Abstract
Nucleos(t)ide analogues play pivotal roles as antiviral, cytotoxic or immunosuppressive agents. Here, we review recent reports of nucleoside analogues that exhibit broad-spectrum activity towards multiple life-threatening RNA and DNA viruses. We also present a discussion about nucleoside antimetabolites—approved antineoplastic agents—that have recently been shown to have antiviral and/or antibacterial activity. The approved drugs and drug combinations, as well as recently identified candidates for investigation and/or experimentation, are discussed. Several examples of repurposed drugs that have already been approved for use are presented. This strategy can be crucial for the first-line treatment of acute infections or coinfections and for the management of drug-resistant strains.
Keywords: Nucleosides, Nucleotides, Prodrugs, Antiviral therapy, Chain termination, Antineoplastic agents
Abbreviations of virus names
- AdV
Adenovirus
- CHIKV
Chikungunya virus
- CMV
Cytomegalovirus
- DENV
Dengue virus
- EBOV
Ebola virus
- EBV
Epstein–Barr virus
- FLUAV
Influenzavirus A
- HBV
Hepatitis B virus
- HCV
Hepatitis C virus
- HIV
Human immunodeficiency viruses
- HMPV
Human metapneumovirus
- HSV
Herpes simplex virus
- MARV
Marburg virus
- RSV
Human orthopneumovirus
- MulV
Murine leukaemia virus
- RVFV
Rift Valley fever virus
- SINV
Sindbis virus
- VZV
Varicella zoster virus
- YFV
Yellow fever virus
- ZIKV
Zika virus
1. Introduction
Epidemics and pandemics have had significant impacts on human history for centuries. Recently, the World Health Organization (WHO) has been issuing a report on new viral pathogens that pose a threat to public health almost every year. Emerging epidemics caused by new pathogens or by strains that are more pathogenic than the preceding viral pathogens necessitate the development of effective strategies for combating and preventing viral infections. Immunoprophylaxis by a specific vaccination is one of the most important strategies for combating many infectious diseases. However, there are still many viruses for which no effective vaccine is available on the market. In these cases, the use of effective antiviral drugs is the only possible way to fight against infections caused by viruses.
The introduction of new antiviral agents for clinical use has revolutionized the treatment of many viral infections caused by either DNA or RNA viruses (De Clercq and Li, 2016; De Clercq, 2013a; Chaudhuri et al., 2018). Most of the approved drugs have been licensed for the treatment of infections caused by a single virus. However, some drugs with antiviral activity against several viruses have also been discovered, suggesting their universal mechanism of action. Such drugs belonging to the group of broad-spectrum antivirals are of particular interest since their pleiotropic effect may show activity against other viruses that have been undefined thus far (Ianevski et al., 2018, 2019). Recently, several approved antiviral and anticancer drugs from the nucleos(t)ide antimetabolite group have been reported to show newly discovered antiviral/antibacterial activities (Jordheim et al., 2013; Thomson and Lamont, 2019).
Nucleos(t)ide analogues are much more structurally diverse than their naturally occurring counterparts (Seley-Radtke and Yates, 2018; Yates and Seley-Radtke, 2019). Modifications may be introduced in the nucleobase, the sugar moiety or the phosphate residue. Nucleobases may be modified by halogenation, azotation, N-conjugation, ring opening or the introduction of another heterocyclic system. In the sugar moiety, substituents can be exchanged or removed, the configuration of carbon atoms in the ring can be changed, additional heteroatoms can be introduced into the ring, or the oxygen in the ring can be replaced with another atom. Moreover, the ring size can be changed or replaced with an acyclic fragment. The phosphate fragment may be protected, replaced by another phosphorus-containing group or by a fragment derived from another compound (e.g., an amino acid) or completely eliminated.
This review summarizes currently available nucleos(t)ide-based drugs and their acyclic analogues that exhibit multi-target activity against viral infections of great medical importance (e.g., herpes simplex virus (HSV), varicella zoster virus (VZV), human immunodeficiency virus (HIV), hepatitis B virus (HBV) and hepatitis C virus (HCV)) and/or that are known antineoplastic agents used to treat cancer. Approved nucleos(t)ide-based drugs with multi-target activity and compounds being tested in clinical trials or evaluated in preclinical assays are listed in Table 1 . In this paper, the term “approval date” means the date on which the drug was approved by the US Food and Drug Administration (FDA) unless otherwise stated.
Table 1.
Approved nucleos(t)ide-based antiviral and antineoplastic drugs with multi-target activity.
| Name | Type | Approved antiviral drug (approval date) | Approved antineoplastic drug (approval date) | Active clinical-stage developmenta | Experimental development |
|---|---|---|---|---|---|
| Acyclovir | Acyclic guanosine analogue | HSV, VZV (1982) | Breast cancer (Shaimerdenova et al., 2017) EBV (Pagano et al., 2018) |
||
| Azacitidine | Cytidine analogue | Myelodysplastic syndrome (2004) | AdV (Alexeeva et al. (2001); (Alexeeva et al., 2015) HMPV (Bösl et al., 2019) HIV-1 (Dapp et al., 2009; Rawson et al., 2016a) HIV-1 – synergy in combination with resveratrol (Rawson et al., 2016b) HIV-2 (Beach et al., 2014) RVFV (Ianevski et al., 2018) HTLV-1 (Diamantopoulos et al., 2012) HSV-1, FLUAV (Ianevski et al., 2018) |
||
| Brivudine | Thymidine analogue | HSV-1, VZV (2002)b | |||
| Clofarabine | Adenosine analogue | Acute lymphoblastic leukaemia (2004) | HIV-1 (Daly et al., 2016) HIV-1, HIV-2 (Beach et al., 2014) |
||
| Decitabine | Cytidine analogue | Myelodysplastic syndrome (2006) | HIV-1 (Clouser et al., 2010) HIV-1 – synergy in combination with gemcitabine (Clouser et al., 2010) HIV-1 – synergy in combination with resveratrol (Jonathan M.O. Rawson et al., 2016b) MuLV (Clouser et al., 2012) |
||
| Famciclovir | Acyclic guanosine analogue | HSV, VZV (1994) | |||
| Galidesivir | Adenosine analogue | EBOV (n/a) | MARV (phase 1, NCT03800173) YFV (phase 1, NCT03891420) |
ZIKV (Julander et al., 2017) broad-spectrum antivirals (Westover et al., 2018) | |
| Ganciclovir | Acyclic guanosine analogue | HSV, VZV, CMV (1989) | EBV (Pagano et al., 2018) | ||
| Gemcitabine | Cytidine analogue | Various carcinomas (1995): non-small cell lung cancer, pancreatic cancer, bladder cancer breast cancer ovarian cancer | HIV-1 (Rawson et al. (2013); Clouser et al. (2010); (Clouser et al., 2012) HIV-1 – synergy in combination with decitabine (Clouser et al., 2010) MuLV (Clouser et al., 2012) HIV-2 (Beach et al., 2014) ZIKV (Kuivanen et al., 2017) Enteroviruses including poliovirus (Kang et al., 2015; Zhang et al., 2017) Enteroviruses – synergy with ribavirin (Kang et al., 2015) Rhinoviruses (Song et al., 2017) HCV (Beran et al., 2012) Coronaviruses (Dyall et al., 2014) SINV, HSV-1, FLUAV (Denisova et al., 2012) Gram-positive bacteria (Jordheim et al., 2012; Sandrini et al., 2007; Thomson and Lamont, 2019) |
||
| Lamivudine | L-Cytidine analogue | HIV (1999) HBV (1995) |
|||
| Penciclovir | Acyclic guanosine analogue | HSV, VZV (1996) | |||
| Ribavirin | Nucleoside analogue | RSV, HCV (1985) viral haemorrhagic fevers | HBV (phase 3, (NCT03759782, in combination with tenofovir) | Enteroviruses (Bauer et al., 2017) Influenza virus (Pauly and Lauring, 2015) |
|
| Sofosbuvir | Uridine nucleotide analogue | HCV (2013) | HBV (phase 2, NCT03312023; I combination with ledipasvir) | DENV (Xu et al., 2017) YFV (De Freitas et al., 2019) ZIKV (Mesci et al., 2018; Bullard-Feibelman et al., 2017) CHIKV (Ferreira et al., 2019) |
|
| Telbivudine | L-Thymidine | HBV (2006) | Immunomodulatory, anti-inflammatory properties (Van Linthout et al., 2018) | ||
| Tenofovir disoproxil | Acyclic adenosine nucleotide analogue | HIV (2001) HBV (2008) |
|||
| Tenofovir alafenamide | Acyclic adenosine nucleotide analogue | HBV (2016) HIV (several combination, see Table 2) |
HBV (phase 2, NCT03434353, in combination with inarigivir) | ||
| Trifluridine | Thymidine analogue | HSV (1980) | Metastatic colorectal cancer (2015) in combination with tipiracil | Mycoplasma pneumonia (Sun and Wang, 2013) | |
| Valaciclovir | Acyclic guanosine analogue | HSV, VZV, CMV (1995) | |||
| Valganciclovir | Acyclic guanosine analogue | HSV, VZV, CMV (2001) | EBV (Pagano et al., 2018) | ||
| Vidarabine | Arabinosyl adenine analogue | HSV, VZV (1976) |
Clinical data from ClinicalTrials.gov (see https://www.clinicaltrials.gov/) in July 2019.
Approved by European Medicines Agency (EMA).
2. Multi-target nucleos(t)ide-based drugs in the treatment and prophylaxis of HIV, HBV and HCV infections
HIV, HBV and HCV are three blood-borne viruses that cause emerging infectious diseases in humans worldwide (Leoni et al., 2018). According to the WHO, viral hepatitis caused 1.34 million deaths in 2015, a number that is comparable to the number of annual deaths caused by tuberculosis and that is even higher than those attributed to HIV. A global hepatitis report concluded that mortality from HIV, tuberculosis, and malaria is now declining, while mortality from viral hepatitis has been increasing over time (World Health Organization, 2017). In the last report, the WHO estimated that in 2015, 257 million people, that is, 3.5% of the population, were living with chronic HBV infection. Individuals in the African and Western Pacific regions accounted for 68% of those infected. These individuals are at risk of developing severe complications, including cirrhosis and hepatocellular carcinoma. In 2015, hepatitis B resulted in 887,000 deaths, mostly due to complications. Among the 36.7 million persons living with HIV in 2015, an estimated 2.7 million had chronic HBV infection, and 2.3 million had been infected with HCV. Liver diseases constitute the major cause of morbidity and mortality among those living with HIV and coinfected with viral hepatitis. People with these conditions should be prioritized for diagnosis and provided appropriate and effective treatment for both HIV and hepatitis. Currently, HIV and HBV preventive strategies and treatment options are characterized by lifelong and chronic treatment, while for HCV, short-term and curative treatment is available. In contrast to HCV, for which a definitive cure has been developed because it does not persist in cells, the elimination of HBV and HIV infections worldwide is primarily hindered by their persistence in the host organism (Leoni et al., 2018).
