Abstract
Background
Chronic venous insufficiency (CVI) is a common condition caused by valvular dysfunction with or without associated obstruction, usually in the lower limbs. It might result in considerable discomfort with symptoms such as pain, itchiness and tiredness in the legs. Patients with CVI may also experience swelling and ulcers. Phlebotonics are a class of drugs often used to treat CVI. This is an update of a review first published in 2005.
Objectives
To assess the efficacy and safety of phlebotonics administered both orally and topically for treatment of signs and symptoms of lower extremity CVI.
Search methods
For this update, the Cochrane Vascular Trials Search Co‐ordinator (TSC) searched the Specialised Register (August 2015), as well as the Cochrane Central Register of Controlled Trials (CENTRAL; 2015, Issue 7). The reference lists of the articles retrieved by electronic searches were searched for additional citations. We also contacted pharmaceutical companies and searched the World Health Organization (WHO) International Clinical Trials Registry Platform Search Portal for ongoing studies (last searched in August 2015).
Selection criteria
Randomised, double‐blind, placebo‐controlled trials (RCTs) assessing the efficacy of rutosides, hidrosmine, diosmine, calcium dobesilate, chromocarbe, Centella asiatica, disodium flavodate, french maritime pine bark extract, grape seed extract and aminaftone in patients with CVI at any stage of the disease.
Data collection and analysis
Two review authors independently extracted data and assessed the quality of included RCTs. We estimated the effects of treatment by using risk ratios (RRs), mean differences (MDs) and standardised mean differences (SMDs), according to the outcome assessed. We calculated 95% confidence interval (CIs) and percentage of heterogeneity (I2). Additionally, we performed sensitivity analyses.
Main results
We included 66 RCTs of oral phlebotonics, but only 53 trials provided quantifiable data (involving 6013 participants; mean age 50 years) for the efficacy analysis: 28 for rutosides, 10 hidrosmine and diosmine, nine calcium dobesilate, two Centella asiatica, two aminaftone, two french maritime pine bark extract and one grape seed extract. No studies evaluating topical phlebotonics, chromocarbe, naftazone or disodium flavodate fulfilled the inclusion criteria.
Moderate‐quality evidence suggests that phlebotonics reduced oedema in the lower legs compared with placebo. Phlebotonics showed beneficial effects among participants including reduced oedema (RR 0.70, 95% CI 0.63 to 0.78; I2 = 20%; 1245 participants) and ankle circumference (MD ‐4.27 mm, 95% CI ‐5.61 to ‐2.93 mm; I2 = 47%; 2010 participants). Low‐quality evidence reveals no difference in the proportion of ulcers cured with phlebotonics compared with placebo (RR 0.94, 95% CI 0.79 to 1.13; I2 = 5%; 461 participants). In addition, phlebotonics showed greater efficacy for trophic disorders, cramps, restless legs, swelling and paraesthesia, when compared with placebo. We identified heterogeneity for the variables of pain, itching, heaviness, quality of life and global assessment by participants. For quality of life, it was not possible to pool the studies because heterogeneity was high. However, high‐quality evidence suggests no differences in quality of life for calcium dobesilate compared with placebo (MD ‐0.60, 95% CI ‐2.15 to 0.95; I2 = 40%; 617 participants), and low‐quality evidence indicates that in the aminaftone group, quality of life was improved over that reported in the placebo group (MD ‐10.00, 95% CI ‐17.01 to ‐ 2.99; 79 participants). Moderate‐quality evidence shows that the phlebotonics group had greater risk of non‐severe adverse events than the placebo group (RR 1.21, 95% CI 1.05 to 1.41; I2 = 0; 3975 participants). Gastrointestinal disorders were the most frequently reported adverse events.
Authors' conclusions
Moderate‐quality evidence shows that phlebotonics may have beneficial effects on oedema and on some signs and symptoms related to CVI such as trophic disorders, cramps, restless legs, swelling and paraesthesia when compared with placebo but can produce more adverse effects. Phlebotonics showed no differences compared with placebo in ulcer healing. Additional high‐quality RCTs focused on clinically important outcomes are needed to improve the evidence base.
Plain language summary
Drugs to improve blood flow for people who have poor blood circulation in the veins of their legs
Background
Insufficient blood circulation in the veins of the legs might be caused by genetic factors, may occur after trauma, or may result from a blood clot. Poor movement of blood up the legs may cause swelling and puffiness, feelings of heaviness, tingling, cramps, pain, varicose veins and changes in skin pigmentation. If severe insufficient blood circulation occurs, ulcers and skin wasting can develop. Drugs such as natural flavonoids extracted from plants and similar synthetic products may improve blood circulation. These drugs are known collectively as venoactive drugs or phlebotonics. This review examined evidence from randomised controlled clinical trials comparing these drugs versus inactive treatment (placebo), generally given over one to three months.
Key results
In total, 66 studies (53 with quantifiable data, including 6013 participants; mean age 50 years) met the eligibility criteria for this review (current until August 2015). Moderate‐quality evidence from 13 studies (involving 1245 people) suggests that phlebotonics reduce puffiness (oedema) compared with placebo. Low quality evidence suggests there is no difference in the proportion of healed ulcers with phlebotonics compared with placebo. For quality of life, it was not possible to combine all studies because of differences between the studies. However, individual phlebotonic treatments shows high quality evidence there is no difference in quality of life for the phlebotonic calcium dobesilate. Low‐quality evidence revealed improvement of quality of life for aminaftone when compared to placebo. Furthermore evidence suggests phlebotonics have beneficial effects on trophic disorders, cramps, restless legs, swelling and tingling. However, the relevance of these findings to the overall clinical state remains unclear. Moderate‐quality evidence from 33 studies (involving 3975 people) shows that phlebotonics produce more side effects, especially gastrointestinal disorders.
Quality of the evidence
The quality of evidence was downgraded because of selective reporting for the outcome ulcer healing, for incomplete outcome data for the outcomes ulcer healing, oedema and adverse events and for unclear randomisation and imprecision of the overall results for the outcome quality of life.
Summary of findings
Summary of findings for the main comparison. Phlebotonics compared with placebo for venous insufficiency.
| Phlebotonics compared with placebo for venous insufficiency | ||||||
| Patient or population: patients with venous insufficiency Settings: hospital and ambulatory settings Intervention: phlebotonics Comparison: placebo | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Placebo | Phlebotonics | |||||
|
Oedema in the lower legs (dichotomous variable) Follow‐up: 1‐6 months |
575 per 1000 | 403 per 1000 (362 to 449) | RR 0.70 (0.63 to 0.78) | 1245 (13 studies) | ⊕⊕⊕⊝ Moderatea | Evidence of a positive effect of phlebotonics for patients with CVI regarding oedema in the lower legs with a statistically significant lower risk ratio for the phlebotonics group |
|
Oedema in the lower legs (circumference, mm) Follow‐up: 1‐12 months |
Mean oedema in the lower legs (circumference, mm) in the intervention groups was 4.27 mm lower (5.61 to 2.93 lower) | 2010 (15 studies) | ⊕⊕⊕⊝ Moderateb | Evidence of a positive effect of phlebotonics for patients with CVI regarding oedema in the lower legs with statistically significant lower mean oedema in the lower legs in the intervention group | ||
|
Ulcer cured Follow‐up: 1‐12 months |
381 per 1000 | 358 per 1000 (301 to 430) | RR 0.94 (0.79 to 1.13) | 461 (6 studies) | ⊕⊕⊝⊝ Lowc,d | No evidence of an effect of phlebotonics for patients with CVI regarding ulcer healing. Differences between phlebotonics and placebo groups were not statistically significant |
|
Quality of life: aminaftone Follow‐up: mean 6 months |
Mean quality of life in the intervention groups was
10 lower (17.01 to 2.99 lower) |
79 (1 study) | ⊕⊕⊝⊝ Lowe,f | Evidence of an effect of phlebotonics for patients with CVI regarding quality of life | ||
|
Quality of life: dobesilate Follow‐up: 2‐12 months |
Mean quality of life in the intervention groups was 0.60 lower (2.15 lower to 0.95 higher) | 617 (2 studies) | ⊕⊕⊕⊕ High | No evidence of an effect of phlebotonics for patients with CVI regarding quality of life. Differences between phlebotonics and placebo groups were not statistically significant | ||
|
Adverse events Follow‐up: 1‐12 months |
126 per 1000 | 153 per 1000 (132 to 177) | RR 1.21 (1.05 to 1.40) | 4054 (34 studies) | ⊕⊕⊕⊝ Moderateg | Evidence of a greater incidence of adverse events in the phlebotonics group than in the placebo group |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate Very low quality: We are very uncertain about the estimate | ||||||
aOne study rated as high risk of bias for incomplete outcome data (number of participants excluded after randomisation was important (51/120; 42.5%), no ITT analysis conducted) bSome studies presented unclear risk of bias cOne study rated as high risk of bias for incomplete outcome data and selective reporting because this study was not published dOne study rated as high risk of bias for selective reporting eThe generation of randomisation was unclear fThe confidence interval was wide gOne study rated as high risk of bias for incomplete outcome data (number of participants who withdrew prematurely was described, but percentage was high (34%), no ITT analysis conducted)
Background
Description of the condition
Chronic venous insufficiency (CVI) is a condition in which veins are unable to transport blood unidirectionally toward the heart with flow adapted to tissue drainage needs, temperature regulation and haemodynamic reserve, regardless of their position and activity. CVI first manifests as an increase in venous tension (venous hypertension, or high blood pressure in the veins) with or without reflux (Kurz 1999). Depending on its cause, CVI can be congenital, primary (with undetermined cause) or secondary (post‐thrombotic, post‐traumatic or other). Depending on its pathophysiology, CVI can be related to occlusion (blocked veins), reflux or both. Finally, it might depend on superficial or deep venous systems or on perforator anomalies (Porter 1995).
CVI is an important cause of discomfort and inability to work, and many people find it difficult to live with this condition. Its prevalence has not been clearly determined because available studies regarding this subject are few, and those that are available present limitations. Some studies do not cover the whole pathological spectrum and focus only on varicose veins or ulcers; others do not use standardised definitions of the illness and apply a variety of diagnostic criteria (Nicolaides 2000). As a result, prevalence has been estimated at between 1% and 50% (Evans 1999; Stanhope 1975; Van den Oever 1998). The Framingham Study showed an annual incidence of 2.6% among women and 1.9% among men (Brand 1988). In a recent publication of the Edinburgh Vein Study, incidence of CVI was reported as 1% among the general population of the UK (Robertson 2014).
Causes of CVI are unknown, although it has been associated with venous dilation, deformity and valvular venous incompetence. Trophic skin disorders and venous ulcers result from severe varicose illness (Carpentier 2000). Varicose veins have a multi‐factorial origin related to advanced age and certain lifestyles (sedentary life), pregnancy, hereditary factors and obesity. Risk of ulcers may be increased by trauma and previous episodes of deep venous thrombosis (clinical or subclinical) (Scott 1995).
Clinical manifestations of CVI differ according to stage of the illness and can include feelings of heaviness in the extremities, paraesthesia (tingling), cramps, pain, oedema (swellings), varicose veins, skin pigmentation, varicose sores and signs of skin atrophy (wasting). Symptoms are frequently related to extent of disease. Underlying venous disease (superficial, deep or both, with or without obstruction) has a major impact on both manifestations of the disease and response to treatment. Since 1994, International Consensus has been used to define and classify CVI in a standardised fashion (Porter 1995). According to this Consensus, clinical signs (C), aetiology (E), anatomical distribution (A) and physiological conditions (P) (CEAP) are used to classify CVI. A later revision of the CEAP classification established a means of differentiating between chronic venous disorder (referring to all morphology and functional abnormalities of the venous system) and CVI (reserved for more advanced stages of the disease with oedema, skin changes or venous ulcers) (Eklöf 2004). In parallel, a venous clinical severity score (ranging from none (0) to severe (3)) was established to assess pain, varicose veins, venous oedema, skin pigmentation, inflammation, induration, active ulcer (number, duration and size) and use of compression therapy (Vasquez 2010).
Description of the intervention
Surgery, sclerotherapy and mechanical compression are generally preferred treatments for CVI. However, pharmacological treatments or phlebotonics are often used because they are easy to administer, and because compliance with compressive treatments (such as elastic stockings) is often poor.
Phlebotonics represent a heterogeneous group of medications used to treat CVI. Most of these drugs are natural flavonoids extracted from plants. Synthetic products with flavonoid‐like properties are also used to treat venous disorders. In the Anatomical Therapeutic Chemical (ATC) system, phlebotonics are classified as vasoprotective agents (ATC 2015). Within this classification system, active substances are divided into different groups according to the organ or system on which they act and their therapeutic, pharmacological and chemical properties. Phlebotonics are known as venoactive drugs whose mechanism of action is not scientifically well established despite the availability of numerous studies examining their pharmacological and clinical properties. These medications are associated with effects on macrocirculation (e.g. they may improve venous tone) (Tsouderos 1991) and on microcirculatory parameters (e.g. they may decrease capillary hyperpermeability) (Behar 1988).
Why it is important to do this review
Although phlebotonics are commercialised in many countries, in others they are not widely available. In some countries, such as Spain, for certain phlebotonics (calcium dobesilate, chromocarbe and naftazone) the CVI indication has been withdrawn, and for several other phlebotonics, such as aminaftone, diosmine, hidrosmine, escin and some rutosides, conditions of use during exacerbations of CVI have been limited to two or three months by the Spanish Ministry of Health (Spanish Min. Health).
Controversy surrounds the clinical relevance of the efficacy and benefit‐risk balance of phlebotonics. Case‐control studies have found that risk of agranulocytosis is associated with some phlebotonics (Ibañez 2000; Ibáñez 2005; Kaufman 1991). As efficacy is not well defined and serious harmful effects have been associated with phlebotonics, evaluation of available evidence is needed.
Objectives
To assess the efficacy and safety of phlebotonics administered both orally and topically for treatment of signs and symptoms of lower extremity CVI.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised, double‐blind, controlled trials assessing the efficacy and/or safety of phlebotonics compared with placebo in patients with CVI at any stage of the disease. We excluded from this systematic review (SR) studies that did not meet the above criteria. We did not choose specific diagnostic classifications of CVI a priori because most of the studies were carried out before 1994 ‐ the year of the international diagnostic consensus of CVI. Therefore, we included RCTs with different diagnostic criteria. We included studies in which use of compression measures (support tights) was similar across groups.
Types of participants
Participants included males and females over 18 years of age suffering from any type of CVI. CVI could be diagnosed according to explicit clinical criteria and/or by objective instruments. Patient background, ethnicity and medical co‐morbidities at the beginning of the study did not influence the decision to include or exclude the study. We excluded studies that included patients with active thrombophlebitis and those including pregnant women.
Types of interventions
We considered the following interventions to treat CVI acceptable for inclusion: treatments including venoactive drugs or phlebotonics, administered orally or topically, at any dosage and independently of the duration of treatment, compared with placebo. We did not include in this review studies that compared phlebotonics among themselves or with any other therapeutic method (i.e. support tights or surgery).
-
Natural products.
Flavonoids: rutoside, french maritime pine bark extract, grape seed extract, diosmine and hidrosmine, disodium flavodate.
Saponosides: Centella asiatica.
Synthetic products: calcium dobesilate, naftazone, aminaftone, chromocarbe.
We excluded escin (horse chestnut seed extract), as it is covered in another Cochrane review (Pittler 2012).
Pentoxifylline is classified as a peripheral vasodilator, not as a vasoprotective agent (ATC 2015); therefore, we excluded it from this review.
Types of outcome measures
We included studies that assessed any of the following outcome measures.
Primary outcomes
Oedema in the lower limb measured by the dichotomous variable 'oedema' and the continuous variables 'ankle perimeter circumference' and 'volume of the leg'.
Specific quality of life (QoL) scales (e.g. Chronic Venous Insufficiency International Questionnaire (CIVIQ)).
Secondary outcomes
-
Assessment of CVI: objective signs
Skin manifestations such as venous ulcers and trophic alterations (e.g. lipodermatosclerosis (hardening of the skin that may cause red/brown pigmentation and is accompanied by wasting of subcutaneous fat), telangiectasia (small red points on the skin caused by permanently opened tiny blood vessels), reticular veins (dilated veins that show as a net‐like pattern on the skin), varicose veins (permanently dilated veins)).
-
Assessment of CVI: subjective symptoms
Pain in the lower legs.
Cramps in the lower legs.
Restless legs.
Itching in the lower legs.
Feeling of heaviness in the lower legs.
Swelling in the lower legs.
Paraesthesias (abnormal sensations, such as prickling, burning, tingling) in the lower legs.
Satisfaction of participants.
-
Adverse events
Adverse reactions experienced by participants during the trial, as reported by questionnaire or related by participants and specified within the publication.
Search methods for identification of studies
Electronic searches
For this update, the Cochrane Vascular Trials Search Co‐ordinator (TSC) searched the Specialised Register (August 2015), along with the Cochrane Central Register of Controlled Trials (http://www.metaxis.com/CRSWeb/Index.asp) (CENTRAL; 2015, Issue 7). See Appendix 1 for details of the search strategy used to search the CRS. The Specialised Register is maintained by the TSC and is constructed from weekly electronic searches of MEDLINE, EMBASE, CINAHL, AMED, and through handsearching relevant journals. The full list of the databases, journals and conference proceedings which have been searched, as well as the search strategies used are described in the Specialised Register section of the Cochrane Vascular module in The Cochrane Library (www.cochranelibrary.com).
Searching other resources
For this update, we searched the reference lists of articles retrieved by electronic searches for additional citations. We also contacted authors of unpublished studies.
We searched for ongoing studies in the World Health Organization (WHO) International Clinical Trials Registry Platform Search Portal (http://apps.who.int/trialsearch) (last searched August 2015, using the terms "chronic venous" AND "placebo" and the recruitment status "recruiting patients").
Data collection and analysis
Selection of studies
In the first version of this SR, two review authors (MMZ and RV, DC or EV) assessed independently the eligibility of studies identified by the searches. Some disagreements arose about the eligibility assessment; consequently, a third review author (XB) evaluated these studies independently and discussed them with the rest of the team, and a consensus opinion was reached. In the present update, two review authors (RV and SU) assessed independently the eligibility of new studies identified by the searches. A third review author (MMZ) helped to resolve disagreements.
Data extraction and management
In the update of this SR, two review authors (RV and SU) independently extracted data from new studies and entered them on a previously tested standardised form. A third review author (MMZ) checked the extracted data. Collected information includes characteristics of study participants, characteristics of intervention and control groups and outcome characteristics of every group of participants. For cross‐over studies, we extracted and analysed only data related to the first period of treatment.
Assessment of risk of bias in included studies
Two review authors (RV and SU) assessed independently the risk of bias of included studies. A third review author (MMZ) helped to resolve disagreements. We specifically assessed the randomisation method (sequence generation and allocation concealment); blinding of participants, caregivers/study researchers and outcome assessors to the intervention; whether outcome data were incomplete; and selection bias.
Once this information was gathered, review authors classified each study into one of three levels of risk of bias: low, unclear or high, based on the criteria specified in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
We also evaluated the quality of the evidence by using the GRADE (Grades of Recommendation, Assessment, Development and Evaluation Working Group) system and developed a 'Summary of findings' table (Schünemann 2011). We rated the quality (certainty) of the evidence as high, moderate, low or very low while considering several components (risk of bias, consistency, directness, precision and publication bias).
Measures of treatment effect
We estimated effects of treatment with phlebotonics by using risk ratios (RRs) for dichotomous variables and mean differences (MDs) or standardised mean differences (SMDs) for continuous variables, along with their corresponding 95% confidence intervals (CIs). We calculated SMDs when studies used different instruments to measure the same variable.
Unit of analysis issues
The unit of analysis was the individual participant.
Dealing with missing data
We analysed dichotomous variables by applying the intention‐to‐treat (ITT) principle to analyse every individual in the randomly assigned treatment group regardless of whether individuals completed treatment or withdrew prematurely from the study. We included in the ITT analysis only studies that provided data from all randomised participants, or that stated the number of participants lost during follow‐up. We numerically imputed missing values due to withdrawal of participants or loss to follow‐up as therapeutic failures in both comparative groups. For continuous variables, we analysed data as provided by study authors, either per protocol or as ITT values.
Assessment of heterogeneity
Before obtaining global effect estimators, we carried out an analysis to detect the presence of heterogeneity by using the I2 statistic. The I2 statistic describes the percentage of total variation across studies that is due to heterogeneity rather than to sampling error (Higgins 2011b). When statistical heterogeneity was high (I2 > 75%), we did not pool studies. For levels of I2 less than 50%, we applied a fixed‐effect model; for levels of I2 greater than 50% but less than 75%, we applied a random‐effects model (DerSimonian 1986).
Assessment of reporting biases
We constructed a funnel plot to assess whether oedema (dichotomous variable) was subject to publication bias.
Data synthesis
We obtained data from the included studies for variables evaluated at the end of treatment. In addition, we obtained data from measures of change when no significant baseline differences were evident between compared groups. We then pooled these together with other similar continuous outcomes.
We split outcomes of variables measured by ordinal categorical scales in the included studies into two groups of response. We considered one group as showing success (no signs or symptoms or mild manifestations) and the other as showing failure (moderate, severe or very severe persistence of signs and symptoms).
Summary of findings
We used the principles of the GRADE system to assess the quality of the body of evidence associated with main outcomes and constructed a ’Summary of findings’ (SoF) table using GRADE profiler software (GRADEpro 2008). The GRADE approach appraises the quality of a body of evidence according to the extent to which one can be confident that an estimate of effect or association reflects the item being assessed. Evaluation of the quality of a body of evidence considers within‐study risk of bias, directness of the evidence, heterogeneity in the data, precision of effect estimates and additional considerations (including risk of publication bias) (Schünemann 2011).
Two review authors (MMZ and RV) independently assessed the quality of the body of evidence on the following outcomes.
Oedema in the lower legs (dichotomous variable).
Oedema in the lower legs (circumference mm).
Quality of life.
Participants with ulcer cured.
Participants with adverse events.
Subgroup analysis and investigation of heterogeneity
Apart from the overall analysis of phlebotonics, we carried out subgroup analyses of the active principles. These included looking at the influence on results of the following phlebotonics: rutosides, hidrosmine, diosmine, calcium dobesilate, disodium flavodate, grape seed extract, french maritime pine bark extract, chromocarbe and aminaftone.
Sensitivity analysis
We performed sensitivity analyses to assess the influence on data of assumptions and decisions of review authors during the review process. We re‐analysed data by:
excluding studies that used compression measures;
excluding unpublished studies; and
excluding studies with high or unclear risk of bias.
Results
Description of studies
Details of all included studies are provided in the Characteristics of included studies, Characteristics of ongoing studies and Characteristics of excluded studies tables.
We applied no language restrictions.
Results of the search
See Figure 1.
1.
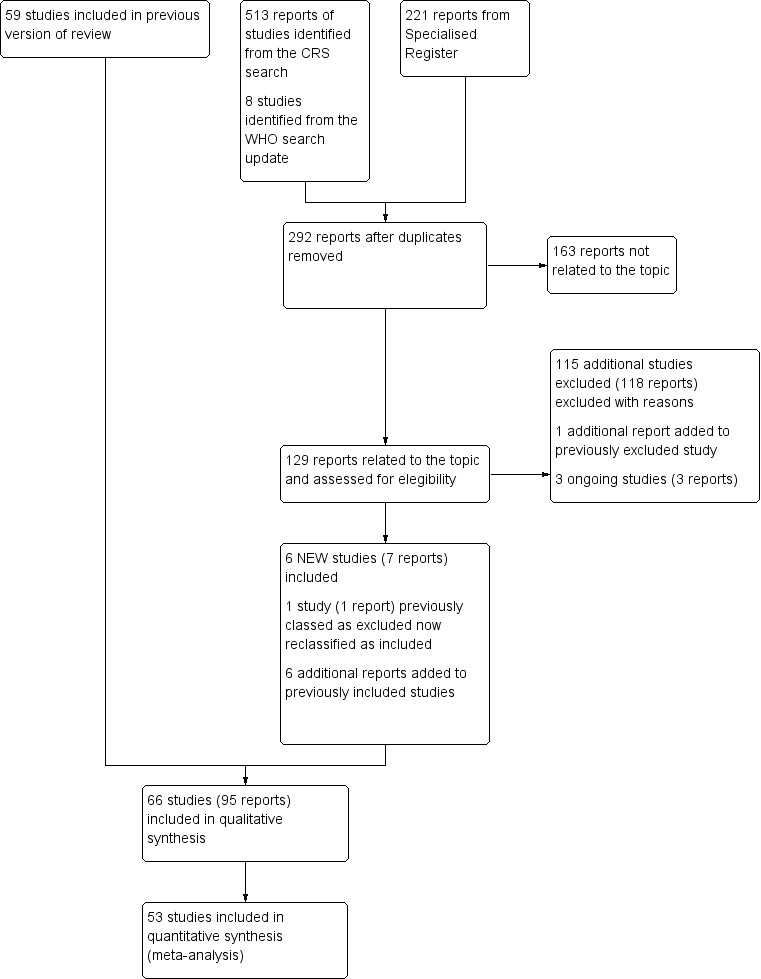
Study flow diagram.
Included studies
For this update, we identified six new included studies (Belczak 2014; DOBESILATO500/2; Martinez‐Zapata 2008; Padros 1972; Rabe 2011; Rose 1970). We reclassified one study that was previously excluded as an included study (Cesarone 2002). We obtained information from researchers about the unpublished and interrupted clinical trial DOBESILATO500/2. In total, we included 66 studies. Of the 66 included double‐blind, placebo‐controlled clinical trials, we did not include 13 studies in the efficacy analysis; 10 studies corresponded to the rutoside group (Bergqvist 1981; Cloarec 1994; Jongste 1986; Mann 1981; Nocker 1990; Prerovsky 1972; Renton 1994; Rose 1970; Rudofsky 1989; Sentou 1984), two corresponded to calcium dobesilate (Padros 1972; Pecchi 1990) and another corresponded to french bark pine extract (Petrassi 2000). Most studies were published in English, but five were published in German (Biland 1982; Kiesewetter 1997; Koscielnny 1996; Padros 1972; Pedersen 1992), eight in French (Cauwenberge 1978; Chassignolle 1994; Padros 1972; Planchon 1990; Thebaut 1985; Vin 1994; Welch 1985; Zucarelli 1987), four in Spanish (Flota‐Cervera 2008; Klüken 1971; Marinello 2002; Serralde 1990) and three in Italian (Allegra 1981; Lazzarini 1982; Pecchi 1990).
We excluded these studies from the efficacy analysis for these reasons.
Only mean data were provided without standard deviations (SDs) or standard errors (SEs) (Sentou 1984).
Medians were provided instead of means (Renton 1994).
Outcomes were reported by graph only (Nocker 1990; Rose 1970; Rudofsky 1989).
First period data were not provided in studies of cross‐over design (Padros 1972; Prerovsky 1972).
No data were provided for any variable (Bergqvist 1981; Cloarec 1994; Jongste 1986).
Measured changes were reported when significant differences in baseline were noted between compared groups (Mann 1981; Petrassi 2000).
A quasi‐randomisation method was used in which treatments were alternatively allocated depending on participants' order of arrival (Pecchi 1990).
At baseline, a significant imbalance in the ulcer area was evident between groups (1130 mm2 in the rutoside group vs 430 mm2 in the placebo group; P value = 0.039) (Mann 1981).
Of the 53 studies with oral phlebotonics included in the efficacy analysis, studied phlebotonics corresponded to 28 studies of rutosides, 10 of hidrosmine and diosmine, nine of calcium dobesilate, two of Centella asiatica, two of aminaftone, one of french maritime pine bark extract and one of grape seed extract. No studies with topical phlebotonics or chromocarbe or naftazone or disodium flavodate fulfilled the inclusion criteria. Length of treatment and participant follow‐up ranged from 28 days to four months, except for two studies, in which follow‐up lasted six months.
Overall, we included 6013 participants in the meta‐analysis; 81% were female and 19% were male; mean age was 50 years (range 32 to 62 years). The mean number of participants included per clinical trial was 113 (range 20 to 660). All participants met the respective CVI criteria of every study, although we noted variation between studies in degree of progression to CVI, as well as in diagnostic classification criteria applied. Only 28% of studies reported the diagnostic classification used. Among studies that did report on the diagnostic classification of CVI, the CEAP classification (Belczak 2014; Danielsson 2002; DOBESILATO500/2; Labs 2004; Marinello 2002; Martinez‐Zapata 2008; Rabe 2011; Vanscheidt 2002a; Vanscheidt 2002b) was used most often, followed by Widmer's classification (Casley‐Smith 1988; Cloarec 1996; Koscielnny 1996; Parrado 1999; Unkauf 1996). Wert's was the only other classification used (Kiesewetter 1997).
Differences in severity of disease were observed: Some studies (Cornu‐Thenard 1985; Danielsson 2002; Gilly 1994; Hachen 1982; Thebaut 1985) were performed with participants at early and symptomatic CVI stages, and others (Casley‐Smith 1988; DOBESILATO500/2; Guilhou 1997; Lazzarini 1982; Marinello 2002; Planchon 1990; Schultz‐Ehrenburg 1993; Vanscheidt 2002a) included participants at advanced stages because of long progression of the disease or the presence of venous ulcers. However, most studies included participants at moderate CVI stages with oedema, skin pigmentation, varicose veins and post‐thrombotic syndromes.
Ten studies specified that investigators used compression therapy (DOBESILATO500/2; Guilhou 1997; Laurent 1988; Lazzarini 1982; Marinello 2002; Martinez‐Zapata 2008; Planchon 1990; Rabe 2011; Schultz‐Ehrenburg 1993; Zucarelli 1987).
Ten studies used a visual analogue scale (VAS) to measure subjective variables (Alterkamper 1987; Cesarone 2002; DOBESILATO500/2; Labs 2004; Martinez‐Zapata 2008; Rabe 2011; Unkauf 1996; Vanscheidt 2002b; Widmer 1990; Zucarelli 1987). Other studies used ordinal categorical scales with a scoring system from ‐3 to +1 (Hachen 1982), ‐1 to + 1 (Casley‐Smith 1988), 0 to 1 (Ihme 1996), 0 to 2 (Biland 1982; Ihme 1996; Kiesewetter 1997), 0 to 3 (Allegra 1981; Arcangeli 2000; Cloarec 1996; Cornu‐Thenard 1985; Danielsson 2002; Diebschlag 1994; Dominguez 1992; Gilly 1994; Jongste 1989; Languillat 1988; Laurent 1988; Lazzarini 1982; Parrado 1999; Planchon 1990; Pointel 1986; Pulvertaft 1983; Serralde 1990; Thebaut 1985; Tsouderos 1989; Welch 1985), 0 to 4 (Balmer 1980; Chassignolle 1994; Fermoso 1992; Flota‐Cervera 2008), 0 to 5 (Rabe 2011), 0 to 7 (Labs 2004) or 0 to 9 (Dominguez 1992). Likewise, some of these scales were used to evaluate signs or objective variables such as oedema or trophic disorders. Methods used to measure oedema included metric tape to measure ankle or calf circumference and plethysmographic values (used in most studies) to determine leg volume.
Excluded studies
For this update, we excluded an additional 115 studies (Akbulut 2010; Allaert 1992; Amato 1994; Androulakis 1989; Avram 1996; Bacci 2003; Bastide 1976; Batchvarova 1989; Batchvarova 1989a; Behar 1993; Belcaro 1986; Belcaro 1995; Belcaro 2002; Belcaro 2003; Belcaro 2008; Belcaro 2008b; Bello 1990; Beltramino 1999; Bento 2006; Berson 1978; Berson 1980; Bohm 1989; Bolliger 1972; Bosse 1985; Brami 1983; Brock 1991; Brock 2001; Carstens 1985; Cesarone 1992; Cesarone 1994; Cesarone 2001b; Cesarone 2001d; Cesarone 2001e; Cesarone 2003; Cesarone 2005; Cesarone 2006; Cesarone 2006a; Cesarone 2006b; Cesarone 2006c; Cesarone 2006d; Cesarone 2010; Chiummariello 2009; Cospite 1989; Cospite 1996; Cospite 1998; Delacroix 1981; Delecluse 1991; de Parades 1990; Dustmann 1984; Erdlen 1989; Erler 1991; Fitzgerald 1967; Glinski 1999; Gonzalez‐Fajardo 1990; Henriet 1995; Honorato 1990; Horvath 1985; Incandela 2001a; Incandela 2001b; Incandela 2002b; ISRCTN5340167; Janssens 1999; Janssens 1999a; Jantet 2000; Kalus 2004; Koch 2002; Koltringer 1993; Kostering 1985; Krähenbühl 1975; Krcílek 1973; Le Dévéhat 1989; Lefebvre 1991; Marastoni 1982; Marastoni 1982a; Monreal 1994; Monreal 1997; Monteil‐Seurin 1993; Monteverde 1987; Morales 1993; Muschietti 1978; Naser‐Hijazi 2004; NCT01654016; NCT02191163; NCT02191254; NCT02191280; Neumann 1995; Neumann‐Mangoldt 1979; Nill 1970; Ottillinger 2001; Paciaroni 1982; Partsch 1981; Paul 1983; Pauschinger 1987; Pecking 1998; Pointel 1987b; Pokrovskii 2005; Questel 1983; Rabe 2011b; Rehn 1993; Rehn 1993b; Riccioni 2004; Roztocil 1977; Roztocil 2003; Sadoun 1993; Sanctis 2001; Schmeck‐Lindenau 2003; Stefanini 1996; Steiner 1990; Steiner 1992; Strefezza 2010; Topalov 1990; Tsukanov 2010; Turio 2000; Weindorf 1987; Zuccarelli 1996), making a total of 163 studies excluded for a variety of reasons (see Characteristics of excluded studies for details). In total, we excluded 31 studies because they did not use placebo as a control (Amato 1994; Avram 1996; Belcaro 1986; Belcaro 2002; Beltramino 1999; Berson 1976; Berson 1980; Brock 1991; Brock 2001; Cesarone 2005; Cesarone 2006; Cesarone 2006a; Cesarone 2006b; Cospite 1989; Cospite 1998; Honorato 1990; ISRCTN5340167; Koch 2002; Marastoni 1982a; Monreal 1994; Monteverde 1987; Muschietti 1978; Neumann 1995; Rehn 1993; Rehn 1996; Sadoun 1993; Stefanini 1996; Stegmann 1987; Strefezza 2010; Tsukanov 2010; Zicot 1993), 56 because the intervention used by researchers was not included in this SR (Akbulut 2010; Bacci 2003; Bastide 1976; Batchvarova 1989a; Behar 1993; Bello 1990; Bento 2006; Berson 1978; Bohm 1989; Bolliger 1972; Bosse 1985; Brami 1983; Carstens 1985; Cataldi 2001; Cesarone 2001b; Chiummariello 2009; Cospite 1996; de Parades 1990; Delacroix 1981; Delecluse 1991; Dustmann 1984; Erdlen 1989; Erler 1991; Henriet 1995; Horvath 1985; Janssens 1999a; Kiesewetter 2000; Koltringer 1993; Krähenbühl 1975; Krcílek 1973; Languillat 1988b; Marastoni 1982; Monteil‐Seurin 1993; Morales 1993; NCT02191163; NCT02191254; NCT02191280; Neumann‐Mangoldt 1979; Nill 1970; Ottillinger 2001; Paciaroni 1982; Partsch 1981; Paul 1983; Pauschinger 1987; Pointel 1987b; Pokrovskii 2005; Rabe 2011b; Riccioni 2004; Sanctis 2001; Steiner 1990; Steiner 1992; Topalov 1990; Turio 2000; Weindorf 1987; Widmer 1972; Zuccarelli 1996), 29 because no clinical endpoints were assessed or only outcomes not included in this SR were reported (Androulakis 1989; Auteri 1990; Belcaro 1995; Belcaro 2008; Boisseau 1995; Bort 1995; Cesarone 1992; Cesarone 1994; Cesarone 2001; Cesarone 2001c; Chant 1973; Clemens 1986; Duchene 1988; Forconi 1977; Gonzalez‐Fajardo 1990; Incandela 1995; Incandela 1996; Janssens 1999; Kalus 2004; Kostering 1985; Languillat 1989; Le Dévéhat 1989; Le Dévéhat 1997; Naser‐Hijazi 2004; Neumann 1988; Neumann 1990; Questel 1983; Roztocil 1977; Seydewitz 1992), 16 because they were not double‐blinded (Belcaro 1989; Blume 1996; Cesarone 2001a; Cesarone 2010; De Anna 1989; De Sanctis 2001; Frausini 1985; Glinski 1999; Granger 1995; Incandela 2001; Incandela 2002; Menyhei 1994; NCT01654016; Petruzzellis 2002; Roztocil 2003; Steru 1988) and seven because they were not considered RCTs (Batchvarova 1989; Belcaro 2008b; Berson 1978; Cesarone 2006c; Fitzgerald 1967; Jantet 2000; Pollastri 1982). Furthermore, we excluded 24 studies because the study population did not include patients with venous insufficiency (Allaert 1992; Belcaro 2003; Boccalon 1989; Cesarone 2001d; Cesarone 2001e; Cesarone 2002a; Cesarone 2003; Cesarone 2006d; Friederich 1978; Gouny 1999; Incandela 2001a; Incandela 2001b; Incandela 2002b; Kranendonk 1993; Lambelet 1973; Lefebvre 1991; Monreal 1997; Pecking 1998; Petruzzellis 1990; Rehn 1993b; Rish 1972; Schmeck‐Lindenau 2003; Steiner 1986; Strauss 1992).
Risk of bias in included studies
Only four studies (Labs 2004; Martinez‐Zapata 2008; Rabe 2011; Vanscheidt 2002a) presented low risk of bias (see Characteristics of included studies, Figure 2 and Figure 3).
2.
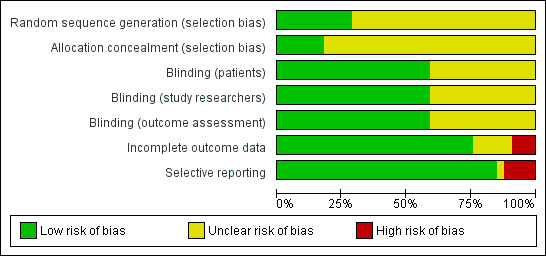
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
3.

Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
Allocation
Of the 66 studies included, 19 (29%) submitted details on the randomisation process (see Characteristics of included studies).
Only 12 (18%) studies provided an accurate explanation of the allocation concealment process. Two used the sealed envelope method (Danielsson 2002; Pedersen 1992), four used indistinguishable number packaging (Biland 1982; Padros 1972; Rabe 2011; Rose 1970), one used randomised numbered bottles provided by an external investigator (Belczak 2014), two used allocation concealment by direct phone calls (DOBESILATO500/2; Martinez‐Zapata 2008) and the remaining three studies (Jongste 1989; Labs 2004; Vanscheidt 2002a) used computerised random assignment.
Blinding
Of the 66 studies included, 39 (59%) reported that the placebo used was identical to the active treatment; thus participants, study researchers and outcome assessors were blinded to the intervention. The other studies did not mention whether placebo had identical characteristics to those of the active drug (see Characteristics of included studies).
Incomplete outcome data
Of the 66 studies included, 51 (77%) reported participant withdrawals. The percentage of withdrawn participants ranged from 0% to 42.5% (see Characteristics of included studies). Only seven (16%) studies included in the efficacy analysis stated that investigators carried out an ITT analysis (Dominguez 1992; Guilhou 1997; Ihme 1996; Martinez‐Zapata 2008; Rabe 2011; Unkauf 1996; Vanscheidt 2002a). Six studies had high risk of bias in this domain (Cauwenberge 1978; DOBESILATO500/2; Mann 1981; Rose 1970; Sentou 1984; Vanscheidt 2002b): four described an important percentage of losses (42.5% Cauwenberge 1978; 18% Mann 1981; 39% Rose 1970; 34% Vanscheidt 2002b), one interrupted recruitment because financial support was interrupted (DOBESILATO500/2) and one did not specify the number of participants included (Sentou 1984).
Selective reporting
Of the 66 studies included, 56 (85%) reported all outcomes specified in the methods section. We evaluated six studies as having high risk of selective reporting bias because we noted differences between outcomes reported in the methods and results sections (Cloarec 1994; Jongste 1986; Jongste 1989; Mann 1981), and because data before the cross‐over were not reported (Padros 1972; Rose 1970). One study was interrupted, and results of this study were not published (DOBESILATO500/2). Lazzarini 1982 provided no information about adverse events.
Figure 4 shows that all studies, except one (Casley‐Smith 1988), are located symmetrically around the effect measure at the top of the pyramid, indicating highly precise results. Apart from one imprecise study favouring phlebotonics (Casley‐Smith 1988), no small or heterogeneous studies provided results favouring placebo or phlebotonics.
4.

Funnel plot of comparison: 1 Phlebotonics vs placebo, outcome: 1.1 Oedema in the lower legs (dichotomous variable).
Effects of interventions
See: Table 1
See Table 1 for the main comparison. Results of all analysed outcomes are specified in an additional Table 6. Results of outcomes analysed by active agent (aminaftone, calcium dobesilate, Centella asiatica, diosmine and hidrosmine, french maritime pine bark extract, grape seed extract and rutosides) are specified in Table 7; Table 8; Table 9; Table 10; Table 11; Table 12; and Table 13, respectively.
