Abstract
Background
Vasectomy is an increasingly popular and effective family planning method. A variety of vasectomy techniques are used worldwide, including vas occlusion techniques (excision and ligation, thermal or electrocautery, and mechanical and chemical occlusion methods), as well as vasectomy with vas irrigation or with fascial interposition. Vasectomy guidelines largely rely on information from observational studies. Ideally, the choice of vasectomy techniques should be based on the evidence from randomized controlled trials (RCTs).
Objectives
The objective of this review was to compare the effectiveness, safety, acceptability and costs of vasectomy techniques for male sterilization.
Search methods
In February 2014, we updated the searches of CENTRAL, MEDLINE, POPLINE and LILACS. We looked for recent clinical trials in ClinicalTrials.gov and the International Clinical Trials Registry Platform. Previous searches also included EMBASE. For the initial review, we searched the reference lists of relevant articles and book chapters.
Selection criteria
We included RCTs comparing vasectomy techniques, which could include suture ligature, surgical clips, thermal or electrocautery, chemical occlusion, vas plugs, vas excision, open‐ended vas, fascial interposition, or vas irrigation.
Data collection and analysis
We assessed all titles and abstracts located in the literature searches. Two reviewers independently extracted data from articles identified for inclusion. Outcome measures include contraceptive efficacy, safety, discontinuation, and acceptability. Peto odds ratios (OR) with 95% confidence intervals (CI) were used for dichotomous outcomes, such as azoospermia. The mean difference (MD) was used for the continuous variable of operating time.
Main results
Six studies met the inclusion criteria. One trial compared vas occlusion with clips versus a conventional vasectomy technique. No difference was found in failure to reach azoospermia (no sperm detected). Three trials examined vasectomy with vas irrigation. Two studies looked at irrigation with water versus no irrigation, while one examined irrigation with water versus the spermicide euflavine. None found a difference between the groups for time to azoospermia. However, one trial reported that the median number of ejaculations to azoospermia was lower in the euflavine group compared to the water irrigation group. One high‐quality trial compared vasectomy with fascial interposition versus vasectomy without fascial interposition. The fascial interposition group was less likely to have vasectomy failure. Fascial interposition had more surgical difficulties, but the groups were similar in side effects. Lastly, one trial found that an intra‐vas was less likely to produce azoospermia than was no‐scalpel vasectomy. More men were satisfied with the intra‐vas device, however.
Authors' conclusions
For vas occlusion with clips or vasectomy with vas irrigation, no conclusions can be made as those studies were of low quality and underpowered. Fascial interposition reduced vasectomy failure. An intra‐vas device was less effective in reducing sperm count than was no‐scalpel vasectomy. RCTs examining other vasectomy techniques were not available. More and better quality research is needed to examine vasectomy techniques.
Keywords: Humans, Male, Aminoacridines, Oligospermia, Oligospermia/etiology, Randomized Controlled Trials as Topic, Spermatocidal Agents, Surgical Instruments, Therapeutic Irrigation, Vas Deferens, Vas Deferens/surgery, Vasectomy, Vasectomy/methods
Plain language summary
Vasectomy methods for birth control in men
Vasectomy is a surgical method used in men to cut or tie the vas deferens. The vas is a tube that delivers sperm from the testicles. The purpose of vasectomy is to provide permanent birth control. Vasectomy methods include different ways to close the vas. Variations to a vasectomy may be irrigation (flushing fluid through the vas) and fascial interposition (placing a layer of body tissue between the cut ends of the vas). Ideally, the choice of vasectomy method should be based on the best evidence from controlled trials. This review looked at how well the vasectomy methods work, how safe they were, the costs, and whether the men liked the method.
In February 2014, we updated the computer searches for studies of vasectomy methods. For the initial review, we also looked at reference lists of articles and book chapters. We included randomized controlled trials in any language.
We found six studies. One trial compared closing the vas with clips versus the usual cutting of the vas. The groups did not differ in reaching a low sperm count or in side effects. Three trials looked at flushing fluids through the vas: two compared vasectomy with water flushing versus vasectomy alone, and one compared using water versus euflavine (which kills sperm). None found a difference between the groups in time to low sperm count. However, one trial found that the usual number of ejaculations before low sperm count was lower with euflavine than with water. One trial that compared vasectomy with and without fascial interposition was a high‐quality large study. The fascial interposition group was less likely to have vasectomy failure. However, the surgery was more difficult. Side effects were about the same in the two groups. Lastly, one trial looked at a device placed into the vas versus vasectomy without a scalpel. The intra‐vas device did not work as well for reaching a low sperm count but more men liked the method.
Most of the studies that looked at vasectomy methods were small, not done well, or had poor reports. Therefore, we cannot say if the methods work well, are safe or are liked by men. Vasectomy with fascial interposition worked better than simply cutting and tying the vas, but the surgery was more difficult. More and better research is needed on vasectomy methods.
Background
Vasectomy is a popular, highly effective, and relatively low‐cost permanent family planning method (PIP 1992). From the health payer perspective, vasectomy is one of the three least expensive methods of contraception in the US (Trussell 2009). The proportion of vasectomies that fail (defined as lack of azoospermia on semen analysis or presence of pregnancy) is generally considered to be between zero and 2%, with most studies reporting a failure rate of less than 1% (RCOG 1999; Page 2008). The three main causes of failure are operative failure, unprotected intercourse before the semen is cleared of sperm, and spontaneous early or late recanalization of the vas. Failure rates are generally lower when vasectomy is performed by more experienced surgeons (Schwingl 2000).
Complications following vasectomy are relatively uncommon with fewer than 3% of cases requiring medical attention (PIP 1992). Most common complications are hematoma, bleeding, infection, acute and chronic pain, and congestive epididymitis (RCOG 1999). Despite concern over the long‐term health risks associated with vasectomy, such as an increased risk of prostate cancer, long‐term adverse consequences have not been established (Bernal‐Delgado 1998; RCOG 1999; Cox 2002; Page 2008).
Description of the intervention
A range of techniques to occlude the vas deferens, including excision and ligation, surgical clips, thermal or electrocautery, and chemical occlusion, have been developed in an attempt to reduce complications and failure rates of the vasectomy procedure. Although the method employed varies considerably between providers and regions, excision and ligation remains the most common method of vasectomy worldwide. The occlusion techniques usually involve excision of a short length of the vas to reduce the chances of two ends of the vas rejoining (recanalization). Fascial interposition, in which one end of the vas is covered by either the sheath tissues of the vas itself or with adjacent connective tissue, is also widely used in conjunction with occlusion techniques to reduce the risk of recanalization. A controversial and less widespread practice involves leaving the testicular end of the vas unsealed to allow sperm to flow out of the vas in order to minimize pressure on and damage to the epididymis (Errey 1986). Finally, some surgeons have proposed irrigation of the distal vas deferens with sterile water or a spermicidal solution at the time of vasectomy to hasten the clearance of lingering sperm (Gandrup 1981; Mason 2002).
Two main methods are used to approach the vas for vasectomy: the traditional incisional method and the no‐scalpel technique (Li 1991; PIP 1992). These methods can be combined with any of the vas occlusion techniques already mentioned, and are the subject of a review titled 'Scalpel versus no‐scalpel incision for vasectomy' (Cook 2007).
Why it is important to do this review
Information concerning the relative effectiveness, safety, acceptability, and costs of these different vasectomy techniques is vital for decision making by both health service providers and clients. However, the majority of studies to date are retrospective case series conducted by a single surgeon. These studies are problematic as they may underestimate failure rates for a number of reasons, including lower failure rates observed in experienced surgeons, high rates for losses to follow up, short‐term follow up, rates calculated using all men (rather than those who return for follow up) as the denominator, and suspected underreporting of pregnancy by couples. In addition, comparisons between studies are difficult due to variability in the surgical techniques and follow‐up protocols used as well as different definitions of failure (Schwingl 2000). In addition, most studies do not describe the semen analysis methods they used. Ideally, the choice of vasectomy techniques should be based on the best available evidence from randomized controlled trials.
Objectives
The objective of this review was to compare the effectiveness, safety, acceptability and costs of vasectomy techniques for male sterilization. We did not consider different approaches to the vas (i.e., scalpel versus no‐scalpel), as another review addresses those issues (Cook 2007).
Methods
Criteria for considering studies for this review
Types of studies
Randomized controlled trials are included in this review. No language restrictions were placed on the reporting of the trials.
Types of participants
Men of reproductive age undergoing vasectomy for sterilization.
Types of interventions
We examined the following vasectomy techniques:
Suture ligature
Surgical clips
Thermal or electrocautery
Chemical occlusion
Vas plugs
Vas excision
Open‐ended vas
Fascial interposition
Vas irrigation
Types of outcome measures
We focused on clinically relevant outcome measures,
Primary outcomes
The primary outcome measure was azoospermia (no detectable sperm with the method used in the trial), either as the rate at post‐vasectomy follow‐up visits or the time to azoospermia.
