 | July 2015 |
| Zepatier™ | A fixed-dose combination tablet of 100 mg grazoprevir QD + 50 mg elbasvir QD for 12 weeks, or with ribavirin for 12 or 16 weeks. | GT-1, GT-4 | Jan. 2016 |
| Epclusa® | A fixed-dose combination tablet of 400 mg sofosbuvir + 100 mg velpatasvir with or without ribavirin, QD for 12 weeks. | GT-1 to GT-6 | June 2016 |
Victrelis® and Incivek® were discontinued. Except for Technivie™, all the HCV therapies above could be applied to patients with cirrhosis. Sunvepra and Vanihep approved in Japan are not listed in Table 1.
It is worth mentioning that treatment success of HCV therapies is commonly evaluated by the sustained virologic response (SVR) at the post-treatment for 8 weeks (SVR8), 12weeks (SVR12) or 24 weeks (SVR24). For instance, SVR rates may vary profoundly when HCV therapies are used against different genotypes, patients with or without compensated cirrhosis, and patients experienced with or without previous treatments. Resistance aspects of HCV DAAs also play a role in the treatment success (Cuypers et al., 2016, Sarrazin, 2016). Therefore, American and European guidelines for Hepatitis C treatments have been proposed for different scenarios (AASLD/IDSA HCV Guidance Panel, 2015, European Association for Study of Liver, 2015). In this section, we aimed at summarizing the effectiveness of FDA-approved therapies against HCV mono-infections in clinical trials or real-world studies. Chemical formulas of the approved NS3/4A inhibitors, NS5A inhibitors, NS5B nucleoside inhibitors, and NS5B non-nucleoside inhibitors are highlighted in Fig. 2, Fig. 3, Fig. 4, Fig. 5 , respectively.
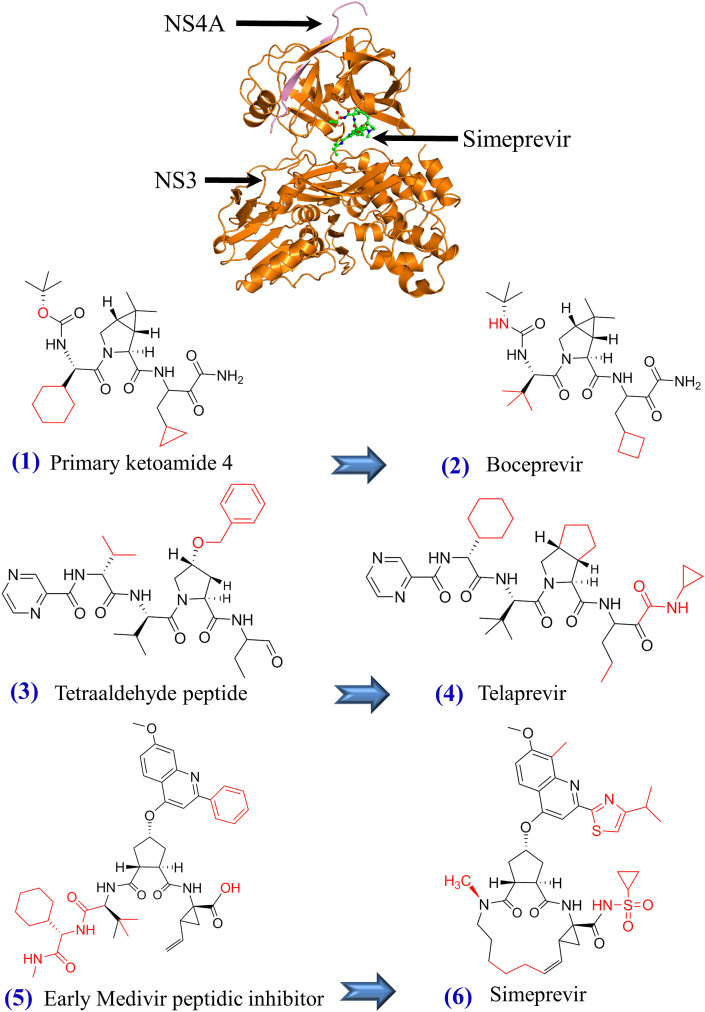
Fig. 2.
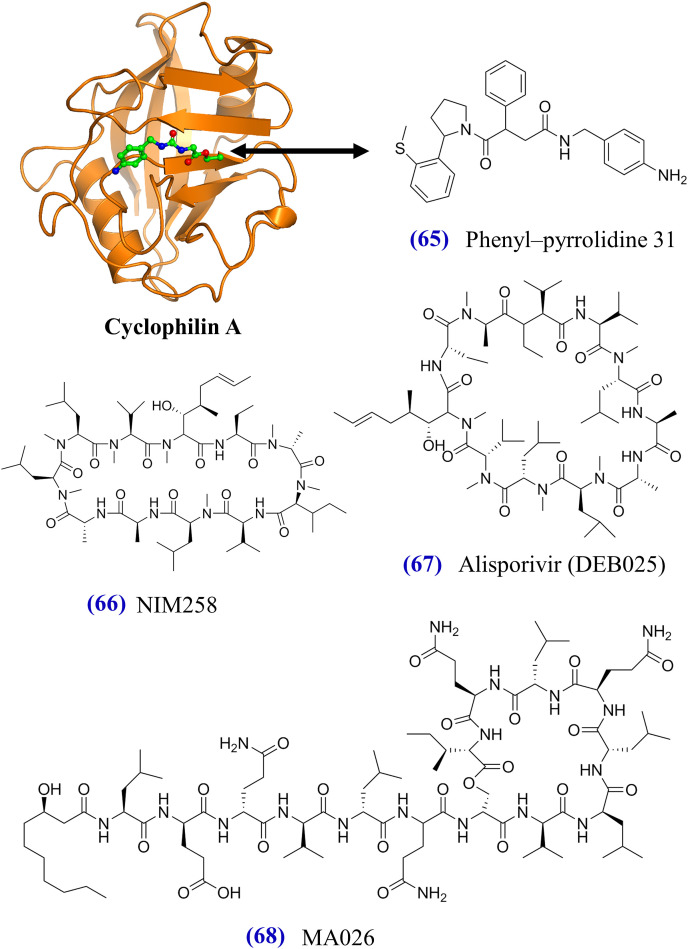
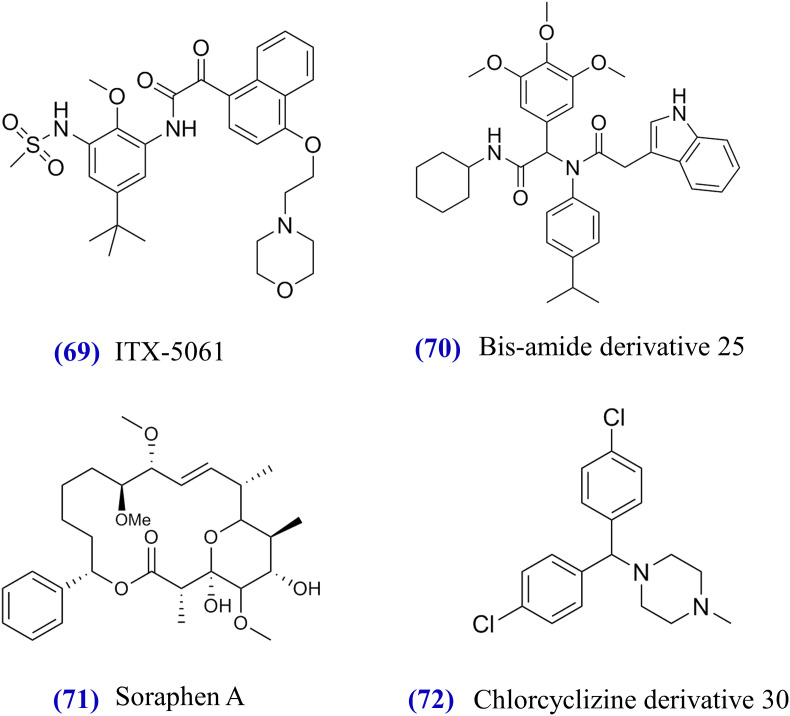
Tertiary structure of HCV NS3/4A protease and structural formulas of approved or experimental NS3/4A inhibitors from (1) to (18). The tertiary structure of NS3/4A protease in complex with simeprevir (PDB codes: 3KEE and 4B76) is shown on top. HCV NS3 and NS4A proteins are displayed in orange and pink, respectively. Beneath the NS3/4A protein, chemical structures of approved and experimental NS3/4A inhibitors (Table 20) are demonstrated. Blue arrows indicate the optimization from initial compounds to FDA-approved compounds such as boceprevir (Njoroge et al., 2008), telaprevir (Kwong et al., 2011), simeprevir (Rosenquist et al., 2014), and grazoprevir (Harper et al., 2012, Liverton et al., 2008). Red structures indicate the differences between initial compounds and FDA- approved compounds.
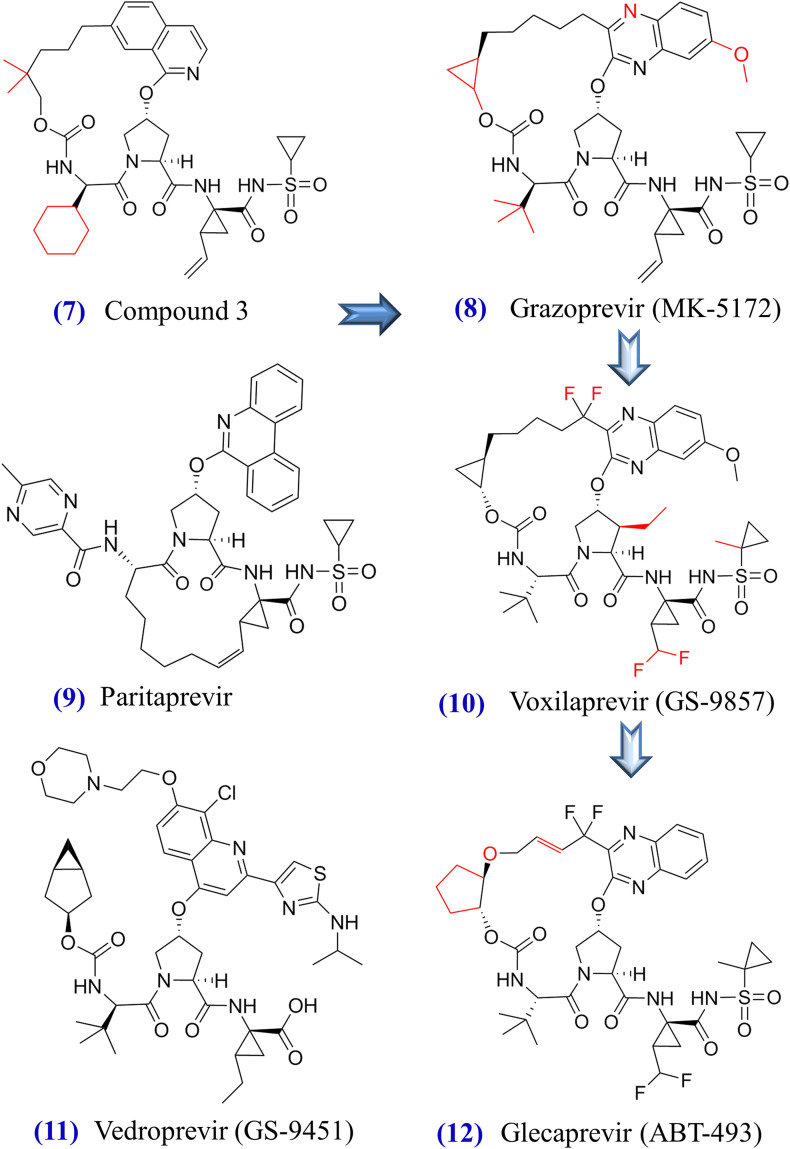
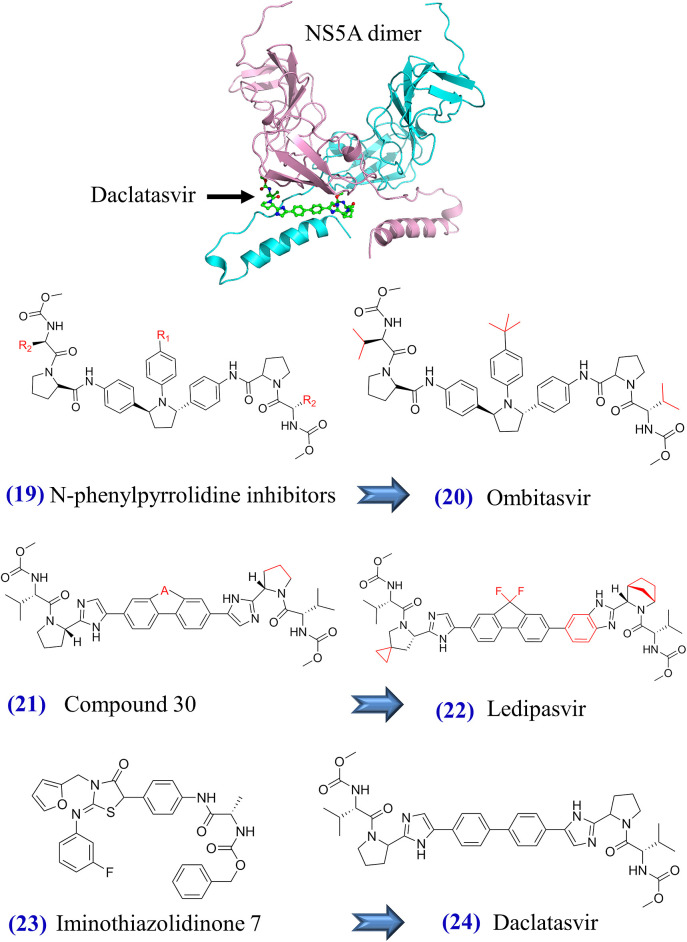
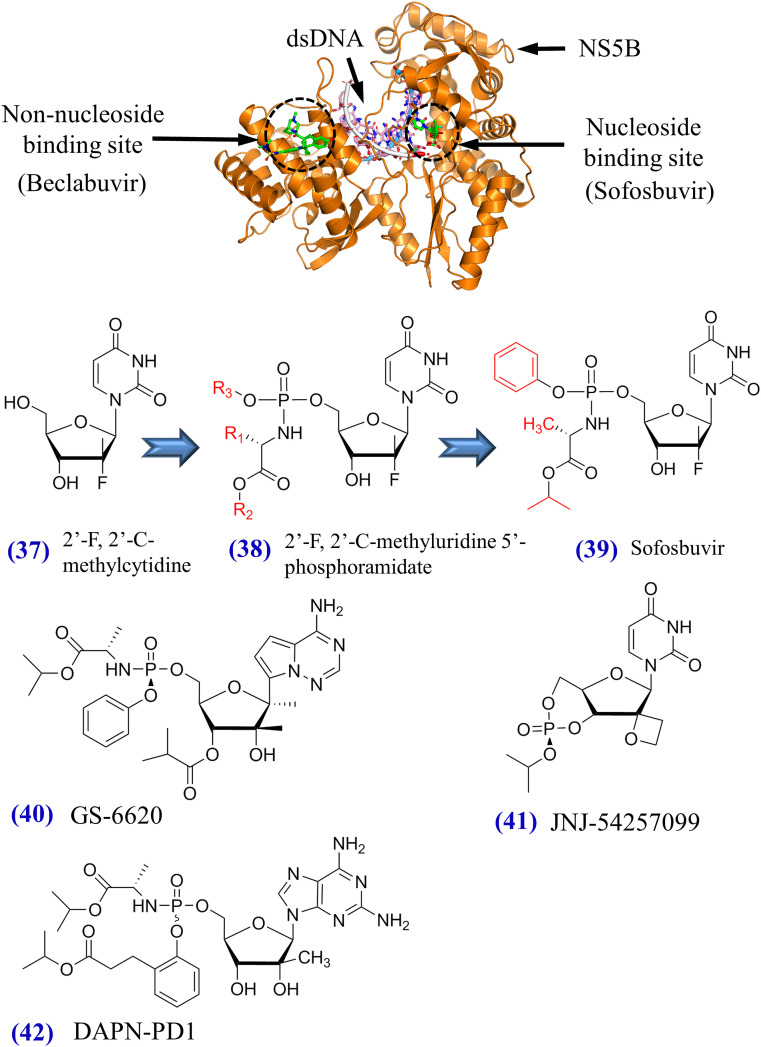
Fig. 3.
Tertiary structure of HCV NS5A and structural formulas of approved or experimental NS5A inhibitors from (19) to (36). Two units of an NS5A dimer are colored by pink and cyan, respectively. NS5A inhibitor daclatasvir is also illustrated. Blue arrows indicate the optimization from initial compounds to FDA-approved compounds such as ombitasvir (DeGoey et al., 2014), ledipasvir (Link et al., 2014), daclatasvir (Belema and Meanwell, 2014), and elbasvir (Coburn et al., 2013). Other NS5A inhibitors are summarized in Table 20.
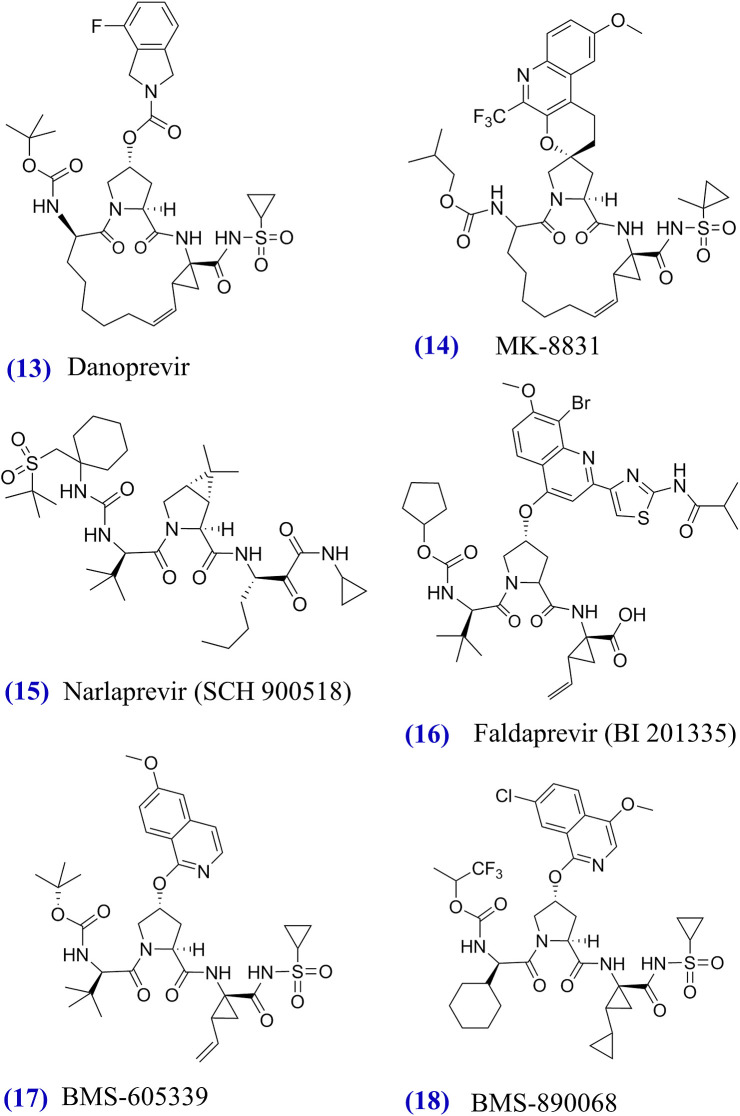
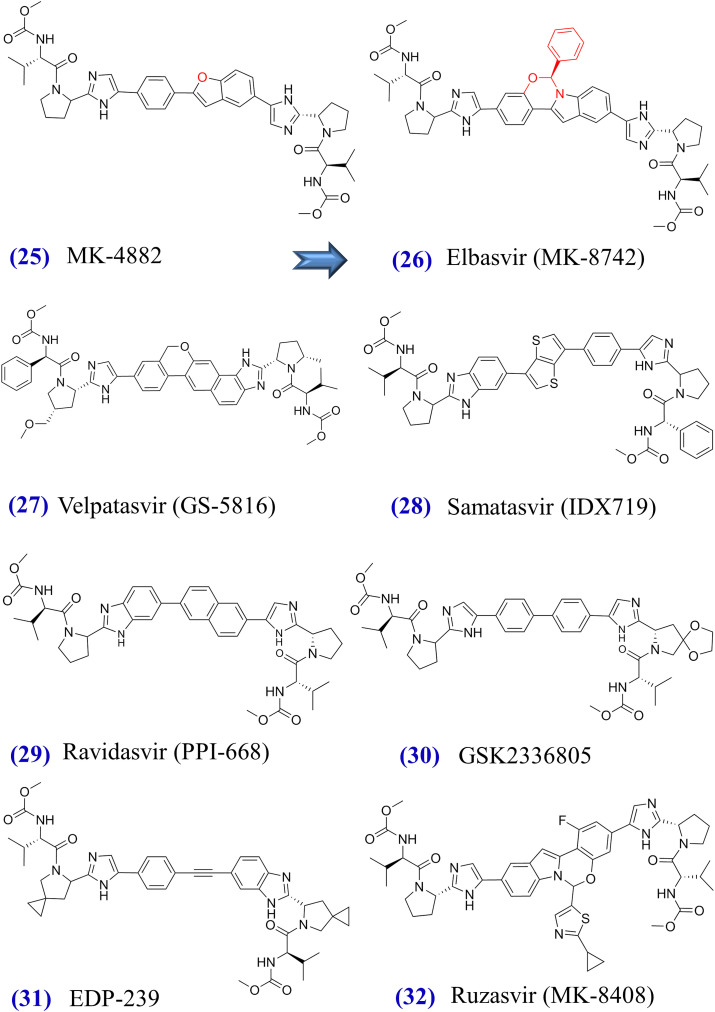
Fig. 4.
Tertiary structure of HCV NS5B and structural formulas of approved or experimental nucleoside inhibitors from (37) to (42). NS5B structure in complex with beclabuvir and sofosbuvir diphosphate (PDB codes: 4NLD and 4WTG) is visualized on top. The discovery of sofosbuvir undertakes the optimization path from 2′-F, 2′-C-methylcytidine to 2′-F, 2′-C-methyluridine 5’-phosphoramidate (Sofia et al., 2010). Structural formulas of GS-6620, JNJ-54257099, and DAPN-PD1 are also demonstrated.
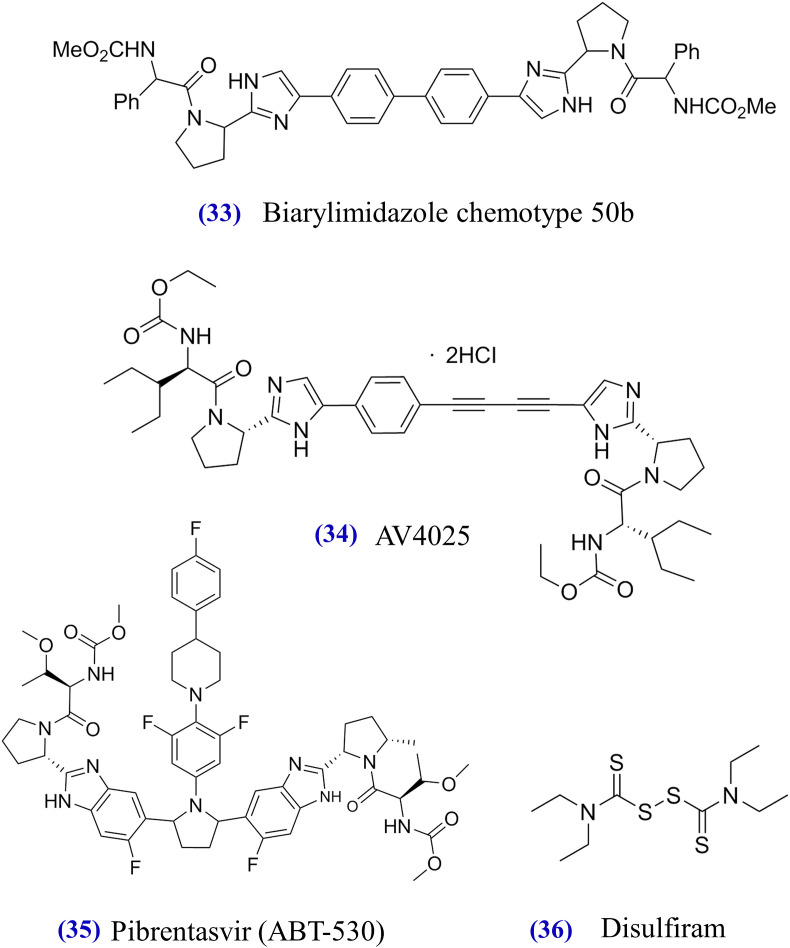
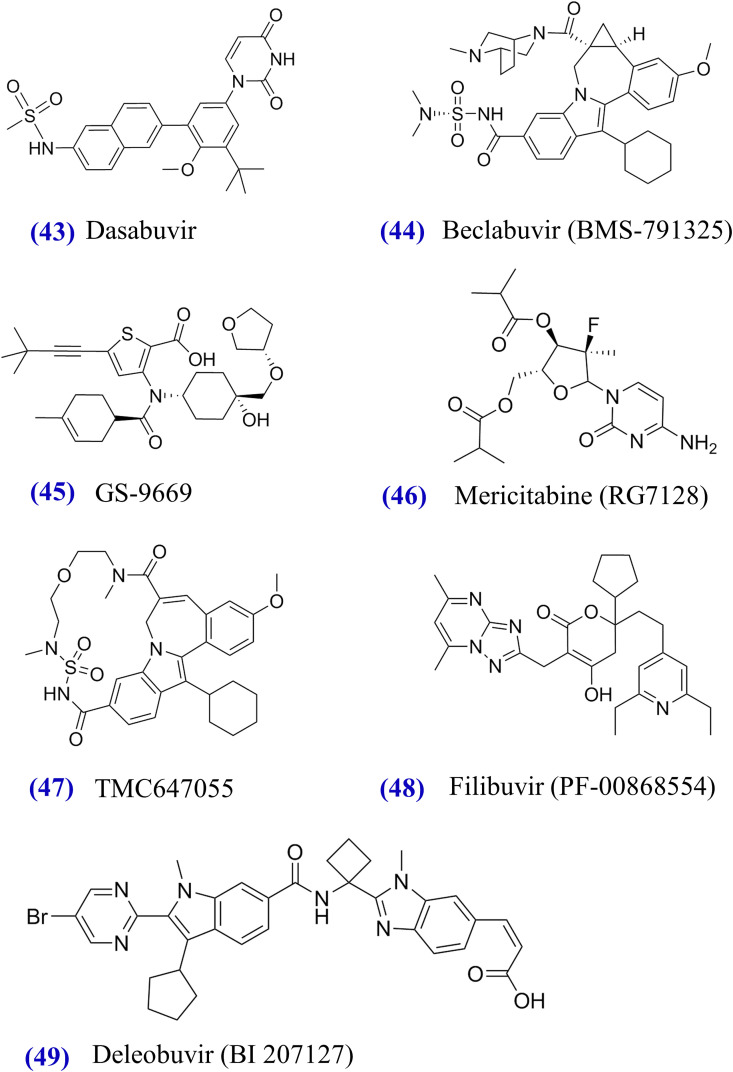
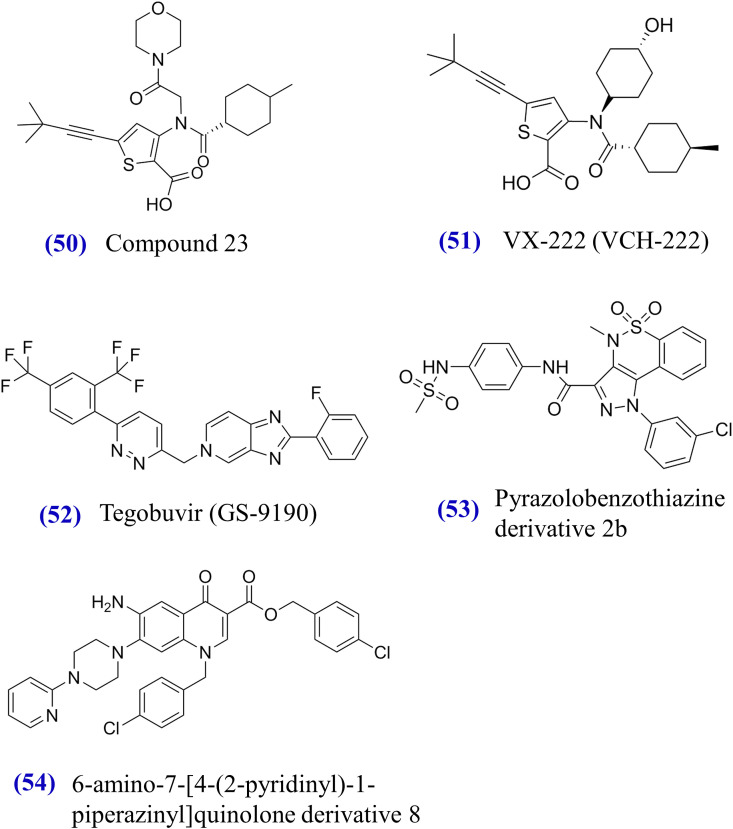
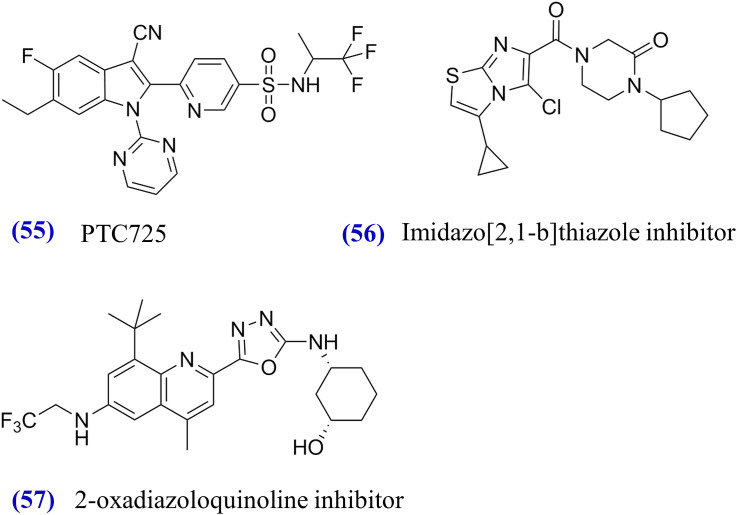
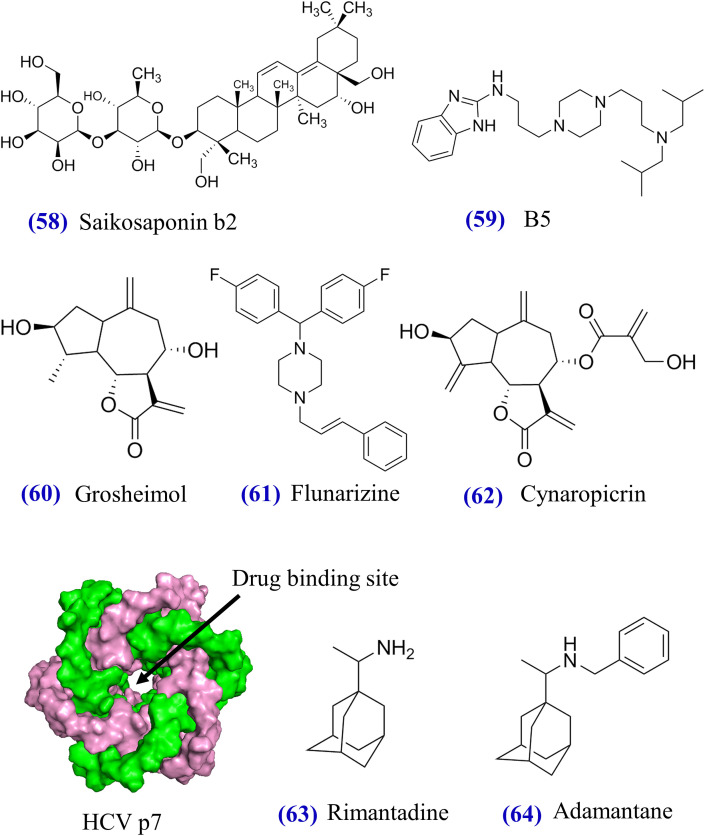
Fig. 5.
Structural formulas of NS5B non-nucleoside inhibitors from (43) to (54). FDA-approved dasabuvir and experimental compounds target the non-nucleoside binding site in NS5B (see Fig. 4).
4.1. Boceprevir (Victrelis®) + PegIFNα + RBV
Boceprevir (formerly SCH503034) in combination with PegIFNα/RBV was the first FDA-approved therapy against HCV genotype 1 infections (Table 1). After the failure of screening efforts over four million compounds, boceprevir was derived from an -ketoamide (Fig. 2) using structure-based drug design approaches (Njoroge et al., 2008). The advancement of structure-based drug design was promoted by the discovery of NS3 protease crystal structures revealed in 1996 (Kim et al., 1996, Love et al., 1996). As a potent NS3 protease inhibitor, boceprevir blocks the serine hydroxyl of HCV NS3/4A protease (Njoroge et al., 2008). According to in vitro experiments, the EC50 values of boceprevir were 196 ± 56 nM against GT-1a, 251 ± 71 nM against GT-1b, 283 ± 36 nM against GT-2a, 315 ± 30 nM against GT-2b, and 159 ± 5 nM against GT-3a (Silva et al., 2013). In May 2011, the FDA approved the clinical use of boceprevir plus PegIFNα/RBV in the treatment of HCV genotype 1 infection (Table 1).
The efficacy of the approved boceprevir-based therapy (PegIFNα/RBV for 4 weeks followed by 200 mg boceprevir TID plus PegIFNα/RBV for 44 weeks) was demonstrated in phase 2 and 3 clinical trials. Here, we summarize SVR24 rates of this therapy against genotype 1 infections in regard to cirrhosis and prior treatment history (Table 4 ). For treatment-naïve patients without cirrhosis, SVR24 rates reached 59.2% (87/147) in the HCV-TARGET study (Sterling et al., 2015), 64% (387/604) in a phase 3 study (Poordad et al., 2013), 76.3% (74/97) in the SPRINT-1 study (Kwo et al., 2010), and 67.4% (223/331) in the SPRINT-2 study (Poordad et al., 2011). For treatment-experienced patients without cirrhosis, SVR24 rates were 41.7% (68/163) in the HCV-TARGET study (Sterling et al., 2015), 64.1% (86/134) in a phase 3 study (Flamm et al., 2013), 66.4% (17/22) in the RESPOND-2 study (Bacon et al., 2011), and 64.2% (104/162) in the PROVIDE study (Vierling et al., 2014). For treatment-naïve patients with cirrhosis, SVR24 rates were approximately 32%–55% in phase 2 or 3 studies (Sterling et al., 2015, Poordad et al., 2011, Poordad et al., 2013, Kwo et al., 2010). As for treatment-experienced patients with cirrhosis, SVR24 rates were between 31.1% and 77.3% in clinical trials (Table 3). Although boceprevir plus PegIFNα/RBV was the first FDA-approved therapy, its efficacy was superseded by new DAAs, and its discontinuation was announced by Merck in 2015.
Table 4.
Efficacy of 1125 mg telaprevir BID plus PegIFNα/RBV for 12w + PegIFNα/RBV for 12w or 36w.
| Cirrhosis | Prior treatment | SVR12 rate in GT-1 | Study and trial phase | Ref. |
|---|---|---|---|---|
| No cirrhosis |
Naïve | 1a: 82.3% (28/34), 1b: 78% (32/41) | MALACHITE-I, phase 3 | Dore et al., 2016a |
| Null response | 56.5% (13/23) | MALACHITE-II, phase 3 | ||
| Partial response | 75% (9/12) | |||
| Relapse | 75% (9/12) | |||
| Null response | 50% (95/190) | ATTAIN, phase 3 | Reddy et al., 2015a | |
| Partial response | 72.3% (86/119) | |||
| Naïve | 62.2% (69/111) | Phase 3 | Kumada et al., 2016 | |
| Naïve | 77.78% (245/315) | OPTIMIZE, phase 3 | Buti et al., 2014 | |
| Naïve | 61.8% (272/440) a | HCV-TARGET, phase 3 |
Sterling et al., 2015 |
|
| Experienced | 59.3% (300/506) a | |||
| Cirrhosis | Naïve | 53.7% (29/54) | OPTIMIZE, phase 3 | Buti et al., 2014 |
| Naïve | 43.5% (103/237) a | HCV-TARGET, phase 3 | Sterling et al., 2015 | |
| Experienced | 48.4% (194/401) a | |||
| Null response | 31.3% (15/48) | ATTAIN, phase 3 | Reddy et al., 2015a | |
| Partial response | 51.9% (14/27) | |||
| Relapse | 74.2% (92/124) | ANRS CO20, phase 3 | Hezode et al., 2014 | |
| Partial response | 40% (54/135) | |||
| Null response | 19.4% (6/31) | |||
1a: HCV genotype 1a, 1b: HCV genotype 1b.
SVR24 rates were evaluated in the clinical study.
Table 3.
Efficacy of PegIFNα/RBV for 4 weeks + 200 mg boceprevir TID plus PegIFNα/RBV for 44 weeks.
| Cirrhosis | Prior treatment a | SVR24 rate in GT-1 | Study and trial phase | Ref. |
|---|---|---|---|---|
| No cirrhosis |
Naïve | 76.3% (74/97) | SPRINT-1, phase 2 | Kwo et al., 2010 |
| Naïve | 67.4% (223/331) | SPRINT-2, phase 2 | Poordad et al., 2011 | |
| Experienced | 66.4% (85/128) | RESPOND-2, phase 3 | Bacon et al., 2011 | |
| Naïve | 59.2% (87/147) | HCV-TARGET, phase 3 | Sterling et al., 2015 | |
| Experienced | 41.7% (68/163) | |||
| Null response | 40.8% (20/49) | PROVIDE, phase 3 | Vierling et al., 2014 | |
| Partial response | 67% (57/85) | |||
| Relapse | 96.4% (27/28) | |||
| Naïve | 64.1% (387/604) | Protocol 6086, phase 3 | Poordad et al., 2013 | |
| Non-response | 47.2% (17/36) | P05685AM2, phase 3 |
Flamm et al., 2013 |
|
| Relapse | 70.4% (69/98) | |||
| Cirrhosis | Naïve | 41.7% (10/24) | SPRINT-2, phase 2 | Poordad et al., 2011 |
| Naïve | 50% (3/6) | SPRINT-1, phase 2 | Kwo et al., 2010 | |
| Naïve | 55% (33/60) | Protocol 6086, phase 3 | Poordad et al., 2013 | |
| Naïve | 32% (16/50) | HCV-TARGET, phase 3 | Sterling et al., 2015 | |
| Experienced | 31.1% (28/90) | |||
| Relapse | 53.9% (55/102) b | ANRS CO20, phase 3 | Hezode et al., 2014 | |
| Partial response | 38.3% (36/94) b | |||
| Null response | 0% (0/10) b | |||
| Experienced | 77.3% (17/22) | RESPOND-2, phase 3 | Bacon et al., 2011 | |
Naïve: patients were treatment-naïve prior to therapies in clinical trials. Experienced: patients experienced other HCV therapies prior to therapies in clinical trials.
