Abstract
In adults hospitalized with viral pneumonias the main differential diagnostic consideration is influenza pneumonia. The respiratory viruses causing viral influenza like illnesses (ILIs), e.g., RSV may closely resemble influenza. Rarely, extrapulmonary findings of some ILIs may resemble Legionnaire's disease (LD), e.g., adenovirus, human parainfluenza virus (HPIV-3). We present a most unusual case of human metapneumonovirus pneumonia (hMPV) with some characteristic extrapulmonary findings characteristic of LD, e.g., relative bradycardia, as well as mildly elevated serum transaminases and hyphosphatemia. We believe this is the first reported case of hMPV pneumonia in a hospitalized adult that had some features of LD.
Keywords: Legionnaire's disease mimics, Viral pneumonias, Relative bradycardia, Hyponatremia, Hypophosphatemia, Elevated serum transaminases
Introduction
Human metapneumonovirus (hMPV) is a common cause of pneumonia in children, and has been appreciated as a cause of viral community acquired pneumonia (CAP) in hospitalized adults.1, 2, 3, 4, 5, 6 Unlike other causes of viral ILIs, excluding adenoviral pneumonia, hMPV in adults on occasion may present as focal/segmental infiltrates.7, 8, 9, 10, 11 The potential for hMPV in institutions, hospitals, chronic care facilities and nursing homes have been well described outbreaks.12, 13, 14 Therefore, the diagnosis of hMPV as a cause of CAP in hospitalized adults CAP has important infection control (IC) implications. hMPV pneumonia is more common and most severe in immunosuppressed patients particularly solid organ transplants or bone marrow transplants, but hMPV CAP may occur in immunocompetent adults.1, 2, 3, 4, 5, 6, 15 In hospitalized adults, respiratory viruses presenting as CAP have several clinical features in common, but specific diagnostic findings are few.7, 8, 9, 10 Prior to the availability of PCR for respiratory viruses of nasopharyngeal specimens, it was difficult to diagnose specific viral causes of CAP.11, 12, 13, 14 In hospitalized adults, viral ILI causes of pneumonia may have features mimicking Legionnaire's disease (LD) which has important IC and therapeutic complications.15, 16, 17, 18, 19, 20
We present an interesting case of an elderly female hospitalized for CAP initially thought to have Legionnaire's disease (LD) later diagnosed as hMPV pneumonia.
Case
81 year old female presented with fever, progressive cough, and weakness over four days. She had a past medical history of CML treated with chemotherapy 5 years ago. She was taking no medications. She denied any recent sick contacts. On admission her temperature was 104.4 °F with a pulse of 120/min (relative bradycardia) and a respiratory rate of 16/min. Laboratory tests included a WBC count of 9.8 K/mm3 (neutrophils = 49%, monocytes = 1%, lymphocytes = 47%), and a platelet count of 151 K/mm3 (n = 160–392 K). An ESR, CRP and serum ferritin level were not obtained. Her procalcitonin level was 1.2 mg/ml (n = <0.50 mg/ml). Serum transaminases were minimally elevated and her alkaline phosphatase was normal. On admission, she had otherwise unexplained hyponatremia and hypophosphatemia. Chest X-ray (CXR) showed a left lower lobe infiltrate without pleural effusion (Fig. 1 ). She was empirically treated for CAP with ceftriaxone and azithromycin but her fevers continued for four days. During hospitalization her CXR showed progression of her left lower lobe infiltrate to patchy bibasilar infiltrates (Fig. 2 ). Mycoplasma pneumoniae and Legionella sp. titers were negative. Legionella sp. sputum DFA and urinary antigen were also negative. Nasopharyngeal PCR was positive for human metapneumonovirus (hMPV). She slowly improved clinically and was discharged on hospital day #5.
Fig. 1.
Chest film of 81 year old female with left lower lobe hMPV community acquired pneumonia.