1. Results of all outcomes analysed (all phlebotonics).
| Variables | Dichotomous | Continuous |
| Oedema | RR 0.70 (0.63 to 0.78) | ‐ |
| Oedema (mm) | ‐ | MD ‐4.27 (‐5.61 to ‐2.93) |
| Oedema (volume) | ‐ | SMD ‐0.38 (‐0.50 to ‐0.25) |
| Ulcer cured | NS | ‐ |
| Trophic disorders | RR 0.87 (0.81 to 0.95) | ‐ |
| Pain | ‐ | ‐ |
| Cramps | RR 0.72 (0.58 to 0.89) | ‐ |
| Restless legs | RR 0.81 (0.72 to 0.91) | ‐ |
| Itching | ‐ | ‐ |
| Heaviness | ‐ | ‐ |
| Swelling | RR 0.63 (0.50 to 0.80) | ‐ |
| Paraesthesia | RR 0.67 (0.50 to 0.88) | NS |
| Quality of life | ‐ | ‐ |
| Global assessment by the participant | ‐ | ‐ |
| Adverse events | RR 1.21 (1.05 to 1.40) | ‐ |
| Note: No measures of effect are specified when I2 was > 75% for the subgroup | ||
NS: non‐significant RR: risk ratio MD: mean difference SMD: standardised mean difference
2. Results by pharmacological group: aminaftone.
| Variables | Dichotomous | Continous |
| Oedema | RR 0.53 (0.28 to 0.99) | SMD ‐0.17 (‐0.61 to 0.28) |
| Ulcer cured | NS | ‐ |
| Trophic disorder | NS | ‐ |
| Pain | RR 0.43 (0.23 to 0.79) | ‐ |
| Cramps | RR 0.56 (0.31 to 0.99) | ‐ |
| Itching | RR 0.53 (0.31 to 0.91) | ‐ |
| Heaviness | RR 0.32 (0.17 to 0.60) | ‐ |
| Quality of live | ‐ | MD ‐10.00 (‐17.01 to ‐2.99) |
| Adverse events | NS | ‐ |
| Note: Only 1 study was analysed | ||
MD: mean difference NS: non‐significant RR: risk ratio
3. Results by pharmacological group: calcium dobesilate.
| Variables | Dichotomous | Continuous |
| Oedema | ‐ | ‐ |
| Oedema (mm) | ‐ | NS |
| Oedema (volume) | ‐ | SMD ‐0.50 (‐0.68 to ‐0.31) |
| Ulcer cured | NS | ‐ |
| Pain | RR 0.39 (0.16 to 0.93) | NS |
| Cramps | RR 0.65 (0.50 to 0.84) | ‐ |
| Restless legs | RR 0.73 (0.59 to 0.91) | NS |
| Itching | ‐ | NS |
| Heaviness | NS | NS |
| Swelling | RR 0.19 (0.08 to 0.41) | NS |
| Paraesthesia | NS | ‐ |
| Quality of life | ‐ | NS |
| Global assessment by the participant | ‐ | SMD ‐0.52 (‐0.71 to ‐0.33) |
| Adverse events | NS | ‐ |
| Note: No measures of effect are specified when I2 was > 75% for the subgroup | ||
NS: non‐significant RR: risk ratio SMD: standardised mean difference
4. Results by pharmacological group: Centella asiatica.
| Variables | Dichotomous | Continuous |
| Heaviness | NS | ‐ |
| Global assessment by the participant | RR 0.28 (0.14 to 0.57) | ‐ |
| Adverse events | NS | ‐ |
| Note: Only 1 study was analysed | ||
NS: non‐significant RR: risk ratio
5. Results by pharmacological group: diosmine, hidrosmine.
| Variables | Dichotomous | Continuous |
| Oedema | RR 0.63 (0.46 to 0.86) | ‐ |
| Oedema (mm) | ‐ | MD ‐5.98 (‐7.78 to ‐4.18) |
| Ulcer cured | NS | ‐ |
| Trophic disorder | RR 0.87 (0.81 to 0.94) | ‐ |
| Pain | NS | SMD ‐0.35 (‐0.67 to ‐0.02) |
| Cramps | RR 0.83 (0.70 to 0.98) | SMD ‐0.46 (‐0.78 to ‐0.14) |
| Restless legs | NS | ‐ |
| Itching | NS | ‐ |
| Heaviness | NS | SMD ‐0.69 (‐1.02 to ‐0.36) |
| Swelling | RR 0.70 (0.52 to 0.94) | SMD ‐0.92 (‐1.26 to ‐0.58) |
| Paraesthesia | NS | NS |
| Global assessment by the participant | ‐ | SMD ‐0.81 (‐1.14 to ‐0.47) |
| Adverse events | NS | ‐ |
| Note: No measures of effect are specified when I2 was > 75% for the subgroup | ||
MD: mean difference NS: non‐significant RR: risk ratio SMD: standardised mean difference
6. Results by pharmacological group: french maritime pine bark extract.
| Variables | Dichotomous | Continuous |
| Pain | RR 0.66 (0.48 to 0.91) | SMD ‐1.39 (‐2.09 to ‐0.69) |
| Heaviness | NS | SMD ‐1.50 (‐2.21 to ‐0.79) |
| Swelling | NS | SMD ‐1.65 (‐2.38 to ‐0.92) |
| Note: Only 1 study was analysed | ||
NS: non‐significant RR: risk ratio SMD: standardised mean difference
7. Results by pharmacological group: grape seed extract.
| Variables | Dichotomous | Continuous |
| Oedema | NS | ‐ |
| Adverse events | NS | NS |
| Note: Only 1 study was analysed | ||
NS: non‐significant
8. Results by pharmacological group: rutosides.
| Variables | Dichotomous | Continuous |
| Oedema | RR 0.72 (0.64 to 0.81) | ‐ |
| Oedema (mm) | ‐ | NS |
| Oedema (volume) | ‐ | SMD ‐0.29 (‐0.11 to ‐0.47) |
| Ulcer cured | NS | ‐ |
| Trophic disorder | NS | ‐ |
| Pain | ‐ | SMD ‐0.71 (‐1.23 to ‐0.19) |
| Cramps | RR ‐0.83 (‐1.50 to ‐0.16) | NS |
| Restless legs | NS | ‐ |
| Itching | ‐ | SMD ‐0.58 (‐1.10 to ‐0.06) |
| Heaviness | RR 0.60 (0.48 to 0.74) | ‐ |
| Swelling | RR 0.67 (0.50 to 0.88) | NS |
| Paraesthesias | RR 0.55 (0.37 to 0.83) | NS |
| Global assessment by the participant | ‐ | ‐ |
| Adverse events | RR 1.41 (1.08 to 1.83) | ‐ |
| Note: No measures of effect are specified when I2 was > 75% | ||
NS: non‐significant RR: risk ratio SMD: standardised mean difference
Of the 66 included studies, we excluded 13 studies (Bergqvist 1981; Cloarec 1994; Jongste 1986; Mann 1981; Nocker 1990; Padros 1972; Pecchi 1990; Petrassi 2000; Prerovsky 1972; Renton 1994; Rose 1970; Rudofsky 1989; Sentou 1984) from the efficacy analysis for the reasons explained under Included studies. Belczak 2014 compared three different interventions with placebo. For the analysis, we included only the comparison of aminaftone with placebo because the other two interventions were combinations of different drugs (micronised diosmine and hesperidin; coumarin and troxerutin).
Assessment of CVI: objective signs
Oedema in the lower limb
Dichotomous variable
We included 13 trials in the analysis: seven corresponding to rutosides (Cauwenberge 1972; Cauwenberge 1978; Cloarec 1996; Ihme 1996; Kriner 1985; MacLennan 1994; Welch 1985), two to calcium dobesilate (Casley‐Smith 1988; Labs 2004), two to hidrosmine and diosmine (Fermoso 1992; Planchon 1990), one to grape seed extract (Thebaut 1985) and one to aminaftone (Lazzarini 1982), with a total of 626 participants in the active treatment group and 619 in the placebo group. The overall quality of the evidence was moderate because incomplete outcome data for one study led to high risk of bias (Table 1). Pooled results were statistically significant and favoured phlebotonics (risk ratio (RR) 0.70, 95% confidence interval (CI) 0.63 to 0.78; I2 = 20%) (Analysis 1.1) (Figure 5).
1.1. Analysis.
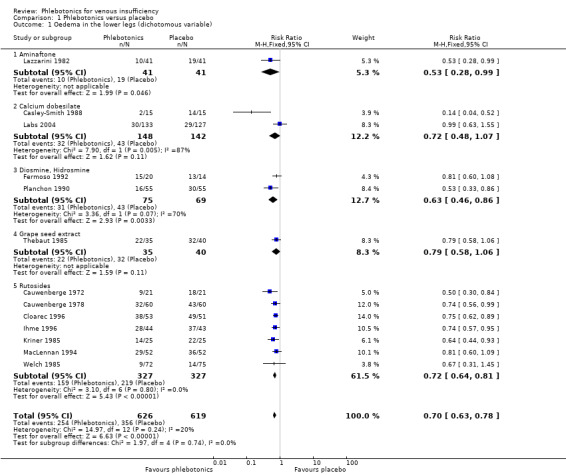
Comparison 1 Phlebotonics versus placebo, Outcome 1 Oedema in the lower legs (dichotomous variable).
5.
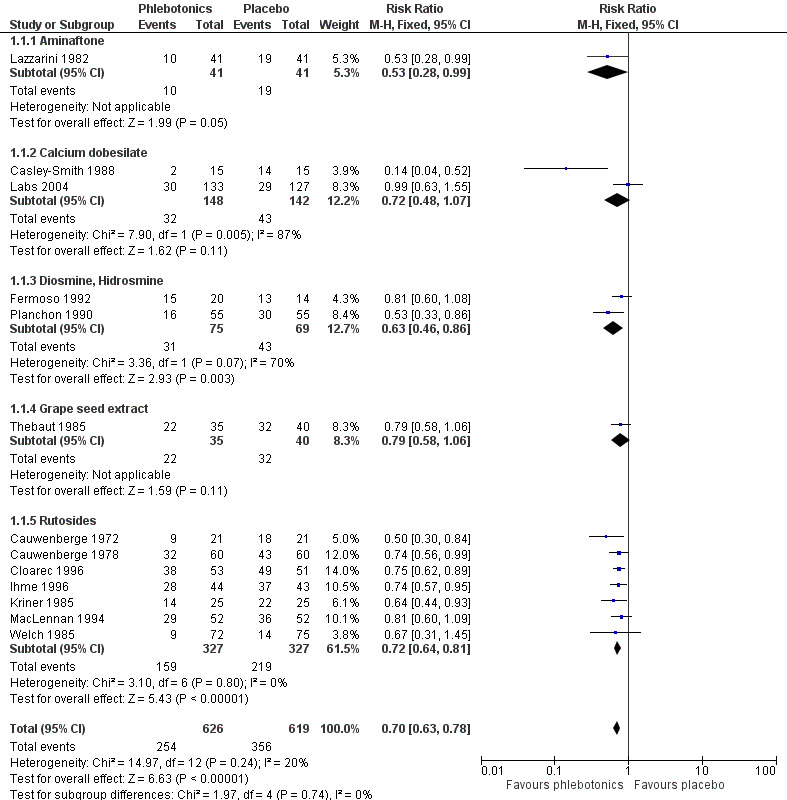
Forest plot of comparison: 1 Phlebotonics vs placebo, outcome: 1.1 Oedema in the lower legs (dichotomous variable).
Continuous variables
Ankle perimeter circumference
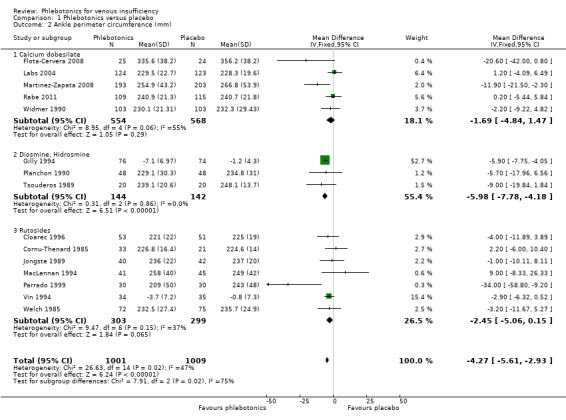
We included 15 studies in the analysis: seven corresponding to rutosides (Cloarec 1996; Cornu‐Thenard 1985; Jongste 1989; MacLennan 1994; Parrado 1999; Vin 1994; Welch 1985), five to calcium dobesilate (Flota‐Cervera 2008; Labs 2004; Martinez‐Zapata 2008; Rabe 2011; Widmer 1990) and three to diosmine (Gilly 1994; Planchon 1990; Tsouderos 1989), with a total of 1001 participants given active treatment and 1009 given placebo. The overall quality of the evidence was moderate because 12 studies had unclear risk of bias. Pooled results significantly favoured phlebotonics (Analysis 1.2) (mean difference (MD) ‐4.27 mm, 95% CI ‐5.61 to ‐2.93; I2 = 47%).
1.2. Analysis.
Comparison 1 Phlebotonics versus placebo, Outcome 2 Ankle perimeter circumference (mm).
Volume of the leg
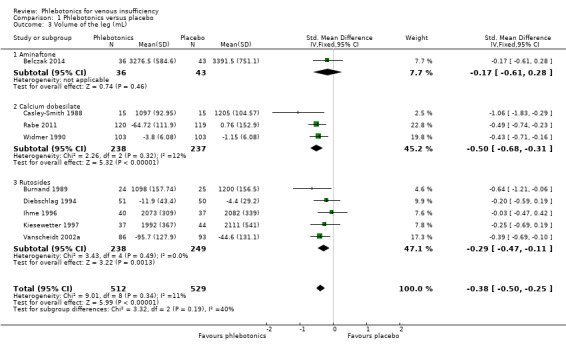
We included nine studies in the analysis: five corresponding to rutosides (Burnand 1989; Diebschlag 1994; Ihme 1996; Kiesewetter 1997; Vanscheidt 2002a), three to calcium dobesilate (Casley‐Smith 1988; Rabe 2011; Widmer 1990) and one to aminaftone (Belczak 2014), with a total of 512 participants treated with phlebotonics and 529 with placebo. Pooled results significantly favoured phlebotonics (Analysis 1.3) (standardised mean difference (SMD) ‐0.38 mL, 95% CI ‐0.50 to ‐0.25; I2 = 11%).
1.3. Analysis.
Comparison 1 Phlebotonics versus placebo, Outcome 3 Volume of the leg (mL).
Skin manifestations
Ulcer cured
Dichotomous variable
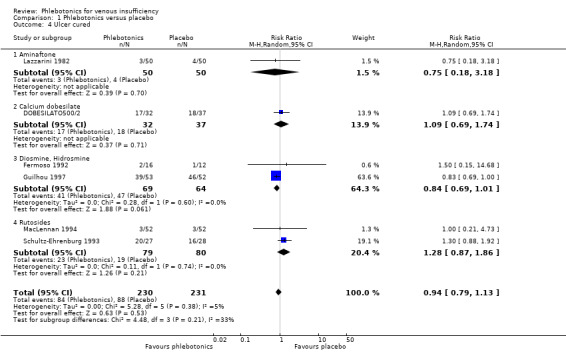
We included six trials in the analysis: one on aminaftone (Lazzarini 1982), one on calcium dobesilate (DOBESILATO500/2), two on diosmine (Fermoso 1992; Guilhou 1997) and two on rutoside (MacLennan 1994; Schultz‐Ehrenburg 1993), with a total of 230 participants in the active treatment group and 231 in the placebo group. Pooled results of these six studies showed no statistically significant differences between phlebotonics and placebo (Analysis 1.4) (RR 0.94; 95% CI 0.79 to 1.13; I2 = 5%). The quality of the evidence was low (Table 1).
1.4. Analysis.
Comparison 1 Phlebotonics versus placebo, Outcome 4 Ulcer cured.
Trophic disorders
Dichotomous variable
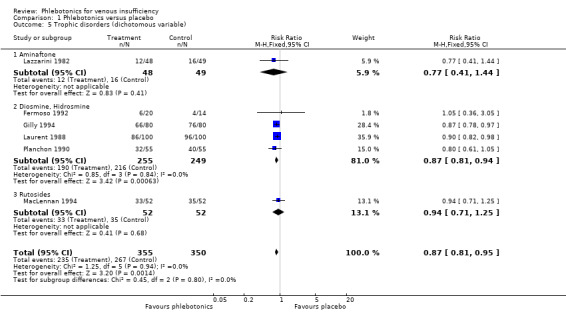
We included six studies in the analysis: four on hidrosmine and diosmine (Fermoso 1992; Gilly 1994; Laurent 1988; Planchon 1990), one on aminaftone (Lazzarini 1982) and one on rutosides (MacLennan 1994), with a total of 355 participants in the phlebotonics group and 350 in the placebo group. Pooled results significantly favoured phlebotonics (Analysis 1.5) (RR 0.87, 95% CI 0.81 to 0.95; I2 = 0%).
1.5. Analysis.
Comparison 1 Phlebotonics versus placebo, Outcome 5 Trophic disorders (dichotomous variable).
Telangiectasia, reticular veins and varicose veins
Included studies did not report data on improvement in skin signs such as telangiectasia, reticular veins and varicose veins. Only Fermoso 1992 reported results regarding varicose veins. Before treatment, 3/16 (18.8%) participants presented varicose veins in the hidrosmine group and 2/12 participants in the placebo group (16.7%). After treatment, one participant from the hidrosmine group was cured of varicose veins, and no participants from the placebo group were cured.
Assessment of CVI: subjective symptoms
Pain in the lower legs
Dichotomous variable
We included 20 trials in the analysis: 10 on rutosides (Balmer 1980; Cauwenberge 1972; Cauwenberge 1978; Jongste 1989; Klüken 1971; Languillat 1988; Pedersen 1992; Pulvertaft 1983; Vanscheidt 2002a; Welch 1985), four on calcium dobesilate (Casley‐Smith 1988; Flota‐Cervera 2008; Hachen 1982; Widmer 1990), four on diosmine and hidrosmine (Biland 1982; Dominguez 1992; Fermoso 1992; Planchon 1990), one on aminaftone (Lazzarini 1982) and one on french maritime pine bark extract (Arcangeli 2000), with a total of 1294 participants treated with phlebotonics and 953 with placebo (Analysis 1.6). The analysis showed heterogeneity (I2 = 78%); therefore, we did not pool the data.
1.6. Analysis.
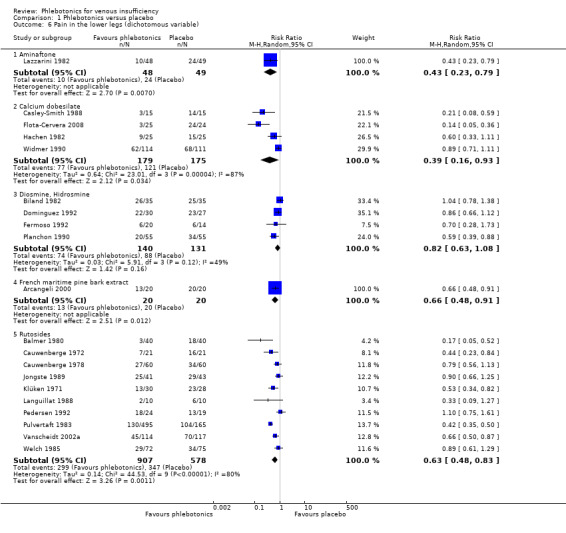
Comparison 1 Phlebotonics versus placebo, Outcome 6 Pain in the lower legs (dichotomous variable).
Continuous variable
We included nine studies in the analysis: four on calcium dobesilate (DOBESILATO500/2; Marinello 2002; Martinez‐Zapata 2008; Rabe 2011), three on rutosides (Cloarec 1996; Cornu‐Thenard 1985; Parrado 1999), one on diosmine (Gilly 1994) and one on french maritime pine bark extract (Arcangeli 2000), with a total of 588 participants assigned to phlebotonics and 597 to placebo (Analysis 1.7). The analysis showed heterogeneity (I2 = 80%); therefore, we did not pool the data.
1.7. Analysis.
Comparison 1 Phlebotonics versus placebo, Outcome 7 Pain in the lower legs (continuous variable).
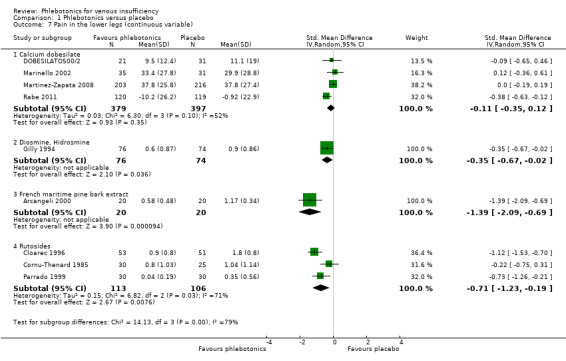
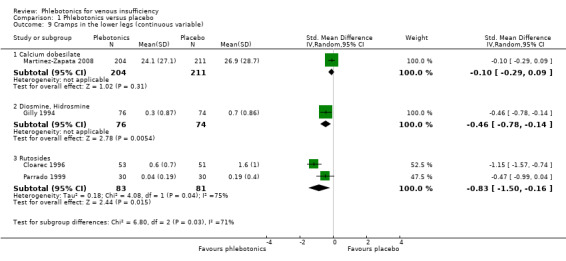
Cramps in the lower legs
Dichotomous variable
We included 14 studies in the analysis: eight on rutosides (Balmer 1980; Cauwenberge 1978; Jongste 1989; Languillat 1988; Pedersen 1992; Pulvertaft 1983; Vin 1994; Welch 1985), three on diosmine and hidrosmine (Biland 1982; Fermoso 1992; Planchon 1990), two on calcium dobesilate (Casley‐Smith 1988; Widmer 1990) and one on aminaftone (Lazzarini 1982), with a total of 1072 participants treated with phlebotonics and 721 with placebo (Analysis 1.8). Pooled results significantly favoured phlebotonics (RR 0.72, 95% CI 0.58 to 0.89; I2 = 73%).
1.8. Analysis.
Comparison 1 Phlebotonics versus placebo, Outcome 8 Cramps in the lower legs (dichotomous variable).
Continuous variable
We included four studies in the analysis: two on rutosides (Cloarec 1996; Parrado 1999), one on calcium dobesilate (Martinez‐Zapata 2008) and one on diosmine (Gilly 1994), with 363 participants treated with phlebotonics and 366 with placebo (Analysis 1.9). The analysis showed heterogeneity (I2 = 86%); therefore, we did not pool the data.
1.9. Analysis.
Comparison 1 Phlebotonics versus placebo, Outcome 9 Cramps in the lower legs (continuous variable).
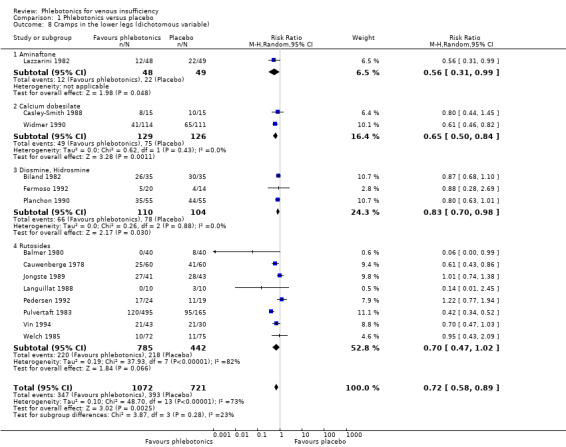
Restless legs
Dichotomous variable
We included seven studies in the analysis: four on rutosides (Balmer 1980; Cauwenberge 1978; Jongste 1989; Pedersen 1992), two on calcium dobesilate (Casley‐Smith 1988; Widmer 1990) and one on diosmine (Biland 1982). A total of 329 participants were treated with phlebotonics and 323 with placebo (Analysis 1.10). Pooled results significantly favoured phlebotonics (RR 0.81, 95% CI 0.72 to 0.91; I2 = 18%).
1.10. Analysis.
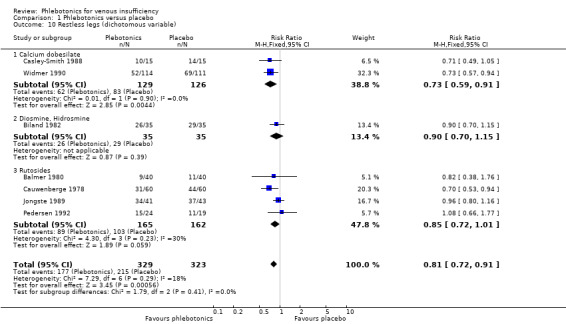
Comparison 1 Phlebotonics versus placebo, Outcome 10 Restless legs (dichotomous variable).
Itching in the lower legs
Dichotomous variable
We included four studies in the analysis: two on rutoside (Pedersen 1992; Vanscheidt 2002a), one on hidrosmine (Fermoso 1992) and one on aminaftone (Lazzarini 1982). A total of 206 participants were included in the active treatment group and 199 in the placebo group (Analysis 1.11). The analysis showed heterogeneity (I2 = 92%); therefore, we did not pool the data.
1.11. Analysis.
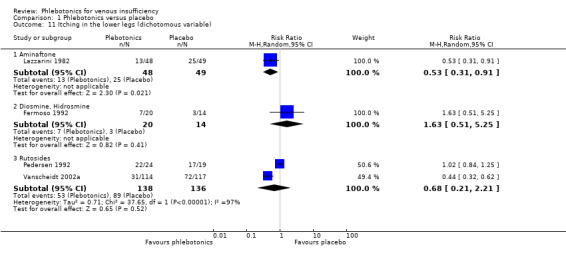
Comparison 1 Phlebotonics versus placebo, Outcome 11 Itching in the lower legs (dichotomous variable).
Continuous variable
We included two studies in the analysis: one on calcium dobesilate (Martinez‐Zapata 2008) and one on rutosides (Parrado 1999). A total of 234 participants were treated with phlebotonics and 242 with placebo (Analysis 1.12). The analysis showed heterogeneity (I2 = 82%), and we did not pool the data.
1.12. Analysis.
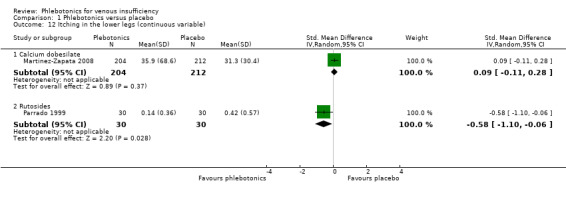
Comparison 1 Phlebotonics versus placebo, Outcome 12 Itching in the lower legs (continuous variable).
Feeling of heaviness in the lower legs
Dichotomous variable
We included 19 studies in the analysis: nine on rutosides (Cauwenberge 1972; Cauwenberge 1978; Jongste 1989; Languillat 1988; Pedersen 1992; Pulvertaft 1983; Vanscheidt 2002a; Vin 1994; Welch 1985), four on diosmine and hidrosmine (Dominguez 1992; Fermoso 1992; Planchon 1990; Tsouderos 1989), three on calcium dobesilate (Casley‐Smith 1988; Hachen 1982; Widmer 1990), one on aminaftone (Lazzarini 1982), one on Centella asiatica (Pointel 1986) and one on french maritime pine bark extract (Arcangeli 2000). A total of 1257 participants were included in the active treatment group and 909 in the placebo group (Analysis 1.13). The analysis showed heterogeneity (I2 = 80%), and we did not pool the data.
1.13. Analysis.
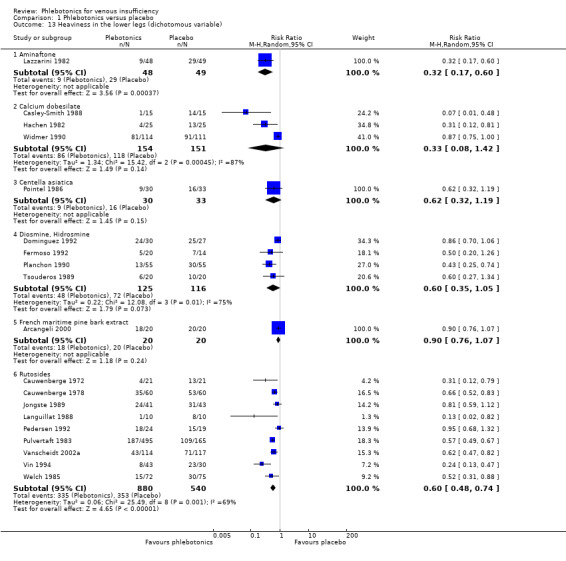
Comparison 1 Phlebotonics versus placebo, Outcome 13 Heaviness in the lower legs (dichotomous variable).
Continuous variable
We included 10 studies in the analysis: six on rutosides (Alterkamper 1987; Cloarec 1996; Cornu‐Thenard 1985; Diebschlag 1994; Parrado 1999; Unkauf 1996), two on calcium dobesilate (Marinello 2002; Martinez‐Zapata 2008), one on diosmine (Gilly 1994) and one on french maritime pine bark extract (Arcangeli 2000). A total of 557 participants were included in the active treatment group and 557 in the placebo group (Analysis 1.14). The analysis showed heterogeneity (I2 = 91%); therefore, we did not pool the data.
1.14. Analysis.
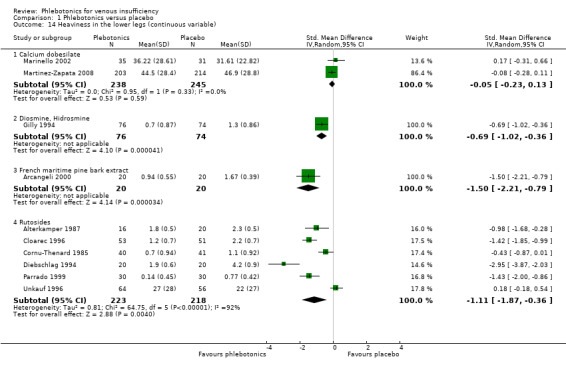
Comparison 1 Phlebotonics versus placebo, Outcome 14 Heaviness in the lower legs (continuous variable).
Swelling in the lower legs
Dichotomous variable
We included 14 studies in the analysis: nine on rutosides (Balmer 1980; Cauwenberge 1978; Jongste 1989; Kriner 1985; Languillat 1988; Pedersen 1992; Vanscheidt 2002a; Vin 1994; Welch 1985), two on calcium dobesilate (Casley‐Smith 1988; Hachen 1982), two on diosmine and hidrosmine (Biland 1982; Fermoso 1992) and one on french maritime pine bark extract (Arcangeli 2000), with 544 participants included in the active treatment group and 528 in the placebo group (Analysis 1.15). Pooled results significantly favoured phlebotonics (RR 0.63, 95% CI 0.50 to 0.80; I2 = 69%).
1.15. Analysis.
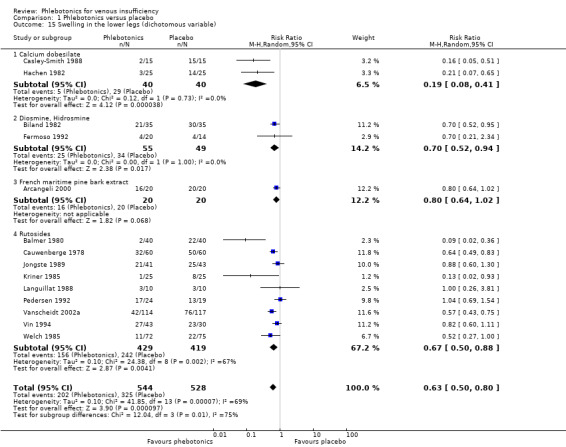
Comparison 1 Phlebotonics versus placebo, Outcome 15 Swelling in the lower legs (dichotomous variable).
Continuous variable
We included six studies in the analysis: three on rutosides (Cloarec 1996; Diebschlag 1994; Unkauf 1996), one on diosmine (Gilly 1994), one on calcium dobesilate (Martinez‐Zapata 2008) and one on french maritime pine bark extract (Arcangeli 2000), with 436 participants assigned to active treatment and 435 to placebo (Analysis 1.16). The analysis showed heterogeneity (I2 = 95%), and we did not pool the data.
1.16. Analysis.
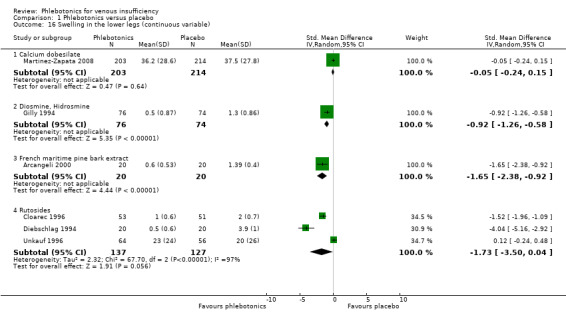
Comparison 1 Phlebotonics versus placebo, Outcome 16 Swelling in the lower legs (continuous variable).
Paraesthesia in the lower legs
Dichotomous variable
We included nine studies in the analysis: four on rutosides (Balmer 1980; Cauwenberge 1978; Pulvertaft 1983; Welch 1985), three on calcium dobesilate (Casley‐Smith 1988; Hachen 1982; Widmer 1990) and two on diosmine and hidrosmine (Fermoso 1992; Planchon 1990), with 896 participants assigned to active treatment and 560 to placebo (Analysis 1.17). Pooled results significantly favoured phlebotonics (RR 0.67, 95% CI 0.50 to 0.88; I2 = 72%).
1.17. Analysis.
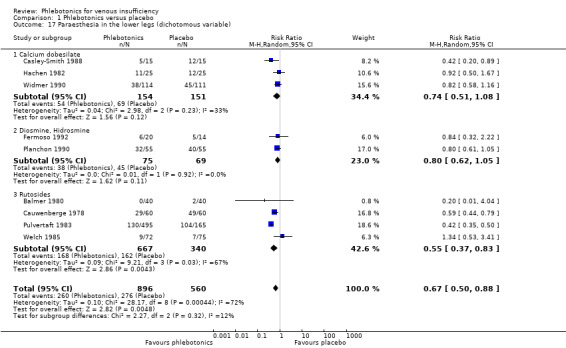
Comparison 1 Phlebotonics versus placebo, Outcome 17 Paraesthesia in the lower legs (dichotomous variable).
Continuous variable
We included two studies in the analysis: one on diosmine (Gilly 1994) and one on rutoside (Cornu‐Thenard 1985), with 97 participants assigned to active treatment and 91 to placebo (Analysis 1.18). Outcomes of the analysis were not statistically significantly different between phlebotonics and placebo (SMD ‐0.15, 95% CI ‐0.44 to 0.13; I2 = 0%).
1.18. Analysis.
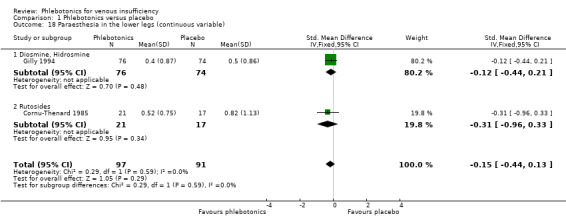
Comparison 1 Phlebotonics versus placebo, Outcome 18 Paraesthesia in the lower legs (continuous variable).
Global assessment measures
Quality of life
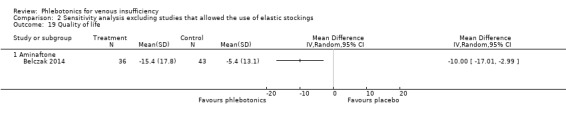
Five studies (Belczak 2014; Martinez‐Zapata 2008; Rabe 2011; Vanscheidt 2002a; Vanscheidt 2002b) evaluated quality of life (QoL). Vanscheidt 2002a and Vanscheidt 2002b assessed QoL by using a questionnaire (EuroQol Measure of Health‐Related QoL and Freiburg Life Quality Assessment, respectively) and therefore did not provide quantifiable results. Martinez‐Zapata 2008 and Rabe 2011 evaluated QoLvia the Chronic Venous Insufficiency International Questionnaire (CIVIQ).Belczak 2014 used a specific questionnaire for chronic venous disease adapted from Cesarone 2006b. It was not possible to pool results of these three studies because heterogeneity was assessed at 76% (Analysis 1.19).
1.19. Analysis.
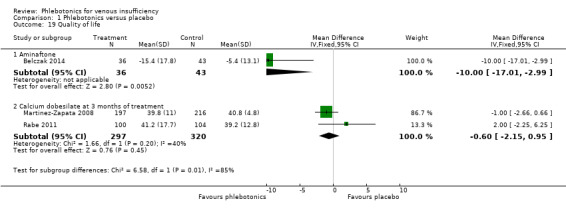
Comparison 1 Phlebotonics versus placebo, Outcome 19 Quality of life.
The subgroup analysis of aminaftone showed favourable results compared with placebo, but the confidence interval was wide because few participants were included (MD ‐10.00, 95% CI ‐17.01 to ‐ 2.99). However, pooled results of the two studies of dobesilate were not statistically significantly different between phlebotonics and placebo (MD ‐0.60, 95% CI ‐2.15 to 0.95; I2 = 40%). The quality of the evidence was low for aminaftone and high for dobesilate (Table 1).
Global assessment by the participant
Dichotomous variable
We included 16 studies in the analysis: eight on rutosides (Burnand 1989; Cloarec 1996; Jongste 1989; Languillat 1988; Parrado 1999; Pedersen 1992; Pulvertaft 1983; Welch 1985), three on calcium dobesilate (Casley‐Smith 1988; Labs 2004; Rabe 2011), four on diosmine (Biland 1982; Chassignolle 1994; Danielsson 2002; Laurent 1988) and one on Centella asiatica (Allegra 1981), with a total of 1265 participants treated with phlebotonics and 939 with placebo (Analysis 1.20). The analysis showed heterogeneity (I2 = 86%), and we did not pool the data.
1.20. Analysis.
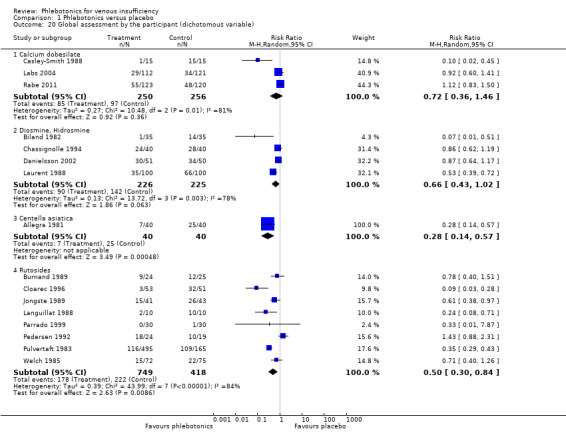
Comparison 1 Phlebotonics versus placebo, Outcome 20 Global assessment by the participant (dichotomous variable).
Continuous variable
We included seven studies in the analysis: four on rutosides (Cesarone 2002; Cloarec 1996; Ihme 1996; Kiesewetter 1997), two on calcium dobesilate (Rabe 2011; Widmer 1990) and one on diosmine (Gilly 1994), with 440 participants treated with phlebotonics and 441 with placebo (Analysis 1.21). The analysis showed heterogeneity (I2 = 85%), and we did not pool the data.
1.21. Analysis.
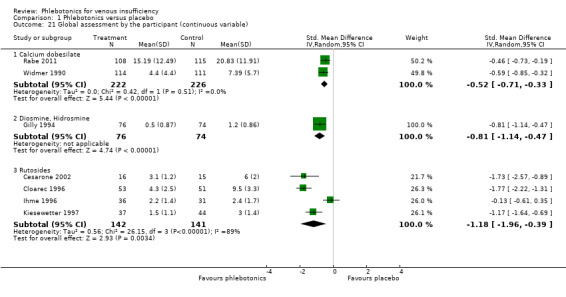
Comparison 1 Phlebotonics versus placebo, Outcome 21 Global assessment by the participant (continuous variable).
Adverse events
Trials considering rutosides (16 trials), hidrosmine‐diosmine (eight trials), calcium dobesilate (seven trials), aminaftone (one trial), grape seed extract (one trial) and Centella asiatica (one trial) reported information on adverse events.
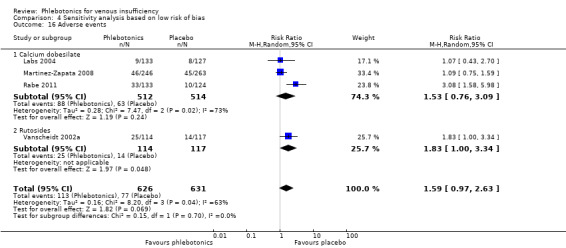
Adverse events
We included in the analysis a total of 2080 participants treated with phlebotonics and 1974 with placebo. Pooled results statistically significantly favoured the placebo group (RR 1.21, 95% CI 1.05 to 1.40; I2 = 0%) (Analysis 1.22) (Figure 6). The quality of the evidence was moderate (Table 1).
1.22. Analysis.
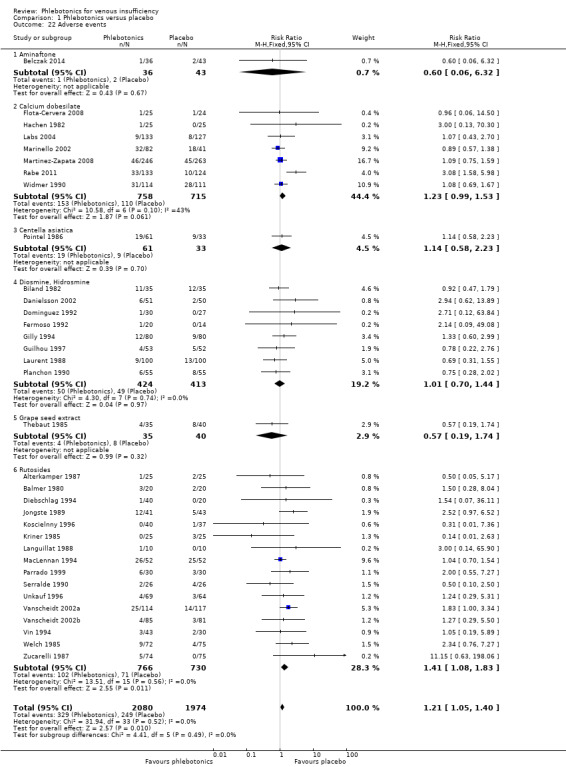
Comparison 1 Phlebotonics versus placebo, Outcome 22 Adverse events.
6.