SVR12 rates were evaluated in the study.
4.2. Telaprevir (Incivek®) + PegIFNα + RBV
In May 2011, the FDA approved the clinical use of 1125 mg telaprevir (Incivek®) twice daily plus PegIFNα/RBV for 12 weeks, followed by PegIFNα/RBV for 12w or 36w. Telaprevir (formerly VX-950) in combination with PegIFNα/RBV was the second FDA-approved therapy against HCV genotype 1 infections (Table 1). Illustrated in Fig. 2, telaprevir was discovered from a viral NS5A/5B substrate (sequence: EDVVCCSMSY) of the HCV protease using structure-based drug design approaches (Kwong et al., 2011). The principle was based on the fact that HCV protease could be inhibited by its own cleavage products (Kwong et al., 2011), a mechanism similar to protease inhibitors explored for HIV (Li and De Clercq, 2016). Telaprevir is a reversible noncovalent NS3 inhibitor with favorable pharmacokinetic profiles in HCV cell cultures and animal models. Moreover, the EC50 values of telaprevir reached 252 ± 54 nM to 953 ± 103 nM in HCV GT1, GT2, and GT3 replicon assays (Silva et al., 2013).
Effectiveness of telaprevir plus PegIFNα/RBV against HCV GT1 was demonstrated in phase 2 and 3 clinical trials (Table 4). SVR12 rates of this therapy were between 62.2% and 80% in treatment-naïve patients without cirrhosis (Table 4). In the group of treatment-experienced patients without cirrhosis, SVR12 rates fell approximately between 50% and 75%. For the treatment-naïve patients with cirrhosis, SVR24 rates were 43.5% and 53.7% in the HCV-TARGET (Sterling et al., 2015) and OPTIMIZE (Buti et al., 2014) studies, respectively. For the treatment-experienced patients with cirrhosis, SVR12 rates were 38.6% and 52.4% in the ATTAIN (Reddy et al., 2015a) and ANRS CO20 (Hezode et al., 2014) studies, respectively.
Although telaprevir showed a favorable efficacy in clinical trials, the telaprevir-based therapy may cause fatal and non-fatal serious skin reactions such as Stevens-Johnson syndrome (SJS), drug reaction with eosinophilia and systemic symptoms (DRESS), and toxic epidermal necrolysis (TEN). Due to the advent of next-generation DAAs, Vertex Pharmaceuticals announced the discontinuation of telaprevir in 2014.
4.3. Sofosbuvir (Sovaldi®) + PegIFNα + RBV
In December 2013, the FDA approved the clinical use of Sovaldi® against HCV genotype 1 or 4 infections: (i) 400 mg sofosbuvir QD plus PegIFNα/RBV for 12 weeks against genotype 1 or 4; (ii) 400 mg sofosbuvir QD plus ribavirin for 12 weeks against genotype 2; (iii) 400 mg sofosbuvir QD plus ribavirin for 24w against genotype 4. Sofosbuvir (formerly GS-7977 or PSI-7977), discovered at Pharmasset in 2007 and acquired by Gilead Sciences in 2011, is the first FDA-approved nucleotide analogue that inhibits HCV NS5B (Lawitz et al., 2015a). As a selective inhibitor of HCV NS5B polymerase (Fig. 4), -D-2’-deoxy-2’--fluoro-2’-β-C-methyluridine nucleosides were selected and the optimization of their phosphoramidate prodrugs led to the discovery of sofosbuvir (Sofia et al., 2010) (Fig. 4). Moreover, sofosbuvir demonstrated potent pan-genotypic activity, and its EC50 values were between 16 ± 3.4 nM and 48 ± 13 nM in HCV GT1, GT2, and GT3 replicons (Lam et al., 2012). The favorable antiviral activity of sofosbuvir was also found in primary hepatocytes from rat, dog, and monkey (Sofia et al., 2010). Importantly, Sovaldi® is the first FDA-approved HCV drug orally administered once-daily, leading to better adherence, excellent tolerability, and safety.
The efficacy of sofosbuvir plus PegIFNα/RBV was demonstrated in a number of phase 2 and 3 clinical trials (Table 5, Table 6, Table 7 ). The efficacy of 400 mg sofosbuvir QD plus PegIFNα/RBV over a period of 12 weeks was demonstrated in clinical studies such as BOSON (Foster et al., 2015a), HCV-TARGET (Feld et al., 2016a), Electron (Gane et al., 2013a), ATOMIC (Kowdley et al., 2013), NEUTRINO (Lawitz et al., 2013a), KULDS (Ogawa et al., 2016), and LONESTAR-2 (Lawitz et al., 2015b). When we merged treatment outcome data to estimate drug efficacy regardless of the distinct nature between different clinical trials, the SVR12 rates of this therapy were approximately 87.6% (659/752) against GT1, 95.6% (482/504) against GT2, 91.3% (220/241) against GT3, 92.3% (36/39) against GT4, 100% (1/1) against GT5, and 100% (11/11) against GT6 (Table 5). In particular, the use of above therapy against genotype 1 or 4 was approved by the FDA. Table 6 illustrates the efficacy of 400 mg sofosbuvir QD plus ribavirin at 12 weeks in clinical studies such as POSITRON (Jacobson et al., 2013), FUSION (Jacobson et al., 2013), Electron (Gane et al., 2013a), FISSION (Lawitz et al., 2013a), and HCV-TARGET (Feld et al., 2016a, Welzel et al., 2016a). The SVR12 rates were approximately 62.8% (22/35) against GT1, 90.8% (750/826) against GT2, 55% (297/540) against GT3, and 73.4% (61/83) against GT4. Table 7 illustrates the efficacy of 400 mg sofosbuvir QD plus ribavirin at 24 weeks in clinical studies such as ASTRAL-2 (Foster et al., 2015b), ASTRAL-3 (Foster et al., 2015b), VALENCE (Zeuzem et al., 2014a), and BOSON (Foster et al., 2015a). SVR12 rates were approximately 58.7% (37/63) against GT1, 100% (17/17) against GT2, 82.4% (610/740) against GT3, and 90.1% (73/81) against GT4. Moreover, recurrent HCV infections after liver transplantation in patients, including those with fibrosing cholestatic hepatitis and decompensated cirrhosis, might be treated by sofosbuvir plus ribavirin, achieving modest efficacy (SVR12: 59%) (Forns et al., 2015a). The most common side effects of sofosbuvir plus PegIFNα/RBV were fatigue, headache, nausea, insomnia and anemia.
Table 5.
Efficacy of 400 mg sofosbuvir QD + PegIFNα/RBV for 12w.
| Cirrhosis | Prior treatment | SVR12 rate |
Study and trial phase | Ref. | |||||
|---|---|---|---|---|---|---|---|---|---|
| GT-1 | GT-2 | GT-3 | GT-4 | GT-5 | GT-6 | ||||
| No cirrhosis |
Experienced | 100% (9/9) | 83.3% (10/12) | LONESTAR-2, phase 2 | Lawitz et al., 2015b | ||||
| Naïve | 100% (4/4) | 100% (7/7) | Electron, phase 2a | Gane et al., 2013a | |||||
| Naïve | 91.5% (43/47) | 93.3% (14/15) | 90% (9/10) | Phase 2a | Lawitz et al., 2013b | ||||
| Experienced | 78.8% (63/80) | Phase 2 | Pol et al., 2015 | ||||||
| Naïve | 87% (275/316) | 81.8% (9/11) | 100% (5/5) | ATOMIC, phase 2 | Kowdley et al., 2013 | ||||
| Naïve | 91.3% (219/240) | 100% (27/27) | 100% (1/1) | 100% (5/5) | NEUTRINO, phase 3 | Lawitz et al., 2013a | |||
| Naïve | 95.8% (68/71) | BOSON, phase 3 | Foster et al., 2015a | ||||||
| Experienced | 94.2% (49/52) | ||||||||
| Naïve | 100% (16/16) | ? | C-EDGE Head-2-Head, phase 3 |
Sperl et al., 2016 | |||||
| Experienced | 100% (1/1) | ? | |||||||
| Naïve | 100% (4/4) | HCV-TARGET, phase 4 | Feld et al., 2016a | ||||||
| Experienced | 75% (3/4) | ||||||||
| Naïve | 98.1% (252/257) | KULDS, real-world study |
Ogawa et al., 2016 |
||||||
| Experienced | 95.9% (95/99) | ||||||||
| Cirrhosis | Experienced | 92.9% (13/14) | 83.3% (10/12) | LONESTAR-2, phase 2 | Lawitz et al., 2015b | ||||
| Naïve | 91.3% (21/23) | BOSON, phase 3 | Foster et al., 2015a | ||||||
| Experienced | 93.8% (15/16) | 85.7% (30/35) | |||||||
| Naïve | 80.8% (42/52) | 0% (0/1) | 100% (1/1) | NEUTRINO, phase 3 | Lawitz et al., 2013a | ||||
| Naïve | 66.7% (2/3) | HCV-TARGET, phase 4 | Feld et al., 2016a | ||||||
| Experienced | 87.5% (7/8) | ||||||||
| Naïve | 95.6% (43/45) | KULDS, real-world study | Ogawa et al., 2016 | ||||||
| Experienced | 82.2% (37/45) | ||||||||
?: Question marks indicate that the data was unavailable in literature.
Table 6.
Efficacy of 400 mg sofosbuvir QD + ribavirin for 12 weeks.
| Cirrhosis | Prior treatment | SVR12 rate |
Study and trial phase | Ref. | |||
|---|---|---|---|---|---|---|---|
| GT-1 | GT-2 | GT-3 | GT-4 | ||||
| No cirrhosis |
Naïve | 84% (21/25) | 100% (4/4) | 100% (6/6) | Electron, phase 2a | Gane et al., 2013a | |
| Null response | 10% (1/10) | ||||||
| Naïve | 90.9% (10/11) | Phase 2 | Ruane et al., 2015 | ||||
| Experienced | 61.5% (8/13) | ||||||
| Experienced | 92.4% (85/92) | 67.9% (57/84) | POSITRON, phase 3 | Jacobson et al., 2013 | |||
| Experienced | 96.2% (25/26) | 36.8% (14/38) | FUSION, phase 3 | ||||
| Naïve | 98.3% (58/59) | 61.4% (89/145) | FISSION, phase 3 | Lawitz et al., 2013a | |||
| Naïve | 91.9% (159/173) | 75% (42/56) | HCV-TARGET, phase 4 | Feld et al., 2016a, Welzel et al., 2016a | |||
| Experienced | 87.5% (42/48) | 84.6% (22/26) | |||||
| Naïve | 97.6% (80/82) | Phase 3 | Omata et al., 2014 | ||||
| Experienced | 96.3% (52/54) | ||||||
| Naïve | 96.7% (29/30) | 0% (0/2) | VALENCE, phase 3 | Zeuzem et al., 2014a | |||
| Experienced | 93.8% (30/32) | 42.9% (3/7) | |||||
| Naïve | 86.4% (19/22) | Egyptian study | Doss et al., 2015 | ||||
| Experienced | 72.7% (16/22) | ||||||
| Naïve or experienced | 86.4% (19/22) | Real-world study | Maasoumy et al., 2016 | ||||
| Cirrhosis | Naïve | 33.3% (1/3) | Phase 2 | Ruane et al., 2015 | |||
| Experienced | 50% (2/4) | ||||||
| Naïve | 100% (2/2) | VALENCE, phase 3 | Zeuzem et al., 2014a | ||||
| Experienced | 77.8% (7/9) | 0% (0/2) | |||||
| Naïve | 76.6% (36/47) | VALOR, phase 4 | Ho et al., 2017 | ||||
| Experienced | 84.2% (16/19) | ||||||
| Experienced | 94.1% (16/17) | 21.4% (3/14) | POSITRON, phase 3 | Jacobson et al., 2013 | |||
| Experienced | 60% (6/10) | 19.2% (5/26) | FUSION, phase 3 | ||||
| Naïve | 71.9% (23/32) | 55.3% (21/38) | HCV-TARGET, phase 4 | Feld et al., 2016a, Welzel et al., 2016a | |||
| Experienced | 86.7% (26/30) | 37.9% (22/58) | |||||
| Naïve | 90.9% (10/11) | 34.2% (13/38) | FISSION, phase 3 | Lawitz et al., 2013a | |||
| Naïve | 100% (8/8) | Phase 3 | Omata et al., 2014 | ||||
| Experienced | 88.9% (8/9) | ||||||
| Naïve | 66.7% (2/3) | Egyptian study | Doss et al., 2015 | ||||
| Experienced | 60% (3/5) | ||||||
| Naïve or experienced | 90% (9/10) | Real-world study | Maasoumy et al., 2016 | ||||
Table 7.
Efficacy of 400 mg sofosbuvir QD + ribavirin for 24 weeks.
| Cirrhosis | Prior treatment | SVR12 rate |
Study and trial phase | Ref. | |||
|---|---|---|---|---|---|---|---|
| GT-1 | GT-2 | GT-3 | GT-4 | ||||
| No cirrhosis |
Experienced | 1a: 80% (8/10), 1b: 50% (3/6) | 100% (5/5) | 0% (0/1) | Phase 2 | Charlton et al., 2015a | |
| Naïve | 100% (11/11) | Phase 2 | Ruane et al., 2015 | ||||
| Experienced | 81.8% (9/11) | ||||||
| Naïve | ? | SPARE, phase 2 | Osinusi et al., 2013 | ||||
| Naïve | 90.4% (141/156) | ASTRAL-2, ASTRAL-3, phase 3 |
Foster et al., 2015b | ||||
| Experienced | 70.9% (22/31) | ||||||
| Naïve | 94.6% (87/92) | VALENCE, phase 3 | Zeuzem et al., 2014a | ||||
| Experienced | 86.7% (85/98) | ||||||
| Naïve | 90.3% (65/72) | BOSON, phase 3 | Foster et al., 2015a | ||||
| Experienced | 81.5% (44/54) | ||||||
| Naïve | 90.5% (19/21) | Real-world study | Doss et al., 2015 | ||||
| Experienced | 95.2% (20/21) | ||||||
| Naïve or experienced | 75% (3/4) | 76.9% (10/13) | Real-world study | Maasoumy et al., 2016 | |||
| Cirrhosis | Experienced | 1a: 66.7% (8/12), 1b: 50% (2/4) | 100% (1/1) | Phase 2 | Charlton et al., 2015a | ||
| Naïve | 100% (3/3) | Phase 2 | Ruane et al., 2015 | ||||
| Experienced | 100% (4/4) | ||||||
| Naïve | ? | SPARE, phase 2 | Osinusi et al., 2013 | ||||
| Naïve | 73.3% (33/45) | ASTRAL-2, ASTRAL-3, phase 3 |
Foster et al., 2015b | ||||
| Experienced | 57.9% (22/38) | ||||||
| Naïve | 92.3% (12/13) | VALENCE, phase 3 | Zeuzem et al., 2014a | ||||
| Experienced | 61.7% (29/47) | ||||||
| Naïve | 81.8% (18/22) | BOSON, phase 3 | Foster et al., 2015a | ||||
| Experienced | 100% (17/17) | 76.5% (26/34) | |||||
| Naïve | 100% (3/3) | Egyptian study | Doss et al., 2015 | ||||
| Experienced | 66.7% (4/6) | ||||||
| Naïve or experienced | 48.1% (13/27) | 52.6% (10/19) | Real-world study | Maasoumy et al., 2016 | |||
?: Question marks indicate that the data was unavailable in literature.
4.4. Simeprevir (Olysio®) + sofosbuvir or PegIFNα/RBV
In November 2013, the FDA approved the use of (i) 150 mg simeprevir QD plus PegIFNα/RBV against genotype 1 or 4 infections; (ii) 150 mg simeprevir plus 400 mg sofosbuvir QD against genotype 1 infections (Table 1). Simeprevir (formerly TMC435) is a potent inhibitor targeting HCV NS3/4A (Rosenquist et al., 2014) (Fig. 2). It is worth mentioning that the NS3/4A inhibitor simeprevir in the combination with the NS5B inhibitor sofosbuvir is considered to efficiently inhibit different stages of HCV life cycle – a principle in line with the standard cocktail treatment for HIV. Simeprevir was discovered during the extensive exploration of novel P2 cyclopentane macrocyclic inhibitors using HCV NS3 protease assays, the cellular replicon system, and structure-based design (Rosenquist et al., 2014). Moreover, EC50 values of simeprevir were 28.4 nM and 8.1 nM in Huh7-derived replicon cells with genotype 1a (strain: H77) or genotype 1b (con1b), respectively (Lin et al., 2009). Indeed, simeprevir showed excellent in vitro and in vivo biological, antiviral and safety pharmacology profiles, which paved its way to clinical trials.
Here, we summarize the efficacy of simeprevir plus sofosbuvir or PegIFNα/RBV in phase 2 and 3 clinical studies such as COSMOS (Lawitz et al., 2014a), OPTIMIST-1 (Kwo et al., 2016), OPTIMIST-2 (Lawitz et al., 2016a), TARGET (El-Khayat et al., 2016, Sulkowski et al., 2016), and ANRS CO22 HEPATHER(112). We attempted to estimate drug efficacy by merging all clinical data regardless of the distinct nature between different clinical trials. (i) For the treatment of 150 mg simeprevir plus 400 mg sofosbuvir QD at 12w, its SVR12 reached 93.8% (407/434) in GT1-infected patients without cirrhosis, 97.9% (476/486) in GT4-infected patients without cirrhosis, 81.7% (371/454) in GT1-infected patients with cirrhosis, 84.8% (84/99) in GT4-infected patients with cirrhosis (Table 8 ). (ii) Regarding the treatment of 150 mg simeprevir plus 400 mg sofosbuvir QD for 24w, its SVR12 reached 96.9% (31/32) in GT1-infected patients without cirrhosis, and 100% (10/10) in GT1-infected patients with cirrhosis (Table 8). (iii) Regarding the treatment of 150 mg simeprevir QD plus PegIFNα/RBV for 12w + PegIFNα/RBV for 12w, its SVR12 reached 76.2% (1087/1426) in GT1-infected patients without cirrhosis, 50.2% (88/175) in GT1- infected patients with cirrhosis (Table 9 ). (iv) Regarding the treatment of 150 mg simeprevir QD plus PegIFNα/RBV for 12w + PegIFNα/RBV for 36w, its SVR12 reached 83.2% (252/303) in GT1-infected patients without cirrhosis, 65.9% (29/44) in GT1-infected patients with cirrhosis (Table 10 ). In the RESTORE study, patients received simeprevir plus PegIFNα/RBV for 12w followed by PegIFNα/RBV for 12w or 36w (Moreno et al., 2015). SVR12 rates were 66.6% (72/108) in GT4-infected patients without cirrhosis, and 40.8% (20/49) in GT4-infected patients with cirrhosis. Furthermore, 12w of simeprevir plus PegIFNα/RBV followed by additional 36w of PegIFNα/RBV was approved for patients co-infected with HIV and HCV infections. In clinical studies, the most common side effects of simeprevir plus sofosbuvir were fatigue, headache and nausea, while simeprevir plus sofosbuvir may have caused common adverse events such as rash, pruritus, nausea, and photosensitivity reactions.
Table 8.
Efficacy of 150 mg simeprevir plus 400 mg sofosbuvir QD for 12w.
| Cirrhosis | Prior treatment | SVR12 rate |
Study and trial phase | Ref. | |
|---|---|---|---|---|---|
| GT-1 | GT-4 | ||||
| 150 mg simeprevir plus 400 mg sofosbuvir QD for 12w | |||||
| No cirrhosis |
Naïve | 100% (4/4) | COSMOS, phase 3 |
(Lawitz et al., 2014a) | |
| Null response | 94.1% (16/17) | ||||
| Naïve | 97.4% (112/115) | OPTIMIST-1, phase 3 | (Kwo et al., 2016) | ||
| Experienced | 95% (38/40) | ||||
| Naïve | 98.3% (285/290) | HCV-TARGET, phase 3 | (El-Khayat et al., 2016) | ||
| Experienced | 97.4% (191/196) | ||||
| Naïve | 100% (11/11) | GALAXY, phase 2 | (O'Leary et al., 2017) | ||
| Naïve | 1a:88.4% (61/69), 1b:97.4% (37/38) | HCV-TARGET, phase 3 |
(Sulkowski et al., 2016) |
||
| Experienced | 1a:89.5% (77/86), 1b:94.4% (51/54) | ||||
| Cirrhosis |
Naïve | 66.6% (2/3) | COSMOS, phase 3 |
(Lawitz et al., 2014a) | |
| Null response | 100% (4/4) | ||||
| Naïve | 88% (44/50) | OPTIMIST-2, phase 3 | (Lawitz et al., 2016a) | ||
| Experienced | 79.2% (42/53) | ||||
| Naïve | 80.8% (42/52) | HCV-TARGET, phase 3 | (El-Khayat et al., 2016) | ||
| Experienced | 88.9% (40/45) | ||||
| Naïve | 1a:83.9% (73/87), 1b:91.7% (33/36) | HCV-TARGET, phase 3 | (Sulkowski et al., 2016) | ||
| Experienced | 1a:75.2% (97/129), 1b:82.1% (64/78) | ||||
| Experienced | 1a:81.8% (9/11), 1b:100% (3/3) | 100% (2/2) | ANRS CO22 HEPATHER | (Hezode et al., 2016) | |
| Naïve or experienced |
80.8% (97/120) |
Real-world study |
(Shiffman et al., 2015) |
||
| 150 mg simeprevir plus 400 mg sofosbuvir QD for 24w | |||||
| No cirrhosis |
Naïve | 100% (2/2) | COSMOS, phase 3 |
(Lawitz et al., 2014a) | |
| Null response | 100% (18/19) | ||||
| Naïve | 100%(11/11) | GALAXY, phase 2 | (O'Leary et al., 2017) | ||
| Cirrhosis | Naïve | 100% (6/6) | COSMOS, phase 3 |
(Lawitz et al., 2014a) | |
| Null Response | 100% (4/4) | ||||
Table 9.
Efficacy of 150 mg simeprevir QD plus PegIFNα/RBV for 12w + PegIFNα/RBV for 12w.
| Cirrhosis | Prior treatment | SVR12 rate in GT-1 | Study and trial phase | Ref. |
|---|---|---|---|---|
| No cirrhosis |
Naïve | 80.5% (62/77) | PILLAR, phase 2b | Fried et al., 2013 |
| Naïve | 88.6% (109/123) | CONCERTO-1, phase 3 | Hayashi et al., 2014 | |
| Non-response | 52.8% (28/53) | CONCERTO-2, phase 3 | Izumi et al., 2014 | |
| Relapse | 95.9% (47/49) | CONCERTO-3, phase 3 | ||
| Naïve | 91.7% (22/24) | CONCERTO-4, phase 3 | Kumada et al., 2015a | |
| Non-response | 38.5% (10/26) | |||
| Relapse | 100% (29/29) | |||
| Relapse | 78.2% (230/294) | PROMISE, phase 3 | Forns et al., 2014 | |
| Naïve | 82.1% (188/229) | QUEST-1, phase 3 | Jacobson et al., 2014 | |
| Naïve | 81.8% (189/231) | QUEST-2, phase 3 | Manns et al., 2014 | |
| Null response | 50.3% (87/173) | ATTAIN, phase 3 |
Reddy et al., 2015a |
|
| Partial response | 72.9% (86/118) | |||
| Cirrhosis | Relapse | 74.4% (29/39) | PROMISE, phase 3 | Forns et al., 2014 |
| Null response | 24.6% (15/61) | ATTAIN, phase 3 | Reddy et al., 2015a | |
| Partial response | 55.6% (15/27) | |||
| Naïve | 58.1% (18/31) | QUEST-1, phase 3 | Jacobson et al., 2014 | |
| Naïve | 64.7% (11/17) | QUEST-2, phase 3 | Manns et al., 2014 | |
Table 10.
Efficacy of 150 mg simeprevir QD plus PegIFNα/RBV for 12w + PegIFNα/RBV for 36w.
| Cirrhosis | Prior treatment | SVR12 rate |
Study and trial phase | Ref. | |
|---|---|---|---|---|---|
| GT-1 | GT-4 | ||||
| No cirrhosis |
Relapser | 87.3% (55/63) | ASPIRE, phase 2b | Zeuzem et al., 2014b | |
| Partial responder | 74.1% (43/58) | ||||
| Null responder | 59.5% (22/37) | ||||
| Naïve | 84.4% (27/32) | RESTOREa, phase 3 | Moreno et al., 2015 | ||
| Experienced | 59.2% (45/76) | ||||
| Naïve | 91% (132/145) | TIGER, phase 3 | Wei et al., 2016 | ||
| Cirrhosis | Relapser | 73.3% (11/15) | ASPIRE, phase 2b | Zeuzem et al., 2014b | |
| Partial responder | 81.8% (9/11) | ||||
| Null responder | 30.8% (4/13) | ||||
| Naïve | 66.7% (2/3) | RESTOREa, phase 3 | Moreno et al., 2015 | ||
| Experienced | 39.1% (18/46) | ||||
| Naïve | 100% (5/5) | TIGER, phase 3 | Wei et al., 2016 | ||
?: Question marks indicate that the data was unavailable in literature.
Patients in the RESTORE study received simeprevir plus PegIFNα/RBV for 12w followed by PegIFNα/RBV for either 12w or 36w (Moreno et al., 2015).
4.5. Ledipasvir + sofosbuvir (Harvoni®)
In October 2014, the FDA approved the fixed-dose combination tablets of 90 mg ledipasvir + 400 mg sofosbuvir (Harvoni®) with or without ribavirin for the treatment of HCV genotype 1, 4, 5 or 6 infections. Ledipasvir is a potent NS5A inhibitor (Fig. 3), while the nucleotide analogue sofosbuvir targets NS5B to inhibit its activity (Fig. 4). Ledipasvir (formerly GS-5885) was discovered through a series of modifications in an unsymmetric benzimidazole-difluorofluorene-imidazole core and distal [2.2.1] azabicyclic ring system (Link et al., 2014). In HCV replicon assays, the EC50 values of ledipasvir were 0.031 nM against GT1a, 0.004 nM against GT1b, 21 nM against GT2a, 16 nM against GT2b, 168 nM against GT3a, 0.39 nM against GT4a, 0.15 nM against GT5a, and 1.1 nM against GT6a (Cheng et al., 2016). Pharmacokinetic studies in animal models (e.g. rats, dogs, monkeys) further supported the potent antiviral activity of ledipasvir (Link et al., 2014).
The efficacy of ledipasvir plus sofosbuvir with or without ribavirin was demonstrated in many clinical studies, including LONESTAR (Lawitz et al., 2014b), ION-1 (Afdhal et al., 2014a), ION-2 (Afdhal et al., 2014b), ION-3 (Kowdley et al., 2014a), SOLAR-1 (Charlton et al., 2015b), SOLAR-2 (Manns et al., 2016), NIAID SYNERGY (Kohli et al., 2015a), TRIO (Younossi et al., 2016), GS-US-337-0113 (Mizokami et al., 2015), and SIRIUS (Bourliere et al., 2015) (see summary in Table 11, Table 12). For instance, the SOLAR-1 and SOLAR-2 studies indicated that the ledipasvir + sofosbuvir + ribavirin therapy for 12 weeks led to high rates of SVR12 (>85%) even in patients with decompensated cirrhotic before and after liver transplantation (Charlton et al., 2015b, Manns et al., 2016). Here, we attempted to estimate drug efficacy by merging all clinical data regardless of the distinct nature between different clinical trials. (i) Regarding the treatment of 400 mg sofosbuvir + 90 mg ledipasvir QD for 12 weeks, the SVR12 rates were 96.1% (3674/3824) in GT1-infected patients without cirrhosis, and 92.2% (867/940) in GT1-infected patients with cirrhosis, 91.6% (44/48) in GT4-infected patients without cirrhosis, 96.8% (31/32) in GT5-infected patients without cirrhosis, and 95.6% (22/23) in GT6-infected patients without cirrhosis (Table 11 ). (ii) Regarding the treatment of 90 mg ledipasvir + 400 mg sofosbuvir QD for 24 weeks, its SVR12 reached 99.3% (266/268) in GT1-infected patients without cirrhosis, and 96.9% (127/131) in GT1-infected patients with cirrhosis. (iii) Regarding the therapy of 90 mg ledipasvir + 400 mg sofosbuvir QD with ribavirin for 12 weeks, SVR12 rates were 98.9% (467/472) in GT1-infected patients without cirrhosis, and 93.3% (393/421) in GT1-infected patients with cirrhosis (Table 12 ). Moreover, the drug resistant mutations at baseline exerted minimal effects on patient responses to the therapy of ledipasvir plus sofosbuvir (Sarrazin et al., 2016). The most common adverse events with the treatment of Harvoni® were headache, fatigue and asthenia.
Table 11.
Efficacy of 90 mg ledipasvir + 400 mg sofosbuvir, QD for 12 weeks.
| Cirrhosis | Prior treatment | SVR12 rate |
Study and trial phase | Ref. | ||||
|---|---|---|---|---|---|---|---|---|
| GT-1 | GT-3 | GT-4 | GT-5 | GT-6 | ||||
| No cirrhosis |
Naïve | 94.7% (18/19) | LONESTAR, phase 2 | Lawitz et al., 2014b | ||||
| Experienced | 100% (8/8) | |||||||
| Naïve | 1a:100% (11/11), 1b:100% (9/9) | Phase 2a | Kohli et al., 2015a | |||||
| Naïve or experienced | 92.9% (13/14) | NIAID, phase 2a | Kohli et al., 2015b | |||||
| Naïve or experienced | 76.2% (16/21) | 95.7% (22/23) | ELECTRON-2, phase 2 | Gane et al., 2015 | ||||
| Experienced | 100% (7/7) | SPARE, phase 2a | Osinusi et al., 2014 | |||||
| Experienced | 91.2% (31/34) | NIAID synergy, phase 2a | Wilson et al., 2016 | |||||
| Naïve | 95.2% (20/21) | Phase 2 | Abergel et al., 2016a | |||||
| Experienced | 84.6% (11/13) | |||||||
| Naïve | 94.4% (17/18) | Phase 2 | (Abergel et al., 2016b) | |||||
| Experienced | 100% (14/14) | |||||||
| Naïve | 100% (70/70) | GS-US-337-0113, phase 3 | Mizokami et al., 2015 | |||||
| Experienced | 100% (60/60) | |||||||
| Naïve | 100% (179/179) | ION-1, phase 3 | Afdhal et al., 2014a | |||||
| Experienced | 96.2% (50/52) | ION-2, phase 3 | Afdhal et al., 2014b | |||||
| Experienced | 94.3% (33/35) | |||||||
| Naïve | 1a: 94.8% (163/172), 1b: 97.7% (43/44) | ION-3, phase 3 | Kowdley et al., 2014a | |||||
| Naïve | 1a: 94.6% (406/429), 1b: 98.3% (172/175) | TRIO, real-world study | Younossi et al., 2016 | |||||
| Naïve | 1a:95.7% (1352/1413), 1b:95.2% (415/436) | Real-world study |
Ioannou et al., 2016 |
|||||
| Experienced | 1a:96.7% (472/488), 1b:95.6% (175/183) | |||||||
| Cirrhosis | Experienced | 90.9% (10/11) | LONESTAR, phase 2 | Lawitz et al., 2014b | ||||
| Naïve | 100% (1/1) | Phase 2 | Abergel et al., 2016a | |||||
| Experienced | 100% (9/9) | |||||||
| Naïve | 100% (3/3) | Phase 2 | Abergel et al., 2016b | |||||
| Experienced | 83.3% (5/6) | |||||||
| Null response | 70% (7/10) | Phase 2 | Gane et al., 2014a | |||||
| Naïve or experienced | 100% (7/7) | NIAID, phase 2a | Kohli et al., 2015b | |||||
| Experienced | 70% (7/10) | ELECTRON-1, phase 2 | Gane et al., 2013b | |||||
| Naïve or experienced | 25% (1/4) | 100% (2/2) | ELECTRON-2, phase 2 | Gane et al., 2015 | ||||
| Naïve | 96.9% (32/33) | ION-1, phase 3 | Afdhal et al., 2014a | |||||
| PI + PegIFNα+RBV | 85.7% (12/14) | ION-2, phase 3 | Afdhal et al., 2014b | |||||
| PegIFNα+RBV | 87.5% (7/8) | |||||||
| Naïve | 100% (13/13) | GS-US-337-0113, phase 3 | Mizokami et al., 2015 | |||||
| Experienced | 100% (28/28) | |||||||
| Naïve | 1a:91.7% (483/527), 1b:93.6% (162/173) | Real-world study | Ioannou et al., 2016 | |||||
| Experienced | 1a:90.7% (68/75), 1b:100% (38/38) | |||||||
| Experienced | 76.9% (10/13) a | 40% (2/5)a | Real-world study | Cheung et al., 2016 | ||||
SVR24 rates were evaluated in the clinical study.
Table 12.
Efficacy of 90 mg ledipasvir + 400 mg sofosbuvir QD for 24 weeks, or with ribavirin for 12 weeks in phase 2 and 3 clinical trials.
| Cirrhosis | Prior treatment | SVR12 rate |
Study and trial phase | Ref. | ||
|---|---|---|---|---|---|---|
| GT-1 | GT-3 | GT-4 | ||||
| 90 mg ledipasvir + 400 mg sofosbuvir QD for 24 weeks | ||||||
| No cirrhosis | Naïve | 99.5% (181/182) | ION-1, phase 3 | Afdhal et al., 2014a | ||
| PI + PegIFNα+RBV | 97.2% (35/36) | ION-2, phase 3 | Afdhal et al., 2014b | |||
| PegIFNα+RBV | 100% (50/50) | |||||
| Cirrhosis |
Naïve | 96.9% (31/32) | ION-1, phase 3 | Afdhal et al., 2014a | ||
| Experienced | 96.1% (74/77) | SIRIUS, phase 2 | Bourliere et al., 2015 | |||
| PI + PegIFNα+RBV | 100% (14/14) | ION-2, phase 3 |
Afdhal et al., 2014b |
|||
| PegIFNα+RBV | 100% (8/8) | |||||
| 90 mg ledipasvir + 400 mg sofosbuvir QD with ribavirin for 12 weeks | ||||||
| No cirrhosis | Experienced | 100% (36/36) | Patients from 5 trials | Wyles et al., 2015 | ||
| Naïve | 100% (25/25) | Phase 2 | Gane et al., 2014a | |||
| Experienced | 100% (9/9) | |||||
| Experienced | 100% (10/10) | LONESTAR, phase 2 | Lawitz et al., 2014b | |||
| Experienced | 100% (7/7) | ELECTRON-1, phase 2 | Gane et al., 2013b | |||
| Naïve | 100% (20/20) | ELECTRON-2, phase 2 | Gane et al., 2015, Gane et al., 2013b | |||
| Experienced | 100% (19/19) | 89.3% (25/28) | ||||
| Naïve or experienced | 96.3% (52/54) | 100% (1/1) | SOLAR-1, phase 2 | Charlton et al., 2015b | ||
| Naïve or experienced | 93.3% (42/45) | 100% (7/7) | SOLAR-2, phase 2 | Manns et al., 2016 | ||
| Naïve | 100% (178/178) | ION-1, phase 3 | Afdhal et al., 2014a | |||
| PI + PegIFNα+RBV | 100% (51/51) | ION-2, phase 3 | Afdhal et al., 2014b | |||
| PegIFNα+RBV | 100% (38/38) | |||||
| Cirrhosis | Experienced | 97.4% (75/77) | SIRIUS, phase 2 | Bourliere et al., 2015 | ||
| Experienced | 100% (11/11) | LONESTAR, phase 2 | Lawitz et al., 2014b | |||
| Experienced | 100% (14/14) | Patients from 5 trials | Wyles et al., 2015 | |||
| Experienced | 100% (9/9) | Phase 2 | Gane et al., 2014a | |||
| Naïve or experienced | 87.3% (96/110) | 100% (3/3) | SOLAR-1, phase 2 | Charlton et al., 2015b | ||
| Naïve or experienced | 91.8% (90/98) | 77.8% (14/18) | SOLAR-2, phase 2 | Manns et al., 2016 | ||
| Experienced | 100% (27/27) | ELECTRON-1, phase 2 | Gane et al., 2013b | |||
| Naïve | 100% (20/20) | 100% (6/6) | ELECTRON-2, phase 2 | Gane et al., 2015, Gane et al., 2013b | ||
| Experienced | 72.7% (16/22) | |||||
| Naïve | 100% (33/33) | ION-1, phase 3 | Afdhal et al., 2014a | |||
| PI + PegIFNα+RBV | 84.6% (11/13) | ION-2, phase 3 | Afdhal et al., 2014b | |||
| PegIFNα+RBV | 77.8% (7/9) | |||||
| Experienced | 89.2% (132/148)a | 61.4% (35/57)a | Real-world study | Cheung et al., 2016 | ||
SVR24 rates were used in the study.
Adding ribavirin to ledipasvir plus sofosbuvir might provide additional efficacy in certain patient populations, but its added value may not compensate for the increased rates of treatment-associated adverse events, for instance, in black patients (Wilder et al., 2016). Ledipasvir plus sofosbuvir for 12w was safe and effective against GT-1 infections in treatment-naïve patients with compensated cirrhosis, but its use for treatment-experienced patients with compensated cirrhosis required the extending treatment duration to 24 weeks (Reddy et al., 2015b).