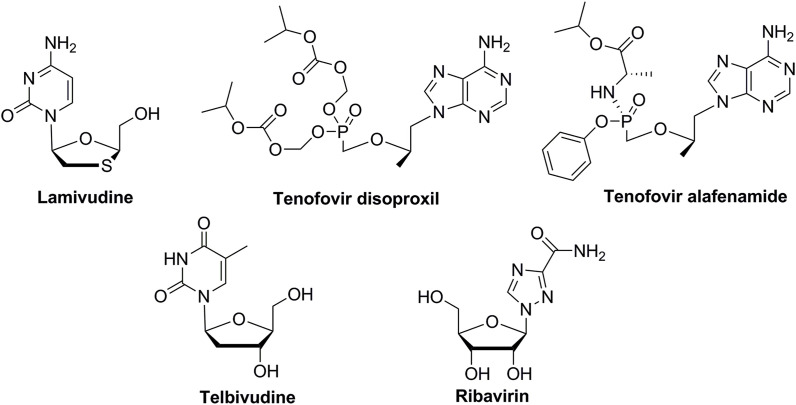
Several nucleos(t)ide-based therapies are currently approved for the treatment of chronic HBV infection (Liu et al., 2018). Approved nucleos(t)ide inhibitors of HBV polymerase include lamivudine, adefovir, telbivudine, entecavir and tenofovir. Two of them, lamivudine and tenofovir, exhibit multi-target activity and are also approved as inhibitors of HIV replication (Table 1, Fig. 1 ). This targeted HBV polymerase is functionally and structurally related to HIV reverse transcriptase, and in the case of both viruses, inhibitors act as chain terminators because they belong to the family of competitive substrate analogue inhibitors (Menéndez-Arias et al., 2014). According to the mechanism of action, the nucleos(t)ide analogue is converted into its active triphosphate form by cellular kinases. Then, the activated nucleos(t)ide inhibitor competes with natural nucleotide substrates for incorporation into the elongating viral DNA chain. The lack of a 3′-OH group in the incorporated nucleos(t)ide analogue prevents the formation of the 5′ to 3′ phosphodiester linkage essential for continued DNA chain elongation, and therefore, the viral DNA growth is terminated. Lamivudine (2′,3′-dideoxy-3′-thia-β-L-cytidine, 3TC) is an analogue of L-cytidine in which a sulphur atom replaces the 3′ carbon of the pentose ring. Tenofovir is an acyclic analogue of adenosine 5′-monophosphate and is marketed in the form of two prodrugs: tenofovir disoproxil (TDF, Viread) and tenofovir alafenamide (TAF, Vemlidy). The roles of the two prodrugs in the treatment and prophylaxis of HIV and HBV infections were comprehensively compared by De Clercq (De Clercq, 2018). The tendency to substitute tenofovir disoproxil with tenofovir alafenamide in both anti-HIV and anti-HBV treatment has been reported, although both drugs pose little or no risk of virus drug resistance.
Fig. 1.
Structures of nucleos(t)ide-based drugs for the treatment of HBV infections.
Telbivudine (L-thymidine) is used in the treatment of hepatitis B infection. Clinical trials have shown that this drug is significantly more effective than lamivudine and less likely to cause resistance. Moreover, telbivudine has some pleiotropic immunomodulatory and anti-inflammatory properties (Rehermann and Bertoletti, 2015). Recently, it was shown that telbivudine confers endothelial-protective effects on B19V-infected endothelial cells and improves the chronic myocarditis associated with B19V transcriptional activity (Van Linthout et al., 2018).
Treatment of HBV infections is usually carried out as a monotherapy; thus, combination therapies are not generally recommended (De Clercq, 2018). One of the exceptions is the use of ribavirin in combination with standard therapy to enhance the current treatment regimens. Ribavirin is commonly used to treat HCV, but there is evidence that it also induces immune effects that positively affect HBV treatment. A study on anti-HBV treatment with ribavirin and tenofovir, compared to tenofovir treatment alone, is currently in a phase 3 clinical trial (NCT03759782).
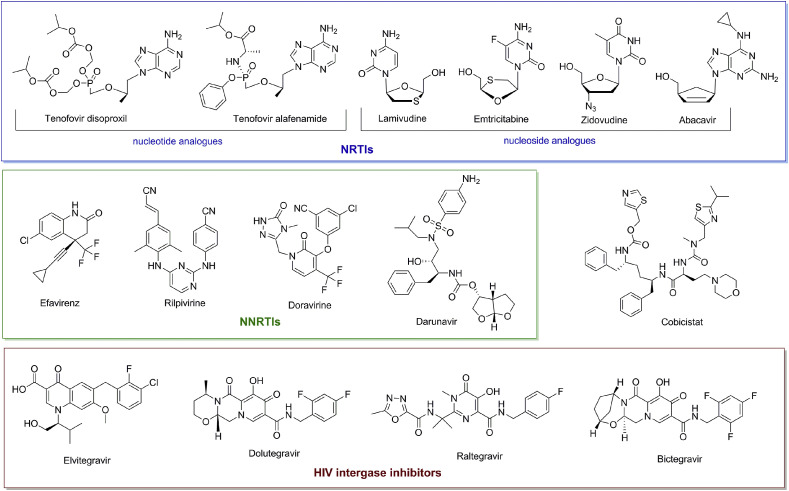
In contrast to HBV, combination treatments have been the standard for the treatment of HIV infection for many years. Nucleoside reverse transcriptase inhibitors (NRTIs) are commonly administered with other drugs in highly active antiretroviral therapy (HAART) to target multiple stages of the HIV life cycle. Lamivudine and tenofovir are among the most important drugs used in combination (Das et al., 2019). According to a survey, among the top 24 small-molecule combinations most frequently utilized as drug components, anti-HIV lamivudine occurred 15 times, while tenofovir disoproxil occurred 9 times. Lamivudine and tenofovir have been combined with other NRTIs (e.g., abacavir, emtricitabine, and zidovudine) or with non-nucleoside reverse transcriptase inhibitors (NNRTIs) (e.g., efavirenz, darunavir, rilpivirine, and doravirine). Inhibitors of HIV integrase (elvitegravir, dolutegravir, raltegravir, and bictegravir) can also be found in several compositions (Table 2 , Fig. 2 ).
Table 2.
Nucleos(t)ide-based multi-target drugs in the treatment of HBV and HIV infections.
| Nucleos(t)ide-type drugs with multi-target activity | Approved anti-HBV monotherapy | Approved combination drug for HIV |
|---|---|---|
| Tenofovir disoproxil fumarate (TDF) | Viread, Gilead, 2008 | Viread, Gilead Sciences, 2001 (tenofovir disoproxil fumarate) Truvada, Gilead Sciences, 2004 (emtricitabine + tenofovir disoproxil fumarate) Atripla, Gilead Sciences, Bristol-Myers Squibb, 2006 (emtricitabine + efavirenz + tenofovir disoproxil fumarate) Complera, Gilead Sciences, 2011 (emtricitabine + rilpivirine + tenofovir disoproxil fumarate) Stribild, Gilead Sciences, 2012 (elvitegravir + cobicistat + emtricitabine + tenofovir disoproxil fumarate) Delstrigo, Merck, 2018 (doravirine + lamivudine +tenofovir disoproxil fumarate) Cimduo, Mylan Pharmaceuticals, 2018 (lamivudine + tenofovir disoproxil fumarate) Symfi Lo, Mylan Pharmaceuticals, 2018 (efavirenz + lamivudine + tenofovir disoproxil fumarate) |
| Tenofovir alafenamide fumarate (TAF) | Vemlidy, Gilead, 2016 | Genvoya, Gilead Sciences 2015 (elvitegravir + cobicistat + emtricitabine, + tenofovir alafenamide) Descovy, Gilead Sciences, 2016 (emtricitabine + tenofovir alafenamide) Odefsey, Gilead Sciences, 2016 (emtricitabine + rilpivirine + tenofovir alafenamide) Symtuza, Janssen Therapeutics, 2018 (darunavir + cobicistat + emtricitabine + tenofovir alafenamide) Biktarvy, Gilead Sciences, 2018 (bictegravir + emtricitabine + tenofovir alafenamide) |
| Lamivudine (3TC) | Epivir, Glaxo Wellcome, 1998 | Combivir, ViiV Healthcare, 2000 (lamivudine + zidovudine) Trizivir, ViiV Healthcare, 2000 (abacavir + lamivudine + zidovudine) Epzicom, ViiV Healthcare, 2004 (abacavir + lamivudine) Triumeq, ViiV HealthCare, 2014 (abacavir + dolutegravir + lamivudine) Dutrebis, Merck, 2015 (lamivudine + raltegravir) Delstrigo, Merck, 2018 (doravirine + lamivudine +tenofovir disoproxil fumarate) Cimduo, Mylan Pharmaceuticals, 2018 (lamivudine + tenofovir disoproxil fumarate) Symfi Lo, Mylan Pharmaceuticals, 2018 (efavirenz + lamivudine + tenofovir disoproxil fumarate) Dovato, ViiV Healthcare, 2019 (dolutegravir + lamivudine) |
Fig. 2.
Structures of nucleos(t)ide-based and non-nucleoside drugs used in combination with tenofovir and lamivudine for the treatment of HIV infections. Abbreviations: NRTIs - nucleoside reverse transcriptase inhibitors, NNRTIs - non-nucleoside reverse transcriptase inhibitors.
One of the recently approved anti-HIV combinations, Biktarvy (bictegravir + emtricitabine + tenofovir alafenamide), is currently under phase 3 and 4 clinical trials for HIV-HBV coinfection (NCT03547908 and NCT03797014). The primary objective of this study is to evaluate the efficacy and safety of a fixed-dose combination in adults coinfected with HIV-1 and HBV. Table 2 presents the most commonly used combinations of NRTIs, NNRTIs and HIV integrase inhibitors, and Fig. 2 shows the structures of the compounds listed in Table 2 grouped according to their chemical characteristics and molecular targets.
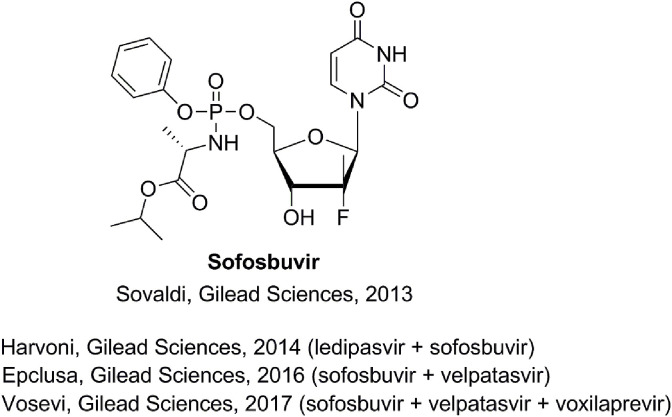
In the last two decades, notable progress has been made in the development of anti-HCV drugs. Treatments with pegylated interferon (PEG-IFN) and ribavirin for HCV eradication have been replaced by the second generation of direct-acting antivirals (DAAs). Compared to previous treatments, DAAs offer better tolerability and HCV eradication in almost 95% of cases (Sagnelli et al., 2017). Single drugs or combinations of two or more DAAs of different classes have been marketed. A highly active drug, sofosbuvir, belonging to the group of nucleotide prodrugs, is one of the most successful examples (Lam et al., 2012; Sofia et al., 2010). Sofosbuvir was approved by the FDA in 2013 for use against chronic hepatitis C infection. Sofosbuvir was the first drug that demonstrated safety and efficacy in treating certain types of HCV infection without the need for co-administration of INF. The high potency of sofosbuvir is attributable, in part, to the first 5′-phosphate group, which was built into the structure of this prodrug, thereby eliminating the first rate-limiting enzymatic transformation into the monophosphate. Additional groups are attached to the phosphorus atom to temporarily mask the two negative charges of the phosphate group, thereby facilitating the entry of the drug into the infected cell (Murakami et al., 2010). Sofosbuvir can be used either alone or in combination. Examples are presented in Fig. 3 .
Fig. 3.
Sofosbuvir alone and in combination with other drugs in the treatment of HCV infections.
Second-generation DAA treatments can also be used for HBV/HCV coinfected patients (Sagnelli et al., 2017). Currently, the drug combination ledipasvir/sofosbuvir is under phase 2 clinical trial for use in HBV infection (NCT03312023). It has been observed that patients who had both hepatitis B and hepatitis C and who were treated for hepatitis C for 12 weeks with a combination of ledipasvir/sofosbuvir had decreased hepatitis B surface antigen levels. This finding was the basis for the hypothesis that a similar decrease could be observed in mono-infected individuals with hepatitis B.
Sofosbuvir was also recently shown to protect against Zika flavivirus (ZIKV) in studies both in vitro and in vivo (Mesci et al., 2018; Bullard-Feibelman et al., 2017). It has been found that HCV and ZIKV RNA polymerases have very similar active sites, confirming that sofosbuvir could also act on ZIKV-infected cells. It was also demonstrated via cellular assays and animal models that sofosbuvir inhibits the replication of other flaviviruses, such as dengue virus (DENV) (Xu et al., 2017), yellow fever virus (YFV) (De Freitas et al., 2019), and chikungunya virus (CHIKV) (Ferreira et al., 2019).
3. Multi-target nucleos(t)ide-based drugs against various herpesviruses
Even though more than 90 antiviral drugs are currently approved for the treatment of viral infections, many are suitable for use only with a single virus (De Clercq and Li, 2016). New antiviral drugs with activity against multiple viral types are being sought, and many of these compounds are undergoing advanced clinical trials (Chaudhuri et al., 2018). Several of these drugs are used for diseases caused by herpesviruses.
