Abstract
Coronavirus Disease 2019 (COVID-19) is spreading rapidly around the world with devastating consequences on patients, health care workers, health systems, and economies. As it reaches low- and middle-income countries, its effects could be even more dire, because it will be difficult for them to respond aggressively to the pandemic. There is a great shortage of all health care providers, who will be at risk due to a lack of personal protection equipment. Social distancing will be almost impossible. The necessary resources to treat patients will be in short supply. The end result could be a catastrophic loss of life. A global effort will be required to support faltering economies and health care systems.
Things fall apart; the centre cannot hold;
Mere anarchy is loosed upon the world.
—William Butler Yeats, The Second Coming
As news of a novel viral illness in China emerged in January 20201 and until the day when the Director General of the World Health Organization (WHO) declared a pandemic,2 those who live and work in low- and middle-income countries (LMICs) held their collective breath. As the single red dot on the world map morphed into red dots in almost every country in the world, the enormity of the problems facing all countries, but especially those with serious economic and health resource challenges, became evident. In this special article, we outline what those problems might be and possible ways to address them.
BACKGROUND
The new coronavirus, officially named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), probably emerged in November 2019 and first caused cases of pneumonia of unknown origin in Wuhan, China. The spectrum of illness caused by SARS-CoV-2 is now called Coronavirus Disease 2019 (COVID-19). Initially thought to be transmitted from an animal or bird source to humans, it is now clear that there is efficient and thus widespread human-to-human transmission via airborne droplets. Despite a massive effort to contain the virus within China, it has disseminated throughout the world. As of March 23, 2020, there have been 334,981 confirmed cases, in 189 countries, with 14,652 deaths.3
The clinical spectrum of the disease is quite variable, ranging from undiagnosed asymptomatic infection through mild upper respiratory infection to severe viral pneumonia leading to respiratory failure and death.4 The incidence of respiratory failure in Wuhan was 54% overall; of those patients who died, 98% had respiratory failure compared to 36% of those who survived. All of those who succumbed had sepsis, and 93% had acute respiratory distress syndrome (ARDS), while 42% of survivors had sepsis and 7% had ARDS.4 Also noted in this Wuhan cohort was a 48% prevalence of comorbidities in those who died, most commonly hypertension, diabetes mellitus, and coronary artery disease. Increasing age was also associated with increased risk of death. Overall, in-hospital mortality rate was 28%, and for those requiring mechanical ventilation, it was 97%.
WHAT HAVE WE LEARNED ABOUT COVID-19 SINCE WUHAN?
The disease has spread rapidly throughout the world.3 Existing antiviral medications seem to be ineffective.5 The number of deaths from COVID-19 is staggering. Italy, which has become another major epicenter of the outbreak, is reporting, as of March 21,2020, a total of 48,452 cases with 3770 associated deaths.6 Countries have closed their borders, enforced strict social isolation and quarantine procedures, and increased testing for the virus. Travel has almost ceased worldwide. Businesses have closed, and economies are almost collapsing. Yet it seems the virus continues to spread, and health care systems are being overwhelmed.7 Why are some countries responding better than others?
China put in place extraordinary measures, including tracing and testing of COVID-19 contacts, and major quarantine restrictions, which included a complete lockdown that prevented all travel and commerce in and out of the Wuhan region.8 Normal life was basically suspended.
In contrast, Singapore seems to have done better with a much less severe approach.9 Singapore applied a comprehensive surveillance strategy early on in the outbreak, with rigorous tracing of all case contacts followed by rapid quarantining. It used widespread testing so a patient with any suspicion of COVID-19 could be rapidly tested. Strict infection control practices were instituted at health care facilities, and health care workers were provided with adequate personal protective equipment (PPE). Communication of information to the population was clear and transparent. Request for the public to exercise social responsibility in containing the spread of the virus was met with compliance. With these measures, Singapore has been relatively successful in managing the outbreak; however, new cases are beginning to occur, likely from travelers returning home. As a result, Singapore has now adopted more stringent measures on social distancing. In efforts to continue tracing COVID-19 contacts, the Government of Singapore has developed a contact tracing app, “Trace Together,” that works by Bluetooth technology.10 Singapore will make this freely available globally.
