Abstract
Background:
The second victim effect is defined as emotional distress experienced by providers involved in mistakes. This study characterizes events contributing to the second victim effect among a diverse sample of physician mothers, describes the impact on both provider and patient, and seeks to determine the association between experiencing a mistake and burnout.
Methods:
In this mixed-methods study, an anonymous, cross-sectional survey was posted to an online network of over 65000 physician mothers on June 17, 2016. Self-reported involvement in a mistake provided opportunity to describe the error and impact on both provider and patient. Free text responses were qualitatively coded to identify error types. Hypothesizing that making a mistake contributes to burnout, self-reported burnout was examined using a single question. We used logistic regression to estimate the association between involvement in a mistake and burnout, adjusting for practice years, setting, and specialty.
Results:
5782 members completed the survey for an estimated response rate of 16.5% based on 34956 active users during the survey period. 2859 respondents reported involvement in a mistake (49%), which was associated with higher reported burnout (p<0.0001). 56% of those reporting a mistake provided descriptions. Qualitative analysis revealed that self-reported treatment errors were more common and diagnostic errors were most often reported to result in greater patient harm. Of those involved in a mistake, 82% reported feelings of guilt; 2.2% reported reducing clinical workload, taking leave, or leaving the profession.
Conclusions:
Physician mothers involved in errors experience negative outcomes and may be at increased risk for burnout. Additional research should focus on strategies to mitigate burnout associated with the second victim effect, particularly among women physicians and those with family responsibilities.
INTRODUCTION
The distress and self-doubt experienced by providers after involvement in an adverse event, medical error or unanticipated patient outcome is known as the “second victim” phenomenon.[1,2] It has been defined by Scott et al. as: “A health care provider…who becomes victimized in the sense that the provider is traumatized by the event. Frequently, second victims feel personally responsible for unexpected patient outcomes and feel as though they have failed their patients, second-guessing their clinical skills and knowledge base.”[2]
Not surprisingly, physicians involved in errors have reported significant emotional distress and decreased work satisfaction.[3] Experiencing emotional distress related to an adverse event has also been associated with unfavorable work-related outcomes including higher rates of turnover intention, absenteeism, and decreased joy associated with work.[4–6] Some providers report changing their roles after involvement in an adverse event, at times seeking non-clinical positions or jobs perceived to be associated with less risk.[6] These outcomes may be compounded by a lack of meaningful institutional support for second victims.[7]
The literature has found that women physicians may be more likely than men to experience negative emotional and professional outcomes related to adverse events, and that these outcomes may be more pronounced among women with family responsibilities.[8,9] Indeed, a recent study found that following adverse patient outcomes, women surgeons experienced a greater decline in referrals than male surgeons with similar adverse outcomes.[10] Yet, several of the largest studies that inform our understanding of physicians and the second victim effect involve primarily male physician respondents.[3,11]
In this study, Second Victim Adverse Event Experiences: Decisions and Repercussions for Mothers in Medicine (SAVE DR MoM), we sought to understand the types of adverse events, mistakes and near misses experienced by a diverse sample of physician mothers across a wide range of specialties and practice settings, the impact of such events on both the patients and physicians involved and the association between experiencing an adverse event, medical error or near miss and burnout.
METHODS
Study Setting and Participants
The Physician Moms Group, founded in 2014, is an online community of over 70000 diverse physician members who identify as mothers.[12] We posted an anonymous, cross-sectional survey on the group’s secret Facebook group on June 17, 2016 followed by two reminder posts in July 2016. Detailed survey methods are reported in additional studies.[8,13] Briefly, a total of 5782 members completed the survey for an estimated response rate of 16.5% based on 34956 active users during the survey period and 36% based on the estimated 16059 unique views.[8]
The Committee on Human Research at the University of California, San Francisco, reviewed and approved this study (16–19306).
Measures
In addition to demographic information, the survey also asked respondents about involvement in a medical mistake, the outcome for the patient, and the impact on the respondent.
To understand whether or not the respondent was involved in a medical mistake, we asked “Have you ever been personally involved with a mistake (serious, minor or a ‘near miss’) in your career?” Possible responses were yes or no. Those who responded yes were also asked to briefly describe the mistake or near miss and what caused it in free text format. For the purposes of the survey question and as previously defined by Wu et al., a mistake was defined as an act or omission for which the respondent felt responsible, that had or could have had serious or potentially serious consequences for the patient, and that would have been judged wrong by knowledgeable peers at the time it occurred.[14]
Respondents were then asked about patient outcome using the following categorical responses: harm, extra visit/monitoring but no other harm, hospitalization or procedure required, permanent disability, death or other.[15] Respondents were subsequently asked about the impact the mistake had on them personally. Possible responses included shame, guilt, loss of confidence, sadness, anger, difficulty sleeping, need to take leave from work, need for counseling/mental health support, permanent reduction in clinical role, end to clinical work or other.[2,3,7,11] Respondents were asked to select all applicable responses.