Herpesviruses, classified in the DNA virus family, include several different viruses, such as HSV-1; HSV-2; VZV, which may also be called HHV-3; Epstein–Barr virus (EBV or HHV-4); human cytomegalovirus (CMV or HHV-5); human herpesvirus 6 and 7 (HHV-6 and HHV-7); and Kaposi's sarcoma-associated herpesvirus (KSHV, also known as HHV-8), which cause a wide spectrum of diseases, especially in vertebrates (Littler and Zhou, 2007; Luczkowiak et al., 2019). According to a WHO report, approximately 70% of the worldwide population younger than 50 years old is infected with HSV-1 or HSV-2. HSV is a highly infectious virus that causes so-called cold sores of the mouth (in cases of infection with HSV-1) or on the genitals (in cases of infection with HSV-2). These viruses can also attack the central nervous system and cause encephalitis. HSV-1 can be transmitted through oral contact, while HSV-2 is spread through sexual contact (Looker et al., 2015; Das and Hong, 2018). For VZV, which is another herpesvirus, the infection occurs most often in childhood and causes chickenpox. Unfortunately, even in cured patients, the virus remains latent in the body (cervical ganglia) and can be reactivated when the host's immune system is weakened (Littler and Zhou, 2007).
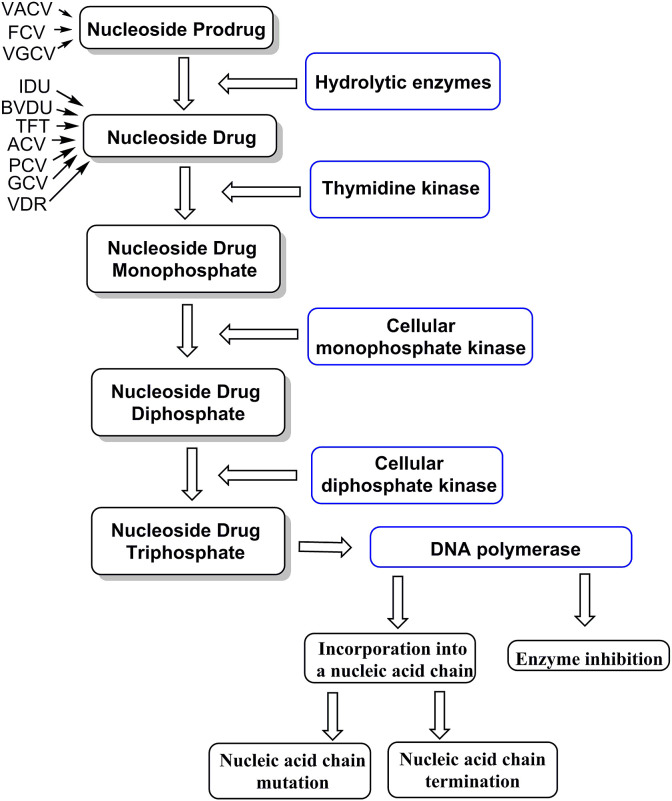
Drugs used clinically for treating herpesvirus infections can be divided into two categories: nucleoside analogues and non-nucleoside drugs. Both types of drugs target viral DNA polymerase. Nucleoside-type drugs enter cells through concentrative nucleoside transporters (Cano-Soldado and Pastor-Anglada, 2012). Inside the cell, these transporters undergo phosphorylation with a nucleoside kinase (e.g., thymidine kinase). This initial rate-limiting step leads to a monophosphate metabolite. The herpesvirus thymidine kinase is characterized as having broader substrate specificity than that of its counterpart in mammalian cells, and as a result, drugs targeting herpesviruses have relatively low toxicity (Andrei et al., 2012). The second and third phosphorylation steps are performed by viral kinases. The triphosphorylated nucleoside formed in this way is the active form of this type of drug, and it can bind to the active sites of the viral DNA polymerase and act as a competitive inhibitor of this enzyme during viral DNA synthesis. The active form of nucleoside-type drugs can also act as a substrate for the viral enzyme and can be incorporated into the DNA chain, preventing the prolongation of the viral DNA and possibly causing the accumulation of mutations in the multiplying viruses or the induction of apoptosis (Scheme 1 ) (Jordheim et al., 2013; Das and Hong, 2018). To increase the oral bioavailability of some of the anti-herpesvirus drugs, such as acyclovir, penciclovir or ganciclovir, an amino acid esterification strategy is applied to obtain compounds such as valaciclovir, famciclovir and valganciclovir, respectively. These “prodrugs” are rapidly converted into the active form of the nucleoside-type drugs by enzymes in the liver and intestinal walls (Weller et al., 1993).
Scheme 1.
Mechanism of action of nucleoside-type drugs and prodrugs against herpesviruses. Abbreviations: ACV – acyclovir, BVDU – brivudine, IDU – idoxuridine, FCV – famciclovir, GCV – ganciclovir, PCV - penciclovir, TFT - trifluridine, VACV - valaciclovir, VDR – vidarabine, and VGCV – valganciclovir.
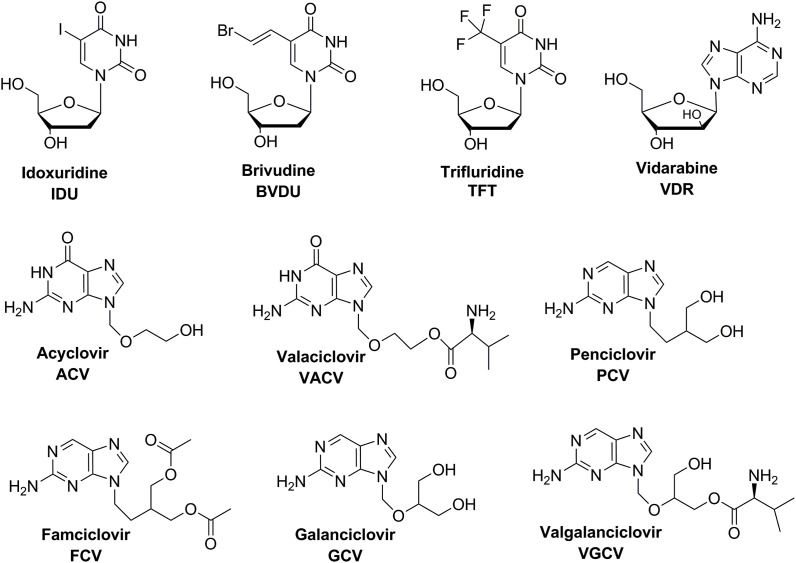
As described above, some of the nucleotide-based anti-herpesvirus drugs are active against more than one virus. Idoxuridine (IDU, 5-iodo-2′-deoxyuridine, Fig. 4 ) is an iodinated thymidine analogue and the first antiherpetic drug, discovered by W. Prusoff in 1959 (Prusoff, 1959), to be licensed by the FDA, in 1963, for the treatment of HSV. It is also effective in local therapy against VZV (Essmann and Wildenhoff, 1980; Nikkeis and Piérard, 1994). However, significant toxicity is associated with its systemic use. The mechanism of action of idoxuridine is not exactly defined, but the triphosphate inhibits viral DNA synthesis and is incorporated into both viral and cellular DNA. Currently, in the United States, idoxuridine is approved for only topical treatment of HSV keratitis, but in Europe, idoxuridine in DMSO is available for the treatment of herpes labialis, herpes genitalis and herpes zoster (Aoki, 2015).
Fig. 4.
Nucleoside-based marketed drugs against various herpesviruses.
Brivudine (BVDU, 5-[2-bromovinyl]-2′-deoxyuridine), similar to idoxuridine, is a 5-substituted thymidine analogue approved as a drug for use against a wide range of herpesviruses. Brivudine is highly specific against HSV-1 and VZV; however, it does not show activity against HSV-2 (Topalis et al., 2016). This drug is widely available in Europe, except the United Kingdom, and many other countries, except the United States (De Clercq, 2004; Andrei et al., 2005). It was also found that brivudine might be used to treat EBV encephalitis. However, clinical trials are still required to confirm its effective and safe use as an anti-EBV drug (Lin et al., 1985; Lahmer et al., 2010). The results of a comparison of brivudine, famciclovir and valaciclovir treatment in immunocompetent adult patients with herpes zoster indicate that brivudine may be the first choice in cases of severe herpes zoster because of its ability to promptly control pain and its once-a-day use (Yaldiz et al., 2016). The literature also describes a novel series of phosphoramidate nucleoside (idoxuridine and brivudine) prodrugs that include amino acid motifs based on L-aspartic acid and L-glutamic acid (so-called ProTides), which have been evaluated for their cytotoxic activity against a panel of cancer cell lines. Compared to parent nucleoside, such as idoxuridine or brivudine, which displayed only weak to moderate activity, the corresponding ProTide showed increased cytotoxic activity (Gao et al., 2016).
Trifluridine (trifluorothymidine, 5-trifluoromethyl-2′-deoxyuridine, TFT) belongs to a group of fluorinated pyrimidine analogues. This compound is used as an anti-HSV drug in therapy for HSV-induced epithelial keratitis. After its conversion to trifluridine monophosphate, it inhibits thymidylate synthetase, which is elevated in different cancer cell lines. After further phosphorylation, the corresponding triphosphate competitively inhibits DNA polymerases with respect to thymidine triphosphate (Aoki, 2015). Trifluridine in combination with tipiracil (Lonsurf) has been approved in Japan, the United States, and the European Union for the treatment of adult patients with metastatic colorectal cancer who were previously subjected to chemotherapy involving fluoropyrimidine, oxaliplatin and irinotecan (Burness and Duggan, 2016; Matsuoka et al., 2018). Phase 3 clinical trials are also underway to collect additional data about the safety and efficacy of trifluridine-tipiracil during the treatment of patients with metastatic colorectal cancer (NCT03306394). Trifluridine was also tested as an antibacterial agent. Specifically, it was found that trifluridine strongly inhibits Mycoplasma pneumoniae growth in vitro (Sun and Wang, 2013). Unfortunately, no clinical trials have been undertaken in this direction in recent years.
There are six approved acyclic guanosine analogues, namely, acyclovir, ganciclovir, valaciclovir, valganciclovir, penciclovir, and famciclovir (Fig. 4). First, acyclovir (ACV, [9-(2-hydroxyethoxy)methyl)guanine]) was originally designed as an inhibitor of adenosine deaminases, but in 1977, it was discovered to be an effective antiherpetic drug (Elion et al., 1977). Acyclovir is most active against HSV-1, but its activity against HSV-2 and VZV has also been demonstrated (Schaeffer et al., 1978). Acyclovir is also active against EBV and, at high concentrations, against CMV. Its activity is based on the inhibition of the DNA polymerase, which causes DNA chain termination because the active acyclovir form, the triphosphate, lacks the 3′-hydroxyl group required for DNA chain elongation (Laskin, 1984; Ostrosky-Zeichner and Rex, 2008). The bioavailability of oral acyclovir is relatively poor (15–21%); thus, high doses of this drug are required. It can also be administered in topical form. This drug has an excellent safety profile because acyclovir triphosphate is a much better substrate for the viral polymerase than for the cellular polymerase. Additionally, because the affinity of acyclovir for the viral thymidine kinase is approximately 200-fold greater than that for the cellular thymidine kinase, a higher concentration of its active metabolite is observed in infected cells (Kimberlin, 2018; Das and Hong, 2018). In 2017, studies conducted to determine the effect of acyclovir on breast cancer MCF-7 cells were described (Shaimerdenova et al., 2017). The obtained results demonstrate the suppressive effect of acyclovir on breast cancer cells. Acyclovir treatment decreases the proliferation rate as well as the growth of cells and correlates with upregulation of apoptosis associated with caspase-3. Acyclovir also inhibits the colony formation ability and cell invasion capacity of cancer cells. These results demonstrate the possibility of partial suppression of cancer cell proliferation using this antiviral agent. However, further research is necessary to determine the mechanism of the anticancer activity of acyclovir. The literature also describes an approach based on the phosphorylation of acyclovir by the viral thymidine kinase but not the cellular enzyme (Yao et al., 2013). Phosphorylated acyclovir inhibits cellular DNA synthesis and kills infected cells. It was assumed that phosphorylated acyclovir would be a cytotoxic agent when properly delivered to the cancer cells. To facilitate the targeted delivery of phosphorylated acyclovir to the tumour, lipid/calcium/phosphate nanoparticles with a membrane/core structure were used to encapsulate the phosphorylated drug. The nanoparticles containing phosphorylated acyclovir facilitated its delivery to the tumour, which contributed to the significantly enhanced inhibition of tumour growth without obvious toxicity.