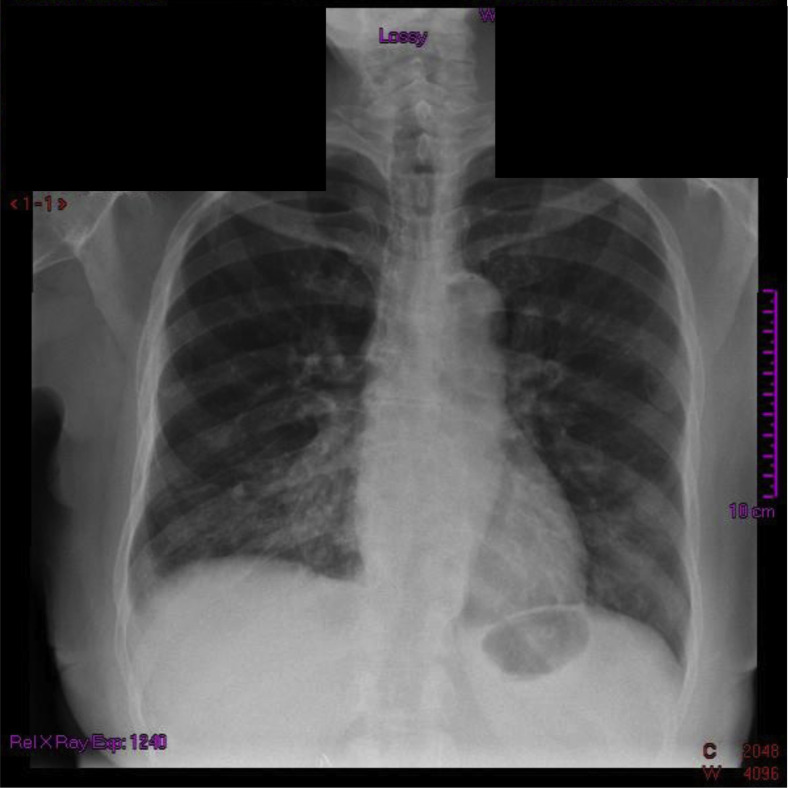
Fig. 2.
Repeat chest film of 81 year old female with hMPV community acquired pneumonia showing progression of her left lower lobe infiltrate at day #5 of hospitalization.
Discussion
In infectious disease, diagnosis is paramount. Appropriate empiric therapy is likely to be suboptimal without narrowing diagnostic possibilities to the most likely possibilities pending definitive pathogen identification. Adults ill enough to be hospitalized with a viral ILI may be caused by any one of several respiratory viruses, e.g., hMPV, rhinoviruses/enteroviruses (R/E), respiratory syncytial virus (RSV), coronaviruses (COR), adenoviruses (AdV), or human parainfluenza viruses (HPIV).7, 8, 9, 10, 11 In hospitalized adults, some viral ILIs may mimic influenza. Alternately, some ILIs may mimic LD, e.g., adenovirus, HPIV-3.1, 7, 8, 9, 10, 15
Viral PCR of respiratory secretions has provided a rapid and definitive diagnosis of the viral etiology of ILIs in hospitalized adults. However, PCR is expensive and not available/utilized at all institutions.7, 8, 9, 10, 11, 12, 13 In such situations, clinicians are faced with the diagnostic dilemma of differentiating influenza and ILIs influenza from adenovirus and LD.15 Adults hospitalized with LD usually have high fevers (>102 °F) with relative bradycardia. Extrapulmonary clinical features with LD include headache, mental confusion, watery diarrhea (± abdominal pain). Leukocytosis is the rule as is relative lymphopenia. Non-specific laboratory tests common in LD include hypophosphatemia, hyponatremia, mild/elevations of serum transaminases, highly elevated serum ferritin levels (>2 × n), elevated CPK levels, or microscopic hematuria.16, 17, 18 Diagnostic specificity of non-specific findings is increased when combined.19, 20
ILIs are so named because they have clinical features in common with influenza. Influenza A findings are strain dependent, i.e., during the swine influenza A (H1N1) pandemic, a normal WBC count or leukopenia was the rule. Whereas in the last influenza A (H3N2) epidemic, leukocytosis was the rule. Both H1N1 and H3N2 influenza A pneumonia are accompanied by relative lymphopenia and thrombocytopenia. Some influenza patients have mild transient elevations of serum transaminases. Findings that argue strongly against a diagnosis of influenza include relative bradycardia, a highly elevated ESR (>90 mm/h) or a highly elevated serum ferritin (>2 × normal) level.16, 20
In our case of hMPV pneumonia there some were features that suggested influenza A, e.g., thrombocytopenia. However, relative bradycardia suggested LD (Table 1 ).16, 19, 20 The presence of hyponatremia, hypophosphatemia, and mildly elevated serum transaminases also mimicked LD. Our hMPV patient had a CXR with focal patchy infiltrates unusual for a viral CAP but usual for LD. Arguing against the diagnosis of LD, was the presence of thrombocytopenia and lymphocytosis rather than relative lymphopenia and a normal platelet count (Table 2 ). Legionella sp. titers and urinary antigen tests were negative. The definitive diagnosis of her CAP was established by PCR of respiratory secretions demonstrating hMPV.