Self-reported burnout using a single item from the widely used Mini Z Burnout Survey was also assessed.[16] The Mini Z burnout survey includes a single item burnout question (the single item is validated against the Maslach Burnout Inventory) and 9 items related to outcomes or potential causes of burnout.[17] To increase response rates to the online survey, we sought to identify an item that captured burnout in a concise manner and therefore selected the single item burnout question which is worded as follows: Using your own definition of “burnout,” please select one of the answers below. Survey respondents were given the following options to select from: 1) I enjoy my work. I have no symptoms of burnout. 2) I am under stress, and don’t always have as much energy as I did, but I don’t feel burned out. 3) I am definitely burning out and have one or more symptoms of burnout, e.g. emotional exhaustion. 4) The symptoms of burnout that I’m experiencing won’t go away. 5) I think about work frustrations a lot. I feel completely burned out. I am at the point where I may need to seek help.[18]
Analysis
We applied mixed-methods to the analysis of this structured and unstructured data. We present summary statistics for frequency of patient responses by involvement in medical mistake (Table 1). Chi square tests were used to ascertain differences between respondents who did or did not report experiencing a medical mistake.
Table 1:
Respondent characteristics
| Respondentsa, No. (%) | ||||
|---|---|---|---|---|
| Total, N=5782 (%) | Reported medical mistake n=2859c (49) |
No reported medical mistake n=2723 (47) |
P Valued | |
| Characteristic b | ||||
| Years in Practice | ||||
| 0–4 years | 1994 | 916 (46) | 1021 (51) | <0.01 |
| 5–9 yearse | 2205 | 1104 (50) | 1027 (46) | |
| 10–14 years | 942 | 511 (54) | 400 (42) | |
| ≥ 15 years | 616 | 322 (52) | 262 (43) | |
| Race/ethnicity | ||||
| Non-Hispanic White | 4000 | 2041 (51) | 1821 (46) |
<0.01 |
| Non-Hispanic Black | 211 | 108 (51) | 94 (45) | |
| Asian | 792 | 370 (47) | 404 (51) | |
| Hispanic | 440 | 201 (46) | 222 (50) | |
| Other | 266 | 111 (42) | 148 (56) | |
| Marital status | ||||
| Not currently married, never married, or divorced | 315 | 151 (48) | 154 (49) | 0.54 |
| Married | 5457 | 2706 (50) | 2568 (47) | |
| Trainee, resident, or fellow | ||||
| No | 5244 | 2612 (50) | 2451 (47) | 0.08 |
| Yes | 534 | 247 (46) | 272 (51) | |
| Medical Specialty | ||||
| Anesthesia | 187 | 89 (48) | 94 (50) | 0.48 |
| Dermatology | 103 | 39 (38) | 61 (59) | 0.01 |
| Emergency medicine | 516 | 308 (60) | 181 (35) | <0.01 |
| Family medicine | 950 | 491 (52) | 423 (45) | 0.10 |
| Internal medicine | 1291 | 593 (46) | 657 (51) | <0.01 |
| Neurology | 139 | 52 (37) | 86 (62) | <0.01 |
| Obstetrics-gynecology | 709 | 443 (62) | 239 (34) | <0.01 |
| Ophthalmology | 96 | 40 (42) | 53 (55) | 0.11 |
| Pathology | 95 | 34 (36) | 60 (63) | <0.01 |
| Pediatrics | 1166 | 556 (48) | 575 (49) | 0.12 |
| Psychiatry | 314 | 105 (33) | 202 (64) | <0.01 |
| Radiology | 109 | 51 (47) | 50 (46) | 0.88 |
| Surgery | 278 | 158 (57) | 114 (41) | 0.02 |
| Other | 61 | 35 (57) | 26 (43) | 0.33 |
| Practice Setting | ||||
| Private practice | 2143 | 1067 (50) | 1021 (48) | 0.79 |
| Academic | 1957 | 988 (50) | 913 (47) | |
| Public hospital | 444 | 210 (47) | 207 (47) | |
| HMO | 266 | 137 (52) | 122 (46) | |
| VA | 103 | 50 (49) | 46 (45) | |
| Military | 105 | 56 (53) | 48 (46) | |
| Not currently working or retired | 124 | 52 (42) | 64 (52) | |
| Burnout | ||||
| No | 3545 | 1678 (47) | 1759 (50) | <.01 |
| Yes | 2208 | 1175 (53) | 957 (43) | |
97.7% of respondents were from the United States
Missing data points not shown (missing reponses include 200 (3.5%) missing values for self-reported involvement in a medical mistake, 25 (0.4%) missing values for years in practice, 73 (1.3%) missing values for race/ethnicity, 22 (0.4%) missing values for practice setting, 10 missing values for marital status (0.2%), 4 (0.1%) missing values for training status, and 29 (0.5%) missing values for burnout)
Logistic regression model used to assess relationship between involvement in medical mistake and burnout, adjusted for years in practice, practice setting, and medical specialty
Chi-square test, α=0.05
Referent group
In parallel, we used a qualitative approach to analyze the free-text responses in which respondents described mistakes.[19,20] We employed deductive coding, incorporating a previously identified framework for error type initially described in 1993 by Leape et al., which divides errors into four categories: 1) diagnostic (error or delay in diagnosis, failure to employ indicated tests, use of outmoded tests or therapy and failure to act on results of monitoring or testing), 2) treatment (error in the performance of an operation, procedure, or test, error in administering the treatment, error in the dose or method of using a drug, avoidable delay in treatment or in responding to an abnormal test and inappropriate care), 3) preventive (failure to provide prophylactic treatment, inadequate monitoring or follow-up of treatment) and 4) other (failure of communication, equipment failure and other system failure).[21,22] Two authors independently reviewed free-text responses and categorized them according to this framework. Respondents’ free text descriptions of the mistake were also deductively coded to identify contributing factors including patient, provider, and system-related factors using a framework previously described by Gandhi et al.[23] A third author resolved disagreements. The proportion of patients reported to experience harm resulting from errors categorized as diagnostic was compared to both the proportion of patients reported to experience harm related to errors categorized as treatment and the proportion of patients reported to experience harm related to errors categorized as other (other was defined in Figure 2 to include errors categorized as preventive, other or unknown in Table 2A) using T tests. Patient harm was defined as any patient outcome selected by a respondent except for ‘no harm.’ The proportion of patients reported to experience severe harm (defined as permanent disability or death) resulting from diagnostic error was also compared to the proportion of patients reported to experience severe harm resulting from treatment errors.