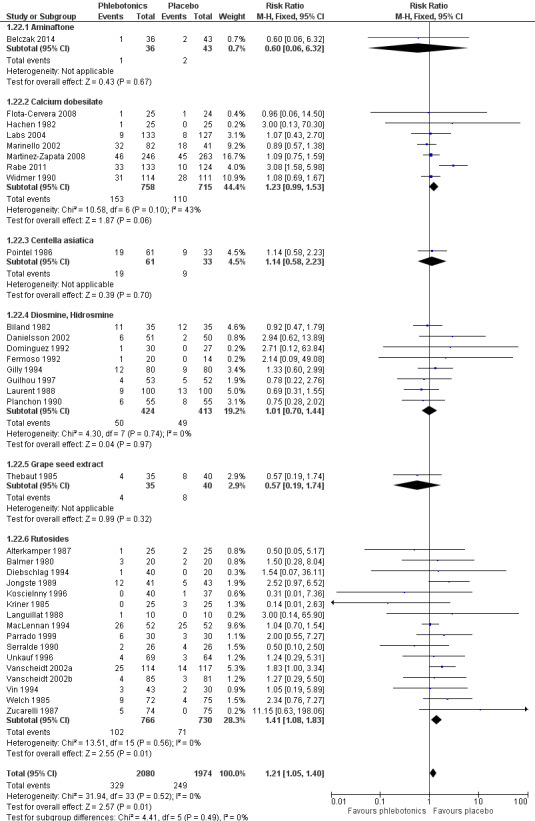
Forest plot of comparison: 1 Phlebotonics vs placebo, outcome: 1.22 Adverse events.
Adverse events analysed by active agent
Aminaftone
Only one trial reported adverse events (Belczak 2014). One participant presented with headache in the group given aminaftone, and two in the placebo group dropped out as the result of subjective worsening of leg pain (RR 0.60, 95% CI 0.06 to 6.32).
Calcium dobesilate
In total, seven trials evaluated adverse events (Flota‐Cervera 2008; Hachen 1982; Labs 2004; Marinello 2002; Martinez‐Zapata 2008; Rabe 2011; Widmer 1990). Twenty per cent of participants in the calcium dobesilate group (153/758) experienced an adverse event and 15.4% (110/715) in the placebo group. Pooled results showed no statistically significant differences between phlebotonics and placebo (RR 1.23, 95% CI 0.99 to 1.53; I2 = 43%; P value = 0.06). The most common adverse event was a gastrointestinal event (epigastric discomfort, vomiting). No agranulocytosis or white blood cell disorders were identified. Nineteen participants were withdrawn from the calcium dobesilate group and 10 from the placebo group as the result of adverse events.
Centella asiatica
One study reported information on adverse events (Pointel 1986). Thirty‐one per cent of participants in the Centella asiatica group (19/61) suffered from adverse events and 27.3% (9/33) in the placebo group. Comparison between groups showed no statistically significant differences between phlebotonics and placebo (RR 1.14, 95% CI 0.58 to 2.23). Two participants who took Centella asiatica 120 mg withdrew ‐ one because of gastralgia (gastric colic) and the other because of neurological absence (absence of nerve activity). One participant taking placebo discontinued the study because of cyanosis of the extremities (bluish discolouration caused by lack of oxygen in the blood).
Diosmine and hidrosmine
Eight studies reported the number of participants who experienced adverse events (Biland 1982; Danielsson 2002; Dominguez 1992; Fermoso 1992; Gilly 1994; Guilhou 1997; Laurent 1988; Planchon 1990). Fifty adverse events were identified in the hidrosmine and diosmine group (50/424) and 49 (49/413) in the placebo group. Pooled results showed no statistically significant differences between phlebotonics and placebo (RR 1.01, 95% CI 0.70 to 1.44; I2 = 0%). Gastrointestinal disorders were the most significant adverse events (heartburn and nausea): 12 cases were reported in the hidrosmine and diosmine group and 11 in the placebo group.
Nine participants withdrew from the hidrosmine group and 11 from the placebo group as the result of adverse events.
Grape seed extract
One study reported information regarding adverse events (Thebaut 1985). Eleven per cent of participants (4/35) receiving active treatment reported adverse effects (three withdrew): Two participants had gastralgia, one participant had a headache and one had an allergic reaction. Twenty per cent of participants in the placebo group (8/40) experienced adverse effects (one withdrew); these included constipation, gastralgia, tiredness, dry mouth and discomfort. Pooled results showed no statistically significant differences between phlebotonics and placebo (RR 0.57, 95% CI 0.19 to 1.74).
Rutoside
Sixteen trials reported information regarding the number of participants who experienced adverse events (Alterkamper 1987; Balmer 1980; Diebschlag 1994; Jongste 1989; Koscielnny 1996; Kriner 1985; Languillat 1988; MacLennan 1994; Parrado 1999; Serralde 1990; Unkauf 1996; Vanscheidt 2002a; Vanscheidt 2002b; Vin 1994; Welch 1985; Zucarelli 1987). Thirteen per cent of participants (102/766) in the rutoside group suffered from adverse events and 9.7% (71/730) in the placebo group. Comparison between groups statistically significantly favoured the placebo group (RR 1.41, 95% CI 1.08 to 1.83; I2 = 0%). The most common adverse events were gastrointestinal in nature (constipation, dry mouth, epigastric discomfort, vomiting): 90 in the rutoside group and 62 in the placebo group, followed by headache (23 in the rutoside group, 21 in the placebo group) and tiredness (17 in the rutoside group, nine in the placebo group).
Six participants withdrew from the rutoside group and 13 from the placebo group as the result of adverse events.
Sensitivity analysis
Exclusion of studies using compression measures (elastic stockings)
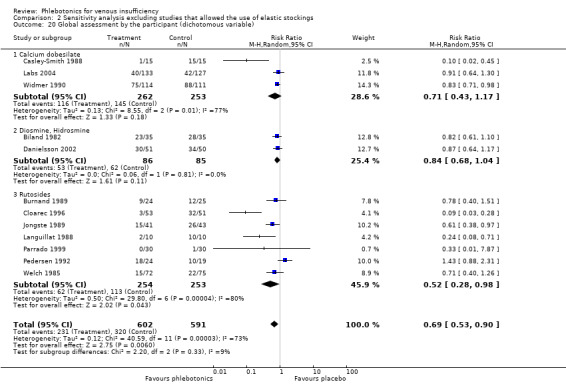
When we re‐analysed the data excluding studies that allowed the use of elastic stockings (Balmer 1980; DOBESILATO500/2; Guilhou 1997; Laurent 1988; MacLennan 1994; Martinez‐Zapata 2008; Rabe 2011; Schultz‐Ehrenburg 1993; Zucarelli 1987), we found that general results did not change, except for the following variables.
Global analysis of the dichotomous variable pain significantly favoured phlebotonics (Analysis 2.6) (RR 0.69, 95% CI 0.57 to 0.82; 1467 participants; 17 studies; I2 = 67%).
Global analysis of the continuous variable cramps significantly favoured phlebotonics (Analysis 2.9) (SMD ‐0.70, 95% CI ‐1.15 to ‐0.24; 314 participants; three studies; I2 = 73%).
Global analysis of the dichotomous variable global assessment by the participant significantly favoured phlebotonics (Analysis 2.20) (RR 0.69, 95% CI 0.53 to 0.90; 1193 participants; 12 studies; I2 = 73%).
Global analysis of the continuous variable quality of life showed favourable results compared with placebo, but the confidence interval was wide because few participants were included (Analysis 2.19) (MD ‐10.00, 95% CI ‐17.01 to ‐ 2.99).
2.6. Analysis.
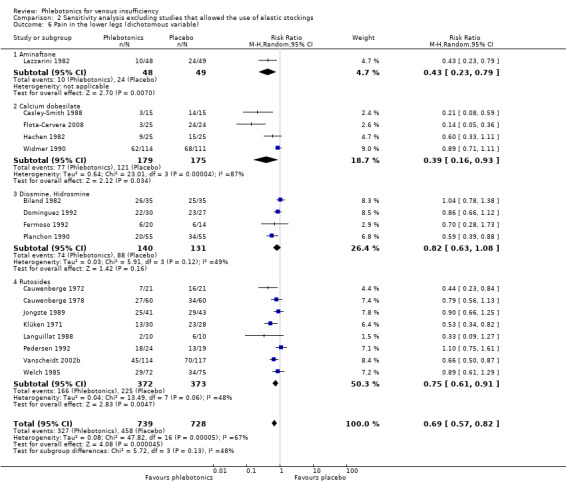
Comparison 2 Sensitivity analysis excluding studies that allowed the use of elastic stockings, Outcome 6 Pain in the lower legs (dichotomous variable).
2.9. Analysis.
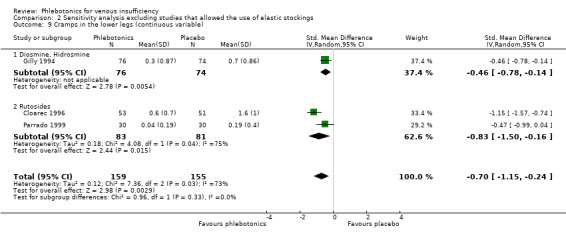
Comparison 2 Sensitivity analysis excluding studies that allowed the use of elastic stockings, Outcome 9 Cramps in the lower legs (continuous variable).
2.20. Analysis.
Comparison 2 Sensitivity analysis excluding studies that allowed the use of elastic stockings, Outcome 20 Global assessment by the participant (dichotomous variable).
2.19. Analysis.
Comparison 2 Sensitivity analysis excluding studies that allowed the use of elastic stockings, Outcome 19 Quality of life.
Exclusion of unpublished data
Only one study, which focused on rutosides, was not published (Welch 1985). When we re‐analysed the data while excluding this study, we found results very similar to those of the main analysis for all outcomes.
Analysis based on studies at low risk of bias
Exclusion of studies at high or unclear risk of bias
In judging quality levels based on the aforementioned criteria, we identified only four studies (Labs 2004; Martinez‐Zapata 2008; Rabe 2011; Vanscheidt 2002a) with low risk of bias. Consequently, limited sensitivity analyses for the included variables were possible.
Results changed only for the following variables.
Analysis of the dichotomous variable oedema in one study on calcium dobesilate (Labs 2004) was not significantly different between phlebotonics and placebo (Analysis 4.1) (RR 0.99, 95% CI 0.63 to 1.55; 260 participants).
Global analysis of the continuous variable oedema (measure of ankle circumference in mm) in three studies on calcium dobesilate (Labs 2004; Martinez‐Zapata 2008; Rabe 2011) was not significantly different between phlebotonics and placebo (Analysis 4.2) (MD ‐2.34 mm, 95% CI ‐8.79 to 4.11; 867 participants; I2 = 65%).
Analysis of the continuous variable oedema (measure of leg volume in mL) in two studies (Rabe 2011; Vanscheidt 2002a) favoured phlebotonics (Analysis 4.3) (MD ‐59.08 mL, 95% CI ‐84.40 to ‐33.76; 418 participants; I2 = 0%).
Analysis of the dichotomous variable itching in one study on rutoside (Vanscheidt 2002a) favoured phlebotonics (Analysis 4.7) (RR 0.44, 95%CI 0.32 to 0.62; 231 participants).
Analysis of the continuous variable itching in one study on calcium dobesilate (Martinez‐Zapata 2008) was not significantly different (Analysis 4.8) (MD 4.60 cm, 95% CI ‐5.66 to 14.86; 416 participants).
Analysis of the dichotomous variable heaviness in one study on rutoside (Vanscheidt 2002a) favoured phlebotonics (Analysis 4.9) (RR 0.62, 95% CI 0.47 to 0.82; 231 participants).
Analysis of the continuous variable heaviness in one study on calcium dobesilate (Martinez‐Zapata 2008) was not significantly different between phlebotonics and placebo (Analysis 4.10) (MD ‐2.40 cm, 95% CI ‐7.89 to 3.09; 417 participants).
Analysis of the continuous variable swelling in one study on calcium dobesilate (Martinez‐Zapata 2008) was not significantly different between phlebotonics and placebo (Analysis 4.12) (MD ‐1.30 cm, 95% CI ‐6.72 to 4.12; 417 participants).
Analysis of the dichotomous variable global assessment by the participant in two studies on calcium dobesilate (Labs 2004; Rabe 2011) was not significantly different between phlebotonics and placebo (Analysis 4.14) (RR 1.04, 95% CI 0.81 to 1.32; 476 participants; I2 = 0%).
Analysis of the continuous variable global assessment by the participant in one study on calcium dobesilate (Rabe 2011) favoured phlebotonics (Analysis 4.15) (MD ‐5.64, 95% CI ‐8.85 to ‐2.43; 223 participants).
Analysis of the dichotomous variable adverse events in the four included studies was not significantly different between phlebotonics and placebo (Analysis 4.16) (RR 1.59, 95% CI 0.97 to 2.63; 1257 participants; I2 = 63%).
4.1. Analysis.
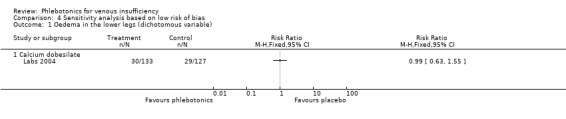
Comparison 4 Sensitivity analysis based on low risk of bias, Outcome 1 Oedema in the lower legs (dichotomous variable).
4.2. Analysis.
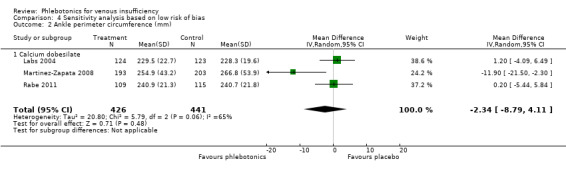
Comparison 4 Sensitivity analysis based on low risk of bias, Outcome 2 Ankle perimeter circumference (mm).
4.3. Analysis.
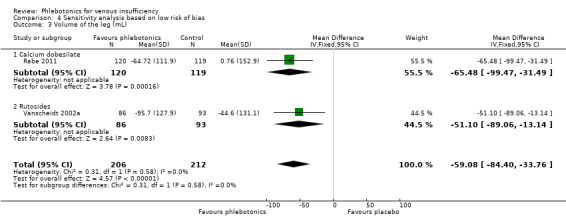
Comparison 4 Sensitivity analysis based on low risk of bias, Outcome 3 Volume of the leg (mL).
4.7. Analysis.
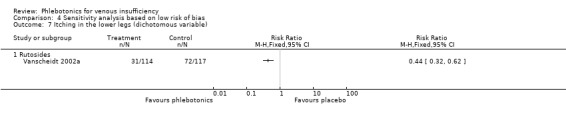
Comparison 4 Sensitivity analysis based on low risk of bias, Outcome 7 Itching in the lower legs (dichotomous variable).
4.8. Analysis.
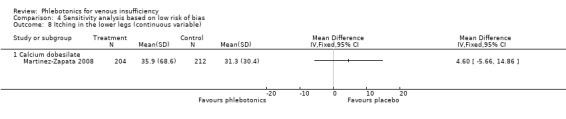
Comparison 4 Sensitivity analysis based on low risk of bias, Outcome 8 Itching in the lower legs (continuous variable).
4.9. Analysis.
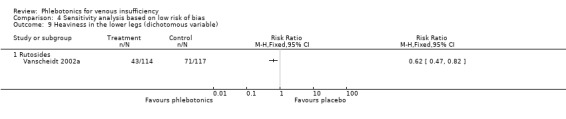
Comparison 4 Sensitivity analysis based on low risk of bias, Outcome 9 Heaviness in the lower legs (dichotomous variable).
4.10. Analysis.
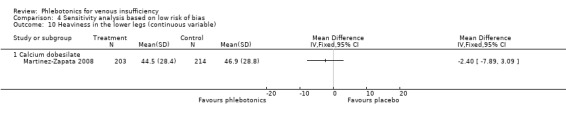
Comparison 4 Sensitivity analysis based on low risk of bias, Outcome 10 Heaviness in the lower legs (continuous variable).
4.12. Analysis.
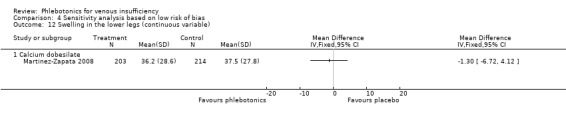
Comparison 4 Sensitivity analysis based on low risk of bias, Outcome 12 Swelling in the lower legs (continuous variable).
4.14. Analysis.
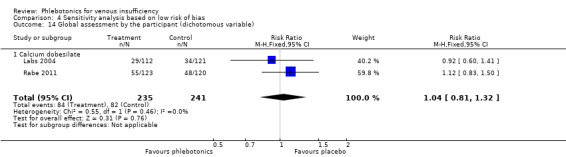
Comparison 4 Sensitivity analysis based on low risk of bias, Outcome 14 Global assessment by the participant (dichotomous variable).
4.15. Analysis.
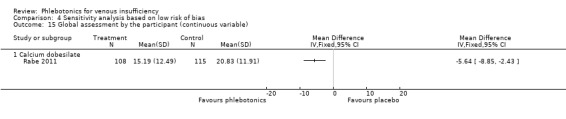
Comparison 4 Sensitivity analysis based on low risk of bias, Outcome 15 Global assessment by the participant (continuous variable).
4.16. Analysis.
Comparison 4 Sensitivity analysis based on low risk of bias, Outcome 16 Adverse events.
Discussion
Summary of main results
We evaluated the efficacy and safety of phlebotonics in the treatment of chronic venous insufficiency (CVI). Only analyses of studies with oral phlebotonics were possible because no identified study of topical phlebotonics met the inclusion criteria of this systematic review (SR). This SR included 66 randomised controlled trials (RCTs) and analysed data from 53 trials involving 6013 participants. Studies included in the review generally provided objective measurement of ankle and calf oedema reduction, as well as subjective assessment of other signs and symptoms of CVI. According to the intention‐to‐treat (ITT) analysis, studies showed a moderate beneficial effect for the dichotomous variable oedema. Analyses in general point to possible beneficial efficacy of phlebotonics for oedema. In addition, phlebotonics showed possible beneficial effects for trophic disorders, cramps, swelling, paraesthesia and restless legs.
However, regarding results of the dichotomous variable ulcer cured and the continuous variable paraesthesias, we found no differences between phlebotonics and placebo. For quality of life (QoL) the results were heterogeneous; evidence of low quality favoured aminaftone, and high‐quality evidence showed no significant differences between calcium dobesilate and placebo. Furthermore, the incidence of adverse events was higher in the phlebotonics group than in the placebo group. Gastrointestinal disorders were the most frequently reported adverse events among studies that provided this information (rutosides, calcium dobesilate, diosmine‐hidrosmine). Our SR did not report agranulocytosis associated with calcium dobesilate, although this adverse effect was described in a previous case‐control study that detected potential risk of agranulocytosis, with an incidence rate of 1.21 cases per 10,000 patient‐years of treatment (Ibañez 2000; Ibáñez 2005). This could be explained by the small number of participants in the included RCTs and the short period of participant follow‐up provided.
One study on aminaftone presented favourable results for the dichotomous variables oedema, pain, cramps, itching and heaviness, although this is an old study that was not replicated later (Lazzarini 1982). Another more recent study of aminaftone presented favourable results for the continuous variables oedema (volume) and QoL, and non‐significant results for adverse events (Belczak 2014). Calcium dobesilate showed favourable results for continuous volume of the leg and global assessment by the participant. Meanwhile, results were not significant for the following continuous variables: ankle perimeter circumference, pain, restless legs, itching, heaviness and QoL. Calcium dobesilate showed favourable results for the following dichotomous variables: cramps, restless legs and swelling. However, it did not present significant differences in the dichotomous variables ulcer cured and paraesthesia. The incidence of adverse events was similar between phlebotonics and placebo groups. Centella asiatica was assessed in two studies. One study showed non‐significant results compared with placebo in the dichotomous variable heaviness (Pointel 1986); the other study showed favourable results for Centella asiatica in the dichotomous variable global assessment by the participant (Allegra 1981). The number of participants with adverse events was not significantly different between Centella asiatica and placebo. Diosmine and hidrosmine showed favourable results for the dichotomous variables oedema and trophic disorders. Results of analyses of the dichotomous and continuous variables cramps and swelling favoured the diosmine and hidrosmine group, as did results of analyses of the continuous variables pain, restless, heaviness and global assessment by the participant. Results of analyses of the dichotomous variables ulcer cured, ulcer, pain, restlessness, itching, heaviness and paraesthesia were non‐significant. The incidence of adverse events was not significant when we compared diosmine and hidrosmine with placebo. French maritime pine bark extract was assessed in only one study and was favoured in both dichotomous and continuous variables of pain (Arcangeli 2000). Results favoured phlebotonics in the continuous variables heaviness and swelling but were non‐significant in the dichotomous variables heaviness and swelling. Grape seed extract was assessed in one study, with non‐significant results reported in the dichotomous variable oedema (Thebaut 1985). Rutosides were included in the greatest number of clinical trials, showing favourable results for the dichotomous variables oedema, swelling and paraesthesia, although results were not significant for the corresponding continuous variable. Results of the variables ulcer cured, trophic disorder and restless legs were non‐significant when compared with placebo. The incidence of adverse events significantly favoured the placebo group.
No evidence was found regarding the efficacy of disodium flavodate, naftazone, chromocarbe or topical phlebotonics.
Overall completeness and applicability of evidence
Several limitations were identified in the included studies. Only 28% of studies specified standard diagnostic criteria for CVI, and different studies applied different criteria. Only nine studies (Belczak 2014; Danielsson 2002; DOBESILATO500/2; Labs 2004; Marinello 2002; Martinez‐Zapata 2008; Rabe 2011; Vanscheidt 2002a; Vanscheidt 2002b) used the currently accepted Clinical‐Aetiology‐Anatomy‐Pathophysiology (CEAP) classification (Porter 1995). Therefore, homogeneity in diagnostic criteria is limited, and potential misclassification bias cannot be ruled out. Furthermore, we were unable to perform a subgroup analysis by CVI stage because severity of CVI was variable.
In most RCTs, the way in which participants were included is heterogeneous, and this may have led to differences in response to treatment. In addition, too few participants were included in the studies, and investigators failed to find statistically significant differences when an effect could have occurred (beta error, or type II error). Different instruments were used to measure signs and symptoms, and sometimes results were inconclusive; some were positive, and others were not significant. Only five RCTs assessed the variable QoL using a standardised questionnaire (Belczak 2014; Martinez‐Zapata 2008; Rabe 2011; Vanscheidt 2002a; Vanscheidt 2002b), but two studies (Vanscheidt 2002a; Vanscheidt 2002b) did not provide quantifiable information. Although some studies favoured phlebotonics, the clinical relevance of these findings remains questionable.
Although infrequent, important signs such as venous ulcers have been poorly evaluated. Only six studies included participants with venous ulcers (DOBESILATO500/2; Fermoso 1992; Guilhou 1997; Lazzarini 1982; MacLennan 1994; Schultz‐Ehrenburg 1993) and, when pooled, showed none that yielded a difference in ulcer healing.
All studies addressing trophic disorders (Fermoso 1992; Gilly 1994; Laurent 1988; Lazzarini 1982) except for two (MacLennan 1994; Planchon 1990) did not define this term. However, in two studies, trophic disorders were assessed subjectively as present or absent (Fermoso 1992; MacLennan 1994), or as reported on semiquantitative four‐item scales (Gilly 1994; Lazzarini 1982; Planchon 1990). Therefore, although data from the examination of trophic alterations were analysed, these results should be interpreted with caution.
Most studies provided short‐term results (one to three months). Given the chronic nature of the disease, more long‐term data on the efficacy and safety of phlebotonics are needed (at least one‐year follow‐up). To achieve homogeneous data collection and to specify evidence on the efficacy of phlebotonics, measurement of signs and symptoms should be standardised. Although we have done a subgroup analysis by drugs, we noted that different doses were involved, and we are unable to comment on which is the optimal dose.
Quality of the evidence
Risk of bias of the included studies is somewhat uncertain regarding randomisation and blinding because only a limited number of studies specifically reported details regarding these issues. It is difficult to determine whether this is a result of poor design or publication restrictions. As a result, among the 66 RCTs included in this SR, 38 explained the double‐blinding procedure in detail, 18 provided data on randomisation and 10 explained blinding of the randomisation. Furthermore, 13 studies had attrition bias. These issues were not addressed in the remaining included studies, and this adds uncertainty to the quality of evidence. Only four studies (Labs 2004; Martinez‐Zapata 2008; Rabe 2011; Vanscheidt 2002a) were graded as having low risk of bias.
In the clinical area of CVI, results lack reliability if the RCT did not include a placebo group because of seasonal exacerbations (spring and summer) that might be self limiting and highly subjective symptoms. Consequently, an adequate control group is needed, and both randomisation and treatment should be appropriately blinded (preferably double‐blinded). For this reason, studies that did not include a control group and single‐blinded studies were excluded from the SR. Among studies identified as double‐blinded, those with inappropriate blinding of treatments or randomisation were excluded from the meta‐analyses.
We adopted a conservative approach in our SR, which prioritised the ITT analysis in terms of both treatment losses and failures. On the other hand, we used change measures only if conditions of the compared groups at baseline were the same, to avoid bias in the assessment of results related to participants' baseline differences.
We evaluated the quality of the body of evidence using the GRADE (Grades of Recommendation, Assessment, Development and Evaluation Working Group) approach (Schünemann 2011), which is based on five considerations including study limitations, directness of the evidence, heterogeneity in the data, precision of effect estimates and additional considerations (including risk of publication bias) to assess the quality of the body of evidence for a priori selected outcomes (in our SR, these included the dichotomous variable of oedema in the lower legs and the continuous variables of oedema in the lower legs, quality of life, participants with ulcer cured and participants with adverse events) (Table 1).
In this SR, the overall quality of evidence is ranked from low (ulcer cured and QoL for aminaftone) to moderate (dichotomous and continuous outcomes of oedema and adverse events) to high (QoL for calcium dobesilate).
Reasons for rating down the quality of evidence for the outcome ulcer cured include the presence of selective reporting and incomplete outcome data; for the outcome QoL for aminaftone unclear generation of randomisation and imprecision (wide confidence intervals); for the dichotomous variables oedema and adverse events incomplete outcome data and for the continuous variable oedema unclear risk of bias of one trial.
Potential biases in the review process
Sensitivity analyses did not significantly alter the results of this review. Whether elastic stockings were used did not influence pooled results, supporting the view that an appropriate randomisation method results in a homogeneous distribution of the groups under comparison.
Any SR is influenced by the quality of included studies and reports. In this respect, we classified only four RCTs as having low risk of bias, and we considered most included studies to have moderate risk of potential bias. We excluded RCTs with high risk of bias. Therefore, conclusions about the results of these studies should be interpreted with caution.
The heterogeneity of several analysis variables may be due to the following.
Different diagnosis classification criteria have been applied; therefore, characteristics of the included population in terms of degree of progression of CVI might vary among studies.
No standardisation is involved in measuring variables, given the different scales that have been used, some of which are not validated. Although the same criteria were applied to the data dichotomisation (participants without symptoms/signs or with mild symptoms/sign vs participants with moderate to severe symptoms/signs), these may not be equally relevant, as they result from the application of different scales.
On the other hand, the same subjectivity of collected variables may represent differences among individuals and may influence the variability of results.
In addition, efficacy of evaluated treatments may not be the same because different active principles were used. This explains observed differences among treatments in the subgroup analysis.
All these considerations limit the validity of included clinical trials and the conclusions of this review. The existence of such heterogeneity restricts the importance of its detection in the process of generating hypotheses (i.e. phlebotonics could be effective for treatment of the pain, cramps, heaviness and swelling of CVI).
Only 51% of included studies reported information on adverse events. However, to adequately assess adverse events related to phlebotonics, it is necessary to include observational study designs that were excluded from our review.
Agreements and disagreements with other studies or reviews
Several reviews have tried to evaluate the clinical benefit of phlebotonics. Some of these used poor methods, which did not include information on search strategies and data collection sources, extraction and statistical treatment (diosmine, escin and rutosides (Diehm 1996b); flavonoids, tribenosides, escin and calcium dobesilate (Markwardt 1996); rutosides (Wadworth 1992); flavonoids (Rabe 2013)). Other reviews are more elaborate and were developed systematically (global phlebotonics (Boada 1999); calcium dobesilate (Ciapponi 2004); escin (Pittler 1998); rutosides (Aziz 2015; Poynard 1994)). Four reviews pursued data meta‐analysis (Aziz 2015; Boada 1999; Ciapponi 2004; Poynard 1994).
One review specifically evaluated hydroxyethylrutosides: Review authors included 15 randomised studies and applied a per‐protocol (PP) analysis. They stated that rutosides were better than control for controlling symptoms of pain, cramps and heaviness (Aziz 2015).
Another review analysed rutosides: Review authors included 12 randomised, double‐blind, placebo‐controlled studies and applied an ITT analysis. They stated that rutosides were better than placebo for controlling symptoms of pain, cramps, heaviness, swelling and tiredness of affected legs. They mentioned no CVI signs (Poynard 1994).
Another review covered all drugs that have been evaluated for CVI through randomised, double‐blind, placebo‐controlled trials without concomitant compression procedures. These included traditional agents such as hidrosmine, diosmine, escin, rutosides and calcium dobesilate, along with other, less usual ones such as extract of Centella asiatica, benzarone, tribenoside, flunarizine, dihydroergotamine mesylate and mucopolysaccharide sulphate. The conclusion of the Boada 1999 review was that phlebotonics might improve leg heaviness in patients with CVI. Review authors presented no conclusive data regarding other signs or symptoms. However, review authors performed PP rather than ITT analysis and provided no information on individual phlebotonics (Boada 1999).
The review led by Ciapponi analysed calcium dobesilate: Review authors included 10 double‐blind, randomised, placebo‐controlled studies and applied a PP analysis. They stated that calcium dobesilate was better than placebo for controlling cramps and discomfort. Subgroup analysis showed greater efficacy in more severe cases of the disease in terms of improving symptoms (pain, heaviness and swelling) and signs (leg volume). Sensitivity analysis based on the ITT analysis did not influence these results (Ciapponi 2004).
Except for Aziz 2015, the above‐cited reviews were published a relatively long time ago and have not been updated. Our SR updates evidence on phlebotonics in general and by drug group.
Authors' conclusions
Implications for practice.
Phlebotonics present limited efficacy for oedema and for some signs and symptoms related to chronic venous insufficiency (CVI). Investigators reported no differences compared with placebo for ulcer healing. Additional high‐quality randomised controlled trials (RCTs) are needed to improve the evidence base, with greater attention paid to methodological quality and clinically important outcomes.
Moderate‐quality evidence supports the efficacy of phlebotonics in oedema. Low‐quality evidence indicates that these drugs do not influence ulcer healing.
Some specific groups of phlebotonics were effective for certain symptoms and signs; however, given the limited number of studies and the discordance in their results, these findings are uncertain.
On the other hand, moderate‐quality evidence shows that phlebotonics are associated with higher risk of adverse events than placebo, especially in the rutoside group. Studies included in this systematic review (SR) provided only short‐term safety data; therefore, the middle‐ and long‐term safety of phlebotonics could not be estimated.
Implications for research.
As a result of the importance of phlebotonics and the limitations of current evidence, high‐quality RCTs are needed to evaluate the efficacy and adverse effects of this group of drugs in an independent and rigorous manner. However, the new studies included in this SR have improved methodological aspects and have already considered in a standardised manner the diagnostic classification of participants, measurement of signs and symptoms, larger sample sizes and longer follow‐up, and future trials should continue these recommendations. Additional research regarding quality of life (QoL) and both ulcers and trophic disorders is needed, particularly with an accurate definition of the term and the use of objective measurements. More and better assessments of venous ulcers should be made, and QoL surveys specifically validated for CVI should be introduced. Furthermore, currently available data on safety refer to a short administration period; therefore, long‐term observational follow‐up studies are needed to better define the safety profile of each of the phlebotonics and to outline more clearly the risk/benefit ratio.
When the efficacy of phlebotonics is investigated, restriction criteria are recommended to avoid situations that are more likely to result in adverse effects, including long‐term administration, important co‐morbidity, leucopenia, ageing and multiple medications. In addition, researchers involved in these trials should make an explicit statement regarding their conflicts of interest.
What's new
| Date | Event | Description |
|---|---|---|
| 21 August 2015 | New search has been performed | Searches rerun, 6 new studies included, 2 publications added to already included studies and 1 study reclassified as an included study, 115 new studies excluded and 3 new ongoing studies identified |
| 21 August 2015 | New citation required and conclusions have changed | Searches rerun, 6 new studies included, 1 study reclassified as an included study, 115 new studies excluded and 3 new ongoing studies identified. New authors have joined the review team. Risk of bias assessed for all included studies and 'Summary of findings' table added. Review updated according to current Cochrane reporting guidelines |
History
Protocol first published: Issue 3, 2001 Review first published: Issue 3, 2005
| Date | Event | Description |
|---|---|---|
| 8 July 2008 | Amended | Converted to new review format |
| 14 November 2006 | Amended | Edited update. CDSR citations updated |
Acknowledgements
We would like to thank Marta Roqué for statistical advice provided on the first version of this review. We also want to express our acknowledgement to the Spanish Drug Agency for providing us with several papers used in an in‐house assessment process, and to Dr. A. Cachá, a member of the Safety Committee Task Force of the Agencia Española del Medicamento, who initially participated in the process of selection of clinical trials.
We also acknowledge the Cochrane Vascular TSC for assistance in searching for trials.