4.6. Ombitasvir + paritaprevir + ritonavir + dasabuvir (Viekira Pak™)
In December 2014, the FDA approved the fixed-dose combination tablets of paritaprevir + ombitasvir + ritonavir copackaged with dasabuvir (Viekira Pak™). Regarding the mechanisms of drug action, paritaprevir (formerly ABT-450), ombitasvir (ABT-267), and dasabuvir (ABT-333) are antiviral inhibitors against HCV NS3/4A, NS5A, and NS5B proteins, respectively. In addition to its known function as a booster to HIV protease inhibitors (De Clercq and Li, 2016), ritonavir in Viekira Pak™ effectively inhibits human gene CYP3A encoding important enzymes in the human body that oxidize small foreign organic molecules for drug metabolism. The inhibition of CYP3A-mediated metabolism of paritaprevir thus increases the plasma concentration of paritaprevir. In replicon cell lines, paritaprevir demonstrates potent activities against different genotypes, and the EC50 values of paritaprevir were estimated to be 1.0 ± 0.33 nM against GT1a, 0.21 ± 0.07 nM against GT1b, 5.3 ± 1.2 nM against GT2a, 19 ± 5.2 nM against GT3a, 0.09 ± 0.03 nM against GT4a, and 0.69 ± 0.09 nM against GT6a (Pilot-Matias et al., 2015). Based on cell-culture experiments, it has been shown that EC50 values of ombitasvir were approximately 14.1 ± 6.8 pM against GT1a, 5.0 ± 1 pM against GT1b, 12.4 ± 2.7 pM against GT2a, 4.3 ± 1.2 pM against GT2b, 19.3 ± 5.8 pM against GT3a, 1.71 ± 0.88 pM against GT4a, 4.3 ± 0.9 pM against GT5a, and 415 ± 97 pM against GT6a (DeGoey et al., 2014). Regarding the discovery of ombitasvir, it was optimized from a symmetric series of N-phenylpyrrolidine-based inhibitors with chiral pyrrolidine-based cores (DeGoey et al., 2014) (Fig. 3). As for dasabuvir (Fig. 5), it is a nonnucleoside inhibitor that targets the allosteric site within the NS5B palm region (Liu et al., 2012). The EC50 values of dasabuvir were 7.7 nM against GT1a and 1.8 nM against GT1b in replicon cell lines (Kati et al., 2015).
As the first co-formulated triple-DAA therapy, Viekira Pak™ offers significant improvement against genotype 1. Here, we summarize the efficacy of Viekira Pak™ in phase 2 and 3 clinical studies, including PEARL-II (Andreone et al., 2014), PEARL-III (Ferenci et al., 2014), PEARL-IV (Ferenci et al., 2014), SAPPHIRE-I (Feld et al., 2014), RUBY-I (Pockros et al., 2016), AVIATOR (Kowdley et al., 2014b), MALACHITE-I (Dore et al., 2016a), MALACHITE-II (Dore et al., 2016a), TURQUOISE-II (Poordad et al., 2014), TURQUOISE-III (Feld et al., 2016b), and SAPPHIRE-II (Zeuzem et al., 2014c). (i) Table 13 highlights the efficacy of 12.5 mg ombitasvir + 75 mg paritaprevir + 50 mg ritonavir once-daily fixed-dose two pills plus 250 mg dasabuvir BID for 12w. We attempted to estimate drug efficacy by merging all clinical data regardless of the distinct nature between different clinical trials. The SVR12 rates of this regimen reached 96.9% (1065/1099) in GT1-infected patients without cirrhosis, and 100% (84/84) in GT1-infected patients with cirrhosis in GT1-infected patients with cirrhosis. (ii) Table 14 shows the efficacy of 12.5 mg ombitasvir + 75 mg paritaprevir + 50 mg ritonavir once-daily fixed-dose two pills plus 250 mg dasabuvir BID plus ribavirin for 12w. Based on clinical studies, the SVR12 rates of this therapy reached 96.4% (2518/2612) in GT1-infected patients without cirrhosis, and 95.7% (630/658) in GT1-infected patients with cirrhosis. (iii) Table 15 illustrates the efficacy of 12.5 mg ombitasvir + 75 mg paritaprevir + 50 mg ritonavir fixed-dose two pills QD plus 250 mg dasabuvir BID plus ribavirin for 24w. In the TURQUOISE-II study, SVR12 rates reached 95.9% (165/172) in GT1-infected patients with cirrhosis (Poordad et al., 2014). Overall, the SVR12 rates of Viekira Pak™ achieved above 90% in the treatment of GT1-infected patients with or without cirrhosis. The most common side effects of Viekira Pak™ in these clinical studies were fatigue, nausea, skin rash, pruritus, insomnia, and asthenia.
Table 13.
Efficacy of 12.5 mg ombitasvir + 75 mg paritaprevir + 50 mg ritonavir fixed-dose two pills QD plus 250 mg dasabuvir BID for 12w.
| Cirrhosis | Prior treatment | SVR12 in GT-1 | Study and trial phase | Ref. |
|---|---|---|---|---|
| No cirrhosis |
Naïve | 88.6% (70/79) a | AVIATOR, phase 2b | Kowdley et al., 2014b |
| Null response | 1b: 100% (32/32) | PEARL-II, phase 3 | Andreone et al., 2014 | |
| Partial response | 1b: 100% (26/26) | |||
| Relapse | 1b: 100% (33/33) | |||
| Naïve | 1a: 90.2% (185/205), 1b:99% (207/209) | PEARL-IV, PEARL-III, phase 3 | Ferenci et al., 2014 | |
| Naïve, stage 4 or 5 chronic kidney disease | 1b: 100% (7/7) | RUBY-I, phase 3 | Pockros et al., 2016 | |
| Naïve | 1b: 97.6% (81/83) | MALACHITE-I, phase 3 | Dore et al., 2016a | |
| Naïve | 1b: 97.8% (391/400) | Real-world study |
Ioannou et al., 2016 |
|
| Experienced | 1b: 99% (103/104) | |||
| Cirrhosis | Naïve | 1b: 100% (27/27) | TURQUOISE-III, phase 3b | Feld et al., 2016b |
| Experienced | 1b: 100% (33/33) | |||
| Naïve | 1b: 100% (24/24) | Real-world study | Ioannou et al., 2016 | |
SVR24 rates were evaluated in the clinical study.
Table 14.
Efficacy of 12.5 mg ombitasvir + 75 mg paritaprevir + 50 mg ritonavir fixed-dose two pills QD plus 250 mg dasabuvir BID plus ribavirin for 12w.
| Cirrhosis | Prior treatment | SVR12 rate in GT-1 | Study and trial phase | Ref. |
|---|---|---|---|---|
| No cirrhosis |
Naïve | 95% (38/40) a | AVIATOR, phase 2b | Kowdley et al., 2014b |
| Null response | 95.5% (21/22) a | |||
| Naïve | 97.2% (35/36) | Phase 2 | Lalezari et al., 2015 | |
| Experienced | 100% (2/2) | |||
| Null response | 1b:93.5% (29/31) | PEARL-II, phase 3 | Andreone et al., 2014 | |
| Partial response | 1b:96% (24/25) | |||
| Relapse | 1b:100% (32/32) | |||
| Naïve | 1a: 97% (97/100), 1b:99.5% (209/210) | PEARL-IV, PEARL-III, phase 3 | Ferenci et al., 2014 | |
| Naïve | 1a: 97.1% (67/69), 1b: 98.8% (83/84) | MALACHITE-I | Dore et al., 2016a | |
| Null response | 100% (49/49) | MALACHITE-II, phase 3 | ||
| Partial response | 100% (25/25) | |||
| Relapse | 96.3% (26/27) | |||
| Naïve | 1a:95.3% (307/322), 1b:98% (148/151) | SAPPHIRE-I, phase 3 | Feld et al., 2014 | |
| Null response | 95.3% (82/86) | SAPPHIRE-II, phase 3 | Zeuzem et al., 2014c | |
| Partial response | 100% (65/65) | |||
| Relapse to PegIFNα+RBV | 95.2% (139/146) | |||
| Naïve, stage 4/5 chronic kidney disease | 1a: 84.6% (11/13) | RUBY-I, phase 3 | Pockros et al., 2016 | |
| Naïve | 1a:95% (689/725), 1b:98.6% (140/142) | Real-world study |
Ioannou et al., 2016 |
|
| Experienced | 1a:94.6% (212/224), 1b:97.9% (47/48) | |||
| Cirrhosis | Naïve | 1a: 92.2% (59/64), 1b:100% (22/22) | TURQUOISE-II, phase 3 | Poordad et al., 2014 |
| Null response to PegIFNα/RBV | 1a:80% (40/50), 1b:100% (25/25) | |||
| Partial response to PegIFNα/RBV | 1a: 100% (11/11), 1b:85.7% (6/7) | |||
| Relapse to PegIFNα/RBV | 1a: 93.3% (14/15), 1b:100% (14/14) | |||
| Naïve | 1a:95.5% (190/199), 1b:100% (133/133) | Real-world study | Ioannou et al., 2016 | |
| Experienced | 1a:96.6% (56/58), 1b:100% (60/60) | |||
SVR24 rates were evaluated in the clinical study.
Table 15.
Efficacy of 12.5 mg ombitasvir + 75 mg paritaprevir + 50 mg ritonavir fixed-dose two pills QD plus 250 mg dasabuvir BID plus ribavirin for 24w.
| Cirrhosis | Prior treatment | SVR12 rate in GT-1 | Study and trial phase | Ref. |
|---|---|---|---|---|
| Cirrhosis | Naïve | 1a: 92.9% (52/56), 1b:100% (18/18) | TURQUOISE-II, phase 3 | Poordad et al., 2014 |
| Null response to PegIFNα/RBV | 1a:92.9% (39/42), 1b:100% (20/20) | |||
| Partial response to PegIFNα/RBV | 1a: 100% (10/10), 1b:100% (3/3) | |||
| Relapse to PegIFNα/RBV | 1a: 100% (13/13), 1b:100% (10/10) |
4.7. Ombitasvir + paritaprevir + ritonavir (Technivie™)
In July 2015, the FDA approved the fixed-dose combination of ombitasvir plus paritaprevir plus ritonavir with or without ribavirin for GT4-infected patients without cirrhosis. Technivie™ is the first FDA-approved therapy solely against the GT4 infections. Basically, Technivie™ lacks dasabuvir in comparison to Viekira Pak™, while both products are manufactured by Abbvie.
Several clinical studies such as the PEARL-I study (Lawitz et al., 2015c, Hezode et al., 2015) and the GIFT-I study (Kumada et al., 2015b) were designed to illustrate the efficacy of Technivie™ (Table 16 ). As for the fixed-dose combination of 12.5 mg ombitasvir + 75 mg paritaprevir + 50 mg ritonavir taken two tablets once daily for 12 weeks, the SVR12 rates were 95% (400/421) in GT1-infected patients without cirrhosis, 95.7% (135/141) in GT1-infected patients with cirrhosis, and 90.9% (40/44) in GT4-infected patients without cirrhosis. In the PEARL-I study (Hezode et al., 2015), the SVR12 rate of Technivie™ plus ribavirin achieved 100% in 91 GT4-infected patients without cirrhosis. The most common adverse events were asthenia, nausea, fatigue, and insomnia.
Table 16.
Efficacy of Technivie™ with or without ribavirin for 12 weeks.
| Cirrhosis | Prior treatment | SVR12 rate |
Study and trial phase | Ref. | ||
|---|---|---|---|---|---|---|
| GT-1 1b | GT-2 | GT-4 | ||||
| 12.5 mg ombitasvir + 75 mg paritaprevir + 50 mg ritonavir fixed-dose two pills QD for 12w | ||||||
| No cirrhosis | Experienced | 88.9% (16/18) | 72.2% (13/18) | Phase 2 | Chayama et al., 2015 | |
| Experienced | 90% (36/40) | PEARL-I, phase 2b | Lawitz et al., 2015c | |||
| Naïve | 95.2% (40/42) | 90.9% (40/44) | PEARL-I, phase 2b | Hezode et al., 2015 | ||
| Naïve | 95.7% (198/207) | GIFT-I, phase 3 | Kumada et al., 2015b | |||
| Experienced | 96.5% (110/114) | |||||
| Cirrhosis |
Naïve | 97.9% (46/47) | PEARL-I, phase 2b | Lawitz et al., 2015c | ||
| Experienced | 96.2% (50/52) | |||||
| Naïve | 100% (9/9) | GIFT-I, phase 3 |
Kumada et al., 2015b |
|||
| Experienced | 90.9% (30/33) | |||||
| 12.5 mg ombitasvir + 75 mg paritaprevir + 50 mg ritonavir fixed-dose two pills QD plus ribavirin BID for 12w | ||||||
| No cirrhosis | Naïve | 100% (42/42) | PEARL-I, phase 2b | Hezode et al., 2015 | ||
| Experienced | 100% (49/49) | |||||
4.8. Daclatasvir (Daklinza™) + sofosbuvir (Sovaldi®)
In July 2015, the FDA approved the clinical use of 60 mg daclatasvir QD plus 400 mg sofosbuvir QD with or without ribavirin for 12 weeks against HCV genotype 1 or 3 infections. Noteworthy, daclatasvir and sofosbuvir bind to the NS5A and NS5B proteins, respectively. Daclatasvir (BMS-790052) was designed by the extensive optimization of a leading iminothiazolidinone (Fig. 3) obtained from the high throughput phenotypic screening (Belema and Meanwell, 2014). Daclatasvir in the symmetric and dimeric form may bind at positions 31 and 93 of HCV NS5A, thus interfering with the protein-protein interactions at the membrane interface (Nettles et al., 2014). Moreover, the cooperative interaction between daclatasvir and other NS5A inhibitors (e.g. syn-395) suggests the possible synergistic anti-HCV activity, providing additional options for HCV combination therapy (Sun et al., 2015). In HCV replicons, the EC50 values of daclatasvir achieved 0.05 ± 0.013 nM against GT1a, 0.009 ± 0.004 nM against GT1b, 0.071 ± 0.017 nM against GT2a, 0.146 ± 0.034 nM against GT3a, 0.012 ± 0.004 nM against GT4a, and 0.033 ± 0.01 nM against GT5a (Table 2). Moreover, pharmacokinetic analyses in animal models (e.g. rat, dog, cynomolgus monkey) further supported the potent antiviral activity of daclatasvir (Belema and Meanwell, 2014). In addition to the combination of daclatasvir plus sofosbuvir, daclatasvir was previously considered to be used with asunaprevir (Poordad et al., 2015, Muir et al., 2015, Toyota et al., 2016). Although the combination of daclatasvir plus asunaprevir was declined by the FDA, this regimen was approved in Japan.
Table 2.
Antiviral activity of FDA-approved compounds in HCV cell culture.
| Protein | Compound | In vitro activity (EC50, nM) |
Ref. | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| GT-1a | GT-1b | GT-2a | GT-2b | GT-3a | GT-4a | GT-5a | GT-6a | |||
| NS3/4A | Boceprevir (SCH503034) | 196 ± 56 | 251 ± 71 | 283 ± 36 | 315 ± 30 | 159 ± 5 | – | – | – | Silva et al., 2013 |
| Telaprevir (VX-950) | 395 ± 16 | 285 ± 60 | 252 ± 54 | 402 ± 52 | 953 ± 103 | – | – | – | Silva et al., 2013 | |
| Paritaprevir (ABT-450) | 1.0 ± 0.33 | 0.21 ± 0.07 | 5.3 ± 1.2 | – | 19 ± 5.2 | 0.09 ± 0.03 | – | 0.69 ± 0.09 | Pilot-Matias et al., 2015 | |
| Grazoprevir (MK-5172) | 0.4 ± 0.2 | 0.5 ± 0.3 | 2.3 ± 1.2 | 3.7 ± 1.1 | 2.1 ± 1 | 0.3 ± 0.2 | 6.6 ± 0.6 | 0.9 ± 0.1 | Lahser et al., 2016 | |
| Simeprevir (TMC435) | 28.4 (19–39.7) | 8.1 (4.5–11.9) | – | – | – | – | – | – | Lin et al., 2009 | |
| NS5A | Daclatasvir (BMS-790052) | 0.05 ± 0.013 | 0.009 ± 0.004 | 0.071 ± 0.017 | – | 0.146 ± 0.034 | 0.012 ± 0.004 | 0.033 ± 0.01 | Gao et al., 2010 | |
| Ledipasvir (GS-5885) | 0.031 | 0.004 | 21 | 16 | 168 | 0.39 | 0.15 | 1.1 | Cheng et al., 2016 | |
| Ombitasvir (ABT-267) | 0.0141 ± 0.0068 | 0.005 ± 0.0019 | 0.0124 ± 0.0027 | 0.0043 ± 0.0012 | 0.0193 ± 0.0058 | 0.00171 ± 0.00088 | 0.0043 ± 0.0009 | 0.415 ± 0.097 | DeGoey et al., 2014 | |
| Elbasvir (MK-8742) | 0.004 ± 0.002 | 0.003 ± 0.001 | 0.003 ± 0.001 | 3.4 ± 2.6 | 0.14 ± 0.09 | 0.0003 ± 0.0001 | 0.001 ± 0.001 | 0.009 ± 0.006 | Lahser et al., 2016 | |
| Velpatasvir (GS-5816) | 0.013 | 0.015 | 0.009 | 0.01 | 0.013 | 0.009 | 0.059 | 0.007 | Cheng et al., 2013 | |
| NS5B | Sofosbuvir (GS-7977) | 44 ± 4.7 | 48 ± 13 | 37 ± 3.6 | 20 ± 4.4 | 16 ± 3.4 | – | – | – | Lam et al., 2012 |
| Dasabuvir (ABT-333) | 7.7 ± 3.8 | 1.8 ± 0.98 | – | – | – | – | – | – | Kati et al., 2015 | |
-: Unavailable data. Information of HCV strains and experimental settings is available in the literature.
The efficacy of daclatasvir plus sofosbuvir was proved in several clinical studies (Table 17 ) such as A1444040 (Sulkowski et al., 2014a), ALLY-1 (Poordad et al., 2016a), ALLY-3 (Nelson et al., 2015), and ALLY-3+ (Leroy et al., 2016). Here, we attempted to estimate drug efficacy by merging all clinical data regardless of the distinct nature between different clinical trials. (i) Regarding the treatment of 60 mg daclatasvir + 400 mg sofosbuvir QD for 12w, the SVR12 rates were 99% (100/101) in GT1-infected patients without cirrhosis, 88.8% (103/116) in GT1-infected patients with cirrhosis, 96.3% (105/109) in GT3-infected patients without cirrhosis, and 62.5% (20/32) in GT3-infected patients with cirrhosis (Table 17). (ii) Regarding the treatment of 60 mg daclatasvir + 400 mg sofosbuvir QD + ribavirin for 12w, the SVR12 rates were 100% (33/33) in GT1-infected patients without cirrhosis versus 92% (23/25) with cirrhosis, and 94.1% (16/17) in GT3-infected patients without cirrhosis versus 83.3% (15/18) with cirrhosis (Table 17). In a real-world study enrolling 485 patients, SVR12 rates of daclatasvir plus sofosbuvir achieved more than 90% regardless of HCV genotypes, cirrhosis, liver transplant or HIV/HCV coinfection status (Welzel et al., 2016b). The most common adverse events in clinical studies were headache and fatigue.
Table 17.
Efficacy of 60 mg daclatasvir + 400 mg sofosbuvir QD with or without ribavirin for 12 weeks.
| Cirrhosis | Prior treatment | SVR12 rate |
Study and trial phase | Ref. | ||
|---|---|---|---|---|---|---|
| GT-1 | GT-2 | GT-3 | ||||
| 60 mg daclatasvir + 400 mg sofosbuvir QD for 12w | ||||||
| No cirrhosis | Naïve | 100% (35/35) | A1444040, phase 3 | Sulkowski et al., 2014a | ||
| Naïve | 97.3% (73/75) | ALLY-3, phase 3 | Nelson et al., 2015 | |||
| Experienced | 94.1% (32/34) | |||||
| Experienced or naive | ? | ? | ANRS CO23 CUPILT | Coilly et al., 2016 | ||
| Naïve | 100% (25/25) | ANRS/AFEF Hepather | Pol et al., 2017 | |||
| Experienced | 97.6% (40/41) | |||||
| Cirrhosis |
Naïve | 100% (6/6) | AI444040, phase 3 | Sulkowski et al., 2014a | ||
| Naïve | 1a: 83.3% (5/6), 1b: 100% (1/1) | ALLY-1, phase 3 | Poordad et al., 2016a | |||
| Experienced | 1a: 100% (7/7), 1b: 100% (2/2) | |||||
| Naïve | 57.9% (11/19) | ALLY-3, phase 3 | Nelson et al., 2015 | |||
| Experienced | 69.2% (9/13) | |||||
| Experienced or naive | ? | ? | ANRS CO23 CUPILT | Coilly et al., 2016 | ||
| Naïve | 79.5% (31/39) | ANRS/AFEF Hepather | Pol et al., 2017 | |||
| Experienced | 92.8% (51/55) | |||||
| Experienced | 66.7% (2/3) a | 40% (2/5) a | Real-world study | Cheung et al., 2016 | ||
| 60 mg daclatasvir + 400 mg sofosbuvir QD + ribavirin for 12w | ||||||
| No cirrhosis | Naïve | 1a:100% (8/8), 1b:100% (1/1) | 100% (5/5) | ALLY-1, phase 3 | Poordad et al., 2016a | |
| Experienced | 1a:100% (10/10), 1b:100% (5/5) | 83.3% (5/6) | ||||
| Experienced | 100% (2/2) | ALLY-3+, phase 3 | Leroy et al., 2016 | |||
| Naïve | 100% (4/4) | |||||
| Naïve | ?/36 | A1444040, phase 3 | Sulkowski et al., 2014a | |||
| Naïve | 100% (1/1) | ANRS/AFEF Hepather | Pol et al., 2017 | |||
| Experienced | 100% (8/8) | |||||
| Naïve | 100% (5/5) | Real-world study | Mangia et al., 2016 | |||
| Experienced | 100% (3/3) | |||||
| Cirrhosis | Naïve | 50% (1/2) | ALLY-3+, phase 3 | Leroy et al., 2016 | ||
| Experienced | 87.5% (14/16) | |||||
| Naïve | 100% (2/2) | ANRS/AFEF Hepather | Pol et al., 2017 | |||
| Experienced | 91.3% (21/23) | |||||
| Naïve | ?/5 | A1444040, phase 3 | Sulkowski et al., 2014a | |||
| Experienced | 88.2% (30/34) a | 69.2% (72/104)a | Real-world study | Cheung et al., 2016 | ||
?: Question marks indicate that the data was unavailable.
SVR24 rates were used in the study.
4.9. Elbasvir + grazoprevir (Zepatier™)
In January 2016, the FDA approved the fixed-dose combination of 100 mg grazoprevir plus 50 mg elbasvir with or without ribavirin against HCV genotype 1 or 4 infections (Table 1). Grazoprevir (MK-5172) and elbasvir (MK-8742) bind to HCV NS3/4A and NS5A, respectively. On the one hand, grazoprevir (Fig. 2) was discovered using a molecular modeling-derived strategy that optimized the contacts of protease inhibitors with a P2-to-P4 macrocyclic ring to the HCV NS3/4A active sites (Harper et al., 2012, Liverton et al., 2008). On the other hand, elbasvir was discovered by introducing a tetracyclic indole into the early clinical candidate MK-4882 (Fig. 3) that significantly improved its virologic profiles (Coburn et al., 2013). In HCV cell-based replicons, the EC50 values of grazoprevir were 0.4 nM against GT1a, 0.5 nM against GT1b, 2.3 nM against GT2a, 2.1 nM against GT3a, 0.3 nM against GT4a, 6.6 nM against GT5a, and 0.9 nM against GT6a (Lahser et al., 2016). Meanwhile, EC50 values of elbasvir achieved 0.004 nM against GT1a, 0.003 nM against GT1b, 0.003 nM against GT2a, 0.14 nM against GT3a, 0.0003 nM against GT4a, 0.001 nM against GT5a, and 0.009 nM against GT6 (Lahser et al., 2016). The combination of grazoprevir plus elbasvir not only exhibited a potent activity against HCV replication, but harbored a higher genetic barrier to drug resistance compared to individual compounds (Lahser et al., 2016). Overall, both grazoprevir and elbasvir attained potent antiviral activities in cell culture assays and animal models (Lahser et al., 2016, Harper et al., 2012, Coburn et al., 2013).
The efficacy of grazoprevir plus elbasvir was proven in many clinical trials such as C-EDGE (Zeuzem et al., 2015a), C-EDGE CO-STAR (Dore et al., 2016b), C-EDGE Head-2-Head (Sperl et al., 2016), C-EDGE TE (Kwo et al., 2017), C-SURFER (Roth et al., 2015), C-SCAPE (Brown et al., 2015), C-WORTHY (Sulkowski et al., 2015, Lawitz et al., 2015d), and C-SALVAGE (Forns et al., 2015b). Here, we attempted to estimate drug efficacy by merging all clinical data regardless of the distinct nature between different clinical trials (Table 18 ). (i) Regarding the therapy of 100 mg grazoprevir QD + 50 mg elbasvir QD for 12w, the SVR12 rates were 95.5% (751/786) in GT1-infected patients without cirrhosis, 96.3% (181/188) in GT1-infected patients with cirrhosis, 94.1% (32/34) in GT4-infected patients without cirrhosis, and 63.2% (12/19) in GT6-infected patients without cirrhosis (Table 18). (ii) Regarding the treatment of 100 mg grazoprevir QD + 50 mg elbasvir QD + RBV BID for 12w, its SVR12 rates fulfilled 94.6% (142/150) in GT1-infected patients without cirrhosis, and 94.8% (73/77) in GT1-infected patients with cirrhosis. With limited number of enrolled patients described in the C-SCAPE study (Brown et al., 2015), the SVR12 rates in non-cirrhotic patients were 80% (24/30), 100% (10/10), 100% (4/4), and 75% (3/4) against GT2, GT4, GT5, or GT6 infections, respectively. Due to the enrollment of patients co-infected with HCV and HIV in the C-EDGE TE study (Kwo et al., 2017), we were unable to obtain the SVR12 data of grazoprevir + elbasvir + RBV to treat HCV mono-infections. The most common side effects of Zepatier™ were anemia and headache. Furthermore, NS5A polymorphisms at 4 amino acid positions (M28, Q30, L31, Y93) may reduce the treatment efficacy in clinical trials (Komatsu et al., 2017). Overall, the combination of grazoprevir plus elbasvir with or without ribavirin is effective and safe for patients with GT1 or GT4 infections (see Table 19).
Table 18.
Efficacy of Zepatier™ with or without ribavirin in phase 2 and 3 clinical trials.
| Cirrhosis | Prior treatment | SVR12 rate |
Study and trial phase * | Ref. | ||||
|---|---|---|---|---|---|---|---|---|
| GT-1 | GT-2 | GT-4 | GT-5 | GT-6 | ||||
| 100 mg grazoprevir QD + 50 mg elbasvir QD for 12w | ||||||||
| No cirrhosis | Naïve | 97.7% (43/44) | C-WORTHY, phase 2 | Sulkowski et al., 2015 | ||||
| Experienced | 89.5% (17/19) | Lawitz et al., 2015d | ||||||
| Naïve | 1a: 91.7% (144/157), 1b: 97.9% (95/97) |
100% (16/16) | 80% (8/10) | C-EDGE, phase 3 | Zeuzem et al., 2015a | |||
| Naïve | 100% (92/92) | C-SURFER, phase 3 | Roth et al., 2015 | |||||
| Experienced | 94.4% (17/18) | |||||||
| Naïve or Experienced | ? | ? | C-EDGE Head-2-Head, phase 3 | Sperl et al., 2016 | ||||
| Naïve | 1a: 94.5% (104/110), 1b: 90.9% (20/22) |
87.5% (7/8) | 20% (1/5) | C-EDGE CO-STAR, phase 3 | Dore et al., 2016b | |||
| Naïve | 90% (9/10) | 25% (1/4) | 75% (3/4) | C-SCAPE, phase 2 | Brown et al., 2015 | |||
| Cirrhosis |
Naïve | 96.6% (28/29) | C-WORTHY, phase 2 | Lawitz et al., 2015d | ||||
| Null response | 92.9% (13/14) | |||||||
| Naïve | 100% (4/4) | C-SURFER, phase 3 | Roth et al., 2015 | |||||
| Experienced | 100% (2/2) | |||||||
| Naïve or Experienced | ? | ? | C-EDGE Head-2-Head, phase 3 | Sperl et al., 2016 | ||||
| Naïve | 1a: 93.3% (28/30), 1b: 100% (6/6) |
100% (4/4) | C-EDGE CO-STAR, phase 3 | Dore et al., 2016b | ||||
| Naïve | 1a: 94.1% (32/34), 1b: 100% (34/34) |
100% (2/2) | C-EDGE, phase 3 | Zeuzem et al., 2015a | ||||
| 100 mg grazoprevir QD + 50 mg elbasvir QD + ribavirin BID for 12w | ||||||||
| No cirrhosis | Experienced | 95.2% (20/21) | C-WORTHY, phase 2 | Lawitz et al., 2015d | ||||
| Naïve | 92.9% (79/85) | Sulkowski et al., 2015 | ||||||
| Naïve | 80% (24/30) | 100% (10/10) | 100% (4/4) | 75% (3/4) | C-SCAPE, phase 2 | Brown et al., 2015 | ||
| PI-treated | 97.7% (43/44) | C-SALVAGE, phase 2 | Forns et al., 2015b | |||||
| Cirrhosis |
PI-treated | 94.1% (32/34) | ||||||
| Naïve | 96.9% (31/32) | C-WORTHY, phase 2 |
Lawitz et al., 2015d |
|||||
| Null response | 90.9% (10/11) | |||||||
| 100 mg grazoprevir QD + 50 mg elbasvir QD + ribavirin BID for 16w | ||||||||
| No cirrhosis | Null or partial response to PegIFNα/RBV | ? | ? | C-EDGE TE, phase 3 | Kwo et al., 2017 | |||
| Cirrhosis | ? | ? | ||||||
?: Question marks indicate that the SVR12 data was unavailable in literature.
Table 19.
Efficacy of Epclusa® in phase 2 and 3 clinical trials.
| Cirrhosis | Prior treatment | SVR12 rate |
Study and trial phase | Ref. | |||||
|---|---|---|---|---|---|---|---|---|---|
| GT-1 | GT-2 | GT-3 | GT-4 | GT-5 | GT-6 | ||||
| 400 mg sofosbuvir + 100 mg velpatasvir fixed-dose, single pill, QD for 12w | |||||||||
| No cirrhosis | Experienced | 100% (20/20) | 100% (27/27) | GS-US-342-0109, phase 2 | Pianko et al., 2015 | ||||
| Naïve | 100% (28/28) | 100% (10/10) | 92.6% (25/27) | 85.7% (6/7) | 100% (5/5) | Phase 2 | Everson et al., 2015 | ||
| Naïve or experienced | 1a: 97.5% (157/161), 1b: 100% (94/94) |
100% (93/93) | 100% (89/89) | 96.6% (28/29) | 100% (35/35) | ASTRAL-1, phase 3 | Feld et al., 2015a | ||
| Naïve | 99% (99/100) | 98.2% (160/163) | ASTRAL-2, ASTRAL-3, phase 3 | Foster et al., 2015b | |||||
| Experienced | 100% (15/15) | 91.2% (31/34) | |||||||
| Cirrhosis |
Experienced | 100% (7/7) | 88.5% (23/26) | GS-US-342-0109, phase 2 | Pianko et al., 2015 | ||||
| Naïve or experienced | 1a:100% (49/49), 1b: 95.8% (23/24) |
100% (10/10) | 100% (27/27) | 100% (5/5) | 100% (6/6) | ASTRAL-1, phase 3 | Feld et al., 2015a | ||
| Naïve | 100% (15/15) | 93% (40/43) | ASTRAL-2, ASTRAL-3, phase 3 | Foster et al., 2015b | |||||
| Experienced | 100% (4/4) | 89.2% (33/37) | |||||||
| Naïve or experienced | 1a: 88% (44/50), 1b: 88.9% (16/18) |
100% (4/4) | 50% (7/14) | 100% (4/4) | ASTRAL-4, phase 3 | Curry et al., 2015 | |||
| 400 mg sofosbuvir + 100 mg velpatasvir fixed-dose, single pill, QD + ribavirin for 12w | |||||||||
| No cirrhosis | Experienced | 100% (18/18) | 100% (26/26) | GS-US-342-0109, phase 2 | Pianko et al., 2015 | ||||
| Cirrhosis | Experienced | 90% (9/10) | 96.2% (25/26) | GS-US-342-0109, phase 2 | Pianko et al., 2015 | ||||
| Naïve or Experienced | 1a: 94.4% (51/54), 1b: 100% (14/14) |
100% (4/4) | 84.6% (11/13) | 100% (2/2) | ASTRAL-4, phase 3 | Curry et al., 2015 | |||
The combination of 100 mg grazoprevir + 50 mg elbasvir + 400 mg sofosbuvir was recently evaluated in the phase 2 C-SWIFT study (Lawitz et al., 2016b). After the therapy of this triple-drug combination at 6 or 8 weeks, treatment-naïve patients infected with GT1 or GT3 infections demonstrated high SVR12 rates (>80%) (Lawitz et al., 2016b). Such findings suggest that an NS3/4A inhibitor plus an NS5A inhibitor and an NS5B inhibitor may offer better SVR12 rates and short-duration therapy.
4.10. Sofosbuvir + velpatasvir (Epclusa®)
In June 2016, the FDA approved Epclusa® as the first fixed-dose combination of 400 mg sofosbuvir plus 100 mg velpatasvir (GS-5816) with or without ribavirin against HCV genotype 1 to 6 infections. Epclusa® is the first pan-genotypic therapy approved for the treatment of all HCV genotypes except genotype 7. While the global prevalence of genotype 7 is rather low (Murphy et al., 2015), a case report showed the treatment success of Epclusa® in one patient infected with HCV genotype 7 (Schreiber et al., 2016). As the key component of Epclusa®, velpatasvir (Fig. 3) was discovered as a second-generation NS5A inhibitor with potent antiviral activity in cell culture assays. EC50 values of velpatasvir were 0.013 nM against GT1a, 0.015 nM against GT1b, 0.009 nM against GT2a, 0.01 nM against GT2b, 0.013 nM against GT3a, 0.009 nM against GT4, 0.059 nM against GT5, and 0.007 nM against GT6 (Cheng et al., 2013). Moreover, sofosbuvir is the best-in-class NS5B inhibitor manufactured by Gilead Sciences. Thus the fast approval of sofosbuvir plus velpatasvir marks a new era of anti-HCV therapies that effectively cure the majority of HCV-infected patients regardless of HCV genotypes. Unlike most FDA-approved therapies which require 12- to 24-week treatment, Epclusa® also attained a promising efficacy at 8 weeks (Everson et al., 2015).
Effectiveness of sofosbuvir plus velpatasvir was demonstrated in phase 2 and 3 clinical studies such as ASTRAL-1 (Feld et al., 2015a), ASTRAL-2 (Foster et al., 2015b), ASTRAL-3 (Foster et al., 2015b), and ASTRAL-4 (Curry et al., 2015) (see summary in Table 19). Here, we attempted to collect treatment outcomes and to estimate drug efficacy with integrated data regardless of the distinct nature between different clinical trials. (i) As for the fixed-dose combination of 400 mg sofosbuvir + 100 mg velpatasvir once daily for 12w, the SVR12 rates were 98.7% (299/303) in GT1-infected patients without cirrhosis versus 93.9% (139/148) with cirrhosis, 99.5% (217/218) in GT2-infected patients without cirrhosis versus 100% (33/33) with cirrhosis, 96.8% (243/251) in GT3-infected patients without cirrhosis versus 85.8% (103/120) with cirrhosis, 98.9% (95/96) in GT4-infected patients without cirrhosis versus 100% (31/31) with cirrhosis, 96.5% (28/29) in GT5-infected patients without cirrhosis versus 100% (5/5) with cirrhosis, and 100% (40/40) in GT6-infected patients without cirrhosis versus 100% (6/6) with cirrhosis (Table 19). (ii) As for the fixed-dose combination of 400 mg sofosbuvir + 100 mg velpatasvir once daily plus ribavirin for 12w, its SVR12 scored 100% (18/18) in GT1-infected patients without cirrhosis versus 94.8% (74/78) with cirrhosis, and 100% (26/26) in GT3-infected patients without cirrhosis versus 92.3% (36/39) with cirrhosis (Table 19). The most common adverse events observed in clinical studies were nausea, headache, fatigue, insomnia, anemia, and diarrhea.
5. New agents under development
During the past three years, advancements of HCV drug discovery have been made to produce a large amount of new inhibitors with better potency and safety profiles. In our previous reviews, we described experimental compounds against HCV infections (De Clercq, 2015, De Clercq, 2012, De Clercq, 2014, De Clercq and Li, 2016). In this section, we update the recent progress of anti-HCV agents targeting NS3/4A (Fig. 2), NS4B (Fig. 6 ), NS5A (Fig. 3), NS5B (Fig. 4, Fig. 5), E1/E2 or p7 proteins (Fig. 7 ). Immuno-stimulators and host targeting agents that inhibit host proteins are also summarized (see Table 20 , Fig. 8 ).
Fig. 6.
Chemical formulas of experimental NS4B inhibitors fromSarrazin, 2016, AASLD/IDSA HCV Guidance Panel, 2015, European Association for Study of Liver, 2015.
Fig. 7.
Chemical formulas of experimental E1/E2 inhibitors from (58) to (62) and the tertiary structure of p7 and its experimental inhibitors from (63) to (64). Six units of the hexameric p7 channel are colored accordingly (PDB code: 2M6X). The drug binding site is located in the center of HCV p7 channel (OuYang et al., 2013).
Table 20.
Summary of potent HCV inhibitors explored between 2011 and 2016.
| Drug type | Drug name | Current stage |
|---|---|---|
| NS3/4A inhibitor | Asunaprevir (BMS-650032), boceprevir (SCH503034), telaprevir (VX-950), paritaprevir (ABT-450), grazoprevir (MK-5172), simeprevir (TMC435), vaniprevir (MK-7009) | Approved drugs |
| Voxilaprevir (GS-9857), glecaprevir (ABT-493), danoprevir (ITMN-191, R7227), vedroprevir (GS-9451) a, faldaprevir a, narlaprevir (SCH900518) a | Clinical tests | |
| BMS-605339, MK-8831, BMS-890068 | Preclinical tests | |
| NS4B inhibitor | PTC725, piperazinone derivatives, imidazo[2,1-b]thiazole agents | Preclinical tests |
| NS5A inhibitor | Daclatasvir (BMS-790052), ledipasvir (GS-5885), ombitasvir (ABT-267), elbasvir (MK-8742), velpatasvir (GS-5816) | Approved drugs |
| Pibrentasvir (ABT-530), ravidasvir (PPI-668), GSK2336805, ruzasvir (MK-8408), EDP-239, samatasvir (IDX719) a | Clinical tests | |
| Biphenylimidazole analogues, AV4025, disulfiram | Preclinical tests | |
| NS5B nucleoside inhibitor | Sofosbuvir (GS-7977, PSI-7977) | Approved drugs |
| MK-3682, mericitabine (RG7128) a, GS-6620 a, JNJ-54257099 a | Clinical tests | |
| NS5B non-nucleoside inhibitor | Dasabuvir (ABT-333) | Approved drugs |
| Beclabuvir (BMS-791325), TMC647055, GS-9669, filibuvira, lomibuvir (VX-222)a, tegobuvir (GS-9190)a, deleobuvir (BI207127) a | Clinical tests | |
| 6-aminoquinolone derivatives, pyrazolobenzothiazines | Preclinical tests | |
| E1/E2, p7 inhibitor | Adamantane, chlorcyclizine, cynaropicrin, flunarizine, grosheimol, saikosaponin b2, rimantadine, benzimidazole derivative B5, | Preclinical tests |
| Immuno-stimulator and cellular protein inhibitor | ITX-5061, alisporivir (DEB025) a | Clinical tests |
| NIM258, MA026, soraphen A, isothiazolo[5,4-b]pyridines, phenyl–pyrrolidine derivatives, bis-amide derivatives | Preclinical tests |
Discontinued compounds. See details in a recent review addressing the discontinued HCV drugs (Gentile et al., 2015).