Table 1.
Relative bradycardia.a Temperature-pulse relationships.
| Temperature | Appropriate pulse response (beats/min) | Relative bradycardia If pulse (beats/min) |
|---|---|---|
| 106 °F (41.1 °C) | 150 | <140 |
| 105 °F (40.6 °C) | 140 | <130 |
| 104 °F (40.7 °C) | 130 | <120 |
| 103 °F (39.4 °C) | 120 | <110 |
| 102 °F (38.9 °C) | 110 | <100 |
Relative bradycardia refers to heart rates that are inappropriately slow relative to body temperature (pulse must be taken simultaneously with temperature elevation). Applies to adult patients with temperature ≥102 °F; does not apply to patients with second/third-degree heart block, pacemaker-induced rhythms, or those taking beta-blockers, diltiazem, or verapamil.
Adapted from: Cunha BA. Antibiotic Essentials (14th ed). Jay Pee Medical Publishers, New Delhi, 2015.
Table 2.
Legionnaire's disease: similarities and differences with this case of hMPV pneumonia.
| Features in common with LD (mimicking LD) | Features arguing against a diagnosis of LD |
|---|---|
|
LD = Legionnaires disease; CXR = chest X-ray; DX = diagnosis.
Besides LD, the only CAPs associated with relative bradycardia are Q fever and psittacosis.
Except for adenovirus and rarely HPIV-3 pneumonia, viral pneumonias have minimal/no infiltrates on CXR early, and late may develop bilateral interstitial infiltrates. However, with the aforementioned exceptions viral infiltrates on CXR are never focal/segmental.
Conclusions
This is an interesting case of hMPV CAP an elderly normal host who presented in springtime during a non-seasonal increase in LD incidence at our hospital. hMPV has a non-seasonal distribution, and patients presenting with a viral CAP during the non-winter months should consider hMPV in the diagnosis.2, 3, 4, 5 Our patient had a remote history of CML treated with chemotherapy 5 years ago, and there is only one reported case of fatal hMPV pneumonia in a patient with active AML and adenocarcinoma of the lung.6
This case mimicked LD with high fevers and relative bradycardia, hyponatremia, hypophosphatemia and mildly elevated serum transaminases. Against the diagnosis of LD was lymphocytosis and the presence of thrombocytopenia.16, 20 Influenza was ruled out by PCR and LD was ruled out by specific testing (Legionella sp. titers and urinary antigens). Expectedly, her fevers due to hMPV continued despite empiric antimicrobial therapy for CAP (with Legionella activity). We conclude that in hospitalized adults with hMPV pneumonia, like adenovirus and HPIV-3, may have some clinical findings that mimic LD.
Footnotes
All authors: no funding or conflict of interest.