Italy, on the other hand, has been ravaged by this disease.6,11 The mean age of those who have died has been 81 years, and more than two-thirds of these individuals were past smokers or had chronic disease such as diabetes mellitus, cardiovascular disease, or cancer. In spite of widespread aggressive measures imposed by the Italian government, the incidence and death rate continue to rise. It is clear that, even in countries with strong economies and sturdy health care systems, there can be variable responses and case fatality rates with the outbreak.
WHAT ARE THE PROBABLE SCENARIOS FOR COVID-19 AND ITS IMPACT ON LESS ADVANTAGED REGIONS OF THE WORLD?
At this point, it seems that the SARS-CoV-2 has spread to almost every country in the world.3 Even though many LMICs have closed their borders to prevent travel-related dissemination, it is merely a matter of time before community-level spread becomes the norm.12 LMICs frequently have large populations living in overcrowded conditions where “social distancing” is impossible to maintain, where clean water is rarely available in every household, and where supplies of hand sanitizer are impossible to find. Thus people living in LMICs will generally be unable to follow the usual public health advice on how to reduce thespread of virus and infection. Mr Cyril Ramaphosa, President of the Republic of South Africa, accurately described the pandemic as a “national disaster.”13 One infected case in South Korea was determined to have been responsible for 3900 secondary cases.14 With such rapid, exponential spread, the situation in LMICs, refugee camps, and war-torn regions will be catastrophic.
Health care facilities in LMICs will be overwhelmed by patients with COVID-19. They are already overcrowded with those suffering from pneumonia, human immunodeficiency virus (HIV), tuberculosis (TB), and malaria, and patients in need of surgical treatment. COVID-19 testing will be useful in confirming that patients have a viral illness and therefore do not require precious antibiotics. Hospital beds will be in short supply, but unlike well-off, high-income countries (HICs), poorer countries will be unable to significantly reduce their surgical volumes to make room for COVID-19 patients. This is because the largest segment of surgical volume in LMICs is emergent and urgent surgeries that cannot be safely postponed.15 Moreover, a large percentage of these cases are patients undergoing cesareandeliveries.15,16 If cesarean deliveries are delayed or cancelled, there is a likely risk of worsening already high maternal and neonatal mortality rates. Another major challenge will be the shortage of intensive care beds.17 Even if they were abundant, there is a significant shortage of resources such as oxygen, ventilators, infusion pumps, and all of the other necessities for taking care of patients with severe respiratory failure.18 Even water and electricity supplies cannot be relied on in LMICs.
That brings us to the most overwhelming shortage of all―namely, health care personnel, including physicians―especially, anesthesiologists, who are on the front lines of any pandemic like COVID-19.19 In many LMICs, anesthesiologists take care of patients in intensive care units (ICUs). They will be called on to intubate sick patients in emergency departments and in the operating rooms, as will nonphysician anesthesia providers. These health care workers will be at extremely high risk for infection, as intubation is considered one of the highest-risk procedures when dealing with COVID-19 patients.20
Lessons learned from the SARS epidemic in 2003 included the importance of full personal protection when performing high-risk procedures.21 This is already also clear from the current COVID-19 pandemic, as there have been deaths of many health care professionals in both China and Italy.22,23 Adequate PPE is mandated in all available guidelines for managing COVID-19 patients.20 PPE is in enormous demand around the world, and procurement will thus prove especially difficult in LMICs. The prospect of losing any of our already scarce colleagues to this disease is terrifying. Just as the world was waking up to the necessity of having safe anesthesia and surgery as part of universal health care,24,25 all of the efforts may be sidelined or derailed by an enemy <1 μm in diameter.
WHAT SHOULD THE WORLD BE DOING TO HELP?
Financial Aid
In the midst of their own crisis, well-resourced governments and organizations should remember the needs of those less well-off. Economies will be devastated all over the world. This is the time to consider debt erasure for countries most in need. The International Monetary Fund has committed US$10 billion in interest-free loans to low-income countries.26 The United Nations has released emergency funds to assist vulnerable countries in the fight.27 Much more will be needed now and in the foreseeable future.
The World Economic Forum has launched a COVID Action Platform to pull together a public–private partnership to support action on the pandemic.28 It is likely that a fund similar to the Global Fund for HIV/acquired immune deficiency syndrome (AIDS), TB, and malaria will be needed to further support the development of medications and vaccines for COVID-19. A fund such as the US President’s Emergency Plan for Aids Relief (PEPFAR) will be required to provide medications and vaccines when they become available. PEPFAR is the largest commitment ever made by 1 government to address a single disease.