Appendices
Appendix 1. CRS search strategy
| Search run on Fri Aug 21 2015 | ||
| #1 | MESH DESCRIPTOR Venous Insufficiency EXPLODE ALL TREES | 333 |
| #2 | (insuffic* or insufic* or CVI or isch* or incompet* ):TI,AB,KY | 29524 |
| #3 | (saphenous or vein* or veno*):TI,AB,KY | 21111 |
| #4 | #1 OR #2 OR #3 | 48620 |
| #5 | MESH DESCRIPTOR Flavonoids EXPLODE ALL TREES | 1732 |
| #6 | MESH DESCRIPTOR Saponins EXPLODE ALL TREES | 149 |
| #7 | MESH DESCRIPTOR Calcium Dobesilate | 37 |
| #8 | *rutin*:TI,AB,KY | 516 |
| #9 | *rutoside*:TI,AB,KY | 183 |
| #10 | (*escin* or *aescin* or *essaven*):TI,AB,KY | 196 |
| #11 | (*rosskastani* or *aesculus*):TI,AB,KY | 23 |
| #12 | (horse near3 (chestnut or chest‐nut)):TI,AB,KY | 42 |
| #13 | (calcium near2 dobesilate):TI,AB,KY | 81 |
| #14 | (naftazone* or aminaftone* or aminaphtone* or chromocarbe* ):TI,AB,KY | 18 |
| #15 | (bark* near3 extract):TI,AB,KY | 80 |
| #16 | (*french* near3 maritime*):TI,AB,KY | 26 |
| #17 | (*grape* near3 *seed*):TI,AB,KY | 67 |
| #18 | (disodium* near2 flavodate*):TI,AB,KY | 3 |
| #19 | (*dioxium* or hidrosmin* or *diosmin*):TI,AB,KY | 102 |
| #20 | (*venostasin* or *venorutin* or pycnogenol* ):TI,AB,KY | 86 |
| #21 | (*flavono* or *flaven* or centella or aminaftone ):TI,AB,KY | 1007 |
| #22 | *phlebotonic*:TI,AB,KY | 8 |
| #23 | (*quercetin or hesperidin or saponosides or saponin* ):TI,AB,KY | 465 |
| #24 | daflon:TI,AB,KY | 70 |
| #25 | #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 | 3207 |
| #26 | #4 AND #25 | 513 |
Data and analyses
Comparison 1. Phlebotonics versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Oedema in the lower legs (dichotomous variable) | 13 | 1245 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.63, 0.78] |
| 1.1 Aminaftone | 1 | 82 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.28, 0.99] |
| 1.2 Calcium dobesilate | 2 | 290 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.48, 1.07] |
| 1.3 Diosmine, Hidrosmine | 2 | 144 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.46, 0.86] |
| 1.4 Grape seed extract | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.58, 1.06] |
| 1.5 Rutosides | 7 | 654 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.64, 0.81] |
| 2 Ankle perimeter circumference (mm) | 15 | 2010 | Mean Difference (IV, Fixed, 95% CI) | ‐4.27 [‐5.61, ‐2.93] |
| 2.1 Calcium dobesilate | 5 | 1122 | Mean Difference (IV, Fixed, 95% CI) | ‐1.69 [‐4.84, 1.47] |
| 2.2 Diosmine, Hidrosmine | 3 | 286 | Mean Difference (IV, Fixed, 95% CI) | ‐5.98 [‐7.78, ‐4.18] |
| 2.3 Rutosides | 7 | 602 | Mean Difference (IV, Fixed, 95% CI) | ‐2.45 [‐5.06, 0.15] |
| 3 Volume of the leg (mL) | 9 | 1041 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.38 [‐0.50, ‐0.25] |
| 3.1 Aminaftone | 1 | 79 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.17 [‐0.61, 0.28] |
| 3.2 Calcium dobesilate | 3 | 475 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.50 [‐0.68, ‐0.31] |
| 3.3 Rutosides | 5 | 487 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.29 [‐0.47, ‐0.11] |
| 4 Ulcer cured | 6 | 461 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.79, 1.13] |
| 4.1 Aminaftone | 1 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.18, 3.18] |
| 4.2 Calcium dobesilate | 1 | 69 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.69, 1.74] |
| 4.3 Diosmine, Hidrosmine | 2 | 133 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.69, 1.01] |
| 4.4 Rutosides | 2 | 159 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [0.87, 1.86] |
| 5 Trophic disorders (dichotomous variable) | 6 | 705 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.81, 0.95] |
| 5.1 Aminaftone | 1 | 97 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.41, 1.44] |
| 5.2 Diosmine, Hidrosmine | 4 | 504 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.81, 0.94] |
| 5.3 Rutosides | 1 | 104 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.71, 1.25] |
| 6 Pain in the lower legs (dichotomous variable) | 20 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.1 Aminaftone | 1 | 97 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.23, 0.79] |
| 6.2 Calcium dobesilate | 4 | 354 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.16, 0.93] |
| 6.3 Diosmine, Hidrosmine | 4 | 271 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.63, 1.08] |
| 6.4 French maritime pine bark extract | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.48, 0.91] |
| 6.5 Rutosides | 10 | 1485 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.48, 0.83] |
| 7 Pain in the lower legs (continuous variable) | 9 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Calcium dobesilate | 4 | 776 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.35, 0.12] |
| 7.2 Diosmine, Hidrosmine | 1 | 150 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.67, ‐0.02] |
| 7.3 French maritime pine bark extract | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.39 [‐2.09, ‐0.69] |
| 7.4 Rutosides | 3 | 219 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.71 [‐1.23, ‐0.19] |
| 8 Cramps in the lower legs (dichotomous variable) | 14 | 1793 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.58, 0.89] |
| 8.1 Aminaftone | 1 | 97 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.31, 0.99] |
| 8.2 Calcium dobesilate | 2 | 255 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.50, 0.84] |
| 8.3 Diosmine, Hidrosmine | 3 | 214 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.70, 0.98] |
| 8.4 Rutosides | 8 | 1227 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.47, 1.02] |
| 9 Cramps in the lower legs (continuous variable) | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 9.1 Calcium dobesilate | 1 | 415 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.29, 0.09] |
| 9.2 Diosmine, Hidrosmine | 1 | 150 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.78, ‐0.14] |
| 9.3 Rutosides | 2 | 164 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.83 [‐1.50, ‐0.16] |
| 10 Restless legs (dichotomous variable) | 7 | 652 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.72, 0.91] |
| 10.1 Calcium dobesilate | 2 | 255 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.59, 0.91] |
| 10.2 Diosmine, Hidrosmine | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.70, 1.15] |
| 10.3 Rutosides | 4 | 327 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.72, 1.01] |
| 11 Itching in the lower legs (dichotomous variable) | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 11.1 Aminaftone | 1 | 97 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.31, 0.91] |
| 11.2 Diosmine, Hidrosmine | 1 | 34 | Risk Ratio (M‐H, Random, 95% CI) | 1.63 [0.51, 5.25] |
| 11.3 Rutosides | 2 | 274 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.21, 2.21] |
| 12 Itching in the lower legs (continuous variable) | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 12.1 Calcium dobesilate | 1 | 416 | Std. Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.11, 0.28] |
| 12.2 Rutosides | 1 | 60 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐1.10, ‐0.06] |
| 13 Heaviness in the lower legs (dichotomous variable) | 19 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 13.1 Aminaftone | 1 | 97 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.17, 0.60] |
| 13.2 Calcium dobesilate | 3 | 305 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.08, 1.42] |
| 13.3 Centella asiatica | 1 | 63 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.32, 1.19] |
| 13.4 Diosmine, Hidrosmine | 4 | 241 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.35, 1.05] |
| 13.5 French maritime pine bark extract | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.76, 1.07] |
| 13.6 Rutosides | 9 | 1420 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.48, 0.74] |
| 14 Heaviness in the lower legs (continuous variable) | 10 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 14.1 Calcium dobesilate | 2 | 483 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.23, 0.13] |
| 14.2 Diosmine, Hidrosmine | 1 | 150 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.69 [‐1.02, ‐0.36] |
| 14.3 French maritime pine bark extract | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.50 [‐2.21, ‐0.79] |
| 14.4 Rutosides | 6 | 441 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.11 [‐1.87, ‐0.36] |
| 15 Swelling in the lower legs (dichotomous variable) | 14 | 1072 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.50, 0.80] |
| 15.1 Calcium dobesilate | 2 | 80 | Risk Ratio (M‐H, Random, 95% CI) | 0.19 [0.08, 0.41] |
| 15.2 Diosmine, Hidrosmine | 2 | 104 | Risk Ratio (M‐H, Random, 95% CI) | 0.7 [0.52, 0.94] |
| 15.3 French maritime pine bark extract | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.64, 1.02] |
| 15.4 Rutosides | 9 | 848 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.50, 0.88] |
| 16 Swelling in the lower legs (continuous variable) | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 16.1 Calcium dobesilate | 1 | 417 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.24, 0.15] |
| 16.2 Diosmine, Hidrosmine | 1 | 150 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.92 [‐1.26, ‐0.58] |
| 16.3 French maritime pine bark extract | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.65 [‐2.38, ‐0.92] |
| 16.4 Rutosides | 3 | 264 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.73 [‐3.50, 0.04] |
| 17 Paraesthesia in the lower legs (dichotomous variable) | 9 | 1456 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.50, 0.88] |
| 17.1 Calcium dobesilate | 3 | 305 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.51, 1.08] |
| 17.2 Diosmine, Hidrosmine | 2 | 144 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.62, 1.05] |
| 17.3 Rutosides | 4 | 1007 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.37, 0.83] |
| 18 Paraesthesia in the lower legs (continuous variable) | 2 | 188 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.15 [‐0.44, 0.13] |
| 18.1 Diosmine, Hidrosmine | 1 | 150 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.12 [‐0.44, 0.21] |
| 18.2 Rutosides | 1 | 38 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.31 [‐0.96, 0.33] |
| 19 Quality of life | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 19.1 Aminaftone | 1 | 79 | Mean Difference (IV, Fixed, 95% CI) | ‐10.0 [‐17.01, ‐2.99] |
| 19.2 Calcium dobesilate at 3 months of treatment | 2 | 617 | Mean Difference (IV, Fixed, 95% CI) | ‐0.60 [‐2.15, 0.95] |
| 20 Global assessment by the participant (dichotomous variable) | 16 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 20.1 Calcium dobesilate | 3 | 506 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.36, 1.46] |
| 20.2 Diosmine, Hidrosmine | 4 | 451 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.43, 1.02] |
| 20.3 Centella asiatica | 1 | 80 | Risk Ratio (M‐H, Random, 95% CI) | 0.28 [0.14, 0.57] |
| 20.4 Rutosides | 8 | 1167 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.30, 0.84] |
| 21 Global assessment by the participant (continuous variable) | 7 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 21.1 Calcium dobesilate | 2 | 448 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐0.71, ‐0.33] |
| 21.2 Diosmine, Hidrosmine | 1 | 150 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.81 [‐1.14, ‐0.47] |
| 21.3 Rutosides | 4 | 283 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.18 [‐1.96, ‐0.39] |
| 22 Adverse events | 34 | 4054 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [1.05, 1.40] |
| 22.1 Aminaftone | 1 | 79 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.06, 6.32] |
| 22.2 Calcium dobesilate | 7 | 1473 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.23 [0.99, 1.53] |
| 22.3 Centella asiatica | 1 | 94 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.58, 2.23] |
| 22.4 Diosmine, Hidrosmine | 8 | 837 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.70, 1.44] |
| 22.5 Grape seed extract | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.19, 1.74] |
| 22.6 Rutosides | 16 | 1496 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.41 [1.08, 1.83] |
Comparison 2. Sensitivity analysis excluding studies that allowed the use of elastic stockings.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Oedema in the lower legs (dichotomous variable) | 12 | 1131 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.60, 0.76] |
| 1.1 Aminaftone | 1 | 82 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.28, 0.99] |
| 1.2 Calcium dobesilate | 2 | 290 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.48, 1.07] |
| 1.3 Diosmine, Hidrosmine | 2 | 144 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.46, 0.86] |
| 1.4 Grape seed extract | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.58, 1.06] |
| 1.5 Rutosides | 6 | 540 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.58, 0.78] |
| 2 Ankle perimeter circumference (mm) | 10 | 1212 | Mean Difference (IV, Fixed, 95% CI) | ‐4.59 [‐6.02, ‐3.16] |
| 2.1 Calcium dobesilate | 3 | 502 | Mean Difference (IV, Fixed, 95% CI) | ‐0.80 [‐4.95, 3.34] |
| 2.2 Diosmine, Hidrosmine | 2 | 246 | Mean Difference (IV, Fixed, 95% CI) | ‐5.90 [‐7.72, ‐4.07] |
| 2.3 Rutosides | 5 | 464 | Mean Difference (IV, Fixed, 95% CI) | ‐3.28 [‐6.06, ‐0.50] |
| 3 Volume of the leg (mL) | 8 | 802 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.34 [‐0.48, ‐0.20] |
| 3.1 Aminaftone | 1 | 79 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.17 [‐0.61, 0.28] |
| 3.2 Calcium dobesilate | 2 | 236 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.51 [‐0.77, ‐0.25] |
| 3.3 Rutosides | 5 | 487 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.29 [‐0.47, ‐0.11] |
| 4 Ulcer cured | 2 | 128 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.27, 3.10] |
| 4.1 Aminaftone | 1 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.18, 3.18] |
| 4.2 Diosmine, Hidrosmine | 1 | 28 | Risk Ratio (M‐H, Random, 95% CI) | 1.5 [0.15, 14.68] |
| 5 Trophic disorders (dichotomous variable) | 5 | 601 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.79, 0.94] |
| 5.1 Aminaftone | 1 | 97 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.41, 1.44] |
| 5.2 Diosmine, Hidrosmine | 4 | 504 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.81, 0.94] |
| 6 Pain in the lower legs (dichotomous variable) | 17 | 1467 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.57, 0.82] |
| 6.1 Aminaftone | 1 | 97 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.23, 0.79] |
| 6.2 Calcium dobesilate | 4 | 354 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.16, 0.93] |
| 6.3 Diosmine, Hidrosmine | 4 | 271 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.63, 1.08] |
| 6.4 Rutosides | 8 | 745 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.61, 0.91] |
| 7 Pain in the lower legs (continuous variable) | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Diosmine, Hidrosmine | 1 | 150 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.67, ‐0.02] |
| 7.2 Rutosides | 2 | 164 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.96 [‐1.33, ‐0.59] |
| 8 Cramps in the lower legs (dichotomous variable) | 12 | 1603 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.57, 0.91] |
| 8.1 Aminaftone | 1 | 97 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.31, 0.99] |
| 8.2 Calcium dobesilate | 2 | 255 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.50, 0.84] |
| 8.3 Diosmine, Hidrosmine | 2 | 104 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.69, 1.09] |
| 8.4 Rutosides | 7 | 1147 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.50, 1.06] |
| 9 Cramps in the lower legs (continuous variable) | 3 | 314 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.70 [‐1.15, ‐0.24] |
| 9.1 Diosmine, Hidrosmine | 1 | 150 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.78, ‐0.14] |
| 9.2 Rutosides | 2 | 164 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.83 [‐1.50, ‐0.16] |
| 10 Restless legs (dichotomous variable) | 6 | 572 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.72, 0.91] |
| 10.1 Calcium dobesilate | 2 | 255 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.59, 0.91] |
| 10.2 Diosmine, Hidrosmine | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.70, 1.15] |
| 10.3 Rutosides | 3 | 247 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.73, 1.01] |
| 11 Itching in the lower legs (dichotomous variable) | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 11.1 Aminaftone | 1 | 97 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.31, 0.91] |
| 11.2 Diosmine, Hidrosmine | 1 | 34 | Risk Ratio (M‐H, Random, 95% CI) | 1.63 [0.51, 5.25] |
| 11.3 Rutosides | 2 | 274 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.21, 2.21] |
| 12 Itching in the lower legs (continuous variable) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 12.1 Rutosides | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Heaviness in the lower legs (dichotomous variable) | 16 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 13.1 Aminaftone | 1 | 97 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.17, 0.60] |
| 13.2 Calcium dobesilate | 3 | 305 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.08, 1.42] |
| 13.3 Centella asiatica | 1 | 63 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.32, 1.19] |
| 13.4 Diosmine, Hidrosmine | 3 | 201 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.29, 1.22] |
| 13.5 Rutosides | 8 | 531 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.38, 0.80] |
| 14 Heaviness in the lower legs (continuous variable) | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 14.1 Diosmine, Hidrosmine | 1 | 150 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.69 [‐1.02, ‐0.36] |
| 14.2 Rutosides | 5 | 360 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.27 [‐2.22, ‐0.32] |
| 15 Swelling in the lower legs (dichotomous variable) | 12 | 952 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.53, 0.82] |
| 15.1 Calcium dobesilate | 2 | 80 | Risk Ratio (M‐H, Random, 95% CI) | 0.19 [0.08, 0.41] |
| 15.2 Diosmine, Hidrosmine | 2 | 104 | Risk Ratio (M‐H, Random, 95% CI) | 0.7 [0.52, 0.94] |
| 15.3 Rutosides | 8 | 768 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.58, 0.89] |
| 16 Swelling in the lower legs (continuous variable) | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 16.1 Diosmine, Hidrosmine | 1 | 150 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.92 [‐1.26, ‐0.58] |
| 16.2 Rutosides | 3 | 264 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.73 [‐3.50, 0.04] |
| 17 Paraesthesias in the lower legs (dichotomous variable) | 7 | 716 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.64, 0.88] |
| 17.1 Calcium dobesilate | 3 | 305 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.58, 1.01] |
| 17.2 Diosmine, Hidrosmine | 2 | 144 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.61, 1.06] |
| 17.3 Rutosides | 2 | 267 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.68 [0.51, 0.91] |
| 18 Paraesthesias in the lower legs (continuous variable) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 18.1 Diosmine, Hidrosmine | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 Quality of life | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 19.1 Aminaftone | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 Global assessment by the participant (dichotomous variable) | 12 | 1193 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.53, 0.90] |
| 20.1 Calcium dobesilate | 3 | 515 | Risk Ratio (M‐H, Random, 95% CI) | 0.71 [0.43, 1.17] |
| 20.2 Diosmine, Hidrosmine | 2 | 171 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.68, 1.04] |
| 20.3 Rutosides | 7 | 507 | Risk Ratio (M‐H, Random, 95% CI) | 0.52 [0.28, 0.98] |
| 21 Global assessment by the participant (continuous variable) | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 21.1 Diosmine, Hidrosmine | 1 | 150 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.81 [‐1.14, ‐0.47] |
| 21.2 Rutosides | 3 | 252 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.02 [‐1.96, ‐0.09] |
| 22 Adverse events | 25 | 2490 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.23 [1.00, 1.51] |
| 22.1 Aminaftone | 1 | 79 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.06, 6.32] |
| 22.2 Calcium dobesilate | 4 | 584 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.74, 1.62] |
| 22.3 Centella asiatica | 1 | 94 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.58, 2.23] |
| 22.4 Diosmine, Hidrosmine | 6 | 532 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.76, 1.79] |
| 22.5 Grape seed extract | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.19, 1.74] |
| 22.6 Rutosides | 12 | 1126 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.54 [1.08, 2.19] |
2.1. Analysis.
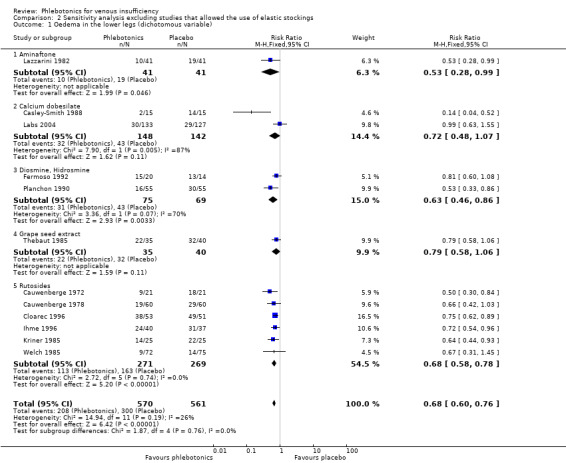
Comparison 2 Sensitivity analysis excluding studies that allowed the use of elastic stockings, Outcome 1 Oedema in the lower legs (dichotomous variable).
2.2. Analysis.
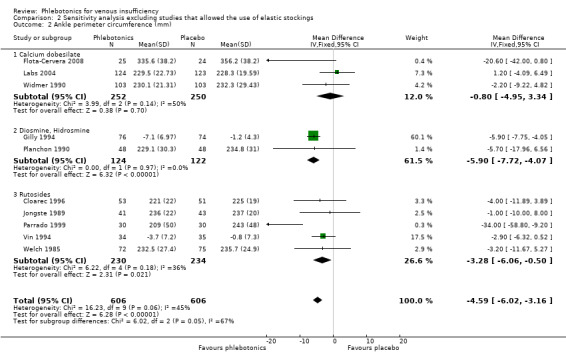
Comparison 2 Sensitivity analysis excluding studies that allowed the use of elastic stockings, Outcome 2 Ankle perimeter circumference (mm).
2.3. Analysis.
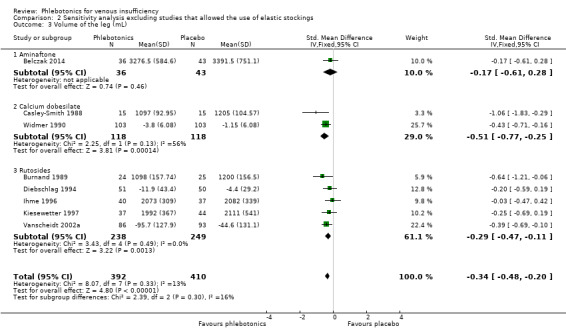
Comparison 2 Sensitivity analysis excluding studies that allowed the use of elastic stockings, Outcome 3 Volume of the leg (mL).
2.4. Analysis.
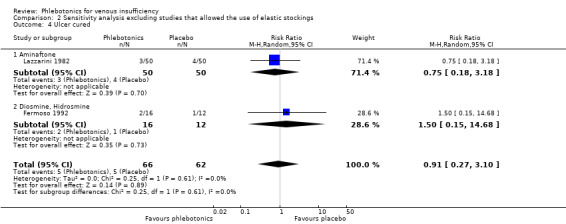
Comparison 2 Sensitivity analysis excluding studies that allowed the use of elastic stockings, Outcome 4 Ulcer cured.
2.5. Analysis.
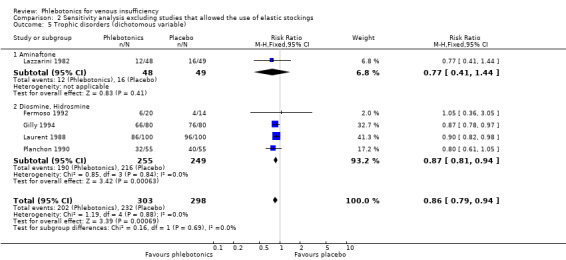
Comparison 2 Sensitivity analysis excluding studies that allowed the use of elastic stockings, Outcome 5 Trophic disorders (dichotomous variable).
2.7. Analysis.
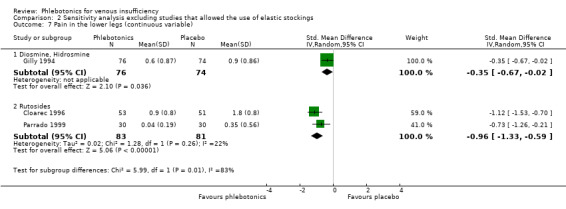
Comparison 2 Sensitivity analysis excluding studies that allowed the use of elastic stockings, Outcome 7 Pain in the lower legs (continuous variable).
2.8. Analysis.
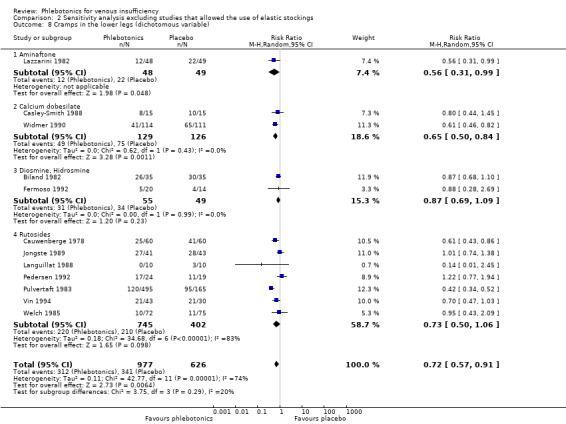
Comparison 2 Sensitivity analysis excluding studies that allowed the use of elastic stockings, Outcome 8 Cramps in the lower legs (dichotomous variable).
2.10. Analysis.
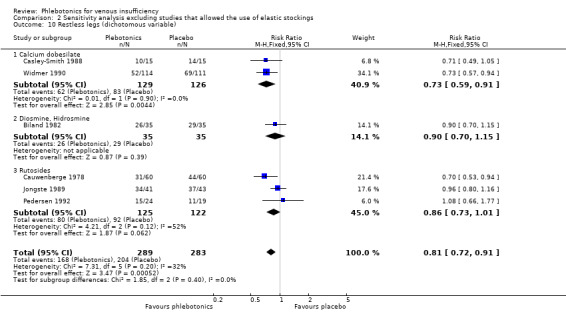
Comparison 2 Sensitivity analysis excluding studies that allowed the use of elastic stockings, Outcome 10 Restless legs (dichotomous variable).
2.11. Analysis.
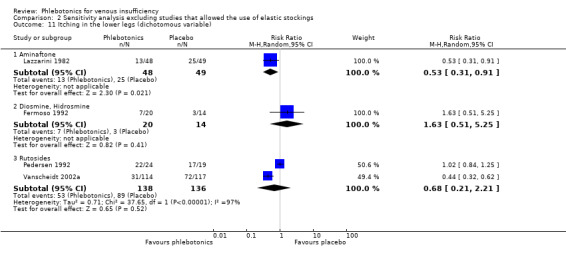
Comparison 2 Sensitivity analysis excluding studies that allowed the use of elastic stockings, Outcome 11 Itching in the lower legs (dichotomous variable).
2.12. Analysis.
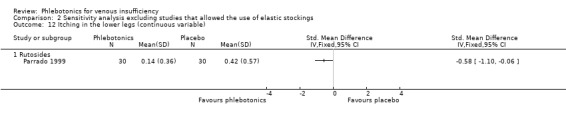
Comparison 2 Sensitivity analysis excluding studies that allowed the use of elastic stockings, Outcome 12 Itching in the lower legs (continuous variable).
2.13. Analysis.
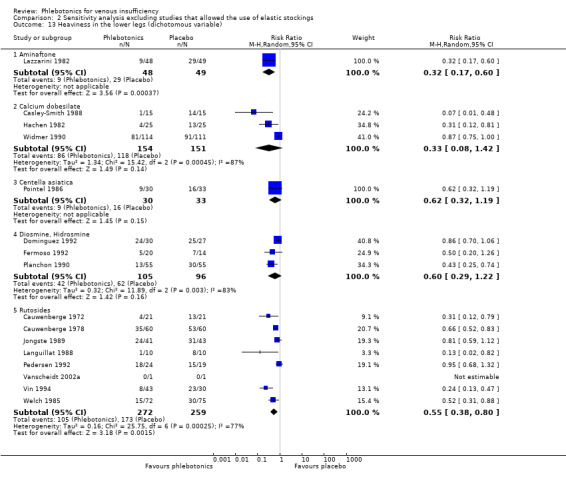
Comparison 2 Sensitivity analysis excluding studies that allowed the use of elastic stockings, Outcome 13 Heaviness in the lower legs (dichotomous variable).
2.14. Analysis.
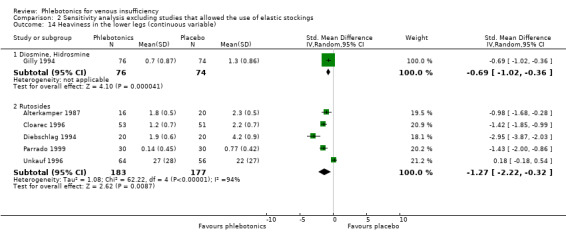
Comparison 2 Sensitivity analysis excluding studies that allowed the use of elastic stockings, Outcome 14 Heaviness in the lower legs (continuous variable).
2.15. Analysis.
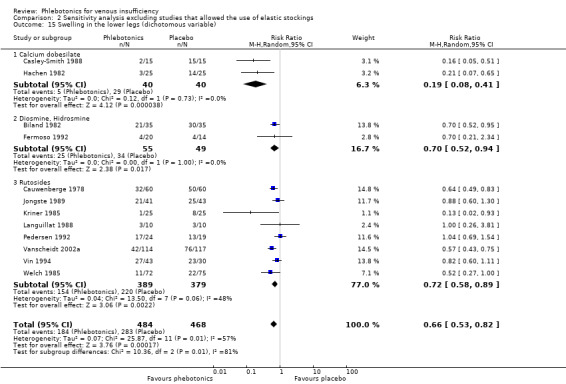
Comparison 2 Sensitivity analysis excluding studies that allowed the use of elastic stockings, Outcome 15 Swelling in the lower legs (dichotomous variable).
2.16. Analysis.
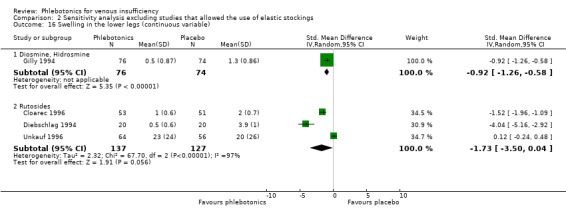
Comparison 2 Sensitivity analysis excluding studies that allowed the use of elastic stockings, Outcome 16 Swelling in the lower legs (continuous variable).
2.17. Analysis.
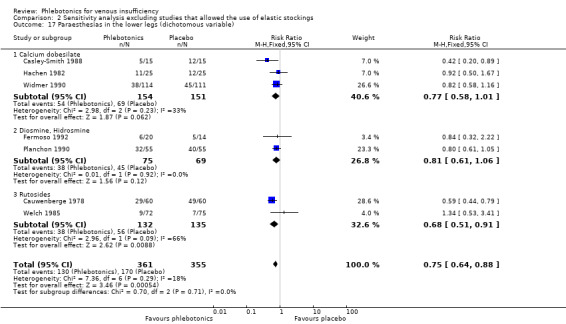
Comparison 2 Sensitivity analysis excluding studies that allowed the use of elastic stockings, Outcome 17 Paraesthesias in the lower legs (dichotomous variable).
2.18. Analysis.
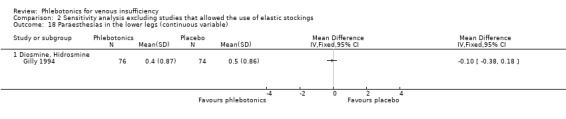
Comparison 2 Sensitivity analysis excluding studies that allowed the use of elastic stockings, Outcome 18 Paraesthesias in the lower legs (continuous variable).
2.21. Analysis.
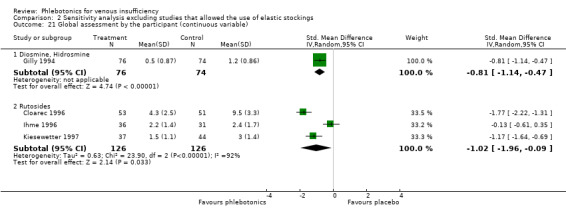
Comparison 2 Sensitivity analysis excluding studies that allowed the use of elastic stockings, Outcome 21 Global assessment by the participant (continuous variable).
2.22. Analysis.
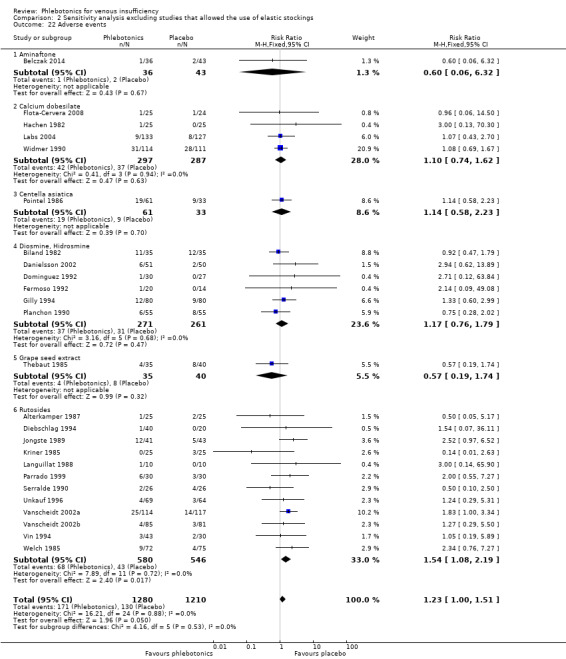
Comparison 2 Sensitivity analysis excluding studies that allowed the use of elastic stockings, Outcome 22 Adverse events.
Comparison 3. Sensitivity analysis of published studies only.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Oedema in the lower legs (dichotomous variable) | 12 | 1088 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.63, 0.78] |
| 1.1 Aminaftone | 1 | 82 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.28, 0.99] |
| 1.2 Calcium dobesilate | 2 | 290 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.48, 1.07] |
| 1.3 Diosmine, Hidrosmine | 2 | 144 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.46, 0.86] |
| 1.4 Grape seed extract | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.58, 1.06] |
| 1.5 Rutosides | 6 | 497 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.64, 0.81] |
| 2 Ankle perimeter circumference (mm) | 13 | 1796 | Mean Difference (IV, Random, 95% CI) | ‐3.61 [‐6.77, ‐0.45] |
| 2.1 Calcium dobesilate | 5 | 1122 | Mean Difference (IV, Random, 95% CI) | ‐3.17 [‐8.37, 2.02] |
| 2.2 Diosmine, Hidrosmine | 3 | 286 | Mean Difference (IV, Random, 95% CI) | ‐5.98 [‐7.78, ‐4.18] |
| 2.3 Rutosides | 5 | 388 | Mean Difference (IV, Random, 95% CI) | ‐2.18 [‐9.79, 5.43] |
| 3 Volume of the leg (mL) | 9 | 1041 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.38 [‐0.50, ‐0.25] |
| 3.1 Aminaftone | 1 | 79 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.17 [‐0.61, 0.28] |
| 3.2 Calcium dobesilate | 3 | 475 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.50 [‐0.68, ‐0.31] |
| 3.3 Rutosides | 5 | 487 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.29 [‐0.47, ‐0.11] |
| 4 Patients with ulcer (dichotomous variable) | 5 | 392 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.78, 1.15] |
| 4.1 Aminaftone | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.18, 3.18] |
| 4.2 Diosmine, Hidrosmine | 2 | 133 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.70, 1.03] |
| 4.3 Rutosides | 2 | 159 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.84, 1.87] |
| 5 Trophic disorders (dichotomous variable) | 6 | 705 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.81, 0.95] |
| 5.1 Aminaftone | 1 | 97 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.41, 1.44] |
| 5.2 Diosmine, Hidrosmine | 4 | 504 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.81, 0.94] |
| 5.3 Rutosides | 1 | 104 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.71, 1.25] |
| 6 Pain in the lower legs (dichotomous variable) | 18 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.1 Aminaftone | 1 | 97 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.23, 0.79] |
| 6.2 Calcium dobesilate | 4 | 354 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.16, 0.93] |
| 6.3 Diosmine, Hidrosmine | 4 | 271 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.63, 1.08] |
| 6.4 French maritime pine bark extract | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.48, 0.91] |
| 6.5 Rutosides | 8 | 1318 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.45, 0.84] |
| 7 Pain in the lower legs (continuous variable) | 8 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Calcium dobesilate | 3 | 724 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.41, 0.18] |
| 7.2 Diosmine, Hidrosmine | 1 | 150 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.67, ‐0.02] |
| 7.3 French maritime pine bark extract | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.39 [‐2.09, ‐0.69] |
| 7.4 Rutosides | 3 | 219 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.71 [‐1.23, ‐0.19] |
| 8 Cramps in the lower legs (dichotomous variable) | 12 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 8.1 Aminaftone | 1 | 97 | Risk Ratio (M‐H, Random, 95% CI) | 0.56 [0.31, 0.99] |
| 8.2 Calcium dobesilate | 2 | 255 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.50, 0.84] |
| 8.3 Diosmine, Hidrosmine | 3 | 214 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.70, 0.98] |
| 8.4 Rutosides | 6 | 1060 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.45, 1.05] |
| 9 Cramps in the lower legs (continuous variable) | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 9.1 Calcium dobesilate | 1 | 415 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.29, 0.09] |
| 9.2 Diosmine, Hidrosmine | 1 | 150 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.78, ‐0.14] |
| 9.3 Rutosides | 2 | 164 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.83 [‐1.50, ‐0.16] |
| 10 Restless legs (dichotomous variable) | 7 | 652 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.72, 0.91] |
| 10.1 Calcium dobesilate | 2 | 255 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.59, 0.91] |
| 10.2 Diosmine, Hidrosmine | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.70, 1.15] |
| 10.3 Rutosides | 4 | 327 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.72, 1.01] |
| 11 Itching in the lower legs (dichotomous variable) | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 11.1 Aminaftone | 1 | 97 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.31, 0.91] |
| 11.2 Diosmine, Hidrosmine | 1 | 34 | Risk Ratio (M‐H, Random, 95% CI) | 1.63 [0.51, 5.25] |
| 11.3 Rutosides | 2 | 274 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.21, 2.21] |
| 12 Itching in the lower legs (continuous variable) | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 12.1 Calccium dobesilate | 1 | 416 | Std. Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.11, 0.28] |
| 12.2 Rutosides | 1 | 60 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐1.10, ‐0.06] |
| 13 Heaviness in the lower legs (dichotomous variable) | 17 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 13.1 Aminaftone | 1 | 97 | Risk Ratio (M‐H, Random, 95% CI) | 0.32 [0.17, 0.60] |
| 13.2 Calcium dobesilate | 3 | 305 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.08, 1.42] |
| 13.3 Centella asiatica | 1 | 63 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.32, 1.19] |
| 13.4 Diosmine, Hidrosmine | 4 | 241 | Risk Ratio (M‐H, Random, 95% CI) | 0.60 [0.35, 1.05] |
| 13.5 French maritime pine bark extract | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.76, 1.07] |
| 13.6 Rutosides | 7 | 1253 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.49, 0.78] |
| 14 Heaviness in the lower legs (continuous variable) | 9 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 14.1 Calcium dobesilate | 2 | 483 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.23, 0.13] |
| 14.2 Diosmine, Hidrosmine | 1 | 150 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.69 [‐1.02, ‐0.36] |
| 14.3 French maritime pine bark extract | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.50 [‐2.21, ‐0.79] |
| 14.4 Rutosides | 5 | 360 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.27 [‐2.22, ‐0.32] |
| 15 Swelling in the lower legs (dichotomous variable) | 12 | 905 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.49, 0.81] |
| 15.1 Calcium dobesilate | 2 | 80 | Risk Ratio (M‐H, Random, 95% CI) | 0.19 [0.08, 0.41] |
| 15.2 Diosmine, Hidrosmine | 2 | 104 | Risk Ratio (M‐H, Random, 95% CI) | 0.7 [0.52, 0.94] |
| 15.3 French maritime pine bark extract | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.64, 1.02] |
| 15.4 Rutosides | 7 | 681 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.49, 0.91] |
| 16 Swelling in the lower legs (continuous variable) | 6 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 16.1 Calcium dobesilate | 1 | 417 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.24, 0.15] |
| 16.2 Diosmine, Hidrosmine | 1 | 150 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.15 [‐1.50, ‐0.80] |
| 16.3 French maritime pine bark extract | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.65 [‐2.38, ‐0.92] |
| 16.4 Rutosides | 3 | 264 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.73 [‐3.50, 0.04] |
| 17 Paraesthesias in the lower legs (dichotomous variable) | 8 | 1309 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.48, 0.84] |
| 17.1 Calcium dobesilate | 3 | 305 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.51, 1.08] |
| 17.2 Diosmine, Hidrosmine | 2 | 144 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.62, 1.05] |
| 17.3 Rutosides | 3 | 860 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.35, 0.66] |
| 18 Paraesthesias in the lower legs (continuous variable) | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 18.1 Diosmine, Hidrosmine | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 Quality of life | 3 | 696 | Mean Difference (IV, Fixed, 95% CI) | ‐1.04 [‐2.55, 0.47] |
| 19.1 Aminaftone | 1 | 79 | Mean Difference (IV, Fixed, 95% CI) | ‐10.0 [‐17.01, ‐2.99] |
| 19.2 Calcium dobesilate at 3 months of treatment | 2 | 617 | Mean Difference (IV, Fixed, 95% CI) | ‐0.60 [‐2.15, 0.95] |
| 20 Global assessment by the participant (dichotomous variable) | 15 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 20.1 Calcium dobesilate | 4 | 758 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.61, 1.19] |
| 20.2 Centella asiatica | 1 | 80 | Risk Ratio (M‐H, Random, 95% CI) | 0.28 [0.14, 0.57] |
| 20.3 Diosmine, Hidrosmine | 4 | 451 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.59, 0.96] |
| 20.4 Rutosides | 6 | 1000 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.26, 0.97] |
| 21 Global assessment by the participant (continuous variable) | 7 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 21.1 Calcium dobesilate | 2 | 448 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐0.71, ‐0.33] |
| 21.2 Diosmine, Hidrosmine | 1 | 150 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.81 [‐1.14, ‐0.47] |
| 21.3 Rutosides | 4 | 283 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.18 [‐1.96, ‐0.39] |
| 22 Adverse events | 32 | 3887 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [1.03, 1.38] |
| 22.1 Aminaftone | 1 | 79 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.06, 6.32] |
| 22.2 Calcium dobesilate | 7 | 1473 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.23 [0.99, 1.53] |
| 22.3 Centella asiatica | 1 | 94 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.58, 2.23] |
| 22.4 Diosmine, Hidrosmine | 8 | 837 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.70, 1.44] |
| 22.5 Grape seed extract | 1 | 75 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.19, 1.74] |
| 22.6 Rutosides | 14 | 1329 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.34 [1.02, 1.76] |
3.1. Analysis.
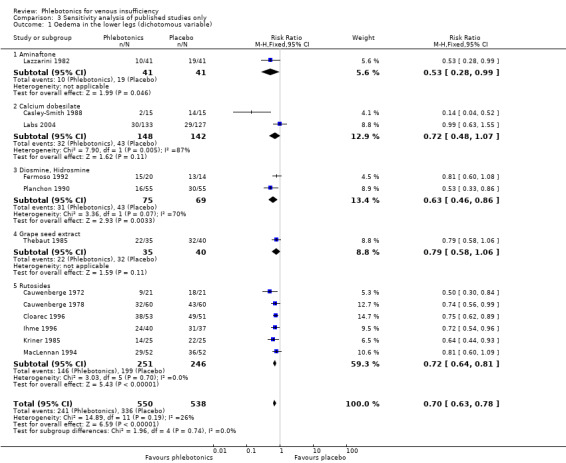
Comparison 3 Sensitivity analysis of published studies only, Outcome 1 Oedema in the lower legs (dichotomous variable).
3.2. Analysis.
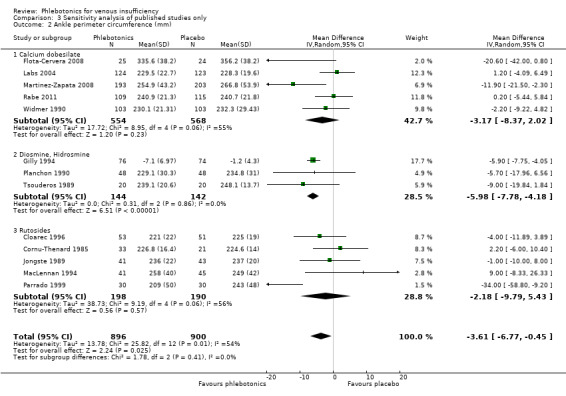
Comparison 3 Sensitivity analysis of published studies only, Outcome 2 Ankle perimeter circumference (mm).
3.3. Analysis.
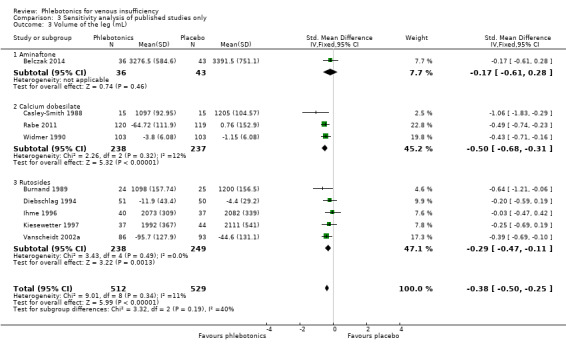
Comparison 3 Sensitivity analysis of published studies only, Outcome 3 Volume of the leg (mL).
3.4. Analysis.
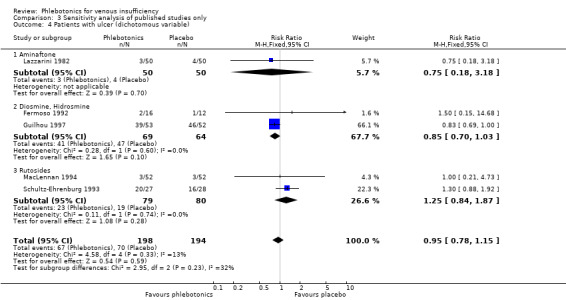
Comparison 3 Sensitivity analysis of published studies only, Outcome 4 Patients with ulcer (dichotomous variable).
3.5. Analysis.
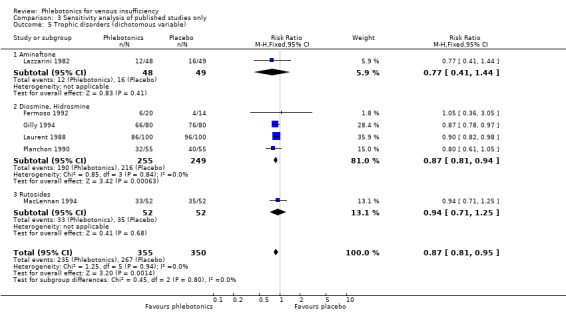
Comparison 3 Sensitivity analysis of published studies only, Outcome 5 Trophic disorders (dichotomous variable).
3.6. Analysis.
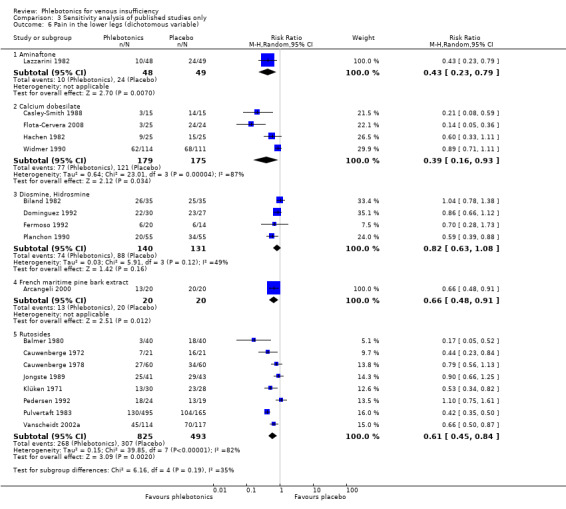
Comparison 3 Sensitivity analysis of published studies only, Outcome 6 Pain in the lower legs (dichotomous variable).
3.7. Analysis.
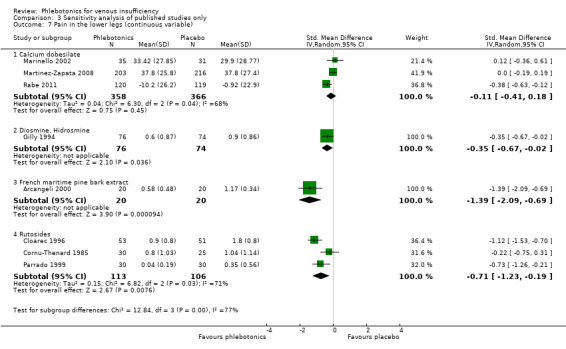
Comparison 3 Sensitivity analysis of published studies only, Outcome 7 Pain in the lower legs (continuous variable).
3.8. Analysis.
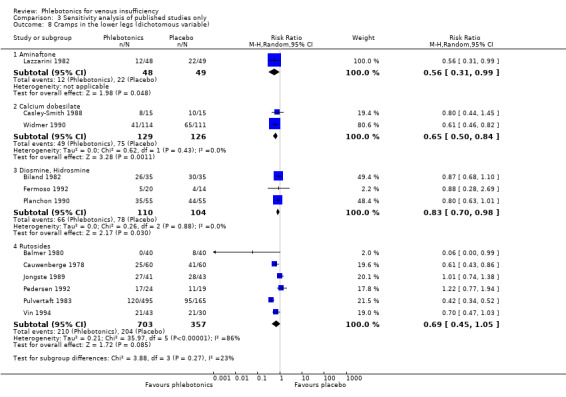
Comparison 3 Sensitivity analysis of published studies only, Outcome 8 Cramps in the lower legs (dichotomous variable).
3.9. Analysis.
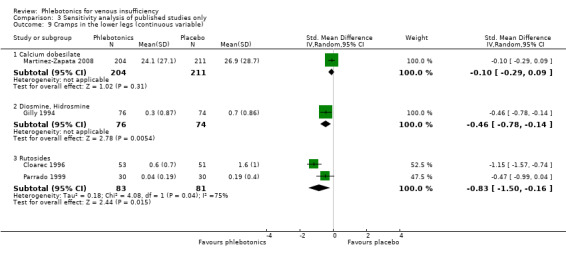
Comparison 3 Sensitivity analysis of published studies only, Outcome 9 Cramps in the lower legs (continuous variable).
3.10. Analysis.
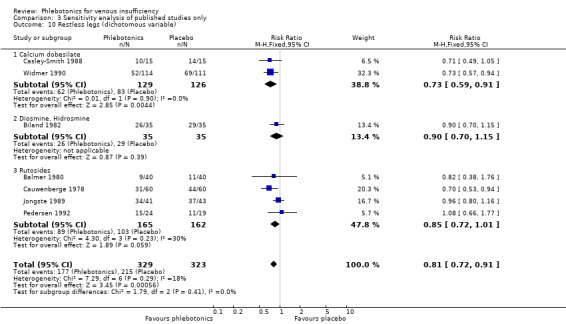
Comparison 3 Sensitivity analysis of published studies only, Outcome 10 Restless legs (dichotomous variable).