Secondary outcomes
Secondary outcomes included the following measures:
Incidence of recanalization
Appearance of sperm in the ejaculate following a period of azoospermia
Incidence of repeat vasectomy
Adverse events including, but not limited to, vasovagal episodes, hematoma, scrotal abscess, wound infection, epididymo‐orchitis, local pain and tenderness, reaction to suture material, bleeding, chronic testicular/scrotal pain and congestive epididymitis
Cost analysis
Operating time
Consumer acceptability measures
Provider acceptability measures.
Search methods for identification of studies
Electronic searches
In February 2014, we conducted computerized searches of the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE using PubMed, POPLINE and LILACS. In addition, we searched for recent clinical trials through ClinicalTrials.gov and the International Clinical Trials Registry Platform (ICTRP). The strategies are given in Appendix 1. The earlier strategies, which also included EMBASE, are shown in Appendix 2.
Searching other resources
We obtained relevant randomized and controlled trials from a search of publications describing vas occlusion techniques for male sterilization. We searched the reference lists of all identified studies for additional, previously unidentified trials. Relevant book chapters and review articles were searched for all relevant trials. In addition, we attempted to find unpublished randomized controlled trials through personal communication with experts.
Data collection and analysis
Selection of studies
Two reviewers assessed the titles and abstracts from our literature search and evaluated copies of all possibly relevant articles to determine eligibility. Discrepancies were resolved by discussion.
Data extraction and management
Before examining the identified trials for possible inclusion, we developed and field tested a data collection form, as described in the Cochrane Reviewers' Handbook 4.2 (Clarke 2003); similar methods can now be found in Higgins 2011. Two reviewers independently collected the data on the extraction forms. We extracted the data under unblinded conditions (Berlin 1997). In addition to the outcomes measures, we systematically extracted data on the following variables: lost to follow‐up rates, type and location of health care setting (e.g., mobile or static unit and time available for the operation), surgeon experience level, age of the men, total number of men included and inclusion/exclusion criteria. Discrepancies were resolved by discussion or by consulting a third reviewer. When necessary we contacted the authors of the trials to seek additional information. Correct entry of the data was verified by one other reviewer.
Assessment of risk of bias in included studies
We assessed the methodological quality of the eligible articles, according to the principles in Higgins 2005. The assessment of the validity of studies focused on the method of generating the allocation sequence, the use and method of allocation concealment, the use and method of blinding, exclusion of participants after randomization and loss to follow up.
Data synthesis
We could not combine the clinical outcomes of any of the studies for meta‐analysis as the studies varied in type of intervention and the methods used to assess the outcomes. When possible, we described the method used by the investigators to assess objective outcomes. Peto odds ratios with 95% confidence intervals were used for dichotomous outcomes, such as azoospermia. The mean difference (MD) was used for the continuous variable of operating time. Fixed effect and random effects will give the same result if a comparison includes a single study (Higgins 2011).
Results
Description of studies
After evaluation of the abstracts, we excluded articles that were clearly not randomized controlled trials or did not focus on interventions or outcomes measures included in this review. Six studies met the inclusion criteria for the review: three on vas irrigation and one each on vas occlusion techniques, fascial interposition, and an intra‐vas device.
VAS OCCLUSION WITH CLIPS VERSUS LIGATION AND EXCISION
Gupta 1977 compared vas occlusion with two tantalum clips (no transection of the vas) versus vasectomy (transection of the vas with both ends of the vas ligated and looped back). Initially, one clip was used in the vas occlusion arm, but because leakage was noted on a vasogram, the intervention was changed to two clips being applied to each vas. This change in the intervention occurred at an unspecified point during the study. The primary outcome measure was failure to achieve azoospermia. Semen was examined at one, two and three months after vasectomy. A participant was defined as free of sperm if one specimen revealed azoospermia. The methods used for semen analysis were not described. Follow up was reported to continue for one year after vasectomy, but the nature of this follow up was not reported. Other outcome measures were adverse events and consumer acceptability. Participants in this study received antibiotics as a prophylactic measure. The study did not describe the experience level of the surgeons.
VASECTOMY WITH VAS IRRIGATION
The ancillary technique of vas irrigation was examined with vasectomy in three studies. Two trials compared vasectomy plus water irrigation versus vasectomy without irrigation (Berthelsen 1975; Mason 2002); one study examined vasectomy plus irrigation with water versus the spermicide euflavine (Gandrup 1981). The method of irrigation varied between the studies, as did the method of determining the primary outcome measures. None of these studies described the experience level of the surgeons.
Berthelsen 1975 compared vasectomy (vas excision with both ends tied combined with fascial interposition) with irrigation of the distal vas with sterile water versus vasectomy without irrigation. In the vas irrigation group a plastic cannula was inserted in the distal vas before resection of the vas and irrigated with 40 ml of sterile water. The primary outcome measure was number of ejaculations to azoospermia, which was defined as two consecutive specimens free of sperm. Participants were requested to send in every fourth ejaculate until two consecutive samples were free of sperm. The preparation was stained with a Papanicolau stain and viewed under 40x magnification. If no spermatozoa were seen under 50 fields of vision, the sample was classified as free of sperm. Other outcome measures were time to azoospermia, adverse events and procedure time.
Mason 2002 compared vasectomy (vas excision with both ends tied combined with fascial interposition) with irrigation of the distal vas (10 ml of sterile water) versus vasectomy without irrigation. In the vas irrigation group, a blunt cannula was inserted in the distal vas after resection of the vas and irrigated with 10 ml of sterile water. The primary outcome measure was time to azoospermia defined by two consecutive semen specimens. Participants provided semen for analysis at 6 and 12 weeks post‐operatively and thereafter every 4 weeks, until two consecutive specimens were free of sperm. Specimens were returned by mail, centrifuged and stained with a Papanicolau stain. Fresh semen analyses were requested if there was suspicion of recanalization, but the basis for suspicion was not described. Other outcome measures were failure to reach azoospermia, recanalization and adverse events.
Gandrup 1981 compared vasectomy (vas excision with both ends of the vas tied combined with fascial interposition) with euflavine irrigation of the distal vas (5 ml 1:100 euflavine) versus vasectomy with water irrigation of the vas (5 ml sterile water) repeated three times. In both groups, a blunt injection needle was inserted in the distal vas and irrigated before resection. The primary outcome measure was time to azoospermia. Every two weeks, beginning one week post‐operatively, the participants mailed smears from semen samples after having performed a vital staining of the spermatozoa. Under 1000x magnification, 200 fields of vision were viewed. Completely stained spermatozoa were considered to be infertile, while partially stained or unstained spermatozoa were regarded as potentially fertile. When two consecutive samples showed azoospermia, the men were declared sterile and ceased to submit specimens. Other outcome measures were number of ejaculations until azoospermia, adverse events, and incidence of recanalization.
VASECTOMY WITH AND WITHOUT FASCIAL INTERPOSITION
Sokal 2004 compared vasectomy (no scalpel approach with ligation and excision) combined with fascial interposition versus vasectomy (no scalpel approach with ligation and excision) without fascial interposition. Surgeons involved in the study were all experienced in performing vasectomies. The results of the interim analysis were partially reported earlier in Chen‐Mok 2003 (Sokal 2004). We contacted the authors to obtain supplemental information. The primary outcome measure was time to azoospermia (two consecutive semen specimens that were free of sperm and at least two weeks apart). Two weeks after surgery, each participant underwent a physical examination. Follow‐up visits, during which semen was collected and analyzed by technicians blinded to technique group, were scheduled every 4 weeks through week 34 or until vasectomy success. Semen analysis was performed according to the Semen Analysis Guidelines, which are based on WHO 1999. Other outcome measures were time to azoospermia or severe oligozoospermia (defined as 1 to < 100,000 sperm / ml semen) in two consecutive specimens at least two weeks apart and vasectomy failure based on semen analysis. Early vasectomy failure was defined as more than five million motile sperm per ml at 14 weeks or later. Late failure was more than 100,000 sperm / mL with any motility.
INTRA‐VAS DEVICE VERSUS NO‐SCALPEL VASECTOMY
Song 2006 compared an intra‐vas device versus no‐scalpel vasectomy. The shell of the intra‐vas device (IVD) was mainly urethane, and it was filled with medical grade nylon thread. The IVD measured 1 mm in outer diameter, 0.6 mm in inner diameter, and 17 mm in length. The IVD was inserted into the vasal lumen via a small incision. Two grooves near the head and tail were intended to fix the device within the vas and to prevent sperm transport between the device and the vas wall. Contraceptive success was defined as azoospermia or severe oligozoospermia (< 3 million / mL) without motile sperm. Operating time was assessed. Follow up involved visits at the 3rd and 12th months postoperatively. Participant satisfaction was assessed by questionnaire at the 12th‐month follow up.