Practical Aid
Nongovernmental organizations (NGOs) that normally work in low-income countries also need to offer support and practical help. For example, the Lifebox Foundation, partnering with Smile Train and Gradian Health Care, has secured 1650 pulse oximeters for distribution to countries most in need (K. Torgeson, CEO Lifebox, personal communication, March 23, 2020). Since most of the complications of COVID-19 are respiratory, pulse oximeters will be essential in the management of patients. However, without reliable oxygen supplies, oximeters will not help. Massive efforts will be needed to improve oxygen availability. These will include not only a steady supply of oxygen tanks with a reliable delivery service but also provision of new oxygen concentrators and regular maintenance of those already available. Without oxygen, many lives will be unnecessarily lost. Doctors without Borders (Médecins Sans Frontières, MSF) is providing health education activities, distributing soap and PPE for health care workers, and reinforcing hygiene measures in all of its facilities.29 Will other NGOs stepup to help?
Clear Communication
Governments, departments of health, and medical professional organizations need to be providing clear and unequivocal information about COVID-19: how to prevent its spread, who needs to be tested for it, and how to manage it if one becomes infected.
One of the major problems for LMICs is communication. Radio, television, and newspapers are no longer the main methods of conveying information. Social media in all of its forms is much more likely to carry the message. WHO has recognized this and launched a messaging service in conjunction with WhatsApp and Facebook.30 People can access the service, ask questions, and get advice. Many journals, for example, The Lancet and The New England Journal of Medicine, are publishing all articles on COVID-19 with free access to everyone.31,32 The same is true for anesthesia journals like Anesthesia & Analgesia. Likewise, the Cochrane Library is available for unrestricted access for all, with special collections on infection control measures and evidence relevant to critical care.33 UpToDate (Wolters Kluwer, Waltham, MA) is also providing open access to clinical content on COVID-19.34
Advice on ManagingPatients
There are many advisories and guidelines available on the management of COVID-19 patients in the ICU and operating suite.35,36 Most of them apply to countries with significant resources and strong health care systems. They often include links to other useful sites for information. For example, Reference28 includes links to the WHO site, the US Centers for Disease Control and Prevention (CDC), and the Public Health Agency for Canada, all of which have very useful information available.
Most LMICs will have to adapt these resource documents to their needs and to the availability of equipment and resources at their centers. We are including 1 table and 2 figures that may be useful for those working in areas where resources are scarce. TheTable emphasizes the key points in managing patients. Figure 1 offers some low-cost suggestions for creating or extending PPE. Figure 2 offers recommendations on oxygen therapy. In addition, we are recommending applying a very useful system for those working in ICUs.37 This rubric is very practical and contains many educational materials filed under an A, B, C system. The African Federation for Emergency Medicine has also prepared a useful booklet for those working in LMICs.38
Figure 1.

Low-cost solutions to create or extend the use of PPEs. Details, photos, and links can be found on https://aspa-2000.com/2020/03/27/low-cost-suggestions-to-creating-or-extending-ppe/. DIY indicates do it yourself; PPE, personal protective equipment.
Figure 2.