References
- 1.Johnstone J., Majumdar S.R., Fox J.D., Marrie T.J. Viral infection in adults hospitalized with community-acquired pneumonia: prevalence, pathogens and presentation. Chest. 2008;134:1141–1148. doi: 10.1378/chest.08-0888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johnstone J., Majumdar S.R., Fox J.D., Marrie T.J. Human metapneumovirus pneumonia in adults: results of a prospective study. Clin Infect Dis. 2008;46:571–574. doi: 10.1086/526776. [DOI] [PubMed] [Google Scholar]
- 3.Al-Turab M., Chehade W., Al-Mulla F., AL-Nakib W. Human metapneumovirus in patients with respiratory tract infection in Kuwait. J Med Virol. 2011;83:1811–1817. doi: 10.1002/jmv.22193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kroll J.L., Weinberg A. Human metapneumovirus. Semin Respir Crit Care Med. 2011;32:447–453. doi: 10.1055/s-0031-1283284. [DOI] [PubMed] [Google Scholar]
- 5.Shahda S., Carlos W.G., Kiel P.J. The human metapneumovirus: a case series and review of the literature. Transpl Infect Dis. 2011;13:324–328. doi: 10.1111/j.1399-3062.2010.00575.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Godet C., LeGoff J., Beby-Defaux A. Human metapneumovirus pneumonia in patients with hematological malignancies. J Clin Virol. 2014;61:593–596. doi: 10.1016/j.jcv.2014.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Falsey A.R., Walsh E.E. Viral pneumonia in older adults. Clin Infect Dis. 2006;42:518–524. doi: 10.1086/499955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.High K.P. Pneumonia in older adults. New categories add complexity to diagnosis and care. Postgrad Med. 2005;118:18–20. doi: 10.3810/pgm.2005.10.1697. [DOI] [PubMed] [Google Scholar]
- 9.Ruuskanen O., Lahti E., Jennings L.C., Murdoch D.R. Viral pneumonia. Lancet. 2011;377:1264–1275. doi: 10.1016/S0140-6736(10)61459-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cesairo T.C. Viruses associated with pneumonia in adults. Clin Infect Dis. 2012;55:107–113. doi: 10.1093/cid/cis297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Widmer K., Griffen M.R., Zhu Y., Williams J.V., Talbot H.K. Respiratory syncytial virus and human metapneumovirus associated emergency department and hospital burden in adults. Influenza Other Respir Viruses. 2014;8:347–352. doi: 10.1111/irv.12234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Souza J.S., Watanabe A., Carraro E., Granato C., Beliei N. Severe metapneumovirus infections among immunocompetent and immunocompromised patients admitted to hospital with respiratory infection. J Med Virol. 2013;85:530–536. doi: 10.1002/jmv.23477. [DOI] [PubMed] [Google Scholar]
- 13.Jain B., Singh A.K., Dangi T. High prevalence of human metapneumovirus subtype B in cases presenting as severe acute respiratory illness: an experience at tertiary care hospital. Clin Respir J. 2014;8:225–233. doi: 10.1111/crj.12064. [DOI] [PubMed] [Google Scholar]
- 14.Falsley A.R., McElhaney J.E., Beran J. Respiratory syncytial virus and other respiratory viral infections in older adults with moderate to severe influenza-like illness. J Infect Dis. 2014;209:1873–1881. doi: 10.1093/infdis/jit839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cunha B.A. Severe adenovirus mimicing legionella community-acquired pneumonia (CAP) Eur J Clin Microbiol Infect Dis. 2009;28:313–315. doi: 10.1007/s10096-008-0611-6. [DOI] [PubMed] [Google Scholar]
- 16.Cunha B.A. Legionnaires disease: clinical differentiation from typical and other atypical pneumonias. Infect Dis Clin N Amer. 2010;24:73–105. doi: 10.1016/j.idc.2009.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cunha B.A., Strollo S., Schoch P. Extremely elevated erythrocyte sedimentation rates (ESRs) in Legionnaires disease. Eur J Clin Microbiol Infect Dis. 2010;29:1567–1569. doi: 10.1007/s10096-010-1016-x. [DOI] [PubMed] [Google Scholar]
- 18.Cunha B.A. Hypophosphatemia: diagnostic significance in Legionnaires disease. Am J Med. 2006;119:e5–e6. doi: 10.1016/j.amjmed.2005.11.026. [DOI] [PubMed] [Google Scholar]
- 19.Cunha B.A. The clinical diagnosis of Legionnaires disease: the diagnostic value of combining non-specific laboratory tests. J Infect. 2008;56:395–397. doi: 10.1016/j.jinf.2008.02.009. [DOI] [PubMed] [Google Scholar]
- 20.Cunha B.A., Wu G., Raza M. Clinical diagnosis of Legionnaire's disease: six characteristic criteria. Am J Med. 2015;128:e21–e22. doi: 10.1016/j.amjmed.2015.01.030. [DOI] [PubMed] [Google Scholar]