Risk of bias in included studies
Overall, the description of study methods was poor. Only Sokal 2004 reported the methods of generating the allocation sequence and of concealing the allocation sequence. Due to the nature of the interventions, blinding of the operator was not possible. However, only Sokal 2004 clearly described whether participants and outcome assessors were blinded and Song 2006 stated that it was open. Most did not report information to judge the adequacy of the blinding methods (Schulz 2002a). Many trials did not report details concerning number and reasons for exclusions after randomization and loss to follow up for each group. More information was obtained on the interim analysis for fascial interposition study (Chen‐Mok 2003 of Sokal 2004) by contacting the authors. Two studies stated an a priori hypothesis and sample size calculation (Berthelsen 1975; Sokal 2004).
Overall the methodological quality of the studies was poor, with one exception (Sokal 2004). Inadequate allocation concealment and exclusion of participants after randomization may result in bias (Schulz 1995; Schulz 2002b). None of the trials was conducted or sponsored by a pharmaceutical company. One trial was performed by independent organizations, Family Health International and EngenderHealth (Sokal 2004).
VAS OCCLUSION WITH CLIPS VERSUS LIGATION AND EXCISION
Gupta 1977 was reported as a randomized controlled trial but did not describe the method of randomization. No information was available regarding a priori hypothesis or sample size calculation. Allocation concealment and blinding of participants or outcome assessors were not described. Losses to follow up and exclusions after randomization were not reported. Due to the unclear methods in this study and the inadequate reporting of results, the risk of bias is high. In addition to these concerns, the intervention was changed at an unspecified time during the course of the study.
VASECTOMY WITH VAS IRRIGATION
All of the studies that examined vas irrigation were of poor quality.
Berthelsen 1975 randomized using random numbers. Allocation concealment was not described. The outcome assessor was blinded. Blinding of participants was not reported. Participants were excluded after randomization because of semen analysis protocol deviations and use of general anesthesia instead of local anesthesia. The overall rate of exclusions after randomization was 36%. Loss to follow up rates greater than 20 percent may threaten the validity of trials (Strauss 2005). The a priori hypothesis stated that irrigation should reduce the number of postoperative ejaculations before azoospermia by 10 in order for the procedure to have any clinical value. Because of the long‐time lapse from operation to azoospermia, 59 men were operated on before the necessary 30 men had fulfilled the test for azoospermia.
Mason 2002 randomized by drawing lots. Allocation concealment and participant or outcome assessor blinding were not described. The number of men randomized into each group and the number of men in each group excluded after randomization because of semen analysis protocol violation was not reported. The overall rate of exclusions after randomization was 18.5%.
Gandrup 1981 randomized using random numbers. Allocation concealment was not described. The trial was described as double‐blinded. The term 'double‐blind' denotes a trial in which the participants, investigators, and assessors all remain unaware of the intervention assignments throughout the trial (Schulz 2002a). Lost to follow‐up rates were not described. There were exclusions after randomization due to incorrect preparation of smears (3.6%), but the numbers of these were not described.
VASECTOMY WITH AND WITHOUT FASCIAL INTERPOSITION
Sokal 2004 was a large, well‐conducted randomized controlled trial that examined fascial interposition. The authors provided additional details of the study design. Participants were randomized using a randomly permuted block randomization scheme using three different sizes. Sequentially‐numbered, opaque, sealed envelopes were used for allocation concealment. Rates for loss to follow up were low and similar in both groups. An a priori sample size calculation was available. Plans were to enroll 1200 men, but enrollment was halted after the interim analysis as described in the earlier report of Chen 2003.
INTRA‐VAS DEVICE VERSUS NO‐SCALPEL VASECTOMY
The randomized open trial of Song 2006 was a relatively large study with 288 that compared an intra‐vas device versus no‐scalpel method. No information was reported on method of randomization or allocation concealment nor sample size determination. Losses by the 12th month were low and similar for the two groups.
Effects of interventions
Most studies were small and underpowered except for Sokal 2004 and Song 2006. We could not aggregate the clinical outcomes of any of the studies due to variations in the interventions and the methods used to assess or report the outcomes. Furthermore, some of the outcomes were not reported in all studies. None of the trials had cost data, and only two studies provided data on acceptability. Three studies reported operating time but only one had sufficient data for analysis in RevMan.
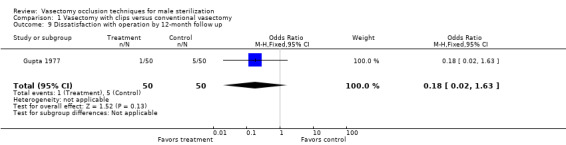
VAS OCCLUSION WITH CLIPS VERSUS LIGATION AND EXCISION
Gupta 1977 enrolled 100 participants: 50 in the vas occlusion by clips group and 50 in the vasectomy by vas ligation and excision. The number of clips used changed during the study. Losses to follow up and exclusions after randomization were not described. The groups did not differ in the numbers who reached azoospermia at two months or three months. At three months, 100% of participants were reported to have reached azoospermia, but the authors did not describe how this was evaluated. Adverse events were similar for the two groups at the 12‐month follow up: the groups did not differ in reported pain, wound infection or ligature abscess, epididymo‐orchitis, hematoma, hydrocele, and palpable nodule. Dissatisfaction with the procedure was also similar for the groups.
VASECTOMY WITH VAS IRRIGATION
Berthelsen 1975 enrolled 59 participants: 29 in the water irrigation group and 30 in the no irrigation group. A large number of exclusions (36%) followed randomization: one exclusion following randomization in each group, as the participant had a general anesthetic rather than local; 8 participants in the water irrigation group and 11 in the no irrigation group because they did not follow the instructions. Medians and interquartile ranges were reported, so no data were available for analysis with RevMan. For the primary outcome, the number of ejaculations to azoospermia, participants were paired chronologically by the time of operation, and the differences between the numbers of ejaculation were compared. This type of analysis seems incompatible with a randomized study and calls into question the methods employed. The median number of days to azoospermia was 53 (interquartile range 36.5 to 90) for the water irrigation group compared 65.5 (interquartile range 55 to 96.5) for the no irrigation group. The incidence of recanalization was zero in both groups. Adverse events were reported to have included secretion around the skin sutures, pain, bleeding, and bruising. No difference was reported in frequency of complications between the two groups, but no details of these were reported. Operation time was 10 minutes longer in the water irrigation group.
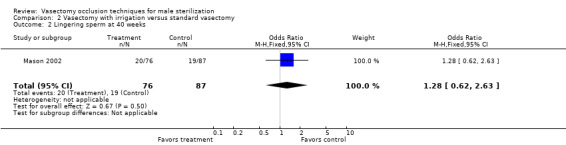
Mason 2002 enrolled 200 participants but provided no breakdown of the initial number in each group. Numerous instances of exclusions after randomization and losses to follow up were reported. The study had 22 participants who did not return any samples or who had an insufficient number of samples, and 15 sent in samples after a long delay. This left 163 of the 200 included in the analysis: 76 in water irrigation group and 87 in no irrigation group. The groups did not differ in the proportions that reached azoospermia at 16 weeks or in those with lingering sperm at 40 weeks. The groups were similar in the mean number of days to azoospermia: 28.6 (range 11.7 to 85.5) for the water irrigation group and 26.4 (range 12.5 to 79.7) for the no irrigation group. No variance data were reported so the means could not be analyzed in this review. Six of the water irrigation group and seven of the no irrigation group did not achieve azoospermia with a mean time from vasectomy of 595 and 535 days, respectively. No adverse events were reported. A transient desire to urinate was described in the irrigation group.
Gandrup 1981 enrolled 36 men in their study. Of these, 16 were in the euflavine irrigation group and 20 were in the water irrigation group. Lost to follow‐up rates and exclusions after randomization were not described. However, two participants reached azoospermia on the first semen specimens and did not appear in the denominators used for analysis. Furthermore, 3.6% of the smears were not suitable to analyze due to faulty preparation of the specimens. Medians and ranges were reported, so no data were available for analysis with RevMan. The median number of days to azoospermia was similar for the two groups: 42 (range 21 to 127) in the euflavine irrigation group compared to 33 (range 7 to 68) in the water irrigation group. The median number of ejaculations to azoospermia was 12 (range 3 to 33) in the euflavine irrigation group compared to 16 ejaculations (range 5 to 34) in the water irrigation group (P < 0.05 from paper). No instances of prostate‐vesiculitis or hemospermia were found in either group. Although no instances of recanalization were reported, the participants were not followed after they submitted two specimens that were free of sperm.