Figure 2:
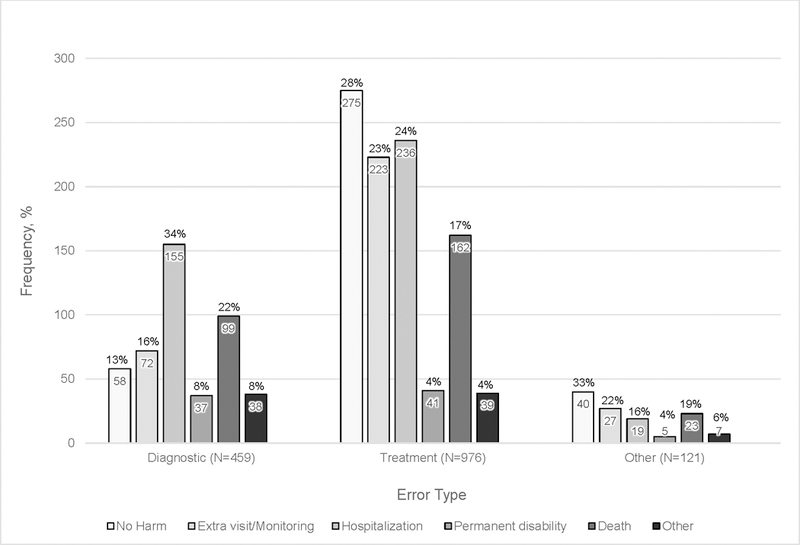
Distribution of reported patient outcomes by categorized error type
Tables 2A and 2B:
Types and contributing factors of events described by respondents
| Mistake type and definition[21,22] | Respondents describing mistake, No. (%) (n=1556) |
Representative Quoteg |
|---|---|---|
| Treatment | 976 (63) | “I was in residency, MICU consults. Called to assess a healthy…woman who was…dyspneic and hypoxic. We found she had a large PE. No room in MICU so moved her to cardiac step-down w a/c. I passed her on to the floor team. Heard in the AM she crashed overnight and was unable to be resuscitated. I wasn’t there but can’t shake feeling I could have done more for her.” “Medication error. Multifactorial, but final call was my call and my error.“ |
| Error in the performance of an operation, procedure, or test | ||
| Error in administering the treatment | ||
| Error in the dose or method of using a drug | ||
| Avoidable delay in treatment or in responding to an abnormal test | ||
| Inappropriate (not indicated) care | ||
| Diagnostic | 459 (30) | “Missed an abnormal…finding that was later picked up by my peer while I was on maternity leave. No change in patient outcome but every time I see that patient, I feel disappointed and inadequate.” “I delayed diagnosis of a surgical emergency. It was not something I’d seen before and was afraid to wake up surgeon because I was not sure. I admitted the patient but surgical management was delayed by several hours.” |
| Error or delay in diagnosis | ||
| Failure to employ indicated tests | ||
| Use of outmoded tests or therapy | ||
| Failure to act on results of monitoring or testing | ||
| Preventive | 18 (1) | “Patient not put on appropriate antimicrobial prophylaxis.” “[Drug] toxicity in a patient I had not checked a level on in awhile (6 months).” |
| Failure to provide prophylactic treatment | ||
| Inadequate monitoring or follow-up of treatment | ||
| Other: other system failure | 35 (2) | “pharmacy dispensed different drug than what we ordered.” “I recently posted the results on a series of wrong (sic) patients thanks to the emr that I got no live training for and no training on desktop mgt. My staff caught it…I do not think this caused harm but did cause stress to me.“ |
| Other: failure of communication | 34 (2) | “It was a system error. I never received test results from radiology on a patient in clinic. The patient called a month later asking about CT results and they were abnormal. We didn’t have a a good system in place at the time to ensure that never happened. We do now.” “Was not called on a CT result for a week. I may not have been fully responsible but I felt sick when I found out. “ |
| Other: equipment failure | 8 (1) | “Trach, vent dependent…pt went into severe respiratory distress & Bradycardia. He was coded for an hour. Tried to externally pace but I feel that the pacer was not delivering shocks. Nurse said it was working fine. Still disagree…Not even sure if he is still alive” “Surgical error--broken sheath when equipment being removed” |
| Unknown | 26 (2) | “Felt I had to do something I was uncomfortable doing.” “Exhausted, end of 18 hour day, after a weekend on call. Or was getting sick, I knew something was wrong, but was literally too tired to realize what the problem was. Only after M&M conference was I able to realize it wasn’t a knowledge deficit, just an exhaustion issue.” |
| Contributing factors and definition[23] |
Respondents describing mistakeh, No. (%) (n=1556) |
Representative Quoteg |
|---|---|---|
| Cognitive | 1215 (78) | “Missed a lung ca in a pt complaining of sob and palpitations bc I got so sidetracked…“ “This wasn’t recent but it’s the one that haunts me. While intubating a [patient]…in medical school, I was handed a packaged LMA and didn’t realize there’s a plastic cap over the bottom, which I inserted into the patient, who desaturated very temporarily and had a scrape to the airway… |
| Judgment | ||
| Vigilance or memory | ||
| Lack of knowledge | ||
| Other systems | 573 (37) | “I was a second year IM resident on call alone…A patient needed to have an airway secured for sedation, and I was unable to obtain the airway. We had no backup….” “Wrong medication dosage. Felt likely due to multiple physician interruptions during the day, breaking concentration, and increasing risk of writing the wrong dose.“ |
| Lack of supervision | ||
| Workload | ||
| Interruptions | ||
| Technology problems | ||
| Fatigue | ||
| Communication | 288 (19) | “Wrong dose of insulin given in the OR because I did not effectively communicate with the resident who was assisting me in the case“ “Retained lap. Count done incorrectly“ |