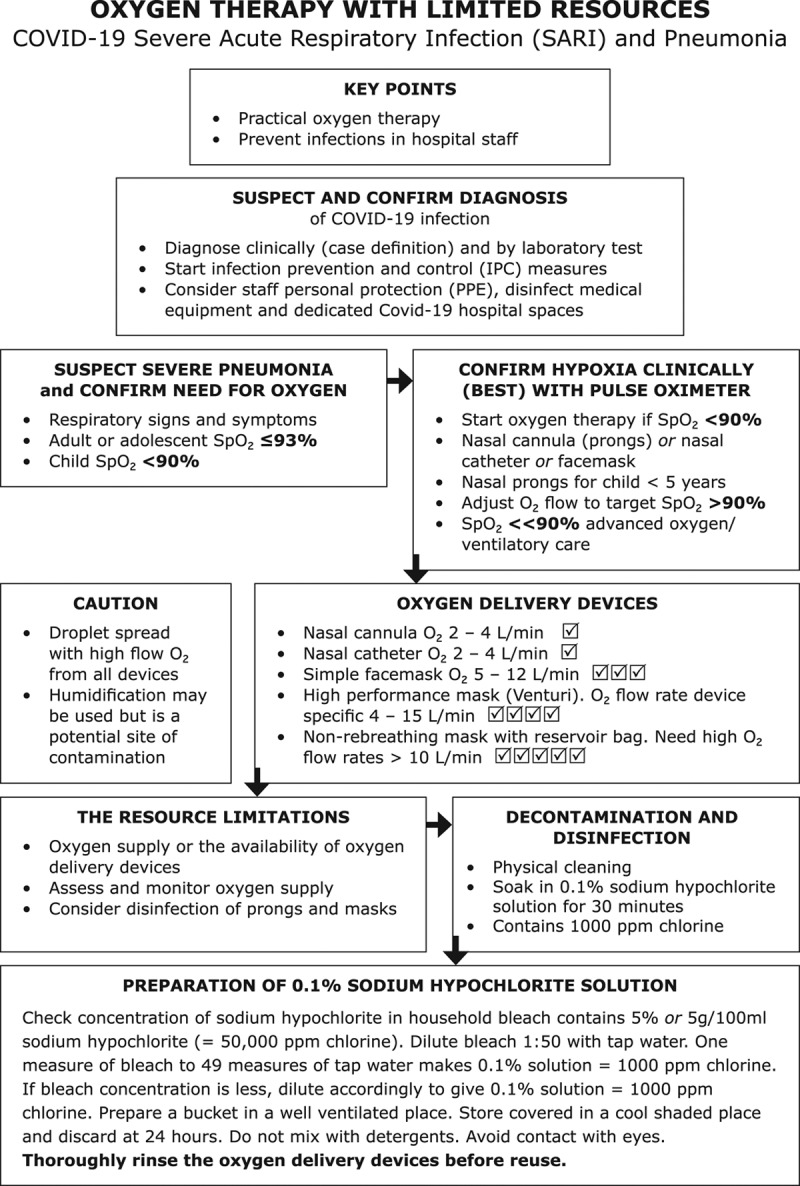
Provided courtesy of Dr Haydn Perndt, AM, FFARCS, FANZCA, MPH &TM, Clinical Associate Professor, School of Medicine, University of Tasmania, Australia. E-mail: haydn.perndt@utas.ed.au. COVID-19 indicates Coronavirus Disease 2019; Spo2, peripheral oxygen saturation.
Table.
Key Point Checklist
| 1. | Hand washing: soap and water; alcohol-based sanitizer |
| 2. | Dedicated triage and inpatient areas for COVID-19 patients |
| 3. | Personal protective equipment: practical, locally sourced |
| 4. | Therapeutic plan: locally devised, known to and agreed on by all staff |
| 5. | Oxygen: increased supplies, maintenance of existing sources |
Abbreviation: COVID-19, Coronavirus Disease 2019.
Treatment
Unfortunately, there are no medications demonstrated to successfully treat COVID-19. Work continues apace to find them. False claims may be made, which can result in fatal outcomes.39 In addition, normal medication supply chains may be severely affected by the worldwide shutdown of factories, leaving many patients unable to access their normal medication supplies.40
Current treatment is supportive. In many mild cases, people may convalesce at home. However, the severe cases are placing enormous strain on hospitals because of their growing numbers and the large percentage of patients who are requiring intensive care management. These severe cases are posing the greatest threat to health care workers in terms of cross-infection, and their resource needs will outstrip those available in many low-resource environments. There will be many ethical challenges to be faced. Guidance is available from several sources,41 and we suggest having clear agreement on the relevant issues as soon as possible. Each center will have to make its own decisions based on its currently available resources.
WHAT WILL BE THE LONG-TERM EFFECTS OF THE COVID-19 PANDEMIC ON FRAGILE HEALTH CARE SYSTEMS?
To answer this question, we can only rely on what has been learned from the Ebola epidemic of 2014–2016 in West Africa. According to a report of the United Nations Development Group (UNDG), at that time, the epidemic was “the longest, largest, deadliest and most complex” in history.42 COVID-19 is already orders of magnitude greater than this.