Fig. 8.
Cellular protein inhibitors and immuno-stimulators from (65) to (72). Tertiary structure of host protein cyclophilin A in complex with phenyl–pyrrolidine 31 is visualized (PDB code: 3RDD). In addition, cyclophilin A inhibitors include alisporivir, bis-amide derivative 25, and NIM258 (Table 20). Other compounds target other host proteins to offer antiviral activity (see details in Section 5).
5.1. NS3/4A inhibitors
Development of NS3/4A inhibitors has been characterized in recent reviews (De Clercq, 2014, De Clercq and Li, 2016, McCauley and Rudd, 2016). Here, we highlight the latest advancement of danoprevir, voxilaprevir, vedroprevir, MK-8831, faldaprevir, ABT-493, BMS-605339, and BMS-890068. Discontinued NS3/4A inhibitors were GS-9256 (Sheng et al., 2012a), faldaprevir, and narlaprevir.
Voxilaprevir - Voxilaprevir (GS-9857, see Fig. 2) is an NS3/4A inhibitor entering advanced stages of clinical trials. The therapy of 100 mg voxilaprevir in combination with 100 mg velpatasvir plus 400 mg sofosbuvir once daily is now examined in phase 3 clinical trials. In previous phase 2 clinical trials investigating this triple-DAA therapy at 8 weeks, SVR12 rates were 100% (36/36) in treatment-naïve GT1-infected patients without cirrhosis, and 94% (31/33) in treatment-naïve GT1-infected patients with cirrhosis (Lawitz et al., 2016c). In addition, this 12-week treatment attained an SVR12 rate of 100% in DAA-experienced patients with or without cirrhosis (Lawitz et al., 2016c). Another phase 2 study further showed its high efficacy in patients infected with genotype 1, 2, 3, 4, or 6, demonstrating that the SVR12 rates were 100% (36/36) in treatment-experienced patients without cirrhosis versus 97% (28/29) in treatment-experienced patients with cirrhosis (Gane et al., 2016a). The third clinical trial investigated the 4w, 6w and 8w treatment of this combination therapy against genotype 1 or 3 infections, demonstrating that 8-week treatment provided high SVR12 rates in most treatment-naïve or -experienced patients with or without compensated cirrhosis (Gane et al., 2016b). In clinical trials, voxilaprevir, sofosbuvir plus velpatasvir was well-tolerated and caused mild or moderate adverse events (Lawitz et al., 2016c, Gane et al., 2016a, Gane et al., 2016b, Rodriguez-Torres et al., 2016). In October 2016, Gilead Sciences announced the latest findings from four phase 3 trials (POLARIS-1 to POLARIS-4) in which the SVR12 rates of once-daily single tablet containing voxilaprevir, sofosbuvir, and velpatasvir were more than 96% in treatment-failure patients infected with GT1 to GT6 (http://www.gilead.com/). On December 8, 2016, Gilead Sciences submitted the new drug application of sofosbuvir, velpatasvir plus voxilaprevir. Overall, this combination therapy offers short-duration treatment and potentially provides salvage therapy for DAA-experienced patients.
Vedroprevir - Vedroprevir (GS-9451) is a reversible noncovalent inhibitor that effectively binds to the active site of HCV NS3/4A protease (Sheng et al., 2012b). The EC50 values of vedroprevir were determined to be 13 nM and 5.4 nM in GT1a and GT1b replicon cell lines, respectively (Yang et al., 2014). Moreover, the pharmacokinetic properties of vedroprevir were shown in rats, dogs, and monkeys (Sheng et al., 2012b). In a phase 2 clinical trial, the combination of vedroprevir, ledipasvir, tegobuvir plus ribavirin led to an SVR12 rate of 63% in GT1-infected patients without cirrhosis (Wyles et al., 2014). In the phase 2 TRILOGY-2 study, the combination of vedroprevir plus ledipasvir and sofosbuvir for 8 weeks reached an SVR12 rate of 95% (21/22) in GT1-infected patients with cirrhosis (Lawitz et al., 2016d). In another phase 2a trial, 100% (20/20) of GT1-infected patients without cirrhosis maintained SVR12 after the treatment of vedroprevir plus ledipasvir and sofosbuvir for 6 weeks (Kohli et al., 2015a). As of October 2016, a phase 3 trial of vedroprevir has not been established in the drug pipelines of Gilead Sciences (www.gilead.com).
Danoprevir - Danoprevir (ITMN-191, RG7227) was discovered based on the joint efforts of the structure-based design, the investigation of structure-activity relationship, and the optimization of drug metabolism and pharmacokinetics (Jiang et al., 2014a). This macrocyclic noncovalent reversible NS3/4A inhibitor had a slow-off rate and exhibited favorable potency across multiple HCV genotypes (Jiang et al., 2014a). The IC50 values of danoprevir (Fig. 2) were 1.6 nM against GT2b, 3.5 nM against GT3a, and 0.2 nM–0.4 nM against GT1a, GT1b, GT4, GT5 or GT6 infection (Jiang et al., 2014a). Moreover, danoprevir may restore the insulin sensitivity in GT1-infected patients (Moucari et al., 2010). Early clinical studies supported the clinical use of danoprevir plus PegIFNα/RBV that offered modest potency and safety against GT1 infection (Gane et al., 2011, Gane et al., 2014b, Forestier et al., 2011, Marcellin et al., 2013). In the INFORM-1 trial, danoprevir plus mericitabine significantly reduced HCV RNA levels in GT1-infected patients (Gane et al., 2010). In the MATTERHORN study, the combination of danoprevir/r, mericitabine plus PegIFNα/RBV for 12 weeks was well-tolerated and yielded an SVR24 rate of 84.6% against GT1 infections (Feld et al., 2015b). In a phase 2a trial enrolling 25 GT1-infected patients without cirrhosis, the four-week treatment of danoprevir, ledipasvir plus sofosbuvir exhibited an SVR12 rate of 40% (10/25) (Kohli et al., 2015c). According to the information in ClinicalTrials.gov, a phase 3 trial of danoprevir has not been found.
Glecaprevir - Glecaprevir (ABT-493) and pibrentasvir (ABT-530) from AbbVie inhibit the activity of HCV NS3/4A (Fig. 2) and NS5A (Fig. 3), respectively. The efficacy and safety of 200 mg ABT-493 plus 120 mg ABT-530 in cirrhotic patients infected with GT1 or GT3 was demonstrated by phase 2 clinical trials (Gane et al., 2016c, Poordad et al., 2016b). The SVR12 rates succeeded by ABT-493 plus ABT-530 were 96% (26/27) of GT1-infected patients, and 96% (27/28) of GT3-infected patients (Gane et al., 2016c). Meanwhile, the SVR12 rate of ABT-493 plus ABT-530 and ribavirin reached up to 100% (27/27) among GT1-infected patients (Gane et al., 2016c). In the phase 2 MAGELLAN-I study, the SVR12 rate of 200 mg ABT-493 plus 120 mg ABT-530 reached 100% in 6 GT1-infected patients without cirrhosis (Poordad et al., 2016b). Phase 3 trials of ABT-493 and ABT-530 are ongoing.
Faldaprevir/deleobuvir - Faldaprevir (BI 201335) and deleobuvir (BI 207127) are two experimental inhibitors targeting NS3/4A (Fig. 2) and NS5B (Fig. 5), respectively. In the phase 2 SOUND-C2 study, faldaprevir and the nonnucleoside inhibitor deleobuvir plus ribavirin offered SVR12 rates ranging from 52% to 69% in treatment-naïve GT1-infected patients (Zeuzem et al., 2013). Although the degree of liver fibrosis may not affect the efficacy of faldaprevir plus deleobuvir and ribavirin (Zeuzem et al., 2015b), the SVR12 rate of this therapy was rather lower than that of the other DAAs. NS5B variations at amino acid position 499 may reduce the treatment response (Berger et al., 2016). Further pursuit of faldaprevir plus deleobuvir was discontinued in 2014.
Narlaprevir - Narlaprevir (SCH 900518, see Fig. 2) is a second-generation NS3/4A protease inhibitor derived from boceprevir (Arasappan et al., 2010). In comparison to boceprevir, narlaprevir showed better potency, pharmacokinetic profiles, and physicochemical characteristics (Arasappan et al., 2010). Early clinical studies suggested that narlaprevir plus PegIFN/RBV offered an SVR12 rate up to 59.3% (19/32) in GT1-infected patients (de Bruijne et al., 2010). After a single dose of 200 mg, narlaprevir exposures were higher in cirrhotic patients than in healthy patients (Isakov et al., 2016). A phase 3 trial of narlaprevir (ClinicalTrials, gov identifier: NCT00689390) was terminated due to post-marketing commitments. Further development of narlaprevir was discontinued.
BMS-605339 - BMS-605339 (Fig. 2) was discovered as an acylsulfonamide-based tripeptide to inhibit HCV NS3/4A protease (Scola et al., 2014a). Although the potential cardiovascular liabilities in a clinical trial of BMS-605339 immediately prompted its discontinuation, small modifications in its P2* isoquinolone ring led to the discovery of asunaprevir (BMS-650032) – a compound free of cardiovascular liabilities (Scola et al., 2014b). BMS-605339 has remained in the pre-clinical stage.
MK-8831 - MK-8831 (Fig. 2) with a novel spiro-proline macrocycle is a follow-up compound of MK-5172 (Neelamkavil et al., 2016). Based on rational computational modeling and structure-guided designs, MK-8831 was found to offer robust pan-genotypic activity and good coverage of NS3/4A resistant strains (Neelamkavil et al., 2016).
BMS-890068 - The optimization of the approved NS3/4A inhibitor asunaprevir led to a potent acyclic, tripeptidic, acyl sulfonamide inhibitor called BMS-890068 (Fig. 2) that enhanced potency, safety, metabolic stability, and pharmacokinetic profiles (Sun et al., 2016). BMS-890068 has remained in the pre-clinical stage.
5.2. NS4B inhibitors
As of today, there is no NS4B inhibitor approved by the FDA. A recent review highlighted the achievements made in the discovery of NS4B inhibitors, although most NS4B inhibitors remain in the preliminary stages (Cannalire et al., 2016).
PTC725 - NS4B inhibitor PTC725 (Fig. 6) was discovered through the optimization of 6-(indol-2-yl)pyridine-3-sulfonamides (Zhang et al., 2014). This compound exhibited potent activities against GT1 infections and offered favorable pharmacokinetic profiles in rats, dogs, and monkeys (Zhang et al., 2014). The clinical uses of PTC725 require further investigation.
2-oxadiazoloquinoline derivative - A novel NS4B inhibitor harboring a 2-oxadiazoloquinoline scaffold showed promising inhibitory activity in vitro. The EC50 values of this compound were 0.08 nM against GT1a, 0.1 nM against GT1b, 3 nM against GT2a, 3.7 nM against GT3a, 0.9 nM against GT4a, and 3.1 nM against GT6a (Phillips et al., 2014). Its clinical use requires further investigation.
Imidazo[2,1-b]thiazole derivative - Experimental NS4B inhibitors with the imidazo[2,1-b]thiazole scaffold yielded synergistic responses with simeprevir, daclatasvir, and sofosbuvir so as to lower drug doses for the inhibition of HCV GT1b infections (Wang et al., 2015). Clinical uses of these new NS4B compounds require further investigation.
Piperazinone - High-throughput drug screen identified piperazinone derivatives to effectively inhibit GT1 infections through a direct binding with HCV NS4B (Kakarla et al., 2014). Nevertheless, the piperazinone class was insufficient to inhibit GT2 infections; thus, its development was discontinued (Kakarla et al., 2014).
5.3. NS5A inhibitors
A number of experimental NS5A inhibitors are currently under development (Table 20). Although most of them remain preclinical candidates, several compounds (e.g. samatasvir, ravidasvir, GSK2336805) successfully advanced into clinical trials. In this section, we provide an overview of new NS5A inhibitors, including ABT-530, ruzasvir, ravidasvir, GSK2336805, EDP-239, samatasvir, biphenylimidazole analogues, and disulfiram (Fig. 3).
Pibrentasvir - Pibrentasvir (ABT-530) was tested in a phase 2 trial enrolling 10 treatment-naïve GT3-infected patients without cirrhosis (Poordad et al., 2016c). The treatment of ABT-530, paritaprevir, ritonavir plus ribavirin cured 9 of 10 patients without severe adverse events. Moreover, ABT-530 in combined with ABT-493 showed high efficacy and safety profiles in phase 2 clinical trials (see Section 5.1). Further development of ABT-530 is therefore expected.
Ruzasvir - Ruzasvir (MK-8408) is a potent next-generation NS5A inhibitor discovered by an iterative lead optimization so that compounds were stepwise screened against a select panel of HCV replicon cells (Asante-Appiah et al., 2014). This compound maintained an EC50 < 5 pM across HCV GT1 to GT6 (Asante-Appiah et al., 2014). MK-3682 is a uridine nucleotide analogue that targets HCV NS5B. In the C-CREST 1 and 2 phase 2 clinical studies, two triple-drug combinations (MK-3682 + grazoprevir + elbasvir, MK-3682 + grazoprevir + MK-8408) were examined in 240 treatment-naïve non-cirrhotic patients infected with GT1 to GT3 infections (Gane et al., 2016d). It has been shown that the 8-week regimen of 450 mg MK-3682, 100 mg grazoprevir plus 60 mg MK-8408 effectively gained 90.1% (55/61) of SVR24 against GT1 to GT3 infections (Gane et al., 2016d). Phase 2 clinical trials are ongoing.
Samatasvir - As a potent NS5A inhibitor, samatasvir (IDX719) selectively inhibited HCV replication (Bilello et al., 2014). Its EC50 values accomplished 4.1–6.2 pM against GT1a, 2.4 pM against GT1b, 21–24 pM against GT2a, 17–23 pM against GT3a, 2–6 pM against GT4a, and 18 pM against GT5a (Bilello et al., 2014). In a 3-day proof-of-concept study, the samatasvir-based monotherapy was well-tolerated and reduced HCV RNA levels substantially in 34 GT1-infected patients and 30 patients infected with GT2, GT3, or GT4 infections (Vince et al., 2014). In the absence of Merck and Janssen pipelines, samatasvir appears to be discontinued.
Ravidasvir - As an NS5A inhibitor, ravidasvir (PPI-668) is a dimeric benzimidazole–naphthylene– imidazole derivative. The EC50 values of this compound were up to 0.12 nM, 0.01 nM, and 1.14 nM against HCV GT1a, GT1b, and GT3a infections, respectively (Zhong et al., 2016). The efficacy and safety profiles of ravidasvir in combination with other inhibitors (e.g. faldaprevir, sofosbuvir) were demonstrated in preliminary clinical trials (Zhong et al., 2016). Phase 2 and 3 trials of ravidasvir are ongoing (ClinicalTrials, gov identifier: NCT02371408).
GSK2336805 - On the basis that ketal-based 4-spiropyrrolidines improved potency against NS5A GT1b mutants, GSK2336805 is a spiroketal pyrrolidine harboring the 1,4-dioxa-7-azaspiro[4.4] nonane motif was designed to effectively inhibit GT1b mutants bearing L31V and Y93H in NS5A (Kazmierski et al., 2014). In comparison to daclatasvir, GSK2336805 significantly reduced HCV RNA levels in a 20-day study (Kazmierski et al., 2014). In a phase 1 study, GSK2336805 plus PegIFN/RBV exhibited rapid and significant antiviral activity in GT1-infected patients (Wilfret et al., 2013). Furthermore, mutations in the N-terminal region of NS5A caused decreased activity of GSK2336805 (Walker et al., 2014). Ongoing trials are currently unavailable in the database of ClinicalTrials,gov.
EDP-239 - EDP-239 is a potent and selective compound that inhibits NS5A activity and interferes with HCV replication (Owens et al., 2016a). Resistance profiles of EDP-239 in a randomized clinical study revealed drug resistant mutations in NS5A such as L31M and Q30H/R for GT1a, L31M and Y93H for GT1b (Owens et al., 2016b). Ongoing trials for EDP-239 are currently unavailable in the database of ClinicalTrials,gov.
Biarylimidazole - A novel biarylimidazole chemotype 50b with potent inhibitory activity towards GT1a and GT1b was discovered in order to remove the embedded aniline moiety of early NS5A drug candidates that caused genotoxicity in various short-term tests (Belema et al., 2014).
AV4025 - As an active NS5A inhibitor, AV4025 containing 5-[4-(4-imidazol-4-yl-phenyl)-buta-1,3-diynyl]-1H-imidazole linkers offered potent antiviral activity (EC50 = 3.4 ± 0.2 pM for GT1b) and favorable pharmacokinetic features in rats and dogs (Ivachtchenko et al., 2014).
Disulfiram - As an old antialcoholism drug discovered in 1920s, disulfiram was recently identified to be a novel Zn-ejector that ejected Zn2+ from the labile Zn-site in NS5A, thus leading to the inhibition of HCV infection (Lee et al., 2016).
5.4. NS5B inhibitors
Inspired by two FDA-approved NS5B inhibitors (sofosbuvir, dasabuvir), many experimental compounds are currently under evaluation. Several candidates have reached advanced clinical trials. This section highlights recent progress of newly discovered NS5B inhibitors (see Table 20, Fig. 4, Fig. 5).
Beclabuvir - The introduction of a cyclopropyl moiety into the indolobenzazepine inhibitors led to the discovery of the nonnucleoside beclabuvir (BMS-791325) with favorable antiviral, safety, and pharmacokinetic properties (Gentles et al., 2014). Clinical trials were carried out to examine the combination of beclabuvir, daclatasvir plus asunaprevir with or without ribavirin (Poordad et al., 2015, Muir et al., 2015, Toyota et al., 2016, Everson et al., 2014, Everson et al., 2016, Hassanein et al., 2015). The SVR12 rates of 75 mg beclabuvir, 30 mg daclatasvir plus 200 mg asunaprevir were up to 100% (11/11) against GT4 in an exploratory study (Hassanein et al., 2015), 88.8% (71/80) against GT1 in a phase 2a study (Everson et al., 2016), 94% (15/16) against GT1 in another phase 2a study (Everson et al., 2014), 91.3% (379/415) against GT1 in the UNITY-1 study (Poordad et al., 2015), 90.1% (92/102) against GT1 in the UNITY-2 study (Muir et al., 2015), and 96% (208/217) against GT1 in a phase 3 study (Toyota et al., 2016). Overall, the triple-DAA regimen of beclabuvir plus daclatasvir and asunaprevir exerts promising activity against GT1 infection.
GS-9669 - Non-nucleoside analogue GS-9669 with the N-alkyl substituent and the N-acyl group was discovered through the optimization of lomibuvir and thiophene analogues (Lazerwith et al., 2014). GS-9669 binds to the thumb site II of HCV NS5B polymerase and inhibits viral replication (Gane et al., 2014a). In HCV replicon assays, the EC50 values of GS-9669 were less than 11 nM against GT1 and GT5, but less antiviral activity was rated against GT2 to GT4 (Fenaux et al., 2013). In the phase 2 TRILOGY-1 study, the combination of GS-9669 plus ledipasvir and sofosbuvir for 8 weeks reached SVR12 rates above 82% in the treatment of GT-infected patients with cirrhosis (Lawitz et al., 2016d). In another phase 2a trial, 95% (19/20) of GT1-infected patients without cirrhosis maintained SVR12 when they were treated with GS-9669 plus ledipasvir and sofosbuvir for 6 weeks (Kohli et al., 2015a). In a phase 2a trial enrolling 25 GT1-infected patients without cirrhosis, the four-week treatment of GS-9669, danoprevir, ledipasvir plus sofosbuvir had an SVR12 rate up to 20% (5/25) (Kohli et al., 2015c). Whether GS-9669 would enter phase 3 clinical trial remains unclear.
Thiophene carboxylate allosteric inhibitor - Similar to GS-9669, the improvement of lomibuvir led to the discovery of a novel thiophene carboxylate allosteric inhibitor called compound 23 (Court et al., 2016) (Fig. 5). This compound improved potency and physicochemical properties in vitro (Court et al., 2016). In HCV replicons, the EC50 values of compound 23 reached up to 37 nM and 23 nM against GT1a and GT1b, respectively (Court et al., 2016). This compound has remained in the pre-clinical phase.
Mericitabine - Mericitabine (RG7128) is the prodrug of cytidine nucleoside analogue RO5855 for the inhibition of HCV NS5B polymerase. Previously, mericitabine was considered to be combined with danoprevir against GT1 infection (Gane et al., 2010), or with PegIFN plus ribavirin against GT1 or GT4 infection (Pockros et al., 2013, Wedemeyer et al., 2013). The former therapy did not exhibit any severe adverse events in the INFORM-1 trial (Gane et al., 2010). The latter therapy had its SVR24 rates up to 56.8% in the JUMP-C trial (Pockros et al., 2013) and 50.6% in the PROPEL trial (Wedemeyer et al., 2013). Moreover, substitutions L159F and L320F in NS5B conferred low-level resistance to mericitabine and cross-resistance to sofosbuvir and GS-938 (Tong et al., 2014). In 2016, Roche discontinued mericitabine due to a decreased number of participants in the clinical trials.
Deleobuvir - Based on an initial hit from high-throughput screening over a compound library, non-nucleoside inhibitor deleobuvir (BI 207127) was optimized using NMR-guided conformational restrictions and scaffold replacements (LaPlante et al., 2014). In healthy patients, deleobuvir was well-tolerated and exhibited a moderate to high clearance with favorable pharmacokinetic profiles (Chen et al., 2015). Deleobuvir was discontinued in 2013.
DAPN-PD1 - As a novel NS5B inhibitor,-D-2′—C-methyl-2,6-diaminopurine-ribonucleotide (DAPN) phosphoramidate prodrug 1 (PD1) is metabolized intracellularly into two distinct bioactive nucleoside triphosphate (TP) analogues that effectively inhibit the NS5B-mediated RNA polymerization (Ehteshami et al., 2016). This compound presents a novel strategy that combines the intracellular delivery of two inhibitory metabolites with different incorporation profiles (Zhou et al., 2015).
TMC647055 - TMC647055 is a nonzwitterionic 17-membered-ring macrocycle that exhibits potent antiviral activity in respect of cross-genotypic coverage, virus suppression, and resistance selection (Cummings et al., 2014). As a nonnucleoside NS5B inhibitor, TMC647055 in combination with TMC435 was evaluated in phase 1 clinical trials; yet, its resistant mutations remain a concern (Wang et al., 2016). Information about the phase 2 trials of TMC647055 was not available in clinicaltrials.gov.
Filibuvir / VX-222 - Nonnucleoside inhibitors filibuvir (PF-00868554) and VX-222 (VCH-222) bind to the thumb II allosteric pocket of NS5B and prevent HCV subgenomic replicon (Yi et al., 2012). The EC50 values of filibuvir and VX-222 achieved up to 70 nM and 5 nM, respectively (Yi et al., 2012). Moreover, NS5B substitutions M423T and I482L could affect the antiviral activity of filibuvir and VX-222 (Yi et al., 2012). In phase 1 studies, filibuvir plus PegIFN/RBV was well-tolerated and induced significant RNA reductions in treatment-naïve patients infected with GT1 (Wagner et al., 2011). In phase 1 and 2 clinical studies, the thiophene-2-carboxylic acid derivative VX-222 showed effective potency and significant reductions of HCV RNA in GT1-infected patients (Jiang et al., 2014b). Development of filibuvir was discontinued in 2013, while a phase 3 trial of VX-222 is yet unavailable (clinicaltrials.gov).
GS-6620 - GS-6620 in the C-nucleoside class of NS5B inhibitors (De Clercq, 2016) was discovered during a series optimization of a 1’-cyano-2′—C-methyl 4-aza-7,9-dideaza adenosine analogue (Cho et al., 2014). C-nucleoside monophosphate prodrug GS-6620 exhibited potent activity against GT1 to GT6 infections; its EC50 values were between 0.048 and 0.68 M (Feng et al., 2014). Moreover, GS-6620 showed a high barrier to drug resistance in vitro (Feng et al., 2014). In October 2016, GS-6620 was absent in the drug pipeline of Gilead Sciences.
Tegobuvir - Tegobuvir (GS-9190) is an imidazopyridine derivative that binds to the -hairpin in the palm site of HCV NS5B (Eltahla et al., 2014, Shih et al., 2011). The EC50 values of tegobuvir were less than 16 nM, but > 100 nM for GT2 to GT6 (Wong et al., 2012). A phase 1b study showed that Y448H conferred drug resistance to tegobuvir in treatment-naïve GT1-infected patients receiving GS-9190 monotherapy. Altogether, the clinical use of tegobuvir is limited in that advanced DAAs offer pan-genotypic activity with better efficacy. Tegobuvir was discontinued in 2011.
JNJ-54257099 - As an NS5B inhibitor, JNJ-54257099 is a cyclic phosphate ester derivative in the class of 2’-deoxy-2’-spirooxetane uridine nucleotide prodrugs (Jonckers et al., 2016). This compound profoundly decreased HCV RNA levels in mouse models of HCV GT1a and GT3a infections in a dose-dependent manner (Jonckers et al., 2016). In 2016, a phase 1 trial of JNJ-54257099 was terminated (ClinicalTrials.gov identifier: NCT02510248).
6-aminoquinolone derivative - As a novel 6-aminoquinolone derivative, the 6-amino-7-[4-(2-pyridinyl)-1- piperazinyl] quinolone derivative 8 binds to the allosteric site of NS5B and exhibits a potent antiviral activity against HCV NS5B polymerase (EC50 = 3.03 M, IC50 = 0.069 M for GT1b) (Manfroni et al., 2014a). The derivative 8 has remained in the pre-clinical stages.
Pyrazolobenzothiazines - Novel pyrazolobenzothiazines were discovered to target the NS5B palm site I, exhibiting potent antiviral effect without anti-metabolic effect in HCV replicon assays (Manfroni et al., 2014b). This drug class has remained in the pre-clinical stage.
5.5. E1/E2 and p7 inhibitors
As of November 2016, no E1/E2 inhibitor has been approved by the FDA. A number of molecules (e.g. L-ficolin (Hamed et al., 2014)) can neutralize the viral glycoproteins E1 and E2, leading to the inhibition of viral attachment during the HCV viral entry. Although most E1/E2 inhibitors remain in preclinical studies, HCV entry inhibitors can be interesting because they offer an alternative strategy to clear HCV infections (Qian et al., 2016). Herein, we highlight newly discovered compounds that target HCV E1/E2 proteins (Fig. 7).
Benzimidazole derivative - In primary hepatocytes, a novel benzimidazole derivative B5 inhibited HCV infections in a dose-dependent and pan-genotypic manner (Vausselin et al., 2016). The IC50 values of B5 were approximately between 0.77 M and 2.93 M in HCV GT1 to GT6 replicons. While the benzimidazole derivative B5 may interfere with the HCV entry, the resistance profile of B5 was attributed to a single mutation F291I in HCV E1 (Vausselin et al., 2016).
Cynaropicrin/grosheimol - Natural products cynaropicrin and grosheimol were extracted from the wild Egyptian artichoke (Elsebai et al., 2015). These two compounds in the group of sesquiterpene lactones efficiently inhibited GT1 to GT7 infections (Elsebai et al., 2015). Although their mechanisms of action remain unclear, cynaropicrin and grosheimol may interfere with HCV viral entry (Elsebai et al., 2015).
Saikosaponin b2 - Saikosaponin b2 is a naturally occurring terpenoid extracted from Bupleurum kaoi root that acts on HCV glycoprotein E2, leading to the inhibition of HCV infection in the early stages (Lin et al., 2015). This natural product showed pan-genotypic activity and acts at non-cytotoxic concentrations (Lin et al., 2015). Clinical uses of saikosaponin b2 require further investigation.
Chlorcyclizine derivative - A chlorcyclizine derivative called compound 30 was optimized from the antihistamine piperazine drug called chlorcyclizine HCI using the structure-activity analysis (He et al., 2016). Compound 30 may act by the interruption of viral entry into host cells (He et al., 2015). This compound increased anti-HCV activity and selectivity in HCV replicon assays (He et al., 2016).
Flunarizine - Flunarizine was identified as a submicromolar HCV inhibitor in a whole life cycle screen of a compound library including clinically approved drugs (Perin et al., 2016). This compound targeted to the E1 fusion peptide and inhibited HCV membrane fusion in a genotype-dependent manner (Perin et al., 2016). While flunarizine is a calcium antagonist that effectively combats the pathophysiology of migraine, its anti-HCV activity is preferable for genotype 2 infections (Prigozhin and Modis, 2016).
Monoclonal antibodies - Human monoclonal antibodies with breadth of neutralization and synergy were explored for the inhibition of HCV GT1, GT2 and GT3 infections (Carlsen et al., 2014). These potent neutralizing antibodies target various epitopes on HCV E1/E2 envelope proteins (Carlsen et al., 2014).
Adamantane/rimantadine - When the structure of HCV p7 was fully crystalized, in silico compound selection identified promising agents (e.g. adamantane, rimantadine) that interfered with p7 based on high-throughput screening (Foster et al., 2014). Preliminary analyses showed the rational development of potent p7 drugs (Foster et al., 2014), but further clinical trials are still required.
5.6. Immuno-stimulators and cellular protein inhibitors
In this section, we provide an overview of newly discovered agents that inhibit host proteins (e.g. cyclophilin A, cyclin G associated kinase, scavenger receptor B1).
Alisporivir - Alisporivir (DEB025, see Fig. 8) is a nonimmune-suppressive compound that targets the host protein cyclophilin A to block the peptidyl-prolyl cis/trans isomerase activity (Pawlotsky et al., 2015). Additionally, alisporivir inhibits the interaction between cyclophilin A and NS5A in a dose-dependent manner (Coelmont et al., 2010). Of interest, alisporivir acts synergistically with NS5A inhibitors (e.g. daclatasvir, sofosbuvir) to achieve significant antiviral effects (Chatterji et al., 2014). Moreover, alisporivir stimulates antigen presentation and promotes antigen-specific CD8+ T cell activation by 40%, thereby leading to the significant anti-HCV activity (Esser-Nobis et al., 2016). In the phase 2 VITAL-1 study enrolling GT2- or GT3-infected patients, the SVR24 rate of alisporivir plus PegIFN and ribavirin (92%, 56/61) was higher than that of alisporivir alone (72%, 13/18) (Pawlotsky et al., 2015). Alisporivir was discontinued in phase 3 studies due to severe adverse events unassociated with cyclophilin inhibition (Ahmed-Belkacem et al., 2016).
Bis-amide derivative - To pursue cyclophilin inhibitors, a novel bis-amide derivative called compound 25 was discovered using molecular modeling-based design and structure-activity exploration (Yang et al., 2015). This compound efficiently inhibited HCV replication and restored host immune responses without acute toxicity in vitro and in vivo (Yang et al., 2015).
NIM258 - NIM258 (Fig. 8) is a modified cyclosporin analogue that acts as non-immunosuppressive cyclophilin A inhibitor with promising pharmacokinetic profiles against HCV infection (Fu et al., 2014). In comparison to alisporivir, NIM258 decreased transporter inhibition, but maintained comparable efficacy against cyclophilin A (Fu et al., 2014).
Phenyl–pyrrolidine derivative - Phenyl–pyrrolidine derivative 31 (Fig. 8) was discovered to inhibit cyclophilin A using nucleic magnetic resonance, X-ray crystallography and structure-based compound optimization (Ahmed-Belkacem et al., 2016). The EC50 value of this inhibitor was 0.4 ± 0.3 M against HCV1b in Huh7 cells. In addition, this inhibitor could be a broad-spectrum high-barrier-to-resistance inhibitor against HIV and coronaviruses as well (Ahmed-Belkacem et al., 2016).
Isothiazolo[5,4-b]pyridine - Isothiazolo[5,4-b]pyridines were developed to target cyclin G associated kinase (GAK) which is a serine/threonine protein kinase associated with cyclin G in cell cycle regulation (Kovackova et al., 2015). It is known that GAK is essential for HCV entry and assembly (Kovackova et al., 2015). Drug mechanisms of isothiazolo[5,4-b]pyridines were thereby traced to their inhibition upon HCV entry and assembly (Kovackova et al., 2015). Lead derivatives of isothiazolo[5,4-b]pyridines showed potent anti-HCV activity with Kd < 9 nM (Kovackova et al., 2015).
ITX-5061 - ITX-5061 (Fig. 8) is an inhibitor of scavenger receptor B1 - an essential receptor for HCV entry (Syder et al., 2011). As a host factor antagonist, ITX-5061 could be combined with DAAs without conferring cross-resistance in vitro (Zhu et al., 2012). In a phase 1b clinical trial, 150 mg ITX-5061 per day for up to 28 days was safe and well tolerated (Sulkowski et al., 2014b).
MA026 - MA026 (Fig. 8) is a lipocyclodepsipeptide isolated from the fermentation broth of Pseudomonas sp (Shimura et al., 2013). While MA026 effectively inhibits HCV entry, the possible antiviral mechanism can be traced to the interaction between MA026 and an HCV entry receptor called claudin-1 using the phase display screening and surface plasmon resonance binding analyses (Shimura et al., 2013).
Soraphen A - As a natural product, soraphen A is a myxobacterial metabolite that interferes with the membranous web formation, leading to the inhibition of HCV replication (Koutsoudakis et al., 2015). The EC50 values of soraphen A were up to 2.3 nM against HCV GT2a infection (Koutsoudakis et al., 2015).
6. Conclusions and future perspectives
In this review, we provide an overview of FDA-approved therapies and newly discovered agents against HCV GT1 to GT6 infections. Moreover, this study presents the first detailed survey of drug efficacy of all FDA-approved therapies based on more than 100 clinical trials and real-world studies. Similar to HIV cocktail therapies, HCV combination therapies containing two or three DAAs to block different stages of the viral life cycle can offer favorable inhibitory efficacy and low incidences of side effects. Unlike the first generation of anti-HCV drugs with pegylated interferons and ribavirin, many FDA-approved DAAs directly bind to HCV proteins (NS3/4A, NS5A, NS5B). Furthermore, the pursuit of next generation anti-HCV inhibitors yields a large number of investigational agents with novel mechanisms of drug actions. Most inhibitors have been synthesized to inhibit HCV proteins (E1/E2, p7, NS4B) or human proteins (e.g. cyclophilin A, cyclin G associated kinase, scavenger receptor B1). Accumulated over the past five years, a large pool of FDA-approved drugs and promising experimental inhibitors provides a strong reinforcement to cure HCV infections in most patients. Nevertheless, many challenges lie ahead to develop next generation DAAs against HCV infections in worldwide populations.
The first challenge is the development of effective therapies for difficult-to-treat populations such as HCV-infected patients with end-stage renal diseases (Morales and Fabrizi, 2015), HCV-infected patients before and after kidney transplantation (Ferenci, 2015, Gambato et al., 2014), HCV-infected patients with liver graft infection (Felmlee et al., 2016), and HCV-infected patients with compensated and decompensated cirrhosis (Ferenci et al., 2015). It has been suggested that treating HCV-infected patients early in their disease course may prevent HCV-related cirrhosis and its complications (AASLD/IDSA HCV Guidance Panel, 2015), whilst the pre-emptive DAA treatment may benefit the prevention and treatment of liver graft infection (Felmlee et al., 2016). A recent study reported unexpected high rates of early tumor recurrence after the treatment of DAAs in 103 HCV-infected patients with prior hepatocellular carcinoma (Reig et al., 2016). Despite the high potency of DAAs, the occurrence of liver cancer cannot be reduced in HCV-infected cirrhotic patients with sustained virologic response (Conti et al., 2016). Nevertheless, a following study integrating three distinct prospective cohorts showed no increased risk of HCC recurrence in 267 patients after DAA treatments (Thecollaborative st, 2016). Whether DAA treatments increase HCC occurrence or recurrence rates will remain a subject for debate until very large patient cohorts have emerged with a proper control arm to assess this important question (Llovet and Villanueva, 2016).
The second challenge is the demanding request of pan-genotypic drugs with minimal drug resistance. On the one hand, it is crucial to apply pan-genotypic therapies for all HCV genotypes, especially when genotyping tests are unavailable in resource-limited areas. Until today, Epclusa® is the only therapy approved for the treatment of GT1 to GT6 infections. On the other hand, drug resistance remains a concern, and natural variations in different genotypes may confer resistance to genotype-specific drugs (Sarrazin, 2016, Pawlotsky, 2016). For instance, NS5A resistance-associated substitutions were presented in 8–16% of GT1-infected patients prior to the treatment of ledipasvir plus sofosbuvir, while their presence exerted a negative impact on treatment outcomes (Zeuzem et al., 2017). Moreover, HCV GT3 variants within the NS5A region not only reduced sensitivity to nucleotide analogues (e.g. sofosbuvir) but also increased viral fitness in cell culture systems (Ramirez et al., 2016). In addition, many NS3/4A inhibitors show potent activities against GT1 but not GT3, because of the polymorphisms between HCV genotypes in the drug binding pocket, as well as the substantial loss of intermolecular hydrogen bonding interactions and dynamic cross-correlations between NS3/4A inhibitors and the active site of NS3/4A in GT3 (Soumana et al., 2016). Lists of HCV resistance-associated substitutions are available at (Sarrazin, 2016, Pawlotsky, 2016). Altogether, development of pan-genotypic drugs remains important.
The third challenge is the optimization of simple regimens with low pill burden and shorter treatment duration. Recent attempts have been made to shorten the course of anti-HCV treatment from the recommended 48 weeks to 8 weeks or even less. For instance, findings of an open-label phase 2a trial suggested that 3 weeks of response-guided therapy (e.g. sofosbuvir + ledipasvir + asunaprevir, sofosbuvir + daclatasvir + simeprevir, sofosbuvir + daclatasvir + asunaprevir) not only accomplished an SVR12 rate of 100%, but drastically reduced the cost of therapy, improved drug adherence, and eliminated the incidences of adverse events (Lau et al., 2016). In another phase 2 study, ledipasvir plus sofosbuvir for 6 weeks also exhibited an SVR12 of 100% in 20 patients with acute GT1 mono-infection (Deterding et al., 2017). Novel HCV therapeutics may aim at shorter treatment duration with optimal efficacy.