To increase the oral bioavailability of antiviral drugs, a prodrug strategy can be applied. Valaciclovir (VACV, L-valyl ester of acyclovir) is a highly efficient and safe prodrug of acyclovir. It can be dosed orally and is absorbed in the gastrointestinal tract through both a passive transcellular mechanism and an active peptide transporter mechanism. The prodrug is then converted to acyclovir in the liver and intestinal walls by specific enzymes (Weller et al., 1993). The oral bioavailability of valaciclovir is much higher than that of acyclovir, reaching almost 50%. In clinical trials, valaciclovir has a similar antiviral activity and safety profile as acyclovir; therefore, it has superseded acyclovir for the treatment of HSV or VZV infections (O'Brien and Campoli-Richards, 1989; Littler and Zhou, 2007).
Penciclovir (PCV, 9-[4-hydroxy-3-(hydroxymethyl)butyl]guanine), developed in Beecham Pharmaceuticals Laboratories, is an acyclic guanosine analogue. Penciclovir-triphosphate, its active metabolite, competitively inhibits the replicative function of the viral DNA polymerase. Unlike acyclovir, penciclovir is not considered a DNA chain terminator due to the presence of the 3′-OH group in the acyclic part of PCV, which allows DNA chain elongation. Incorporated penciclovir probably distorts the DNA conformation and then induces the suppression of further DNA elongation (Piret and Boivin, 2011). Penciclovir has broad-spectrum antiviral activity against HSV, VZV and even EBV. It is less active than acyclovir, but its longer half-life and higher intracellular concentration compensate for the lower antiviral effect. Phosphorylated penciclovir concentrations can be as much as 200-fold higher than those of phosphorylated acyclovir (Littler and Zhou, 2007; Kimberlin, 2018). The bioavailability of penciclovir upon oral administration is poor, at approximately 5%; therefore, its prodrug famciclovir (FCV, 6-deoxypenciclovir diacetate) was designed and approved for clinical use against HSV and VZV in 1994 (Tyring et al., 1995; Luber and Flaherty, 1996). Studies in mouse models have shown that the main advantage in using famciclovir over using other drugs is its ability to prevent latent HSV-1 infections (Thackray and Field, 1998).
Ganciclovir (GCV, 9-[(1,3-dihydroxy-2-propoxymethyl)]guanine) differs from acyclovir in that it has an extra hydroxymethyl group in the acyclic chain. Due to its highly efficient action against CMV, ganciclovir has been approved for use in the treatment of infections with this virus, which belongs to the so-called beta-herpesvirus group. Ganciclovir, similar to acyclovir, is also active against alpha-herpesviruses such as HSV-1 and HSV-2 and has similar activity against VZV (Kimberlin, 2018). Ganciclovir has been used with some success in treating HHV-6 infections (Nakano et al., 2009) and has also been proven to be effective against the in vitro replication of EBV and HHV-8 (De Clercq, 2007). It has bioavailability in the oral form; less than 10% of the drug is absorbed after oral administration (Jabs et al., 1986). For this reason, ganciclovir prodrugs have been explored. Valganciclovir (VGCV, 9-[(2-hydroxy-1-valyloxymethyl)ethoxymethyl]guanine), which was approved by the FDA in 2001, is the first example of such a prodrug. Valganciclovir is well absorbed after oral administration (over 60%). The addition of a valyl ester group to ganciclovir makes it a good substrate of the two peptide transporters (PEPT1 and PEPT2), which increase its absorption. The ester linkage between the valyl group and ganciclovir is easily hydrolysed by intestinal esterase and hepatic esterase (Sugawara et al., 2000).
Vidarabine (VDR, 9-β-D-arabinofuranosyladenine) is an analogue of adenosine isolated from Streptomyces antibioticus. Vidarabine, unlike previously discussed drugs, does not require viral enzymes at any step of the triphosphorylation process to generate an active metabolite. When phosphorylated by cellular enzymes, vidarabine is in the active triphosphate form. The lack of specificity is responsible for its toxicity. Vidarabine is oncogenic and teratogenic in laboratory animal models. Vidarabine triphosphate acts as a competitive inhibitor of viral and cellular DNA polymerase. It functions as a chain terminator after incorporation into the DNA. Additionally, this metabolite also inhibits other viral and cellular enzymes, such as ribonucleoside reductase and S-adenosylhomocysteine hydrolase, which may also contribute to the antiviral and toxic effects of vidarabine (Aoki, 2015; Theobald, 2016). Vidarabine was initially used as an antiviral drug for the systematic treatment of HSV and VZV infections (De Clercq, 2013b). Vidarabine is used less currently than it was in the past. It is mainly used against cases of acyclovir-resistant herpesviruses. Due to its relative insolubility in aqueous media, vidarabine is mainly administered topically (Littler and Zhou, 2007). A few years ago, it was proposed that vidarabine could be applied as a potent and selective inhibitor of adenylyl cyclase 5 for the treatment of two human diseases: heart failure and cancer. This conclusion was based on the results of animal testing (Iwatsubo et al., 2012; Vatner et al., 2013). Unfortunately, in the following year, findings indicating that VDR is neither a potent nor a selective cyclase 5 inhibitor were published (Seifert, 2014).
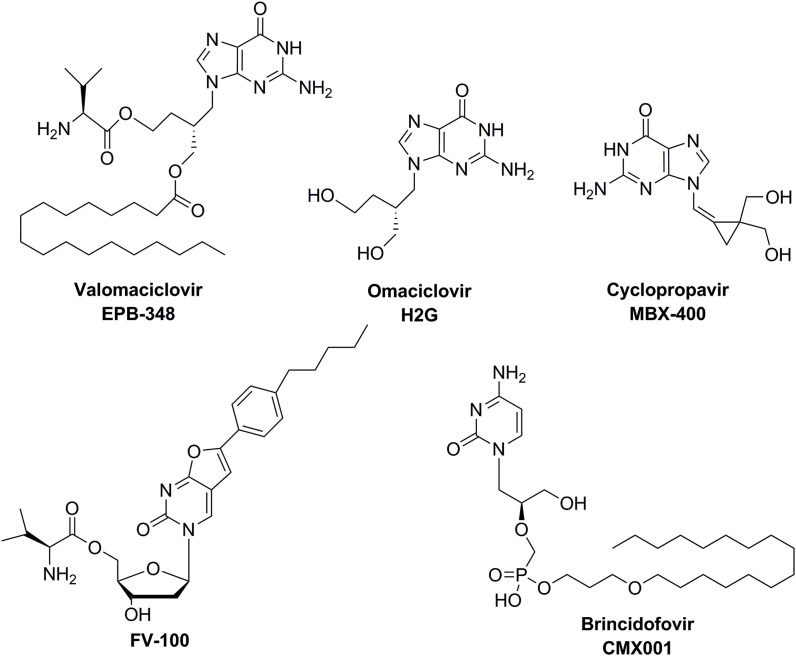
The research and development of a significant number of nucleos(t)ide analogues were terminated in the preclinical assay stage due to the toxicity they induced in animal models. High toxicity was also the reason for the rejection of many compounds during clinical trials. Examples of nucleos(t)ide-based analogues that exhibit high activity against herpesviruses but were not approved as drugs are shown in Fig. 5 and are described below.
Fig. 5.
Additional nucleos(t)ide-based antiviral agents against various herpesviruses.
Valomaciclovir (EPB-348) is a prodrug that has undergone the preliminary stages of clinical trials for the inhibition of viral DNA polymerase. This ester nucleoside analogue is rapidly converted to omaciclovir (H2G) in vivo and subsequently converted by viral enzymes into the phosphorylated form that binds to VZV polymerase. In vitro studies have shown its activity against HSV-1 and VZV (Abele et al., 1991). Valomaciclovir was under phase 2 clinical trials for EBV-infectious mononucleosis (NCT00575185) as well as for the treatment of herpes zoster (NCT00831103).
Cyclopropavir (MBX-400) is another extensively investigated compound. It is a methylenecyclopropane nucleoside analogue structurally related to drugs such as acyclovir, ganciclovir and penciclovir. In vitro studies demonstrated its activity against such herpesviruses as CMV, HHV-6 and HHV-8 (Price and Prichard, 2011). Cyclopropavir was in phase 1 clinical trials to assess its safety and pharmacokinetics (NCT01433835) and (NCT02454699).
Another compound exhibiting strong antiviral activity is FV-100. This compound has a high selectivity for VZV. Unfortunately, its activity was not observed in comparative studies of other herpesviruses (Mcguigan et al., 2007). This drug was tested in a phase 2 clinical trial in comparison with valaciclovir for herpes zoster (NCT00900783) and in a phase 3 clinical trial in comparison with valaciclovir for the prevention of post-herpetic neuralgia (NCT02412917).
Brincidofovir (CMX001), which is a lipid conjugate of cidofovir, seems to be the most promising antiviral compound. In contrast to the latter, brincidofovir is orally available. It is absorbed in the small intestine and transported throughout the body as a phospholipid. It crosses target cell membranes by facilitated and passive diffusion. Additionally, it has a long intracellular half-life (Painter et al., 2012). Brincidofovir presents broad-spectrum antiviral activity against DNA viruses such as herpesviruses, adenoviruses and poxviruses (Price and Prichard, 2011; Florescu et al., 2012; Quenelle et al., 2010). It was studied for safety and efficacy against adenovirus (AdV) infection (phase 3 clinical trials; NCT02087306) and against serious diseases or conditions caused by DNA viruses (phase 3; NCT01143181). Another clinical trial (phase 2) revealed that patients taking brincidofovir were resistant to CMV infection (NCT942305). Unfortunately, the results of the phase 3 trial (NCT01769170) showed that the effect was only observed during active drug administration and disappeared immediately after treatment. Moreover, a significant number of patients developed diarrhoea. As a result, two other clinical trials for CMV prevention (NCT02439970 and NCT02439957) were stopped.
4. Nucleoside antimetabolites - approved antineoplastic drugs with potential antiviral/antibacterial activity
Nucleoside antimetabolites are used against a broad range of human cancers, including leukaemias, lymphomas, and pancreatic, breast, bladder, ovarian, colon or kidney cancer. By mimicking the physiological role of their natural counterparts, they interfere with cellular metabolism, incorporate into DNA or RNA, inhibit enzymes (essential polymerases, DNA methyltransferases, kinases, phosphorylases, thymidylate synthase or ribonucleotide reductase) and thus inhibit cell division and viral replication (Jordheim et al., 2013). Among the major players are purine analogues (including the commonly used cladribine, approved in 1992; fludarabine, approved in 1991; second-generation clofarabine, approved in 2004; and nelarabine, approved in 2005) and pyrimidine analogues (first approved in cytarabine in 1969, gemcitabine in 1996, azacytidine in 2004, decitabine in 2006, and floxuridine in 1970), which have had important roles in several cancer treatments (Parker, 2009). Some of the cytotoxic nucleoside analogues have recently proven their broad-spectrum antiviral activity towards life-threatening viruses (Ianevski et al., 2018, 2019). Among them, the cytidine analogue gemcitabine was reported to be 6th on the list of broad-spectrum antivirals that show in vitro activities (Ianevski et al., 2019). Additionally, it was recently reported that several nucleoside analogues clinically approved as antivirals or antineoplastic agents also show antibacterial activity (Thomson and Lamont, 2019). Examples of such drugs include gemcitabine, zidovudine, 5-fluorouracil, floxuridine, idoxuridine and thiopurines. The application limitations of some nucleoside analogues as antibiotics could be connected with their side effects and toxicity (e.g., myelosuppression or pulmonary toxicity). However, the concentrations of nucleoside analogues that inhibited the growth of bacteria were lower than those used for the treatment of cancer patients, which can reduce the problem of toxicity (Jordheim et al., 2012). The antibiotic potency of nucleoside analogues could be useful, especially in hospital settings, to treat multi-drug-resistant bacteria.