3.11. Analysis.
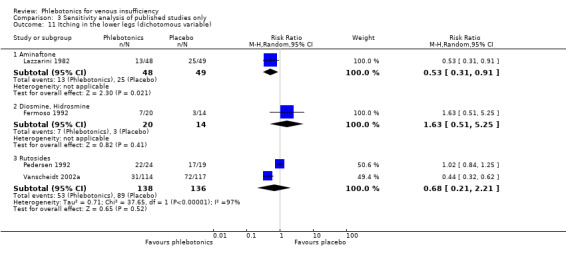
Comparison 3 Sensitivity analysis of published studies only, Outcome 11 Itching in the lower legs (dichotomous variable).
3.12. Analysis.
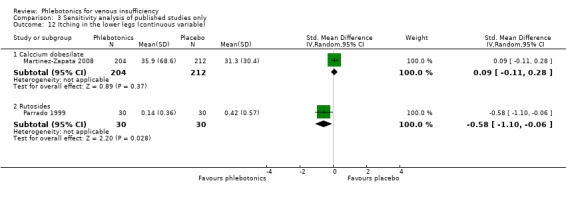
Comparison 3 Sensitivity analysis of published studies only, Outcome 12 Itching in the lower legs (continuous variable).
3.13. Analysis.
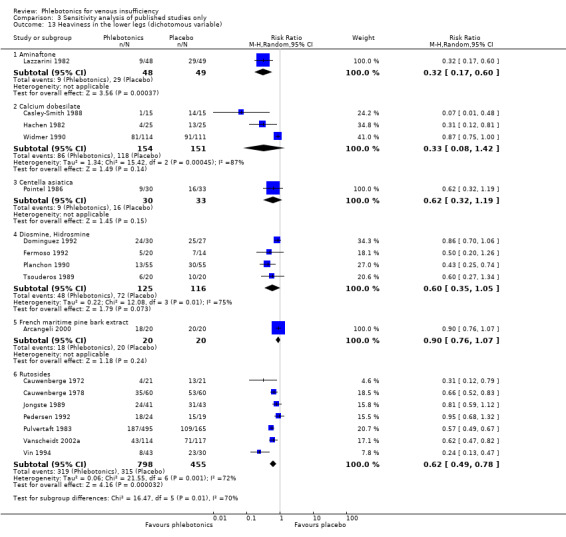
Comparison 3 Sensitivity analysis of published studies only, Outcome 13 Heaviness in the lower legs (dichotomous variable).
3.14. Analysis.
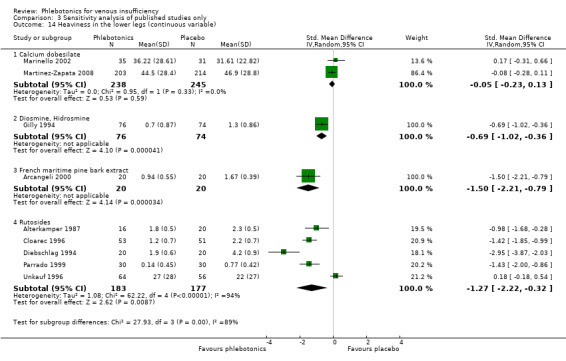
Comparison 3 Sensitivity analysis of published studies only, Outcome 14 Heaviness in the lower legs (continuous variable).
3.15. Analysis.
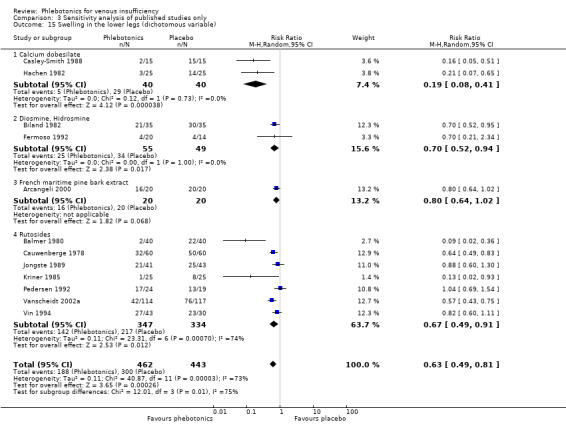
Comparison 3 Sensitivity analysis of published studies only, Outcome 15 Swelling in the lower legs (dichotomous variable).
3.16. Analysis.
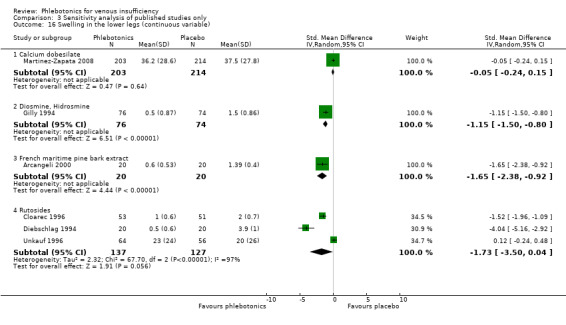
Comparison 3 Sensitivity analysis of published studies only, Outcome 16 Swelling in the lower legs (continuous variable).
3.17. Analysis.
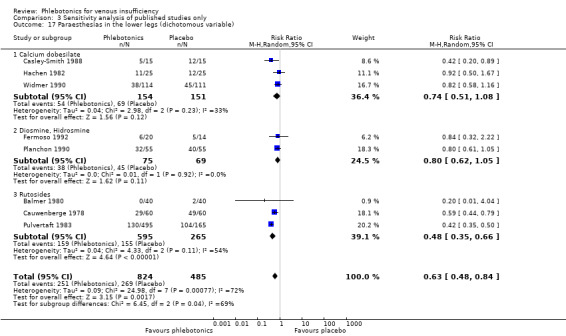
Comparison 3 Sensitivity analysis of published studies only, Outcome 17 Paraesthesias in the lower legs (dichotomous variable).
3.18. Analysis.
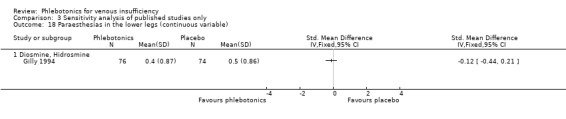
Comparison 3 Sensitivity analysis of published studies only, Outcome 18 Paraesthesias in the lower legs (continuous variable).
3.19. Analysis.
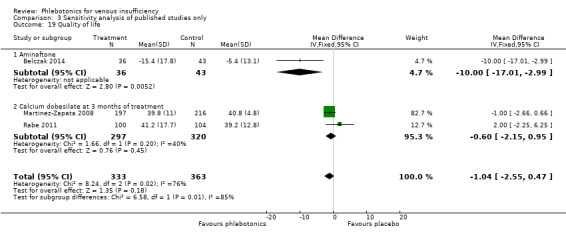
Comparison 3 Sensitivity analysis of published studies only, Outcome 19 Quality of life.
3.20. Analysis.
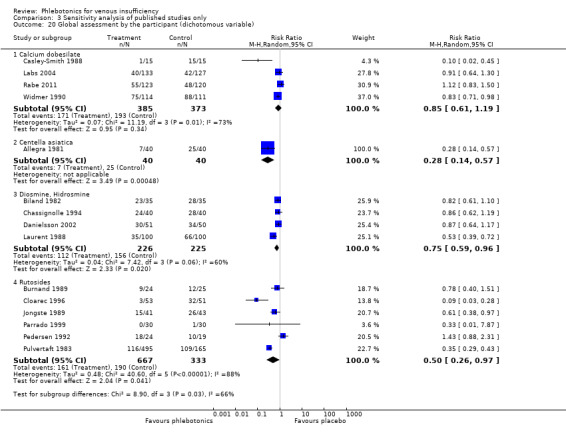
Comparison 3 Sensitivity analysis of published studies only, Outcome 20 Global assessment by the participant (dichotomous variable).
3.21. Analysis.
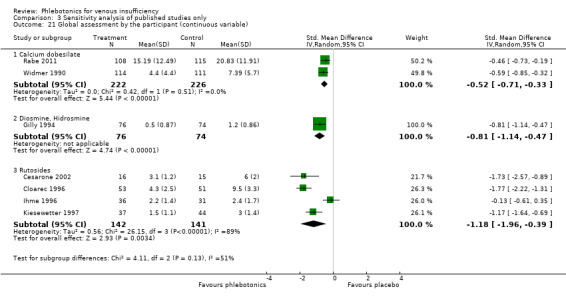
Comparison 3 Sensitivity analysis of published studies only, Outcome 21 Global assessment by the participant (continuous variable).
3.22. Analysis.
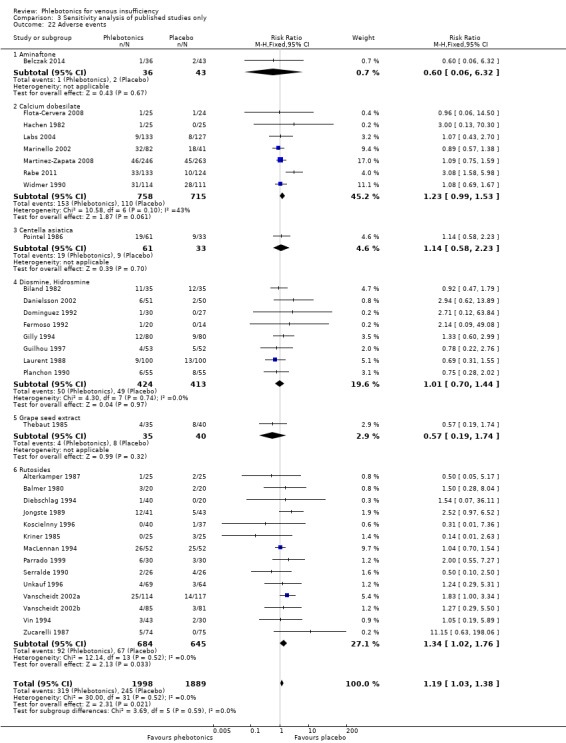
Comparison 3 Sensitivity analysis of published studies only, Outcome 22 Adverse events.
Comparison 4. Sensitivity analysis based on low risk of bias.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Oedema in the lower legs (dichotomous variable) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Calcium dobesilate | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Ankle perimeter circumference (mm) | 3 | 867 | Mean Difference (IV, Random, 95% CI) | ‐2.34 [‐8.79, 4.11] |
| 2.1 Calcium dobesilate | 3 | 867 | Mean Difference (IV, Random, 95% CI) | ‐2.34 [‐8.79, 4.11] |
| 3 Volume of the leg (mL) | 2 | 418 | Mean Difference (IV, Fixed, 95% CI) | ‐59.08 [‐84.40, ‐33.76] |
| 3.1 Calcium dobesilate | 1 | 239 | Mean Difference (IV, Fixed, 95% CI) | ‐65.48 [‐99.47, ‐31.49] |
| 3.2 Rutosides | 1 | 179 | Mean Difference (IV, Fixed, 95% CI) | ‐51.1 [‐89.06, ‐13.14] |
| 4 Pain in the lower legs (dichotomous variable) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 Rutosides | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Pain in the lower legs (continuous variable) | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Calcium dobesilate | 2 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Cramps in the lower legs (continuous variable) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 Calcium dobesilate | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Itching in the lower legs (dichotomous variable) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.1 Rutosides | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Itching in the lower legs (continuous variable) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 8.1 Calcium dobesilate | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Heaviness in the lower legs (dichotomous variable) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9.1 Rutosides | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Heaviness in the lower legs (continuous variable) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 Calcium dobesilate | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Swelling in the lower legs (dichotomous variable) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 11.1 Rutosides | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Swelling in the lower legs (continuous variable) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 12.1 Calcium dobesilate | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Quality of life | 2 | 617 | Mean Difference (IV, Fixed, 95% CI) | ‐0.60 [‐2.15, 0.95] |
| 13.1 Calcium dobesilate at 3 months of treatment | 2 | 617 | Mean Difference (IV, Fixed, 95% CI) | ‐0.60 [‐2.15, 0.95] |
| 14 Global assessment by the participant (dichotomous variable) | 2 | 476 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.81, 1.32] |
| 14.1 Calcium dobesilate | 2 | 476 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.81, 1.32] |
| 15 Global assessment by the participant (continuous variable) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 15.1 Calcium dobesilate | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Adverse events | 4 | 1257 | Risk Ratio (M‐H, Random, 95% CI) | 1.59 [0.97, 2.63] |
| 16.1 Calcium dobesilate | 3 | 1026 | Risk Ratio (M‐H, Random, 95% CI) | 1.53 [0.76, 3.09] |
| 16.2 Rutosides | 1 | 231 | Risk Ratio (M‐H, Random, 95% CI) | 1.83 [1.00, 3.34] |
4.4. Analysis.
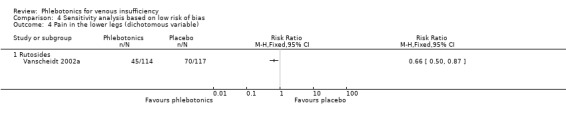
Comparison 4 Sensitivity analysis based on low risk of bias, Outcome 4 Pain in the lower legs (dichotomous variable).
4.5. Analysis.
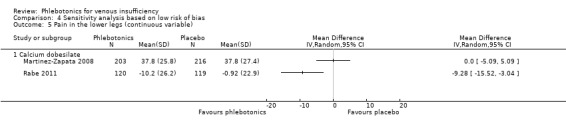
Comparison 4 Sensitivity analysis based on low risk of bias, Outcome 5 Pain in the lower legs (continuous variable).
4.6. Analysis.
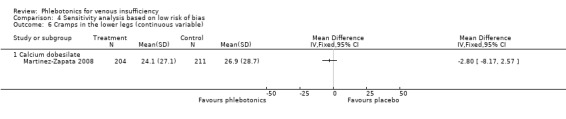
Comparison 4 Sensitivity analysis based on low risk of bias, Outcome 6 Cramps in the lower legs (continuous variable).
4.11. Analysis.
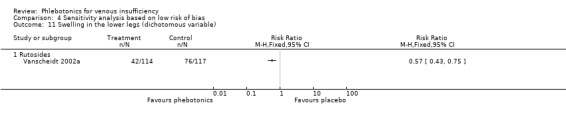
Comparison 4 Sensitivity analysis based on low risk of bias, Outcome 11 Swelling in the lower legs (dichotomous variable).
4.13. Analysis.
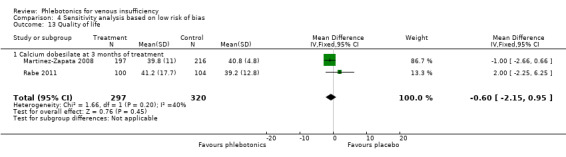
Comparison 4 Sensitivity analysis based on low risk of bias, Outcome 13 Quality of life.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Allegra 1981.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: table of random numbers Exclusions post randomisation: none Losses to follow‐up: none |
|
| Participants | Country: Italy Setting: hospital Number: 80 patients Age: not stated Gender: not stated Inclusion criteria: patients with postphlebitic syndrome, oedema of the lower limb, phlebolymphoedema, constitutional venous stasis, varices Exclusion criteria: not stated |
|
| Interventions | Treatment: 2 × 10 mg Centella tablets 3× per day Control: placebo Duration: 30 days Follow‐up: 30 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The assignment of patients to one of two treatments, labelled as A or B, was made randomly using a special randomization list" Comment: a randomisation list is generally accepted as a fair method of ensuring a random sequence |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information given about methods used for allocation concealment |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Low risk | Comment: no exclusions post randomisation and no losses to follow‐up |
| Selective reporting | Unclear risk | Comment: the number of participants in both groups was described. However, a table with important characteristics was lacking; this could lower the generalisability. Adverse events, tolerability and signs of intolerance were presented |
Alterkamper 1987.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: 3/50 (6%) |
|
| Participants | Country: France Setting: not stated Number: 50 patients Age: mean 53 ± 9 years Gender: 13 M:37 F Inclusion criteria: symptomatic stage I to II of CVI Exclusion criteria: oedemas requiring compression, post‐thrombotic syndrome, lymphoedema; cardiac, renal or hepatic failure; diuretics; pregnancy; severe disease |
|
| Interventions | Treatment: 1.86 mg ruscus and 75 mg hesperidin. 2 capsules 3× per day Control: placebo Duration: 28 days Follow‐up: 28 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "In a randomized double‐blind study..." Comment: no information given about method of randomisation |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information given about allocation concealment |
| Blinding (patients) | Low risk | Quote: "The Phlebodril and placebo capsules had the same external appearance" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "The Phlebodril and placebo capsules had the same external appearance" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "The Phlebodril and placebo capsules had the same external appearance" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Quote: "Three patients dropped out for reasons unconnected with this study" Comment: number in each group described, and number of participants who dropped out of the study prematurely presented |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Arcangeli 2000.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: none |
|
| Participants | Country: Italy Setting: clinical centre Number: 40 patients Age: mean 57.95 ± 12.78 years pycnogenol group; mean 61.40 ± 10.62 years placebo group Gender: 13 M:27 F Inclusion criteria: symptomatic CVI as a consequence of deep venous thrombosis or idiopathic venous lymphatic deficiency Exclusion criteria: cardiovascular, diuretics, analgesic or anti‐inflammatory drugs |
|
| Interventions | Treatment: french maritime pine bark extract, 100 mg 3× per day Control: placebo Duration: 69 days Follow‐up: 60 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "After the 2‐week run‐in period, the patients were randomly divided into two groups and assigned to a treatment with Pycnogenol, 100 mg × 3/day or a placebo for a period of 2 months" Comment: no method of randomisation stated |
| Allocation concealment (selection bias) | Unclear risk | Comment: no method of allocation concealment stated |
| Blinding (patients) | Low risk | Quote: "The placebo visually matched the test drug" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "The placebo visually matched the test drug" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "The placebo visually matched the test drug" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: no exclusions post randomisation and no losses to follow‐up described |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Balmer 1980.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: none |
|
| Participants | Country: Switzerland Setting: not stated Number: 40 patients Age: mean 46.2 ± 14.1 years active group; mean 52.3 ± 14.1 years placebo group Gender: 4 M:36 F Inclusion criteria: CVI without venous ulcers Exclusion criteria: varicose ulcers |
|
| Interventions | Treatment: oxirutoside 900 mg per day Control: placebo Duration: 28 days Follow‐up: 28 days Compression therapy was allowed if participants were unwilling to abandon this support |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The trial was double‐blind, randomised, placebo controlled, between patients..." Comment: no information given about method of randomisation used |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information given about method of treatment allocation used |
| Blinding (patients) | Low risk | Quote: "Patients receiving respectively the test drug or identical placebo" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "Patients receiving respectively the test drug or identical placebo" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "Patients receiving respectively the test drug or identical placebo" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: no exclusions post randomisation and no losses to follow‐up |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Belczak 2014.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: 9/136 (6.6%) |
|
| Participants | Country: Brazil Setting: Department of Vascular Surgery of Sao Camilo Medical School Number: 136 patients Age: mean 52.8 ± 16.4 years active group; mean 50.6 ± 13.1 years placebo group Gender: 33 M:103 F Inclusion criteria: treatment‐naïve (no history of pharmacological or compression therapy), CVD (CEAP grades 2 to 5) Exclusion criteria: other conditions that might produce lower extremity‐related symptoms |
|
| Interventions | Treatments: micronised diosmine (450 mg) + hesperidin (50 mg), aminaftone (75 mg), coumarin (15 mg), troxerutin (90 mg) Control: placebo Duration: 112 days Follow‐up: 112 days Compression therapy: not used |
|
| Outcomes | Primary
Secondary
|
|
| Notes | Funding: all medications and placebos purchased by the investigators | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The patients were randomly divided into four groups" Comments: no methods of randomisation described |
| Allocation concealment (selection bias) | Low risk | Quote: "All tablets (active and placebo) were randomly divided into numbered bottles by an external investigator..." |
| Blinding (patients) | Low risk | Quote: "All tablets (active and placebo) were randomly divided into numbered bottles by an external investigator, and the contents of each bottle were unmasked only at the time of statistical analysis" |
| Blinding (study researchers) | Low risk | Quote: "All tablets (active and placebo) were randomly divided into numbered bottles by an external investigator, and the contents of each bottle were unmasked only at the time of statistical analysis" |
| Blinding (outcome assessment) | Low risk | Quote: "Assessors were blind to the treatment groups" |
| Incomplete outcome data | Low risk | Comment: very few participants lost to follow‐up |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Bergqvist 1981.
| Methods | Study design: randomised, cross‐over, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: 6/149 (4%) |
|
| Participants | Country: Sweden. Setting: outpatient clinic and local population Number: 149 patients Age: 'adults' Gender: 33 M:116 F Inclusion criteria: symptoms related to varicose veins and CVI Exclusion criteria: not stated |
|
| Interventions | Treatment: oxirutoside 1000 mg intravenous injection followed by 1 tablet of 500 mg per 8 hours Control: placebo Duration: 28 days Follow‐up: 28 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "They were then randomly allocated to treatment with either HR or identical placebo" Comment: no details of randomisation method provided |
| Allocation concealment (selection bias) | Unclear risk | Comment: no method of allocation concealment described |
| Blinding (patients) | Low risk | Quote: "The placebo regime was identical" and "... or identical placebo" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "The placebo regime was identical" and "... or identical placebo" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "The placebo regime was identical" and "... or identical placebo" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described. Loss to follow‐up described along with exclusions after randomisation, including reasons |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Biland 1982.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: 14/70 (20%) |
|
| Participants | Country: Germany Setting: hospital Number: 70 patients Age: mean 43 ± 13 years diosmine group; mean 39 ± 12.5 years placebo group Gender: 7 M:49 F Inclusion criteria: symptoms related to CVI and oedema Exclusion criteria: phlebitis, venous thromboses, post‐thrombotic syndrome, ulcus cruris, heart insufficiency, recent sclerotherapy or venous stripping, trauma, neuropathy, arthrosis, pregnancy |
|
| Interventions | Treatment: diosmine 450 mg plus hesperidin 50 mg, 2 capsules twice a day Control: placebo Duration: 28 days Follow‐up: 28 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The study was double‐blind, randomized, placebo with Daflon" Comment: no method of randomisation stated |
| Allocation concealment (selection bias) | Low risk | Quote: "Placebo tablets were given in indistinguishable numbered packaging" Comment: Indistinguishable number packaging ensures a fair method of allocation concealment |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Low risk | Comment: numbers of participants in each group reported, along with participants excluded after randomisation,reasons for exclusion and information on compliance |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Burnand 1989.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: none |
|
| Participants | Country: UK Setting: hospital Number: 49 patients Age: mean 53 years Gender: 18 M:31 F Inclusion criteria: venous reflux by volumetry, with varicose veins and lipodermatosclerosis Exclusion criteria: patients with ankle‐to‐arm arterial Doppler pressure ratio < 1.0 (significant arterial disease) |
|
| Interventions | Treatment: oxerutin (Paroven) 500 mg per 12 hours Control: placebo Duration: 30 days Follow‐up: 30 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "A double‐blind controlled trial was undertaken.." and "the two groups of patients were balanced and randomized by trial number so that as far as possible an equal number in each group..." Comment: no details of randomisation method provided |
| Allocation concealment (selection bias) | Unclear risk | Comment: no methods of allocation concealment described |
| Blinding (patients) | Low risk | Quote: "Were given Paroven 500 mg bd or identical placebo" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "Were given Paroven 500 mg bd or identical placebo" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "This code was not broken until the completion of the study" Comment: outcome assessors blinded |
| Incomplete outcome data | Low risk | Comment: neither exclusions post randomisation nor losses to follow‐up described |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Casley‐Smith 1988.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: none |
|
| Participants | Country: Australia Setting: university Number: 60 patients Age: 'adults' Gender: 28 M:32 F Inclusion criteria: 30 normal volunteer participants and 30 patients with CVI grade I to III Widmer (dilated subcutaneous veins, alteration of pigmentation, open or healed crural ulcer) Exclusion criteria: not stated |
|
| Interventions | Treatment: calcium dobesilate 1000 mg per day Control: placebo Duration: 42 days Follow‐up: 42 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "A randomized, double‐blind, placebo‐controlled technique was used. Because of carryover effects, a matched‐pair technique was used" Comment: no methods of randomisation stated |
| Allocation concealment (selection bias) | Unclear risk | Comment: no methods of allocation concealment stated |
| Blinding (patients) | Low risk | Quote: "Calcium dobesilate, or an identical placebo, were administered..." Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "Calcium dobesilate, or an identical placebo, were administered..." Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "Calcium dobesilate, or an identical placebo, were administered..." Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: no exclusions post randomisation and no losses to follow‐up described |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Cauwenberge 1972.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: 7/44 (16%) |
|
| Participants | Country: Belgium Setting: Liège Number: 44 patients Age: 'adults' Exclusion criteria: not stated Gender: not stated Inclusion criteria: varicose veins and postphlebitic syndrome Exclusion criteria: not stated |
|
| Interventions | Treatment: O‐(beta‐hydroxyethyl)‐rutoside 900 mg per day Control: placebo Duration: 28 days Follow‐up: 28 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | Description of 2 clinical trials (CTs): One is a parallel CT, and the other is a cross‐over CT. Only the parallel CT is included | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "44 patients were treated randomly and under double‐blind conditions" Comment: no specific methods stated for randomisation of participants |
| Allocation concealment (selection bias) | Unclear risk | Comment: no specific methods stated for allocation concealment |
| Blinding (patients) | Low risk | Quote: "In addition, a placebo identical in appearance to the active drug..." Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "In addition, a placebo identical in appearance to the active drug..." Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "In addition, a placebo identical in appearance to the active drug..." Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Unclear risk | Comment: number in each group described, including drop‐outs and those excluded after randomisation during follow‐up (7/44; 16%); reasons for drop‐out not provided |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Cauwenberge 1978.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: not stated Losses to follow‐up: 51/120 (42.5%) |
|
| Participants | Country: Belgium Setting: Liège Number: 120 patients Age: 'adults' Gender: not stated Inclusion criteria: varicose veins, postphlebitic syndrome Exclusion criteria: symptoms not attributed to CVI |
|
| Interventions | Treatment: O‐(beta‐hydroxyethyl)‐rutoside 1200 mg per day Control: placebo Duration: 90 days Follow‐up: 90 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The patients are divided into two series according to the degree of symptoms. Within these two series, patients were distributed randomly into two groups, receiving respectively the active ingredient or placebo" Comment: no method of randomisation stated |
| Allocation concealment (selection bias) | Unclear risk | Comment: no method of allocation concealment stated |
| Blinding (patients) | Low risk | Quote: "We also used a placebo of identical presentation" Comment: Identical placebo ensure double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "We also used a placebo of identical presentation" Comment: Identical placebo ensure double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "We also used a placebo of identical presentation" Comment: Identical placebo ensure double‐blinding |
| Incomplete outcome data | High risk | Comment: number of participants in each group described, but no information given on important characteristics of participants. Number of persons excluded after randomisation was important (51/120; 42.5%). Reasons for exclusion were given |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Cesarone 2002.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: none |
|
| Participants | Country: Italy Setting: hospital Number: 46 patients and 10 healthy individuals Age: 44 to 45 years Gender: percentages/numbers of men and women not specified Inclusion criteria: severe superficial venous incompetence with a normal deep venous system Exclusion criteria: diabetes, peripheral arterial disease |
|
| Interventions | Treatment A: hidroxirutoxide 500 mg tid Treatment B: hidroxirutoxide 1000 mg tid Control (group C): placebo tid Treatment D: hidroxirutoxide 1000 mg/d Duration: 28 days Follow‐up: 28 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: no randomisation methods stated |
| Allocation concealment (selection bias) | Unclear risk | Comment: no methods of allocation concealment stated |
| Blinding (patients) | Low risk | Comment: placebo used with the same frequency as in experimental groups |
| Blinding (study researchers) | Low risk | Comment: placebo used with the same frequency as in experimental groups |
| Blinding (outcome assessment) | Low risk | Comment: placebo used with the same frequency as in experimental groups |
| Incomplete outcome data | Low risk | Comment: no exclusions post randomisation and no losses to follow‐up |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Chassignolle 1994.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: 4/40 (10%) |
|
| Participants | Country: France Setting: hospital Number: 40 patients Age: 32.0 (1.3) years active group; 35.6 (1.1) years placebo group Gender: female Inclusion criteria: women with functional CVI Exclusion criteria: not stated |
|
| Interventions | Treatment: diosmine 1000 mg per day Control: placebo Duration: 60 days Follow‐up: 60 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomly assigned to two parallel groups of 20" Comment: no randomisation methods stated |
| Allocation concealment (selection bias) | Unclear risk | Comment: no methods of allocation concealment stated |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described, number of participants who dropped out prematurely stated and reasons for dropping out described |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Cloarec 1994.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: 16/120 (13%) Losses to follow‐up: not stated |
|
| Participants | Country: France Setting: not stated Number: 120 patients Age: mean 50 years Gender: not stated Inclusion criteria: history of CVI for several years Exclusion criteria: not stated |
|
| Interventions | Treatment: O‐(beta‐hydroxyethyl)‐rutoside 2000 mg per day Control: placebo Duration: 56 days Follow‐up: 56 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | This clinical trial is published in abstract format; not possible to extract data showing results | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "A multicenter double blind randomized clinical trial was designed" Comment: no methods described for randomisation of participants |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information given about methods used for allocation concealment |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Low risk | Comment: only 13% drop‐out rate (16/120) for violation of study protocol reported |
| Selective reporting | High risk | Comment: no protocol identified. In the methods section, subjective symptoms identified that were not reported in the results section (pain, heaviness, swelling, restless leg, cramps, presence of pitting oedema) |
Cloarec 1996.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: 5/109 (5%) Losses to follow‐up: none |
|
| Participants | Country: France Setting: outpatient university clinic in a military hospital Number: 109 patients Age: 48 ± 14 years active group; 53.6 ± 13.6 years placebo group Gender: 16 M:88 F Inclusion criteria: CVI (Widmer grade II) and oedema and symptoms Exclusion criteria: elastic stockings, arterial insufficiency, venous ulcers or superficial thrombophlebitis, venous surgery or sclerotherapy in the preceding 6 months, other possible causes of leg oedema, pregnancy, irregular menstrual cycles; therapy with diuretics, steroids, anti‐inflammatories or venous drugs |
|
| Interventions | Treatment: O‐(beta‐hydroxyethyl)‐rutoside 1000 mg per 12 hours Control: placebo Duration: 60 days Follow‐up: 60 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "For this reason, we undertook a randomized, double‐blind, placebo‐controlled trial..." Comment: no methods for randomisation of participants described |
| Allocation concealment (selection bias) | Unclear risk | Comment: no methods for allocation concealment described |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Low risk | Comment: only 5% drop‐out rate (5/109) for violation of study protocol. Number in each group provided, along with reasons for exclusion after randomisation and information on compliance |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Cornu‐Thenard 1985.
| Methods | Study design: randomised, multi‐centre, double‐blind, placebo‐controlled Method of randomisation: random distribution of numbered batches Exclusions post randomisation: not stated Losses to follow‐up: not stated |
|
| Participants | Country: France Setting: not stated Number: 83 patients Age: 20 to 65 years; mean 43.73 ± 11.92 years active group; mean 43.55 ± 11.42 years placebo group Gender: 6 M:77 F Inclusion criteria: symptoms related to CVI Exclusion criteria: severe damage to venous musculature requiring urgent treatment ‐ surgery or sclerosis; surgical operation on venous or deep or superficial vein thrombosis in the past year; sclerosis or heavy support bandages (light support bandages not excluded), major trophic lesions, Raynaud's syndrome, arteritis, lymphoedema, renal or cardiac insufficiency; anti‐migraine treatment, analgesic or anti‐inflammatory treatment, diuretic treatment, low‐sodium diet, treatment for cardiovascular system (except nifedipine) |
|
| Interventions | Treatment: extract Ruscus aculeatus 75 mg plus hesperidin 75 mg plus ascorbic acid 50 mg per day (Cyclo 3) Control: placebo Duration: 60 days Follow‐up: 60 days Light compression therapy allowed |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A double‐blind comparative study against placebo, using two groups treated in parallel, after random distribution of numbered batches of the two treatments to be compared" Comment: seems like a fair method of randomisation was conducted |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information given about methods used for allocation concealment |
| Blinding (patients) | Low risk | Quote: "The two products to be compared were presented in the form of identical capsules for both Cyclo 3 and placebo" Comment: Identical placebo ensures a fair method used for double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "The two products to be compared were presented in the form of identical capsules for both Cyclo 3 and placebo" Comment: Identical placebo ensures a fair method used for double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "The two products to be compared were presented in the form of identical capsules for both Cyclo 3 and placebo" Comment: Identical placebo ensures a fair method used for double‐blinding |
| Incomplete outcome data | Unclear risk | Quote: no information provided about participants who withdrew prematurely from the trial |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Danielsson 2002.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: sealed envelope principle Exclusions post randomisation: none Losses to follow‐up: 4/101 (4%) |
|
| Participants | Country: Sweden Setting: hospital Number: 101 patients Age: 18 to 65 years Gender: 28 M:73 F Inclusion criteria: symptomatic CVI with reflux venous, CEAP II classification Exclusion criteria: diabetes; inflammatory, heart, renal, hepatic or peripheral arterial disease. Treatment with diuretics or anti‐inflammatory drugs (steroids, NSAIDs). Allergic reactions to venoactive drugs |
|
| Interventions | Treatment: micronised purified flavonoid fraction (MPFF) 1000 mg per day Control: placebo Duration: 60 days Follow‐up: 60 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | No description of double‐blind | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "One hundred and one patients with symptomatic CVD were randomly allocated to treatment with either MPFF (51 patients) or placebo..." Comment: no methods described for randomisation of participants |
| Allocation concealment (selection bias) | Low risk | Quote: "After informed consent, patients were randomised in a blinded fashion (sealed envelope principle)" Comment: sealed envelope principle considered a good method to ensure allocation concealment |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described. In addition, information given about numbers of participants who withdrew prematurely (4/101; 4%) |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Diebschlag 1994.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: none |
|
| Participants | Country: Germany Setting: not stated Number: 60 postmenopausal females Age: 'adults' Gender: 60 F Inclusion criteria: stage II CVI (oedema and symptoms) Exclusion criteria: not stated |
|
| Interventions | Treatment: oxerutin 500 mg per day or 1000 mg per day Control: placebo Duration: 84 days Follow‐up period: 112 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The study design consisted of a double‐blind placebo controlled, randomized parallel group comparison with three treatment groups" Comment: no methods described for randomisation |
| Allocation concealment (selection bias) | Unclear risk | Comment: no methods described for allocation concealment |
| Blinding (patients) | Low risk | Quote: "All medications appeared to be identical with respect to volume, colour of the bottle and the smell of solution. The difference in taste could be accepted as this type is of solution was not commercially available and, therefore, unknown and unidentifiable to patients" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "All medications appeared to be identical with respect to volume, colour of the bottle and the smell of solution. The difference in taste could be accepted as this type is of solution was not commercially available and, therefore, unknown and unidentifiable to patients" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "All medications appeared to be identical with respect to volume, colour of the bottle and the smell of solution. The difference in taste could be accepted as this type is of solution was not commercially available and, therefore, unknown and unidentifiable to patients" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: no exclusions post randomisation and no losses to follow‐up |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
DOBESILATO500/2.
| Methods | Study design: randomised, multi‐centre, double‐blind, placebo‐controlled Method of randomisation: random list generated by computer Exclusions post randomisation: study interrupted Losses to follow‐up: study interrupted |
|
| Participants | Country: Spain Setting: hospital Number: 69 patients Age: 60.9 (13.9) years placebo; 63.0 (20.5) years calcium dobesilate Gender: 36 M:33 F Inclusion criteria: adult patients with venous ulcer (CEAP 6) that affected epidermis, dermis and/or subcutaneous tissue, with an area superior to 3 cm2, an ankle‐arm index 0.9 or superior and written informed consent of patients Exclusion criteria: diabetes mellitus I or II. Renal failure and dialysis. Vascular surgery needed Impossibility to use compressive measures on the leg. Use of topical antibiotics, silver dressing, growth factors; plasma‐rich platelets, skin graft, pentoxifylline, ultrasound, laser, hyperbaric oxygen, electrical stimulation or vacuum. Pregnancy. Breast feeding. No anti‐contraceptive measures. Allergy or intolerance to phlebotonics. Background of neutropenia or leucopenia. Basal leucocytes < 3.500/mL |
|
| Interventions | Treatment: calcium dobesilate 500 mg 3× per day (capsules) Control: placebo Duration: 180 days Follow‐up period: 365 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | Financial support for Laboratories Dr Esteve was withdrawn and the study was interrupted. Register at clinicatrial.gov: NCT00979836 We obtained information from researchers who conducted this unpublished and interrupted clinical trial |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The allocation to treatment was randomised, centralised and computer stratified in blocks, by ulcer size and centre" Comment: Random sequence ensured by computer‐stratified blocks |
| Allocation concealment (selection bias) | Low risk | Comment: Treatment allocated by researcher phoning the co‐ordinating centre |
| Blinding (patients) | Low risk | Quote: "... to placebo (inactive capsules of identical appearance and weight) twice a day" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "... to placebo (inactive capsules of identical appearance and weight) twice a day" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "... to placebo (inactive capsules of identical appearance and weight) twice a day" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | High risk | Study was interrupted when only 69 of the 230 necessary participants were included |
| Selective reporting | High risk | Study was not published |
Dominguez 1992.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: computer‐generated random number table Exclusions post randomisation: none Losses to follow‐up: 7/57 (12%) |
|
| Participants | Country: Spain Setting: hospital Number: 57 patients Age: 20 to 65 years Gender: 5 M:52 F Inclusion criteria: symptomatic CVI and varicose veins and oedema Exclusion criteria: elastic bandages, anti‐inflammatory drugs and diuretics not permitted. Surgical operation, thrombophlebitis, pregnancy, diabetes, cardiopathy, hepatopathy, nephropathy, varicose veins secondary to extrinsic compression and varicose ulcers excluded |
|
| Interventions | Treatment: hidrosmine 600 mg per day Control: placebo Duration: 45 days Follow‐up: 45 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "On entry, patients were assigned to one or other of the two treatment groups according to a computer‐generated random number table" Comment: computer‐generated random number table considered a fair method to ensure good randomisation |
| Allocation concealment (selection bias) | Unclear risk | Comment: no methods of allocation concealment described |
| Blinding (patients) | Low risk | Quote: "The medications were supplied in identical capsule form" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "The medications were supplied in identical capsule form" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "The medications were supplied in identical capsule form" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group reported, along with information on compliance, drop‐outs (7/57; 12%), reasons for drop‐out and adverse events. ITT analysis conducted |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Fermoso 1992.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: 6/34 (18%) |
|
| Participants | Country: Spain Setting: hospital Number: 34 patients Age: mean 53 ± 18 (range 21 to 86) years Gender: 20 M:14 F Inclusion criteria: CVI (varicose veins and/or disturbances of venous circulation by Doppler) Exclusion criteria: not stated |
|
| Interventions | Treatment: hidrosmine 600 mg per day Control: placebo Duration: 28 days Follow‐up: 28 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The 34 patients chosen were randomly assigned to two treatment groups" Comment: no methods of randomisation described |
| Allocation concealment (selection bias) | Unclear risk | Comment: no methods of allocation concealment described |
| Blinding (patients) | Low risk | Quote: "And the other group received placebo capsules indistinguishable from the hidrosmin capsules, according to the double‐blind technique" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "And the other group received placebo capsules indistinguishable from the hidrosmin capsules, according to the double‐blind technique" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "And the other group received placebo capsules indistinguishable from the hidrosmin capsules, according to the double‐blind technique" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described. In addition, number of participants who prematurely withdrew from the study (6/34; 18%) described |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Flota‐Cervera 2008.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: none |
|
| Participants | Country: Mexico Setting: hospital Number: 49 patients (25 in the calcium dobesilate group; 24 in the placebo group) Age: mean 52.20 ± 8.45 years Gender: 5 M:44 F Inclusion criteria: venous oedema Exclusion criteria: not stated |
|
| Interventions | Treatment: calcium dobesilate 1500 mg per day Control: placebo Duration: 49 days Follow‐up: 49 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "A single center, prospective, randomized double‐blind, parallel group, placebo‐controlled" Comment: no method of randomisation generation described |
| Allocation concealment (selection bias) | Unclear risk | Quote: "A single center, prospective, randomized double‐blind, parallel group, placebo‐controlled" Comment: no method of allocation concealment described |
| Blinding (patients) | Low risk | Comment: placebo capsules identical to calcium dobesilate capsules |
| Blinding (study researchers) | Low risk | Comment: placebo capsules identical to calcium dobesilate capsules |
| Blinding (outcome assessment) | Low risk | Comment: placebo capsules identical to calcium dobesilate capsules |
| Incomplete outcome data | Low risk | Comment: no exclusions post randomisation and no losses to follow‐up |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Gilly 1994.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: 10/160 (6%) |
|
| Participants | Country: France Setting: hospital Number: 160 patients Age: 'adults' Gender: 26 M:134 F Inclusion criteria: symptomatic disturbances of the veno‐lymphatic system Exclusion criteria: other or associated vascular diseases; oedema of cardiac, renal or hepatic origin; symptoms or signs of arterial, metabolic, neurological or orthopaedic origin; pregnancy; recent venous surgery; deep or superficial thrombosis in the past 6 months |
|
| Interventions | Treatment: micronised purified flavonoid fraction (MPFF) 1000 mg per day Control: placebo Duration: 42 days Follow‐up: 42 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Eighty patients were randomly allocated to the S 5682 group and eighty patients to the placebo group" Comment: no method of randomisation described |
| Allocation concealment (selection bias) | Unclear risk | Comment: no method of allocation concealment described |
| Blinding (patients) | Low risk | Quote: "Patients fulfilling the inclusion criteria were randomly allocated to receive one S 5682 tablet twice daily or matching placebo" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "Patients fulfilling the inclusion criteria were randomly allocated to receive one S 5682 tablet twice daily or matching placebo" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "Patients fulfilling the inclusion criteria were randomly allocated to receive one S 5682 tablet twice daily or matching placebo" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described. In addition, adverse events experienced, number of drop‐outs and reasons for drop‐outs described. Methods used for imputing missed data not described. Six per cent of participants lost to follow‐up |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Guilhou 1997.