The US CDC estimates that there were just under 29,000 infected patients and just over 11,000 deaths during the Ebola epidemic of 2014–2016 in West Africa.43 Liberia lost 8% of its doctors, nurses, and midwives;Sierra Leone 7%;and Guinea 1%. The epidemic set back the management of all health care services and especially treatment and control of TB, HIV, and malaria. The number of women giving birth in health centers in Sierra Leone dropped by 30%; cesareandeliveryrate dropped by 60%.44 It is estimated that $2.2 billion was lost from the gross domestic product of the 3 countries. The United States, the United Kingdom, and Germany donated over US$3.5 billion in aid.43 The UNDG observed that “the global community is ill prepared for a devastating pandemic like Ebola, and the next pandemic should not take the world by surprise.”42 How correct this prediction has been.
Another lesson to be learned from the Ebola epidemic has to do with “health security.” This will not be a term familiar to most people, but it certainly will become so. Basically, health security means protection from threats to our health.45 With modern travel and globalization, an epidemic in West Africa or China, or anywhere else in the world, can easily become a threat in another location far away. Thus it is imperative that governments and supranational organizations like the WHO work together to reduce the risks everywhere. There are International Health Regulations that aim to stop the spread of infectious diseases.46 However, they need to be expanded and modernized to address the issues of our time. “Collective health security is the sum of individual health security, and compels global action to provide individuals in all countries with access to essential health care. This is indispensable for achievement of individual health security and, therefore, collective health and human security.”45
CONCLUSIONS
In the absence of specific, effective treatment and given a lack of resources in managing active COVID-19 patients,prevention and early containment of the disease appear to be the most feasible option for LMICs. As the global COVID-19 situation unfolds and countries are forced to take unprecedented drastic measure,including border closures, travel bans, and social distancing, we will likely witness the devastating and profound impact of this pandemic not only in health care but also on the world economy. This will further reduce resources available for health care, not just in managing COVID-19 patients, but also for those with many other major medical conditions. This will be particularly challenging for LMICs. The recent catastrophic clinical scenarios in many HICs, including Italy, Spain, France, the United States, and the United Kingdom, caused by a shortage of PPE, as well as other vital material and human resources, are a solemn reminder that many LMICs will be facing similar or likely much worse constraints and outcomes.
In the midst of all this doom and gloom, thousands of volunteers work tirelessly to ensure that food and medical supplies reach the millions of our fellow human beings in LMICs who need them. Increased connectivity allows rapid sharing of information and resources, all of which could help in “flattening the curve” in an attempt to avoid overwhelming individual health care systems. In the end, we must rely on the generosity of mankind and the resilience of the human spirit.
DISCLOSURES
Name: Choon-Looi Bong, MB ChB, FRCA.
Contribution: This author helped write and edit the manuscript.
Conflicts of Interest: None.
Name: Christopher Brasher, MB BS, FANZCA.
Contribution: This author helped write and edit the manuscript.
Conflicts of Interest: None.
Name: Edson Chikumba, MB ChB, MMed (Anaesthesia).
Contribution: This author helped write and edit the manuscript.
Conflicts of Interest: None.
Name: Robert McDougall, MB BS, FANZCA.
Contribution: This author helped write and edit the manuscript.
Conflicts of Interest: R. McDougall is Senior Editor, Global Health Section, Anesthesia & Analgesia.
Name: Jannicke Mellin-Olsen, MD, DPH.
Contribution: This author helped write and edit the manuscript.
Conflicts of Interest: J. Mellin-Olsen is President of the World Federation of Societies of Anaesthesiologists.
Name: Angela Enright, MB BCh BAO, FRCPC.
Contribution: This author helped write and edit the manuscript.
Conflicts of Interest: A. Enright is Executive Section Editor, Global Health, Anesthesia & Analgesia; Board Member of the Lifebox Foundation; former President of the World Federation of Societies of Anaesthesiologists.
This manuscript was handled by: Thomas R. Vetter, MD, MPH.
Footnotes
Funding: None.
Conflicts of Interest: See Disclosures at the end of the article.
Reprints will not be available from the authors.
REFERENCES
- 1.Shih G, Sun LH. Specter of possible new virus emerging from central China raises alarms across Asia. Available at: https://www.washingtonpost.com/world/asia_pacific/specter-of-possible-new-virus-emerging-from-central-china-raises-alarms-across-asia/2020/01/08/3d33046c-312f-11ea-971b-43bec3ff9860_story.html. Accessed March 20, 2020.