| Handoffs | ||
| Failure to establish clear lines of responsibility | ||
| Conflict | ||
| Some other failure of communication | ||
| Patient-related | 171 (11) | “pt lost to follow up. i’m pretty sure had…ca [cancer]. i should have called her more and made sure she did her imaging. should have been more clear about my concerns for her: maybe she didn’t understand?“ “Patient did not do full work up I recommended and I didn’t push for frequent enough followup“ |
| Nonadherence | ||
| Atypical presentation | ||
| Complicated medical history | ||
| Information about medical history of poor quality | ||
| Other | ||
| Technical | 148 (10) | “Bowel perforation during elective robotic surgery“ “Incidental bladder injury during c-section“ |
| Unknown | 212 (14) | “Complication of a procedure. Patient coded and died.” “Bad heart tracing-don’t know why. Not sure anything could have been done differently, but makes you wonder. “ |
Although no identifying information was collected, authors redacted information from free text descriptions of mistakes if any potentially identifiable details were included
Authors assigned multiple contributing factors to each response, when applicable, therefore percentages do not add to 100%
Notably, while most respondents described a mistake they committed and for which they felt responsible, a small number described an event primarily involving the actions of another healthcare provider. The authors include these responses in the qualitative analysis because respondents reported feeling directly involved in these events and reported that these events had direct impact on them emotionally and professionally. Specifically, 49 (3%) respondents described an error that they believed someone else to be responsible for; 33 (2%) described an event that primarily involved another healthcare provider but for which the respondent still felt responsible. Because the taxonomies for medical mistakes in the literature are still relatively nascent, we also performed inductive coding without a pre-specified framework for all of these free text responses.[24]
Application of the frameworks permitted free-text responses to be categorized and analyzed as categorical variables. We then examined the association between reporting a medical mistake and reporting burnout. Participants who reported at least one symptom of burnout were categorized as experiencing physician burnout. We used a logistic regression model to estimate odds ratios (ORs) and corresponding 95% confidence intervals (CIs) for the relationship between burnout and making a mistake, adjusting for years in practice, practice setting and medical specialty.
Data were collected by the Physician Moms Group study moderators on REDCap and statistical analysis was performed using SAS software, Version 9.4.
RESULTS
A total of 5782 providers responded to the survey (Table 1). The respondents reflect experience across a wide range of clinical disciplines and practice settings. 72% of respondents reported being in practice for over 5 years, 70% were white and 94% were married. 9% of respondents reported being in training (residency or fellowship) at the time of the survey. The most frequently designated specialties included family medicine (16%), internal medicine (22%), pediatrics (20%) and OBGYN (12%). Over a third of respondents (37%) reported working in a private practice setting while another third (34%) reported working in an academic setting. 38% of respondents reported experiencing burnout (Table 1).
Of those responding to the survey, 2859 (49%) self-reported a mistake (Table 1 and Figure 1); 200 (3%) respondents did not respond to the self-reported mistake question. Significant differences existed between respondents who did, versus those who did not, report experiencing a medical mistake with regard to number of years in practice, race/ethnicity, specialty, and self-reported burnout (Table 1).
Figure 1:
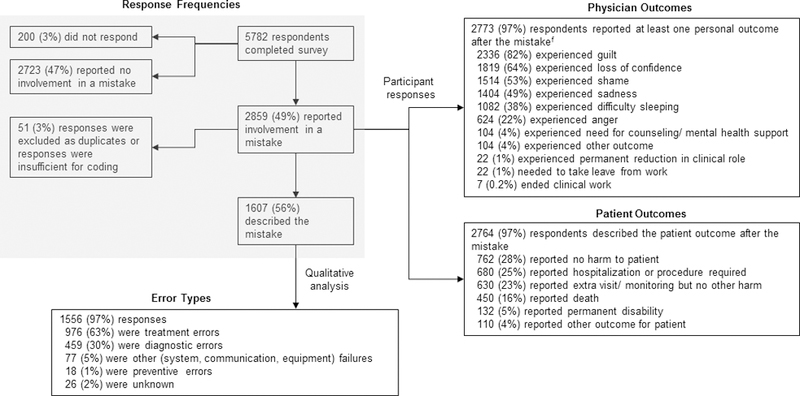
Flow chart depicting survey responses and qualitative analysis
f Respondents could select multiple outcomes
Of the 2859 respondents stating that they made a medical mistake, 2764 (97%) reported the outcome for the patient, 2773 (97%) reported experiencing at least one adverse personal outcome, and 1607 (56%) provided free text descriptions of the mistake (Figure 1). Of the 1607 free text descriptions, 1556 (97%) described a specific mistake, near miss, adverse event, or provided a more general statement about a mistake or adverse event. The remaining 3% of free text descriptions did not contain sufficient information for further qualitative analysis.