Given the breakthroughs achieved by the current DAAs, we anticipate that in the next decade we will witness the substantial decrease of HCV infections in global populations. The ultimate eradication of HCV infections also requires universal diagnosis of HCV infections, improving access to health care, and the potential implementation of a prophylactic HCV vaccine. To supplement this review, an update of HCV drug development will be available at our online platform (http://www.virusface.com).
Acknowledgements
We wholeheartedly thank Mrs. Christiane Callebaut for her proficient editorial assistance. This study was supported by the National Nature Science Foundation of China [31571368] and the Project of Innovation-driven Plan of Central South University [2016CX031].
Contributor Information
Guangdi Li, Email: liguangdi.research@gmail.com.
Erik De Clercq, Email: erik.declercq@kuleuven.be.
References
- AASLD/IDSA HCV Guidance Panel Hepatitis C guidance: AASLD-IDSA recommendations for testing, managing, and treating adults infected with hepatitis C virus. Hepatology. 2015;62:932–954. doi: 10.1002/hep.27950. [DOI] [PubMed] [Google Scholar]
- Abergel A., Metivier S., Samuel D., Jiang D., Kersey K., Pang P.S., Svarovskaia E., Knox S.J., Loustaud-Ratti V., Asselah T. Ledipasvir plus sofosbuvir for 12 weeks in patients with hepatitis C genotype 4 infection. Hepatology. 2016;64:1049–1056. doi: 10.1002/hep.28706. [DOI] [PubMed] [Google Scholar]
- Abergel A., Asselah T., Metivier S., Kersey K., Jiang D., Mo H., Pang P.S., Samuel D., Loustaud-Ratti V. Ledipasvir-sofosbuvir in patients with hepatitis C virus genotype 5 infection: an open-label, multicentre, single-arm, phase 2 study. Lancet Infect. Dis. 2016;16:459–464. doi: 10.1016/S1473-3099(15)00529-0. [DOI] [PubMed] [Google Scholar]
- Afdhal N., Zeuzem S., Kwo P., Chojkier M., Gitlin N., Puoti M., Romero-Gomez M., Zarski J.P., Agarwal K., Buggisch P., Foster G.R., Brau N., Buti M., Jacobson I.M., Subramanian G.M., Ding X., Mo H., Yang J.C., Pang P.S., Symonds W.T., McHutchison J.G., Muir A.J., Mangia A., Marcellin P., ION-1 Investigators Ledipasvir and sofosbuvir for untreated HCV genotype 1 infection. N. Engl. J. Med. 2014;370:1889–1898. doi: 10.1056/NEJMoa1402454. [DOI] [PubMed] [Google Scholar]
- Afdhal N., Reddy K.R., Nelson D.R., Lawitz E., Gordon S.C., Schiff E., Nahass R., Ghalib R., Gitlin N., Herring R., Lalezari J., Younes Z.H., Pockros P.J., Di Bisceglie A.M., Arora S., Subramanian G.M., Zhu Y., Dvory-Sobol H., Yang J.C., Pang P.S., Symonds W.T., McHutchison J.G., Muir A.J., Sulkowski M., Kwo P., ION-2 Investigators Ledipasvir and sofosbuvir for previously treated HCV genotype 1 infection. N. Engl. J. Med. 2014;370:1483–1493. doi: 10.1056/NEJMoa1316366. [DOI] [PubMed] [Google Scholar]
- Aghemo A., Rumi M.G., Colombo M. Pegylated interferons alpha2a and alpha2b in the treatment of chronic hepatitis C. Nat. Rev. Gastroenterol. Hepatol. 2010;7:485–494. doi: 10.1038/nrgastro.2010.101. [DOI] [PubMed] [Google Scholar]
- Ahmed-Belkacem A., Colliandre L., Ahnou N., Nevers Q., Gelin M., Bessin Y., Brillet R., Cala O., Douguet D., Bourguet W., Krimm I., Pawlotsky J.M., Guichou J.F. Fragment-based discovery of a new family of non-peptidic small-molecule cyclophilin inhibitors with potent antiviral activities. Nat. Commun. 2016;7:12777. doi: 10.1038/ncomms12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andreone P., Colombo M.G., Enejosa J.V., Koksal I., Ferenci P., Maieron A., Mullhaupt B., Horsmans Y., Weiland O., Reesink H.W., Rodrigues L., Jr., Hu Y.B., Podsadecki T., Bernstein B. ABT-450, ritonavir, ombitasvir, and dasabuvir achieves 97% and 100% sustained virologic response with or without ribavirin in treatment-experienced patients with HCV genotype 1b infection. Gastroenterology. 2014;147:359–365. doi: 10.1053/j.gastro.2014.04.045. e351. [DOI] [PubMed] [Google Scholar]
- Antonelli A., Ferri C., Galeazzi M., Giannitti C., Manno D., Mieli-Vergani G., Menegatti E., Olivieri I., Puoti M., Palazzi C., Roccatello D., Vergani D., Sarzi-Puttini P., Atzeni F. HCV infection: pathogenesis, clinical manifestations and therapy. Clin. Exp. Rheumatol. 2008;26:S39–S47. [PubMed] [Google Scholar]
- Arasappan A., Bennett F., Bogen S.L., Venkatraman S., Blackman M., Chen K.X., Hendrata S., Huang Y., Huelgas R.M., Nair L., Padilla A.I., Pan W., Pike R., Pinto P., Ruan S., Sannigrahi M., Velazquez F., Vibulbhan B., Wu W., Yang W., Saksena A.K., Girijavallabhan V., Shih N.Y., Kong J., Meng T., Jin Y., Wong J., McNamara P., Prongay A., Madison V., Piwinski J.J., Cheng K.C., Morrison R., Malcolm B., Tong X., Ralston R., Njoroge F.G. Discovery of narlaprevir (SCH 900518): a potent, second generation HCV NS3 serine protease inhibitor. ACS Med. Chem. Lett. 2010;1:64–69. doi: 10.1021/ml9000276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asante-Appiah E., Liu R., Curry S., McMonagle P., Agrawal S., Carr D., Rokosz L., Lahser F., Bystol K., Chase R., Black S., Ferrari E., Ingravallo P., Chen S., Tong L., Yu W., Kozlowski J. 2014. MK-8408, a Potent and Selective NS5A Inhibitor with a High Genetic Barrier to Resistance and Activity against HCV Genotypes 1-6, Abstr 40. 65th Annual Meeting of the American Association for the Study of Liver Diseases, Boston, MA, Nov 7–11. [Google Scholar]
- Backus L.I., Belperio P.S., Shahoumian T.A., Loomis T.P., Mole L.A. Real-world effectiveness of ledipasvir/sofosbuvir in 4,365 treatment-naive, genotype 1 hepatitis C-infected patients. Hepatology. 2016;64:405–414. doi: 10.1002/hep.28625. [DOI] [PubMed] [Google Scholar]
- Bacon B.R., Gordon S.C., Lawitz E., Marcellin P., Vierling J.M., Zeuzem S., Poordad F., Goodman Z.D., Sings H.L., Boparai N., Burroughs M., Brass C.A., Albrecht J.K., Esteban R., HCV RESPOND-2 Investigators Boceprevir for previously treated chronic HCV genotype 1 infection. N. Engl. J. Med. 2011;364:1207–1217. doi: 10.1056/NEJMoa1009482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartenschlager R., Penin F., Lohmann V., Andre P. Assembly of infectious hepatitis C virus particles. Trends Microbiol. 2011;19:95–103. doi: 10.1016/j.tim.2010.11.005. [DOI] [PubMed] [Google Scholar]
- Bartenschlager R., Lohmann V., Penin F. The molecular and structural basis of advanced antiviral therapy for hepatitis C virus infection. Nat. Rev. Microbiol. 2013;11:482–496. doi: 10.1038/nrmicro3046. [DOI] [PubMed] [Google Scholar]
- Belema M., Meanwell N.A. Discovery of daclatasvir, a pan-genotypic hepatitis C virus NS5A replication complex inhibitor with potent clinical effect. J. Med. Chem. 2014;57:5057–5071. doi: 10.1021/jm500335h. [DOI] [PubMed] [Google Scholar]
- Belema M., Nguyen V.N., Romine J.L., St Laurent D.R., Lopez O.D., Goodrich J.T., Nower P.T., O'Boyle D.R., 2nd, Lemm J.A., Fridell R.A., Gao M., Fang H., Krause R.G., Wang Y.K., Oliver A.J., Good A.C., Knipe J.O., Meanwell N.A., Snyder L.B. Hepatitis C virus NS5A replication complex inhibitors. Part 6: discovery of a novel and highly potent biarylimidazole chemotype with inhibitory activity toward genotypes 1a and 1b replicons. J. Med. Chem. 2014;57:1995–2012. doi: 10.1021/jm4016203. [DOI] [PubMed] [Google Scholar]
- Berger C., Romero-Brey I., Radujkovic D., Terreux R., Zayas M., Paul D., Harak C., Hoppe S., Gao M., Penin F., Lohmann V., Bartenschlager R. Daclatasvir-like inhibitors of NS5A block early biogenesis of hepatitis C virus-induced membranous replication factories, independent of RNA replication. Gastroenterology. 2014;147:1094–1105. doi: 10.1053/j.gastro.2014.07.019. e1025. [DOI] [PubMed] [Google Scholar]
- Berger K.L., Sarrazin C., Nelson D.R., Scherer J., Sha N., Marquis M., Cote-Martin A., Vinisko R., Stern J.O., Mensa F.J., Kukolj G. Resistance analyses of HCV NS3/4A protease and NS5B polymerase from clinical studies of deleobuvir and faldaprevir. PLoS One. 2016;11:e0160668. doi: 10.1371/journal.pone.0160668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilello J.P., Lallos L.B., McCarville J.F., La Colla M., Serra I., Chapron C., Gillum J.M., Pierra C., Standring D.N., Seifer M. In vitro activity and resistance profile of samatasvir, a novel NS5A replication inhibitor of hepatitis C virus. Antimicrob. Agents Chemother. 2014;58:4431–4442. doi: 10.1128/AAC.02777-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boson B., Denolly S., Turlure F., Chamot C., Dreux M., Cosset F.L. Daclatasvir prevents Hepatitis C virus infectivity by blocking transfer of the viral genome to assembly sites. Gastroenterology. 2017;7:895–907. doi: 10.1053/j.gastro.2016.11.047. e814. [DOI] [PubMed] [Google Scholar]
- Bourliere M., Bronowicki J.P., de Ledinghen V., Hezode C., Zoulim F., Mathurin P., Tran A., Larrey D.G., Ratziu V., Alric L., Hyland R.H., Jiang D., Doehle B., Pang P.S., Symonds W.T., Subramanian G.M., McHutchison J.G., Marcellin P., Habersetzer F., Guyader D., Grange J.D., Loustaud-Ratti V., Serfaty L., Metivier S., Leroy V., Abergel A., Pol S. Ledipasvir-sofosbuvir with or without ribavirin to treat patients with HCV genotype 1 infection and cirrhosis non-responsive to previous protease-inhibitor therapy: a randomised, double-blind, phase 2 trial (SIRIUS) Lancet Infect. Dis. 2015;15:397–404. doi: 10.1016/S1473-3099(15)70050-2. [DOI] [PubMed] [Google Scholar]
- Brown A., Hezode C., Zuckerman E., Foster G., Zekry A., Roberts S., Howe A., Durkan C., Badshah C., Zhang B., Robertson M., Wahl J., Barr E., Haber B. 50th Annual Meeting of the European Association for the Study of the Liver (EASL), Vienna, Austria. April 2015. C-SCAPE: efficacy and safety of 12 weeks of grazoprevir ± elbasvir ± ribavirin in patients with HCV GT2, 4, 5, or 6 infection. [Google Scholar]
- de Bruijne J., Bergmann J.F., Reesink H.W., Weegink C.J., Molenkamp R., Schinkel J., Tong X., Li J., Treitel M.A., Hughes E.A., van Lier J.J., van Vliet A.A., Janssen H.L., de Knegt R.J. Antiviral activity of narlaprevir combined with ritonavir and pegylated interferon in chronic hepatitis C patients. Hepatology. 2010;52:1590–1599. doi: 10.1002/hep.23899. [DOI] [PubMed] [Google Scholar]
- Buti M., Agarwal K., Horsmans Y., Sievert W., Janczewska E., Zeuzem S., Nyberg L., Brown R.S., Jr., Hezode C., Rizzetto M., Parana R., De Meyer S., De Masi R., Luo D., Bertelsen K., Witek J. Telaprevir twice daily is noninferior to telaprevir every 8 hours for patients with chronic hepatitis C. Gastroenterology. 2014;146:744–753. doi: 10.1053/j.gastro.2013.11.047. e743. [DOI] [PubMed] [Google Scholar]
- Cannalire R., Barreca M.L., Manfroni G., Cecchetti V. A Journey around the medicinal chemistry of hepatitis C virus inhibitors targeting NS4B: from target to preclinical drug candidates. J. Med. Chem. 2016;59:16–41. doi: 10.1021/acs.jmedchem.5b00825. [DOI] [PubMed] [Google Scholar]
- Carlsen T.H., Pedersen J., Prentoe J.C., Giang E., Keck Z.Y., Mikkelsen L.S., Law M., Foung S.K., Bukh J. Breadth of neutralization and synergy of clinically relevant human monoclonal antibodies against HCV genotypes 1a, 1b, 2a, 2b, 2c, and 3a. Hepatology. 2014;60:1551–1562. doi: 10.1002/hep.27298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catanese M.T., Uryu K., Kopp M., Edwards T.J., Andrus L., Rice W.J., Silvestry M., Kuhn R.J., Rice C.M. Ultrastructural analysis of hepatitis C virus particles. Proc. Natl. Acad. Sci. U. S. A. 2013;110:9505–9510. doi: 10.1073/pnas.1307527110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlton M., Gane E., Manns M.P., Brown R.S., Jr., Curry M.P., Kwo P.Y., Fontana R.J., Gilroy R., Teperman L., Muir A.J., McHutchison J.G., Symonds W.T., Brainard D., Kirby B., Dvory-Sobol H., Denning J., Arterburn S., Samuel D., Forns X., Terrault N.A. Sofosbuvir and ribavirin for treatment of compensated recurrent hepatitis C virus infection after liver transplantation. Gastroenterology. 2015;148:108–117. doi: 10.1053/j.gastro.2014.10.001. [DOI] [PubMed] [Google Scholar]
- Charlton M., Everson G.T., Flamm S.L., Kumar P., Landis C., Brown R.S., Jr., Fried M.W., Terrault N.A., O'Leary J.G., Vargas H.E., Kuo A., Schiff E., Sulkowski M.S., Gilroy R., Watt K.D., Brown K., Kwo P., Pungpapong S., Korenblat K.M., Muir A.J., Teperman L., Fontana R.J., Denning J., Arterburn S., Dvory-Sobol H., Brandt-Sarif T., Pang P.S., McHutchison J.G., Reddy K.R., Afdhal N., SOLAR-1 Investigators Ledipasvir and sofosbuvir plus ribavirin for treatment of HCV infection in patients with advanced liver disease. Gastroenterology. 2015;149:649–659. doi: 10.1053/j.gastro.2015.05.010. [DOI] [PubMed] [Google Scholar]
- Chatterji U., Garcia-Rivera J.A., Baugh J., Gawlik K., Wong K.A., Zhong W., Brass C.A., Naoumov N.V., Gallay P.A. The combination of alisporivir plus an NS5A inhibitor provides additive to synergistic anti-hepatitis C virus activity without detectable cross-resistance. Antimicrob. Agents Chemother. 2014;58:3327–3334. doi: 10.1128/AAC.00016-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chayama K., Notsumata K., Kurosaki M., Sato K., Rodrigues L., Jr., Setze C., Badri P., Pilot-Matias T., Vilchez R.A., Kumada H. Randomized trial of interferon- and ribavirin-free ombitasvir/paritaprevir/ritonavir in treatment-experienced hepatitis C virus-infected patients. Hepatology. 2015;61:1523–1532. doi: 10.1002/hep.27705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L.Z., Sabo J.P., Philip E., Rowland L., Mao Y., Latli B., Ramsden D., Mandarino D.A., Sane R.S. Mass balance, metabolite profile, and in vitro-in vivo comparison of clearance pathways of deleobuvir, a hepatitis C virus polymerase inhibitor. Antimicrob. Agents Chemother. 2015;59:25–37. doi: 10.1128/AAC.03861-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng G., Yu M., Peng B., Lee Y.-J., Trejo-Martin A., Gong R., Bush C., Worth A., Nash M., Chan K., Yang H., Beran R., Tian Y., Perry J., Taylor J., Yang C., Paulson M., Delaney W., Link J.O. GS-5816, a second generation hcv ns5a inhibitor with potent antiviral activity, broad genotypic coverage and a high resistance barrier. J. Hepatol. 2013;58:S484–S485. [Google Scholar]
- Cheng G., Tian Y., Doehle B., Peng B., Corsa A., Lee Y.J., Gong R., Yu M., Han B., Xu S., Dvory-Sobol H., Perron M., Xu Y., Mo H., Pagratis N., Link J.O., Delaney W. Vitro antiviral activity and resistance profile characterization of the hepatitis C virus NS5A inhibitor ledipasvir. Antimicrob. Agents Chemother. 2016;60:1847–1853. doi: 10.1128/AAC.02524-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung M.C., Walker A.J., Hudson B.E., Verma S., McLauchlan J., Mutimer D.J., Brown A., Gelson W.T., MacDonald D.C., Agarwal K., Foster G.R., Irving W.L., HCV Research UK Outcomes after successful direct-acting antiviral therapy for patients with chronic hepatitis C and decompensated cirrhosis. J. Hepatol. 2016;65:741–747. doi: 10.1016/j.jhep.2016.06.019. [DOI] [PubMed] [Google Scholar]
- Cho A., Zhang L., Xu J., Lee R., Butler T., Metobo S., Aktoudianakis V., Lew W., Ye H., Clarke M., Doerffler E., Byun D., Wang T., Babusis D., Carey A.C., German P., Sauer D., Zhong W., Rossi S., Fenaux M., McHutchison J.G., Perry J., Feng J., Ray A.S., Kim C.U. Discovery of the first C-nucleoside HCV polymerase inhibitor (GS-6620) with demonstrated antiviral response in HCV infected patients. J. Med. Chem. 2014;57:1812–1825. doi: 10.1021/jm400201a. [DOI] [PubMed] [Google Scholar]
- Choo Q.L., Kuo G., Weiner A.J., Overby L.R., Bradley D.W., Houghton M. Isolation of a cDNA clone derived from a blood-borne non-A, non-B viral hepatitis genome. Science. 1989;244:359–362. doi: 10.1126/science.2523562. [DOI] [PubMed] [Google Scholar]
- De Clercq E. The race for interferon-free HCV therapies: a snapshot by the spring of 2012. Rev. Med. Virol. 2012;22:392–411. doi: 10.1002/rmv.1727. [DOI] [PubMed] [Google Scholar]
- De Clercq E. Current race in the development of DAAs (direct-acting antivirals) against HCV. Biochem. Pharmacol. 2014;89:441–452. doi: 10.1016/j.bcp.2014.04.005. [DOI] [PubMed] [Google Scholar]
- De Clercq E. Development of antiviral drugs for the treatment of hepatitis C at an accelerating pace. Rev. Med. Virol. 2015;25:254–267. doi: 10.1002/rmv.1842. [DOI] [PubMed] [Google Scholar]
- De Clercq E. C-nucleosides to Be revisited. J. Med. Chem. 2016;59:2301–2311. doi: 10.1021/acs.jmedchem.5b01157. [DOI] [PubMed] [Google Scholar]
- De Clercq E., Li G. Approved antiviral drugs over the past 50 years. Clin. Microbiol. Rev. 2016;29:695–747. doi: 10.1128/CMR.00102-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coburn C.A., Meinke P.T., Chang W., Fandozzi C.M., Graham D.J., Hu B., Huang Q., Kargman S., Kozlowski J., Liu R., McCauley J.A., Nomeir A.A., Soll R.M., Vacca J.P., Wang D., Wu H., Zhong B., Olsen D.B., Ludmerer S.W. Discovery of MK-8742: an HCV NS5A inhibitor with broad genotype activity. ChemMedChem. 2013;8:1930–1940. doi: 10.1002/cmdc.201300343. [DOI] [PubMed] [Google Scholar]
- Coelmont L., Hanoulle X., Chatterji U., Berger C., Snoeck J., Bobardt M., Lim P., Vliegen I., Paeshuyse J., Vuagniaux G., Vandamme A.M., Bartenschlager R., Gallay P., Lippens G., Neyts J. DEB025 (Alisporivir) inhibits hepatitis C virus replication by preventing a cyclophilin A induced cis-trans isomerisation in domain II of NS5A. PLoS One. 2010;5:e13687. doi: 10.1371/journal.pone.0013687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coilly A., Fougerou-Leurent C., de Ledinghen V., Houssel-Debry P., Duvoux C., Di Martino V., Radenne S., Kamar N., D'Alteroche L., Leroy V., Canva V., Lebray P., Moreno C., Dumortier J., Silvain C., Besch C., Perre P., Botta-Fridlund D., Anty R., Francoz C., Abergel A., Debette-Gratien M., Conti F., Habersetzer F., Rohel A., Rossignol E., Danjou H., Roque-Afonso A.M., Samuel D., Duclos-Vallee J.C., Pageaux G.P., ANRS C023 CUPILT study group Multicentre experience using daclatasvir and sofosbuvir to treat hepatitis C recurrence - the ANRS CUPILT study. J. Hepatol. 2016;65:711–718. doi: 10.1016/j.jhep.2016.05.039. [DOI] [PubMed] [Google Scholar]
- Conti F., Buonfiglioli F., Scuteri A., Crespi C., Bolondi L., Caraceni P., Foschi F.G., Lenzi M., Mazzella G., Verucchi G., Andreone P., Brillanti S. Early occurrence and recurrence of hepatocellular carcinoma in HCV-related cirrhosis treated with direct-acting antivirals. J. Hepatol. 2016;65:727–733. doi: 10.1016/j.jhep.2016.06.015. [DOI] [PubMed] [Google Scholar]
- Court J.J., Poisson C., Ardzinski A., Bilimoria D., Chan L., Chandupatla K., Chauret N., Collier P.N., Das S.K., Denis F., Dorsch W., Iyer G., Lauffer D., L'Heureux L., Li P., Luisi B.S., Mani N., Nanthakumar S., Nicolas O., Rao B.G., Ronkin S., Selliah S., Shawgo R.S., Tang Q., Waal N.D., Yannopoulos C.G., Green J. Discovery of novel thiophene-based, thumb pocket 2 allosteric inhibitors of the hepatitis C NS5B polymerase with improved potency and physicochemical profiles. J. Med. Chem. 2016;59:6293–6302. doi: 10.1021/acs.jmedchem.6b00541. [DOI] [PubMed] [Google Scholar]
- Cox A.L. MEDICINE. Global control of hepatitis C virus. Science. 2015;349:790–791. doi: 10.1126/science.aad1302. [DOI] [PubMed] [Google Scholar]
- Cummings M.D., Lin T.I., Hu L., Tahri A., McGowan D., Amssoms K., Last S., Devogelaere B., Rouan M.C., Vijgen L., Berke J.M., Dehertogh P., Fransen E., Cleiren E., van der Helm L., Fanning G., Nyanguile O., Simmen K., Van Remoortere P., Raboisson P., Vendeville S. Discovery and early development of TMC647055, a non-nucleoside inhibitor of the hepatitis C virus NS5B polymerase. J. Med. Chem. 2014;57:1880–1892. doi: 10.1021/jm401396p. [DOI] [PubMed] [Google Scholar]
- Curry M.P., O'Leary J.G., Bzowej N., Muir A.J., Korenblat K.M., Fenkel J.M., Reddy K.R., Lawitz E., Flamm S.L., Schiano T., Teperman L., Fontana R., Schiff E., Fried M., Doehle B., An D., McNally J., Osinusi A., Brainard D.M., McHutchison J.G., Brown R.S., Jr., Charlton M., Investigators A- Sofosbuvir and velpatasvir for HCV in patients with decompensated cirrhosis. N. Engl. J. Med. 2015;373:2618–2628. doi: 10.1056/NEJMoa1512614. [DOI] [PubMed] [Google Scholar]
- Cuypers L., Li G., Libin P., Piampongsant S., Vandamme A.-M., Theys K. Genetic diversity and selective pressure in hepatitis C virus genotypes 1-6: significance for direct-acting antiviral treatment and drug resistance. Viruses. 2015;7:5018–5039. doi: 10.3390/v7092857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuypers L., Ceccherini-Silberstein F., Van Laethem K., Li G., Vandamme A.M., Rockstroh J.K. Impact of HCV genotype on treatment regimens and drug resistance: a snapshot in time. Rev. Med. Virol. 2016;26:408–434. doi: 10.1002/rmv.1895. [DOI] [PubMed] [Google Scholar]
- DeGoey D.A., Randolph J.T., Liu D., Pratt J., Hutchins C., Donner P., Krueger A.C., Matulenko M., Patel S., Motter C.E., Nelson L., Keddy R., Tufano M., Caspi D.D., Krishnan P., Mistry N., Koev G., Reisch T.J., Mondal R., Pilot-Matias T., Gao Y., Beno D.W., Maring C.J., Molla A., Dumas E., Campbell A., Williams L., Collins C., Wagner R., Kati W.M. Discovery of ABT-267, a pan-genotypic inhibitor of HCV NS5A. J. Med. Chem. 2014;57:2047–2057. doi: 10.1021/jm401398x. [DOI] [PubMed] [Google Scholar]
- Deterding K., Spinner C.D., Schott E., Welzel T.M., Gerken G., Klinker H., Spengler U., Wiegand J., Zur Wiesch J.S., Pathil A., Cornberg M., Umgelter A., Zollner C., Zeuzem S., Papkalla A., Weber K., Hardtke S., von der Leyen H., Koch A., von Witzendorff D., Manns M.P., Wedemeyer H., HepNet Acute HCVIVSG Ledipasvir plus sofosbuvir fixed-dose combination for 6 weeks in patients with acute hepatitis C virus genotype 1 monoinfection (HepNet Acute HCV IV): an open-label, single-arm, phase 2 study. Lancet Infect. Dis. 2017;17:215–222. doi: 10.1016/S1473-3099(16)30408-X. [DOI] [PubMed] [Google Scholar]
- Disease G.B.D., Injury I., Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1545–1602. doi: 10.1016/S0140-6736(16)31678-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dore G.J., Conway B., Luo Y., Janczewska E., Knysz B., Liu Y., Streinu-Cercel A., Caruntu F.A., Curescu M., Skoien R., Ghesquiere W., Mazur W., Soza A., Fuster F., Greenbloom S., Motoc A., Arama V., Shaw D., Tornai I., Sasadeusz J., Dalgard O., Sullivan D., Liu X., Kapoor M., Campbell A., Podsadecki T. Efficacy and safety of ombitasvir/paritaprevir/r and dasabuvir compared to IFN-containing regimens in genotype 1 HCV patients: the MALACHITE-I/II trials. J. Hepatol. 2016;64:19–28. doi: 10.1016/j.jhep.2015.08.015. [DOI] [PubMed] [Google Scholar]
- Dore G.J., Altice F., Litwin A.H., Dalgard O., Gane E.J., Shibolet O., Luetkemeyer A., Nahass R., Peng C.Y., Conway B., Grebely J., Howe A.Y., Gendrano I.N., Chen E., Huang H.C., Dutko F.J., Nickle D.C., Nguyen B.Y., Wahl J., Barr E., Robertson M.N., Platt H.L., C-EDGE CO-STAR Study Group Elbasvir-Grazoprevir to Treat Hepatitis C Virus Infection in Persons Receiving Opioid Agonist Therapy: A Randomized Trial. Ann. Intern Med. 2016;165:625–634. doi: 10.7326/M16-0816. [DOI] [PubMed] [Google Scholar]
- Doss W., Shiha G., Hassany M., Soliman R., Fouad R., Khairy M., Samir W., Hammad R., Kersey K., Jiang D., Doehle B., Knox S.J., Massetto B., McHutchison J.G., Esmat G. Sofosbuvir plus ribavirin for treating Egyptian patients with hepatitis C genotype 4. J. Hepatol. 2015;63:581–585. doi: 10.1016/j.jhep.2015.04.023. [DOI] [PubMed] [Google Scholar]
- Dubuisson J., Cosset F.L. Virology and cell biology of the hepatitis C virus life cycle: an update. J. Hepatol. 2014;61:S3–S13. doi: 10.1016/j.jhep.2014.06.031. [DOI] [PubMed] [Google Scholar]
- Egger D., Wolk B., Gosert R., Bianchi L., Blum H.E., Moradpour D., Bienz K. Expression of hepatitis C virus proteins induces distinct membrane alterations including a candidate viral replication complex. J. Virol. 2002;76:5974–5984. doi: 10.1128/JVI.76.12.5974-5984.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehteshami M., Tao S., Ozturk T., Zhou L., Cho J.H., Zhang H., Amiralaei S., Shelton J.R., Lu X., Khalil A., Domaoal R.A., Stanton R.A., Suesserman J.E., Lin B., Lee S.S., Amblard F., Whitaker T., Coats S.J., Schinazi R.F. Biochemical characterization of the active anti-hepatitis C virus metabolites of 2,6-diaminopurine ribonucleoside prodrug compared to sofosbuvir and BMS-986094. Antimicrob. Agents Chemother. 2016;60:4659–4669. doi: 10.1128/AAC.00318-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Khayat H.R., Fouad Y.M., Maher M., El-Amin H., Muhammed H. Efficacy and safety of sofosbuvir plus simeprevir therapy in Egyptian patients with chronic hepatitis C: a real-world experience. Gut. 2016 doi: 10.1136/gutjnl-2016–312012. [DOI] [PubMed] [Google Scholar]
- El-Serag H.B. Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology. 2012;142:1264–1273. doi: 10.1053/j.gastro.2011.12.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elsebai M.F., Koutsoudakis G., Saludes V., Perez-Vilaro G., Turpeinen A., Mattila S., Pirttila A.M., Fontaine-Vive F., Mehiri M., Meyerhans A., Diez J. Pan-genotypic hepatitis C virus inhibition by natural products derived from the wild Egyptian artichoke. J. Virol. 2015;90:1918–1930. doi: 10.1128/JVI.02030-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eltahla A.A., Tay E., Douglas M.W., White P.A. Cross-genotypic examination of hepatitis C virus polymerase inhibitors reveals a novel mechanism of action for thumb binders. Antimicrob. Agents Chemother. 2014;58:7215–7224. doi: 10.1128/AAC.03699-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esser-Nobis K., Schmidt J., Nitschke K., Neumann-Haefelin C., Thimme R., Lohmann V. The cyclophilin-inhibitor alisporivir stimulates antigen presentation thereby promoting antigen-specific CD8(+) T cell activation. J. Hepatol. 2016;64:1305–1314. doi: 10.1016/j.jhep.2016.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- European Association for Study of Liver EASL recommendations on treatment of hepatitis C 2015. J. Hepatol. 2015;63:199–236. doi: 10.1016/j.jhep.2015.03.025. [DOI] [PubMed] [Google Scholar]
- Everson G.T., Sims K.D., Rodriguez-Torres M., Hezode C., Lawitz E., Bourliere M., Loustaud-Ratti V., Rustgi V., Schwartz H., Tatum H., Marcellin P., Pol S., Thuluvath P.J., Eley T., Wang X., Huang S.P., McPhee F., Wind-Rotolo M., Chung E., Pasquinelli C., Grasela D.M., Gardiner D.F. Efficacy of an interferon- and ribavirin-free regimen of daclatasvir, asunaprevir, and BMS-791325 in treatment-naive patients with HCV genotype 1 infection. Gastroenterology. 2014;146:420–429. doi: 10.1053/j.gastro.2013.10.057. [DOI] [PubMed] [Google Scholar]
- Everson G.T., Towner W.J., Davis M.N., Wyles D.L., Nahass R.G., Thuluvath P.J., Etzkorn K., Hinestrosa F., Tong M., Rabinovitz M., McNally J., Brainard D.M., Han L., Doehle B., McHutchison J.G., Morgan T., Chung R.T., Tran T.T. Sofosbuvir with velpatasvir in treatment-naive noncirrhotic patients with genotype 1 to 6 hepatitis C virus infection: a randomized trial. Ann. Intern Med. 2015;163:818–826. doi: 10.7326/M15-1000. [DOI] [PubMed] [Google Scholar]
- Everson G.T., Sims K.D., Thuluvath P.J., Lawitz E., Hassanein T., Rodriguez-Torres M., Desta T., Hawkins T., Levin J.M., Hinestrosa F., Rustgi V., Schwartz H., Younossi Z., Webster L., Gitlin N., Eley T., Huang S.P., McPhee F., Grasela D.M., Gardiner D.F. Daclatasvir + asunaprevir + beclabuvir +/- ribavirin for chronic HCV genotype 1-infected treatment-naive patients. Liver Int. 2016;36:189–197. doi: 10.1111/liv.12964. [DOI] [PubMed] [Google Scholar]
- Feld J.J., Kowdley K.V., Coakley E., Sigal S., Nelson D.R., Crawford D., Weiland O., Aguilar H., Xiong J., Pilot-Matias T., DaSilva-Tillmann B., Larsen L., Podsadecki T., Bernstein B. Treatment of HCV with ABT-450/r-ombitasvir and dasabuvir with ribavirin. N. Engl. J. Med. 2014;370:1594–1603. doi: 10.1056/NEJMoa1315722. [DOI] [PubMed] [Google Scholar]
- Feld J.J., Jacobson I.M., Hezode C., Asselah T., Ruane P.J., Gruener N., Abergel A., Mangia A., Lai C.L., Chan H.L., Mazzotta F., Moreno C., Yoshida E., Shafran S.D., Towner W.J., Tran T.T., McNally J., Osinusi A., Svarovskaia E., Zhu Y., Brainard D.M., McHutchison J.G., Agarwal K., Zeuzem S., Investigators A- Sofosbuvir and velpatasvir for HCV genotype 1, 2, 4, 5, and 6 infection. N. Engl. J. Med. 2015;373:2599–2607. doi: 10.1056/NEJMoa1512610. [DOI] [PubMed] [Google Scholar]
- Feld J.J., Jacobson I.M., Jensen D.M., Foster G.R., Pol S., Tam E., Jablkowski M., Berak H., Vierling J.M., Yoshida E.M., Perez-Gomez H.R., Scalori A., Hooper G.J., Tavel J.A., Navarro M.T., Shahdad S., Kulkarni R., Le Pogam S., Najera I., Eng S., Lim C.Y., Shulman N.S., Yetzer E.S. Randomized study of danoprevir/ritonavir-based therapy for HCV genotype 1 patients with prior partial or null responses to peginterferon/ribavirin. J. Hepatol. 2015;62:294–302. doi: 10.1016/j.jhep.2014.09.013. [DOI] [PubMed] [Google Scholar]
- Feld J.J., Maan R., Zeuzem S., Kuo A., Nelson D.R., Di Bisceglie A.M., Manns M.P., Sherman K., Frazier L.M., Sterling R., Mailliard M., Schmidt M., Akushevich L., Vainorius M., Fried M.W. Effectiveness and safety of sofosbuvir-based regimens for chronic HCV genotype 3 infection: results of the HCV-TARGET study. Clin. Infect. Dis. 2016;63:776–783. doi: 10.1093/cid/ciw387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feld J.J., Moreno C., Trinh R., Tam E., Bourgeois S., Horsmans Y., Elkhashab M., Bernstein D.E., Younes Z., Reindollar R.W., Larsen L., Fu B., Howieson K., Polepally A.R., Pangerl A., Shulman N.S., Poordad F. Sustained virologic response of 100% in HCV genotype 1b patients with cirrhosis receiving ombitasvir/paritaprevir/r and dasabuvir for 12weeks. J. Hepatol. 2016;64:301–307. doi: 10.1016/j.jhep.2015.10.005. [DOI] [PubMed] [Google Scholar]
- Felmlee D.J., Coilly A., Chung R.T., Samuel D., Baumert T.F. New perspectives for preventing hepatitis C virus liver graft infection. Lancet Infect. Dis. 2016;16:735–745. doi: 10.1016/S1473-3099(16)00120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenaux M., Eng S., Leavitt S.A., Lee Y.J., Mabery E.M., Tian Y., Byun D., Canales E., Clarke M.O., Doerffler E., Lazerwith S.E., Lew W., Liu Q., Mertzman M., Morganelli P., Xu L., Ye H., Zhang J., Matles M., Murray B.P., Mwangi J., Zhang J., Hashash A., Krawczyk S.H., Bidgood A.M., Appleby T.C., Watkins W.J. Preclinical characterization of GS-9669, a thumb site II inhibitor of the hepatitis C virus NS5B polymerase. Antimicrob. Agents Chemother. 2013;57:804–810. doi: 10.1128/AAC.02052-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng J.Y., Cheng G., Perry J., Barauskas O., Xu Y., Fenaux M., Eng S., Tirunagari N., Peng B., Yu M., Tian Y., Lee Y.J., Stepan G., Lagpacan L.L., Jin D., Hung M., Ku K.S., Han B., Kitrinos K., Perron M., Birkus G., Wong K.A., Zhong W., Kim C.U., Carey A., Cho A., Ray A.S. Inhibition of hepatitis C virus replication by GS-6620, a potent C-nucleoside monophosphate prodrug. Antimicrob. Agents Chemother. 2014;58:1930–1942. doi: 10.1128/AAC.02351-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferenci P. Treatment of hepatitis C in difficult-to-treat patients. Nat. Rev. Gastroenterol. Hepatol. 2015;12:284–292. doi: 10.1038/nrgastro.2015.53. [DOI] [PubMed] [Google Scholar]
- Ferenci P., Bernstein D., Lalezari J., Cohen D., Luo Y., Cooper C., Tam E., Marinho R.T., Tsai N., Nyberg A., Box T.D., Younes Z., Enayati P., Green S., Baruch Y., Bhandari B.R., Caruntu F.A., Sepe T., Chulanov V., Janczewska E., Rizzardini G., Gervain J., Planas R., Moreno C., Hassanein T., Xie W., King M., Podsadecki T., Reddy K.R., PEARL-III Study, PEARL-IV Study ABT-450/r-ombitasvir and dasabuvir with or without ribavirin for HCV. N. Engl. J. Med. 2014;370:1983–1992. doi: 10.1056/NEJMoa1402338. [DOI] [PubMed] [Google Scholar]