- 2.WHO Director-General’s opening remarks at the media briefing on COVID-19 on 11 March 2020. Available at: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. Accessed March 20, 2020.
- 3.Novel coronavirus (COVID-19) situation. Available at: https://experience.arcgis.com/experience/685d0ace521648f8a5beeeee1b9125cd. Accessed March 23, 2020.
- 4.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baden LR, Rubin EJ. COVID-19 – The search for effective therapy. N Engl J Med. 2020 March 18 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Integrated surveillance of COVID-19 in Italy. Available at: https://www.epicentro.iss.it/coronavirus/bollettino/Infografica_21marzo%20ENG.pdf. Accessed March 22, 2020.
- 7.Buchholz K.Upward trajectory or flattening the curve? This is how countries are faring with COVID-19 cases. Available at: https://www.weforum.org/agenda/2020/03/upward-trajectory-flattening-curve-how-countries-are-faring-coronavirus-covid-19/. Accessed March 22, 2020.
- 8.Fisher D, Wilder-Smith A. The global community needs to swiftly ramp up the response to contain COVID-19. Lancet. 2020 March 18 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee VJ, Chiew CJ, Khong WX. Interrupting transmission of COVID-19: lessons from containment efforts in Singapore. J Travel Med. 2020. March 13 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baharudin H.Software for Singapore contact tracing app to be free for global use. Available at: https://www.straitstimes.com/singapore/software-for-spore-contact-tracing-app-to-be-free-for-global-use. Accessed March 26, 2020.
- 11.Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020March12 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.WHO COVID -19 Situation Report 63. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200323-sitrep-63-covid-19.pdf?sfvrsn=d97cb6dd_2. Accessed March 23, 2020.
- 13.Nordling L. A ticking time bomb: scientists worry about coronavirus spread in Africa. Available at: https://www.sciencemag.org/news/2020/03/ticking-time-bomb-scientists-worry-about-coronavirus-spread-africa. Accessed March 23, 2020.
- 14.Shim E, Tariq A, Choi W, Lee Y, Chowell G. Transmission potential and severity of COVID-19 in South Korea. Int J Infect Dis. 2020 March 10 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Prin M, Guglielminotti J, Mtalimanja O, Li G, Charles A. Emergency-to-elective surgery ratio: a global indicator of access to surgical care. World J Surg. 2018;42:1971–1980. [DOI] [PubMed] [Google Scholar]
- 16.Kushner A, Groen RS, Kingham TP. Percentage of cesarean sections among total surgical procedures in sub-Saharan Africa: possible indicator of the overall adequacy of surgical care. World J Surg. 2020 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 17.Murthy S, Leligdowicz A, Adhikari NK. Intensive care unit capacity in low-income countries: a systematic review. PLoS One. 2015;10:e0116949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Malelelo-Ndou H, Ramathuba DU, Netshisaulu KG. Challenges experienced by health care professionals working in resource-poor intensive care settings in the Limpopo province of South Africa. Curationis. 2019;42:e1–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kempthorne P, Morriss WW, Mellin-Olsen J, Gore-Booth J. The WFSA Global Anesthesia Workforce Survey. Anesth Analg. 2017;125:981–990. [DOI] [PubMed] [Google Scholar]
- 20.COVID-19 airway recommendations during airway manipulation. Available at: https://www.cas.ca/en/practice-resources/news/cas-articles/2020/covid-19-recommendations-during-airway-manipulation. Accessed March 23, 2020.
- 21.Scales DC, Green K, Chan AK, et al. Illness in intensive care staff after brief exposure to severe acute respiratory syndrome. Emerg Infect Dis. 2003;9:1205–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Woodward A. Several young doctors in China have died of the coronavirus. Medical workers are far more vulnerable to infection than the general population. Business Insider. Available at: https://www.businessinsider.com/why-coronavirus-killed-young-chinese-doctors-2020-2. Accessed March 25, 2020. [Google Scholar]
- 23.Reguly E.Italian doctors tell stories of sorrow and hope. Globe and Mail. Available at: https://www.theglobeandmail.com/world/article-two-front-line-italian-covid-19-doctors-tell-their-stories-of-fatigue/. Accessed March 25, 2020.