VASECTOMY WITH AND WITHOUT FASCIAL INTERPOSITION
Sokal 2004 enrolled 841 men with 419 assigned to fascial interposition and 422 to no fascial interposition. The plan was to recruit 1200 participants, but enrollment was halted after the first 400 men had completed at least 10 weeks of follow up. The interim analysis indicated a difference by age group, as discussed in the earlier report of Chen‐Mok 2003 (Sokal 2004). Follow up continued for the planned 34 weeks for those men already enrolled in the study. Using Cox's proportional hazards regression, the authors reported the hazard ratio (HR) of successful vasectomy was greater for the fascial interposition group than the no fascial interposition group (controlling for participant age and surgeon experience). For azoospermia, the HR was 1.35, and for severe oligozoospermia the HR was 1.32 (P < 0.001 reported for both). For men less than 30 years, the fascial interposition group was reportedly much more likely to achieve azoospermia (HR 2.3) (P < 0.001 from paper). Vasectomy success did not differ between the two groups, but vasectomy failure was less likely at 34 weeks in the fascial interposition group (OR 0.42; 95% CI 0.26 to 0.70). Results were indeterminate for some men. The groups did not differ in the reported adverse events at six weeks (sperm granuloma, epididymitis or orchitis, scrotal pain or swelling, hematomas, or infection). For the men with vasectomy success, no difference was noted in scrotal pain within 3 months of the 12‐month follow up. These reports were for mild or moderate pain; none reported severe pain. Sokal 2004 reported the surgery took 2 to 3 minutes longer for the fascial interposition than for non‐fascial interposition; mean times were 14.3 minutes and 11.7 minutes, respectively. In 14% of 419 cases, the fascial interposition posed some difficulty for the surgeons, but in only 2% of cases were the surgeons unable to perform the fascial interposition on one or both vas.
INTRA‐VAS DEVICE VERSUS NO‐SCALPEL VASECTOMY
Song 2006 assigned 288 men to either the intra‐vas device or the no‐scalpel method. The intra‐vas group was less likely to achieve azoospermia than the no‐scalpel group at the 3rd month (OR 0.14; 95% CI 0.06 to 0.29) as well as at the 12th month (OR 0.17; 95% CI 0.08 to 0.36). For pain, the reporting was not clear: for the intra‐vas group, 17 had pain after surgery while 10 reportedly had pain by the 12th‐month follow up (only 4 were lost to follow up). Consequently, the meaning of the OR for the later pain assessment is not clear (OR 0.44; 95% CI 0.20 to 0.96) although it appears to favor the intra‐vas group. Time for the surgical procedure was longer for the intra‐vas group than for the no‐scalpel group (WMD 4.90; 95% CI 0.59 to 9.21). By the 12th month, the intra‐vas group was slightly less likely to have had granuloma (0.29; 95% CI 0.08 to 1.06) and more likely to be satisfied with the procedure (OR 1.86; 95% CI 1.09 to 3.19).
Discussion
Summary of main results
Few controlled clinical trials examining vasectomy techniques have been conducted. Of the trials conducted, the interventions examined were vas irrigation, vas occlusion with clips, fascial interposition, and an intra‐vas device. No trials were identified that examined thermal or electrocautery, chemical occlusions, or open‐ended vas.
Vas occlusion with clips is not a widespread vasectomy technique (Schwingl 2000). Enhancing the potential for reversal is the main rationale for the use of this technique (Gupta 1977; Schwingl 2000). The trials that compared vas occlusion with clips versus a conventional vasectomy technique did not find a difference between the two groups with regard to the primary outcome of failure to reach azoospermia (Gupta 1977). Adverse events were similar for the two groups by 12 months as was dissatisfaction with the procedure. The risk of bias is high since the study was of poor quality (Schulz 2002a), and it was also small and therefore underpowered. In addition, Gupta 1977 changed the intervention partway through the study. Consequently, determining whether vas occlusion with clips is a more effective method than conventional vasectomy is not possible.
Similarly, vas irrigation is not widely used with vasectomy (Schwingl 2000). Hastening the clearance of sperm from the vas deferens and reducing time to azoospermia is the rationale for this technique. None of the three trials that examined vas irrigation found a difference between the groups in the primary outcome of time to azoospermia. Gandrup 1981, though, reported that the median number of ejaculations to azoospermia was lower in the euflavine group compared to the water irrigation group. Adverse events were uncommon and similar in both arms (Berthelsen 1975; Gandrup 1981; Mason 2002). Berthelsen 1975 found that the operating time was 10 minutes longer in the irrigation group. As with the vas occlusion studies, these trials were all of poor quality. In addition to this, the studies were relatively small and therefore underpowered. Therefore, it is unknown whether vas irrigation hastens the onset of azoospermia.
Regarding vas irrigation, some experts believe that the presence of motile sperm in semen after four to six weeks is more likely to be the result of transient early recanalization rather than residual sperm in the distal vas (D Sokal, personal communication). Thus, the success of vas irrigation based on azoospermia would be difficult to assess without an attempt to assess whether early recanalization had occurred. The occurrence of transient early recanalization appears to be relatively common with some methods of vas occlusion and would complicate the assessment of vas irrigation.
Fascial interposition is an increasingly widespread vasectomy technique and is used to separate the ends of the vas to reduce the chances of recanalization. One trial that compared vasectomy with fascial interposition versus vasectomy without fascial interposition was a high quality, large study with a low risk of bias (Sokal 2004). The trial was halted early due to the results of the interim analysis as reported earlier in Chen‐Mok 2003 (Sokal 2004). The fascial interposition group was more likely to have vasectomy success. Adverse events did not differ between the groups. Yet fascial interposition was also associated with more surgical difficulties. Fascial interposition likely improves the effectiveness of vasectomy.
An intra‐vas device was less likely to achieve azoospermia than the no‐scalpel method (Song 2006). However, the intra‐vas device was also associated with fewer adverse events.
None of the trials could be combined due to differences in the types of interventions. Variability in the nature of vasectomy interventions between trials is to be expected, as there is potential for variation not only in the techniques, but also in the comparison of types of techniques.
Quality of the evidence
The methods of determining the primary outcomes differed between studies (e.g., the timing and duration of follow up and the methods of semen analysis) or were inadequately described. Methods for semen analysis have been largely standardized (WHO 1999), but the need remains for standardization of follow‐up protocols, evaluation of success and failure, recanalization and statistical analysis.
The quality and adequacy of reporting was low for many trials, making the risk of bias high (Schulz 1995). Three trials were conducted over two decades ago when trial methods were often described inadequately and were of poorer quality. However, despite the introduction of the CONSORT guidelines (Moher 2001), Mason 2002 and Song 2006 reported the study methods inadequately. The CONSORT guidelines have since been updated (CONSORT 2009). Furthermore, most studies did not have all of the relevant outcomes, such as operating time and acceptability measures. None of the trials conducted cost analysis.
Authors' conclusions
Implications for practice.
Fascial interposition appears to improve effectiveness. High quality trials regarding other vasectomy techniques are unavailable. Practitioners should bear in mind that greater experience in a vasectomy technique is associated with higher rates of vasectomy success.
Implications for research.
High quality, adequately reported randomized controlled trials are required to compare the effectiveness, safety and acceptability of all vasectomy techniques. In addition, work is needed in the standardization of follow‐up protocols, evaluation of vasectomy success and failure, recanalization and statistical analysis.
What's new
| Date | Event | Description |
|---|---|---|
| 4 March 2014 | New citation required but conclusions have not changed | Searches were updated; no new trials were eligible for inclusion. |
History
Protocol first published: Issue 1, 2003 Review first published: Issue 3, 2004
| Date | Event | Description |
|---|---|---|
| 17 October 2011 | New search has been performed | Searches were updated. No new trials were included. Two new studies were excluded (Jee 2010; Singh 2010). An ongoing trial was updated (Sokala). |
| 9 March 2009 | New search has been performed | Updated searches; no completed RCTs were included. Added searches of clinical trials databases; listed one trial in progress. |
| 15 April 2008 | Amended | Converted to new review format. |
| 20 December 2006 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
From FHI 360:
Carol Manion helped with the literature searches.
David Grimes and David Sokal reviewed the initial manuscript. David Grimes did the second data abstraction in 2006 and 2009.
In 2014, Florence Carayon helped with the searches and reviewed the search results.