The majority of reported errors were categorized as being related to treatment/management mistakes with diagnostic errors as the next most common category (Table 2A). A small percentage of the mistakes described were classified as “other” (communication failures, equipment failures or system failures), preventive or unknown (Table 2A).[21,22] Most errors had more than one contributing cause, most commonly cognition, systems factors, and communication (Table 2B).[23] The sample quotes highlighted in Tables 2A and 2B are representative examples of respondents’ descriptions for each type of mistake and contributing factor. These responses were included in the qualitative analysis and are included in the tables to provide context for the reader. To protect the identity of the patient and the respondent, potentially identifying information was redacted from the respondents’ descriptions.
Respondents were also asked about the patient outcome related to the mistake they described. Figure 2 displays the distribution of patient outcomes as selected by respondents who self-reported a mistake by categorized error type. While treatment or management errors were the most common across all categories of reported patient outcomes, errors coded as diagnostic were more often reported by respondents as resulting in greater patient harm; 88% of patients experiencing a diagnostic error were reported to experience some type of harm as compared to 72% of patients experiencing a treatment or management related error (P<0.0001). In addition, 30% of patients experiencing a diagnostic error were reported to experience severe harm in the form of death or permanent disability as compared to 21% of patients experiencing a treatment or management related error (P=0.0002).
Survey respondents were asked about the emotional and professional impact of the self-reported mistake on themselves. Figure 3 displays the outcomes experienced by 2773 respondents. Guilt was the most commonly experienced feeling in response to the self-reported mistake, followed by loss of confidence, shame and sadness. Some respondents reported a need to take leave from work or formally reduce their clinical roles (Figure 3). Although a minority of respondents (N=7) reported an end to clinical work altogether, they vividly described their experiences as follows:
Figure 3:
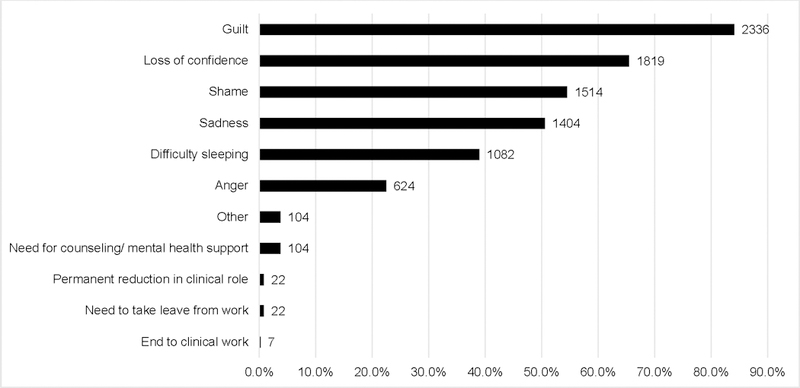
Emotions and reactions experienced by respondents who self-reported making a mistake
f Respondents could select multiple outcomes
“Saw [a young] patient in ED…Next day patient returned coding and died. Autopsy showed that patient had aspirated…Still blame myself because I debated admitting him when he came in the first time. i wasn’t 100% comfortable letting him go home... When they brought him coding I froze and died inside when I saw him. Two other doctors coded him instead of me. I have never worked another shift in that ER after working there for over ten years.”
Another respondent reporting an end to clinical work stated:
“I wrote an order for a medicine that was slighlty incorrect… The patient suffered no harm, but the family was very upset. It lead to an RCA [Root Cause Analysis] conference and in preparing for the conference, I realized I had misinterpreted some advice from an academic physician and should not have even prescribed the treatment to begin with and that it may have indeed caused harm. The episode led to severe feelings of guilt and failure, prompting me to see a therapist and start anti-depressant medication. This occured about 1.5 years before I left my practice.”
Self-reported involvement in a medical mistake was associated with higher self-reported burnout, with 41% percent of respondents who self-reported a mistake reporting experiencing burnout versus 35% of those who did not report a mistake reporting experiencing burnout (adjusted odds ratio 1.26; 95% CI, 1.12–1.42; p <0.001); 29 (0.5%) of all survey respondents did not respond to the self-reported burnout question.
DISCUSSION
To our knowledge, this is the largest study of the second victim experience among U.S. physicians over their careers across such a diversity of specialties and practice settings that also includes detailed information about actual mistakes, the impact on the provider, and the reported outcome for the patient. In addition, this is the first second victim study to focus on the specific experience of women physicians—specifically those who identify as mothers—with regard to the impact of mistakes and adverse events and the relationship to burnout.