- Ferenci P., Kozbial K., Mandorfer M., Hofer H. HCV targeting of patients with cirrhosis. J. Hepatol. 2015;63:1015–1022. doi: 10.1016/j.jhep.2015.06.003. [DOI] [PubMed] [Google Scholar]
- Flamm S.L., Lawitz E., Jacobson I., Bourliere M., Hezode C., Vierling J.M., Bacon B.R., Niederau C., Sherman M., Goteti V., Sings H.L., Barnard R.O., Howe J.A., Pedicone L.D., Burroughs M.H., Brass C.A., Albrecht J.K., Poordad F. Boceprevir with peginterferon alfa-2a-ribavirin is effective for previously treated chronic hepatitis C genotype 1 infection. Clin. Gastroenterol. Hepatol. 2013;11:81–87. doi: 10.1016/j.cgh.2012.10.006. [DOI] [PubMed] [Google Scholar]
- Forestier N., Larrey D., Marcellin P., Guyader D., Patat A., Rouzier R., Smith P.F., Qin X., Lim S., Bradford W., Porter S., Seiwert S.D., Zeuzem S. Antiviral activity of danoprevir (ITMN-191/RG7227) in combination with pegylated interferon alpha-2a and ribavirin in patients with hepatitis C. J. Infect. Dis. 2011;204:601–608. doi: 10.1093/infdis/jir315. [DOI] [PubMed] [Google Scholar]
- Forns X., Lawitz E., Zeuzem S., Gane E., Bronowicki J.P., Andreone P., Horban A., Brown A., Peeters M., Lenz O., Ouwerkerk-Mahadevan S., Scott J., De La Rosa G., Kalmeijer R., Sinha R., Beumont-Mauviel M. Simeprevir with peginterferon and ribavirin leads to high rates of SVR in patients with HCV genotype 1 who relapsed after previous therapy: a phase 3 trial. Gastroenterology. 2014;146:1669–1679. doi: 10.1053/j.gastro.2014.02.051. e1663. [DOI] [PubMed] [Google Scholar]
- Forns X., Charlton M., Denning J., McHutchison J.G., Symonds W.T., Brainard D., Brandt-Sarif T., Chang P., Kivett V., Castells L., Prieto M., Fontana R.J., Baumert T.F., Coilly A., Londono M.C., Habersetzer F. Sofosbuvir compassionate use program for patients with severe recurrent hepatitis C after liver transplantation. Hepatology. 2015;61:1485–1494. doi: 10.1002/hep.27681. [DOI] [PubMed] [Google Scholar]
- Forns X., Gordon S.C., Zuckerman E., Lawitz E., Calleja J.L., Hofer H., Gilbert C., Palcza J., Howe A.Y., DiNubile M.J., Robertson M.N., Wahl J., Barr E., Buti M. Grazoprevir and elbasvir plus ribavirin for chronic HCV genotype-1 infection after failure of combination therapy containing a direct-acting antiviral agent. J. Hepatol. 2015;63:564–572. doi: 10.1016/j.jhep.2015.04.009. [DOI] [PubMed] [Google Scholar]
- Foster T.L., Thompson G.S., Kalverda A.P., Kankanala J., Bentham M., Wetherill L.F., Thompson J., Barker A.M., Clarke D., Noerenberg M., Pearson A.R., Rowlands D.J., Homans S.W., Harris M., Foster R., Griffin S. Structure-guided design affirms inhibitors of hepatitis C virus p7 as a viable class of antivirals targeting virion release. Hepatology. 2014;59:408–422. doi: 10.1002/hep.26685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster G.R., Pianko S., Brown A., Forton D., Nahass R.G., George J., Barnes E., Brainard D.M., Massetto B., Lin M., Han B., McHutchison J.G., Subramanian G.M., Cooper C., Agarwal K., Boson Study Group Efficacy of sofosbuvir plus ribavirin with or without peginterferon-alfa in patients with hepatitis C virus genotype 3 infection and treatment-experienced patients with cirrhosis and hepatitis C virus genotype 2 infection. Gastroenterology. 2015;149:1462–1470. doi: 10.1053/j.gastro.2015.07.043. [DOI] [PubMed] [Google Scholar]
- Foster G.R., Afdhal N., Roberts S.K., Brau N., Gane E.J., Pianko S., Lawitz E., Thompson A., Shiffman M.L., Cooper C., Towner W.J., Conway B., Ruane P., Bourliere M., Asselah T., Berg T., Zeuzem S., Rosenberg W., Agarwal K., Stedman C.A., Mo H., Dvory-Sobol H., Han L., Wang J., McNally J., Osinusi A., Brainard D.M., McHutchison J.G., Mazzotta F., Tran T.T., Gordon S.C., Patel K., Reau N., Mangia A., Sulkowski M., ASTRAL-2 Investigators, ASTRAL-3 Investigators Sofosbuvir and Velpatasvir for HCV Genotype 2 and 3 Infection. N. Engl. J. Med. 2015;373:2608–2617. doi: 10.1056/NEJMoa1512612. [DOI] [PubMed] [Google Scholar]
- Fried M.W., Buti M., Dore G.J., Flisiak R., Ferenci P., Jacobson I., Marcellin P., Manns M., Nikitin I., Poordad F., Sherman M., Zeuzem S., Scott J., Gilles L., Lenz O., Peeters M., Sekar V., De Smedt G., Beumont-Mauviel M. Once-daily simeprevir (TMC435) with pegylated interferon and ribavirin in treatment-naive genotype 1 hepatitis C: the randomized PILLAR study. Hepatology. 2013;58:1918–1929. doi: 10.1002/hep.26641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu J., Tjandra M., Becker C., Bednarczyk D., Capparelli M., Elling R., Hanna I., Fujimoto R., Furegati M., Karur S., Kasprzyk T., Knapp M., Leung K., Li X., Lu P., Mergo W., Miault C., Ng S., Parker D., Peng Y., Roggo S., Rivkin A., Simmons R.L., Wang M., Wiedmann B., Weiss A.H., Xiao L., Xie L., Xu W., Yifru A., Yang S., Zhou B., Sweeney Z.K. Potent nonimmunosuppressive cyclophilin inhibitors with improved pharmaceutical properties and decreased transporter inhibition. J. Med. Chem. 2014;57:8503–8516. doi: 10.1021/jm500862r. [DOI] [PubMed] [Google Scholar]
- Gambato M., Lens S., Navasa M., Forns X. Treatment options in patients with decompensated cirrhosis, pre- and post-transplantation. J. Hepatol. 2014;61:S120–S131. doi: 10.1016/j.jhep.2014.07.020. [DOI] [PubMed] [Google Scholar]
- Gane E.J., Roberts S.K., Stedman C.A., Angus P.W., Ritchie B., Elston R., Ipe D., Morcos P.N., Baher L., Najera I., Chu T., Lopatin U., Berrey M.M., Bradford W., Laughlin M., Shulman N.S., Smith P.F. Oral combination therapy with a nucleoside polymerase inhibitor (RG7128) and danoprevir for chronic hepatitis C genotype 1 infection (INFORM-1): a randomised, double-blind, placebo-controlled, dose-escalation trial. Lancet. 2010;376:1467–1475. doi: 10.1016/S0140-6736(10)61384-0. [DOI] [PubMed] [Google Scholar]
- Gane E.J., Rouzier R., Stedman C., Wiercinska-Drapalo A., Horban A., Chang L., Zhang Y., Sampeur P., Najera I., Smith P., Shulman N.S., Tran J.Q. Antiviral activity, safety, and pharmacokinetics of danoprevir/ritonavir plus PEG-IFN alpha-2a/RBV in hepatitis C patients. J. Hepatol. 2011;55:972–979. doi: 10.1016/j.jhep.2011.01.046. [DOI] [PubMed] [Google Scholar]
- Gane E.J., Stedman C.A., Hyland R.H., Ding X., Svarovskaia E., Symonds W.T., Hindes R.G., Berrey M.M. Nucleotide polymerase inhibitor sofosbuvir plus ribavirin for hepatitis C. N. Engl. J. Med. 2013;368:34–44. doi: 10.1056/NEJMoa1208953. [DOI] [PubMed] [Google Scholar]
- Gane E.J., Stedman C.A., Hyland R.H., Ding X., Svarovskaia E.S., Pang P.S., Symonds W.T. 2013. Once Daily Sofosbuvir/Ledipasvir Fixed-dose Combination with or without Ribavirin: Data from the ELECTRON Trials, Abstr 64rd Annual Meeting of the American Association for the Study of Liver Diseases, Washington, DC Nov 1-5 2013. [Google Scholar]
- Gane E.J., Stedman C.A., Hyland R.H., Ding X., Svarovskaia E., Subramanian G.M., Symonds W.T., McHutchison J.G., Pang P.S. Efficacy of nucleotide polymerase inhibitor sofosbuvir plus the NS5A inhibitor ledipasvir or the NS5B non-nucleoside inhibitor GS-9669 against HCV genotype 1 infection. Gastroenterology. 2014;146:736–743. doi: 10.1053/j.gastro.2013.11.007. e731. [DOI] [PubMed] [Google Scholar]
- Gane E.J., Rouzier R., Wiercinska-Drapalo A., Larrey D.G., Morcos P.N., Brennan B.J., Le Pogam S., Najera I., Petric R., Tran J.Q., Kulkarni R., Zhang Y., Smith P., Yetzer E.S., Shulman N.S. Efficacy and safety of danoprevir-ritonavir plus peginterferon alfa-2a-ribavirin in hepatitis C virus genotype 1 prior null responders. Antimicrob. Agents Chemother. 2014;58:1136–1145. doi: 10.1128/AAC.01515-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gane E.J., Hyland R.H., An D., Svarovskaia E., Pang P.S., Brainard D., Stedman C.A. Efficacy of ledipasvir and sofosbuvir, with or without ribavirin, for 12 weeks in patients with HCV genotype 3 or 6 infection. Gastroenterology. 2015;149:1454–1461. doi: 10.1053/j.gastro.2015.07.063. e1451. [DOI] [PubMed] [Google Scholar]
- Gane E., Kowdley K.V., Pound D., Stedman C.A., Davis M., Etzkorn K., Gordon S.C., Bernstein D., Everson G., Rodriguez-Torres M., Tsai N., Khalid O., Yang J.C., Lu S., Dvory-Sobol H., Stamm L.M., Brainard D.M., McHutchison J.G., Tong M., Chung R.T., Beavers K., Poulos J.E., Kwo P.Y., Nguyen M.H. Efficacy of sofosbuvir, velpatasvir, and GS-9857 in patients with hepatitis C virus genotype 2, 3, 4, or 6 infections in an open-label, phase 2 trial. Gastroenterology. 2016;151:902–909. doi: 10.1053/j.gastro.2016.07.038. [DOI] [PubMed] [Google Scholar]
- Gane E.J., Schwabe C., Hyland R.H., Yang Y., Svarovskaia E., Stamm L.M., Brainard D.M., McHutchison J.G., Stedman C.A. Efficacy of the combination of sofosbuvir, velpatasvir, and the NS3/4A protease inhibitor GS-9857 in treatment-naive or previously treated patients with hepatitis C virus genotype 1 or 3 infections. Gastroenterology. 2016;151:448–456. doi: 10.1053/j.gastro.2016.05.021. [DOI] [PubMed] [Google Scholar]
- Gane E., Poordad F., Wang S., Asatryan A., Kwo P.Y., Lalezari J., Wyles D.L., Hassanein T., Aguilar H., Maliakkal B., Liu R., Lin C.W., Ng T.I., Kort J., Mensa F.J. High efficacy of ABT-493 and ABT-530 treatment in patients with HCV genotype 1 or 3 infection and compensated cirrhosis. Gastroenterology. 2016;151:651–659. doi: 10.1053/j.gastro.2016.07.020. e651. [DOI] [PubMed] [Google Scholar]
- Gane E.J., Pianko S., Roberts S.K., Thompson A.J., Zeuzem S., Zuckerman E., Ari Z.B., Foster G.R., Agarwal K., Laursen A.L., Gertoft J., Gao W., Huang H.-C., Fitzgerald B., Li J.J., Wan S., Dutko F., Nguyen B.-Y.T., Wahl J., Barr E., Butterton J.R., Esteban R. EASL - European Association for the Study of the Liver; Barcelona: 2016. High Efficacy of an 8-Week, 3-Drug Regimen of MK-3682/Grazoprevir/MK-8408 in HCV Genotype 1, 2, or 3-Infected Patients: SVR24 Data from the Phase 2 C-CREST 1 and 2 Studies, Abstr 38. April 14–17. [Google Scholar]
- Gao M., Nettles R.E., Belema M., Snyder L.B., Nguyen V.N., Fridell R.A., Serrano-Wu M.H., Langley D.R., Sun J.H., O'Boyle D.R., 2nd, Lemm J.A., Wang C., Knipe J.O., Chien C., Colonno R.J., Grasela D.M., Meanwell N.A., Hamann L.G. Chemical genetics strategy identifies an HCV NS5A inhibitor with a potent clinical effect. Nature. 2010;465:96–100. doi: 10.1038/nature08960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ge P.S., Runyon B.A. Treatment of patients with cirrhosis. N. Engl. J. Med. 2016;375:767–777. doi: 10.1056/NEJMra1504367. [DOI] [PubMed] [Google Scholar]
- Gentile I., Buonomo A.R., Zappulo E., Borgia G. Discontinued drugs in 2012-2013: hepatitis C virus infection. Expert Opin. Investig. Drugs. 2015;24:239–251. doi: 10.1517/13543784.2015.982274. [DOI] [PubMed] [Google Scholar]
- Gentles R.G., Ding M., Bender J.A., Bergstrom C.P., Grant-Young K., Hewawasam P., Hudyma T., Martin S., Nickel A., Regueiro-Ren A., Tu Y., Yang Z., Yeung K.S., Zheng X., Chao S., Sun J.H., Beno B.R., Camac D.M., Chang C.H., Gao M., Morin P.E., Sheriff S., Tredup J., Wan J., Witmer M.R., Xie D., Hanumegowda U., Knipe J., Mosure K., Santone K.S., Parker D.D., Zhuo X., Lemm J., Liu M., Pelosi L., Rigat K., Voss S., Wang Y., Wang Y.K., Colonno R.J., Gao M., Roberts S.B., Gao Q., Ng A., Meanwell N.A., Kadow J.F. Discovery and preclinical characterization of the cyclopropylindolobenzazepine BMS-791325, a potent allosteric inhibitor of the hepatitis C virus NS5B polymerase. J. Med. Chem. 2014;57:1855–1879. doi: 10.1021/jm4016894. [DOI] [PubMed] [Google Scholar]
- Gosert R., Egger D., Lohmann V., Bartenschlager R., Blum H.E., Bienz K., Moradpour D. Identification of the hepatitis C virus RNA replication complex in Huh-7 cells harboring subgenomic replicons. J. Virol. 2003;77:5487–5492. doi: 10.1128/JVI.77.9.5487-5492.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotte M., Feld J.J. Direct-acting antiviral agents for hepatitis C: structural and mechanistic insights. Nat. Rev. Gastroenterol. Hepatol. 2016;13:338–351. doi: 10.1038/nrgastro.2016.60. [DOI] [PubMed] [Google Scholar]
- Hamed M.R., Brown R.J., Zothner C., Urbanowicz R.A., Mason C.P., Krarup A., McClure C.P., Irving W.L., Ball J.K., Harris M., Hickling T.P., Tarr A.W. Recombinant human L-ficolin directly neutralizes hepatitis C virus entry. J. Innate Immun. 2014;6:676–684. doi: 10.1159/000362209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper S., McCauley J.A., Rudd M.T., Ferrara M., DiFilippo M., Crescenzi B., Koch U., Petrocchi A., Holloway M.K., Butcher J.W., Romano J.J., Bush K.J., Gilbert K.F., McIntyre C.J., Nguyen K.T., Nizi E., Carroll S.S., Ludmerer S.W., Burlein C., DiMuzio J.M., Graham D.J., McHale C.M., Stahlhut M.W., Olsen D.B., Monteagudo E., Cianetti S., Giuliano C., Pucci V., Trainor N., Fandozzi C.M., Rowley M., Coleman P.J., Vacca J.P., Summa V., Liverton N.J. Discovery of MK-5172, a macrocyclic hepatitis C virus NS3/4a protease inhibitor. ACS Med. Chem. Lett. 2012;3:332–336. doi: 10.1021/ml300017p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassanein T., Sims K.D., Bennett M., Gitlin N., Lawitz E., Nguyen T., Webster L., Younossi Z., Schwartz H., Thuluvath P.J., Zhou H., Rege B., McPhee F., Zhou N., Wind-Rotolo M., Chung E., Griffies A., Grasela D.M., Gardiner D.F. A randomized trial of daclatasvir in combination with asunaprevir and beclabuvir in patients with chronic hepatitis C virus genotype 4 infection. J. Hepatol. 2015;62:1204–1206. doi: 10.1016/j.jhep.2014.12.025. [DOI] [PubMed] [Google Scholar]
- Hayashi N., Izumi N., Kumada H., Okanoue T., Tsubouchi H., Yatsuhashi H., Kato M., Ki R., Komada Y., Seto C., Goto S. Simeprevir with peginterferon/ribavirin for treatment-naive hepatitis C genotype 1 patients in Japan: CONCERTO-1, a phase III trial. J. Hepatol. 2014;61:219–227. doi: 10.1016/j.jhep.2014.04.004. [DOI] [PubMed] [Google Scholar]
- He S., Lin B., Chu V., Hu Z., Hu X., Xiao J., Wang A.Q., Schweitzer C.J., Li Q., Imamura M., Hiraga N., Southall N., Ferrer M., Zheng W., Chayama K., Marugan J.J., Liang T.J. Repurposing of the antihistamine chlorcyclizine and related compounds for treatment of hepatitis C virus infection. Sci. Transl. Med. 2015;7 doi: 10.1126/scitranslmed.3010286. 282ra249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He S., Xiao J., Dulcey A.E., Lin B., Rolt A., Hu Z., Hu X., Wang A.Q., Xu X., Southall N., Ferrer M., Zheng W., Liang T.J., Marugan J.J. Discovery, optimization, and characterization of novel chlorcyclizine derivatives for the treatment of hepatitis C virus infection. J. Med. Chem. 2016;59:841–853. doi: 10.1021/acs.jmedchem.5b00752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hezode C., Fontaine H., Dorival C., Zoulim F., Larrey D., Canva V., De Ledinghen V., Poynard T., Samuel D., Bourliere M., Alric L., Raabe J.J., Zarski J.P., Marcellin P., Riachi G., Bernard P.H., Loustaud-Ratti V., Chazouilleres O., Abergel A., Guyader D., Metivier S., Tran A., Di Martino V., Causse X., Dao T., Lucidarme D., Portal I., Cacoub P., Gournay J., Grando-Lemaire V., Hillon P., Attali P., Fontanges T., Rosa I., Petrov-Sanchez V., Barthe Y., Pawlotsky J.M., Pol S., Carrat F., Bronowicki J.P., Cupic Study Group Effectiveness of telaprevir or boceprevir in treatment-experienced patients with HCV genotype 1 infection and cirrhosis. Gastroenterology. 2014;147:132–142. doi: 10.1053/j.gastro.2014.03.051. e134. [DOI] [PubMed] [Google Scholar]
- Hezode C., Asselah T., Reddy K.R., Hassanein T., Berenguer M., Fleischer-Stepniewska K., Marcellin P., Hall C., Schnell G., Pilot-Matias T., Mobashery N., Redman R., Vilchez R.A., Pol S. Ombitasvir plus paritaprevir plus ritonavir with or without ribavirin in treatment-naive and treatment-experienced patients with genotype 4 chronic hepatitis C virus infection (PEARL-I): a randomised, open-label trial. Lancet. 2015;385:2502–2509. doi: 10.1016/S0140-6736(15)60159-3. [DOI] [PubMed] [Google Scholar]
- Hezode C., Chevaliez S., Scoazec G., Soulier A., Varaut A., Bouvier-Alias M., Ruiz I., Roudot-Thoraval F., Mallat A., Feray C., Pawlotsky J.M. Retreatment with sofosbuvir and simeprevir of patients with hepatitis C virus genotype 1 or 4 who previously failed a daclatasvir-containing regimen. Hepatology. 2016;63:1809–1816. doi: 10.1002/hep.28491. [DOI] [PubMed] [Google Scholar]
- Ho S.B., Monto A., Peyton A., Kaplan D.E., Byrne S., Moon S., Copans A., Rossaro L., Roy A., Le H., Dvory-Sobol H., Zhu Y., Brainard D.M., Guyer W., Shaikh O., Fuchs M., Morgan T.R., Valor study team Efficacy of sofosbuvir plus ribavirin in veterans with hepatitis C virus genotype 2 infection, compensated cirrhosis, and multiple comorbidities. Clin. Gastroenterol. Hepatol. 2017;15:282–288. doi: 10.1016/j.cgh.2016.05.024. [DOI] [PubMed] [Google Scholar]
- Ioannou G.N., Beste L.A., Chang M.F., Green P.K., Lowy E., Tsui J.I., Su F., Berry K. Effectiveness of sofosbuvir, ledipasvir/sofosbuvir, or paritaprevir/ritonavir/ombitasvir and dasabuvir regimens for treatment of patients with hepatitis C in the veterans affairs national health care system. Gastroenterology. 2016;151:457–471. doi: 10.1053/j.gastro.2016.05.049. e455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isakov V., Koloda D., Tikhonova N., Kikalishvili T., Krasavina E., Lekishvili K., Malaya I., Ryska M., Samsonov M., Tolkacheva V. Pharmacokinetics of new HCV NS3 protease inhibitor narlaprevir following single dose use with or without ritonavir in patients with liver cirrhosis. Antimicrob. Agents Chemother. 2016;60:7098–7104. doi: 10.1128/AAC.01044-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivachtchenko A.V., Mitkin O.D., Yamanushkin P.M., Kuznetsova I.V., Bulanova E.A., Shevkun N.A., Koryakova A.G., Karapetian R.N., Bichko V.V., Trifelenkov A.S., Kravchenko D.V., Vostokova N.V., Veselov M.S., Chufarova N.V., Ivanenkov Y.A. Discovery of novel highly potent hepatitis C virus NS5A inhibitor (AV4025) J. Med. Chem. 2014;57:7716–7730. doi: 10.1021/jm500951r. [DOI] [PubMed] [Google Scholar]
- Izumi N., Hayashi N., Kumada H., Okanoue T., Tsubouchi H., Yatsuhashi H., Kato M., Ki R., Komada Y., Seto C., Goto S. Once-daily simeprevir with peginterferon and ribavirin for treatment-experienced HCV genotype 1-infected patients in Japan: the CONCERTO-2 and CONCERTO-3 studies. J. Gastroenterol. 2014;49:941–953. doi: 10.1007/s00535-014-0949-8. [DOI] [PubMed] [Google Scholar]
- Jacobson I.M., Gordon S.C., Kowdley K.V., Yoshida E.M., Rodriguez-Torres M., Sulkowski M.S., Shiffman M.L., Lawitz E., Everson G., Bennett M., Schiff E., Al-Assi M.T., Subramanian G.M., An D., Lin M., McNally J., Brainard D., Symonds W.T., McHutchison J.G., Patel K., Feld J., Pianko S., Nelson D.R., Study P., Study F. Sofosbuvir for hepatitis C genotype 2 or 3 in patients without treatment options. N. Engl. J. Med. 2013;368:1867–1877. doi: 10.1056/NEJMoa1214854. [DOI] [PubMed] [Google Scholar]
- Jacobson I.M., Dore G.J., Foster G.R., Fried M.W., Radu M., Rafalsky V.V., Moroz L., Craxi A., Peeters M., Lenz O., Ouwerkerk-Mahadevan S., De La Rosa G., Kalmeijer R., Scott J., Sinha R., Beumont-Mauviel M. Simeprevir with pegylated interferon alfa 2a plus ribavirin in treatment-naive patients with chronic hepatitis C virus genotype 1 infection (QUEST-1): a phase 3, randomised, double-blind, placebo-controlled trial. Lancet. 2014;384:403–413. doi: 10.1016/S0140-6736(14)60494-3. [DOI] [PubMed] [Google Scholar]
- Jiang Y., Andrews S.W., Condroski K.R., Buckman B., Serebryany V., Wenglowsky S., Kennedy A.L., Madduru M.R., Wang B., Lyon M., Doherty G.A., Woodard B.T., Lemieux C., Geck Do M., Zhang H., Ballard J., Vigers G., Brandhuber B.J., Stengel P., Josey J.A., Beigelman L., Blatt L., Seiwert S.D. Discovery of danoprevir (ITMN-191/R7227), a highly selective and potent inhibitor of hepatitis C virus (HCV) NS3/4A protease. J. Med. Chem. 2014;57:1753–1769. doi: 10.1021/jm400164c. [DOI] [PubMed] [Google Scholar]
- Jiang M., Zhang E.Z., Ardzinski A., Tigges A., Davis A., Sullivan J.C., Nelson M., Spanks J., Dorrian J., Nicolas O., Bartels D.J., Rao B.G., Rijnbrand R., Kieffer T.L. Genotypic and phenotypic analyses of hepatitis C virus variants observed in clinical studies of VX-222, a nonnucleoside NS5B polymerase inhibitor. Antimicrob. Agents Chemother. 2014;58:5456–5465. doi: 10.1128/AAC.03052-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonckers T.H., Tahri A., Vijgen L., Berke J.M., Lachau-Durand S., Stoops B., Snoeys J., Leclercq L., Tambuyzer L., Lin T.I., Simmen K., Raboisson P. Discovery of 1-((2R,4aR,6R,7R,7aR)-2-Isopropoxy-2-oxidodihydro-4H,6H-spiro[furo[3,2-d][1,3,2]d ioxaphosphinine-7,2'-oxetan]-6-yl)pyrimidine-2,4(1H,3H)-dione (JNJ-54257099), a 3'-5'-cyclic phosphate ester prodrug of 2'-deoxy-2'-spirooxetane uridine triphosphate useful for HCV inhibition. J. Med. Chem. 2016;59:5790–5798. doi: 10.1021/acs.jmedchem.6b00382. [DOI] [PubMed] [Google Scholar]
- Kakarla R., Liu J., Naduthambi D., Chang W., Mosley R.T., Bao D., Steuer H.M., Keilman M., Bansal S., Lam A.M., Seibel W., Neilson S., Furman P.A., Sofia M.J. Discovery of a novel class of potent HCV NS4B inhibitors: SAR studies on piperazinone derivatives. J. Med. Chem. 2014;57:2136–2160. doi: 10.1021/jm4012643. [DOI] [PubMed] [Google Scholar]
- Kati W., Koev G., Irvin M., Beyer J., Liu Y., Krishnan P., Reisch T., Mondal R., Wagner R., Molla A., Maring C., Collins C. In vitro activity and resistance profile of dasabuvir, a nonnucleoside hepatitis C virus polymerase inhibitor. Antimicrob. Agents Chemother. 2015;59:1505–1511. doi: 10.1128/AAC.04619-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazmierski W.M., Maynard A., Duan M., Baskaran S., Botyanszki J., Crosby R., Dickerson S., Tallant M., Grimes R., Hamatake R., Leivers M., Roberts C.D., Walker J. Novel spiroketal pyrrolidine GSK2336805 potently inhibits key hepatitis C virus genotype 1b mutants: from lead to clinical compound. J. Med. Chem. 2014;57:2058–2073. doi: 10.1021/jm4013104. [DOI] [PubMed] [Google Scholar]
- Kim J.L., Morgenstern K.A., Lin C., Fox T., Dwyer M.D., Landro J.A., Chambers S.P., Markland W., Lepre C.A., O'Malley E.T., Harbeson S.L., Rice C.M., Murcko M.A., Caron P.R., Thomson J.A. Crystal structure of the hepatitis C virus NS3 protease domain complexed with a synthetic NS4A cofactor peptide. Cell. 1996;87:343–355. doi: 10.1016/s0092-8674(00)81351-3. [DOI] [PubMed] [Google Scholar]
- Kohli A., Osinusi A., Sims Z., Nelson A., Meissner E.G., Barrett L.L., Bon D., Marti M.M., Silk R., Kotb C., Gross C., Jolley T.A., Sidharthan S., Petersen T., Townsend K., Egerson D., Kapoor R., Spurlin E., Sneller M., Proschan M., Herrmann E., Kwan R., Teferi G., Talwani R., Diaz G., Kleiner D.E., Wood B.J., Chavez J., Abbott S., Symonds W.T., Subramanian G.M., Pang P.S., McHutchison J., Polis M.A., Fauci A.S., Masur H., Kottilil S. Virological response after 6 week triple-drug regimens for hepatitis C: a proof-of-concept phase 2A cohort study. Lancet. 2015;385:1107–1113. doi: 10.1016/S0140-6736(14)61228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohli A., Kapoor R., Sims Z., Nelson A., Sidharthan S., Lam B., Silk R., Kotb C., Gross C., Teferi G., Sugarman K., Pang P.S., Osinusi A., Polis M.A., Rustgi V., Masur H., Kottilil S. Ledipasvir and sofosbuvir for hepatitis C genotype 4: a proof-of-concept, single-centre, open-label phase 2a cohort study. Lancet Infect. Dis. 2015;15:1049–1054. doi: 10.1016/S1473-3099(15)00157-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohli A., Kattakuzhy S., Sidharthan S., Nelson A., McLaughlin M., Seamon C., Wilson E., Meissner E.G., Sims Z., Silk R., Gross C., Akoth E., Tang L., Price A., Jolley T.A., Emmanuel B., Proschan M., Teferi G., Chavez J., Abbott S., Osinusi A., Mo H., Polis M.A., Masur H., Kottilil S. Four-week direct-acting antiviral regimens in noncirrhotic patients with hepatitis C virus genotype 1 infection: an open-label, nonrandomized trial. Ann. Intern Med. 2015;163:899–907. doi: 10.7326/M15-0642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komatsu T.E., Boyd S., Sherwat A., Tracy L., Naeger L.K., O'Rear J.J., Harrington P.R. Regulatory analysis of effects of hepatitis C virus NS5A polymorphisms on efficacy of elbasvir and grazoprevir. Gastroenterology. 2017;152:586–597. doi: 10.1053/j.gastro.2016.10.017. [DOI] [PubMed] [Google Scholar]
- Koutsoudakis G., Romero-Brey I., Berger C., Perez-Vilaro G., Monteiro Perin P., Vondran F.W., Kalesse M., Harmrolfs K., Muller R., Martinez J.P., Pietschmann T., Bartenschlager R., Bronstrup M., Meyerhans A., Diez J. Soraphen A: a broad-spectrum antiviral natural product with potent anti-hepatitis C virus activity. J. Hepatol. 2015;63:813–821. doi: 10.1016/j.jhep.2015.06.002. [DOI] [PubMed] [Google Scholar]
- Kovackova S., Chang L., Bekerman E., Neveu G., Barouch-Bentov R., Chaikuad A., Heroven C., Sala M., De Jonghe S., Knapp S., Einav S., Herdewijn P. Selective inhibitors of cyclin G associated kinase (GAK) as anti-hepatitis C agents. J. Med. Chem. 2015;58:3393–3410. doi: 10.1021/jm501759m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowdley K.V., Lawitz E., Crespo I., Hassanein T., Davis M.N., DeMicco M., Bernstein D.E., Afdhal N., Vierling J.M., Gordon S.C., Anderson J.K., Hyland R.H., Dvory-Sobol H., An D., Hindes R.G., Albanis E., Symonds W.T., Berrey M.M., Nelson D.R., Jacobson I.M. Sofosbuvir with pegylated interferon alfa-2a and ribavirin for treatment-naive patients with hepatitis C genotype-1 infection (ATOMIC): an open-label, randomised, multicentre phase 2 trial. Lancet. 2013;381:2100–2107. doi: 10.1016/S0140-6736(13)60247-0. [DOI] [PubMed] [Google Scholar]
- Kowdley K.V., Gordon S.C., Reddy K.R., Rossaro L., Bernstein D.E., Lawitz E., Shiffman M.L., Schiff E., Ghalib R., Ryan M., Rustgi V., Chojkier M., Herring R., Di Bisceglie A.M., Pockros P.J., Subramanian G.M., An D., Svarovskaia E., Hyland R.H., Pang P.S., Symonds W.T., McHutchison J.G., Muir A.J., Pound D., Fried M.W., ION-3 Investigators Ledipasvir and sofosbuvir for 8 or 12 weeks for chronic HCV without cirrhosis. N. Engl. J. Med. 2014;370:1879–1888. doi: 10.1056/NEJMoa1402355. [DOI] [PubMed] [Google Scholar]
- Kowdley K.V., Lawitz E., Poordad F., Cohen D.E., Nelson D.R., Zeuzem S., Everson G.T., Kwo P., Foster G.R., Sulkowski M.S., Xie W., Pilot-Matias T., Liossis G., Larsen L., Khatri A., Podsadecki T., Bernstein B. Phase 2b trial of interferon-free therapy for hepatitis C virus genotype 1. N. Engl. J. Med. 2014;370:222–232. doi: 10.1056/NEJMoa1306227. [DOI] [PubMed] [Google Scholar]
- Kumada H., Hayashi N., Izumi N., Okanoue T., Tsubouchi H., Yatsuhashi H., Kato M., Rito K., Komada Y., Seto C., Goto S. Simeprevir (TMC435) once daily with peginterferon-alpha-2b and ribavirin in patients with genotype 1 hepatitis C virus infection: the CONCERTO-4 study. Hepatol. Res. 2015;45:501–513. doi: 10.1111/hepr.12375. [DOI] [PubMed] [Google Scholar]
- Kumada H., Chayama K., Rodrigues L., Jr., Suzuki F., Ikeda K., Toyoda H., Sato K., Karino Y., Matsuzaki Y., Kioka K., Setze C., Pilot-Matias T., Patwardhan M., Vilchez R.A., Burroughs M., Redman R. Randomized phase 3 trial of ombitasvir/paritaprevir/ritonavir for hepatitis C virus genotype 1b-infected Japanese patients with or without cirrhosis. Hepatology. 2015;62:1037–1046. doi: 10.1002/hep.27972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumada H., Suzuki F., Suzuki Y., Toyota J., Karino Y., Chayama K., Kawakami Y., Fujiyama S., Ito T., Itoh Y., Tamura E., Ueki T., Ishikawa H., Hu W., McPhee F., Linaberry M., Hughes E. Randomized comparison of daclatasvir + asunaprevir versus telaprevir + peginterferon/ribavirin in Japanese hepatitis C virus patients. J. Gastroenterol. Hepatol. 2016;31:14–22. doi: 10.1111/jgh.13073. [DOI] [PubMed] [Google Scholar]
- Kuo G., Choo Q.L., Alter H.J., Gitnick G.L., Redeker A.G., Purcell R.H., Miyamura T., Dienstag J.L., Alter M.J., Stevens C.E. An assay for circulating antibodies to a major etiologic virus of human non-A, non-B hepatitis. Science. 1989;244:362–364. doi: 10.1126/science.2496467. [DOI] [PubMed] [Google Scholar]
- Kwo P.Y., Lawitz E.J., McCone J., Schiff E.R., Vierling J.M., Pound D., Davis M.N., Galati J.S., Gordon S.C., Ravendhran N., Rossaro L., Anderson F.H., Jacobson I.M., Rubin R., Koury K., Pedicone L.D., Brass C.A., Chaudhri E., Albrecht J.K. Efficacy of boceprevir, an NS3 protease inhibitor, in combination with peginterferon alfa-2b and ribavirin in treatment-naive patients with genotype 1 hepatitis C infection (SPRINT-1): an open-label, randomised, multicentre phase 2 trial. Lancet. 2010;376:705–716. doi: 10.1016/S0140-6736(10)60934-8. [DOI] [PubMed] [Google Scholar]
- Kwo P., Gitlin N., Nahass R., Bernstein D., Etzkorn K., Rojter S., Schiff E., Davis M., Ruane P., Younes Z., Kalmeijer R., Sinha R., Peeters M., Lenz O., Fevery B., De La Rosa G., Scott J., Witek J. Simeprevir plus sofosbuvir (12 and 8 weeks) in hepatitis C virus genotype 1-infected patients without cirrhosis: OPTIMIST-1, a phase 3, randomized study. Hepatology. 2016;64:370–380. doi: 10.1002/hep.28467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwo P., Gane E., Peng C.Y., Pearlman B., Vierling J.M., Serfaty L., Buti M., Shafran S., Stryszak P., Lin L., Gress J., Black S., Dutko F.J., Robertson M., Wahl J., Lupinacci L., Barr E., Haber B. Effectiveness of elbasvir and grazoprevir combination, with or without ribavirin, for treatment-experienced patients with chronic hepatitis C infection. Gastroenterology. 2017;152:164–175. doi: 10.1053/j.gastro.2016.09.045. [DOI] [PubMed] [Google Scholar]
- Kwong A.D., Kauffman R.S., Hurter P., Mueller P. Discovery and development of telaprevir: an NS3-4A protease inhibitor for treating genotype 1 chronic hepatitis C virus. Nat. Biotechnol. 2011;29:993–1003. doi: 10.1038/nbt.2020. [DOI] [PubMed] [Google Scholar]
- Lahser F.C., Bystol K., Curry S., McMonagle P., Xia E., Ingravallo P., Chase R., Liu R., Black T., Hazuda D., Howe A.Y., Asante-Appiah E. The combination of grazoprevir, a hepatitis C virus (HCV) NS3/4A protease inhibitor, and elbasvir, an HCV NS5A inhibitor, demonstrates a high genetic barrier to resistance in HCV genotype 1a replicons. Antimicrob. Agents Chemother. 2016;60:2954–2964. doi: 10.1128/AAC.00051-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lalezari J., Sullivan J.G., Varunok P., Galen E., Kowdley K.V., Rustgi V., Aguilar H., Felizarta F., McGovern B., King M., Polepally A.R., Cohen D.E. Ombitasvir/paritaprevir/r and dasabuvir plus ribavirin in HCV genotype 1-infected patients on methadone or buprenorphine. J. Hepatol. 2015;63:364–369. doi: 10.1016/j.jhep.2015.03.029. [DOI] [PubMed] [Google Scholar]
- Lam A.M., Espiritu C., Bansal S., Micolochick Steuer H.M., Niu C., Zennou V., Keilman M., Zhu Y., Lan S., Otto M.J., Furman P.A. Genotype and subtype profiling of PSI-7977 as a nucleotide inhibitor of hepatitis C virus. Antimicrob. Agents Chemother. 2012;56:3359–3368. doi: 10.1128/AAC.00054-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaPlante S.R., Bos M., Brochu C., Chabot C., Coulombe R., Gillard J.R., Jakalian A., Poirier M., Rancourt J., Stammers T., Thavonekham B., Beaulieu P.L., Kukolj G., Tsantrizos Y.S. Conformation-based restrictions and scaffold replacements in the design of hepatitis C virus polymerase inhibitors: discovery of deleobuvir (BI 207127) J. Med. Chem. 2014;57:1845–1854. doi: 10.1021/jm4011862. [DOI] [PubMed] [Google Scholar]