Appendices
Appendix 1. Search strategy 2014
CENTRAL (2011 to 21 Feb 2014)
vasectomy [in title, abstract, or keywords]
MEDLINE via PubMed (01 Jun 2011 to 21 Feb 2014)
(((sterilization, sexual AND (male OR men)) OR vasectomy) NOT (animal NOT human)) AND (Clinical Trial[ptyp])
POPLINE (2011 to 25 Feb 2014)
Keyword: Vasectomy Filter by keywords: Research report
LILACS (2011 to 21 Feb 2014)
(men OR male OR hombres OR homens OR masculino) AND (sterilization, sexual OR esterilizacao sexual OR esterilizacion sexual) or vasectomy OR vasecomia [Words]
ClinicalTrials.gov (01 Jun 2011 to 18 Feb 2014)
Search term: vasectomy
ICTRP (01 Jun 2011 to 25 Feb 2014)
vasectomy (general search)
Appendix 2. Previous search strategies
2011
CENTRAL (2009 to 13 Oct 2011)
vasectomy [in title, abstract, or keywords]
MEDLINE via PubMed (Mar 2009 to 13 Oct 2011)
(((sterilization, sexual AND (male OR men)) OR vasectomy)) AND ((clinical trials OR random allocation OR double‐blind method OR single‐blind method OR research design OR comparative study OR evaluation studies OR follow‐up studies OR prospective studies OR intervention studies OR evaluation studies OR randomized controlled trial[pt] OR controlled clinical trial[pt] OR clinical trial[pt] OR ((singl* OR doubl* OR tripl* OR trebl*) AND (blind OR mask)) OR random OR latin square OR control* OR prospectiv* OR volunteer) NOT (animal NOT human))
POPLINE (13 Oct 2011 and past five years)
(clinical trials / comparative studies) & ((vas occlusion / vas ligation / vasectomy / male sterilization) NOT vas reanastomosis)
LILACS (13 Oct 2011)
(men OR male OR hombres OR homens OR masculino) AND (sterilization, sexual OR esterilizacao sexual OR esterilizacion sexual) [Words] or vasectomy OR vasecomia [Words] and 2009 OR 2010 OR 2011 [Country, year publication]
ClinicalTrials.gov (13 Oct 2011)
vasectomy
ICTRP (13 Oct 2011)
vasectomy
2009
CENTRAL (24 Feb 2009)
vasectomy [in title, abstract, or keywords]
MEDLINE via PubMed (06 Mar 2009)
(((sterilization, sexual AND (male OR men)) OR vasectomy)) AND ((clinical trials OR random allocation OR double‐blind method OR single‐blind method OR research design OR comparative study OR evaluation studies OR follow‐up studies OR prospective studies OR intervention studies OR evaluation studies OR randomized controlled trial[pt] OR controlled clinical trial[pt] OR clinical trial[pt] OR ((singl* OR doubl* OR tripl* OR trebl*) AND (blind OR mask)) OR random OR latin square OR control* OR prospectiv* OR volunteer) NOT (animal NOT human))
EMBASE (06 Mar 2009)
((((vasectomy OR male(w)sterilization OR (vas AND excision) OR ((vas(w)irrigation) OR (fascial AND interposition) OR (suture ligature(w)vas) OR (vas AND irrigation) OR (open‐ended AND vas) OR (surgical(w)clips AND vas) OR (electrocautery AND vas) OR (chemical(w)occlusion AND vas)) AND ((method OR methods) OR technique OR techniques))) AND human) NOT vasovasostomy
POPLINE (06 Mar 2009)
(clinical trials / comparative studies) & ((vas occlusion / vas ligation / vasectomy / male sterilization) NOT vas reanastomosis)
LILAC (06 Mar 2009)
(men OR male OR hombres OR homens OR masculino) AND (sterilization, sexual OR esterilizacao sexual OR esterilizacion sexual) [Words] or vasectomy OR vasecomia [Words] and 2006 OR 2007 OR 2008 OR 2009 [Country, year publication]
ClinicalTrials.gov (Feb 2009)
vasectomy
ICTRP (Feb 2009)
vasectomy
Data and analyses
Comparison 1. Vasectomy with clips versus conventional vasectomy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Azoospermia at 2 months | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.84 [0.69, 4.94] |
| 2 Azoospermia at 3 months | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Pain by 12‐month follow up | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.07, 2.03] |
| 4 Wound infection or ligature abscess by 12‐month follow up | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.01, 1.95] |
| 5 Vasitis/epididymo‐orchitis by 12‐month follow up | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.04, 5.58] |
| 6 Hematoma by 12‐month follow up | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 8.21] |
| 7 Acute hydrocele by 12‐month follow up | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 8.21] |
| 8 Palpable nodule (sperm granuloma) by 12‐month follow up | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.03, 2.18] |
| 9 Dissatisfaction with operation by 12‐month follow up | 1 | 100 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.18 [0.02, 1.63] |
1.1. Analysis.
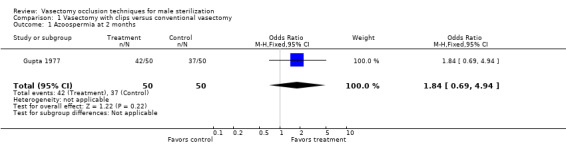
Comparison 1 Vasectomy with clips versus conventional vasectomy, Outcome 1 Azoospermia at 2 months.
1.2. Analysis.
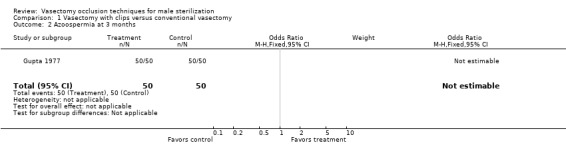
Comparison 1 Vasectomy with clips versus conventional vasectomy, Outcome 2 Azoospermia at 3 months.
1.3. Analysis.
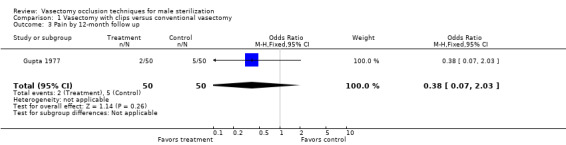
Comparison 1 Vasectomy with clips versus conventional vasectomy, Outcome 3 Pain by 12‐month follow up.
1.4. Analysis.
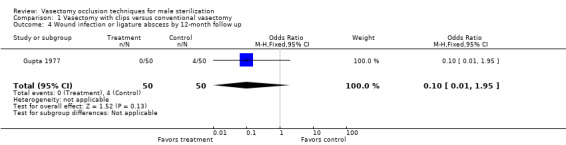
Comparison 1 Vasectomy with clips versus conventional vasectomy, Outcome 4 Wound infection or ligature abscess by 12‐month follow up.
1.5. Analysis.
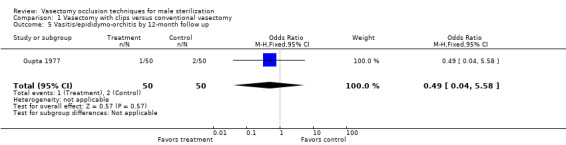
Comparison 1 Vasectomy with clips versus conventional vasectomy, Outcome 5 Vasitis/epididymo‐orchitis by 12‐month follow up.
1.6. Analysis.
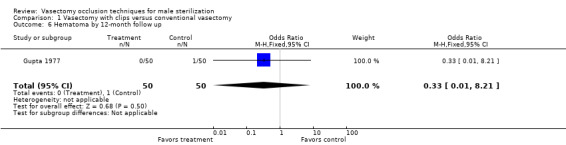
Comparison 1 Vasectomy with clips versus conventional vasectomy, Outcome 6 Hematoma by 12‐month follow up.
1.7. Analysis.
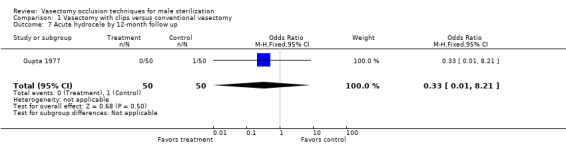
Comparison 1 Vasectomy with clips versus conventional vasectomy, Outcome 7 Acute hydrocele by 12‐month follow up.
1.8. Analysis.
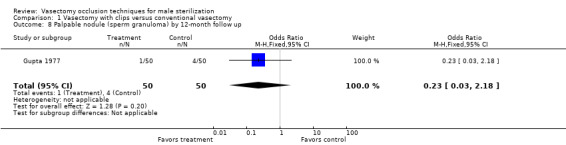
Comparison 1 Vasectomy with clips versus conventional vasectomy, Outcome 8 Palpable nodule (sperm granuloma) by 12‐month follow up.
1.9. Analysis.
Comparison 1 Vasectomy with clips versus conventional vasectomy, Outcome 9 Dissatisfaction with operation by 12‐month follow up.
Comparison 2. Vasectomy with irrigation versus standard vasectomy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Azoospermia at 16 weeks | 1 | 163 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.31, 1.28] |
| 2 Lingering sperm at 40 weeks | 1 | 163 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.62, 2.63] |
2.1. Analysis.
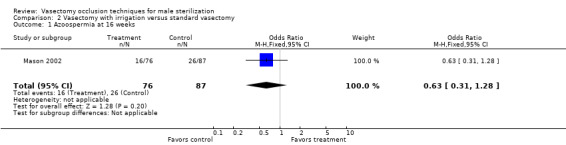
Comparison 2 Vasectomy with irrigation versus standard vasectomy, Outcome 1 Azoospermia at 16 weeks.
2.2. Analysis.
Comparison 2 Vasectomy with irrigation versus standard vasectomy, Outcome 2 Lingering sperm at 40 weeks.