Shanafelt et al. examined the relationship between a self-reported major medical error and burnout among 7905 U.S. surgeons; while a significant association with burnout was found, the study was limited to surgeons, asked only about the preceding 3 months, did not provide detailed information on the mistakes themselves and 86.7% of respondents were male.[11] Waterman et al. examined survey data from 3171 U.S. and Canadian physicians in internal and family medicine, pediatrics and surgery to understand the impact of errors; while respondents indicated errors had a significant emotional and professional impact and female respondents were found to experience increased distress as compared to males, the authors did not describe the mistakes or patient outcomes and 77% of respondents in the study were male.[3] Using survey data from 5788 nurses and physicians, Van Gerven et al. found that involvement in an adverse event was associated with an increased risk of burnout, but the study was limited to the inpatient acute care hospital and psychiatric hospital settings, asked only about the prior 6 months and did not contain information on the mistakes themselves; in addition, physicians accounted for only 20.6% of respondents in the study.[25] While Wu et al. did chartacterize the types of mistakes contributing to the second victim effect as well as the impact on the provider and the patient early on, the study was small, involving 114 house officers, was limited to internal medicine, and only a third of respondents were women.[14] Therefore, existing studies on the second victim effect draw primarily from the experience of male physician respondents, have been conducted across a more limited range of specialties and settings, and do not consistently provide information on the mistakes and patient outcomes contributing to the second victim effect.
We found that over the course of physician mothers’ careers in medicine, mistakes were common; almost 50% of respondents in the study reported involvement in a mistake. Given that underreporting of mistakes is well-established, we believe that mistakes occur more frequently than our results and other studies might suggest.[26] Despite the anonymous nature of the survey, respondents may have been hesitant to report a mistake because of stigma or fear of legal repercussion. In fact, several of the respondents who self-reported a mistake declined to share a free text description and instead used the space provided to indicate that they would prefer not to describe the event out of fear of negative professional consequences.
Of those who admitted to having ever been involved in a mistake, over 50% described the event in detail and reported the associated patient outcome. Qualitative analysis of these 1556 descriptions revealed that although treatment and management errors occurred most frequently, diagnostic errors more often resulted in a greater degree of patient harm as reported by survey respondents (Figure 2). This further supports the need to focus on diagnostic error as a major patient safety issue.[27] We acknowledge that respondents may have been more likely to report a mistake in which patient harm occurred because such a mistake may have had a greater impact on them personally and may therefore have been more memorable.
In addition, 97% of physicians involved in a mistake reported at least one adverse outcome for themselves, with the majority reporting 2 or more (Figure 3). Wu et al. described similar adverse emotional outcomes for internal medicine residents surveyed about their experiences with mistakes during training but as noted above, the study was small, limited to internal medicine and two-thirds of respondents were male.[14] The results from our study suggest that feelings of guilt, loss of confidence, shame and other adverse outcomes including negative professional consequences—the second victim phenomenon—are extremely common among physician mothers who report involvement in a medical mistake at all levels of training and from all specialties.
It is possible that distress experienced by women following adverse patient outcomes or errors may in part be related to the potentially greater professional consequences for women physicians, but further research is needed in this area.[10] Furthermore female physicians under stress may be perceived differently by patients as compared to male physicians and may demonstrate differences in assistance-seeking behavior, which has important implications for health care institutions seeking to support women effectively.[28–30]
While numerous studies report significant emotional responses among healthcare providers involved in mistakes, ours is the first to focus on the second victim experience of physician women—specifically physician mothers—over the course of their careers and from a diversity of specialties and practice settings.[2,3,7,11,14,25] This study also adds to the growing literature demonstrating that involvement in an adverse event can lead to increased burnout.[11,25] We found that those respondents who self-reported making a mistake were more likely to experience burnout as compared to those who did not, suggesting that the association between the second victim effect and burnout may be of particular relevance not only for women physicians, but for physician mothers.[30]
The findings in this study suggest that is incumbent on healthcare institutions to meaningfully support physician mothers involved in adverse events, medical mistakes and challenging patient cases so that these highly trained individuals remain a resilient part of the healthcare workforce. Many of the mistake descriptions in this study suggest that respondents perceived a lack of support and a culture of blame, which likely contributed to the adverse personal and professional outcomes for those participating in the study. While numerous institutions have developed second victim programs offering various forms of support to providers, there is tremendous unmet need across the majority of our healthcare system.[31–34] Preliminary research is promising; dedicating resources to establish formal support programs has been shown to be effective. Those who receive support may perceive workplace culture more positively.[4,33] Formal support programs may also have the potential to save institutions real dollars by decreasing the need for employees to take time off or leave work altogether.[35]
Despite its wide geographic reach, larger size, and inclusion of varied specialties and practice settings, this study does have limitations. The estimated response rates for the study were 16.5% based on 34956 active users during the survey period and 36% based on an estimated 16059 unique views.[8,13] While the sample includes only women physicians with children who participate in a social media group, and therefore does not represent all US physicians, it should be noted that as of 2017, women comprise over 50% of medical school matriculants.[36] In addition, this study does not explain exactly how gender and family responsibilities may mediate the second victim effect and burnout for this cohort because similar data are not available for male physician parents or non-parent physicians. We also acknowledge that respondents are likely to differ from non-respondents. Furthermore, the relationship between categorized error type and degree of patient harm as reported by survey respondents must be interpreted with caution. It is possible that diagnostic errors as coded in this study were found to more frequently result in a greater degree of reported patient harm because respondents may be more likely to remember mistakes that caused greater harm.