| Methods | Study design: randomised, multi‐centre, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: 6/107 (6%) |
|
| Participants | Country: France Setting: hospital Number: 107 patients Age: 'adults' Gender: 30 M:77 F Inclusion criteria: venous ulcers Exclusion criteria: not stated Randomisation of treatment stratified according to ulcer size: < 10 cm or ≥ 10 cm |
|
| Interventions | Treatment: diosmine 450 mg plus hesperidin 50 mg per 12 hours plus compression stockings Control: placebo and standard compression stockings Duration: 60 days Follow‐up: 60 days |
|
| Outcomes | Primary endpoint
Secondary endpoint
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Randomisation of treatment was stratified according to the size of the ulcers" Comment: no method of randomisation described |
| Allocation concealment (selection bias) | Unclear risk | Comment: no method of allocation concealment described |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described. ITT analysis conducted. Information provided about participants who withdrew prematurely from the study, along with reasons for premature withdrawal |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Hachen 1982.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: 2/50 (4%) |
|
| Participants | Country: Switzerland Setting: hospital Number: 50 females Age: 10 to 45 years Gender: 50 F Inclusion criteria: recent onset of CVI; no venous surgery, presence of symptoms (heaviness, fatigue, etc.) or aggravation during prolonged sitting or standing or during premenstrual periods Exclusion criteria: pregnancy, diabetes, polyneuropathy, osteo‐articular lesions in the legs, arterial peripheral insufficiency, oral contraceptives, poor co‐operation |
|
| Interventions | Treatment: calcium dobesilate 1000 mg per day Control: placebo Duration: 28 days Follow‐up: 28 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Fifty female patients with recent onset of venous insufficiency were randomly allocated to two subgroups receiving either calcium dobesilate or a corresponding placebo" Comment: no method of randomisation of participants described |
| Allocation concealment (selection bias) | Unclear risk | Comment: no method of allocation concealment described |
| Blinding (patients) | Low risk | Quote: "Fifty female patients with recent onset of venous insufficiency were randomly allocated to two subgroups receiving either calcium dobesilate or a corresponding placebo" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "Fifty female patients with recent onset of venous insufficiency were randomly allocated to two subgroups receiving either calcium dobesilate or a corresponding placebo" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "Fifty female patients with recent onset of venous insufficiency were randomly allocated to two subgroups receiving either calcium dobesilate or a corresponding placebo" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described. Participants who withdrew prematurely from the trial described, along with reasons for withdrawal. Four per cent of participants lost to follow‐up |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Ihme 1996.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: Rancode computer software Exclusions post randomisation: none Losses to follow‐up: 11/77 (14%) |
|
| Participants | Country: Germany Setting: hospital Number: 77 patients Age: mean 57.3 ± 9.6 years active group; mean 59.8 ± 7.3 years placebo group Gender: 24 M:53 F Inclusion criteria: CVI stages I and II (oedema, symptoms, stem varicosis, post‐thrombotic syndrome, valvular insufficiency of the deep veins) Exclusion criteria: varicosis with surgical indication; active or healed ulcus cruris; acute thrombosis or venous inflammation; oedema due to cardiac or renal insufficiency; treatment with a diuretic, dihydroergotamine or any other drugs for venous therapy; other severe disorder |
|
| Interventions | Treatment: Buckwheat herb tea (rutoside) 270 mg per day Control: placebo Duration: 90 days Follow‐up: 112 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomisation was carried out by Rancode computer software (IDV Gauting, Germany)" Comment: Randomisation seems like a fair method to ensure a random sequence of participants |
| Allocation concealment (selection bias) | Unclear risk | Comment: no methods of allocation concealment described |
| Blinding (patients) | Low risk | Quote: "A blinded taste test with pharmacists demonstrated that the teas were similar in taste and appearance and hard to distinguish" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "A blinded taste test with pharmacists demonstrated that the teas were similar in taste and appearance and hard to distinguish" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "A blinded taste test with pharmacists demonstrated that the teas were similar in taste and appearance and hard to distinguish" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described. Number of drop‐outs and reasons for dropping out of the trial described. ITT analysis conducted |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Jongste 1986.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: none |
|
| Participants | Country: The Netherlands Setting: outpatient Number: 80 patients Age: 20 to 75 years Gender: male and female; breakdown not given Inclusion criteria: unilateral post‐thrombotic syndrome Exclusion criteria: elastic stockings; diuretics; venoactive drugs; open venous ulcers; paralysis of the leg with post‐thrombotic syndrome; arterial disease; oedema of other origin; regular users of anti‐inflammatories, corticosteroids or analgesics |
|
| Interventions | Treatment: O‐(beta‐Hydroxyethyl)‐rutosides 1200 mg per day Control: placebo Duration: 56 days Follow‐up: 56 days |
|
| Outcomes | Primary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The trial was double blind, randomised, placebo controlled between patients" Comment: no methods of randomisation described |
| Allocation concealment (selection bias) | Unclear risk | Comment: no methods of allocation concealment described. |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Low risk | Quote: number of participants in each group described. No losses reported |
| Selective reporting | High risk | Comment: no published protocol identified. In the methods section, outcomes of “restless legs” and “venous pressure” reported, but in the results/conclusion sections, no data regarding these outcomes reported |
Jongste 1989.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: computerised random assignment method used Exclusions post randomisation: 17/101 (17%) Losses to follow‐up: 3 (0.3%) |
|
| Participants | Country: The Netherlands Setting: hospital Number: 101 patients Age: 53 ± 12 years active group; 54 ± 13 years placebo group Gender: 48 M:35 F Inclusion criteria: unilateral post‐thrombotic syndrome > 6 months' duration and history of venography with deep vein thrombosis Exclusion criteria: elastic stockings; veno‐active drugs within 2 weeks of entry into the trial; active venous ulcer; pregnancy; age > 75 years |
|
| Interventions | Treatment: oxirutosides 1200 mg per day Control: placebo Duration: 56 days Follow‐up: 56 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | Concealment of placebo not explicit | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Upon entering the study, patients were randomly assigned to receive either HR or placebo with the use of a computerized random assignment method" Comment: computerised random assignment method generally accepted as a good method to generate a random sequence of participants |
| Allocation concealment (selection bias) | Low risk | Quote: "A series of coded sealed envelopes for decoding any particular case was supplied to the local hospital pharmacy" Comment: sealed envelopes generally accepted as a good method of allocation concealment |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described, along with number of participants who dropped out and number who experienced adverse events |
| Selective reporting | High risk | Comment: no published protocol identified. In the methods section, outcomes of “restless legs” and “venous pressure” reported, but in the results/conclusion sections, no data regarding these outcomes reported |
Kiesewetter 1997.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: not stated Losses to follow‐up: not stated |
|
| Participants | Country: Germany Setting: university Number: 81 patients Age: mean 59 ± 7 years Gender: 26 M:55 F Inclusion criteria: stage I to II of Wert CVI Exclusion criteria: acute thromboses; ulcus cruris; heart insufficiency; recent venous surgery; venoactive drugs |
|
| Interventions | Treatment: 500 mg Buckwheat herb and 30 mg troxerutin. 2 tablets 3× per day Control: placebo Duration: 84 days Follow‐up: 112 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "For randomization of patients, the program was 'Rancode' of the company IDV data analysis and experimental design, Gauting, used" Comment: computerised generation of a random sequence generally accepted as a fair method of randomisation |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information given about methods used for allocation concealment |
| Blinding (patients) | Low risk | Quote: "The same number of identical‐looking placebo tablets consisting of lactose were given" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "The same number of identical‐looking placebo tablets consisting of lactose were given" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "The same number of identical‐looking placebo tablets consisting of lactose were given" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Unclear risk | Comment: number of participants in each group described. No information provided about participants who prematurely dropped out of the study |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Klüken 1971.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: not stated Losses to follow‐up: not stated |
|
| Participants | Country: Germany Setting: hospital Number: 60 patients Age: 'adults' Gender: not stated Inclusion criteria: CVI (varicoses or post‐thrombotic syndrome) Exclusion criteria: not stated |
|
| Interventions | Treatment: troxerutin 75 mg and coumarin 15 mg per day Control: placebo Duration: 21 days Follow‐up: 21 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Double‐blind, randomized, placebo‐controlled. In two parallel groups" Comment: information about methods of randomisation not provided |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information about methods of allocation concealment provided |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Unclear risk | Comment: number of participants in each group described. No information provided about the number of participants who dropped out of the study prematurely or the number who experienced adverse events |
| Selective reporting | Unclear risk | Comment: no published protocol identified. No outcomes reported in the methods section |
Koscielnny 1996.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: 6/77 (8%) |
|
| Participants | Country: Germany Setting: university Number: 94 patients selected; 67 randomised Age: 'adults' Gender: not stated Inclusion criteria: CVI stage I to II Widmer Exclusion criteria: not stated |
|
| Interventions | Treatment: Buckwheat herb tea 3× 1.8 g per day Control: placebo tea Duration: 84 days Follow‐up: 112 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "After a placebo period of two weeks, patients were randomly assigned to active treatment or a placebo group" Comment: no information about methods of randomisation provided |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information about methods of allocation concealment provided |
| Blinding (patients) | Low risk | Quote: "Placebo is with taste and appearance indistinguishable from the treatment" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "Placebo is with taste and appearance indistinguishable from the treatment" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "Placebo is with taste and appearance indistinguishable from the treatment" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in both placebo and treatment groups described, along with the most important participant characteristics, numbers of participants who dropped out prematurely, reasons for drop‐out, influence of drop‐outs and information on compliance |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Kriner 1985.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: not stated Losses to follow‐up: not stated |
|
| Participants | Country: Germany Setting: hospital Number: 50 patients Age: 'adults' Gender: not stated Inclusion criteria: disturbances of venous blood flow, oedema Exclusion criteria: not stated |
|
| Interventions | Treatment: ruscus extract 75 mg and hesperidin 75 mg 2 × 2 capsules per day. rutoside cream once per day Control: placebo Duration: 28 days Follow‐up: 28 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The two groups were balanced and comparable with respect to age, weight, and type and duration of disturbances" Comment: no method of randomisation described |
| Allocation concealment (selection bias) | Unclear risk | Comment: no method of allocation concealment described |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Unclear risk | Comment: number in each group described, but important characteristics lacking. In addition, number of participants who dropped out prematurely or were excluded after randomisation not described |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Labs 2004.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: computerised random assignment method Exclusions post randomisation: 7/260 (0.3%), protocol violation Losses to follow‐up: 21/260 (8%) |
|
| Participants | Country: Switzerland Setting: university Number: 260 patients Age: 20 to 70 years Gender: 16 M:201 F Inclusion criteria: CVI class 1 to 4 (CEAP classification), oedema and symptoms Exclusion criteria: CVI class 5 to 6 (CEAP classification); other causes of oedema (cardiac, renal, etc.); hypertension with change in treatment within 6 weeks of study start; obesity; peripheral arterial occlusive disease; venous surgery in the past 12 months or sclerotherapy during the past 6 months; irregular menstrual cycle; elevated transaminases; neutropenia; significant renal insufficiency; gastrointestinal disease; allergy to study medication; pregnant or lactating women; unreliable patient (psychiatric disorders, alcoholism, etc.); compression stockings or bandages; diuretics; venotropic medication; antiphlogistic drugs; corticosteroids; analgesics |
|
| Interventions | Treatment: calcium dobesilate 1500 mg per day Control: placebo Duration: 28 days Follow‐up: 42 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | Reasons for withdrawal unknown | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The corresponding boxes were randomized in balanced blocks and were labelled by the sponsor with the study number, the dosage, the batch numbers, with the patient number and with the note 'for clinical trials only'. The randomization was done by BIOMETRIX S. A., CH‐1911 Gland, Switzerland, using appropriate software" Comment: computer‐generated list of random numbers accepted as a good method for generating a random sequence of participants |
| Allocation concealment (selection bias) | Low risk | Quote: "The allocation of the study treatment to each patient was done according to the next available consecutive patient number printed on the prescription card and on the label of the box. This number was recorded on each page of the CRF.¨ and ¨Each investigator was provided with a sealed envelope containing the code for each patients randomisation number" Comment: seems like a fair method of allocation concealment |
| Blinding (patients) | Low risk | Quote: "For the double‐blind treatment period, the boxes, labels, and capsules containing Doxium 500 and placebo were identical in appearance for each drug, to ensure patient and investigator blinding" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "For the double‐blind treatment period, the boxes, labels, and capsules containing Doxium 500 and placebo were identical in appearance for each drug, to ensure patient and investigator blinding" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "For the double‐blind treatment period, the boxes, labels, and capsules containing Doxium 500 and placebo were identical in appearance for each drug, to ensure patient and investigator blinding" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described. Adverse events, participant experience, compliance and number of participants who dropped out prematurely reported (29/260 participants) |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Languillat 1988.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: none |
|
| Participants | Country: France Setting: hospital Number: 20 patients Age: 20 and 65 years Gender: 1 M:19 F Inclusion criteria: symptomatic CVI and oedema Exclusion criteria: previous venous sclerosis; surgery or elastic support; trophic disturbances; ulcers or permanent oedema; cardiac, renal, hepatic insufficiency or arterial disease; Raynaud's phenomenon; lymphoedema; pregnancy; venoactive drugs; any significant change in patient lifestyle or work |
|
| Interventions | Treatment: extract Ruscus aculeatus 450 mg plus hesperidin 450 mg plus ascorbic acid 300 mg per 12 hours Control: placebo Duration: 28 days Follow‐up: 42 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "This was a double‐blind placebo‐controlled trial with two groups of patients treated in parallel" Comment: no method of randomisation described |
| Allocation concealment (selection bias) | Unclear risk | Comment: no method of allocation concealment described |
| Blinding (patients) | Low risk | Quote: "The double‐blind nature of the trial was guaranteed by the strictly identical appearance of treatment units (capsules) as well as their packaging (bottles and bags of treatment kits)" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "The double‐blind nature of the trial was guaranteed by the strictly identical appearance of treatment units (capsules) as well as their packaging (bottles and bags of treatment kits)" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "The double‐blind nature of the trial was guaranteed by the strictly identical appearance of treatment units (capsules) as well as their packaging (bottles and bags of treatment kits)" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described, along with the most important baseline characteristics. No losses reported |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Laurent 1988.
| Methods | Study design: 2 randomised, double‐blind, placebo‐controlled studies analysed together Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: 5/200 (2.5%) |
|
| Participants | Country: France Setting: hospital Number: 200 patients Age: mean 49 (range 22 to 82) years Gender: 26 M:174 F Inclusion criteria: One study included patients with functional venous insufficiency (presence of symptoms but not signs); n = 83. The other study included patients with chronic organic venous insufficiency (varicose disease, post‐thrombotic syndrome); n = 117 Elastic stockings permitted Exclusion criteria: not exclusively venous symptoms (arterial, neurological or metabolic origin, disorders of static equilibrium); venotropic drugs in the past 3 months; pregnancy; prolonged immobilisation |
|
| Interventions | Treatment: diosmine 450 mg plus hesperidin 50 mg per 12 hours Control: placebo Duration: 60 days Follow‐up: 60 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Randomized trials were conducted versus placebo using appropriate statistical tests determined a priori" Comment: no methods of sequence generation specified |
| Allocation concealment (selection bias) | Unclear risk | Comment: no methods of allocation concealment described |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group provided, along with inclusion and exclusion criteria and characteristics of participants Number of participants who experienced adverse events presented, along with number who dropped out of the study. Losses 2.5% |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Lazzarini 1982.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: not stated Losses to follow‐up: not stated |
|
| Participants | Country: Italy Setting: hospital Number: 100 patients Age: 'adults' Gender: 23 M:74 F Inclusion criteria: stratification for participant groups: varicose legs, ulcer, thrombophlebitis, slight CVI Exclusion criteria: not stated |
|
| Interventions | Treatment: aminaftone 150 mg per day Control: placebo Duration: 60 days Follow‐up: 60 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The trial was conducted in 100 patients, informed consent and randomized into two groups of 50 and 50 and double‐blind treatment, the first with Capillarema and the second with placebo" Comment: method of randomisation not stated |
| Allocation concealment (selection bias) | Unclear risk | Comment: no method of allocation concealment described |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Unclear risk | Comment: number of participants in each group described, but important baseline characteristics lacking. In addition, number of participants who withdrew prematurely not described |
| Selective reporting | High risk | Comment: no information regarding adverse events provided |
MacLennan 1994.
| Methods | Study design: 2 independent, randomised, double‐blind, cross‐over, placebo‐controlled trials
Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: 16/104 (15%) |
|
| Participants | Country: UK Setting: hospital Number: 104 patients Age: ≥ 65 years Gender: 24 M:62 F Inclusion criteria: unilateral or bilateral symptoms and signs of CVI. Compression stockings allowed Exclusion criteria: bed‐bound or with cardiac or renal or hepatic disease or clinically important obesity; arterial insufficiency of the legs |
|
| Interventions | Treatment
Follow‐up: 180 days Participants who wore elastic support stockings had to continue to wear them throughout the study |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization was made according to a computer‐generated randomization list in blocks of 10" Comment: computer‐generated randomisation list generally accepted as an appropriate way to generate a random sequence of participants |
| Allocation concealment (selection bias) | Unclear risk | Comment: no method of allocation concealment stated |
| Blinding (patients) | Low risk | Quote: "Patients from each centre in the randomised control group were given placebo capsules identical in appearance" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "Patients from each centre in the randomised control group were given placebo capsules identical in appearance" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "Patients from each centre in the randomised control group were given placebo capsules identical in appearance" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: number of participants described, along with the most important characteristics, number of drop‐outs, adverse events and information on compliance |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Mann 1981.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: 5/28 (18%) |
|
| Participants | Country: UK Setting: outpatient Number: 28 patients Age: mean 69 years active treatment; mean 63 years placebo Gender: not stated Inclusion criteria: ≥ 1 venous ulcer Exclusion criteria: not stated |
|
| Interventions | Treatment: hidroxirutoside 1000 mg per day Control: placebo Duration: 90 days Follow‐up: 90 days Concomitant therapy: topical therapy and an "elastoweb" bandage |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: no information provided about the method used for randomisation |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information provided about the method used for allocation concealment |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | High risk | Comment: number of participants for each group described, but no information provided about participants lost to follow‐up or dropped out. Data were missing from the analysis and adverse events were not described. Losses were reported as 18% |
| Selective reporting | High risk | Comment: no protocol identified. Differences were noted between methods and results for the following outcomes: tiredness, heaviness, tender legs, distended veins, nights disturbed, daytime cramps |
Marinello 2002.
| Methods | Study design: randomised, multi‐centre, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: 21/123 (17%) |
|
| Participants | Country: Spain Setting: hospital Number: 143 patients Age: mean 52.87 (range 19 to 72) years Gender: 25 M:77 F Inclusion criteria: CVI stage CEAP III, IV and V Exclusion criteria: not stated |
|
| Interventions | Treatment: calcium dobesilate 1000 mg per day or calcium dobesilate 2000 mg per day Control: placebo Duration: 84 days Follow‐up: 84 days Elastic stockings permitted |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "In total 143 patients 123 were randomized (41 per treatment group)" Comment: no method of randomisation described |
| Allocation concealment (selection bias) | Unclear risk | Comment: no methods of allocation concealment described |
| Blinding (patients) | Low risk | Quote: "The placebo had the same characteristics which include active treatment. The oral administration was under the same conditions as the active treatment" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "The placebo had the same characteristics which include active treatment. The oral administration was under the same conditions as the active treatment" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "The placebo had the same characteristics which include active treatment. The oral administration was under the same conditions as the active treatment" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described, along with baseline characteristics. In addition, numbers and information provided about adverse events and participants who withdrew prematurely from the study |
| Selective reporting | Low risk | Comment: no published protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Martinez‐Zapata 2008.
| Methods | Study design: randomised, multi‐centre, double‐blind, placebo‐controlled Method of randomisation: computer‐generated random number table Exclusions post randomisation: none Losses to follow‐up: 131/509 (25.7%) |
|
| Participants | Country: Spain Setting: hospital Number: 509 patients Age: mean 53.3 ± 13.3 years treatment group; mean 54.7 ± 14.9 years placebo group Gender: 66 M:443 F Inclusion criteria: adults of either gender with CVD, CEAP clinical grades 1 to 6 and able to complete a QoL questionnaire Exclusion criteria: chronic or acute disease that limited compliance with the protocol, scheduled surgery or sclerotherapy in the coming calendar year, pregnant or lactating women, patients with allergies or known intolerance to the study medication, history of neutropoenia or leucopoenia, baseline serum leucocyte count < 3500/mL |
|
| Interventions | Treatment: 500 mg capsules of oral calcium dobesilate twice a day for 3 months Control: placebo: Inactive capsules of identical appearance and weight Duration: 90 days Follow‐up: 365 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The allocation to treatment was randomised, centralised and computer stratified in blocks of 10 patients, by clinical CEAP classification and centre" Comment: Computer‐stratified blocks ensure a random sequence |
| Allocation concealment (selection bias) | Low risk | Comment: treatment was allocated by researcher phoning the co‐ordinating centre |
| Blinding (patients) | Low risk | Quote: "to placebo (inactive capsules of identical appearance and weight) twice a day" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "to placebo (inactive capsules of identical appearance and weight) twice a day" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "to placebo (inactive capsules of identical appearance and weight) twice a day" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: number in each group was described, and those lost to follow‐up (25.7%) and participants who prematurely withdrew were described. Important characteristics were described, and inclusion and exclusion criteria were reported. ITT analysis was conducted, and imputation technique was described |
| Selective reporting | Low risk | Comment: protocol identified and no differences identified between protocol and article |
Nocker 1990.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: not stated Losses to follow‐up: not stated |
|
| Participants | Country: Germany Setting: university Number: 30 Age: 55 to 59 years Gender: menopausal females Inclusion criteria: stage II CVI with symptoms Exclusion criteria: venoactive drugs, anti‐inflammatories, corticosteroids or diuretics in the last 8 days before the start of the study; use of compression bandages or elastic stockings |
|
| Interventions | Treatment: oxirutoside 600 mg or 900 mg or 1200 mg or 1500 mg per day Control: placebo Duration: 90 days Follow‐up: 112 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomized to one of the five groups, receiving oral solutions of HR in small bottles containing 600, 900, 1200, 1500 mg HR or simply distilled water (controls) with six patients in each group" Comment: no methods described for randomising participants |
| Allocation concealment (selection bias) | Unclear risk | Comment: no methods for allocation concealment described |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Unclear risk | Comment: no data given about drop‐outs. Most important characteristics described with inclusion and exclusion criteria |
| Selective reporting | Low risk | Comment: no protocol identified, but no differences between outcomes reported in the methods section and those reported in the results section |
Padros 1972.
| Methods | Study design: randomised, double‐blind, cross‐over, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: not stated Losses to follow‐up: not stated |
|
| Participants | Country: Spain Setting: university Number: 30 females Age: 48 to 51 years Gender: female Inclusion criteria: CVI with signs (oedema, venous ectasia) and symptoms (heaviness, paraesthesias) Exclusion criteria: not stated |
|
| Interventions | Treatment: calcium dobesilate 250 mg tablet 3× per day Control: placebo tablet 3× per day Duration: 21 days Follow‐up: 28 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: no methods of random sequence generation described |
| Allocation concealment (selection bias) | Low risk | Comment: each bottle of treatment was identical and was numbered in a random way |
| Blinding (patients) | Low risk | Comment: each bottle of treatment was identical. Participants did not know the type of treatment administered |
| Blinding (study researchers) | Low risk | Comment: each bottle of treatment was identical. Researcher did not know the type of treatment administered |
| Blinding (outcome assessment) | Low risk | Comment: each bottle of treatment was identical. Assessor did not know the type of treatment administered |
| Incomplete outcome data | Unclear risk | Comment: no information on losses |
| Selective reporting | High risk | Comment: results before cross‐over not reported |
Parrado 1999.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: table of random numbers Exclusions post randomisation: none Losses to follow‐up: none |
|
| Participants | Country: Argentina Setting: hospital Number: 60 patients Age: 30 to 70 years Gender: 16 M:44 F Inclusion criteria: CVI, stages I to II of the Widmer classification (pigmentation, oedema, varicoses and symptoms) Exclusion criteria: elastic stockings; urgent surgical treatment or venous surgical treatment or sclerotherapy in previous 6 months; cardiac, renal or hepatic insufficiency; anti‐migraine drugs; analgesics; NSAIDs; diuretics or cardiovascular drugs; pregnant women or women who had given birth during previous 3 months |
|
| Interventions | Treatment: Ruscus aculeatus with hesperidin and vitamin C 300 mg per day Control: placebo Duration: 60 days Follow‐up: 60 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The study was double‐blind and patients were randomly allocated to be included in one of two parallel groups by using a table of random numbers" |
| Allocation concealment (selection bias) | Unclear risk | Comment: no methods of allocation concealment described |
| Blinding (patients) | Low risk | Quote: "Bottles, identical in form and presentation contained dobesilate calcium or placebo, according to a randomization code that was opened until the end of experiment" Comments: Identical presentation of intervention and control groups ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "Bottles, identical in form and presentation contained dobesilate calcium or placebo, according to a randomization code that was opened until the end of experiment"; "Neither the patient nor the medical staff did not know the nature of the substance administered, thereby satisfying the conditions of a double‐blind trial" Comments: Identical presentation of intervention and control groups ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "Bottles, identical in form and presentation contained dobesilate calcium or placebo, according to a randomization code that was opened until the end of experiment"; "Neither the patient nor the medical staff did not know the nature of the substance administered, thereby satisfying the conditions of a double‐blind trial" Comments: Identical presentation of intervention and control groups ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: no losses reported |
| Selective reporting | Low risk | Comment: no protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Pecchi 1990.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: use of alternation by order of arrival of each participant Exclusions post randomisation: none Losses to follow‐up: none |
|
| Participants | Country: Italy Setting: university Number: 40 patients Age: mean 48.2 ± 15.7 years Gender: 4 M:36 F Inclusion criteria: primary CVI and post‐thrombotic syndrome Exclusion criteria: postphlebitic syndrome; severe trophic lesions; no venous oedema; patients taking diuretics, corticosteroids or vasoactive drugs; elastic stockings or bandages |
|
| Interventions | Treatment: calcium dobesilate 1000 mg per day Control: placebo Duration: 30 days Follow‐up: 30 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients admitted to the study were randomly divided into two balanced groups treated respectively with calcium or placebo for one month..." Comment: no method of randomisation described |
| Allocation concealment (selection bias) | Unclear risk | Quote: "The allocation to individual patients of either type of treatment was performed according to the access sequence number of the patient" Comment: no method of allocation concealment described |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Low risk | Comment: numbers of participants in both groups described. No losses reported. No baseline characteristics of participants provided |
| Selective reporting | Low risk | Comment: no protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Pedersen 1992.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: not stated Losses to follow‐up: not stated |
|
| Participants | Country: Denmark Setting: not stated Number: 43 patients Age: 'adults' Gender: 8 M:41 F Inclusion criteria: symptoms of CVI and oedema Exclusion criteria: diuretic drugs; venotonic drugs; pregnant women |
|
| Interventions | Treatment: oxirutoside 900 mg per day Control: placebo Duration: 28 days Follow‐up: 28 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "If patients met the inclusion criteria, they were randomised using envelope method, double‐blind treatment with Venoruton 300 mg × 3 daily or placebo" Comment: method of randomisation not described |
| Allocation concealment (selection bias) | Low risk | Quote: "If patients met the inclusion criteria, they were randomised using envelope method, double‐blind treatment with Venoruton 300 mg × 3 daily or placebo" Comment: envelope methods generally accepted as a fair method for allocation concealment |
| Blinding (patients) | Unclear risk | Comment: no methods of blinding described |
| Blinding (study researchers) | Unclear risk | Comment: no methods of blinding described |
| Blinding (outcome assessment) | Unclear risk | Comment: no methods of blinding described |
| Incomplete outcome data | Unclear risk | Comment: number of participants in both groups described, along with the most important characteristics and inclusion and exclusion criteria. Number of participants who withdrew prematurely not described |
| Selective reporting | Low risk | Comment: no protocol identified, but no differences between outcomes reported in the methods section and those reported in the results section |
Petrassi 2000.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: computer‐elaborated simple randomisation table Exclusions post randomisation: none Losses to follow‐up: none |
|
| Participants | Country: Italy Setting: ambulatory Number: 20 patients Age: 47.7 (3.65) years active group; 36.7 (3.66) placebo group Gender: 3 M:19 F Inclusion criteria: CVI symptoms (heaviness and subcutaneous swelling) and venous pressure > 40 mmHg Exclusion criteria: cardiovascular drugs, diuretic drugs and analgesic or anti‐inflammatory compounds |
|
| Interventions | Treatment: french bark pine extract capsules 100 mg 3× per day Control: placebo Duration: 60 days Follow‐up: 60 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "They were treated with placebo or Pycnogenol 100mg × 3/day for 2 months according to a computer elaborated simple randomization table" Comment: computerised randomisation table generally accepted as a proper way to randomise participants |
| Allocation concealment (selection bias) | Unclear risk | Comment: no method described for allocation concealment |
| Blinding (patients) | Low risk | Quote: "The drugs were prepared in white opaque capsules in order to make the slightly pinkish‐coloured Pycnogenol® indistinct from placebo (lactose)" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "The drugs were prepared in white opaque capsules in order to make the slightly pinkish‐coloured Pycnogenol® indistinct from placebo (lactose)" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "The drugs were prepared in white opaque capsules in order to make the slightly pinkish‐coloured Pycnogenol® indistinct from placebo (lactose)" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: number of participants was described in each group, along with the most important characteristics of participants, including inclusion and exclusion criteria. In addition, information was given about drop‐outs and adverse events |
| Selective reporting | Low risk | Comment: no protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Planchon 1990.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: 6/110 (5%) |
|
| Participants | Country: France Setting: hospital Number: 110 participants Age: mean 50 (range 22 to 79) years Gender: 18 M:92 F Inclusion criteria: symptoms of functional and organic (post‐thrombotic syndrome and varices) CVI Exclusion criteria: venous thrombosis; long‐term immobilisation; hepatic, renal and cardiac oedema; neurological, arterial and metabolic symptoms |
|
| Interventions | Treatment: diosmine 450 mg plus hesperidin 50 mg × 2 capsules per day Control: placebo Duration: 60 days Follow‐up: 60 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The award of the therapeutic group membership made by draw lots was ignored until the complete end of the study by both the clinician and the patients" Comment: drawn seems a method of randomisation |
| Allocation concealment (selection bias) | Unclear risk | Comment: no methods of allocation concealment stated |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described, as well as the inclusion and exclusion criteria and the most important characteristics. Numbers of participants who withdrew prematurely were described, including reasons for dropping out, information about compliance and adverse events |
| Selective reporting | Low risk | Comment: no protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Pointel 1986.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: 4 (4%) |
|
| Participants | Country: France Setting: hospital Number: 94 patients Age: mean 49 ± 12 years Gender: 8 M:86 F Inclusion criteria: CVI Exclusion criteria: severe varicose veins requiring an elastic strip, postphlebitic patients, those with unilateral venous insufficiency, those treated with a venoactive drug before the start of the study |
|
| Interventions | Treatment: Centella asiatica (TECA) 120 mg: two 30‐mg capsules twice a day vs Centella asiatica (TECA) 60 mg: one 30‐mg capsule twice a day Control: placebo Duration: 56 days Follow‐up: 56 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The study conducted in four hospitals according to a controlled, randomized, double‐blind (double dummy) study performed on three parallel groups for eight weeks" Comment: no method of randomisation described |
| Allocation concealment (selection bias) | Unclear risk | Comment: no methods of allocation concealment described |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described, along with inclusion and exclusion criteria and important characteristics for participants. In addition, study author reported the number of adverse events that occurred, the number of participants who withdrew prematurely and reasons for dropping out |
| Selective reporting | Low risk | Comment: no protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Prerovsky 1972.
| Methods | Study design: 2 independent, randomised, double‐blind, cross‐over, placebo‐controlled trials
Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: none |
|
| Participants | Country: Czechoslovakia Setting: research centre Number: 50 patients Age: 'adults' Gender: not stated Inclusion criteria: signs (oedema, pigmentation, post‐thrombotic syndrome) and symptoms of CVI Exclusion criteria: not stated |
|
| Interventions | Treatment: oxirutoside 1200 mg per day Control: placebo Duration: 126 days Follow‐up: 126 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "... after the administration of 3 capsules of HR (900 mg) or 3 capsules of placebo in a double blind cross‐over trial in a randomized‐order" Comment: method of randomisation not described |
| Allocation concealment (selection bias) | Unclear risk | Comment: no method of allocation concealment described |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Low risk | Comment: number of participants described in each group, along with the most important characteristics. However, inclusion and exclusion criteria were, apart from clinical features, not well described. Adverse events and drop‐outs were well described |
| Selective reporting | Low risk | Comment: no protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Pulvertaft 1983.
| Methods | Study design: randomised, multi‐centre, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: not stated Losses to follow‐up: 64/660 (10%) |
|
| Participants | Country: UK Setting: general practice Number: 660 patients Age: 54 years Gender: 220 M:440 F Inclusion criteria: symptomatic CVI Exclusion criteria: not stated |
|
| Interventions | Treatment: oxirutoside 1000 mg per day Control: placebo Duration: 28 days Follow‐up: 28 days Participants who wore elastic support had to continue to wear it throughout the study |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Four patients would receive active treatment with Paroven and one would be randomly and blindly treated with placebo" Comment: no method of randomisation described |
| Allocation concealment (selection bias) | Unclear risk | Comment: no method of allocation concealment described |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described, and a table includes the most important characteristics of participants and inclusion and exclusion criteria. In addition, number of participants excluded after randomisation reported |
| Selective reporting | Low risk | Comment: no protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Rabe 2011.
| Methods | Study design: randomised, multi‐centre, double‐blind, placebo‐controlled Method of randomisation: table of random numbers Exclusions post randomisation: 22 (8%) Losses to follow‐up: 32/256 (12.5%) |
|
| Participants | Countries: Germany and Switzerland Setting: not stated Number: 256 patients Age: mean 53.2 ± 11.5 years treatment group; mean 53.5 ± 12.1 years placebo group Gender: 38 M:218 F Inclusion criteria: pitting oedema due to CVI (C3‐C5 according to CEAP classification) and ≥ 1 of the symptoms such as discomfort and pain Exclusion criteria: disease that imitates symptoms of CVI, cardiac insufficiency, ulceration of the lower leg, diabetes mellitus, hypertension, lymphoedema, sclerotherapy during the past 6 months, lipoedema, obesity (BMI > 30 kg/m2), disease of the gastrointestinal tract; female patients who were pregnant, lactating or of childbearing potential and not protected from pregnancy by a sufficiently reliable method; malignant disease |
|
| Interventions | Treatment: calcium dobesilate 1500 mg per day Control: matching placebo Duration: 56 days Follow‐up post treatment: 70 days Elastic stockings permitted |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomization with blocks of four was used. The randomization list was produced by an independent person" Comment: Randomisation list ensures a random sequence |
| Allocation concealment (selection bias) | Low risk | Quote: "The study medication was packed in identical boxes marked with a randomization number each newly randomized patient was given the medication with the lowest randomization number available" Comment: Identical boxes with randomisation provision ensureproper allocation concealment |
| Blinding (patients) | Low risk | Quote: ".... or a matching placebo ... The study medication was packed in identical boxes..." Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "The study medication was packed in identical boxes marked with a randomization number each newly randomized patient was given the medication with the lowest randomization number available" ; ".... or a matching placebo ... The study medication was packed in identical boxes..." Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: ".... or a matching placebo ... The study medication was packed in identical boxes..." Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: number in each group described, as were loss to follow‐up and participants who prematurely withdrew. Important characteristics and inclusion and exclusion criteria reported. ITT analysis conducted, but no methods used for imputation of missing values described |
| Selective reporting | Low risk | Comment: no protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Renton 1994.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: 9/40 (22.5%) |
|
| Participants | Country: UK Setting: ambulatory Number: 40 patients Age: 'adults' Gender: not stated Inclusion criteria: ankle oedema due to mild to moderate venous hypertension Exclusion criteria: peripheral arterial disease, diabetes or normal Doppler ultrasound |
|
| Interventions | Treatment: hidroxirutoside 500 mg × 2 capsules twice a day Control: placebo Duration: 30 days Follow‐up: 30 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "After the final examination, the patients were randomised to receive either...." Comment: no method of randomisation described |
| Allocation concealment (selection bias) | Unclear risk | Comment: no methods of allocation concealment described |
| Blinding (patients) | Low risk | Quote: "The patients were randomised to receive either 2 tablets of 500mg HR twice daily or a placebo of identical appearance" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "The patients were randomised to receive either 2 tablets of 500mg HR twice daily or a placebo of identical appearance" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "The patients were randomised to receive either 2 tablets of 500mg HR twice daily or a placebo of identical appearance" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described, along with information about the most important characteristics and inclusion and exclusion criteria. In addition, study author described the number of participants who experienced adverse events and the number who withdrew prematurely from the study, including reasons for dropping out |
| Selective reporting | Low risk | Comment: no protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Rose 1970.
| Methods | Study design: randomised, double‐blind, cross‐over, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: not stated Losses to follow‐up: 39% (13/33) |
|
| Participants | Country: UK Setting: hospital Number: 33 patients Age: not stated Gender: not stated Inclusion criteria: CVI associate with varicose disorders or postphlebitic syndrome Exclusion criteria: not stated |
|
| Interventions | Treatment: hidroxirutoside 1200 mg per day Control: placebo Duration: 180 days Follow‐up: 270 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: no methods of random sequence generation described |
| Allocation concealment (selection bias) | Low risk | Quote: "The active and the placebo material were numbered in randomised order" Comment: Randomised order prevented knowledge of treatment in advance |
| Blinding (patients) | Low risk | Quote: "The key to the active and placebo capsules was not broken until January of this year, when all the patients had completed treatment for over 6 months" |
| Blinding (study researchers) | Low risk | Quote: "The key to the active and placebo capsules was not broken until January of this year, when all the patients had completed treatment for over 6 months" |
| Blinding (outcome assessment) | Low risk | Quote: "The key to the active and placebo capsules was not broken until January of this year, when all the patients had completed treatment for over 6 months" |
| Incomplete outcome data | High risk | Comment: 39% (13/33) losses; imbalance between groups at the end of follow‐up (17 participants received hidroxirutoside; 8 received placebo) |
| Selective reporting | High risk | Comment: results by symptom before the cross‐over not reported |
Rudofsky 1989.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: randomisation stratified by centre Exclusions post randomisation: none Losses to follow‐up: 10/151 (7%) |
|
| Participants | Country: Germany Setting: hospital Number: 151 patients Age: mean 49.7 (range 21 to 73) years Gender: not stated Inclusion criteria: stage I and II CVI, primary varicosis and post‐thrombotic symptoms Exclusion criteria: morning oedema (stage I to II CVI); acute thrombosis; leg ulcer; other peripheral arterial occlusive disorders; heart failure; severe cardiac arrhythmia; severe hypertension; diuretics; dihydroergotamine products; pregnancy |
|
| Interventions | Treatment: ruscus extract plus hesperidinmethylchalcone × 2 capsules 3 times per day for 4 weeks, then 2 capsules twice per day for 8 weeks Control: placebo Duration: 56 days Follow‐up: 56 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Following randomisation, stratified by centre, the patients then received daily 3x2 capsules of identical appearance, containing either active drug or placebo" Comment: no method of randomisation described |
| Allocation concealment (selection bias) | Unclear risk | Comment: no method of allocation concealment described |
| Blinding (patients) | Low risk | Quote: "Following randomisation, stratified by centre, the patients then received daily 3×2 capsules of identical appearance, containing either active drug or placebo" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "Following randomisation, stratified by centre, the patients then received daily 3×2 capsules of identical appearance, containing either active drug or placebo" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "Following randomisation, stratified by centre, the patients then received daily 3x2 capsules of identical appearance, containing either active drug or placebo" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described, along with important characteristics and inclusion and exclusion criteria. Number of patients who withdrew prematurely described, but no information on the reasons why participants dropped out |
| Selective reporting | Low risk | Comment: no protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Schultz‐Ehrenburg 1993.
| Methods | Study design: 2 prospective, multi‐centre, randomised, double‐blind, placebo‐controlled trials Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: 7/55 (13%) |
|
| Participants | Country: France Setting: outpatient Number: 55 patients Age: 'adults' Gender: not stated Inclusion criteria: unilateral venous leg ulcers and chronic venous insufficiency (deep or superficial) Exclusion criteria: not stated |
|
| Interventions | Treatment
Control: placebo Duration: 84 days Follow‐up: 84 days All participants received pressure bandaging |
|
| Outcomes | Primary
Secondary
|
|
| Notes | Data extraction possible only in trial A | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Two prospective, multicentre, double‐blind, randomized, parallel, placebo‐controlled trial" Comment: no method of randomisation stated |
| Allocation concealment (selection bias) | Unclear risk | Comment: no method of allocation concealment stated |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described, along with number of losses, but not reasons |
| Selective reporting | Low risk | Comment: no protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Sentou 1984.
| Methods | Study design: randomised, double‐blind, placebo‐controlled trial Method of randomisation: not stated Exclusions post randomisation: not stated Losses to follow‐up: 1 participant |
|
| Participants | Country: France Setting: ambulatory Number: not stated Age: 34.6 ± 9.18 years active product; 38.2 ± 12.44 years placebo Gender: female Inclusion criteria: slight or moderate varicose disease Exclusion criteria: surgical indication or trophic disorders, other vasoactive drugs |
|
| Interventions | Treatment: extract Ruscus aculeatus 450 mg plus hesperidin 450 mg plus ascorbic acid 300 mg per day (Cyclo 3: 3 capsules twice per day) Control: placebo Duration: 28 days Follow‐up: 20 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | Number of included participants not specified | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The allocation of the subjects to the Cyclo 3 and placebo groups was done at random, in a blind manner, according to the order of admission in the study" Comment: no method of randomisation described |
| Allocation concealment (selection bias) | Unclear risk | Comment: no method of allocation concealment described |
| Blinding (patients) | Low risk | Quote: "Cyclo 3® and the placebo had an identical appearance" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "Cyclo 3® and the placebo had an identical appearance" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "Cyclo 3® and the placebo had an identical appearance" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | High risk | Comment: number of included participants not specified. Only 1 participant did not accomplish the study protocol |
| Selective reporting | Low risk | Comment: no protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Serralde 1990.