Comparison 3. Vasectomy by ligation and excision, with versus without fascial interposition.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Vasectomy success by 34 weeks | 1 | 841 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.24 [0.88, 1.74] |
| 2 Vasectomy failure by 34 weeks | 1 | 841 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.26, 0.70] |
| 3 Sperm granuloma by 6 weeks | 1 | 841 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.47 [0.90, 2.41] |
| 4 Epididymitis or orchitis by 6 weeks | 1 | 841 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.04 [0.76, 5.50] |
| 5 Scrotal pain or swelling by 6 weeks | 1 | 841 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.43, 2.35] |
| 6 Hematomas by 6 weeks | 1 | 841 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.32, 3.15] |
| 7 Infection by 6 weeks | 1 | 841 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.14, 7.18] |
| 8 Mild or moderate scrotal pain within 3 months of 12‐week follow up among men with vasectomy success | 1 | 672 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.25, 1.39] |
3.1. Analysis.
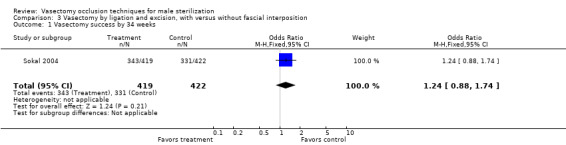
Comparison 3 Vasectomy by ligation and excision, with versus without fascial interposition, Outcome 1 Vasectomy success by 34 weeks.
3.2. Analysis.
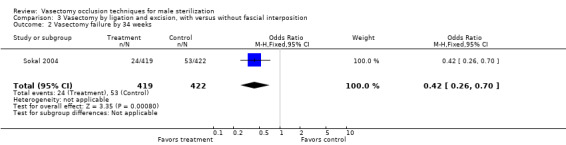
Comparison 3 Vasectomy by ligation and excision, with versus without fascial interposition, Outcome 2 Vasectomy failure by 34 weeks.
3.3. Analysis.
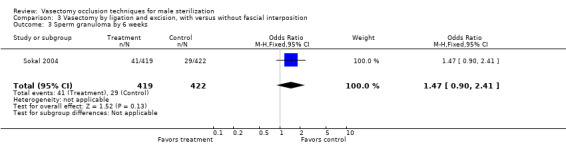
Comparison 3 Vasectomy by ligation and excision, with versus without fascial interposition, Outcome 3 Sperm granuloma by 6 weeks.
3.4. Analysis.
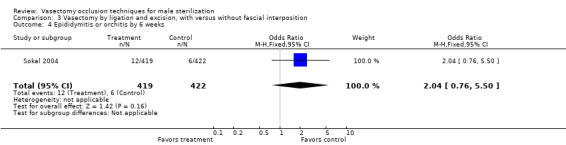
Comparison 3 Vasectomy by ligation and excision, with versus without fascial interposition, Outcome 4 Epididymitis or orchitis by 6 weeks.
3.5. Analysis.
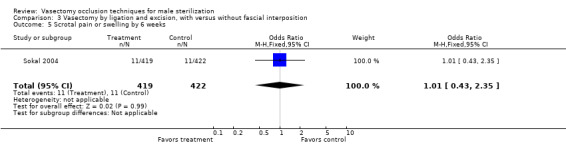
Comparison 3 Vasectomy by ligation and excision, with versus without fascial interposition, Outcome 5 Scrotal pain or swelling by 6 weeks.
3.6. Analysis.
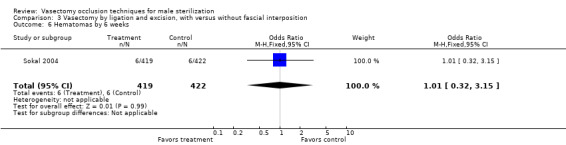
Comparison 3 Vasectomy by ligation and excision, with versus without fascial interposition, Outcome 6 Hematomas by 6 weeks.
3.7. Analysis.
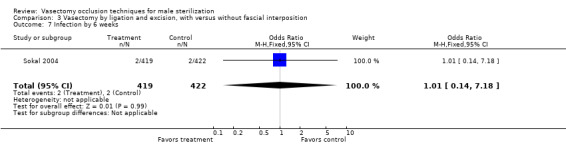
Comparison 3 Vasectomy by ligation and excision, with versus without fascial interposition, Outcome 7 Infection by 6 weeks.
3.8. Analysis.
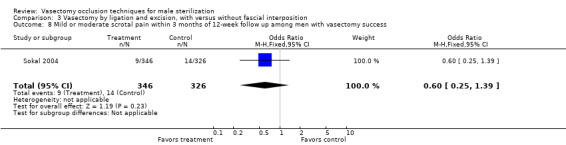
Comparison 3 Vasectomy by ligation and excision, with versus without fascial interposition, Outcome 8 Mild or moderate scrotal pain within 3 months of 12‐week follow up among men with vasectomy success.
Comparison 4. Intra‐vas device versus no‐scalpel vasectomy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Azoospermia at 3rd month | 1 | 288 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.06, 0.29] |
| 2 Azoospermia at 12th month | 1 | 288 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.08, 0.36] |
| 3 Pain with surgery | 1 | 288 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.79 [0.79, 4.06] |
| 4 Pain by 12th month | 1 | 288 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.44 [0.20, 0.96] |
| 5 Congestive epididymitis by 12th month | 1 | 288 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.09 [0.00, 1.60] |
| 6 Granuloma by 12th month | 1 | 288 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.08, 1.06] |
| 7 Satistaction with procedure at 12th month | 1 | 288 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.86 [1.09, 3.19] |
| 8 Operating time | 1 | 288 | Mean Difference (IV, Fixed, 95% CI) | 4.90 [0.59, 9.21] |
4.1. Analysis.
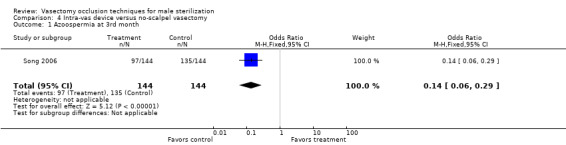
Comparison 4 Intra‐vas device versus no‐scalpel vasectomy, Outcome 1 Azoospermia at 3rd month.
4.2. Analysis.
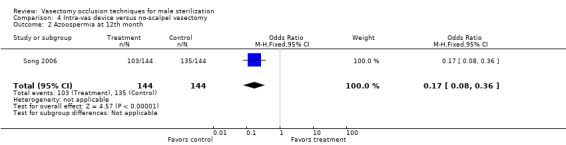
Comparison 4 Intra‐vas device versus no‐scalpel vasectomy, Outcome 2 Azoospermia at 12th month.
4.3. Analysis.
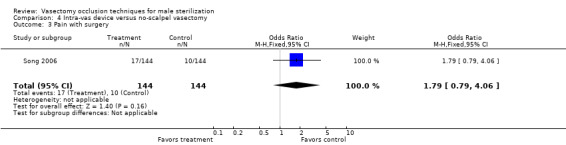
Comparison 4 Intra‐vas device versus no‐scalpel vasectomy, Outcome 3 Pain with surgery.
4.4. Analysis.
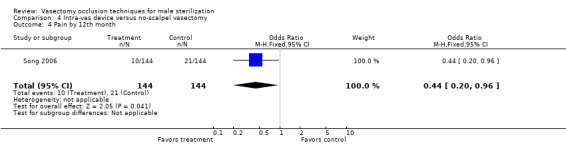
Comparison 4 Intra‐vas device versus no‐scalpel vasectomy, Outcome 4 Pain by 12th month.
4.5. Analysis.
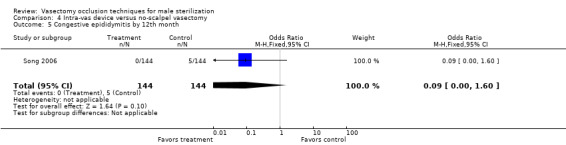
Comparison 4 Intra‐vas device versus no‐scalpel vasectomy, Outcome 5 Congestive epididymitis by 12th month.
4.6. Analysis.
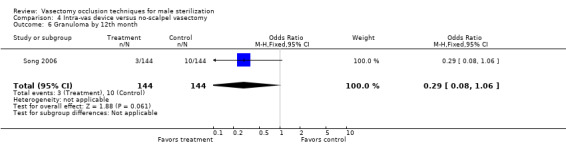
Comparison 4 Intra‐vas device versus no‐scalpel vasectomy, Outcome 6 Granuloma by 12th month.
4.7. Analysis.
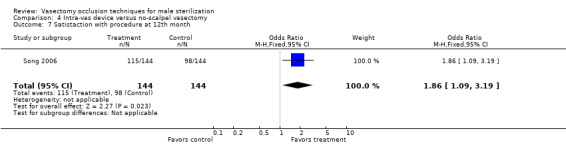
Comparison 4 Intra‐vas device versus no‐scalpel vasectomy, Outcome 7 Satistaction with procedure at 12th month.