Regardless of its generalizability to all US physicians, our results indicate that for physician mothers, the second victim effect remains a significant problem, is associated with burnout and warrants thoughtful intervention.
CONCLUSION
The second victim effect occurs frequently in healthcare and can have emotional and professional consequences for providers; as this study demonstrates, such consequences may be particularly relevant for women providers with family responsibilities. Second victim effects may also contribute to significant burnout in this population. Our study highlights the important need for further research focusing on how gender and family responsibilities may mediate the second victim effect and associated burnout. Additionally, the degree to which women physicians and physician mothers may be at risk for the second victim phenomenon and burnout, as well as other adverse outcomes, as compared to their male counterparts, needs to be better understood so that optimally designed support strategies can be put into place. Further study is needed to better understand what types of support are most effective, in what situation, when, and for what provider type. For example, support from a peer or a group debriefing may be appropriate for certain situations while more extended professional counseling may be most beneficial in others. As Wu acknowledges, “Physicians will always make mistakes. The decisive factor will be how we handle them.”[1]
ACKNOWLEDGMENTS
We thank Hala Sabry, MD, MBA, Mi-Ok Kim, PhD, and Jimmy Hwang, PhD, for their support.
FUNDING
Dr. Sarkar is supported through grants from the National Cancer Institute (K24CA212294) and the Agency for Healthcare Research and Quality (P30HS023558). Dr. Linos is supported by the National Cancer Institute (R21CA212201, the National Institute on Aging (K76AGO54631) and the National Institute of Health (DP2CA225433). The funders had no role in the design, data collection, analysis, or presentation of results
Footnotes
COMPETING INTERESTS
The authors have no conflicts of interest to disclose.
DATA SHARING STATEMENT
Please contact the authors for inquiries regarding the datasets supporting this article, excluding free text responses which may include potentially identifying information.
Contributor Information
Kiran Gupta, University of California San Francisco, Department of Medicine, San Francisco, CA, United States.
Sarah Lisker, University of California San Francisco, Department of Medicine, San Francisco, CA, United States.
Natalie Rivadeneira, University of California San Francisco, Department of Medicine, San Francisco, CA, United States.
Christina Mangurian, University of California San Francisco, Department of Psychiatry, San Francisco, CA, United States.
Dr Eleni Linos, University of California San Francisco, Department of Dermatology, San Francisco, CA, United States.
Urmimala Sarkar, University of California San Francisco, Department of Medicine, San Francisco, CA, United States.
REFERENCES:
- 1.Wu AW. Medical error: the second victim. The doctor who makes the mistake needs help too. BMJ 2000;320:726–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scott SD, Hirschinger LE, Cox KR, et al. The natural history of recovery for the healthcare provider “second victim” after adverse patient events. Qual Saf Health Care 2009;18:325–30. doi: 10.1136/qshc.2009.032870 [DOI] [PubMed] [Google Scholar]
- 3.Waterman AD, Garbutt J, Hazel E, et al. The emotional impact of medical errors on practicing physicians in the United States and Canada. Jt Comm J Qual Patient Saf 2007;33:467–76. [DOI] [PubMed] [Google Scholar]
- 4.Burlison JD, Quillivan RR, Scott SD, et al. The Effects of the Second Victim Phenomenon on Work-Related Outcomes: Connecting Self-Reported Caregiver Distress to Turnover Intentions and Absenteeism. J Patient Saf Published Online First: 2 November 2016. doi: 10.1097/PTS.0000000000000301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lewis EJ, Baernholdt MB, Yan G, et al. Relationship of adverse events and support to RN burnout. J Nurs Care Qual 2015;30:144–52. doi: 10.1097/NCQ.0000000000000084 [DOI] [PubMed] [Google Scholar]
- 6.Rodriquez J, Scott SD. When Clinicians Drop Out and Start Over after Adverse Events. Jt Comm J Qual Patient Saf;44:137–45. doi: 10.1016/j.jcjq.2017.08.008 [DOI] [PubMed] [Google Scholar]
- 7.Ullström S, Andreen Sachs M, Hansson J, et al. Suffering in silence: a qualitative study of second victims of adverse events. BMJ Qual Saf 2014;23:325–31. doi: 10.1136/bmjqs-2013-002035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adesoye T, Mangurian C, Choo EK, et al. Perceived Discrimination Experienced by Physician Mothers and Desired Workplace Changes: A Cross-sectional Survey. JAMA Intern Med 2017;177:1033–6. doi: 10.1001/jamainternmed.2017.1394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seys D, Wu AW, Van Gerven E, et al. Health care professionals as second victims after adverse events: a systematic review. Eval Health Prof 2013;36:135–62. doi: 10.1177/0163278712458918 [DOI] [PubMed] [Google Scholar]
- 10.Sarsons H Interpreting Signals in the Labor Market: Evidence from Medical Referrals [Job Market Paper; ]. 10040. [Google Scholar]
- 11.Shanafelt TD, Balch CM, Bechamps G, et al. Burnout and medical errors among American surgeons. Ann Surg 2010;251:995–1000. doi: 10.1097/SLA.0b013e3181bfdab3 [DOI] [PubMed] [Google Scholar]
- 12.MyPMG. https://mypmg.com/ (accessed 29 Jan 2018).