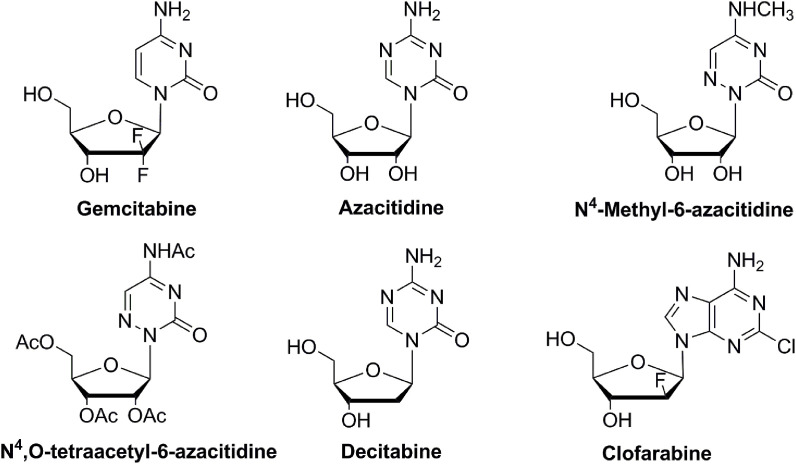
In this chapter, approved antineoplastic drugs from the nucleoside antimetabolite group that have shown potency as broad-spectrum antiviral agents and/or antibacterial agents are discussed (Fig. 6 ).
Fig. 6.
Structures of the nucleoside antimetabolites with potential antiviral activity.
Gemcitabine (dFdC; dFdCyd) is an approved antineoplastic drug (initially approved by the FDA in 1996; brand name Gemzar) used for the treatment of different cancers (e.g., pancreatic, ovarian, lung and breast and bladder cancer) (Hertel et al., 1990; Cerqueira et al., 2007). It is a prodrug that is converted to monophosphate metabolites by deoxycytidine kinase and then to active diphosphate and triphosphate metabolites by nucleoside mono- and diphosphate kinases, respectively. The diphosphate metabolite acts as an inhibitor of ribonucleotide reductase, which is the catalyst for deoxyribonucleotide generation (for DNA synthesis and repair). The triphosphate metabolite in turn competes with natural deoxycytidine-5-triphosphate to incorporate into replicating DNA (Cerqueira et al., 2007). Gemzar in combination with cisplatin was approved in 1998 for the treatment of locally advanced or metastatic non-small cell lung cancer, and Gemzar in combination with paclitaxel was approved as the first-line therapy for women battling metastatic breast cancer. Gemzar demonstrates dose-dependent synergistic activity with cisplatin. In the treatment of advanced ovarian cancer (at least 6 months after completion of platinum-based therapy), gemcitabine is used in combination with carboplatin. Another study showed that co-treatment with gemcitabine and zidovudine re-sensitized gemcitabine-resistant pancreatic cancer by inhibiting the key signalling pathway, Akt-GSK3β-Snail1, in the resistant cells (Namba et al., 2015). Other reports from phase 2 clinical trials have shown that combining brivudine with gemcitabine or cisplatin enhanced their efficacy as a pancreatic cancer therapy (Heinrich et al., 2011). Recently (2018), the FDA approved the premixed, ready-to-infuse formulation called Infugem. Several (13) generic versions of Gemzar have also been approved.
Recently, experimental data on the antiviral activity of gemcitabine have been widely reported (Shin et al., 2018; Ianevski et al., 2019). The broad range of viruses against which gemcitabine has shown activity includes HIV-1 (Rawson et al., 2013; Clouser et al., 2010, 2012), murine leukaemia virus (MuLV) (Clouser et al., 2012), HIV-2 (Beach et al., 2014), ZIKV (Kuivanen et al., 2017), enteroviruses such as poliovirus (Kang et al., 2015; Zhang et al., 2017), rhinoviruses (Song et al., 2017), HCV (Beran et al., 2012), coronaviruses (Dyall et al., 2014), Sindbis virus (SINV), HSV-1 and FLUAV (Denisova et al., 2012). The synergistic effect of gemcitabine combined with low doses of other nucleoside analogues was also reported. It is applied in combination with ribavirin for the treatment of enteroviruses or with decitabine for the treatment of HIV (Kang et al., 2015; Clouser et al., 2010). In most cases, gemcitabine inhibits viruses at low, non-cytotoxic concentrations (Denisova et al., 2012; Kuivanen et al., 2017). Depending on the virus, gemcitabine was shown to be an inhibitor of viral replication, proliferation, RNA and protein synthesis, or production. The gemcitabine antiviral effect on enteroviruses was proposed to be based on two actions. It can be directly incorporated into newly synthesized viral RNA during the polymerization process. Gemcitabine preferentially incorporates into viral RNA since the RNA replication process in viruses is more active than cellular DNA or RNA synthesis. It is also possible that gemcitabine can block the RNA polymerase by binding to the nucleotide-binding regions. Another possibility is that the viral ribonucleotide reductase is inhibited, resulting in an increased mutation rate and loss of viral proliferation capability (Kang et al., 2015). It was postulated that the inhibition of RNA replication might be related to the limited amount of nucleoside available (Song et al., 2017). As a cytidine analogue, gemcitabine was reported to inhibit the salvage pathway of the pyrimidine biosynthesis. Additionally, treatment with gemcitabine activates the expression of several IFN-stimulated genes (including CXCL10, IRF7, IRF9, IFIT1 or DDX58), the major effectors in innate immunity (Lee et al., 2017).
Gemcitabine has also shown antibacterial activity against gram-positive bacteria, such as Enterococcus, Listeria, Bacillus, and Staphylococcus, including multi-drug-resistant strains of Staphylococcus aureus (Thomson and Lamont, 2019; Jordheim et al., 2012; Sandrini et al., 2007). Unfortunately, one study revealed that the treated strains developed resistance to gemcitabine. Such a phenomenon could in turn be overcome by the combination of gemcitabine and gentamicin, which showed synergistic activity and reduced the rate of resistance development (Jordheim et al., 2012). Gemcitabine did not show activity against gram-negative bacteria.
Azacitidine (5-AC; 5-AZC; AZA-CR; 5-azacytidine; Vidaza) is a prodrug and antimetabolite of cytidine that has been approved by the FDA in 2004 for the treatment of all subtypes of myelodysplastic syndrome (MDS). To date, azacytidine has also been approved for the treatment of acute myeloid leukaemia (AML) patients with 20–30% bone marrow (BM) blasts and with >30% BM blasts (Agrawal et al., 2018). Its antineoplastic activity is based on two mechanisms of action: hypomethylation of DNA and direct toxification of abnormal haematopoietic cells in the BM. It is most toxic to cells in the S-phase of the cell cycle (Kaminskas et al., 2005). After incorporation into DNA, azacytosine substitutes for cytosine, forming azacytosine-guanine dinucleotides, which are recognized by DNA methyltransferase as a natural substrate and inhibit the enzyme (Stresemann and Lyko, 2008; Agrawal et al., 2018). This mechanism results in a reduction in DNA methylation. Hypomethylating agents—azacitidine and decitabine—were reported to influence tumour interactions with the host immune system. They activate endogenous retroviral elements that are normally epigenetically silenced (Wolff et al., 2017).
Experimental studies have shown that azacitidine is a potent, broad-spectrum antiviral agent. The range of viruses against which it shows activity includes AdV (Alexeeva et al., 2001, 2015), human metapneumovirus (HMPV) (Bösl et al., 2019), HIV-1 (Dapp et al., 2009; Rawson et al., 2016a), HIV-2 (Beach et al., 2014), Rift Valley fever virus (RVFV) (Ianevski et al., 2018, 2019), human T-lymphotropic virus (HTLV-1) (Diamantopoulos et al., 2012), HSV-1, and FLUAV (Ianevski et al., 2018). A study of azacytidine activity against HIV-1 and HIV-2 revealed that it primarily targets reverse transcription (in the form of 5-azacytidine-triphosphate or 5-aza-2′-deoxycytidine triphosphate). An increase in the HIV-1 mutation rate caused by incorporating azacytidine into viral RNA was observed (Dapp et al., 2009). An additional study indicated that the mutagenesis of HIV-1 was enhanced after the reduction of 5-azacytidine to 5-aza-2′-deoxycytidine, which led to G-to-C hypermutation (Rawson et al., 2016a). A comparison of azacytidine activity towards HIV-1 and HIV-2 revealed better efficacy towards HIV-2 (EC50 values of 20.2 and 14.5 μM, respectively) (Beach et al., 2014). The combination of 5-azacytidine with low concentrations of ribonucleotide reductase inhibitors (e.g., resveratrol) had a synergistic effect and significantly reduced the infectivity of HIV-1. The synergism was explained by the reduced accumulation of reverse transcription products rather than increased viral mutagenesis (Rawson et al., 2016b). A recent study on human adenoviruses revealed that azacytidine itself was an effective antiviral agent over a wide range of concentrations but its derivatives showed even better results, namely, N4-methyl-6-azacytidine and N4,O-tetraacetyl-6-azacytidine, for which high selectivity against AdV and low cytotoxicity were observed (Alexeeva et al., 2015).
Decitabine (DAC; 5-aza-2′-deoxycytidine; Dacogen; Demylocan), another antineoplastic antimetabolite, is a cytidine analogue. This hypomethylating agent was approved by the FDA in 2006 for the treatment of multiple types of myelodysplastic syndrome. It promotes cytotoxic DNA hypomethylation and cell death in rapidly dividing cells by disrupting DNA synthesis. Similar to azacytidine, decitabine also induces immune responses and sensitizes tumours to checkpoint inhibition (Wolff et al., 2017). Additionally, it was shown that in muscle-invasive bladder cancer cells, decitabine treatment (at low non-cytotoxic doses) restored NOTCH1 expression and promoted IL-6 release to induce CK5 differentiation (Ramakrishnan et al., 2017).
The antiviral activity of decitabine has been shown mostly in HIV treatment. Similar to the previously described synergistic effect of azacytidine with resveratrol, the combination of decitabine and resveratrol significantly reduced the levels of HIV-1 reverse transcription products (Rawson et al., 2016b). Another study indicated that the combination of gemcitabine and decitabine at concentrations much lower than those used in cancer treatment synergistically lowered HIV-1 infectivity by 73% and significantly increased the mutation frequency (Clouser et al., 2010).
Clofarabine (CAFdA; Cl-F-Ara-A; Clolar; Evoltra; FDA approval in 2004) is an antineoplastic agent used to treat lymphoblastic leukaemia, specifically acute lymphoblastic leukaemia in paediatric patients aged 1–21 whose disease has relapsed or become refractory after at least two prior treatment regimens. The drug acts as an antimetabolite that interferes with DNA replication. Clofarabine inhibits ribonucleotide reductase, causes termination of DNA chain elongation, and inhibits DNA polymerases. Additionally, it disrupts mitochondrial membrane integrity, which results in the release of apoptosis-inducing factors, pro-apoptotic proteins, and cytochrome C, leading to the activation of programmed cell death pathways.
Clofarabine was reported to be a potent antiretroviral agent. It has shown threefold higher activity against HIV-2 than against HIV-1 (Beach et al., 2014). Further study on the anti-HIV-1 activity of clofarabine revealed its dual inhibitory function in virus replication. It limits the deoxyribonucleoside triphosphate substrates for the synthesis of viral DNA and directly inhibits the DNA polymerase activity of HIV-1 reverse transcriptase (Daly et al., 2016).
5. Concluding remarks
Nucleoside analogues were first studied as antimetabolites, and some of them proved to be antitumour agents. Many of these antitumour agents showed antiviral activity; however, the development of a significant number of nucleos(t)ide-based analogues was terminated during the preclinical assay stages due to the toxicity they induced in animal models.
Long-term exposure to antiviral drugs leads to the emergence of drug resistance. In addition, in some cases, limitations of standard treatment result from significant renal toxic effects. Therefore, there is a constant need for the development of novel therapeutic agents. Currently, more than 100 active antiviral drug candidates are in advanced preclinical or clinical trials. Most of these clinical-stage drug candidates are being tested for activity against HIV, HBV and HCV.
Even though more than 90 antiviral drugs are currently approved for the treatment of viral infections, many of them are suitable for use only with a single virus. New antiviral drugs with activity against multiple viral types are being sought, and many of these compounds are subjects of advanced clinical trials. Moreover, experimental data open the possibility of repurposing broad-spectrum antimetabolites to other viral infections. Because these drugs have already been approved, such an application could save the time and money that are needed to prove their safety. It is possible that a compound that has already been classified as a drug against one virus may be suitable for the treatment of other viral infections. This approach is particularly important for candidates for the treatment of deadly viral infections, such as Ebola virus (EBOV). In this case, the safety threshold would be based on different criteria from those that are currently applied for drugs used to control chronic infections such as HIV and HBV.