4.8. Analysis.
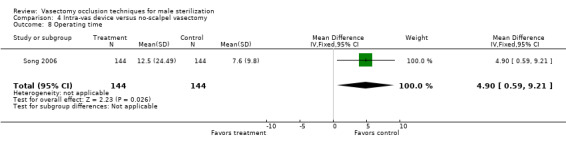
Comparison 4 Intra‐vas device versus no‐scalpel vasectomy, Outcome 8 Operating time.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Berthelsen 1975.
| Methods | Randomized controlled trial with blinding of the outcome assessor. Randomization by random numbers. The use of allocation concealment and blinding of the participants was not reported. High number of exclusions after randomization. | |
| Participants | 59 participants aged 25 to 51 years in an outpatient setting in Denmark. The inclusion and exclusion criteria were not stated. | |
| Interventions | Vasectomy (vas excision with both ends tied combined with fascial interposition) with irrigation of the distal vas with 40 ml of sterile water versus vasectomy without irrigation. | |
| Outcomes | The primary outcome measure was number of ejaculations to azoospermia. Other outcome measures were time to azoospermia, adverse events and procedure time. Medians and interquartile ranges were reported, so no data were available for analysis in this review. | |
| Notes | The report provides an a priori hypothesis and a sample size calculation. Due to the long‐time lapse from operation to azoospermia, 59 men were operated on before the necessary 30 men had fulfilled the test for azoospermia. Analysis not according to intention‐to‐threat principle. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | no information |
Gandrup 1981.
| Methods | Randomized controlled trial. Randomization by random numbers. The use of allocation concealment was not described. The report stated double‐blinding. Lost to follow‐up rates were not described. There were exclusions after randomization due to wrong preparation of smears. | |
| Participants | 36 participants aged 26 to 55 years in an outpatient setting in Denmark. Statistical significant difference in age between the 2 groups. The inclusion and exclusion criteria were not stated. | |
| Interventions | Vasectomy (vas excision with both ends of the vas tied combined with fascial interposition) with irrigation of the distal vas with 5 ml 1:100 euflavine versus vasectomy with irrigation of the vas with 5 ml sterile water repeated three times. | |
| Outcomes | The primary outcome measure was time to azoospermia. Other outcome measures were number of ejaculations until azoospermia, adverse events, and incidence of recanalization. Medians and interquartile ranges were reported, so no data were available for analysis in this review. | |
| Notes | The report does not provide an a priori hypothesis or a sample size calculation. Analysis not according to intention‐to‐threat principle. Euflavine is one of a group of compounds that have anti‐microbial activity. They have been used in the past as a mucous membrane antiseptic, as well as a limited application in urinary tract infection. Authors make the point that euflavine toxicity (local and general) has not been evaluated yet. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | no information |
Gupta 1977.
| Methods | Randomized controlled trial. The method of randomization, the use of allocation concealment and blinding of the participant or outcome assessor was not reported. Lost to follow‐up rates and exclusions after randomization were not described. | |
| Participants | 100 participants aged 35 to 50 years in a hospital setting in India. Inclusion criteria were healthy men requesting sterilization ages 35 to 50 years. Exclusion criteria were not stated. | |
| Interventions | Vas occlusion with 2 tantalum clips (Hemo Clips) with no transection of the vas versus vasectomy (transection of the vas with both ends of the vas tied and looped back). | |
| Outcomes | The primary outcome measure was failure to achieve azoospermia. Other outcome measures were adverse events and consumer acceptability. | |
| Notes | The report does not provide an a priori hypothesis or a sample size calculation. Analysis was probably not according to intention‐to‐treat principle, but it is not possible to determine due to inadequate reporting. Antibiotics were administered as prophylaxis. The intervention changed part way through the study. Initially one clip was used, but after vasograms showed leakage from the vas one was added. The paper does not account for at what point in the study this occurred. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | no information |
Mason 2002.
| Methods | Randomized controlled trial. Randomization by drawing lots. The use of allocation concealment, blinding of participant or outcome assessor was not described. High number of exclusions after randomization. | |
| Participants | 200 participants aged 26 to 62 years in the United Kingdom. The inclusion and exclusion criteria were not stated. | |
| Interventions | Vasectomy (vas excision with both ends tied combined with fascial interposition) with irrigation of the distal vas with 10 ml of sterile water versus vasectomy without irrigation. | |
| Outcomes | The primary outcome measure was time to azoospermia. Other outcome measures were failure to reach azoospermia, recanalization and adverse events. | |
| Notes | The report does not provide an a priori hypothesis or a sample size calculation. Analysis not according to intention‐to‐treat principle. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | no information |
Sokal 2004.
| Methods | Randomized controlled trial with blinding of the outcome assessor. Randomization using randomly permuted block randomization scheme using three different sizes. Allocation concealment was by sequentially numbered, sealed, opaque envelopes. Surgeons were not blinded. A priori sample size estimation provided. | |
| Participants | 841 men in an outpatient setting in eight centers (Brazil, El Salvador, Mexico (2) Nepal, Panama, Sri Lanka, and the US). The inclusion criteria were to satisfy local clinic's criteria for vasectomy and to be willing to provide prevasectomy semen sample as well as semen samples during the planned follow up. The exclusion criteria were history of vasectomy or other genital surgery, acute illness including sexually transmitted infections, history of bleeding disorder, and large varicocele or other scrotal mass. | |
| Interventions | Vasectomy (no scalpel approach with ligation and excision) combined with fascial interposition (N=419) versus vasectomy (no scalpel approach with ligation and excision) without fascial interposition (N=422). | |
| Outcomes | The primary outcome measure was time to azoospermia (two consecutive semen specimens free of sperm and at least 2 weeks apart). Other outcome measures were time to azoospermia or severe oligozoospermia in 2 consecutive specimens at least 2 weeks apart and vasectomy failure based on semen analysis. Vasectomy failure: early failure was > 5 million motile sperm/mL at week 14 or later; late failure was > 100,000 sperm/mL with any motility. The outcome was indeterminate if semen analyses did not meet criteria for success or for failure. | |
| Notes | Interim analysis was reported in Chen‐Mok 2003. Recruitment was halted after the interim analysis due to effect in favor of fascial interposition at predefined significance level. Follow up continued for all enrolled participants. Excluded from the analyses were 15 men who did not return for any semen analysis (9 fascial interposition and 6 no fascial interposition). In addition, 24 were lost to follow up. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | sequentially numbered, sealed, opaque envelopes |
Song 2006.
| Methods | Randomized controlled trial, open‐label. | |
| Participants | 288 men in China. Inclusion criteria were normal medical history, physical exam, and lab results; sperm count > 20 million/mL, motility > 50% and morphology > 30%; aged 24 to 45 years, at least one healthy child, no contraindications for sterilization, healthy partner 18 to 38 years with normal menstrual and delivery history and not using long‐term contraception. | |
| Interventions | Intra‐vas device (IVD) inserted into vasal lumen via mini‐incision (N=144); two grooves near head and tail fix device within vas and prevent sperm transport between device and vas wall versus no‐scalpel vasectomy (NSV) (N=144). | |
| Outcomes | Contraceptive success was azoospermia or severe oligozoospermia (< 3 million/mL) without motile sperm. Follow up involved visits at 3rd and 12th months postoperatively. Participant satisfaction was assessed by questionnaire at 12th month. | |
| Notes | No information on method of randomization or allocation concealment or sample size determination. 10 were lost to follow up by 12th month (4 IVD and 6 NSV). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | no information |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Clausen 1983 | Non‐randomized controlled trial using the date of birth to generate the allocation sequence. |
| Jee 2010 | Not a randomized controlled trial. Abstract mentions randomization but full text stated 'Treatment allocation was determined only by the availability of the microscope'. |
| Kothari 1978 | Did not report outcomes included in this review. |
| Nirapathpongporn 1990 | Not a randomized controlled trial. |
| Pearce 2002 | Non‐randomized controlled trial using alternate allocation. |
| Singh 2010 | Not a randomized trial. Alternate allocation was used. |
| Soebadi 1995 | Reporting was insufficient to decide if this was a randomized or non‐randomized controlled trial. We made contact with the authors but were unable to obtain further information. |
| Sokal 2013 | Study was terminated, according to ClinicalTrials.gov listing of 09 Sep 2013. FHI 360 participation had been terminated due to lack of funding. |
| Sommer 2001 | Abstract that did not report sufficient data to be included in review. Additional information sought from author but did not provide necessary outcome data for review. |
Contributions of authors
M Gallo performed the literature search for the original review. L Cook and H van Vliet extracted the data and wrote the initial review. H van Vliet verified the correct entry of data. A Pun and M Gallo advised on and edited the manuscript. L Lopez updated the review from 2006 to 2014; she reviewed the search results, incorporated new studies and data, and revised the manuscript.
Sources of support
Internal sources
No sources of support supplied
External sources
-
US Agency for International Development, USA.
Support for conducting the review and updates at FHI 360 (through 2011)
-
National Institute of Child Health and Human Development, USA.
Support for conducting the review and updates at FHI 360 (through 2014)
-
Dutch Ministry of Developing Affairs, Netherlands.
Support for conducting the initial review (HVV)
-
World Health Organization (WHO), Switzerland.
Support for conducting the initial review
Declarations of interest
L Lopez is employed at FHI 360 (formerly known as Family Health International), where the included study of Sokal 2004 was conducted. M Gallo was employed at FHI at the time of the initial review. Neither were involved in that study.