| Methods | Study design: randomised, double‐blind, placebo‐controlled trial Method of randomisation: not stated Exclusions post randomisation: not losses Losses to follow‐up: none |
|
| Participants | Country: Mexico Setting: hospital Number: 52 patients Age: 42.4 ± 11.6 years active treatment; 42.3 ± 8.4 years placebo Gender: 11 M:41 F Inclusion criteria: CVI and oedema Exclusion criteria: venoactive drugs, diuretics, anti‐inflammatories and steroid drugs; elastic stockings or bandages; other causes of oedema; superficial thrombophlebitis; venous ulcer; venous surgery; pregnant women |
|
| Interventions | Treatment: oxirutosides 1000 mg per day Control: placebo Duration: 28 days Follow‐up: 56 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The trial was double‐blind, randomized, placebo‐controlled dose of one tablet of 500 mg twice daily HR or identical placebo" Comment: method of randomisation unclear |
| Allocation concealment (selection bias) | Unclear risk | Comment: method of allocation concealment unclear |
| Blinding (patients) | Low risk | Quote: "The trial was double‐blind, randomized, placebo‐controlled dose of one tablet of 500 mg twice daily HR or identical placebo" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "The trial was double‐blind, randomized, placebo‐controlled dose of one tablet of 500 mg twice daily HR or identical placebo" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "The trial was double‐blind, randomized, placebo‐controlled dose of one tablet of 500 mg twice daily HR or identical placebo" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in both groups described, along with inclusion and exclusion criteria and the most important characteristics. Adverse events presented. No losses |
| Selective reporting | Low risk | Comment: no protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Thebaut 1985.
| Methods | Study design: randomised, double‐blind, placebo‐controlled trial Method of randomisation: throwing dice Exclusions post randomisation: not stated Losses to follow‐up: 14/92 (15%) |
|
| Participants | Country: France Setting: ambulatory Number: 92 patients Age: 38.9 ± 10.1 years active treatment; 40.7 ± 11.4 years placebo Gender: 8 M:63 F Inclusion criteria: CVI with leg heaviness or paraesthesias (16 to 65 years old) Exclusion criteria: venoactive drugs, elastic stockings or bandages; deep venous insufficiency by echo Doppler, venous complications, postphlebitic syndrome |
|
| Interventions | Treatment: grape seed extract tablets 300 mg every 8 hours Control: placebo Duration: 28 days Follow‐up: 28 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The method chosen was that of a controlled trial conducted a double‐blind placebo‐controlled with throwing dice assigned treatment" Comment: Throwing dice method seems to be a fair method for generating a random sequence |
| Allocation concealment (selection bias) | Unclear risk | Comment: no information about allocation concealment provided |
| Blinding (patients) | Low risk | Quote: "Two parallel groups were thus formed, the E group received 300mg per day of Endolelon three times daily, P group receiving placebo ‐ in all respects identical to the active pills ‐ and using the same frequency" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "Two parallel groups were thus formed, the E group received 300mg per day of Endolelon three times daily, P group receiving placebo ‐ in all respects identical to the active pills ‐ and using the same frequency" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "Two parallel groups were thus formed, the E group received 300mg per day of Endolelon three times daily, P group receiving placebo ‐ in all respects identical to the active pills ‐ and using the same frequency" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Unclear risk | Comment: number of participants in each group described, along with inclusion and exclusion criteria and the most important characteristics. Information about participants who withdrew prematurely described. In addition, standard deviation lacking in the results |
| Selective reporting | Low risk | Comment: no protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Tsouderos 1989.
| Methods | Study design: randomised, double‐blind, placebo‐controlled trial Method of randomisation: not stated Exclusions post randomisation: not stated Losses to follow‐up: 4 participants |
|
| Participants | Country: France Setting: hospital Number: 40 patients Age: 'adults' Gender: not stated Inclusion criteria: functional CVI Exclusion criteria: not stated |
|
| Interventions | Treatment: diosmine 450 mg plus hesperidin 50 mg per 12 hours Control: placebo Duration: 60 days Follow‐up: 60 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | This publication describes 3 clinical trials. Only 1 is included here. The others are phase 2 clinical trials | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "All the studies were conducted double blind, according to the methodology of controlled trials" Comment: no method of randomisation described |
| Allocation concealment (selection bias) | Unclear risk | Comment: no method of allocation concealment described |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Low risk | Comment: 2 participants lost in each group, but reasons not explained |
| Selective reporting | Low risk | Comment: no protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Unkauf 1996.
| Methods | Study design: randomised, double‐blind, parallel, placebo‐controlled trial Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: 23/133 (17%) |
|
| Participants | Country: Germany Setting: outpatients Number: 133 patients Age: mean 58.9 ± 8.6 years active group; mean 60.6 ± 10.0 years placebo group Gender: 133 F Inclusion criteria: CVI grade II (according to Widmer) Exclusion criteria: premenstrual syndrome oedema; acute phlebitis or thrombosis; cardiac insufficiency or peripheral arterial disease; other venotonic drugs, laxatives, theophylline, diuretics, cardiac glycosides, angiotensin‐converting enzyme or calcium antagonist within preceding 8 days; changes in postmenopausal hormone therapy within preceding 2 months |
|
| Interventions | Treatment: oxerutins 1000 mg per day Control: placebo Duration: 90 days Follow‐up: 90 days All participants received standard compression stockings |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The study had a double‐blind, randomised, multi‐centered, paralel‐group design with two treatment groups" Comment: no method of randomisation described |
| Allocation concealment (selection bias) | Unclear risk | Comment: no method of allocation concealment described |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described, along with the most important characteristics and inclusion and exclusion criteria. ITT analysis conducted. Information about adverse events, exclusion after randomisation and loss to follow‐up given |
| Selective reporting | Low risk | Comment: no protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Vanscheidt 2002a.
| Methods | Study design: randomised, double‐blind, placebo‐controlled trial Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: 52/231 (22.5%) |
|
| Participants | Country: Germany Setting: university Number: 231 patients Age: mean 55.1 (range 23 to 78) years Gender: 48 M:183 F Inclusion criteria: stages 3 to 5 of CEAP Exclusion criteria: surgical treatment of CVI; heart insufficiency; arterial occlusive disease; diabetes mellitus; neuropathy; acute thrombosis; lymphoedema; renal insufficiency or impaired liver function; malignant disease; pregnancy or breast feeding; major surgery; drugs with influence on the veins |
|
| Interventions | Treatment: SB‐LOT (15 mg coumarin and 90 mg troxerutin) 2 tablets 3× per day for 16 weeks Control: placebo Duration: 112 days Follow‐up: 112 days All participants received standard compression stockings during first 4 weeks |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomisation schedule was generated by the validated PC programme RanCode plus, independently to all study participants. It was based on blocks of 4 patients. All medication was pre‐numbered and distributed to the centres" Comment: computer‐generated table of random numbers ensures a random sequence of participants |
| Allocation concealment (selection bias) | Low risk | Quote: "Patients were included in the study by receiving the next consecutive random number. For each patient the study centres were supplied sealed envelopes with the treatment group information" Comment: sealed envelopes and allocation of participants by giving the next consecutive random number ensure fair allocation concealment |
| Blinding (patients) | Low risk | Quote: "Placebo tablets matched the active tablets in taste, smell and appearance" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "Placebo tablets matched the active tablets in taste, smell and appearance" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "Placebo tablets matched the active tablets in taste, smell and appearance" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described, along with the most important characteristics and inclusion and exclusion criteria. In addition, study author stated the number of participants who withdrew from the study prematurely or were excluded after randomisation (22.5%). ITT analysis conducted |
| Selective reporting | Low risk | Comment: no protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Vanscheidt 2002b.
| Methods | Study design: randomised, double‐blind, placebo‐controlled trial Method of randomisation: computer‐generated random number table Exclusions post randomisation: not stated Losses to follow‐up: 56/167 (34%) |
|
| Participants | Country: Germany Setting: university Number: 167 patients Age: mean 53.2 ± 13.3 years active group; mean 53 ± 10.9 years placebo group Gender: 166 F Inclusion criteria: stages I and II of Widmer or CEAP 3 to 4 Exclusion criteria: other diseases with oedema, compression therapy for the past 6 months before the study; support stockings; patients more than 30% overweight; any concomitant medication that may interfere with study treatment |
|
| Interventions | Treatment: Ruscus aculeatus 72 to 75 mg per day Control: placebo Duration: 90 days Follow‐up: 90 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The study was designed as a multi‐center, double‐blind, randomized, placebo‐controlled trial with women suffering from chronic venous insufficiency..." Comment: no method of randomisation described |
| Allocation concealment (selection bias) | Unclear risk | Comment: no method of allocation concealment described |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | High risk | Comment: number of participants in each group described, along with important characteristics and inclusion and exclusion criteria. In addition, number of participants who withdrew prematurely described, but percentage was important (34%) and no ITT analysis performed |
| Selective reporting | Low risk | Comment: no protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Vin 1994.
| Methods | Study design: multi‐centre, randomised, double‐blind, placebo‐controlled with a placebo run‐in period Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: 4/73 (4%) |
|
| Participants | Country: France Setting: hospital Number: 73 patients Age: mean 55.7 ± 15.8 years active treatment; mean 53.6 ± 16.7 years placebo Gender: 10 M:59 F Inclusion criteria: presence of truncal varicose veins with ostial reflux and subjective symptoms of venous origin Exclusion criteria: occlusive arterial disease; osteoarticular disease; diabetes; acute or chronic inflammatory syndromes; haematological diseases; venoactive drugs; pregnancy; smoking |
|
| Interventions | Treatment: troxerutin 3500 mg per day Control: placebo Duration: 60 days Follow‐up: 60 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The study was controlled, double‐blind, randomized, multicentre and with a placebo run‐in period" Comment: no method of randomisation stated |
| Allocation concealment (selection bias) | Unclear risk | Comment: no method of allocation concealment described |
| Blinding (patients) | Low risk | Quote: "They were then randomly allocated to receive either troxerutin, 3500 mg to be taken in the morning for 2 months, or a placebo with identical appearance and taste" Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "They were then randomly allocated to receive either troxerutin, 3500 mg to be taken in the morning for 2 months, or a placebo with identical appearance and taste" Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "They were then randomly allocated to receive either troxerutin, 3500 mg to be taken in the morning for 2 months, or a placebo with identical appearance and taste" Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described, along with the most important characteristics and inclusion and exclusion criteria. In addition, information about participants who withdrew prematurely given, including reasons for dropping out. Adverse events given as well |
| Selective reporting | Low risk | Comment: no protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Welch 1985.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: not stated Exclusions post randomisation: none Losses to follow‐up: 7/147 (5%) |
|
| Participants | Country: Belgium Setting: hospital Number: 147 patients Age: mean 44.5 ± 14 years active group; mean 43.6 ± 14 years placebo group Gender: 26 M:119 F Inclusion criteria: CVI with oedema and ≥ 1 related symptom Exclusion criteria: elastic stockings or compressive bandages; leg oedema from another origin; arterial insufficiency; superficial thrombophlebitis; varicose eczema or ulcer; diuretics, analgesics, steroids, NSAIDs or other venous drugs; pregnancy |
|
| Interventions | Treatment: O‐(beta‐hydroxyethyl)‐rutoside 1000 mg per day Control: placebo Duration: 28 days Follow‐up: 28 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: method of randomisation not given |
| Allocation concealment (selection bias) | Unclear risk | Comment: method of allocation concealment not given |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described, and inclusion and exclusion criteria reported as well for the most important characteristics. Number of participants who dropped out prematurely given, along with numbers of and reasons for adverse events |
| Selective reporting | Low risk | Comment: protocol identified and no differences identified between protocol and article |
Widmer 1990.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: randomisation list prepared by statistician Exclusions post randomisation: none Losses to follow‐up: 17/225 (7%) |
|
| Participants | Country: Switzerland Setting: hospital Number: 225 patients Age: 20 to 70 years Gender: 27 M:181 F Inclusion criteria: CVI grade I to II (alterations in pigmentation, with or without subcutaneous veins, oedema and symptoms of the disease) Exclusion criteria: CVI grade III with open or healed varicose ulcer; venous surgery during past 12 months or sclerotherapy during past 6 months; symptomatic peripheral arterial occlusion; renal or cardiac insufficiency; lymphoedema; diabetes; hypertension; overweight; pregnancy; compression therapy or drugs that might interfere with clinical results (diuretics); intolerance to the active drug of the study |
|
| Interventions | Treatment: calcium dobesilate 1500 mg per day Control: placebo Duration: 28 days Follow‐up: 28 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The patients were treated for 28 days with either Doxium or placebo at the dosage of 3 capsules daily, according to a randomization list prepared by the statistician" Comment: randomisation list assumed to be a fair method of assuring a random sequence |
| Allocation concealment (selection bias) | Unclear risk | Comment: no methods described for allocation concealment |
| Blinding (patients) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (study researchers) | Unclear risk | Comment: no information given about methods used for blinding |
| Blinding (outcome assessment) | Unclear risk | Comment: no information given about methods used for blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described, including most important characteristics and inclusion and exclusion criteria. In addition, reasons for excluding participants after randomisation given, along with number of participants. Number compliant with medication provided, along with adverse events |
| Selective reporting | Low risk | Comment: no protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
Zucarelli 1987.
| Methods | Study design: randomised, double‐blind, placebo‐controlled Method of randomisation: throwing dice Exclusions post randomisation: none Losses to follow‐up: 25/149 (16%) |
|
| Participants | Country: France Setting: outpatients Number: 149 patients Age: mean 33 ± 9.4 years active treatment; mean 32 ± 8 years placebo Gender: 149 F Inclusion criteria: CVI stage I (functional symptoms and oedema) Participants allowed to wear elastic support Exclusion criteria: chronic venous with trophic alterations; varices; phlebitis; postphlebitic syndrome; lymphoedema; arteriopathy; pregnancy; other phlebotonics; anti‐inflammatories; diuretics; anti‐platelet or vasculo‐protector treatments |
|
| Interventions | Treatment: coumarin 10.5 mg per day plus troxerutin 1050 mg per day Control: placebo Duration: 90 days Follow‐up: 90 days |
|
| Outcomes | Primary
Secondary
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The methodology used was that of a controlled trial against placebo in double‐blind perspective with the drawing of lots to constitute two parallel groups" Comment: Drawing of lots seems like a fair method of generating an adequate sequence |
| Allocation concealment (selection bias) | Unclear risk | Comment: no methods of allocation concealment described |
| Blinding (patients) | Low risk | Quote: "Ampules of placebo, which are in all respects comparable to those of the active..." Comment: Identical placebo ensures double‐blinding |
| Blinding (study researchers) | Low risk | Quote: "Ampules of placebo, which are in all respects comparable to those of the active..." Comment: Identical placebo ensures double‐blinding |
| Blinding (outcome assessment) | Low risk | Quote: "Ampules of placebo, which are in all respects comparable to those of the active..." Comment: Identical placebo ensures double‐blinding |
| Incomplete outcome data | Low risk | Comment: number of participants in each group described, along with inclusion and exclusion criteria and the most important characteristics. In addition, tolerance, adverse events and participants who dropped out prematurely described |
| Selective reporting | Low risk | Comment: no protocol identified, and no differences between outcomes reported in the methods section and those reported in the results section |
CEAP classification (clinical signs (C), aetiology (E), anatomical distribution (A) and physiological conditions (P) of CVI) CIVIQ: Chronic Venous Insufficiency International Questionnaire CT: clinical trial CVD: cardiovascular disease CVI: chronic venous insufficiency EuroQoL: Descriptive system of health‐related quality of life states FLQA: Freiburg Life Quality Assessment h: hour ITT: intention‐to‐treat LRR: light reflection rheography NSAIDs: non‐steroidal anti‐inflammatories QoL: quality of life tid: 3 times a day VAS: visual analogue scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Akbulut 2010 | This study assessed the combination of calcium dobesilate and oxerutin |
| Allaert 1992 | This study assessed efficacy of drugs for CVI aggravated by oral contraceptives |
| Amato 1994 | Micronised flavonoid and non‐micronised diosmine were compared |
| Androulakis 1989 | Principal outcome consists of plethysmographic parameters ‐ a surrogate outcome |
| Auteri 1990 | No clinical endpoints were assessed |
| Avram 1996 | Two flavonoids were compared, and no placebo group was included |
| Bacci 2003 | This study assessed a combination of different active products |
| Bastide 1976 | This study assessed dihydroergotamine, which is not included in our review |
| Batchvarova 1989 | This is not a randomised study |
| Batchvarova 1989a | This study assesses a product with escin, which is not included in our review |
| Behar 1993 | This study assesses a product with escin, which is not included in our review |
| Belcaro 1986 | This study compared a rutoside with or without elastic compression and included no placebo group |
| Belcaro 1989 | This was a single‐blind study |
| Belcaro 1995 | Outcomes studied were surrogates (laser Doppler and transcutaneous oximetry) |
| Belcaro 2002 | Venoruton was compared with Daflon |
| Belcaro 2003 | Prophylaxis with Venoruton was provided for flight oedema in normal participants |
| Belcaro 2008 | No clinical endpoints were assessed ‐ only microcirculatory parameters |
| Belcaro 2008b | This controlled clinical trial assessed O‐(β‐Hydroxyethyl)‐rutosides, but the study was not randomised |
| Bello 1990 | Calcium dobesilate was combined with a heparinoid |
| Beltramino 1999 | Two different drugs (Cyclo 3 Fort vs hydroxyethilrutoside) were compared for CVI |
| Bento 2006 | This study assessed a combination of different active products that contain escin |
| Berson 1976 | Comparative group was given a heparinoid rather than placebo |
| Berson 1978 | Two clinical trials are described. One was a non‐controlled clinical trial, and in the other, the control group was given naftazone |
| Berson 1980 | Two different drugs given for CVI were compared |
| Blume 1996 | Inadequate blinding: Initial phase of the trial used 'placebo' that was actually a low concentration of the assessed active drug: coumarin 2 mg and rutoside 100 mg |
| Boccalon 1989 | The purpose of this study was to check effects of active treatment after microcirculatory disturbances caused by heat |
| Bohm 1989 | This study assessed the combination of a diuretic and a drug for CVI |
| Boisseau 1995 | Outcomes were not applicable to this review: Biological parameters were measured (erythrocyte aggregation and fibrinolytic activity) |
| Bolliger 1972 | This study assessed the combination of dimethyl sulfoxide and diphenyl butazone with a rutoside |
| Bort 1995 | No clinical endpoints were assessed ‐ only microcirculatory parameters |
| Bosse 1985 | This study compared 2 drugs (Venalot ‐ combination of coumarin and troxerutin ‐ and Benzarone) for CVI |
| Brami 1983 | This study assessed the efficacy of a combination of dyhigroergocriptine mesilate and caffeine for CVI |
| Brock 1991 | No placebo was given to the control group |
| Brock 2001 | No placebo was given to the control group |
| Carstens 1985 | This study assessed the combination of a diuretic and escin (DIU Venostatin) |
| Cataldi 2001 | The drug studied was a combination of several active principles, one of which was rutin |
| Cesarone 1992 | No clinical endpoints were assessed ‐ only microcirculatory parameters |
| Cesarone 1994 | No clinical endpoints were assessed ‐ only microcirculatory parameters |
| Cesarone 2001 | No clinical endpoints were assessed ‐ only microcirculatory parameters |
| Cesarone 2001a | This was a single‐blind study |
| Cesarone 2001b | This study assessed escin in diabetic microangiopathy |
| Cesarone 2001c | The study was about microvascular parameters: PO2, PCO2 and volume parameters. This was a single‐blind study |
| Cesarone 2001d | This study assessed Centella asiatica for flight microangiopathy |
| Cesarone 2001e | This study assessed Centella asiatica for diabetic microangiopathy |
| Cesarone 2002a | This study assessed hydroxyrutosides for flight microangiopathy |
| Cesarone 2002b | This study assessed variations in plasma free radicals in participants with CVI |
| Cesarone 2003 | This study assessed Venoruton for prophylaxis of flight oedema |
| Cesarone 2005 | This study compared 2 drugs for CVI (beta‐hydroxirutoside and diosmine plus hesperidin) |
| Cesarone 2006 | This study was not double‐blinded |
| Cesarone 2006a | This study compared 2 drugs for CVI (Venoruton and Daflon) |
| Cesarone 2006b | This study compared 2 drugs for CVI (Pycnogenol and Daflon) |
| Cesarone 2006c | This controlled clinical trial was not randomised; it focused on endothelial cells |
| Cesarone 2006d | This study assessed french maritime pine bark for diabetic microangiopathy |
| Cesarone 2010 | This study was not double‐blinded |
| Chant 1973 | Non‐clinical criteria were given |
| Chiummariello 2009 | The drug evaluated is a combination of different products for CVI. This study was not double‐blinded |
| Clemens 1986 | Only haemodynamic venous parameters were assessed by light reflection rheography |
| Cospite 1989 | This study compared 5682 SE (combination of micronised diosmine and hesperidin) vs diosmine |
| Cospite 1996 | This study compared heparan sulphate vs diosmine for CVI |
| Cospite 1998 | This study compared micronised diosmine and hesperidin vs diosmine |
| De Anna 1989 | This was a single‐blind study |
| de Parades 1990 | This study compared Cyclo 3 Fort vs diosmine plus hesperidin for CVI |
| De Sanctis 2001 | This was a single‐blind study |
| Delacroix 1981 | The drug evaluated was escin, which has been excluded from our review |
| Delecluse 1991 | This study compared Diovenor versus a combination of flavonoids |
| Duchene 1988 | Only haemodynamic venous parameters were assessed by plethysmography |
| Dustmann 1984 | The drug evaluated was escin, which has been excluded from our review |
| Erdlen 1989 | Venostasin contains escin, which has been excluded from our review |
| Erler 1991 | This study assessed escin, which has been excluded from our review |
| Fitzgerald 1967 | In this cross‐over, not‐randomised, study, participants received placebo or troxerutin monthly in an alternative way. The paper does not describe numerical results |
| Forconi 1977 | No clinical endpoints were assessed ‐ only microcirculatory parameters |
| Frausini 1985 | This was a single‐blind study |
| Friederich 1978 | Some included patients had thrombophlebitis; these individuals could not be separated out from the patient population |
| Glinski 1999 | This was an open RCT conducted to examine venous ulcers |
| Gonzalez‐Fajardo 1990 | The outcome assessed was a surrogate (photoplethysmographic evaluation) |
| Gouny 1999 | This study looked at the efficacy of hydroxyethyl rutosides in the local treatment of symptoms of venous insufficiency during air travel; this topic does not come under the scope of this review |
| Granger 1995 | It is not specified that the trial was double‐blind |
| Henriet 1995 | This study compared the efficacy of Diovenor (diosmine) vs a combination of different flavonoids |
| Honorato 1990 | This study compared the efficacy of hidrosmine vs diosmine |
| Horvath 1985 | This study assessed the efficacy of dyhidroergotamine, which is not included in our review |
| Incandela 1995 | No clinical endpoints were assessed ‐ only microcirculatory parameters |
| Incandela 1996 | This study looked at the effects of troxerutin on microcirculatory parameters |
| Incandela 2001 | This was a single‐blind study |
| Incandela 2001a | This study assessed escin for diabetic microangiopathy |
| Incandela 2001b | This study assessed Centella asiatica for diabetic microangiopathy |
| Incandela 2002 | This was a single‐blind study |
| Incandela 2002b | This study assessed a rutoside for diabetic microangiopathy |
| ISRCTN5340167 | This study compared micronised purified flavonoid fraction 1000 mg vs 500 mg |
| Janssens 1999 | No clinical endpoints were assessed ‐ only microcirculatory parameters |
| Janssens 1999a | This study looked at the effects of Ginkor Fort (ginkgo biloba), which is not included in our review |
| Jantet 2000 | This was not an RCT |
| Kalus 2004 | No clinical endpoints were assessed ‐ only microcirculatory parameters (cutaneous microcirculation and oxygen supply) |
| Kiesewetter 2000 | This study evaluated red vine leaf extract, an herbal medicine containing several flavonoids that are not included in our review |
| Koch 2002 | This study compared Venostasin and Pycnogenol |
| Koltringer 1993 | This study assessed Ginkgo biloba, which is not included in our review |
| Kostering 1985 | This study assessed microcirculatory parameters |
| Kranendonk 1993 | This study focused on patients who had recently undergone venous surgery. Leg oedema and other symptoms could be attributed to the surgery ‐ not to venous insufficiency |
| Krcílek 1973 | The drug evaluated was escin, which is not included in our review |
| Krähenbühl 1975 | The bencyclan is a drug with cardiovascular depression effects; it is not included in the review |
| Lambelet 1973 | Some included patients had thrombophlebitis; these could not be separated out from the patient population |
| Languillat 1988b | The drug studied (Veliten) was a combination of rutin, ascorbic acid and alpha‐tocopherol. No clinical endpoints were assessed ‐ only microcirculatory parameters |
| Languillat 1989 | No clinical endpoints were assessed ‐ only microcirculatory parameters |
| Le Dévéhat 1989 | Outcomes were not applicable to this review: microcirculatory and haemorrheological parameters |
| Le Dévéhat 1997 | This study assessed troxerutine for CVI: microcirculatory and haemorrheological parameters |
| Lefebvre 1991 | This study assessed troxerutine during pregnancy |
| Marastoni 1982 | This study assessed dihydroergotamine, which is not included in our review |
| Marastoni 1982a | This study compared Centella asiatica vs tribenoside |
| Menyhei 1994 | No placebo group was included |
| Monreal 1994 | Two active products for CVI were compared |
| Monreal 1997 | Investigators examined prevention of post‐thrombotic syndrome with hidrosmine |
| Monteil‐Seurin 1993 | This study compared Cyclo 3 Fort vs diosmine |
| Monteverde 1987 | This study compared extract of Centella asiatica vs beta‐hydroxiethyl‐rutoside |
| Morales 1993 | This RCT assessed escin, which is not included in our review |
| Muschietti 1978 | This study compared natural diosmine, synthetic diosmine and tribenoside |
| Naser‐Hijazi 2004 | This RCT assessed the combination of coumarin and troxerutin (SB‐LOT) in CVI. The objective of this study was to assess effects of SB‐LOT on blood coagulation |
| NCT01654016 | This is an ongoing single‐blinded (outcome assessor) clinical trial about Daflon |
| NCT02191163 | This study assessed the efficacy of the red‐vine‐leaf extract, which is not included in our review (Antistax) |
| NCT02191254 | This study assessed the efficacy of the red‐vine‐leaf extract, which is not included in our review (Antistax) |
| NCT02191280 | This study assessed the efficacy of the red‐vine‐leaf extract, which is not included in our review (Antistax) |
| Neumann 1988 | No clinical endpoints were assessed ‐ only microcirculatory parameters |
| Neumann 1990 | Only haemodynamic venous parameters were assessed by light reflection rheography and transcutaneous oxygen tension measurement (TcPO2) |
| Neumann 1995 | No placebo group was included. This study assessed the efficacy of 1 tablet or 500 mg HR twice daily or class II compressive stockings |
| Neumann‐Mangoldt 1979 | The drug evaluated contained escin and heparin |
| Nill 1970 | This study assessed escin, which is not included in our review |
| Ottillinger 2001 | This study assessed escin, which is not included in our review |
| Paciaroni 1982 | The drug evaluated was escin, which is not included in our review |
| Partsch 1981 | This study assessed oral dyhidroergotamine, which is not included in our review |
| Paul 1983 | The drug evaluated was benzarone, which is not included in our review |
| Pauschinger 1987 | The drug evaluated was escin, which is not included in our review |
| Pecking 1998 | This study assessed Daflon for lymphoedema associated with breast cancer |
| Petruzzellis 1990 | This study included patients with superficial phlebitis |
| Petruzzellis 2002 | This study included 3 comparative groups (2 of different doses of oxirutoside and 1 of placebo), but treatment concealment was incorrect or was not explained correctly |
| Pointel 1987b | This study assessed vitamin C combined with Ruscus aculeatus and anthocyanosides from Ribes nigrum (helps to maintain the integrity of capillaries) |
| Pokrovskii 2005 | This study assessed Ginkgo biloba, which is not included in our review |
| Pollastri 1982 | This was a cross‐over, double‐blind study. The article does not state that this trial was randomised |
| Questel 1983 | No clinical endpoints were assessed ‐ only microcirculatory parameters |
| Rabe 2011b | This study assessed the efficacy of the red‐vine‐leaf extract, which is not included in our review (Antistax) |
| Rehn 1993 | This study compared hidroxirutin vs oxerutin for CVI |
| Rehn 1993b | This study assessed different dose regimens of O‐(beta‐hydroxyethyl) rutosides in healthy volunteers |
| Rehn 1996 | This single‐blind study looked at the bioequivalence of oxerutins |
| Riccioni 2004 | This study assessed the efficacy of the combination of troxerutin plus french maritime pine bark |
| Rish 1972 | This study included patients with thrombophlebitis |
| Roztocil 1977 | This study assessed microcirculatory parameters (capillary filtration) |
| Roztocil 2003 | This was an RCT that was not blinded |
| Sadoun 1993 | This study compared the efficacy of 2 different doses of chromocarbe diethylamine (800 and 1200 mg/d/3 mo) |
| Sanctis 2001 | This study assessed escin, which is not included in our review |
| Schmeck‐Lindenau 2003 | This study assessed the hepatic safety of the combination of coumarin‐troxerutin |
| Seydewitz 1992 | Non‐clinical parameters were evaluated in this study |
| Stefanini 1996 | The control was not placebo ‐ it was balneotherapy |
| Stegmann 1987 | This trial did not include a placebo group as control |
| Steiner 1986 | This study included 20 voluntary, ambulant patients with a history of pregnancy‐related varicosis, with varicosis with CVI or with both |
| Steiner 1990 | This study assessed the drug escin, which is not included in our review |
| Steiner 1992 | This study assessed the drug escin, which is not included in our review |
| Steru 1988 | It is not specified whether this trial was double‐blind |
| Strauss 1992 | The aim of this study was to check the effects of active treatment following oedema caused by the orthostatic test |
| Strefezza 2010 | This study compared the effects of different formulations of heperidin and diosmine |
| Topalov 1990 | This study assessed the efficacy of troxesamol (combination of troxerutin, acetylsalicylic acid and dipyridamole) |
| Tsukanov 2010 | This study looked at doses of a phlebotropic therapy |
| Turio 2000 | This study assessed the efficacy of a combination of vitamin PP (niacin), vitamin C and phyto‐therapeutic extracts titrated in escin, bromelain and anthocyanosides |
| Weindorf 1987 | This study assessed the efficacy of the combination of Ruscus aculeatus and trimethylhespiridinchalcone |
| Widmer 1972 | The active treatment in this study was phlebolan composed of rutin and several anti‐inflammatory agents such as prednisolone and diphenylbutazone |
| Zicot 1993 | This trial did not include a placebo group |
| Zuccarelli 1996 | This study assessed GinKor Fort (Ginkgo biloba), which is not included in our review |
CVI: chronic venous insufficiency HR: hidroxy rutoside PO2: pressure of oxygen in blood PCO2: pressure of carbon dioxide in blood RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
ISRCTN18841175.
| Trial name or title | Effects of micronised purified flavonoic fraction on microcirculation in women suffering from chronic venous disease |
| Methods | Single‐centre double‐blind randomised placebo‐controlled parallel‐group study |
| Participants | 240 females 18 to 30 years old suffering from primary chronic venous disease |
| Interventions | Micronised purified flavonoic fraction 500 mg over 4 menstrual cycles vs placebo |
| Outcomes | Effects on microcirculatory and biological parameters over 4 menstrual cycles |
| Starting date | July 2009 |
| Contact information | Prof Eliete Bouskela. Instituto de Biologia Roberto Alcantara Gomes Dept Ciências Fisiologicasências Fisiologicas Rua Sao Francisco Xavier 524 ‐ PHLC ‐ Sala 104 ‐ Lab. Presq em Microcirculaçao. Rio de Janeiro. Brazil 20550‐013 |
| Notes | Sponsor: Institut de Recherches Internationales Servier (France) |
NCT01532882.
| Trial name or title | Efficacy and safety of diosmine 600 mg vs placebo for painful symptoms in patients with chronic venous disease of lower limbs (EDEN) |
| Methods | Multi‐centre controlled randomised double‐blind placebo‐controlled parallel‐group study |
| Participants | 378 patients with painful symptoms of chronic venous disorder (CVD) of the lower limbs |
| Interventions | Diosmine 600 mg ‐ DIOVENOR vs placebo (1 tablet per day during 28 days) |
| Outcomes | Primary outcome measure: Change in visual analogue scale score for assessment of painful venous symptoms |
| Starting date | January 2012 |
| Contact information | Dr Jean‐Jérôme GUEX, Nice, France 06000 |
| Notes | Sponsor: Innotech International |
NCT01848210.
| Trial name or title | Efficacy and safety of coumarin and troxerutin in the symptomatic treatment of chronic venous insufficiency |
| Methods | Controlled randomised double‐blind placebo‐controlled parallel‐group study |
| Participants | 398 patients with chronic venous insufficiency in the reference leg with the clinical classification C3, or C4a or C4b or C5 |
| Interventions | Coumarin 30 mg, troxerutin 180 mg fixed‐dose combination tablets (Venalot), orally, 3 times daily for up to 16 weeks vs placebo |
| Outcomes | Primary outcome measure: Mean change from baseline in volume of reference leg at week 16 |
| Starting date | May 2013 |
| Contact information | Takeda |
| Notes | Sponsor: Takeda |
Differences between protocol and review
We have noted some differences between the protocol and this systematic review (SR), specifically in the following items.
In the previous version of this SR, we made different assumptions to examine adverse events. In this current SR, we have simplified the analyses. We calculated the risk of adverse events by considering the number of participants with adverse events reported in the papers as the numerator and the number of participants randomised by group as the denominator.
In the previous version of this SR, we considered the Jadad scale (Jadad 1996) and the Cochrane criteria (Clarke 2003) to assess the risk of bias of included RCTs. In this current SR, we used only the current Cochrane criteria to assess risk of bias (Higgins 2011).
In the previous version of this SR, we considered statistical heterogeneity of P value < 0.1 as a reason for not pooling results of the studies. In this current SR, we used the I2 statistic and considered I2 > 75% a reason for not pooling the results of RCTs.
In the previous version of this SR, we specified to use a random‐effects statistical model in all analyses. In this current SR, however, we used this model only when I2 was between 50% and 75%.
In the previous version of this SR, we performed a sensitivity analysis by level of quality of studies according to the Cochrane criteria (Clarke 2003). In this current SR, we performed a sensitivity analysis that included only studies with low risk of bias according to the Cochrane risk of bias (Higgins 2011).
In the previous version of this SR, assessment of publication bias was not specified. In this current SR, we constructed a funnel plot to explore publication bias.
In the previous version of this SR, the quality of evidence was assessed by the Cochrane criteria. In this current SR, we applied GRADE (Grades of Recommendation, Assessment, Development and Evaluation Working Group) (Schünemann 2011) criteria and presented a 'Summary of findings' table (Table 1).
Contributions of authors
All reviewers contributed to development of the protocol, selected and assessed clinical trials and evaluated their quality. In the first version of this SR:
MJ Martinez, RM Moreno and D Capellà extracted data for the first version of this SR. SM Uriona and RWM Vernooij extracted data from new studies and assessed risk of bias of all included studies;
RM Moreno provided clinical experience and insight on the protocol and review reports;
MJ Martinez was responsible for statistical and methodological aspects and for overall compiling of this SR; and
MJ Martinez, RWM Vernooij, SM Uriona, AT Stein, RM Moreno, E Vargas, D Capellà and X Bonfill Cosp were responsible for manuscript development and revision of this SR.
Sources of support
Internal sources
Iberoamerican Cochrane Centre, Spain.
External sources
-
The Chief Scientist Office, Scottish Government Health Directorates, The Scottish Government, UK.
The Cochrane Vascular editorial base is supported by the Chief Scientist Office.
-
Instituto de Salud Carlos III, Spain.
Dr. Mª José Martinez Zapata is funded by a Miguel Servet research contract from the Instituto de Salud Carlos III (CP15/00116).
Declarations of interest
Dr D Capellà, Dr X Bonfill Cosp, Dr RM Moreno and Dr E Vargas were part of an advisory group of the Safety Committee of the Spanish Drug Agency, whose objective was to assess the efficacy and safety of phlebotonics during 2002. Dr MJ Martínez assisted with technical work for this group.
Dr RM Moreno, Dr X Bonfill Cosp and Dr MJ Martínez‐Zapata were authors of a published double‐blind, placebo‐controlled clinical trial (Martinez‐Zapata 2008) that is included in this review. This study was sponsored by Laboratorios Dr Esteve, which markets calcium dobesilate (Doxium). Laboratorios Dr Esteve signed a written commitment to fully respect the researchers' independence and to allow dissemination of results, whatever they could be. Furthermore, Dr RM Moreno, Dr X Bonfill Cosp and Dr MJ Martínez‐Zapata were researchers in the included clinical trial DOBESILATO500/2, which was prematurely interrupted because of lack of funding.
Dr MJ Martínez‐Zapata: none known. Dr RWM Vernooij: none known. Dr SM Uriona Tuma: none known. Dr AT Stein: none known. Dr RM Moreno: none known. Dr E Vargas: none known. Dr D Capellà: chair of the Independent Drug Monitoring Committee of the clinical trial "Neurodegeneration as an early event in the pathogenesis of diabetic retinopathy: a multicentric, prospective, phase II‐III, randomised controlled trial to assess the efficacy of neuroprotective drugs administered topically to prevent or arrest diabetic retinopathy", carried out by the European Consortium for the Early Treatment of Diabetic Retinopathy (EUROCONDOR) with support from the European Commission, FP7‐HEALTH‐2011‐GA No. 278040 and sponsored by BCN Peptides. Dr X Bonfill Cosp: none known.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Allegra 1981 {published data only}
- Allegra C. Pollari G, Criscuolo A, Bonifacio M, Tabassi D. Centella asiatica extract in venous disorders of the lower limbs. Comparative clinico‐instrumental studies with a placebo. Clinica Terapeutica 1981;99(5):507‐13. [PubMed] [Google Scholar]
Alterkamper 1987 {published data only}
- Alterkamper H. Efficacy of antivaricotic drugs can be measured objectively. Phlebologie in der Praxis 1987;2(9‐10):19‐20. [Google Scholar]
Arcangeli 2000 {published data only}
- Arcangeli P. Pycnogenol in chronic venous insufficiency. Fitoterapia 2000;71(3):236‐44. [DOI] [PubMed] [Google Scholar]
Balmer 1980 {published data only}
- Balmer A, Limoni C. Clinical, placebo‐controlled double‐blind study of venoruton in the treatment of chronic venous insufficiency. Importance of the selection of patients. Vasa 1980;9(1):76‐82. [PubMed] [Google Scholar]
- Blume J. Therapy of venous oedemas [Tratamento do edema de origem venosa]. Revista Brasileira de Medicina 1994;51(3):283‐8. [Google Scholar]
Belczak 2014 {published data only}
- Belczak SQ, Sincos IR, Campos W, Beserra J, Nering G, Aun R. Veno‐active drugs for chronic venous disease: a randomized, double‐blind, placebo‐controlled parallel‐design trial. Phlebology 2014;29(7):454‐60. [DOI] [PubMed] [Google Scholar]
Bergqvist 1981 {published data only}
- Berqvist D, Hallböök T, Lindblad B, Lindhagen A. A double‐blind trial of O‐(beta‐hydroxyethyl)‐rutoside in patients with chronic venous insufficiency. Vasa 1981;10(3):253‐60. [PubMed] [Google Scholar]
Biland 1982 {published data only}
- Biland L, Blättler P, Scheibler P, Studer S, Widmer K. Zur therapie sogenannt venosër beinsbeschwerden. Vasa 1982;11(1):53‐8. [PubMed] [Google Scholar]
Burnand 1989 {published data only}
- Burnand KG, Powell S, Bishop C, Stacey M, Pulvertaft T. Effect of Paroven on skin oxygenation in patients with varicose veins. Phlebologie 1989;4(1):15‐22. [Google Scholar]
Casley‐Smith 1988 {published data only}
- Casley‐Smith JR. A double‐blind trial of calcium dobesilate in chronic venous insufficiency. Angiology 1988;39(10):853‐7. [DOI] [PubMed] [Google Scholar]
- Casley‐Smith JR. A double‐blind, placebo ‐controlled, matched‐pair trial of the mode of action of 'Doxium' in the treatment of chronic venous insufficiency. Proceedings of the Union Internationale de Phlebologie ‐ 10th World Congress, Strasbourg, 25‐29 September. London and Paris: John Libbey Eurotext Ltd, 1989.