References
- Abele G., Cox S., Bergman S., Lindborg B., Vissgarden A., Karlstrom A., Harmenberg J., Wahren B. Antiviral activity against VZV and HSV type 1 and type 2 of the (+) and (-) enantiomers of (R,S)-9-[4-hydroxy-2-(hydroxymethyl)butyl]guanine, in comparison to other closely related acyclic nucleosides. Antivir. Chem. Chemother. 1991;2:163–169. doi: 10.1177/095632029100200306. [DOI] [Google Scholar]
- Agrawal K., Das V., Vyas P., Hajdúch M. Nucleosidic DNA demethylating epigenetic drugs – a comprehensive review from discovery to clinic. Pharmacol. Ther. 2018;188:45–79. doi: 10.1016/j.pharmthera.2018.02.006. [DOI] [PubMed] [Google Scholar]
- Alexeeva I., Dyachenko N., Nosach L., Zhovnovataya V., Rybalko S., Lozitskaya R., Fedchuk A., Lozitsky V., Gridina T., Shalamay A., Palchikovskaja L., Povnitsa O. 6-Azacytidine – compound with wide spectrum of antiviral activity. Nucleosides Nucleotides Nucleic Acids. 2001;20:1147–1152. doi: 10.1081/NCN-100002508. [DOI] [PubMed] [Google Scholar]
- Alexeeva I., Nosach L., Palchykovska L., Usenko L., Povnitsa O. Synthesis and comparative study of anti-adenoviral activity of 6-azacytidine and its analogues. Nucleosides Nucleotides Nucleic Acids. 2015;34:565–578. doi: 10.1080/15257770.2015.1034363. [DOI] [PubMed] [Google Scholar]
- Andrei G., Sienaert R., McGuigan C., De Clercq E., Baizarini J., Snoeck R. Susceptibilities of several clinical varicella-zoster virus (VZV) isolates and drug-resistant VZV strains to bicyclic furano pyrimidine nucleosides. Antimicrob. Agents Chemother. 2005;49:1081–1086. doi: 10.1128/AAC.49.3.1081-1086.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrei G., Topalis D., Fiten P., McGuigan C., Balzarini J., Opdenakker G., Snoeck R. In vitro-selected drug-resistant varicella-zoster virus mutants in the thymidine kinase and DNA polymerase genes yield novel phenotype-genotype Associations and highlight differences between antiherpesvirus drugs. J. Virol. 2012;86:2641–2652. doi: 10.1128/jvi.06620-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aoki F.Y. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. eighth ed. 2015. Antivirals against herpes viruses. [Google Scholar]
- Bauer L., Lyoo H., van der Schaar H.M., Strating J.R., van Kuppeveld F.J. Direct-acting antivirals and host-targeting strategies to combat enterovirus infections. Curr. Opin. Virol. 2017;24:1–8. doi: 10.1016/j.coviro.2017.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beach L.B., Rawson J.M., Kim B., Patterson S.E., Mansky L.M. Novel inhibitors of human immunodeficiency virus type 2 infectivity. J. Gen. Virol. 2014;95:2778–2783. doi: 10.1099/vir.0.069864-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beran R.K.F., Sharma R., Corsa A.C., Tian Y., Golde J., Lundgaard G., Delaney IV W.E., Zhong W., Greenstein A.E. Cellular growth kinetics distinguish a cyclophilin inhibitor from an HSP90 inhibitor as a selective inhibitor of hepatitis C virus. PLoS One. 2012;7 doi: 10.1371/journal.pone.0030286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bösl K., Ianevski A., Than T.T., Andersen P.I., Kuivanen S., Teppor M., Zusinaite E., Dumpis U., Vitkauskiene A., Cox R.J., Kallio-Kokko H., Bergqvist A., Tenson T., Oksenych V., Bjørås M., Anthonsen M.W., Shum D., Kaarbø M., Vapalahti O., Windisch M.P., Superti-Furga G., Snijder B., Kainov D., Kandasamy R.K. Critical nodes of virus-host interaction revealed through an integrated network analysis. 2019. bioRxiv 1–23. [DOI] [PMC free article] [PubMed]
- Bullard-Feibelman K.M., Govero J., Zhu Z., Salazar V., Veselinovic M., Diamond M.S., Geiss B.J. The FDA-approved drug sofosbuvir inhibits Zika virus infection. Antivir. Res. 2017;137:134–140. doi: 10.1016/j.antiviral.2016.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burness C.B., Duggan S.T. Trifluridine/tipiracil: a review in metastatic colorectal cancer. Drugs. 2016;76:1393–1402. doi: 10.1007/s40265-016-0633-9. [DOI] [PubMed] [Google Scholar]
- Cano-Soldado P., Pastor-Anglada M. Transporters that translocate nucleosides and structural similar drugs: structural requirements for substrate recognition. Med. Res. Rev. 2012;32:428–457. doi: 10.1002/med.20221. [DOI] [PubMed] [Google Scholar]
- Cerqueira N.M.F.S.A., Fernandes P.A., Ramos M.J. Understanding ribonucleotide reductase inactivation by gemcitabine. Chem. Eur J. 2007;13:8507–8515. doi: 10.1002/chem.200700260. [DOI] [PubMed] [Google Scholar]
- Chaudhuri S., Symons J.A., Deval J. Innovation and trends in the development and approval of antiviral medicines: 1987–2017 and beyond. Antivir. Res. 2018;155:76–88. doi: 10.1016/j.antiviral.2018.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clouser C.L., Holtz C.M., Mullett M., Crankshaw D.L., Briggs J.E., O'Sullivan M.G., Patterson S.E., Mansky L.M. Activity of a novel combined antiretroviral therapy of gemcitabine and decitabine in a mouse model for HIV-1. Antimicrob. Agents Chemother. 2012;56:1942–1948. doi: 10.1128/aac.06161-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clouser C.L., Patterson S.E., Mansky L.M. Exploiting drug repositioning for discovery of a novel HIV combination therapy. J. Virol. 2010;84:9301–9309. doi: 10.1128/jvi.01006-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly M.B., Roth M.E., Bonnac L., Maldonado J.O., Xie J., Clouser C.L., Patterson S.E., Kim B., Mansky L.M. Dual anti-HIV mechanism of clofarabine. Retrovirology. 2016;13:1–12. doi: 10.1186/s12977-016-0254-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dapp M.J., Clouser C.L., Patterson S., Mansky L.M. 5-Azacytidine can induce lethal mutagenesis in human immunodeficiency virus type 1. J. Virol. 2009;83:11950–11958. doi: 10.1128/jvi.01406-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das D., Hong J. Elsevier Inc; 2018. Herpesvirus Polymerase Inhibitors, Viral Polymerases. [Google Scholar]
- Das P., Delost M.D., Qureshi M.H., Smith D.T., Njardarson J.T. A survey of the structures of US FDA approved combination drugs. J. Med. Chem. 2019;62:4265–4311. doi: 10.1021/acs.jmedchem.8b01610. [DOI] [PubMed] [Google Scholar]
- De Clercq E., Li G. Approved antiviral drugs over the past 50 years. Clin. Microbiol. Rev. 2016;29:695–747. doi: 10.1128/CMR.00102-15. Address. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Clercq E. Role of tenofovir alafenamide (TAF) in the treatment and prophylaxis of HIV and HBV infections. Biochem. Pharmacol. 2018;153:2–11. doi: 10.1016/j.bcp.2017.11.023. [DOI] [PubMed] [Google Scholar]
- De Clercq E. Highlights in antiviral drug research: antivirals at the horizon. Med. Res. Rev. 2013;33:1215–1248. doi: 10.1002/med. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Clercq E. Selective anti-herpesvirus agents. Antivir. Chem. Chemother. 2013;23:93–101. doi: 10.3851/IMP2533. [DOI] [PubMed] [Google Scholar]
- De Clercq E. Viruses and viral diseases. Compr. Med. Chem. II. 2007:253–293. doi: 10.1016/b0-08-045044-x/00211-x. [DOI] [Google Scholar]
- De Clercq E. Discovery and development of BVDU (brivudin) as a therapeutic for the treatment of herpes zoster. Biochem. Pharmacol. 2004;68:2301–2315. doi: 10.1016/j.bcp.2004.07.039. [DOI] [PubMed] [Google Scholar]
- De Freitas C.S., Higa L.M., Sacramento C.Q., Ferreira A.C., Reis P.A., Delvecchio R., Monteiro F.L., Barbosa-Lima G., James Westgarth H., Vieira Y.R., Mattos M., Rocha N., Hoelz L.V.B., Leme R.P.P., Bastos M.M., Rodrigues G.O.L., Lopes C.E.M., Queiroz-Junior C.M., Lima C.X., Costa V.V., Teixeira M.M., Bozza F.A., Bozza P.T., Boechat N., Tanuri A., Souza T.M.L. Yellow fever virus is susceptible to sofosbuvir both in vitro and in vivo. PLoS Neglected Trop. Dis. 2019;13 doi: 10.1371/journal.pntd.0007072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denisova O.V., Kakkola L., Feng L., Stenman J., Nagaraj A., Lampe J., Yadav B., Aittokallio T., Kaukinen P., Ahola T., Kuivanen S., Vapalahti O., Kantele A., Tynell J., Julkunen I., Kallio-Kokko H., Paavilainen H., Hukkanen V., Elliott R.M., De Brabander J.K., Saelens X., Kainov D.E. Obatoclax, saliphenylhalamide, and gemcitabine inhibit influenza A virus infection. J. Biol. Chem. 2012;287:35324–35332. doi: 10.1074/jbc.M112.392142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamantopoulos P.T., Michael M., Benopoulou O., Bazanis E., Tzeletas G., Meletis J., Vayopoulos G., Viniou N.A. Antiretroviral activity of 5-azacytidine during treatment of a HTLV-1 positive myelodysplastic syndrome with autoimmune manifestations. Virol. J. 2012;9:1. doi: 10.1186/1743-422X-9-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyall J., Coleman C.M., Hart B.J., Venkataraman T., Holbrook M.R., Kindrachuk J., Johnson R.F., Olinger G.G., Jahrling P.B., Laidlaw M., Johansen L.M., Lear-Rooney C.M., Glass P.J., Hensley L.E., Frieman M.B. Repurposing of clinically developed drugs for treatment of Middle East respiratory syndrome coronavirus infection. Antimicrob. Agents Chemother. 2014;58:4885–4893. doi: 10.1128/aac.03036-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elion G.B., Furman P.A., Fyfe J.A., De Miranda P., Beauchampt L., Schaeffert H.J. Selectivity of action of an antiherpetic agent, 9-(2-hydroxyethoxymethyl)guanine (antiviral chemotherapy/virus-specified thymidine kinase/herpes simplex virus/virus-specified DNA polymerase/acycloguanosine triphosphate) Med. Sci. 1977;74:5716–5720. doi: 10.1073/pnas.74.12.5716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essmann V., Wildenhoff K.E. Antiviral treatment of VaricellaZoster and herpes simplex. Lancet. 1980;315:1337–1339. doi: 10.1016/S0140-6736(80)91790-0. [DOI] [Google Scholar]
- Ferreira A.C., Reis P.A., de Freitas C.S., Sacramento C.Q., Hoelz L.V.B., Bastos M.M., Mattos M., Rocha N., de Azevedo Quintanilha I.G., da Silva Gouveia Pedrosa C., Souza L.R.Q., Loiola E.C., Trindade P., Vieira Y.R., Barbosa-Lima G., de Castro Faria Neto H.C., Boechat N., Rehen S.K., Brüning K., Bozza F.A., Bozza P.T., Souza T.M.L. Beyond members of the Flaviviridae family, sofosbuvir also inhibits chikungunya virus replication. Antimicrob. Agents Chemother. 2019;63 doi: 10.1128/AAC.01389-18. e01389-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Florescu D.F., Pergam S.A., Neely M.N., Qiu F., Johnston C., Way S.S., Sande J., Lewinsohn D.A., Guzman-Cottrill J.A., Graham M.L., Papanicolaou G., Kurtzberg J., Rigdon J., Painter W., Mommeja-Marin H., Lanier R., Anderson M., van der Horst C. Safety and efficacy of CMX001 as salvage therapy for severe adenovirus infections in immunocompromised patients. Biol. Blood Marrow Transplant. 2012;18:731–738. doi: 10.1016/j.bbmt.2011.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao L.J., De Jonghe S., Daelemans D., Herdewijn P. L-Aspartic and l-glutamic acid ester-based ProTides of anticancer nucleosides: synthesis and antitumoral evaluation. Bioorg. Med. Chem. Lett. 2016;26:2142–2146. doi: 10.1016/j.bmcl.2016.03.076. [DOI] [PubMed] [Google Scholar]