- 24.Meara JG, Leather AJ, Hagander L, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386:569–624. [DOI] [PubMed] [Google Scholar]
- 25.World Health Organization. WHA68.15: Strengthening Emergency and Essential Surgical Care and Anaesthesia as a Component of Universal Health Coverage. 2015Geneva: WHO World Health Assembly; [DOI] [PubMed] [Google Scholar]
- 26.Moss K.Donor funding for the global novel coronavirus response. Available at: https://www.kff.org/global-health-policy/issue-brief/donor-funding-for-the-global-novel-coronavirus-response/. Accessed on March 24, 2020.
- 27.UN releases emergency funds to help vulnerable countries fight coronavirus COVID-19. Available at: https://news.un.org/en/story/2020/03/1058391. Accessed March 24, 2020.
- 28.World Economic Forum: COVID Action Platform. Available at: https://www.weforum.org/platforms/covid-action-platform. Accessed March 24, 2020.
- 29.COVID-19: what is MSF doing? Available at: https://www.doctorswithoutborders.ca/article/covid-19-what-msf-doing. Accessed March 24, 2020.
- 30.Lacina L. New health alert service launched with WhatsApp. Available at: https://www.weforum.org/agenda/2020/03/whatsapp-facebook-health-service-coronavirus-fridays-who-briefing/. Accessed March 24, 2020.
- 31.The Lancet: COVID-19 resource center. Available at: https://www.thelancet.com/coronavirus. Accessed March 24, 2020.
- 32.New England Journal of Medicine: Coronavirus (COVID-19). Available at: https://www.nejm.org/coronavirus?query=main_nav_lg. Accessed March 24, 2020.
- 33.Coronavirus (COVID-19) – Cochrane rsources and news. Available at: https://www.cochrane.org/coronavirus-covid-19-cochrane-resources-and-news. Accessed on March 26, 2020.
- 34.UpToDate® Clinical content available to all. Available at: https://www.uptodate.com/home/covid-19-access. Accessed March 26, 2020.
- 35.Liew MF, Siow WT, MacLaren G, Choong See K. Preparing for COVID-19: an early experience from an intensive care unit in Singapore. Crit Care. 2020;24:83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.COVID-19 recommendations during airway manipulation. Available at: https://www.cas.ca/en/practice-resources/news/cas-articles/2020/covid-19-recommendations-during-airway-manipulation. Accessed March 24. 2020.
- 37.Quick ICU training for COVID-19. The Critical Care Education Pandemic Preparedness (CCEPP) Team. Available at: www.quickicutraining.com. Accessed March 27, 2020.
- 38.Emergency Care of COVID-19 in adults in low resource settings. African Federation for Emergency Medicine. Available at: https://afem.africa/resources/. Accessed March 27, 2020.
- 39.Two Nigerians overdose self-medicating with Chloroquine after Trump praised anti-malarial drug as possible COVID-19 treatment. Available at: https://www.democracynow.org/2020/3/23/headlines/two_nigerian_overdose_self_medicating_with_chloroquine_after_trump_praised_anti_malaria_drug_as_possible_covid_19_treatment. Accessed March 24, 2020.
- 40.Chatterjee P. Indian pharma threatened by COVID-19 shutdowns in China. Lancet. 2020;395:675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Emanuel E, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of COVID-19. N Engl J Med. 2020 March 23 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 42.United Nations Development Group. Socio-economic impact of Ebola virus disease in West African Countries. Available at: https://www.undp.org/content/dam/rba/docs/Reports/ebola-west-africa.pdf. Accessed March 25, 2020.
- 43.Cost of the Ebola epidemic. Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/vhf/ebola/history/2014-2016-outbreak/cost-of-ebola.html. Accessed March 26, 2020.
- 44.Shannon FQ, II, Horace-Kwemi E, Najjemba R, et al. Effects of the 2014 Ebola outbreak on antenatal care and delivery outcomes in Liberia: a nation-wide analysis. PHA. 2017;7:588–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Heymann DL, Chen L, Takemi K, et al. Global health security: the wider lessons from the west African Ebola virus disease epidemic. Lancet. 2015;385:1884–1901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.International Health Regulations. WHO 2nd edition published 2008. 2005. Available at: https://www.who.int/ihr/publications/9789241596664/en/. Accessed March 26, 2020.