- 13.Yank V, Rennels C, Linos E, et al. Behavioral Health and Burnout Among Physician Mothers who Care for a Person with a Serious Health Problem, Long-Term Illness or Disability. JAMA Intern Med In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu AW, Folkman S, McPhee SJ, et al. Do house officers learn from their mistakes? JAMA 1991;265:2089–94. [PubMed] [Google Scholar]
- 15.Hoppes M, Mitchell J. Serious Safety Events: A Focus on Harm Classification: Deviation in Care as Link. Chicago: American Society for Healthcare Risk Management; 2014. http://www.ashrm.org/pubs/files/white_papers/SSE-2_getting_to_zero-9-30-14.pdf (accessed 30 Apr 2018). [Google Scholar]
- 16.Linzer M, Poplau S, Babbott S, et al. Worklife and Wellness in Academic General Internal Medicine: Results from a National Survey. J Gen Intern Med 2016;31:1004–10. doi: 10.1007/s11606-016-3720-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rohland BM, Kruse GR, Rohrer JE. Validation of a single-item measure of burnout against the Maslach Burnout Inventory among physicians. Stress Health 2004;20:75–9. doi: 10.1002/smi.1002 [DOI] [Google Scholar]
- 18.Take the Physician Burnout Survey | STEPS Forward. STEPSforward.org; https://www.stepsforward.org/modules/physician-burnout-survey (accessed 12 Oct 2018). [Google Scholar]
- 19.Crabtree BF, Miller WL. Doing qualitative research. 2nd ed Thousand Oaks, Calif. ; London: : SAGE; 1999. https://trove.nla.gov.au/version/7365559 (accessed 12 Oct 2018). [Google Scholar]
- 20.Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs 2008;62:107–15. doi: 10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- 21.Kohn LT, Corrigan JM, Donaldson MS, editors. To Err is Human: Building a Safer Healthcare System. Washington, DC: National Academies Press; 1999. [PubMed] [Google Scholar]
- 22.Leape LL, Lawthers AG, Brennan TA, et al. Preventing medical injury. QRB Qual Rev Bull 1993;19:144–9. [DOI] [PubMed] [Google Scholar]
- 23.Gandhi TK, Kachalia A, Thomas EJ, et al. Missed and delayed diagnoses in the ambulatory setting: a study of closed malpractice claims. Ann Intern Med 2006;145:488–96. [DOI] [PubMed] [Google Scholar]
- 24.Glaser B Doing Grounded Theory: Issues and Discussions Sociology Press 1998. [Google Scholar]
- 25.Van Gerven E, Vander Elst T, Vandenbroeck S, et al. Increased Risk of Burnout for Physicians and Nurses Involved in a Patient Safety Incident. Med Care 2016;54:937–43. doi: 10.1097/MLR.0000000000000582 [DOI] [PubMed] [Google Scholar]
- 26.Noble DJ, Pronovost PJ. Underreporting of patient safety incidents reduces health care’s ability to quantify and accurately measure harm reduction. J Patient Saf 2010;6:247–50. [DOI] [PubMed] [Google Scholar]
- 27.Balogh EP, Miller BT, Ball JR, editors. National Academies of Sciences, Engineering, and Medicine. Improving Diagnosis in Health Care; Washington, DC: 2015. doi: 10.17226/21794 [DOI] [Google Scholar]
- 28.Sanfey H, Fromson J, Mellinger J, et al. Surgeons in Difficulty: An Exploration of Differences in Assistance-Seeking Behaviors between Male and Female Surgeons. J Am Coll Surg 2015;221:621–7. doi: 10.1016/j.jamcollsurg.2015.02.015 [DOI] [PubMed] [Google Scholar]
- 29.Hill KM, Blanch-Hartigan D. Physician gender and apologies in clinical interactions. Patient Educ Couns Published Online First: 11 December 2017. doi: 10.1016/j.pec.2017.12.005 [DOI] [PubMed] [Google Scholar]
- 30.Linzer M, Harwood E. Gendered Expectations: Do They Contribute to High Burnout Among Female Physicians? J Gen Intern Med 2018;33:963–5. doi: 10.1007/s11606-018-4330-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Scott SD, Hirschinger LE, Cox KR, et al. Caring for our own: deploying a systemwide second victim rapid response team. Jt Comm J Qual Patient Saf 2010;36:233–40. [DOI] [PubMed] [Google Scholar]
- 32.Edrees H, Connors C, Paine L, et al. Implementing the RISE second victim support programme at the Johns Hopkins Hospital: a case study. BMJ Open 2016;6:e011708. doi: 10.1136/bmjopen-2016-011708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Merandi J, Liao N, Lewe D, et al. Deployment of a Second Victim Peer Support Program: A Replication Study. Pediatr Qual Saf 2017;2:e031. doi: 10.1097/pq9.0000000000000031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shapiro J, Whittemore A, Tsen LC. Instituting a culture of professionalism: the establishment of a center for professionalism and peer support. Jt Comm J Qual Patient Saf 2014;40:168–77. [DOI] [PubMed] [Google Scholar]
- 35.Moran D, Wu AW, Connors C, et al. Cost-Benefit Analysis of a Support Program for Nursing Staff. J Patient Saf Published Online First: 27 April 2017. doi: 10.1097/PTS.0000000000000376 [DOI] [PubMed] [Google Scholar]
- 36.More Women Than Men Enrolled in U.S. Medical Schools in 2017. https://news.aamc.org/press-releases/article/applicant-enrollment-2017/ (accessed 18 Mar 2018).