- Heinrich J.C., Tuukkanen A., Schroeder M., Fahrig T., Fahrig R. RP101 (Brivudine) binds to heat shock protein HSP27 (HSPB1) and enhances survival in animals and pancreatic cancer patients. J. Cancer Res. Clin. Oncol. 2011;137:1349–1361. doi: 10.1007/s00432-011-1005-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hertel L.W., Boder G.B., Kroin J.S., Rinzel S.M., Poore G. a, Todd G.C., Grindey G.B. Evaluation of the antitumor activity of gemcitabine (2 ′ , 2 ′ evaluation of the antitumor activity of gemcitabine. Cancer Res. 1990;50:4417–4422. [PubMed] [Google Scholar]
- Ianevski A., Andersen P.I., Merits A., Bjørås M., Kainov D. Expanding the activity spectrum of antiviral agents. Drug Discov. Today. 2019;24:1224–1228. doi: 10.1016/j.drudis.2019.04.006. [DOI] [PubMed] [Google Scholar]
- Ianevski A., Zusinaite E., Kuivanen S., Strand M., Lysvand H., Teppor M., Kakkola L., Paavilainen H., Laajala M., Kallio-Kokko H., Valkonen M., Kantele A., Telling K., Lutsar I., Letjuka P., Metelitsa N., Oksenych V., Bjørås M., Nordbø S.A., Dumpis U., Vitkauskiene A., Öhrmalm C., Bondeson K., Bergqvist A., Aittokallio T., Cox R.J., Evander M., Hukkanen V., Marjomaki V., Julkunen I., Vapalahti O., Tenson T., Merits A., Kainov D. Novel activities of safe-in-human broad-spectrum antiviral agents. Antivir. Res. 2018;154:174–182. doi: 10.1016/j.antiviral.2018.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwatsubo K., Bravo C., Uechi M., Baljinnyam E., Nakamura T., Umemura M., Lai L., Gao S., Yan L., Zhao X., Park M., Qiu H., Okumura S., Iwatsubo M., Vatner D.E., Vatner S.F., Ishikawa Y. Prevention of heart failure in mice by an antiviral agent that inhibits type 5 cardiac adenylyl cyclase. Am. J. Physiol. Cell Physiol. 2012;302:H2622–H2628. doi: 10.1152/ajpheart.00190.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jabs D.A., Wingard J.R., de Bustros S., de Miranda P., Saral R., Santos G.W. BW B759U for cytomegalovirus retinitis: intraocular drug penetration. Arch. Ophthalmol. 1986;104:1436–1437. doi: 10.1001/archopht.1986.01050220030009. [DOI] [PubMed] [Google Scholar]
- Jordheim L.P., Ben Larbi S., Fendrich O., Ducrot C., Bergeron E., Dumontet C., Freney J., Doléans-Jordheim A. Gemcitabine is active against clinical multiresistant Staphylococcus aureus strains and is synergistic with gentamicin. Int. J. Antimicrob. Agents. 2012;39:444–447. doi: 10.1016/j.ijantimicag.2012.01.019. [DOI] [PubMed] [Google Scholar]
- Jordheim L.P., Durantel D., Zoulim F., Dumontet C. Advances in the development of nucleoside and nucleotide analogues for cancer and viral diseases. Nat. Rev. Drug Discov. 2013;12:447–464. doi: 10.1038/nrd4010. [DOI] [PubMed] [Google Scholar]
- Julander J.G., Siddharthan V., Evans J., Taylor R., Tolbert K., Apuli C., Stewart J., Collins P., Gebre M., Neilson S., Van Wettere A., Lee Y.M., Sheridan W.P., Morrey J.D., Babu Y.S. Efficacy of the broad-spectrum antiviral compound BCX4430 against Zika virus in cell culture and in a mouse model. Antivir. Res. 2017;137:14–22. doi: 10.1016/j.antiviral.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaminskas E., Farrell A.T., Wang Y.-Ch, Sridhara R., Pazdur R. FDA drug approval summary: azacitidine (5-azacytidine, Vidaza) for injectable suspension. The Oncologist. 2005;10:176–182. doi: 10.1634/theoncologist.10-3-176. [DOI] [PubMed] [Google Scholar]
- Kang H., Kim C., Kim D.E., Song J.H., Choi M., Choi K., Kang M., Lee K., Kim H.S., Shin J.S., Kim J., Han S.B., Lee M.Y., Lee S.U., Lee C.K., Kim M., Ko H.J., Van Kuppeveld F.J.M., Cho S. Synergistic antiviral activity of gemcitabine and ribavirin against enteroviruses. Antivir. Res. 2015;124:1–10. doi: 10.1016/j.antiviral.2015.10.011. [DOI] [PubMed] [Google Scholar]
- Kimberlin D.W. Fifth. ed. 2018. Antiviral Agents. Principles and Practice of Pediatric Infectious Diseases. [Google Scholar]
- Kuivanen S., Bespalov M.M., Nandania J., Ianevski A., Velagapudi V., De Brabander J.K., Kainov D.E., Vapalahti O. Obatoclax, saliphenylhalamide and gemcitabine inhibit Zika virus infection in vitro and differentially affect cellular signaling, transcription and metabolism. Antivir. Res. 2017;139:117–128. doi: 10.1016/j.antiviral.2016.12.022. [DOI] [PubMed] [Google Scholar]
- Lahmer T., Hoffmann D., Heemann U., Küchle C., Frank H. Epstein-Barr virus encephalitis after kidney transplantation and successful treatment with brivudine. Transpl. Int. 2010;23:e24–e25. doi: 10.1111/j.1432-2277.2009.01045.x. [DOI] [PubMed] [Google Scholar]
- Lam A.M., Espiritu C., Bansal S., Micolochick Steuer H.M., Niu C., Zennou V., Keilman M., Zhu Y., Lan S., Otto M.J., Furman P.A. Genotype and subtype profiling of PSI-7977 as a nucleotide inhibitor of hepatitis C virus. Antimicrob. Agents Chemother. 2012;56:3359–3368. doi: 10.1128/aac.00054-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laskin O.L. Acyclovir: pharmacology and clinical experience. Arch. Intern. Med. 1984;144:1241–1246. doi: 10.1001/archinte.1984.00350180181025. [DOI] [PubMed] [Google Scholar]
- Lee K., Kim D.-E., Jang K.-S., Kim S.-J., Cho S., Kim C. Gemcitabine, a broad-spectrum antiviral drug, suppresses enterovirus infections through innate immunity induced by the inhibition of pyrimidine biosynthesis and nucleotide depletion. Oncotarget. 2017;8:115315–115325. doi: 10.18632/oncotarget.23258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leoni M.C., Ustianowski A., Farooq H., Arends J.E. HIV, HCV and HBV: a review of parallels and differences. Infect. Dis. Ther. 2018;7:407–419. doi: 10.1007/s40121-018-0210-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J.C., Smith M.C., Pagano J.S. Comparative efficacy and selectivity of some nucleoside analogs against Epstein-Barr virus. Antimicrob. Agents Chemother. 1985;27:971–973. doi: 10.1128/AAC.27.6.971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littler E., Zhou X.-X. Deoxyribonucleic acid viruses: antivirals for herpesviruses and hepatitis B virus. Compr. Med. Chem. II. 2007:295–327. doi: 10.1016/b0-08-045044-x/00212-1. [DOI] [Google Scholar]
- Liu L.Z., Sun J., Hou J., Chan H.L.Y. Improvements in the management of chronic hepatitis B virus infection. Expert Rev. Gastroenterol. 2018;12:1153–1166. doi: 10.1080/17474124.2018.1530986. [DOI] [PubMed] [Google Scholar]
- Looker K.J., Magaret A.S., May M.T., Turner K.M.E., Vickerman P., Gottlieb S.L., Newman L.M. Global and regional estimates of prevalent and incident herpes simplex virus type 1 infections in 2012. PLoS One. 2015;10:1–17. doi: 10.1371/journal.pone.0140765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luber A.D., Flaherty J.F. Famciclovir for treatment of herpesvirus infections. Ann. Pharmacother. 1996;30:978–985. doi: 10.1177/106002809603000913. [DOI] [PubMed] [Google Scholar]
- Luczkowiak J., Álvarez M., Sebastián-Martín A., Menéndez-Arias L. DNA-dependent DNA polymerases as drug targets in herpesviruses and poxviruses, viral polymerases. 2019.
- Matsuoka K., Nakagawa F., Kobunai T., Takechi T. Trifluridine/tipiracil overcomes the resistance of human gastric 5-fluorouracil-refractory cells with high thymidylate synthase expression. Oncotarget. 2018;9:13438–13450. doi: 10.18632/oncotarget.24412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcguigan C., Pathirana R.N., Migliore M., Adak R., Luoni G., Jones A.T., Díez-Torrubia A., Camarasa M.J., Velázquez S., Henson G., Verbeken E., Sienaert R., Naesens L., Snoeck R., Andrei G., Balzarini J. Preclinical development of bicyclic nucleoside analogues as potent and selective inhibitors of varicella zoster virus. J. Antimicrob. Chemother. 2007;60:1316–1330. doi: 10.1093/jac/dkm376. [DOI] [PubMed] [Google Scholar]
- Menéndez-Arias L., Álvarez M., Pacheco B. Nucleoside/nucleotide analog inhibitors of hepatitis B virus polymerase: mechanism of action and resistance. Curr. Opin. Virol. 2014;8:1–9. doi: 10.1016/j.coviro.2014.04.005. [DOI] [PubMed] [Google Scholar]
- Mesci P., Macia A., Moore S.M., Shiryaev S.A., Pinto A., Huang C.T., Tejwani L., Fernandes I.R., Suarez N.A., Kolar M.J., Montefusco S., Rosenberg S.C., Herai R.H., Cugola F.R., Russo F.B., Sheets N., Saghatelian A., Shresta S., Momper J.D., Siqueira-Neto J.L., Corbett K.D., Beltrão-Braga P.C.B., Terskikh A.V., Muotri A.R. Blocking Zika virus vertical transmission. Sci. Rep. 2018;8:1–13. doi: 10.1038/s41598-018-19526-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murakami E., Tolstykh T., Bao H., Niu C., Micolochick Steuer H.M., Bao D., Chang W., Espiritu C., Bansal S., Lam A.M., Otto M.J., Sofia M.J., Furman P.A. Mechanism of activation of PSI-7851 and its diastereoisomer PSI-7977. J. Biol. Chem. 2010;285:34337–34347. doi: 10.1074/jbc.M110.161802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakano K., Nishinaka K., Tanaka T., Ohshima A., Sugimoto N., Isegawa Y. Detection and identification of U69 gene mutations encoded by ganciclovir-resistant human herpesvirus 6 using denaturing high-performance liquid chromatography. J. Virol. Methods. 2009;161:223–230. doi: 10.1016/j.jviromet.2009.06.016. [DOI] [PubMed] [Google Scholar]
- Namba T., Kodama R., Moritomo S., Hoshino T., Mizushima T. Zidovudine, an anti-viral drug, resensitizes gemcitabine-resistant pancreatic cancer cells to gemcitabine by inhibition of the Akt-GSK3β-Snail pathway. Cell Death Dis. 2015;6:1–11. doi: 10.1038/cddis.2015.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikkeis A.F., Piérard G.E. Recognition and treatment of shingles. Drugs. 1994;48:528–548. doi: 10.2165/00003495-199448040-00004. [DOI] [PubMed] [Google Scholar]
- O'Brien J.J., Campoli-Richards D.M. Acyclovir: an updated review of its antiviral activity, pharmacokinetic properties and therapeutic efficacy. Drugs. 1989;37:233–309. doi: 10.2165/00003495-198937030-00002. [DOI] [PubMed] [Google Scholar]
- Ostrosky-Zeichner L., Rex J.H. 2008. PART 1089–1109.