Edited (no change to conclusions)
References
References to studies included in this review
Berthelsen 1975 {published data only}
- Berthelsen JG. Peroperative irrigation of the vas deferens during vasectomy. Scandinavian Journal of Urology and Nephrology 1976;10:100‐2. [DOI] [PubMed] [Google Scholar]
Gandrup 1981 {published data only}
- Gandrup P, Berthelsen JG, Nielsen OS. Irrigation during vasectomy: a comparison between sterile water and the spermicide Euflavine. Journal of Urology 1982;127:60‐1. [DOI] [PubMed] [Google Scholar]
Gupta 1977 {published data only}
- Gupta AS, Kothari LK, Devpura TP. Vas occlusion by tantalum clips and its comparison with conventional vasectomy in man: reliability, reversibility, and complications. Fertility and Sterility 1977;28:1086‐9. [DOI] [PubMed] [Google Scholar]
Mason 2002 {published data only}
- Mason RG, Dodds L, Swami SK. Irrigation of the vas ‐ does it accelerate the clearance of sperm after vasectomy? The results of a randomized trial. British Journal of Urology International 2001; Vol. 88 Suppl (1):9.
- Mason RG, Dodds L, Swami SK. Sterile water irrigation of the distal vas deferens at vasectomy: does it accelerate clearance of sperm? A prospective randomized trial. Urology 2002;59:424‐7. [DOI] [PubMed] [Google Scholar]
Sokal 2004 {published and unpublished data}
- Chen‐Mok M, Bangiwala SI, Dominik R, Hays M, Irsula B, Sokal D. Termination of a randomized controlled trial of two vasectomy techniques. Controlled Clinical Trials 2003;24:78‐84. [DOI] [PubMed] [Google Scholar]
- Sokal D, Irsula B, Hays M, Chen‐Mok M, Barone MA. Vasectomy by ligation and excision, with or without fascial interposition: a randomized controlled trial. BioMed Central Medicine 2004;2:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Song 2006 {published data only}
- Song L, Gu Y, Lu W, Liang X, Chen Z. A phase II randomized controlled trial of a novel male contraception, an intra‐vas device. International Journal of Andrology 2006;29:489‐95. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Clausen 1983 {published data only}
- Clausen S, Lindenberg S, Lykkegaard Nielsen M, Gerstenberg TC, Praetorius B. A randomized trial of vas occlusion versus vasectomy for male contraception. Scandinavian Journal of Urology and Nephrology 1983;17:45‐6. [DOI] [PubMed] [Google Scholar]
- Gerstenberg TC, Praetorius B, Lykkegaard Nielsen M, Clausen S, Lindenberg S. Sterilization by vas occlusion without transection does not reduce postvasectomy sperm‐agglutinating antibodies in serum. A randomized trial of vas occlusion versus vasectomy. Scandinavian Journal of Urology and Nephrology 1983;17:149‐51. [DOI] [PubMed] [Google Scholar]
Jee 2010 {published data only}
Kothari 1978 {published data only}
- Kothari LK, Gupta AS. Structural changes in the human vas deferens after tantalum clip occlusion and conventional vasectomy. Fertility and Sterility 1978;29:189‐93. [DOI] [PubMed] [Google Scholar]
Nirapathpongporn 1990 {published data only}
- Nirapathpongporn A, Huber DH, Krieger JN. No‐scalpel vasectomy at the King's birthday vasectomy festival. Lancet 1990;335:894‐5. [DOI] [PubMed] [Google Scholar]
Pearce 2002 {published data only}
- Pearce I, Adeyoju A, Bhatt RI, Mokete M, Brown SCW. The effect of perioperative distal vasal lavage on subsequent semen analysis after vasectomy: a prospective randomized controlled trial. British Journal of Urology International 2002;90:282‐5. [DOI] [PubMed] [Google Scholar]
Singh 2010 {published data only}
Soebadi 1995 {published data only}
- Soebadi DM, Gardjito W, Mensink HJA. Intravasal injection of formed‐in‐place medical grade silicone rubber for vas occlusion. International Journal of Andrology 1995;18:45‐52. [DOI] [PubMed] [Google Scholar]
Sokal 2013 {published data only}
- Sokal D, Shekhar C. A randomized controlled trial of three vasectomy techniques. http://clinicaltrials.gov/ct2/show/NCT00612833 (accessed 27 Feb 2014). [NCT00612833]
Sommer 2001 {published data only (unpublished sought but not used)}
- Sommer F, Eusan A, Caspers HP, Esders K, Reddy P, Engelmann U. Effect of flushing the vasa deferentia at the time of vasectomy on the rate of azoospermia. British Journal of Urology International 2001;88(Suppl 1):9. [Google Scholar]
Additional references
Berlin 1997
- Berlin JA. Does blinding of readers affect the results of meta‐analyses. Lancet 1997;350:185‐6. [DOI] [PubMed] [Google Scholar]
Bernal‐Delgado 1998
- Bernal‐Delgado E, Latour‐Perez J, Pradas‐Arnal F, Gomez‐Lopez L. The association between vasectomy and prostate cancer: a systematic review of the literature. Fertility and Sterility 1998;70:191‐200. [DOI] [PubMed] [Google Scholar]
Clarke 2003
- Clarke M, Oxman AD, editors. Cochrane Reviewers' Handbook 4.2.0 [updated March 2003]. The Cochrane Library, Issue 2, 2003. Oxford, UK: Update Software.
CONSORT 2009
- CONSORT group. CONSORT: Transparent reporting of trials. http://www.consort‐statement.org/ (accessed 15 Jul 2009).
Cook 2007
- Cook LA, Pun A, Gallo MF, Lopez LM, Vliet HAAM. Scalpel versus no‐scalpel incision for vasectomy. Cochrane Database of Systematic Reviews 2007, Issue 2. [DOI: 10.1002/14651858.CD004112] [DOI] [PubMed] [Google Scholar]
Cox 2002
- Cox B, Sneyd MJ, Paul C, Delahunt B, Skegg DC. Vasectomy and risk of prostate cancer. Journal of the American Medical Association 2002;287:3110‐5. [DOI] [PubMed] [Google Scholar]
Errey 1986
- Errey BB, Edwards IS. Open‐ended vasectomy: an assessment. Fertility and Sterility 1986;45:843‐6. [DOI] [PubMed] [Google Scholar]
Higgins 2005
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions 4.2.5 [updated May 2005]. www.cochrane.dk/cochrane/handbook/hbook.htm. John Wiley & Sons, Ltd, (accessed 1 June 2005).
Higgins 2011
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions 5.1[updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. John Wiley & Sons, Ltd, (accessed 04 Oct 2011).
Li 1991
- Li SQ, Goldstein M, Zhu J, Huber D. The no‐scalpel vasectomy. Journal of Urology 1991;145:341‐4. [DOI] [PubMed] [Google Scholar]
Moher 2001
- Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel‐group randomised trials. Lancet 2001;357:1191‐4. [PubMed] [Google Scholar]
Page 2008
- Page ST, Amory JK, Bremner WJ. Advances in male contraception. Endocrine Reviews 2008;29:465‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
PIP 1992
- Population Information Program. Vasectomy: new opportunities. Population Reports 1992;Series D(No. 5):2‐6. [Google Scholar]
RCOG 1999
- Royal College of Obstetricians and Gynaecologists. Male and Female Sterilisation. Evidence‐Based Guideline No. 4. London: RCOG Press, 1999. [ISBN: 1 900364 23 9] [Google Scholar]
Schulz 1995
- Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. Journal of the American Medical Association 1995;273:408‐12. [DOI] [PubMed] [Google Scholar]
Schulz 2002a
- Schulz KF, Chalmers I, Altman DG. The landscape and lexicon of blinding in randomized controlled trials. Annals of Internal Medicine 2002;136:254‐9. [DOI] [PubMed] [Google Scholar]
Schulz 2002b
- Schulz KF, Grimes DA. Sample size slippages in randomized trials: exclusions and the lost and wayward. Lancet 2002;359:781‐85. [DOI] [PubMed] [Google Scholar]
Schwingl 2000
- Schwingl PJ, Guess HA. Safety and effectiveness of vasectomy. Fertility and Sterility 2000;73:923‐36. [DOI] [PubMed] [Google Scholar]
Strauss 2005
- Strauss SE, Richardson WS, Glasziou P, Haynes RB. Evidence‐based Medicine: How to Practice and Teach EBM. Third Edition. New York: Churchill Livingstone, 2005. [Google Scholar]
Trussell 2009
- Trussell J, Lalla AM, Doan QV, Reyes E, Pinto L, Gricar J. Cost effectiveness of contraceptives in the United States. Contraception 2009;79:5‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 1999
- World Health Organization. WHO Laboratory Manual for the Examination of Human Semen and Sperm‐Cervical Mucus Interaction. 4th Edition. New York: Cambridge University Press, 1999. [Google Scholar]
References to other published versions of this review
Cook 2004
- Cook L, Vliet H, Pun A, Gallo M. Vasectomy techniques for male sterilization. Human Reproduction 2004;19:2431‐2438. [DOI] [PubMed] [Google Scholar]