- Lau G., Benhamou Y., Chen G., Li J., Shao Q., Ji D., Li F., Li B., Liu J., Hou J., Sun J., Wang C., Chen J., Wu V., Wong A., Wong C.L., Tsang S.T., Wang Y., Bassit L., Tao S., Jiang Y., Hsiao H.M., Ke R., Perelson A.S., Schinazi R.F. Efficacy and safety of 3-week response-guided triple direct-acting antiviral therapy for chronic hepatitis C infection: a phase 2, open-label, proof-of-concept study. Lancet. Gastroenterol. Hepatol. 2016;1:97–104. doi: 10.1016/S2468-1253(16)30015-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawitz E., Mangia A., Wyles D., Rodriguez-Torres M., Hassanein T., Gordon S.C., Schultz M., Davis M.N., Kayali Z., Reddy K.R., Jacobson I.M., Kowdley K.V., Nyberg L., Subramanian G.M., Hyland R.H., Arterburn S., Jiang D., McNally J., Brainard D., Symonds W.T., McHutchison J.G., Sheikh A.M., Younossi Z., Gane E.J. Sofosbuvir for previously untreated chronic hepatitis C infection. N. Engl. J. Med. 2013;368:1878–1887. doi: 10.1056/NEJMoa1214853. [DOI] [PubMed] [Google Scholar]
- Lawitz E., Lalezari J.P., Hassanein T., Kowdley K.V., Poordad F.F., Sheikh A.M., Afdhal N.H., Bernstein D.E., Dejesus E., Freilich B., Nelson D.R., Dieterich D.T., Jacobson I.M., Jensen D., Abrams G.A., Darling J.M., Rodriguez-Torres M., Reddy K.R., Sulkowski M.S., Bzowej N.H., Hyland R.H., Mo H., Lin M., Mader M., Hindes R., Albanis E., Symonds W.T., Berrey M.M., Muir A. Sofosbuvir in combination with peginterferon alfa-2a and ribavirin for non-cirrhotic, treatment-naive patients with genotypes 1, 2, and 3 hepatitis C infection: a randomised, double-blind, phase 2 trial. Lancet Infect. Dis. 2013;13:401–408. doi: 10.1016/S1473-3099(13)70033-1. [DOI] [PubMed] [Google Scholar]
- Lawitz E., Sulkowski M.S., Ghalib R., Rodriguez-Torres M., Younossi Z.M., Corregidor A., DeJesus E., Pearlman B., Rabinovitz M., Gitlin N., Lim J.K., Pockros P.J., Scott J.D., Fevery B., Lambrecht T., Ouwerkerk-Mahadevan S., Callewaert K., Symonds W.T., Picchio G., Lindsay K.L., Beumont M., Jacobson I.M. Simeprevir plus sofosbuvir, with or without ribavirin, to treat chronic infection with hepatitis C virus genotype 1 in non-responders to pegylated interferon and ribavirin and treatment-naive patients: the COSMOS randomised study. Lancet. 2014;384:1756–1765. doi: 10.1016/S0140-6736(14)61036-9. [DOI] [PubMed] [Google Scholar]
- Lawitz E., Poordad F.F., Pang P.S., Hyland R.H., Ding X., Mo H., Symonds W.T., McHutchison J.G., Membreno F.E. Sofosbuvir and ledipasvir fixed-dose combination with and without ribavirin in treatment-naive and previously treated patients with genotype 1 hepatitis C virus infection (LONESTAR): an open-label, randomised, phase 2 trial. Lancet. 2014;383:515–523. doi: 10.1016/S0140-6736(13)62121-2. [DOI] [PubMed] [Google Scholar]
- Lawitz E., Jacobson I.M., Nelson D.R., Zeuzem S., Sulkowski M.S., Esteban R., Brainard D., McNally J., Symonds W.T., McHutchison J.G., Dieterich D., Gane E. Development of sofosbuvir for the treatment of hepatitis C virus infection. Ann. N. Y. Acad. Sci. 2015;1358:56–67. doi: 10.1111/nyas.12832. [DOI] [PubMed] [Google Scholar]
- Lawitz E., Poordad F., Brainard D.M., Hyland R.H., An D., Dvory-Sobol H., Symonds W.T., McHutchison J.G., Membreno F.E. Sofosbuvir with peginterferon-ribavirin for 12 weeks in previously treated patients with hepatitis C genotype 2 or 3 and cirrhosis. Hepatology. 2015;61:769–775. doi: 10.1002/hep.27567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawitz E., Makara M., Akarca U.S., Thuluvath P.J., Preotescu L.L., Varunok P., Morillas R.M., Hall C., Mobashery N., Redman R., Pilot-Matias T., Vilchez R.A., Hezode C. Efficacy and safety of ombitasvir, paritaprevir, and ritonavir in an open-label study of patients with genotype 1b chronic hepatitis C virus infection with and without cirrhosis. Gastroenterology. 2015;149:971–980. doi: 10.1053/j.gastro.2015.07.001. e971. [DOI] [PubMed] [Google Scholar]
- Lawitz E., Gane E., Pearlman B., Tam E., Ghesquiere W., Guyader D., Alric L., Bronowicki J.P., Lester L., Sievert W., Ghalib R., Balart L., Sund F., Lagging M., Dutko F., Shaughnessy M., Hwang P., Howe A.Y., Wahl J., Robertson M., Barr E., Haber B. Efficacy and safety of 12 weeks versus 18 weeks of treatment with grazoprevir (MK-5172) and elbasvir (MK-8742) with or without ribavirin for hepatitis C virus genotype 1 infection in previously untreated patients with cirrhosis and patients with previous null response with or without cirrhosis (C-WORTHY): a randomised, open-label phase 2 trial. Lancet. 2015;385:1075–1086. doi: 10.1016/S0140-6736(14)61795-5. [DOI] [PubMed] [Google Scholar]
- Lawitz E., Matusow G., DeJesus E., Yoshida E.M., Felizarta F., Ghalib R., Godofsky E., Herring R.W., Poleynard G., Sheikh A., Tobias H., Kugelmas M., Kalmeijer R., Peeters M., Lenz O., Fevery B., De La Rosa G., Scott J., Sinha R., Witek J. Simeprevir plus sofosbuvir in patients with chronic hepatitis C virus genotype 1 infection and cirrhosis: a phase 3 study (OPTIMIST-2) Hepatology. 2016;64:360–369. doi: 10.1002/hep.28422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawitz E., Poordad F., Gutierrez J.A., Wells J.T., Landaverde C.E., Evans B., Howe A., Huang H.C., Li J.J., Hwang P., Dutko F.J., Robertson M., Wahl J., Barr E., Haber B. Short-duration treatment with elbasvir/grazoprevir and sofosbuvir for hepatitis C: a randomized trial. Hepatology. 2016;65:439–450. doi: 10.1002/hep.28877. [DOI] [PubMed] [Google Scholar]
- Lawitz E., Reau N., Hinestrosa F., Rabinovitz M., Schiff E., Sheikh A., Younes Z., Herring R., Jr., Reddy K.R., Tran T., Bennett M., Nahass R., Yang J.C., Lu S., Dvory-Sobol H., Stamm L.M., Brainard D.M., McHutchison J.G., Pearlman B., Shiffman M., Hawkins T., Curry M., Jacobson I. Efficacy of sofosbuvir, velpatasvir, and GS-9857 in patients with genotype 1 hepatitis C virus infection in an open-label, phase 2 trial. Gastroenterology. 2016;151:893–901. doi: 10.1053/j.gastro.2016.07.039. [DOI] [PubMed] [Google Scholar]
- Lawitz E., Poordad F., Hyland R.H., Wang J., Liu L., Dvory-Sobol H., Brainard D.M., McHutchison J.G., Gutierrez J.A. Ledipasvir/sofosbuvir-based treatment of patients with chronic genotype-1 HCV infection and cirrhosis: results from two Phase II studies. Antivir. Ther. 2016;21:679–687. doi: 10.3851/IMP3062. [DOI] [PubMed] [Google Scholar]
- Lazerwith S.E., Lew W., Zhang J., Morganelli P., Liu Q., Canales E., Clarke M.O., Doerffler E., Byun D., Mertzman M., Ye H., Chong L., Xu L., Appleby T., Chen X., Fenaux M., Hashash A., Leavitt S.A., Mabery E., Matles M., Mwangi J.W., Tian Y., Lee Y.J., Zhang J., Zhu C., Murray B.P., Watkins W.J. Discovery of GS-9669, a thumb site II non-nucleoside inhibitor of NS5B for the treatment of genotype 1 chronic hepatitis C infection. J. Med. Chem. 2014;57:1893–1901. doi: 10.1021/jm401420j. [DOI] [PubMed] [Google Scholar]
- Lee Y.M., Duh Y., Wang S.T., Lai M.M., Yuan H.S., Lim C. Using an old drug to target a new drug site: application of disulfiram to target the Zn-Site in HCV NS5A protein. J. Am. Chem. Soc. 2016;138:3856–3862. doi: 10.1021/jacs.6b00299. [DOI] [PubMed] [Google Scholar]
- Leroy V., Angus P., Bronowicki J.P., Dore G.J., Hezode C., Pianko S., Pol S., Stuart K., Tse E., McPhee F., Bhore R., Jimenez-Exposito M.J., Thompson A.J. Daclatasvir, sofosbuvir, and ribavirin for hepatitis C virus genotype 3 and advanced liver disease: a randomized phase III study (ALLY-3+) Hepatology. 2016;63:1430–1441. doi: 10.1002/hep.28473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li G., De Clercq E. HIV genome-wide protein associations: a review of 30 Years of research. Microbiol. Mol. Biol. Rev. 2016;80:679–731. doi: 10.1128/MMBR.00065-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin T.I., Lenz O., Fanning G., Verbinnen T., Delouvroy F., Scholliers A., Vermeiren K., Rosenquist A., Edlund M., Samuelsson B., Vrang L., de Kock H., Wigerinck P., Raboisson P., Simmen K. In vitro activity and preclinical profile of TMC435350, a potent hepatitis C virus protease inhibitor. Antimicrob. Agents Chemother. 2009;53:1377–1385. doi: 10.1128/AAC.01058-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin L.T., Chung C.Y., Hsu W.C., Chang S.P., Hung T.C., Shields J., Russell R.S., Lin C.C., Li C.F., Yen M.H., Tyrrell D.L., Lin C.C., Richardson C.D. Saikosaponin b2 is a naturally occurring terpenoid that efficiently inhibits hepatitis C virus entry. J. Hepatol. 2015;62:541–548. doi: 10.1016/j.jhep.2014.10.040. [DOI] [PubMed] [Google Scholar]
- Lindenbach B.D., Rice C.M. Unravelling hepatitis C virus replication from genome to function. Nature. 2005;436:933–938. doi: 10.1038/nature04077. [DOI] [PubMed] [Google Scholar]
- Link J.O., Taylor J.G., Xu L., Mitchell M., Guo H., Liu H., Kato D., Kirschberg T., Sun J., Squires N., Parrish J., Keller T., Yang Z.Y., Yang C., Matles M., Wang Y., Wang K., Cheng G., Tian Y., Mogalian E., Mondou E., Cornpropst M., Perry J., Desai M.C. Discovery of ledipasvir (GS-5885): a potent, once-daily oral NS5A inhibitor for the treatment of hepatitis C virus infection. J. Med. Chem. 2014;57:2033–2046. doi: 10.1021/jm401499g. [DOI] [PubMed] [Google Scholar]
- Liu Y., Lim B.H., Jiang W.W., Flentge C.A., Hutchinson D.K., Madigan D.L., Randolph J.T., Wagner R., Maring C.J., Kati W.M., Molla A. Identification of aryl dihydrouracil derivatives as palm initiation site inhibitors of HCV NS5B polymerase. Bioorg. Med. Chem. Lett. 2012;22:3747–3750. doi: 10.1016/j.bmcl.2012.04.017. [DOI] [PubMed] [Google Scholar]
- Liverton N.J., Holloway M.K., McCauley J.A., Rudd M.T., Butcher J.W., Carroll S.S., DiMuzio J., Fandozzi C., Gilbert K.F., Mao S.S., McIntyre C.J., Nguyen K.T., Romano J.J., Stahlhut M., Wan B.L., Olsen D.B., Vacca J.P. Molecular modeling based approach to potent P2-P4 macrocyclic inhibitors of hepatitis C NS3/4A protease. J. Am. Chem. Soc. 2008;130:4607–4609. doi: 10.1021/ja711120r. [DOI] [PubMed] [Google Scholar]
- Llovet J.M., Villanueva A. Liver cancer: effect of HCV clearance with direct-acting antiviral agents on HCC. Nat. Rev. Gastroenterol. Hepatol. 2016;13:561–562. doi: 10.1038/nrgastro.2016.140. [DOI] [PubMed] [Google Scholar]
- Love R.A., Parge H.E., Wickersham J.A., Hostomsky Z., Habuka N., Moomaw E.W., Adachi T., Hostomska Z. The crystal structure of hepatitis C virus NS3 proteinase reveals a trypsin-like fold and a structural zinc binding site. Cell. 1996;87:331–342. doi: 10.1016/s0092-8674(00)81350-1. [DOI] [PubMed] [Google Scholar]
- Maasoumy B., Vermehren J., Welker M.W., Bremer B., Perner D., Honer Zu Siederdissen C., Deterding K., Lehmann P., Cloherty G., Reinhardt B., Pawlotsky J.M., Manns M.P., Zeuzem S., Cornberg M., Wedemeyer H., Sarrazin C. Clinical value of on-treatment HCV RNA levels during different sofosbuvir-based antiviral regimens. J. Hepatol. 2016;65:473–482. doi: 10.1016/j.jhep.2016.04.006. [DOI] [PubMed] [Google Scholar]
- Maheshwari A., Ray S., Thuluvath P.J. Acute hepatitis C. Lancet. 2008;372:321–332. doi: 10.1016/S0140-6736(08)61116-2. [DOI] [PubMed] [Google Scholar]
- Manfroni G., Cannalire R., Barreca M.L., Kaushik-Basu N., Leyssen P., Winquist J., Iraci N., Manvar D., Paeshuyse J., Guhamazumder R., Basu A., Sabatini S., Tabarrini O., Danielson U.H., Neyts J., Cecchetti V. The versatile nature of the 6-aminoquinolone scaffold: identification of submicromolar hepatitis C virus NS5B inhibitors. J. Med. Chem. 2014;57:1952–1963. doi: 10.1021/jm401362f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manfroni G., Manvar D., Barreca M.L., Kaushik-Basu N., Leyssen P., Paeshuyse J., Cannalire R., Iraci N., Basu A., Chudaev M., Zamperini C., Dreassi E., Sabatini S., Tabarrini O., Neyts J., Cecchetti V. New pyrazolobenzothiazine derivatives as hepatitis C virus NS5B polymerase palm site I inhibitors. J. Med. Chem. 2014;57:3247–3262. doi: 10.1021/jm401688h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mangia A., Arleo A., Copetti M., Miscio M., Piazzolla V., Santoro R., Squillante M.M. The combination of daclatasvir and sofosbuvir for curing genotype 2 patients who cannot tolerate ribavirin. Liver Int. 2016;36:971–976. doi: 10.1111/liv.13069. [DOI] [PubMed] [Google Scholar]
- Manns M.P., Wedemeyer H., Cornberg M. Treating viral hepatitis C: efficacy, side effects, and complications. Gut. 2006;55:1350–1359. doi: 10.1136/gut.2005.076646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manns M., Marcellin P., Poordad F., de Araujo E.S., Buti M., Horsmans Y., Janczewska E., Villamil F., Scott J., Peeters M., Lenz O., Ouwerkerk-Mahadevan S., De La Rosa G., Kalmeijer R., Sinha R., Beumont-Mauviel M. Simeprevir with pegylated interferon alfa 2a or 2b plus ribavirin in treatment-naive patients with chronic hepatitis C virus genotype 1 infection (QUEST-2): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2014;384:414–426. doi: 10.1016/S0140-6736(14)60538-9. [DOI] [PubMed] [Google Scholar]
- Manns M., Samuel D., Gane E.J., Mutimer D., McCaughan G., Buti M., Prieto M., Calleja J.L., Peck-Radosavljevic M., Mullhaupt B., Agarwal K., Angus P., Yoshida E.M., Colombo M., Rizzetto M., Dvory-Sobol H., Denning J., Arterburn S., Pang P.S., Brainard D., McHutchison J.G., Dufour J.F., Van Vlierberghe H., van Hoek B., Forns X., SOLAR-2 investigators Ledipasvir and sofosbuvir plus ribavirin in patients with genotype 1 or 4 hepatitis C virus infection and advanced liver disease: a multicentre, open-label, randomised, phase 2 trial. Lancet Infect. Dis. 2016;16:685–697. doi: 10.1016/S1473-3099(16)00052-9. [DOI] [PubMed] [Google Scholar]
- Marcellin P., Cooper C., Balart L., Larrey D., Box T., Yoshida E., Lawitz E., Buggisch P., Ferenci P., Weltman M., Labriola-Tompkins E., Le Pogam S., Najera I., Thomas D., Hooper G., Shulman N.S., Zhang Y., Navarro M.T., Lim C.Y., Brunda M., Terrault N.A., Yetzer E.S. Randomized controlled trial of danoprevir plus peginterferon alfa-2a and ribavirin in treatment-naive patients with hepatitis C virus genotype 1 infection. Gastroenterology. 2013;145:790–800. doi: 10.1053/j.gastro.2013.06.051. e793. [DOI] [PubMed] [Google Scholar]
- McCauley J.A., Rudd M.T. Hepatitis C virus NS3/4a protease inhibitors. Curr. Opin. Pharmacol. 2016;30:84–92. doi: 10.1016/j.coph.2016.07.015. [DOI] [PubMed] [Google Scholar]
- McGivern D.R., Masaki T., Williford S., Ingravallo P., Feng Z., Lahser F., Asante-Appiah E., Neddermann P., De Francesco R., Howe A.Y., Lemon S.M. Kinetic analyses reveal potent and early blockade of hepatitis C virus assembly by NS5A inhibitors. Gastroenterology. 2014;147:453–462. doi: 10.1053/j.gastro.2014.04.021. e457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messina J.P., Humphreys I., Flaxman A., Brown A., Cooke G.S., Pybus O.G., Barnes E. Global distribution and prevalence of hepatitis C virus genotypes. Hepatology. 2015;61:77–87. doi: 10.1002/hep.27259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizokami M., Yokosuka O., Takehara T., Sakamoto N., Korenaga M., Mochizuki H., Nakane K., Enomoto H., Ikeda F., Yanase M., Toyoda H., Genda T., Umemura T., Yatsuhashi H., Ide T., Toda N., Nirei K., Ueno Y., Nishigaki Y., Betular J., Gao B., Ishizaki A., Omote M., Mo H., Garrison K., Pang P.S., Knox S.J., Symonds W.T., McHutchison J.G., Izumi N., Omata M. Ledipasvir and sofosbuvir fixed-dose combination with and without ribavirin for 12 weeks in treatment-naive and previously treated Japanese patients with genotype 1 hepatitis C: an open-label, randomised, phase 3 trial. Lancet Infect. Dis. 2015;15:645–653. doi: 10.1016/S1473-3099(15)70099-X. [DOI] [PubMed] [Google Scholar]
- Moradpour D., Penin F. Hepatitis C virus proteins: from structure to function. Curr. Top. Microbiol. Immunol. 2013;369:113–142. doi: 10.1007/978-3-642-27340-7_5. [DOI] [PubMed] [Google Scholar]
- Moradpour D., Penin F., Rice C.M. Replication of hepatitis C virus. Nat. Rev. Microbiol. 2007;5:453–463. doi: 10.1038/nrmicro1645. [DOI] [PubMed] [Google Scholar]
- Morales J.M., Fabrizi F. Hepatitis C and its impact on renal transplantation. Nat. Rev. Nephrol. 2015;11:172–182. doi: 10.1038/nrneph.2015.5. [DOI] [PubMed] [Google Scholar]
- Moreno C., Hezode C., Marcellin P., Bourgeois S., Francque S., Samuel D., Zoulim F., Grange J.D., Shukla U., Lenz O., Ouwerkerk-Mahadevan S., Fevery B., Peeters M., Beumont M., Jessner W. Efficacy and safety of simeprevir with PegIFN/ribavirin in naive or experienced patients infected with chronic HCV genotype 4. J. Hepatol. 2015;62:1047–1055. doi: 10.1016/j.jhep.2014.12.031. [DOI] [PubMed] [Google Scholar]
- Mortality GBD, Causes of Death C Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1459–1544. doi: 10.1016/S0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moucari R., Forestier N., Larrey D., Guyader D., Couzigou P., Benhamou Y., Voitot H., Vidaud M., Seiwert S., Bradford B., Zeuzem S., Marcellin P. Danoprevir, an HCV NS3/4A protease inhibitor, improves insulin sensitivity in patients with genotype 1 chronic hepatitis C. Gut. 2010;59:1694–1698. doi: 10.1136/gut.2010.219089. [DOI] [PubMed] [Google Scholar]
- Muir A.J., Poordad F., Lalezari J., Everson G., Dore G.J., Herring R., Sheikh A., Kwo P., Hezode C., Pockros P.J., Tran A., Yozviak J., Reau N., Ramji A., Stuart K., Thompson A.J., Vierling J., Freilich B., Cooper J., Ghesquiere W., Yang R., McPhee F., Hughes E.A., Swenson E.S., Yin P.D. Daclatasvir in combination with asunaprevir and beclabuvir for hepatitis C virus genotype 1 infection with compensated cirrhosis. JAMA. 2015;313:1736–1744. doi: 10.1001/jama.2015.3868. [DOI] [PubMed] [Google Scholar]
- Murphy D.G., Sablon E., Chamberland J., Fournier E., Dandavino R., Tremblay C.L. Hepatitis C virus genotype 7, a new genotype originating from central Africa. J. Clin. Microbiol. 2015;53:967–972. doi: 10.1128/JCM.02831-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahon P., Bourcier V., Layese R., Audureau E., Cagnot C., Marcellin P., Guyader D., Fontaine H., Larrey D., De Ledinghen V., Ouzan D., Zoulim F., Roulot D., Tran A., Bronowicki J.P., Zarski J.P., Leroy V., Riachi G., Cales P., Peron J.M., Alric L., Bourliere M., Mathurin P., Dharancy S., Blanc J.F., Abergel A., Serfaty L., Mallat A., Grange J.D., Attali P., Bacq Y., Wartelle C., Dao T., Benhamou Y., Pilette C., Silvain C., Christidis C., Capron D., Bernard-Chabert B., Zucman D., Di Martino V., Thibaut V., Salmon D., Ziol M., Sutton A., Pol S., Roudot-Thoraval F., Group A.C.C. Eradication of Hepatitis C virus infection in patients with cirrhosis reduces risk of liver and non-liver complications. Gastroenterology. 2017;152:142–156. doi: 10.1053/j.gastro.2016.09.009. e142. [DOI] [PubMed] [Google Scholar]
- Neelamkavil S.F., Agrawal S., Bara T., Bennett C., Bhat S., Biswas D., Brockunier L., Buist N., Burnette D., Cartwright M., Chackalamannil S., Chase R., Chelliah M., Chen A., Clasby M., Colandrea V.J., Davies I.W., Eagen K., Guo Z., Han Y., Howe J., Jayne C., Josien H., Kargman S., Marcantonio K., Miao S., Miller R., Nolting A., Pinto P., Rajagopalan M., Ruck R.T., Shah U., Soriano A., Sperbeck D., Velazquez F., Wu J., Xia Y., Venkatraman S. Discovery of MK-8831, a novel spiro-proline macrocycle as a Pan-Genotypic HCV-NS3/4a protease inhibitor. ACS Med. Chem. Lett. 2016;7:111–116. doi: 10.1021/acsmedchemlett.5b00425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson D.R., Cooper J.N., Lalezari J.P., Lawitz E., Pockros P.J., Gitlin N., Freilich B.F., Younes Z.H., Harlan W., Ghalib R., Oguchi G., Thuluvath P.J., Ortiz-Lasanta G., Rabinovitz M., Bernstein D., Bennett M., Hawkins T., Ravendhran N., Sheikh A.M., Varunok P., Kowdley K.V., Hennicken D., McPhee F., Rana K., Hughes E.A., ALLY-3 Study Team All-oral 12-week treatment with daclatasvir plus sofosbuvir in patients with hepatitis C virus genotype 3 infection: ALLY-3 phase III study. Hepatology. 2015;61:1127–1135. doi: 10.1002/hep.27726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nettles J.H., Stanton R.A., Broyde J., Amblard F., Zhang H., Zhou L., Shi J., McBrayer T.R., Whitaker T., Coats S.J., Kohler J.J., Schinazi R.F. Asymmetric binding to NS5A by daclatasvir (BMS-790052) and analogs suggests two novel modes of HCV inhibition. J. Med. Chem. 2014;57:10031–10043. doi: 10.1021/jm501291c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumann A.U., Lam N.P., Dahari H., Gretch D.R., Wiley T.E., Layden T.J., Perelson A.S. Hepatitis C viral dynamics in vivo and the antiviral efficacy of interferon-alpha therapy. Science. 1998;282:103–107. doi: 10.1126/science.282.5386.103. [DOI] [PubMed] [Google Scholar]
- Njoroge F.G., Chen K.X., Shih N.Y., Piwinski J.J. Challenges in modern drug discovery: a case study of boceprevir, an HCV protease inhibitor for the treatment of hepatitis C virus infection. Acc. Chem. Res. 2008;41:50–59. doi: 10.1021/ar700109k. [DOI] [PubMed] [Google Scholar]
- Ogata N., Alter H.J., Miller R.H., Purcell R.H. Nucleotide sequence and mutation rate of the H strain of hepatitis C virus. Proc. Natl. Acad. Sci. U. S. A. 1991;88:3392–3396. doi: 10.1073/pnas.88.8.3392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogawa E., Furusyo N., Nomura H., Takahashi K., Higashi N., Kawano A., Dohmen K., Satoh T., Azuma K., Nakamuta M., Koyanagi T., Kato M., Shimoda S., Kajiwara E., Hayashi J., Kyushu University Liver Disease Study (KULDS) Group Effectiveness and safety of sofosbuvir plus ribavirin for HCV genotype 2 patients 65 and over with or without cirrhosis. Antivir. Res. 2016;136:37–44. doi: 10.1016/j.antiviral.2016.10.012. [DOI] [PubMed] [Google Scholar]
- O'Leary J.G., Fontana R.J., Brown K., Burton J.R., Jr., Firpi-Morell R., Muir A., O'Brien C., Rabinovitz M., Reddy R., Ryan R., Shprecher A., Villadiego S., Prabhakar A., Brown R.S., Jr. Efficacy and safety of simeprevir and sofosbuvir with and without ribavirin in subjects with recurrent genotype 1 hepatitis C postorthotopic liver transplant: the randomized GALAXY study. Transpl. Int. Off. J. European Soc. Organ Transpl. 2017;30:196–208. doi: 10.1111/tri.12896. [DOI] [PubMed] [Google Scholar]
- Omata M., Nishiguchi S., Ueno Y., Mochizuki H., Izumi N., Ikeda F., Toyoda H., Yokosuka O., Nirei K., Genda T., Umemura T., Takehara T., Sakamoto N., Nishigaki Y., Nakane K., Toda N., Ide T., Yanase M., Hino K., Gao B., Garrison K.L., Dvory-Sobol H., Ishizaki A., Omote M., Brainard D., Knox S., Symonds W.T., McHutchison J.G., Yatsuhashi H., Mizokami M. Sofosbuvir plus ribavirin in Japanese patients with chronic genotype 2 HCV infection: an open-label, phase 3 trial. J. Viral Hepat. 2014;21:762–768. doi: 10.1111/jvh.12312. [DOI] [PubMed] [Google Scholar]
- Osinusi A., Meissner E.G., Lee Y.J., Bon D., Heytens L., Nelson A., Sneller M., Kohli A., Barrett L., Proschan M., Herrmann E., Shivakumar B., Gu W., Kwan R., Teferi G., Talwani R., Silk R., Kotb C., Wroblewski S., Fishbein D., Dewar R., Highbarger H., Zhang X., Kleiner D., Wood B.J., Chavez J., Symonds W.T., Subramanian M., McHutchison J., Polis M.A., Fauci A.S., Masur H., Kottilil S. Sofosbuvir and ribavirin for hepatitis C genotype 1 in patients with unfavorable treatment characteristics: a randomized clinical trial. JAMA. 2013;310:804–811. doi: 10.1001/jama.2013.109309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osinusi A., Kohli A., Marti M.M., Nelson A., Zhang X., Meissner E.G., Silk R., Townsend K., Pang P.S., Subramanian G.M., McHutchison J.G., Fauci A.S., Masur H., Kottilil S. Re-treatment of chronic hepatitis C virus genotype 1 infection after relapse: an open-label pilot study. Ann. Intern Med. 2014;161:634–638. doi: 10.7326/M14-1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OuYang B., Xie S., Berardi M.J., Zhao X., Dev J., Yu W., Sun B., Chou J.J. Unusual architecture of the p7 channel from hepatitis C virus. Nature. 2013;498:521–525. doi: 10.1038/nature12283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens C.M., Brasher B.B., Polemeropoulos A., Rhodin M.H., McAllister N., Peng X., Wang C., Ying L., Cao H., Lawitz E., Poordad F., Rondon J., Box T.D., Zeuzem S., Buggisch P., Lin K., Qiu Y.L., Jiang L., Colvin R., Or Y.S. Preclinical profile and clinical efficacy of a novel hepatitis C virus NS5A inhibitor, EDP-239. Antimicrob. Agents Chemother. 2016;60:6207–6215. doi: 10.1128/AAC.00808-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens C.M., Brasher B.B., Polemeropoulos A., Rhodin M.H., McAllister N., Wong K.A., Jones C.T., Jiang L., Lin K., Or Y.S. Preclinical and clinical resistance profile of EDP-239, a novel hepatitis C virus NS5A inhibitor. Antimicrob. Agents Chemother. 2016;60:6216–6226. doi: 10.1128/AAC.00815-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pawlotsky J.M. Hepatitis C virus resistance to direct-acting antiviral drugs in interferon-free regimens. Gastroenterology. 2016;151:70–86. doi: 10.1053/j.gastro.2016.04.003. [DOI] [PubMed] [Google Scholar]
- Pawlotsky J.M., Flisiak R., Sarin S.K., Rasenack J., Piratvisuth T., Chuang W.L., Peng C.Y., Foster G.R., Shah S., Wedemeyer H., Hezode C., Zhang W., Wong K.A., Li B., Avila C., Naoumov N.V., VITAL-1 study team Alisporivir plus ribavirin, interferon free or in combination with pegylated interferon, for hepatitis C virus genotype 2 or 3 infection. Hepatology. 2015;62:1013–1023. doi: 10.1002/hep.27960. [DOI] [PubMed] [Google Scholar]
- Perin P.M., Haid S., Brown R.J., Doerrbecker J., Schulze K., Zeilinger C., von Schaewen M., Heller B., Vercauteren K., Luxenburger E., Baktash Y.M., Vondran F.W., Speerstra S., Awadh A., Mukhtarov F., Schang L.M., Kirschning A., Muller R., Guzman C.A., Kaderali L., Randall G., Meuleman P., Ploss A., Pietschmann T. Flunarizine prevents hepatitis C virus membrane fusion in a genotype-dependent manner by targeting the potential fusion peptide within E1. Hepatology. 2016;63:49–62. doi: 10.1002/hep.28111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips B., Cai R., Delaney W., Du Z., Ji M., Jin H., Lee J., Li J., Niedziela-Majka A., Mish M., Pyun H.J., Saugier J., Tirunagari N., Wang J., Yang H., Wu Q., Sheng C., Zonte C. Highly potent HCV NS4B inhibitors with activity against multiple genotypes. J. Med. Chem. 2014;57:2161–2166. doi: 10.1021/jm401646w. [DOI] [PubMed] [Google Scholar]
- Pianko S., Flamm S.L., Shiffman M.L., Kumar S., Strasser S.I., Dore G.J., McNally J., Brainard D.M., Han L., Doehle B., Mogalian E., McHutchison J.G., Rabinovitz M., Towner W.J., Gane E.J., Stedman C.A., Reddy K.R., Roberts S.K. Sofosbuvir plus velpatasvir combination therapy for treatment-experienced patients with genotype 1 or 3 hepatitis C virus infection: a randomized trial. Ann. Intern Med. 2015;163:809–817. doi: 10.7326/M15-1014. [DOI] [PubMed] [Google Scholar]
- Pilot-Matias T., Tripathi R., Cohen D., Gaultier I., Dekhtyar T., Lu L., Reisch T., Irvin M., Hopkins T., Pithawalla R., Middleton T., Ng T., McDaniel K., Or Y.S., Menon R., Kempf D., Molla A., Collins C. In vitro and in vivo antiviral activity and resistance profile of the hepatitis C virus NS3/4A protease inhibitor ABT-450. Antimicrob. Agents Chemother. 2015;59:988–997. doi: 10.1128/AAC.04227-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pockros P.J., Jensen D., Tsai N., Taylor R., Ramji A., Cooper C., Dickson R., Tice A., Kulkarni R., Vierling J.M., Lou Munson M., Chen Y.C., Najera I., Thommes J., JUMP-C Investigators JUMP-C: a randomized trial of mericitabine plus pegylated interferon alpha-2a/ribavirin for 24 weeks in treatment-naive HCV genotype 1/4 patients. Hepatology. 2013;58:514–523. doi: 10.1002/hep.26275. [DOI] [PubMed] [Google Scholar]
- Pockros P.J., Reddy K.R., Mantry P.S., Cohen E., Bennett M., Sulkowski M.S., Bernstein D.E., Cohen D.E., Shulman N.S., Wang D., Khatri A., Abunimeh M., Podsadecki T., Lawitz E. Efficacy of direct-acting antiviral combination for patients with hepatitis C virus genotype 1 infection and severe renal impairment or end-stage renal disease. Gastroenterology. 2016;150:1590–1598. doi: 10.1053/j.gastro.2016.02.078. [DOI] [PubMed] [Google Scholar]
- Pol S., Sulkowski M.S., Hassanein T., Gane E.J., Liu L., Mo H., Doehle B., Kanwar B., Brainard D., Subramanian G.M., Symonds W.T., McHutchison J.G., Nahass R.G., Bennett M., Jacobson I.M. Sofosbuvir plus pegylated interferon and ribavirin in patients with genotype 1 hepatitis C virus in whom previous therapy with direct-acting antivirals has failed. Hepatology. 2015;62:129–134. doi: 10.1002/hep.27836. [DOI] [PubMed] [Google Scholar]
- Pol S., Bourliere M., Lucier S., Hezode C., Dorival C., Larrey D., Bronowicki J.P., Ledinghen V.D., Zoulim F., Tran A., Metivier S., Zarski J.P., Samuel D., Guyader D., Marcellin P., Minello A., Alric L., Thabut D., Chazouilleres O., Riachi G., Bourcier V., Mathurin P., Loustaud-Ratti V., D'Alteroche L., Fouchard-Hubert I., Habersetzer F., Causse X., Geist C., Rosa I., Gournay J., Saillard E., Billaud E., Petrov-Sanchez V., Diallo A., Fontaine H., Carrat F., ANRS/AFEF HEPATHER study group Safety and efficacy of daclatasvir-sofosbuvir in HCV genotype 1-mono-infected patients. J. Hepatol. 2017;66:39–47. doi: 10.1016/j.jhep.2016.08.021. [DOI] [PubMed] [Google Scholar]
- Poordad F., McCone J., Jr., Bacon B.R., Bruno S., Manns M.P., Sulkowski M.S., Jacobson I.M., Reddy K.R., Goodman Z.D., Boparai N., DiNubile M.J., Sniukiene V., Brass C.A., Albrecht J.K., Bronowicki J.P., SPRINT-2 Investigators Boceprevir for untreated chronic HCV genotype 1 infection. N. Engl. J. Med. 2011;364:1195–1206. doi: 10.1056/NEJMoa1010494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poordad F., Lawitz E., Reddy K.R., Afdhal N.H., Hezode C., Zeuzem S., Lee S.S., Calleja J.L., Brown R.S., Jr., Craxi A., Wedemeyer H., Nyberg L., Nelson D.R., Rossaro L., Balart L., Morgan T.R., Bacon B.R., Flamm S.L., Kowdley K.V., Deng W., Koury K.J., Pedicone L.D., Dutko F.J., Burroughs M.H., Alves K., Wahl J., Brass C.A., Albrecht J.K., Sulkowski M.S., Protocol 6086 Investigators Effects of ribavirin dose reduction vs erythropoietin for boceprevir-related anemia in patients with chronic hepatitis C virus genotype 1 infection–a randomized trial. Gastroenterology. 2013;145:1035–1044. doi: 10.1053/j.gastro.2013.07.051. e1035. [DOI] [PubMed] [Google Scholar]
- Poordad F., Hezode C., Trinh R., Kowdley K.V., Zeuzem S., Agarwal K., Shiffman M.L., Wedemeyer H., Berg T., Yoshida E.M., Forns X., Lovell S.S., Da Silva-Tillmann B., Collins C.A., Campbell A.L., Podsadecki T., Bernstein B. ABT-450/r-ombitasvir and dasabuvir with ribavirin for hepatitis C with cirrhosis. N. Engl. J. Med. 2014;370:1973–1982. doi: 10.1056/NEJMoa1402869. [DOI] [PubMed] [Google Scholar]
- Poordad F., Sievert W., Mollison L., Bennett M., Tse E., Brau N., Levin J., Sepe T., Lee S.S., Angus P., Conway B., Pol S., Boyer N., Bronowicki J.P., Jacobson I., Muir A.J., Reddy K.R., Tam E., Ortiz-Lasanta G., de Ledinghen V., Sulkowski M., Boparai N., McPhee F., Hughes E., Swenson E.S., Yin P.D., Unity-1 Study Group Fixed-dose combination therapy with daclatasvir, asunaprevir, and beclabuvir for noncirrhotic patients with HCV genotype 1 infection. JAMA. 2015;313:1728–1735. doi: 10.1001/jama.2015.3860. [DOI] [PubMed] [Google Scholar]
- Poordad F., Schiff E.R., Vierling J.M., Landis C., Fontana R.J., Yang R., McPhee F., Hughes E.A., Noviello S., Swenson E.S. Daclatasvir with sofosbuvir and ribavirin for hepatitis C virus infection with advanced cirrhosis or post-liver transplantation recurrence. Hepatology. 2016;63:1493–1505. doi: 10.1002/hep.28446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poordad F., Gordon S.C., Asatryan A., Felizarta F., Reindollar R.W., Landis C., Fried M.W., Bernstein D.E., Ng T.I., Lin C.-W., Liu R., Kort J., Mensa F.J. 51st Annual Meeting of the European Association for the Study of the Liver (EASL), Barcelona, Spain. 15 April 2016. High efficacy of ABT-493 and ABT-530 in HCV genotype 1-infected patients who have failed direct-acting antiviral-containing regimens: the MAGELLAN-I study. [Google Scholar]