- Pagano J.S., Whitehurst C.B., Andrei G. Antiviral drugs for EBV. Cancers. 2018;10:10–15. doi: 10.3390/cancers10060197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Painter W., Robertson A., Trost L.C., Godkin S., Lampert B., Painter G. First pharmacokinetic and safety study in humans of the novel lipid antiviral conjugate CMX001, a broad-spectrum oral drug active against double-stranded DNA viruses. Antimicrob. Agents Chemother. 2012;56:2726–2734. doi: 10.1128/aac.05983-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker W.B. Enzymology of purine and pyrimidine antimetabolites used in the treatment of cancer. Chem. Rev. 2009;109:2880–2893. doi: 10.1021/cr900028p. Enzymology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pauly M.D., Lauring A.S. Effective lethal mutagenesis of influenza virus by three nucleoside analogs. J. Virol. 2015;89:3584–3597. doi: 10.1128/jvi.03483-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piret J., Boivin G. Resistance of herpes simplex viruses to nucleoside analogues: mechanisms, prevalence, and management. Antimicrob. Agents Chemother. 2011;55:459–472. doi: 10.1128/aac.00615-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price N.B., Prichard M.N. Progress in the development of new therapies for herpesvirus infections. Curr. Opin. Virol. 2011;1:548–554. doi: 10.1016/j.coviro.2011.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prusoff W.H. Synthesis and biological activities of iododeoxyuridine, an analog of thymidine. BBA - Biochim. Biophys. Acta. 1959;32:295–296. doi: 10.1016/0006-3002(59)90597-9. [DOI] [PubMed] [Google Scholar]
- Quenelle D.C., Lampert B., Collins D.J., Rice T.L., Painter G.R., Kern E.R. Efficacy of CMX001 against herpes simplex virus infections in mice and correlations with drug distribution studies. J. Infect. Dis. 2010;202:1492–1499. doi: 10.1086/656717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramakrishnan S., Hu Q., Krishnan N., Wang D., Smit E., Granger V., Rak M., Attwood K., Johnson C., Morrison C., Pili R., Chatta G., Guru K., Gueron G., McNally L., Wang J., Woloszynska-Read A. Decitabine, a DNA-demethylating agent, promotes differentiation via NOTCH1 signaling and alters immune-related pathways in muscle-invasive bladder cancer. Cell Death Dis. 2017;8:3217. doi: 10.1038/s41419-017-0024-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rawson J.M., Heineman R.H., Beach L.B., Martin J.L., Schnettler E.K., Dapp M.J., Patterson S.E., Mansky L.M. 5,6-Dihydro-5-aza-2′-deoxycytidine potentiates the anti-HIV-1 activity of ribonucleotide reductase inhibitors. Bioorg. Med. Chem. 2013;21:7222–7228. doi: 10.1016/j.bmc.2013.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rawson Jonathan M.O., Daly M.B., Xie J., Clouser C.L., Landman S.R., Reilly C.S., Bonnac L., Kim B., Patterson S.E., Mansky L.M. 5-Azacytidine enhances the mutagenesis of HIV-1 by reduction to 5-aza-2′-deoxycytidine. Antimicrob. Agents Chemother. 2016;60:2318–2325. doi: 10.1128/aac.03084-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rawson Jonathan M.O., Roth M.E., Xie J., Daly M.B., Clouser C.L., Landman S.R., Reilly C.S., Bonnac L., Kim B., Patterson S.E., Mansky L.M. Synergistic reduction of HIV-1 infectivity by 5-azacytidine and inhibitors of ribonucleotide reductase. Bioorg. Med. Chem. 2016;24:2410–2422. doi: 10.1016/j.bmc.2016.03.052. [DOI] [PubMed] [Google Scholar]
- Rehermann B., Bertoletti A. Immunological aspects of antiviral therapy of chronic hepatitis B virus and hepatitis C virus infections. Hepatology. 2015;61:712–721. doi: 10.1002/hep.27323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sagnelli E., Sagnelli C., Macera M., Pisaturo M., Coppola N. An update on the treatment options for HBV/HCV coinfection. Expert Opin. Pharmacother. 2017;18:1691–1702. doi: 10.1080/14656566.2017.1398233. [DOI] [PubMed] [Google Scholar]
- Sandrini M.P.B., Clausen A.R., On S.L.W., Aarestrup F.M., Munch-Petersen B., Piškur J. Nucleoside analogues are activated by bacterial deoxyribonucleoside kinases in a species-specific manner. J. Antimicrob. Chemother. 2007;60:510–520. doi: 10.1093/jac/dkm240. [DOI] [PubMed] [Google Scholar]
- Schaeffer H.J., Beauchamp L., de Miranda P., Elion G.B., Bauer D.J., Collins P. 9-(2-Hydroxyethoxymethyl) guanine activity against viruses of the herpes group. Nature. 1978;272:583–585. doi: 10.1038/272583a0. [DOI] [PubMed] [Google Scholar]
- Seifert R. Vidarabine is neither a potent nor a selective AC5 inhibitor. Biochem. Pharmacol. 2014;87:543–546. doi: 10.1016/j.bcp.2013.12.025. [DOI] [PubMed] [Google Scholar]
- Seley-Radtke K.L., Yates M.K. The evolution of nucleoside analogue antivirals: a review for chemists and non-chemists. Part 1: early structural modifications to the nucleoside scaffold. Antivir. Res. 2018;154:66–86. doi: 10.1016/j.antiviral.2018.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaimerdenova M., Karapina O., Mektepbayeva D., Alibek K., Akilbekova D. The effects of antiviral treatment on breast cancer cell line. Infect. Agents Cancer. 2017;12:1–10. doi: 10.1186/s13027-017-0128-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin H.J., Kim C., Cho S. Gemcitabine and nucleos(t)ide synthesis inhibitors are broad-spectrum antiviral drugs that activate innate immunity. Viruses. 2018;10:211. doi: 10.3390/v10040211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sofia M.J., Bao D., Chang W., Du J., Nagarathnam D., Rachakonda S., Reddy P.G., Ross B.S., Wang P., Zhang H.R., Bansal S., Espiritu C., Keilman M., Lam A.M., Steuer H.M.M., Niu C., Otto M.J., Furman P.A. Discovery of a luoro-2′-β- C -methyluridine Nucleotide Prodrug (PSI-7977) for the treatment of hepatitis C virus. J. Med. Chem. 2010;53:7202–7218. doi: 10.1021/jm100863x. [DOI] [PubMed] [Google Scholar]
- Song J.H., Kim S.R., Heo E.Y., Lee J.Y., Kim D. eun, Cho S., Chang S.Y., Yoon B. Il, Seong J., Ko H.J. Antiviral activity of gemcitabine against human rhinovirus in vitro and in vivo. Antivir. Res. 2017;145:6–13. doi: 10.1016/j.antiviral.2017.07.003. [DOI] [PubMed] [Google Scholar]
- Stresemann C., Lyko F. Modes of action of the DNA methyltransferase inhibitors azacytidine and decitabine. Int. J. Cancer. 2008;123:8–13. doi: 10.1002/ijc.23607. [DOI] [PubMed] [Google Scholar]
- Sugawara M., Huang W., Fei Y.J., Leibach F.H., Ganapathy V., Ganapathy M.E. Transport of valganciclovir, a ganciclovir prodrug, via peptide transporters PEPT1 and PEPT2. J. Pharm. Sci. 2000;89:781–789. doi: 10.1002/(SICI)1520-6017(200006)89:6<781::AID-JPS10>3.0.CO;2-7. [DOI] [PubMed] [Google Scholar]
- Sun R., Wang L. Inhibition of Mycoplasma pneumoniae growth by FDA-approved anticancer and antiviral nucleoside and nucleobase analogs. BMC Microbiol. 2013;13:184. doi: 10.1186/1471-2180-13-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thackray A.M., Field H.J. Famciclovir and valaciclovir differ in the prevention of herpes simplex virus type 1 latency in mice: a quantitative study. Antimicrob. Agents Chemother. 1998;42:1555–1562. doi: 10.1128/AAC.42.7.1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theobald R.J. 1–5. 2016. Vidarabine. Ref. Modul. Biomed. Sci. [Google Scholar]
- Thomson J.M., Lamont I.L. Nucleoside analogues as antibacterial agents. Front. Microbiol. 2019;10:952. doi: 10.3389/fmicb.2019.00952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topalis D., Gillemot S., Snoeck R., Andrei G. Distribution and effects of amino acid changes in drug-resistant α and β herpesviruses DNA polymerase. Nucleic Acids Res. 2016;44:9530–9554. doi: 10.1093/nar/gkw875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyring S., Barbarash R.A., Nahlik J.E., Cunningham A., Marley J., Heng M., Jones T., Rea T., Boon R., Saltzman R., Bruce S., Harris A., Epstein A., Lowry L., Rubin H., Dupuy J., Hendricks J., Greer J., Rapaport M. Famciclovir for the treatment of acute herpes zoster: effects on acute disease and postherpetic neuralgia. A randomized, double-blind, placebo- controlled trial. Ann. Intern. Med. 1995;123:89–96. doi: 10.7326/0003-4819-123-2-199507150-00002. [DOI] [PubMed] [Google Scholar]
- Van Linthout S., Elsanhoury A., Klein O., Sosnowski M., Miteva K., Lassner D., Abou-El-Enein M., Pieske B., Kühl U., Tschöpe C. Telbivudine in chronic lymphocytic myocarditis and human parvovirus B19 transcriptional activity. ESC Hear. Fail. 2018;5:818–829. doi: 10.1002/ehf2.12341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vatner S.F., Park M., Yan L., Lee G.J., Lai L., Iwatsubo K., Ishikawa Y., Pessin J., Vatner D.E. Adenylyl cyclase type 5 in cardiac disease, metabolism, and aging. Am. J. Physiol. Cell Physiol. 2013;305:H1–H8. doi: 10.1152/ajpheart.00080.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weller S., Blum M.R., Doucette M., Burnette T., Cederberg D.M., Miranda P. De, Smiley M.L. Pharmacolunetics of the acvclovir pro- drug valaciclovir after iscalati and multiple-dose adrninis tration normal volunteers. Clin. Pharmacol. Ther. 1993:595–605. doi: 10.1038/clpt.1993.196. [DOI] [PubMed] [Google Scholar]
- Westover J.B., Mathis A., Taylor R., Wandersee L., Bailey K.W., Sefing E.J., Hickerson B.T., Jung K.H., Sheridan W.P., Gowen B.B. Galidesivir limits Rift Valley fever virus infection and disease in Syrian golden hamsters. Antivir. Res. 2018;156:38–45. doi: 10.1016/j.antiviral.2018.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff F., Leisch M., Greil R., Risch A., Pleyer L. The double-edged sword of (re)expression of genes by hypomethylating agents: from viral mimicry to exploitation as priming agents for targeted immune checkpoint modulation. Cell Commun. Signal. 2017;15:1–14. doi: 10.1186/s12964-017-0168-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . World Health Organisation; 2017. Global Hepatitis Report, 2017. [Google Scholar]
- Xu H.T., Colby-Germinario S.P., Hassounah S.A., Fogarty C., Osman N., Palanisamy N., Han Y., Oliveira M., Quan Y., Wainberg M.A. Evaluation of Sofosbuvir (β-D-2′-deoxy-2′-α-fluoro-2′-β-C-methyluridine) as an inhibitor of Dengue virus replication. Sci. Rep. 2017;7:1–11. doi: 10.1038/s41598-017-06612-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaldiz M., Solak B., Kara R.O., Cosansu N., Erdem M.T. Comparison of famciclovir, valaciclovir, and brivudine treatments in adult immunocompetent patients with herpes zoster. Am. J. Therapeut. 2016;9:1–9. doi: 10.1097/MJT.0000000000000436. [DOI] [PubMed] [Google Scholar]
- Yao J., Zhang Y., Ramishetti S., Wang Y., Huang L. Turning an antiviral into an anticancer drug: nanoparticle delivery of acyclovir monophosphate. J. Control. Release. 2013;170:414–420. doi: 10.1016/j.jconrel.2013.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yates M.K., Seley-Radtke K.L. The evolution of antiviral nucleoside analogues: a review for chemists and non-chemists. Part II: complex modifications to the nucleoside scaffold. Antivir. Res. 2019;162:5–21. doi: 10.1016/j.antiviral.2018.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z., Yang E., Hu C., Cheng H., Chen C.Y., Huang D., Wang R., Zhao Y., Rong L., Vignuzzi M., Shen H., Shen L., Chen Z.W. Cell-based high-throughput screening assay identifies 2′,2′- difluoro-2′-deoxycytidine gemcitabine as a potential antipoliovirus agent. ACS Infect. Dis. 2017;3:45–53. doi: 10.1021/acsinfecdis.6b00116. [DOI] [PMC free article] [PubMed] [Google Scholar]