- Poordad F., Landis C.S., Asatryan A., Jackson D.F., 3rd, Ng T.I., Fu B., Lin C.W., Yao B., Kort J. High antiviral activity of NS5A inhibitor ABT-530 with paritaprevir/ritonavir and ribavirin against hepatitis C virus genotype 3 infection. Liver Int. 2016;36:1125–1132. doi: 10.1111/liv.13067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prigozhin D.M., Modis Y. Flunarizine arrests hepatitis C virus membrane fusion. Hepatology. 2016;63:14–16. doi: 10.1002/hep.28224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian X.J., Zhu Y.Z., Zhao P., Qi Z.T. Entry inhibitors: new advances in HCV treatment. Emerg. Microb. Infect. 2016;5:e3. doi: 10.1038/emi.2016.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramirez S., Mikkelsen L.S., Gottwein J.M., Bukh J. Robust HCV genotype 3a infectious cell culture system permits identification of escape variants with resistance to sofosbuvir. Gastroenterology. 2016;151:973–985. doi: 10.1053/j.gastro.2016.07.013. e972. [DOI] [PubMed] [Google Scholar]
- Reddy K.R., Zeuzem S., Zoulim F., Weiland O., Horban A., Stanciu C., Villamil F.G., Andreone P., George J., Dammers E., Fu M., Kurland D., Lenz O., Ouwerkerk-Mahadevan S., Verbinnen T., Scott J., Jessner W. Simeprevir versus telaprevir with peginterferon and ribavirin in previous null or partial responders with chronic hepatitis C virus genotype 1 infection (ATTAIN): a randomised, double-blind, non-inferiority phase 3 trial. Lancet Infect. Dis. 2015;15:27–35. doi: 10.1016/S1473-3099(14)71002-3. [DOI] [PubMed] [Google Scholar]
- Reddy K.R., Bourliere M., Sulkowski M., Omata M., Zeuzem S., Feld J.J., Lawitz E., Marcellin P., Welzel T.M., Hyland R., Ding X., Yang J., Knox S., Pang P., Dvory-Sobol H., Subramanian G.M., Symonds W., McHutchison J.G., Mangia A., Gane E., Mizokami M., Pol S., Afdhal N. Ledipasvir and sofosbuvir in patients with genotype 1 hepatitis C virus infection and compensated cirrhosis: an integrated safety and efficacy analysis. Hepatology. 2015;62:79–86. doi: 10.1002/hep.27826. [DOI] [PubMed] [Google Scholar]
- Rehermann B. Hepatitis C virus versus innate and adaptive immune responses: a tale of coevolution and coexistence. J. Clin. Investig. 2009;119:1745–1754. doi: 10.1172/JCI39133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reig M., Marino Z., Perello C., Inarrairaegui M., Ribeiro A., Lens S., Diaz A., Vilana R., Darnell A., Varela M., Sangro B., Calleja J.L., Forns X., Bruix J. Unexpected high rate of early tumor recurrence in patients with HCV-related HCC undergoing interferon-free therapy. J. Hepatol. 2016;65:719–726. doi: 10.1016/j.jhep.2016.04.008. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Torres M., Glass S., Hill J., Freilich B., Hassman D., Di Bisceglie A.M., Taylor J.G., Kirby B.J., Dvory-Sobol H., Yang J.C., An D., Stamm L.M., Brainard D.M., Kim S., Krefetz D., Smith W., Marbury T., Lawitz E. GS-9857 in patients with chronic hepatitis C virus genotype 1-4 infection: a randomized, double-blind, dose-ranging phase 1 study. J. Viral Hepat. 2016;23:614–622. doi: 10.1111/jvh.12527. [DOI] [PubMed] [Google Scholar]
- Rosenquist A., Samuelsson B., Johansson P.O., Cummings M.D., Lenz O., Raboisson P., Simmen K., Vendeville S., de Kock H., Nilsson M., Horvath A., Kalmeijer R., de la Rosa G., Beumont-Mauviel M. Discovery and development of simeprevir (TMC435), a HCV NS3/4A protease inhibitor. J. Med. Chem. 2014;57:1673–1693. doi: 10.1021/jm401507s. [DOI] [PubMed] [Google Scholar]
- Roth D., Nelson D.R., Bruchfeld A., Liapakis A., Silva M., Monsour H., Jr., Martin P., Pol S., Londono M.C., Hassanein T., Zamor P.J., Zuckerman E., Wan S., Jackson B., Nguyen B.Y., Robertson M., Barr E., Wahl J., Greaves W. Grazoprevir plus elbasvir in treatment-naive and treatment-experienced patients with hepatitis C virus genotype 1 infection and stage 4-5 chronic kidney disease (the C-SURFER study): a combination phase 3 study. Lancet. 2015;386:1537–1545. doi: 10.1016/S0140-6736(15)00349-9. [DOI] [PubMed] [Google Scholar]
- Ruane P.J., Ain D., Stryker R., Meshrekey R., Soliman M., Wolfe P.R., Riad J., Mikhail S., Kersey K., Jiang D., Massetto B., Doehle B., Kirby B.J., Knox S.J., McHutchison J.G., Symonds W.T. Sofosbuvir plus ribavirin for the treatment of chronic genotype 4 hepatitis C virus infection in patients of Egyptian ancestry. J. Hepatol. 2015;62:1040–1046. doi: 10.1016/j.jhep.2014.10.044. [DOI] [PubMed] [Google Scholar]
- Sarrazin C. The importance of resistance to direct antiviral drugs in HCV infection in clinical practice. J. Hepatol. 2016;64:486–504. doi: 10.1016/j.jhep.2015.09.011. [DOI] [PubMed] [Google Scholar]
- Sarrazin C., Dvory-Sobol H., Svarovskaia E.S., Doehle B.P., Pang P.S., Chuang S.M., Ma J., Ding X., Afdhal N.H., Kowdley K.V., Gane E.J., Lawitz E., Brainard D.M., McHutchison J.G., Miller M.D., Mo H. Prevalence of resistance-associated substitutions in HCV NS5A, NS5B, or NS3 and outcomes of treatment with ledipasvir and sofosbuvir. Gastroenterology. 2016;151:501–512. doi: 10.1053/j.gastro.2016.06.002. e501. [DOI] [PubMed] [Google Scholar]
- Scheel T.K., Rice C.M. Understanding the hepatitis C virus life cycle paves the way for highly effective therapies. Nat. Med. 2013;19:837–849. doi: 10.1038/nm.3248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreiber J., McNally J., Chodavarapu K., Svarovskaia E., Moreno C. Treatment of a patient with genotype 7 hepatitis C virus infection with sofosbuvir and velpatasvir. Hepatology. 2016;64:983–985. doi: 10.1002/hep.28636. [DOI] [PubMed] [Google Scholar]
- Scola P.M., Wang A.X., Good A.C., Sun L.Q., Combrink K.D., Campbell J.A., Chen J., Tu Y., Sin N., Venables B.L., Sit S.Y., Chen Y., Cocuzza A., Bilder D.M., D'Andrea S., Zheng B., Hewawasam P., Ding M., Thuring J., Li J., Hernandez D., Yu F., Falk P., Zhai G., Sheaffer A.K., Chen C., Lee M.S., Barry D., Knipe J.O., Li W., Han Y.H., Jenkins S., Gesenberg C., Gao Q., Sinz M.W., Santone K.S., Zvyaga T., Rajamani R., Klei H.E., Colonno R.J., Grasela D.M., Hughes E., Chien C., Adams S., Levesque P.C., Li D., Zhu J., Meanwell N.A., McPhee F. Discovery and early clinical evaluation of BMS-605339, a potent and orally efficacious tripeptidic acylsulfonamide NS3 protease inhibitor for the treatment of hepatitis C virus infection. J. Med. Chem. 2014;57:1708–1729. doi: 10.1021/jm401840s. [DOI] [PubMed] [Google Scholar]
- Scola P.M., Sun L.Q., Wang A.X., Chen J., Sin N., Venables B.L., Sit S.Y., Chen Y., Cocuzza A., Bilder D.M., D'Andrea S.V., Zheng B., Hewawasam P., Tu Y., Friborg J., Falk P., Hernandez D., Levine S., Chen C., Yu F., Sheaffer A.K., Zhai G., Barry D., Knipe J.O., Han Y.H., Schartman R., Donoso M., Mosure K., Sinz M.W., Zvyaga T., Good A.C., Rajamani R., Kish K., Tredup J., Klei H.E., Gao Q., Mueller L., Colonno R.J., Grasela D.M., Adams S.P., Loy J., Levesque P.C., Sun H., Shi H., Sun L., Warner W., Li D., Zhu J., Meanwell N.A., McPhee F. The discovery of asunaprevir (BMS-650032), an orally efficacious NS3 protease inhibitor for the treatment of hepatitis C virus infection. J. Med. Chem. 2014;57:1730–1752. doi: 10.1021/jm500297k. [DOI] [PubMed] [Google Scholar]
- Scull M.A., Schneider W.M., Flatley B.R., Hayden R., Fung C., Jones C.T., van de Belt M., Penin F., Rice C.M. The N-terminal helical region of the hepatitis C virus p7 Ion Channel protein is critical for infectious virus production. PLoS Pathog. 2015;11:e1005297. doi: 10.1371/journal.ppat.1005297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selzner N., Guindi M., Renner E.L., Berenguer M. Immune-mediated complications of the graft in interferon-treated hepatitis C positive liver transplant recipients. J. Hepatol. 2011;55:207–217. doi: 10.1016/j.jhep.2010.11.012. [DOI] [PubMed] [Google Scholar]
- Sheng X.C., Casarez A., Cai R., Clarke M.O., Chen X., Cho A., Delaney WEt, Doerffler E., Ji M., Mertzman M., Pakdaman R., Pyun H.J., Rowe T., Wu Q., Xu J., Kim C.U. Discovery of GS-9256: a novel phosphinic acid derived inhibitor of the hepatitis C virus NS3/4A protease with potent clinical activity. Bioorg. Med. Chem. Lett. 2012;22:1394–1396. doi: 10.1016/j.bmcl.2011.12.038. [DOI] [PubMed] [Google Scholar]
- Sheng X.C., Appleby T., Butler T., Cai R., Chen X., Cho A., Clarke M.O., Cottell J., Delaney W.E., IV, Doerffler E., Link J., Ji M., Pakdaman R., Pyun H.J., Wu Q., Xu J., Kim C.U. Discovery of GS-9451: an acid inhibitor of the hepatitis C virus NS3/4A protease. Bioorg. Med. Chem. Lett. 2012;22:2629–2634. doi: 10.1016/j.bmcl.2012.01.017. [DOI] [PubMed] [Google Scholar]
- Shepard C.W., Finelli L., Alter M.J. Global epidemiology of hepatitis C virus infection. Lancet Infect. Dis. 2005;5:558–567. doi: 10.1016/S1473-3099(05)70216-4. [DOI] [PubMed] [Google Scholar]
- Shiffman M.L., James A.M., Long A.G., Alexander P.C. Treatment of chronic HCV with sofosbuvir and simeprevir in patients with cirrhosis and contraindications to interferon and/or ribavirin. Am. J. Gastroenterol. 2015;110:1179–1185. doi: 10.1038/ajg.2015.218. [DOI] [PubMed] [Google Scholar]
- Shih I.H., Vliegen I., Peng B., Yang H., Hebner C., Paeshuyse J., Purstinger G., Fenaux M., Tian Y., Mabery E., Qi X., Bahador G., Paulson M., Lehman L.S., Bondy S., Tse W., Reiser H., Lee W.A., Schmitz U., Neyts J., Zhong W. Mechanistic characterization of GS-9190 (Tegobuvir), a novel nonnucleoside inhibitor of hepatitis C virus NS5B polymerase. Antimicrob. Agents Chemother. 2011;55:4196–4203. doi: 10.1128/AAC.00307-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimura S., Ishima M., Nakajima S., Fujii T., Himeno N., Ikeda K., Izaguirre-Carbonell J., Murata H., Takeuchi T., Kamisuki S., Suzuki T., Kuramochi K., Watashi K., Kobayashi S., Sugawara F. Total synthesis and anti-hepatitis C virus activity of MA026. J. Am. Chem. Soc. 2013;135:18949–18956. doi: 10.1021/ja410145x. [DOI] [PubMed] [Google Scholar]
- Silva M.O., Treitel M., Graham D.J., Curry S., Frontera M.J., McMonagle P., Gupta S., Hughes E., Chase R., Lahser F., Barnard R.J., Howe A.Y., Howe J.A. Antiviral activity of boceprevir monotherapy in treatment-naive subjects with chronic hepatitis C genotype 2/3. J. Hepatol. 2013;59:31–37. doi: 10.1016/j.jhep.2013.02.018. [DOI] [PubMed] [Google Scholar]
- Simmonds P. The origin of hepatitis C virus. Curr. Top. Microbiol. Immunol. 2013;369:1–15. doi: 10.1007/978-3-642-27340-7_1. [DOI] [PubMed] [Google Scholar]
- Sofia M.J., Bao D., Chang W., Du J., Nagarathnam D., Rachakonda S., Reddy P.G., Ross B.S., Wang P., Zhang H.R., Bansal S., Espiritu C., Keilman M., Lam A.M., Steuer H.M., Niu C., Otto M.J., Furman P.A. Discovery of a beta-d-2'-deoxy-2'-alpha-fluoro-2'-beta-C-methyluridine nucleotide prodrug (PSI-7977) for the treatment of hepatitis C virus. J. Med. Chem. 2010;53:7202–7218. doi: 10.1021/jm100863x. [DOI] [PubMed] [Google Scholar]
- Soumana D.I., Kurt Yilmaz N., Ali A., Prachanronarong K.L., Schiffer C.A. Molecular and dynamic mechanism underlying drug resistance in genotype 3 hepatitis C NS3/4A protease. J. Am. Chem. Soc. 2016;138:11850–11859. doi: 10.1021/jacs.6b06454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sperl J., Horvath G., Halota W., Ruiz-Tapiador J.A., Streinu-Cercel A., Jancoriene L., Werling K., Kileng H., Koklu S., Gerstoft J., Urbanek P., Flisiak R., Leiva R., Kazenaite E., Prinzing R., Patel S., Qiu J., Asante-Appiah E., Wahl J., Nguyen B.Y., Barr E., Platt H.L. Efficacy and safety of elbasvir/grazoprevir and sofosbuvir/pegylated interferon/ribavirin: a phase III randomized controlled trial. J. Hepatol. 2016;65:1112–1119. doi: 10.1016/j.jhep.2016.07.050. [DOI] [PubMed] [Google Scholar]
- Sterling R.K., Kuo A., Rustgi V.K., Sulkowski M.S., Stewart T.G., Fenkel J.M., El-Genaidi H., Mah'moud M.A., Abraham G.M., Stewart P.W., Akushevich L., Nelson D.R., Fried M.W., Di Bisceglie A.M. Virological outcomes and treatment algorithms utilisation in observational study of patients with chronic hepatitis C treated with boceprevir or telaprevir. Aliment. Pharmacol. Ther. 2015;41:671–685. doi: 10.1111/apt.13095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sulkowski M.S., Gardiner D.F., Rodriguez-Torres M., Reddy K.R., Hassanein T., Jacobson I., Lawitz E., Lok A.S., Hinestrosa F., Thuluvath P.J., Schwartz H., Nelson D.R., Everson G.T., Eley T., Wind-Rotolo M., Huang S.P., Gao M., Hernandez D., McPhee F., Sherman D., Hindes R., Symonds W., Pasquinelli C., Grasela D.M., AI444040 Study Group Daclatasvir plus sofosbuvir for previously treated or untreated chronic HCV infection. N. Engl. J. Med. 2014;370:211–221. doi: 10.1056/NEJMoa1306218. [DOI] [PubMed] [Google Scholar]
- Sulkowski M.S., Kang M., Matining R., Wyles D., Johnson V.A., Morse G.D., Amorosa V., Bhattacharya D., Coughlin K., Wong-Staal F., Glesby M.J., AIDS Clinical Trials Group A5277 Protocol Team Safety and antiviral activity of the HCV entry inhibitor ITX5061 in treatment-naive HCV-infected adults: a randomized, double-blind, phase 1b study. J. Infect. Dis. 2014;209:658–667. doi: 10.1093/infdis/jit503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sulkowski M., Hezode C., Gerstoft J., Vierling J.M., Mallolas J., Pol S., Kugelmas M., Murillo A., Weis N., Nahass R., Shibolet O., Serfaty L., Bourliere M., DeJesus E., Zuckerman E., Dutko F., Shaughnessy M., Hwang P., Howe A.Y., Wahl J., Robertson M., Barr E., Haber B. Efficacy and safety of 8 weeks versus 12 weeks of treatment with grazoprevir (MK-5172) and elbasvir (MK-8742) with or without ribavirin in patients with hepatitis C virus genotype 1 mono-infection and HIV/hepatitis C virus co-infection (C-WORTHY): a randomised, open-label phase 2 trial. Lancet. 2015;385:1087–1097. doi: 10.1016/S0140-6736(14)61793-1. [DOI] [PubMed] [Google Scholar]
- Sulkowski M.S., Vargas H.E., Di Bisceglie A.M., Kuo A., Reddy K.R., Lim J.K., Morelli G., Darling J.M., Feld J.J., Brown R.S., Frazier L.M., Stewart T.G., Fried M.W., Nelson D.R., Jacobson I.M., HCV-TARGET Study Group Effectiveness of simeprevir plus sofosbuvir, with or without ribavirin, in real-world patients with HCV genotype 1 infection. Gastroenterology. 2016;150:419–429. doi: 10.1053/j.gastro.2015.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun J.H., O'Boyle D.R., 2nd, Fridell R.A., Langley D.R., Wang C., Roberts S.B., Nower P., Johnson B.M., Moulin F., Nophsker M.J., Wang Y.K., Liu M., Rigat K., Tu Y., Hewawasam P., Kadow J., Meanwell N.A., Cockett M., Lemm J.A., Kramer M., Belema M., Gao M. Resensitizing daclatasvir-resistant hepatitis C variants by allosteric modulation of NS5A. Nature. 2015;527:245–248. doi: 10.1038/nature15711. [DOI] [PubMed] [Google Scholar]
- Sun L.Q., Mull E., Zheng B., D'Andrea S., Zhao Q., Wang A.X., Sin N., Venables B.L., Sit S.Y., Chen Y., Chen J., Cocuzza A., Bilder D.M., Mathur A., Rampulla R., Chen B.C., Palani T., Ganesan S., Arunachalam P.N., Falk P., Levine S., Chen C., Friborg J., Yu F., Hernandez D., Sheaffer A.K., Knipe J.O., Han Y.H., Schartman R., Donoso M., Mosure K., Sinz M.W., Zvyaga T., Rajamani R., Kish K., Tredup J., Klei H.E., Gao Q., Ng A., Mueller L., Grasela D.M., Adams S., Loy J., Levesque P.C., Sun H., Shi H., Sun L., Warner W., Li D., Zhu J. Discovery of a potent acyclic, tripeptidic, acyl sulfonamide inhibitor of hepatitis C virus NS3 protease as a back-up to asunaprevir with the potential for once-daily dosing. J. Med. Chem. 2016;59:8042–8060. doi: 10.1021/acs.jmedchem.6b00821. [DOI] [PubMed] [Google Scholar]
- Syder A.J., Lee H., Zeisel M.B., Grove J., Soulier E., Macdonald J., Chow S., Chang J., Baumert T.F., McKeating J.A., McKelvy J., Wong-Staal F. Small molecule scavenger receptor BI antagonists are potent HCV entry inhibitors. J. Hepatol. 2011;54:48–55. doi: 10.1016/j.jhep.2010.06.024. [DOI] [PubMed] [Google Scholar]
- Terrault N.A., Zeuzem S., Di Bisceglie A.M., Lim J.K., Pockros P.J., Frazier L.M., Kuo A., Lok A.S., Shiffman M.L., Ben Ari Z., Akushevich L., Vainorius M., Sulkowski M.S., Fried M.W., Nelson D.R., HCV-TARGET Study Group Effectiveness of ledipasvir-sofosbuvir combination in patients with hepatitis C virus infection and factors associated of sustained virologic response. Gastroenterology. 2016;151:1131–1140. doi: 10.1053/j.gastro.2016.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The ANRS collaborative study group on hepatocellular carcinoma Lack of evidence of an effect of direct-acting antivirals on the recurrence of hepatocellular carcinoma: data from three ANRS cohorts. J. Hepatol. 2016;65:734–740. doi: 10.1016/j.jhep.2016.05.045. [DOI] [PubMed] [Google Scholar]
- Thrift A.P., El-Serag H.B., Kanwal F. Global epidemiology and burden of HCV infection and HCV-related disease. Nat. Rev. Gastroenterol. Hepatol. 2017;14:122–132. doi: 10.1038/nrgastro.2016.176. [DOI] [PubMed] [Google Scholar]
- Tong X., Le Pogam S., Li L., Haines K., Piso K., Baronas V., Yan J.M., So S.S., Klumpp K., Najera I. In vivo emergence of a novel mutant L159F/L320F in the NS5B polymerase confers low-level resistance to the HCV polymerase inhibitors mericitabine and sofosbuvir. J. Infect. Dis. 2014;209:668–675. doi: 10.1093/infdis/jit562. [DOI] [PubMed] [Google Scholar]
- Toyota J., Karino Y., Suzuki F., Ikeda F., Ido A., Tanaka K., Takaguchi K., Naganuma A., Tomita E., Chayama K., Fujiyama S., Inada Y., Yoshiji H., Watanabe H., Ishikawa H., Hu W., McPhee F., Linaberry M., Yin P.D., Swenson E.S., Kumada H. Daclatasvir/asunaprevir/beclabuvir fixed-dose combination in Japanese patients with HCV genotype 1 infection. J. Gastroenterol. 2016;52:385–395. doi: 10.1007/s00535-016-1245-6. [DOI] [PubMed] [Google Scholar]
- Vausselin T., Seron K., Lavie M., Mesalam A.A., Lemasson M., Belouzard S., Feneant L., Danneels A., Rouille Y., Cocquerel L., Foquet L., Rosenberg A.R., Wychowski C., Meuleman P., Melnyk P., Dubuisson J. Identification of a new benzimidazole derivative as an antiviral against hepatitis C virus. J. Virol. 2016;90:8422–8434. doi: 10.1128/JVI.00404-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vierling J.M., Davis M., Flamm S., Gordon S.C., Lawitz E., Yoshida E.M., Galati J., Luketic V., McCone J., Jacobson I., Marcellin P., Muir A.J., Poordad F., Pedicone L.D., Albrecht J., Brass C., Howe A.Y., Colvard L.Y., Helmond F.A., Deng W., Treitel M., Wahl J., Bronowicki J.P. Boceprevir for chronic HCV genotype 1 infection in patients with prior treatment failure to peginterferon/ribavirin, including prior null response. J. Hepatol. 2014;60:748–756. doi: 10.1016/j.jhep.2013.12.013. [DOI] [PubMed] [Google Scholar]
- Vince B., Hill J.M., Lawitz E.J., O'Riordan W., Webster L.R., Gruener D.M., Mofsen R.S., Murillo A., Donovan E., Chen J., McCarville J.F., Sullivan-Bolyai J.Z., Mayers D., Zhou X.J. A randomized, double-blind, multiple-dose study of the pan-genotypic NS5A inhibitor samatasvir in patients infected with hepatitis C virus genotype 1, 2, 3 or 4. J. Hepatol. 2014;60:920–927. doi: 10.1016/j.jhep.2014.01.003. [DOI] [PubMed] [Google Scholar]
- Wagner F., Thompson R., Kantaridis C., Simpson P., Troke P.J., Jagannatha S., Neelakantan S., Purohit V.S., Hammond J.L. Antiviral activity of the hepatitis C virus polymerase inhibitor filibuvir in genotype 1-infected patients. Hepatology. 2011;54:50–59. doi: 10.1002/hep.24342. [DOI] [PubMed] [Google Scholar]
- Walker J., Crosby R., Wang A., Woldu E., Vamathevan J., Voitenleitner C., You S., Remlinger K., Duan M., Kazmierski W., Hamatake R. Preclinical characterization of GSK2336805, a novel inhibitor of hepatitis C virus replication that selects for resistance in NS5A. Antimicrob. Agents Chemother. 2014;58:38–47. doi: 10.1128/AAC.01363-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang N.Y., Xu Y., Zuo W.Q., Xiao K.J., Liu L., Zeng X.X., You X.Y., Zhang L.D., Gao C., Liu Z.H., Ye T.H., Xia Y., Xiong Y., Song X.J., Lei Q., Peng C.T., Tang H., Yang S.Y., Wei Y.Q., Yu L.T. Discovery of imidazo[2,1-b]thiazole HCV NS4B inhibitors exhibiting synergistic effect with other direct-acting antiviral agents. J. Med. Chem. 2015;58:2764–2778. doi: 10.1021/jm501934n. [DOI] [PubMed] [Google Scholar]
- Wang H., Cui W., Guo C., Chen B.Z., Ji M. Molecular modeling study on the drug resistance mechanism of NS5B polymerase to TMC647055. Biochem. Cell Biol. 2016;94:147–158. doi: 10.1139/bcb-2015-0109. [DOI] [PubMed] [Google Scholar]
- Webster D.P., Klenerman P., Collier J., Jeffery K.J. Development of novel treatments for hepatitis C. Lancet Infect. Dis. 2009;9:108–117. doi: 10.1016/S1473-3099(09)70020-9. [DOI] [PubMed] [Google Scholar]
- Wedemeyer H., Jensen D., Herring R., Jr., Ferenci P., Ma M.M., Zeuzem S., Rodriguez-Torres M., Bzowej N., Pockros P., Vierling J., Ipe D., Munson M.L., Chen Y.C., Najera I., Thommes J., PROPEL Investigators PROPEL: a randomized trial of mericitabine plus peginterferon alpha-2a/ribavirin therapy in treatment-naive HCV genotype 1/4 patients. Hepatology. 2013;58:524–537. doi: 10.1002/hep.26274. [DOI] [PubMed] [Google Scholar]
- Wei L., Han T., Yang D., Heo J., Shang J., Cheng J., Chen X., Xie Q., Kim J.H., Kalmeijer R., Ouwerkerk-Mahadevan S., Hoeben E., Lenz O., Verbinnen T., Sinha R., Li M., Scott J., Peeters M., Witek J., Tiger team Simeprevir plus peginterferon/ribavirin for HCV genotype 1-infected treatment-naive patients in China and South Korea. J. Gastroenterol. Hepatol. 2016;31:912–920. doi: 10.1111/jgh.13288. [DOI] [PubMed] [Google Scholar]
- Welzel T.M., Dultz G., Zeuzem S. Interferon-free antiviral combination therapies without nucleosidic polymerase inhibitors. J. Hepatol. 2014;61:S98–S107. doi: 10.1016/j.jhep.2014.08.014. [DOI] [PubMed] [Google Scholar]
- Welzel T.M., Nelson D.R., Morelli G., Di Bisceglie A., Reddy R.K., Kuo A., Lim J.K., Darling J., Pockros P., Galati J.S., Frazier L.M., Alqahtani S., Sulkowski M.S., Vainorius M., Akushevich L., Fried M.W., Zeuzem S., HCV-TARGET Study Group Effectiveness and safety of sofosbuvir plus ribavirin for the treatment of HCV genotype 2 infection: results of the real-world, clinical practice HCV-TARGET study. Gut. 2016 doi: 10.1136/gutjnl-2016–311609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welzel T.M., Petersen J., Herzer K., Ferenci P., Gschwantler M., Wedemeyer H., Berg T., Spengler U., Weiland O., van der Valk M., Rockstroh J., Peck-Radosavljevic M., Zhao Y., Jimenez-Exposito M.J., Zeuzem S. Daclatasvir plus sofosbuvir, with or without ribavirin, achieved high sustained virological response rates in patients with HCV infection and advanced liver disease in a real-world cohort. Gut. 2016 doi: 10.1136/gutjnl-2016–312444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilder J.M., Jeffers L.J., Ravendhran N., Shiffman M.L., Poulos J., Sulkowski M.S., Gitlin N., Workowski K., Zhu Y., Yang J.C., Pang P.S., McHutchison J.G., Muir A.J., Howell C., Kowdley K., Afdhal N., Reddy K.R. Safety and efficacy of ledipasvir-sofosbuvir in black patients with hepatitis C virus infection: a retrospective analysis of phase 3 data. Hepatology. 2016;63:437–444. doi: 10.1002/hep.28334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilfret D.A., Walker J., Adkison K.K., Jones L.A., Lou Y., Gan J., Castellino S., Moseley C.L., Horton J., de Serres M., Culp A., Goljer I., Spreen W. Safety, tolerability, pharmacokinetics, and antiviral activity of GSK2336805, an inhibitor of hepatitis C virus (HCV) NS5A, in healthy subjects and subjects chronically infected with HCV genotype 1. Antimicrob. Agents Chemother. 2013;57:5037–5044. doi: 10.1128/AAC.00910-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson E.M., Kattakuzhy S., Sidharthan S., Sims Z., Tang L., McLaughlin M., Price A., Nelson A., Silk R., Gross C., Akoth E., Mo H., Subramanian G.M., Pang P.S., McHutchison J.G., Osinusi A., Masur H., Kohli A., Kottilil S. Successful retreatment of chronic HCV Genotype-1 infection with ledipasvir and sofosbuvir after initial short course therapy with direct-acting antiviral regimens. Clin. Infect. Dis. 2016;62:280–288. doi: 10.1093/cid/civ874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong K.A., Xu S., Martin R., Miller M.D., Mo H. Tegobuvir (GS-9190) potency against HCV chimeric replicons derived from consensus NS5B sequences from genotypes 2b, 3a, 4a, 5a, and 6a. Virology. 2012;429:57–62. doi: 10.1016/j.virol.2012.03.025. [DOI] [PubMed] [Google Scholar]
- Wyles D.L., Rodriguez-Torres M., Lawitz E., Shiffman M.L., Pol S., Herring R.W., Massetto B., Kanwar B., Trenkle J.D., Pang P.S., Zhu Y., Mo H., Brainard D.M., Subramanian G.M., McHutchison J.G., Habersetzer F., Sulkowski M.S. All-oral combination of ledipasvir, vedroprevir, tegobuvir, and ribavirin in treatment-naive patients with genotype 1 HCV infection. Hepatology. 2014;60:56–64. doi: 10.1002/hep.27053. [DOI] [PubMed] [Google Scholar]
- Wyles D., Pockros P., Morelli G., Younes Z., Svarovskaia E., Yang J.C., Pang P.S., Zhu Y., McHutchison J.G., Flamm S., Lawitz E. Ledipasvir-sofosbuvir plus ribavirin for patients with genotype 1 hepatitis C virus previously treated in clinical trials of sofosbuvir regimens. Hepatology. 2015;61:1793–1797. doi: 10.1002/hep.27814. [DOI] [PubMed] [Google Scholar]
- Yang H., Robinson M., Corsa A.C., Peng B., Cheng G., Tian Y., Wang Y., Pakdaman R., Shen M., Qi X., Mo H., Tay C., Krawczyk S., Sheng X.C., Kim C.U., Yang C., Delaney W.E., IV Preclinical characterization of the novel hepatitis C virus NS3 protease inhibitor GS-9451. Antimicrob. Agents Chemother. 2014;58:647–653. doi: 10.1128/AAC.00487-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang S., K RJ Lim S., Choi T.G., Kim J.H., Akter S., Jang M., Ahn H.J., Kim H.Y., Windisch M.P., Khadka D.B., Zhao C., Jin Y., Kang I., Ha J., Oh B.C., Kim M., Kim S.S., Cho W.J. Structure-based discovery of novel cyclophilin a inhibitors for the treatment of hepatitis C virus infections. J. Med. Chem. 2015;58:9546–9561. doi: 10.1021/acs.jmedchem.5b01064. [DOI] [PubMed] [Google Scholar]
- Yi G., Deval J., Fan B., Cai H., Soulard C., Ranjith-Kumar C.T., Smith D.B., Blatt L., Beigelman L., Kao C.C. Biochemical study of the comparative inhibition of hepatitis C virus RNA polymerase by VX-222 and filibuvir. Antimicrob. Agents Chemother. 2012;56:830–837. doi: 10.1128/AAC.05438-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Younossi Z.M., Park H., Gordon S.C., Ferguson J.R., Ahmed A., Dieterich D., Saab S. Real-world outcomes of ledipasvir/sofosbuvir in treatment-naive patients with hepatitis C. Am. J. Manag. Care. 2016;22:SP205–211. [PubMed] [Google Scholar]
- Zeuzem S., Soriano V., Asselah T., Bronowicki J.P., Lohse A.W., Mullhaupt B., Schuchmann M., Bourliere M., Buti M., Roberts S.K., Gane E.J., Stern J.O., Vinisko R., Kukolj G., Gallivan J.P., Bocher W.O., Mensa F.J. Faldaprevir and deleobuvir for HCV genotype 1 infection. N. Engl. J. Med. 2013;369:630–639. doi: 10.1056/NEJMoa1213557. [DOI] [PubMed] [Google Scholar]
- Zeuzem S., Dusheiko G.M., Salupere R., Mangia A., Flisiak R., Hyland R.H., Illeperuma A., Svarovskaia E., Brainard D.M., Symonds W.T., Subramanian G.M., McHutchison J.G., Weiland O., Reesink H.W., Ferenci P., Hezode C., Esteban R., Valence Investigators Sofosbuvir and ribavirin in HCV genotypes 2 and 3. N. Engl. J. Med. 2014;370:1993–2001. doi: 10.1056/NEJMoa1316145. [DOI] [PubMed] [Google Scholar]
- Zeuzem S., Berg T., Gane E., Ferenci P., Foster G.R., Fried M.W., Hezode C., Hirschfield G.M., Jacobson I., Nikitin I., Pockros P.J., Poordad F., Scott J., Lenz O., Peeters M., Sekar V., De Smedt G., Sinha R., Beumont-Mauviel M. Simeprevir increases rate of sustained virologic response among treatment-experienced patients with HCV genotype-1 infection: a phase IIb trial. Gastroenterology. 2014;146:430–441. doi: 10.1053/j.gastro.2013.10.058. e436. [DOI] [PubMed] [Google Scholar]
- Zeuzem S., Jacobson I.M., Baykal T., Marinho R.T., Poordad F., Bourliere M., Sulkowski M.S., Wedemeyer H., Tam E., Desmond P., Jensen D.M., Di Bisceglie A.M., Varunok P., Hassanein T., Xiong J., Pilot-Matias T., DaSilva-Tillmann B., Larsen L., Podsadecki T., Bernstein B. Retreatment of HCV with ABT-450/r-ombitasvir and dasabuvir with ribavirin. N. Engl. J. Med. 2014;370:1604–1614. doi: 10.1056/NEJMoa1401561. [DOI] [PubMed] [Google Scholar]
- Zeuzem S., Ghalib R., Reddy K.R., Pockros P.J., Ben Ari Z., Zhao Y., Brown D.D., Wan S., DiNubile M.J., Nguyen B.Y., Robertson M.N., Wahl J., Barr E., Butterton J.R. Grazoprevir-elbasvir combination therapy for treatment-naive cirrhotic and noncirrhotic patients with chronic hepatitis C virus genotype 1, 4, or 6 infection: a randomized trial. Ann. Intern Med. 2015;163:1–13. doi: 10.7326/M15-0785. [DOI] [PubMed] [Google Scholar]
- Zeuzem S., Soriano V., Asselah T., Gane E.J., Bronowicki J.P., Angus P., Lohse A.W., Stickel F., Mullhaupt B., Roberts S., Schuchmann M., Manns M., Bourliere M., Buti M., Stern J.O., Gallivan J.P., Voss F., Sabo J.P., Bocher W., Mensa F.J., SOUND-C2 Study Group Efficacy and safety of faldaprevir, deleobuvir, and ribavirin in treatment-naive patients with chronic hepatitis C virus infection and advanced liver fibrosis or cirrhosis. Antimicrob. Agents Chemother. 2015;59:1282–1291. doi: 10.1128/AAC.04383-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeuzem S., Mizokami M., Pianko S., Mangia A., Han K.H., Martin R., Svarovskaia E., Dvory-Sobol H., Doehle B., Hedskog C., Yun C., Brainard D.M., Knox S., McHutchison J.G., Miller M.D., Mo H., Chuang W.L., Jacobson I., Dore G.J., Sulkowski M. NS5A resistance-associated substitutions in patients with genotype 1 hepatitis C virus: prevalence and effect on treatment outcome. J. Hepatol. 2017 doi: 10.1016/j.jhep.2017.01.007. [DOI] [PubMed] [Google Scholar]
- Zhang N., Zhang X., Zhu J., Turpoff A., Chen G., Morrill C., Huang S., Lennox W., Kakarla R., Liu R., Li C., Ren H., Almstead N., Venkatraman S., Njoroge F.G., Gu Z., Clausen V., Graci J., Jung S.P., Zheng Y., Colacino J.M., Lahser F., Sheedy J., Mollin A., Weetall M., Nomeir A., Karp G.M. Structure-activity relationship (SAR) optimization of 6-(indol-2-yl)pyridine-3-sulfonamides: identification of potent, selective, and orally bioavailable small molecules targeting hepatitis C (HCV) NS4B. J. Med. Chem. 2014;57:2121–2135. doi: 10.1021/jm401621g. [DOI] [PubMed] [Google Scholar]
- Zhong M., Peng E., Huang N., Huang Q., Huq A., Lau M., Colonno R., Li L. Discovery of ravidasvir (PPI-668) as a potent pan-genotypic HCV NS5A inhibitor. Bioorg. Med. Chem. Lett. 2016;26:4508–4512. doi: 10.1016/j.bmcl.2016.07.066. [DOI] [PubMed] [Google Scholar]
- Zhou L., Zhang H.W., Tao S., Bassit L., Whitaker T., McBrayer T.R., Ehteshami M., Amiralaei S., Pradere U., Cho J.H., Amblard F., Bobeck D., Detorio M., Coats S.J., Schinazi R.F. beta-D-2'-C-Methyl-2,6-diaminopurine ribonucleoside phosphoramidates are potent and selective inhibitors of hepatitis C virus (HCV) and are bioconverted intracellularly to bioactive 2,6-diaminopurine and guanosine 5'-triphosphate forms. J. Med. Chem. 2015;58:3445–3458. doi: 10.1021/jm501874e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu H., Wong-Staal F., Lee H., Syder A., McKelvy J., Schooley R.T., Wyles D.L. Evaluation of ITX 5061, a scavenger receptor B1 antagonist: resistance selection and activity in combination with other hepatitis C virus antivirals. J. Infect. Dis. 2012;205:656–662. doi: 10.1093/infdis/jir802. [DOI] [PMC free article] [PubMed] [Google Scholar]