- Casley‐Smith JR. A double‐blind, placebo‐controlled, matched‐pair trial of the mode of action of 'Doxium' in the treatment of chronic venous insufficiency. Phlebologie 1989;2:709‐11. [Google Scholar]
Cauwenberge 1972 {published data only}
- Cauwenberge H. Double‐blind study of the efficacy of a soluble rutoside derivative in the treatment of venous disease. Archives of Internal Pharmacodynamics and Therapeutics 1972;196(Suppl 196):122‐5. [PubMed] [Google Scholar]
Cauwenberge 1978 {published data only}
- Cauwenberge H. Double‐blind clinical trial to assess the efficacy of 0‐(b‐hidroxy‐ethyl)‐rutosidesin th treatment of venous disorders [Etude en double aveugle de l'efficacité de l'0‐(b‐hidroxyéthyl)‐rutosides dans le traitement des affections veineuses]. Mèdicine et Hygiène 1978;35:4175‐7. [Google Scholar]
Cesarone 2002 {published data only}
- Cesarone MR, Incandela L, DeSanctis MT, Belcaro G, Griffin M, Ippolito E, et al. Treatment of edema and increased capillary filtration in venous hypertension with HR (Paroven, Venoruton; O‐(beta‐hydroxyethyl)‐rutosides): a clinical, prospective, placebo‐controlled, randomized, dose‐ranging trial. Journal of Cardiovascular Pharmacology and Therapeutics 2002;7 Suppl 1:S21‐4. [DOI] [PubMed] [Google Scholar]
Chassignolle 1994 {published data only}
- Chassignolle JF, Amiel M, Lanfranchi G, Barbe R. Activite therapeutique de daflon 500 mg dans l'insuffisance veineuse fonctionnelle. Journal International de Medicine 1994;Suppl 99:32‐5. [Google Scholar]
Cloarec 1994 {published data only}
- Cloarec M, Clement R, Griton P, Guillou GB, Golden G. A double blind three centre trial on efficacy of o‐(beta‐hydroxyethyl) rutosides in patients with venous insufficiency. International Angiology 1994;13 Suppl 1(2):74. [Google Scholar]
Cloarec 1996 {published data only}
- Cloarec M, Clément R, Griton P. A double‐blind clinical trial of hydroxyethylrutosides in the treatment of the symptoms and signs of chronic venous insufficiency. Phlebology 1996;11(2):76‐82. [Google Scholar]
Cornu‐Thenard 1985 {published data only}
- Cornu‐Thenard A, Dahan B, Parades B. Study of the action in venous insufficiency of the legs. Pierre Fabre Medicament Laboratoires (Novartis). Report no. DC982GEC51(2), 1985.
Danielsson 2002 {published data only}
- Danielsson G, Jungbeck C, Peterson K, Norgren L. A randomised controlled trial of micronised purified flavonoid fraction versus placebo in patients with chronic venous disease. European Journal of Vascular and Endovascular Surgery 2002;23(1):73‐6. [DOI] [PubMed] [Google Scholar]
Diebschlag 1994 {published data only}
- Diebschlag W, Nocker W, Lehmacher W, Rehn D. A clinical comparison of two doses of O‐(beta‐hydroxyethyl) rutosides (oxerutins) in patients with chronic venous insufficiency. Journal of Pharmaceutical Medicine 1994;4(1):7‐14. [Google Scholar]
DOBESILATO500/2 {unpublished data only}
- Fundación Iberoamericana Itaca. Randomized, double‐blind multicenter clinical trial comparing the efficacy of calcium dobesilate with placebo in the treatment of ulcer secondaries to chronic venous disease. ClinicalTrials.gov 2009.
Dominguez 1992 {published data only}
- Dominguez C, Brautigham I, González E, González JA, Nazco J, Valiente R, et al. Therapeutic effects of hidrosmin on chronic venous insufficiency of the lower limbs. Current Medical Research and Opinion 1992;12(10):623‐30. [DOI] [PubMed] [Google Scholar]
Fermoso 1992 {published data only}
- Fermoso J, Legido AG, Pino J, Valiente R. Therapeutic value of hidrosmin in the treatment of venous disorders of the lower limbs. Current Therapeutic Research, Clinical and Experimental 1992;52(1):124‐34. [Google Scholar]
Flota‐Cervera 2008 {published and unpublished data}
- Flota LF. Prospective, randomised, double‐blind, placebo controlled, clinical trial that assesses the efficacy of calcium dobesilate in the limphoedema by varicose disease [Estudio clínico prospectivo aleatorizado, doble ciego, con control placebo, para evaluar la eficacia en la resolución del edema de origen lifático, del dobesilato de calcio en pacientes con enfermedad varicosa]. Knoll de Mexico S.A. Laboratorios Dr. Esteve. No de proyec. Knoll‐mex‐02‐99, 003/MEX, 99.
- Flota‐Cervera F, Flota‐Ruiz C, Treviño C, Berber A. Randomized, double blind, placebo‐controlled clinical trial to evaluate the lymphagogue effect and clinical efficacy of calcium dobesilate in chronic venous disease. Angiology 2008;59(3):352‐6. [DOI] [PubMed] [Google Scholar]
Gilly 1994 {published data only}
- Frileux C, Gilly R. Activité thérapeutic de Daflon 500 mg dans l'insuffisance veineuse chronique des membres inférieurs. Journal Internationale de Medicine 1994;Suppl 99:36‐9. [Google Scholar]
- Gilly R, Pillion G, Frileux C. Evaluation of a new venactive micronized flavonoid fraction (S5682) in symptomatic disturbances of the venolymphatic circulation of the lower limb: a double‐blind, placebo‐controlled study. Phlebology 1994;9(2):67‐70. [Google Scholar]
- Thiollet M, Frileux C, Gilly R. Evaluation of a new micronized diosmin in the treatment of chronic venous incompetence: a double‐blind, placebo controlled trial. Journal of Vascular Surgery 1992;15(2):447. [Google Scholar]
Guilhou 1997 {published data only}
- Guilhou JJ, Dereure O, Marzin L, Ouvry P, Zuccarelli F, Debure C, et al. Efficacy of Daflon 500 mg in venous leg ulcer healing: a double‐blind, randomised, controlled versus placebo trial in 107 patients. Angiology 1997;48(1):77‐85. [DOI] [PubMed] [Google Scholar]
Hachen 1982 {published data only}
- Hachen HJ, Lorenz P. Double‐blind clinical and plethysmographic study of calcium dobesilate in patients with peripheral microvascular disorders. Angiology 1982;33(7):480‐8. [DOI] [PubMed] [Google Scholar]
Ihme 1996 {published data only}
- Ihme N, Kiesewetter H, Jung F, Hoffmann KH, Birk A, Müller A, et al. Leg oedema protection from a buckwheat herb tea in patients with chronic venous insufficiency: a single‐centre, randomized, double‐blind, placebo‐controlled clinical trial. European Journal of Clinical Pharmacology 1996;50(6):443‐7. [DOI] [PubMed] [Google Scholar]
Jongste 1986 {published data only}
- Jongste AB, Cate JW, Huisman MV. The effectiveness of o‐(b‐hydroxyethyl)‐rutosides (HR) in the post‐thrombotic syndrome (PTS). Phlebology 1986;85 Suppl 285:837‐9. [Google Scholar]
Jongste 1989 {published data only}
- Jongste AB, Jonker JJC, Huisman MV, Cate JW, Azar AJ. A double‐blind trial on the short‐term efficacy of HR in patients with the post‐thrombotic syndrome. Phlebology 1990;5(Suppl 1):21‐2. [Google Scholar]
- Jongste AB, Jonker JJC, Huisman MV, Cate JW, Azar AJ. A double‐blind three center clinical trial on the short‐term efficacy of O‐(beta‐hydroxyethyl)‐rutosides in patients with post‐thrombotic syndrome. Thrombosis and Haemostasis 1989;62(3):826‐9. [PubMed] [Google Scholar]
Kiesewetter 1997 {published data only}
- Kiesewetter H, Koscielny J, Grützner K, Müller A, Hoffmann KH, Birk A. Buckwheat herb/troxerutin‐combination for the treatment of chronic venous insufficiency. Zeitschrift für Phytotherapie 1997;18(6):341‐6. [Google Scholar]
Klüken 1971 {published data only}
- Klüken N. Double‐blind clinical trial to assess the therapy with drugs for venous disorders [Estudio clínico doble ciego para tratar de objetivar la terapéutica con venofármacos]. Therapiewoche 1971;21:1. [Google Scholar]
Koscielnny 1996 {published data only}
- Koscielnny J, Radtke H, Hoffmann, Jung F, Müller A, Grützner KI, et al. Fagorutin buckwheat herb tea in chronic venous insufficiency. Zeitschrift für Phytotherapie 1996;17(3):147‐59. [Google Scholar]
Kriner 1985 {published data only}
- Kriner E, Braun R, Hirche H, Laak HH. Treatment of venous insufficiency. A double‐blind trial with Phlebodril. Zeitschrift für Allgemeinmedizin 1985;61(9):309‐13. [Google Scholar]
Labs 2004 {published and unpublished data}
- Jaeger K. Efficacy and safety of doxium in chronic venous insufficiency. OM PHARMA (LAB. ESTEVE). Study number: DX‐1994/2.
- Jaeger K. Efficacy and safety of doxium in chronic venous insufficiency. Double‐blind, placebo‐controlled multicentre study. International Angiology 2001;20(2 Suppl 1):239. [PubMed] [Google Scholar]
- Labs KH, Degischer S, Gamba G, Jaeger KA, on behalf of the CVI Study Group. Effectiveness and safety of calcium dobesilate in treating chronic venous insufficiency: randomized, double‐blind, placebo‐controlled trial. Phebology 2004;19(3):123‐9. [Google Scholar]
Languillat 1988 {published data only}
- Languillat N. Trial of Cyclo 3 Fort in venous insufficiency of the lower limbs: Xenon 133 functional investigation of venous circulatory velocity. Pierre Fabre Medicament Laboratories (Novartis). No. Report DC982GEC130(2), 1988.
Laurent 1988 {published data only}
- Laurent R, Gilly R, Frileux C. Clinical evaluation of a venotropic drug in man. Example of Daflon 500 mg. International Angiology 1988;7(2 Suppl):39‐43. [PubMed] [Google Scholar]
Lazzarini 1982 {published data only}
- Lazzarini A, Danieli L. Clinical controlled trial of aminaphtone in lower limbs' phlebopathies and phlebopathic ulcers [Sperimentazione clinica controllata del l´aminaftone flebopatie degli arti inferiori e nelle flebopatiche]. Rassegna Internazionale di Clinica e Terapia 1982;62(12):825‐44. [Google Scholar]
MacLennan 1994 {published data only}
- Dikland WJ. A clinical trial on the effect of hydroxyethylrutosides on venous refilling time as measured by light reflection rheography. Scripta Phlebologica 1995;3:4‐7. [Google Scholar]
- MacLennan WJ, Wilson J, Rattenhuber V, Dikland WJ, Vanerdonckt J, Moriau M. Hydroxyethylrutosides in elderly patients with chronic venous insufficiency. Its efficacy and tolerability. Gerontology 1994;40(1):45‐52. [DOI] [PubMed] [Google Scholar]
Mann 1981 {published data only}
- Mann RJ. A double‐blind trial of oral O‐beta‐hydroxyethyl rutosides for stasis leg ulcers. British Journal of Clinical Practice 1981;35:79‐81. [PubMed] [Google Scholar]
Marinello 2002 {published and unpublished data}
- Marinello J, Videla S. Chronic venous insufficiency of the lower limbs: suitability of transcutaneous blood gas monitoring as an endpoint to evaluate the outcome of pharmacological treatment with calcium dobesilate. Methods and Findings in Experimental and Clinical Pharmacology 2004;26(10):775‐80. [DOI] [PubMed] [Google Scholar]
- Marinello J, et al. Multicentric, randomised, double‐blind, placebo controlled, clinical trial that assess the efficacy of calcium dobesilate in the treatment of venous hypertension in patients with chronic venous insufficiency [Ensayo clínico multicéntrico, doble ciego, aleatorizado, controlado con placebo sobre la eficacia de dobesilato de calcio en el tratamiento de la hipertensión venosa en pacientes afectos de insuficiencia venosa crónica en sus extremidades inferiores. Código: ESCLIN‐004/99]. Laboratorios Dr. Esteve.
Martinez‐Zapata 2008 {published data only}
- Martinez‐Zapata MJ, Moreno RM, Gich I, Urrútia G, Bonfill X, Chronic Venous Insufficiency Study Group. A randomized, double‐blind multicentre clinical trial comparing the efficacy of calcium dobesilate with placebo in the treatment of chronic venous disease. European Journal of Vascular and Endovascular Surgery 2008;35(3):358‐65. [DOI] [PubMed] [Google Scholar]
Nocker 1990 {published data only}
- Nocker W, Diebschlag W. An investigation of dosage effects with drinking solutions of o‐(beta hydroxyethyl)‐rutosides. Vasa 1987;16:365‐9. [PubMed] [Google Scholar]
- Nocker W, Diebschlag W, Lehmacher W. Clinical trials of the dose‐related effects of o‐(beta‐hydroxyethyl)‐rutosides in patients with chronic venous insufficiency. Phlebology 1990;5 Suppl 1:23‐6. [Google Scholar]
- Nocker W, Diebschlag W, Lehmacher W. Three‐month, randomized, double‐blind, dose‐response study with O‐(beta‐hydroxyethyl)‐rutosides drinking solution. Vasa 1989;18(3):235‐8. [PubMed] [Google Scholar]
Padros 1972 {published data only}
- Padros W. Double blind investigation of clinical effectiveness of calcium dobesilate in the venous insufficiency syndrome (Dutch). Ars Medici Internationaal Tijdschrift voor Praktische Therapie 1977;6(8):1977. [Google Scholar]
- Padros W. Double blind study of the action of calcium dobesilate on venous insufficiency syndromes. Ars Medici Revue Internationale de Therapie Pratique 1977;32(8):783‐90. [Google Scholar]
- Padrós W. Controlled study of the effect of calcium dobesilate on syndromes of venous insufficiency. Medicina Clínica 1972;58(6):515‐9. [Google Scholar]
Parrado 1999 {published data only}
- Parrado F, Buzzi A. A study of the efficacy and tolerability of a preparation containing Ruscus aculeatus in the treatment of chronic venous insufficiency of the lower limbs. Clinical Drug Investigation 1999;18(4):255‐61. [Google Scholar]
Pecchi 1990 {published data only}
- Pecchi S, Franco V, Damiani P, Guerrini M, Perri T. Calcium dobesilate in the treatment of primary venous insufficiency of the lower limbs. A controlled clinical study [Il dobesilato di calcio nel trattamento del l´insufficienza venosa primitiva degli arti inferiori]. Clinica Terapeutica 1990;132(6):409‐17. [PubMed] [Google Scholar]
Pedersen 1992 {published data only}
- Pedersen FM, Hamberg O, Sorensen MD, Neland K. The effect of O‐(beta‐hydroxyethyl)‐rutoside (Venoruton) on symptomatic venous insufficiency in the lower limbs. Ugeskrift for Laeger 1992;154(38):2561‐3. [PubMed] [Google Scholar]
Petrassi 2000 {published data only}
- Petrassi C, Mastromarino A, Spartera C. Pycnogenol in chronic venous insufficiency. Phytomedicine 2000;7(5):383‐8. [DOI] [PubMed] [Google Scholar]
Planchon 1990 {published data only}
- Planchon B. Venous insufficiency and Daflon 500 mg [Insuffisance veineuse et Daflon 500 mg]. Artères et Veines 1990;IX(4):376‐80. [Google Scholar]
Pointel 1986 {published data only}
- Pointel JP. Titrated extract of centella asiatica (TECA) in the treatment of venous insufficiency of the lower limbs. Angiology 1986;37(5):420‐1. [DOI] [PubMed] [Google Scholar]
- Pointel JP, Boccalon H, Cloarec M, Devehat C, Joubert M. Titrated extract of Centella asiatica (TECA) in the treatment of venous insufficiency of the lower limbs. Angiology 1987;38(1 Pt 1):46‐50. [DOI] [PubMed] [Google Scholar]
Prerovsky 1972 {published data only}
- Prerovsky I, Roztocil K, Hlavova A, Koleilat Z, Razgova L, Oliva I. The effects of hydroxyethylrutosides after acute and chronic oral administration in patients with venous diseases. A double blind study. Angiologica 1972;9(3‐6):408‐14. [DOI] [PubMed] [Google Scholar]
Pulvertaft 1983 {published data only}
- Pulvertaft TB. General practice treatment of symptoms of venous insufficiency with oxerutins. Results of a 660 patient multicentre study in the UK. Vasa 1983;12(4):373‐6. [PubMed] [Google Scholar]
- Pulvertaft TB. Paroven in the treatment of chronic venous insufficiency. Practitioner 1979;223(1338):838‐41. [PubMed] [Google Scholar]
Rabe 2011 {published data only}
- Rabe E, Jaeger KA, Bulitta M, Pannier F. Calcium dobesilate in patients suffering from chronic venous insufficiency: a double‐blind, placebo‐controlled, clinical trial. Phlebology 2011;26:162–8. [DOI] [PubMed] [Google Scholar]
Renton 1994 {published data only}
- Renton S, Leon M, Belcaro G, Nicolaides AN. The effect of hydroxyethylrutosides on capillary filtration in moderate venous hypertension: a double blind study. International Angiology 1994;13(3):259‐62. [PubMed] [Google Scholar]
Rose 1970 {published data only}
- Rose SS. A report on the use of an hydroxyethylrutoside in symptoms due to venous back pressure and allied conditions in the lower limbs. British Journal of Clinical Practice 1970;24(4):161‐4. [PubMed] [Google Scholar]
Rudofsky 1989 {published data only}
- Rudofsky G, Diehm C, Grub J, Hartmann M, Schultz‐Ehrenburg HU, Bisler H. Ruscus saponines and the flavonoid hesperidinmethylchalcone in the treatment of chronic venous insufficiency. Proceedings of the Union Internationale de Phlebologie ‐ 10th World Congress, Strasbourg, 25‐29 September. London and Paris: John Libbey Eurotext Ltd, 1989:728‐30.
- Rudofsky G, Diehm C, Gruss JD, Hartman M, Schultz‐Ehrenburg HK, Bisler H. Chronic venous insufficiency: treatment with Ruscus extract and trimethyl hesperidine chalcone. Münchener Medizinische Wochenschrift 1990;132(13):205‐10. [Google Scholar]
Schultz‐Ehrenburg 1993 {published data only}
- Schultz‐Ehrenburg U, Müller B. Two multicentre clinical trials of two different dosages of O‐(beta‐hydroxyethyl)‐rutosides in the treatment of leg ulcers. Phlebology 1993;8 Suppl 1:29‐30. [Google Scholar]
Sentou 1984 {published data only}
- Sentou Y. Double blind study of the activity of Cyclo 3 in man. International Angiology 1984;3:106‐9. [Google Scholar]
Serralde 1990 {published data only}
- Serralde CF, Aceves AQ. Clinical trial of the O‐(β‐hydroxy‐ethyl‐rutosides) in patients with chronic venous insufficiency [Ensayo clínico de o‐(beta‐hidroxietil‐rutósidos) en pacientes con insuficiencia venosa crónica]. Revista Médica del Hospital General de México 1990;53(2):102‐6. [Google Scholar]
Thebaut 1985 {published data only}
- Thebaut JF, Thebaut P, Vin F. Trial of vasculoprotective agent (plant products of the flavan class) in functional manifestations of peripheral venous insufficiency (double‐blind trial in 92 cases). Gazette Medicale 1985;92(12):96‐100. [Google Scholar]
Tsouderos 1989 {published data only}
- Tsouderos Y. Are the phlebotonic properties shown in clinical pharmacology predictive of a therapeutic benefit in chronic venous insufficiency. Our experience with Daflon 500 mg. International Angiology 1989;8(4):53‐9. [PubMed] [Google Scholar]
- Tsouderos Y. Venous tone: are the phlebotonic properties predictive of a therapeutic benefit? A comprehensive view of our experience with Daflon 500 mg. Zeitschrift fur Kardiologie 1991;80 Suppl 7:95‐101. [PubMed] [Google Scholar]
Unkauf 1996 {published data only}
- Unkauf M, Rehn D, Klinger J, Motte S, Grobmann K. Investigation of the efficacy of oxerutins compared to placebo in patients with chronic venous insufficiency treated with compression stockings. Arzneimittel‐Forschung 1996;46(5):478‐82. [PubMed] [Google Scholar]
Vanscheidt 2002a {published data only}
- Vanscheidt W, Rabe E, Naser‐Hijazi B, Ramelet AA, Partsch H, Diehm C, et al. The efficacy and safety of a coumarin‐/troxerutin‐combination (SB‐LOT) in patients with chronic venous insufficiency: a double blind placebo‐controlled randomised study. Vasa 2002;31(3):185‐90. [DOI] [PubMed] [Google Scholar]
Vanscheidt 2002b {published data only}
- Vanscheidt W, Jost V, Wolna P, Lücker A, Muller A, Theurer C, et al. Efficacy and safety of a Butcher's broom preparation (Ruscus aculeatus L. extract) compared to placebo in patients suffering from chronic venous insufficiency. Arzneimittel‐Forschung 2002;52(4):243‐50. [DOI] [PubMed] [Google Scholar]
Vin 1994 {published data only}
- Vin E, Chabanel A, Taccoen A, Ducros J, Grufaz J, Hutinel B, et al. Action of Veinamitol 3500 mg on clinical and hemorheological data in CVI. International Angiology 1995;14(Suppl 1):99. [Google Scholar]
- Vin F, Chabanel A, Taccoen A, Ducros J, Gruffaz J, Hutinel B, et al. Action de la troxérutine sur les paramètres cliniques, pléthysmographiques et rhéologiques de l'insuffisance veineuse des membres inférieurs. Etude contrôlée contre placebo. Artères et Veines 1992;XI:333‐42. [Google Scholar]
- Vin F, Chabanel A, Taccoen A, Ducros J, Gruffaz J, Hutinel B, et al. Double‐blind trial of the efficacy of troxerutin in chronic venous insufficiency. Phlebology 1994;9(2):71‐6. [Google Scholar]
Welch 1985 {unpublished data only}
- Welch W, Moriau M, Gysel JP. A double‐blind, placebo controlled trial of o‐(beta‐hydroxyethyl)‐rutosides in patients with chronic venous insufficiency. Novartis 1985.
Widmer 1990 {published data only}
- Widmer L, Biland L, Barras JP. Doxium 500 in chronic venous insufficiency: a double‐blind placebo controlled multicentre study. International Angiology 1990;9(2):105‐10. [PubMed] [Google Scholar]
Zucarelli 1987 {published data only}
- Zucarelli F. Clinical efficacy and tolerability of rutin. Double blind, placebo controlled clinical trial. [Efficacité clinique et tolerance de la coumarine rutine. Étude controlée en double aveugle versus placebo]. Gazette Médicale 1987;94(32):80‐6. [Google Scholar]
References to studies excluded from this review
Akbulut 2010 {published data only}
- Akbulut B. Calcium dobesilate and oxerutin: effectiveness of combination therapy. Phlebology 2010;25:66‐71. [DOI] [PubMed] [Google Scholar]
Allaert 1992 {published data only}
- Allaert FA, Vin F, Levardon M. [Comparative study of the effectiveness of continuous or intermittent courses of a phlebotonic drug on venous disorders disclosed or aggravated by oral, estrogen‐progesterone contraceptives]. Phlébologie 1992;45:167‐73. [PubMed] [Google Scholar]
Amato 1994 {published data only}
- Amato C. Advantage of micronized flavonoidic fraction (daflon 500 mg) in comparison with a nonmicronized diosmin. Angiology 1994;45(6, part 2):531‐6. [PubMed] [Google Scholar]
Androulakis 1989 {published data only}
- Androulakis G, Panoysis PA. Plethysmographic confirmation of the beneficial effect of calcium dobesilate in primary varicose veins. Angiology 1989;40(1):1‐4. [DOI] [PubMed] [Google Scholar]
Auteri 1990 {published data only}
- Auteri A, Blardi P, Frigerio C, Lillo L, Perri T. Pharmacodynamics of troxerutine in patients with chronic venous insufficiency: correlations with plasma drug levels. International Journal of Clinical Pharmacology Research 1990;10(4):235‐41. [PubMed] [Google Scholar]
Avram 1996 {published data only}
- Avram J, Avram R, Colban O, Murariu M, Toma D, Preda D. The treatment of venous insufficiency with daflon 500 mg. International Angiology 1996; Vol. 15, issue 2 Suppl:1‐110.
Bacci 2003 {published data only}
- Bacci PA, Allegra C, Botta G, Mancini S. The role of a multifunctional plant complex in phlebolymphology: randomized, placebo‐controlled double‐blind clinical study. Amercian College of Phlebology. Abstracts from the 17th Annual Congress, August 27 ‐ 31, 2003 — San Diego, California.
Bastide 1976 {published data only}
- Bastide G, Becade P, Goulley Y. Double blind study of Dihydroergotamine Sandoz in venous pathology of lower limbs. Angeiologie 1976;28(5):249‐54. [Google Scholar]
Batchvarova 1989 {published data only}
- Batchvarova V. Clinical effect of Troxevit on chronic venous insufficiency [Effet clinique du Troxevit sur l'insuffisance veineuse chronique]. Phlebologie 1989;42:703‐5. [Google Scholar]
Batchvarova 1989a {published data only}
- Batchvarova V. Effet Clinique du Troxevit sur l'Insuffisance Veineuse Chronique. Vol. 2, London & Paris: John Libby Eurotext Ltd, 1989:703‐5. [Google Scholar]
Behar 1993 {published data only}
- Behar A, Nathan P, Lavieuville M, Allaert FA. Effect of veinotonyl 75 on the capillary permeability test using technetium albumin in cyclic orthostatic edemas. Phlébologie 1993;46(4):721‐31. [PubMed] [Google Scholar]
Belcaro 1986 {published data only}
- Belcaro GV. Treatment of chronic venous hypertension of the lower limbs by O‐(beta‐hydroxyethyl)‐rutoside and elastic compression. Phlebology 85. London: John Libbey, 1986:834‐6.
Belcaro 1989 {published data only}
- Belcaro G, Rulo A, Candiani C. Evaluation of the microcirculatory effects of Venorutin in patients with chronic venous hypertension by laser Doppler flowmetry, transcutaneous PO2 and PCO2 measurements, leg volumetry and ambulatory venous pressure measurements. Vasa 1989;18:146‐51. [PubMed] [Google Scholar]
- Belcaro G, Rulo A, Candiani C. Evaluation of the microcirculatory effects of Venoruton in patients with chronic venous hypertension by laser‐Doppler flowmetry, transcutaneous PO2 and PCO2 measurements, leg volumetry and ambulatory venous pressure measurements. Phlebology 1989;4(1):23‐30. [PubMed] [Google Scholar]
Belcaro 1995 {published data only}
- Belcaro G, Cesarone MR, Sanctis MT, Incandela L, Laurora G, Fevrier B, et al. Laser doppler and transcutaneous oxymetry: modern investigations to assess drug efficacy in chronic venous insufficiency. International Journal of Microcirculation: Clinical and Experimental 1995;15(Suppl 1):45‐9. [DOI] [PubMed] [Google Scholar]
Belcaro 2002 {published data only}
- Belcaro G, Cesarone MR, Bavera P, Ricci A, Renton S, Leon M, et al. HR (Venoruton1000, Paroven, 0‐[beta‐hydroxyethyl]‐rutosides) vs. Daflon 500 in chronic venous disease and microangiopathy: an independent prospective, controlled, randomized trial. Journal of Cardiovascular Pharmacology and Therapeutics 2002;7(3):139‐45. [DOI] [PubMed] [Google Scholar]
Belcaro 2003 {published data only}
- Belcaro G, Cesarone MR, Nicolaides AN, Geroulakos G, Acerbi G, Candiani C, et al. The LONFLIT4‐VENORUTON study: a randomized trial prophylaxis of flight‐edema in normal subjects. Clinical and Applied Thrombosis/Hemostasis 2003;9(1):19‐23. [DOI] [PubMed] [Google Scholar]
- Cesarone MR, Belcaro G, Brandolini R, Renzo A, Bavera P, Dugall M, et al. The LONFLIT4‐Venoruton Study: a randomized trial‐‐prophylaxis of flight‐edema in venous patients. Angiology 2003;54(2):137‐42. [DOI] [PubMed] [Google Scholar]
Belcaro 2008 {published data only}
- Belcaro G. Rosaria Cesarone M, Ledda A, Cacchio M, Ruffini I, Ricci A, et al. O‐(beta‐hydroxyethyl)‐rutosides systemic and local treatment in chronic venous disease and microangiopathy: an independent prospective comparative study. Angiology 2008;59(Suppl 1):7S‐13S. [DOI] [PubMed] [Google Scholar]
Belcaro 2008b {published data only}
- Belcaro G, Cesarone MR, Ledda A, Cacchio M, Ruffini I, Ricci A, et al. 5‐Year control and treatment of edema and increased capillary filtration in venous hypertension and diabetic microangiopathy using O‐(β‐hydroxyethyl)‐rutosides: a prospective comparative clinical registry. Angiology 2008;59(1):14S‐20S. [DOI] [PubMed] [Google Scholar]
Bello 1990 {published data only}
- Bello AA, Meyer K, Garcia AT, Reinaga VV. Calcium dobesilate combined with a heparinoid in the topical treatment of chronic venous insufficiency: a double‐blind study. Acta Therapeutica 1990;16(1):79‐87. [Google Scholar]
Beltramino 1999 {published data only}
- Beltramino R, Penenory A, Buceta AM. An open‐label, randomised multicentre study comparing the efficacy and safety of CYCLO 3 FORT versus hydroxyethyl rutoside in chronic venous lymphatic insufficiency. International Angiology 1999;18(4):337‐42. [PubMed] [Google Scholar]
- Beltramino R, Penenory A, Buceta AM. An open‐label, randomized multicenter study comparing the efficacy and safety of Cyclo 3 Fort versus hydroxyethyl rutoside in chronic venous lymphatic insufficiency. Angiology 2000;51(7):535‐44. [DOI] [PubMed] [Google Scholar]
Bento 2006 {published data only}
- Bento C, Branda˜o DDC, Smith P. A multicentric, IV phase, multidisciplinary, prospective, randomized, double blinded, comparative study to evaluate the castanha‐da‐india, rutina, smilax japicanga and polygonum punctatum combination efficacy and tolerability in the treatment of patients suffering from symptomatic venous insufficiency comparing to placebo treatment. Revista Brasileira de Medicina 2006;63(8):422‐6. [Google Scholar]
Berson 1976 {published data only}
- Berson I. A double blind clinical trial in cases of CVI with doxivenil gel and another gel containing only a heparinoid [Expérimentation clinique dans l'IVC (double aveugle) du gel Doxivenil et d' un gel contenant un héparinoïde seul]. Schweizerische Rundschau fur Medizin Praxis 1976;65(32):991‐3. [PubMed] [Google Scholar]
Berson 1978 {published data only}
- Berson I. About a new medicamentous treatment of the varicose syndrome. Schweiz Rundschau Med (PRAXIS) 1978;67:981‐3. [PubMed] [Google Scholar]
Berson 1980 {published data only}
- Berson I, Geiser J‐D. An open comparative study of two phlebotoniques. Etude Comparative Ouverte Entre Deux phl ‚Botropes Chez Deux Groupes r‚ Partis au Hasard 1980;69(35):1244‐6. [Google Scholar]
Blume 1996 {published data only}
- Blume J. Therapy of venous oedema [Tratamento do edema de origem venosa. Eficácia de um tratamento medicamentoso em combinaçao com o tratamento compresivo]. Revista Brasileira de Medicina 1994;51(3):283‐8. [Google Scholar]
- Blume J, Wüstenberg P. Chronic vein insufficiency. Treatment results with benzopyrones during and after compression therapy [Cronisch‐venöse Insuffizienz (CVI). Behandlungsergebnisse mit benzopyronen und nach Kompressiontherapie]. Therapiewoche 1996;46(10):540‐4. [Google Scholar]
Boccalon 1989 {published data only}
- Boccalon H. Cyclo 3 fort and antagonism of plethysmographic disturbances observed upon exposure to heat: preliminary results. Phlebologie 1989;4(1):59‐62. [Google Scholar]
Bohm 1989 {published data only}
- Bohm C. Venodiuretics: a new combination of diuretic and edema protective drugs. Medizinische Welt 1989;40(30‐31):887‐8. [Google Scholar]
Boisseau 1995 {published data only}
- Boisseau MR, Taccoen A, Garreau C, Vergnes C, Roudaut MF, Garreau‐Gomez B. Fibrinolysis and hemorheology in chronic venous insufficiency: a double‐blind study of troxerutin efficiency. Journal of Cardiovascular Surgery 1995;36(4):369‐74. [PubMed] [Google Scholar]
Bolliger 1972 {published data only}
- Bolliger AA. Results of a double blind trial of percutaneously administered rutoside. Angiologica 1972;9:397‐400. [PubMed] [Google Scholar]
Bort 1995 {published data only}
- Bort H, Hahn M, Klyscz T, Junger M. The influence of rutosides on increased capillary permeability in chronic venous insufficiency as measured by video capillaroscopy. Proceedings of the Union Internationale de Phlebologie ‐ 12th World Congress, London, 3‐8 September. 1995.
Bosse 1985 {published data only}
- Bosse K, Drieschner P, Klose L. Comparative studies concerning the effectiveness of therapeutic agents in chronic venous insufficiency. Phlebologie und Proktologie 1985;14:111‐4. [Google Scholar]
Brami 1983 {published data only}
- Brami C, Morere MCNK, Megret G, Elbaz C. Double‐blind controlled trial against placebo of dihydroergocryptine mesilate plus caffeine in chronic venous insufficiency. Angeiologie 1983;35(8):281‐3. [Google Scholar]
Brock 1991 {published data only}
- Brock FE. Arnica montana and vein disease. Zeitschrift fur Phytotherapie 1991;12(5):141‐5. [Google Scholar]
Brock 2001 {published data only}
- Brock FE. Synergystic effect of vein ‐ typical hydrotherapy according to Kneipp and topical arnica ‐ treatment in patients with chronic venous insufficiency. Erfahrungsheilkunde 2001;50:357‐63. [Google Scholar]
Carstens 1985 {published data only}
- Carstens C, Hampel H. Treatment of oedemata in chronic venous insufficiency by means of an additional therapy with DIU Venostatin. Die Medizinische Welt 1985;36:867‐70. [Google Scholar]
Cataldi 2001 {published data only}
- Cataldi A, Gasbarro V, Viaggi R, Soverini R, Gresta E, Mascoli F. Effectiveness of the association of alphatocopherol, rutin, melilotus and centella asiatica in the treatment of patients affected by chronic venous insufficiency [Efficacia clinica di un'associazine di alfatocoferoli, rutina, meliloto e centella asiatica nel trattamento di pazienti con insufficienza venosa cronica]. Minerva Cardioangiologica 2001;49(2):159‐63. [PubMed] [Google Scholar]
Cesarone 1992 {published data only}
- Cesarone MR, Laurora G, Ricci A, Belcaro G, Pomante P, Candiani C, et al. Acute effects of hydroxyethylrutosides on capillary filtration in normal volunteers, patients with venous hypertension and in patients with diabetic microangiopathy (a dose comparison study). Vasa 1992;21(1):76‐80. [PubMed] [Google Scholar]
Cesarone 1994 {published data only}
- Cesarone MR, Laurora G, Sanctis MT, Incandela L, Grimaldi R, Marelli C, et al. Microcirculatory activity of centella asiatica in venous insufficiency. Minerva Cardioangiologica 1994;42(6):299‐304. [PubMed] [Google Scholar]
Cesarone 2001 {published data only}
- Cesarone MR, Sanctis MT, Incandela L, Belcaro G, Griffin M, Bavera P, et al. Microvascular changes in venous hypertension due to varicose veins after standardized application of Essaven gel‐‐a placebo‐controlled, randomized study. Angiology 2001;52 Suppl 3:S11‐6. [DOI] [PubMed] [Google Scholar]
Cesarone 2001a {published data only}
- Cesarone MR, Belcaro G, Sanctis MT, Incandela L, Cacchio M, Bavera P, et al. Effects of the total triterpenic fraction of Centella asiatica in venous hypertensive microangiopathy: a prospective, placebo‐controlled, randomized trial. Angiology 2001;52 Suppl 2:S15–8. [PubMed] [Google Scholar]
Cesarone 2001b {published data only}
- Cesarone MR, Incandela L, Belcaro G, Sanctis MT, Ricci A, Griffin M. Two‐week topical treatment with Essaven gel in patients with diabetic microangiopathy‐‐a placebo‐controlled, randomized study. Angiology 2001;52 Suppl 3:S43‐8. [DOI] [PubMed] [Google Scholar]
Cesarone 2001c {published data only}
- Cesarone MR, Belcaro G, Rulo A, Griffin M, Ricci A, Ippolito E, et al. Microcirculatory effects of total triterpenic fraction of Centella asiatica in chronic venous hypertension: measurement by laser Doppler, TcPO2‐CO2, and leg volumetry 93. Angiology 2001;52 Suppl 2:S45‐8. [PubMed] [Google Scholar]
Cesarone 2001d {published data only}
- Cesarone MR, Incandela L, Sanctis MT, Belcaro G, Geroulakos G, Griffin M, et al. Flight microangiopathy in medium‐ to long‐distance flights: prevention of edema and microcirculation alterations with total triterpenic fraction of Centella asiatica. Angiology 2001;52 Suppl 2:S33‐7. [PubMed] [Google Scholar]
Cesarone 2001e {published data only}
- Cesarone MR, Incandela L, Sanctis MT, Belcaro G, Bavera P, Bucci M, et al. Evaluation of treatment of diabetic microangiopathy with total triterpenic fraction of Centella asiatica: a clinical prospective randomized trial with a microcirculatory model. Angiology 2001;52 Suppl 2:S49‐54. [PubMed] [Google Scholar]
Cesarone 2002a {published data only}
- Cesarone MR, Belcaro G, Incandela L, Geroulakos G, Griffin M, Lennox A, et al. Flight microangiopathy in medium‐to‐long distance flights: prevention of edema and microcirculation alterations with HR (Paroven, Venoruton; 0‐(beta‐hydroxyethyl)‐rutosides): a prospective, randomized, controlled trial. Journal of Cardiovascular Pharmacology and Therapeutics 2002;7 Suppl 1:S17‐20. [DOI] [PubMed] [Google Scholar]
Cesarone 2002b {published data only}
- Cesarone MR, Incandela L, DeSanctis MT, Belcaro G, Dugall M, Acerbi G. Variations in plasma free radicals in patients with venous hypertension with HR (Paroven, Venoruton; O‐(beta‐hydroxyethyl)‐rutosides): a clinical, prospective, placebo‐controlled, randomized trial. Journal of Cardiovascular Pharmacology and Therapeutics 2002;7 Suppl 1:S25‐8. [DOI] [PubMed] [Google Scholar]
Cesarone 2003 {published data only}
- Cesarone MR, Belcaro G, Geroulakos G, Griffin M, Ricci A, Brandolini R, et al. Flight microangiopathy on long‐haul flights: prevention of edema and microcirculation alterations with Venoruton. Clinical and Applied Thrombosis/Hemostasis 2003;9(2):109‐14. [DOI] [PubMed] [Google Scholar]
Cesarone 2005 {published data only}
- Cesarone MR, Belcaro G, Pellegrini L, Ledda A, Renzo A, Vinciguerra G, et al. HR, 0‐(beta‐hydroxyethyl)‐rutosides, in comparison with diosmin+hesperidin in chronic venous insufficiency and venous microangiopathy: an independent, prospective, comparative registry study. Angiology 2005;56(1):1‐8. [DOI] [PubMed] [Google Scholar]
Cesarone 2006 {published data only}
- Cesarone MR, Belcaro G, Rohdewald P, Pellegrini L, Ledda A, Vinciguerra G, et al. Rapid relief of signs/symptoms in chronic venous microangiopathy with pycnogenol: a prospective, controlled study. Angiology 2006;57:569‐76. [DOI] [PubMed] [Google Scholar]
Cesarone 2006a {published data only}
- Cesarone MR, Belcaro G, Pellegrini L, Ledda A, Vinciguerra G, Ricci A, et al. Venoruton vs Daflon: evaluation of effects on quality of life in chronic venous insufficiency. Angiology 2006;57(2):131‐8. [DOI] [PubMed] [Google Scholar]
Cesarone 2006b {published data only}
- Cesarone MR, Belcaro G, Rohdewald P, Pellegrini L, Ledda A, Vinciguerra G, et al. Comparison of Pycnogenol and Daflon in treating chronic venous insufficiency: a prospective, controlled study. Clinical and Applied Thrombosis/Hemostasis 2006;12(2):205‐12. [DOI] [PubMed] [Google Scholar]
Cesarone 2006c {published data only}
- Cesarone MR, Belcaro G, Pellegrini L, Ledda A, Vinciguerra G, Ricci A, et al. Circulating endothelial cells in venous blood as a marker of endothelial damage in chronic venous insufficiency: improvement with Venoruton. Journal of Cardiovascular Pharmacology and Therapeutics 2006;11(1):93‐8. [DOI] [PubMed] [Google Scholar]
Cesarone 2006d {published data only}
- Cesarone MR, Belcaro G, Rohdewald P, Pellegrini L, Ledda A, Vinciguerra G, et al. Improvement of diabetic microangiopathy with pycnogenol: a prospective, controlled study. Angiology 2006;57:431‐6. [DOI] [PubMed] [Google Scholar]
Cesarone 2010 {published data only}
- Cesarone MR, Belcaro G, Rohdewald P, Pellegrini L, Ledda A, Vinciguerra G, et al. Improvement of signs and symptoms of chronic venous insufficiency and microangiopathy with Pycnogenol: a prospective, controlled study. Phytomedicine 2010;17(11):835‐9. [DOI] [PubMed] [Google Scholar]
Chant 1973 {published data only}
- Chant AD. The effect of paroven (HR) of the clearance of sodium‐24 from the subcutaneous tissues of the foot in patients with varicose veins. Vasa 1973;2(3):288‐91. [PubMed] [Google Scholar]
Chiummariello 2009 {published data only}
- Chiummariello S, Gado F, Monarca C, Ruggiero M, Carlesimo B, Scuderi N, et al. [Multicentric study on a topical compound with lymph‐draining action in the treatment of the phlebostatic ulcer of the inferior limbs]. Il Giornale di chirurgia 2009;30(11‐12):497‐501. [PubMed] [Google Scholar]
Clemens 1986 {published data only}
- Clemens S, Bisler H, Braun R. Phlebodril: Influences on the venous regurgitation. Phlebologie und Proktologie 1986;15(1):15‐9. [Google Scholar]
Cospite 1989 {published data only}
- Cospite M, Dominici A. Double blind study of the pharmacodynamic and clinical activities of 5682 SE in venous insufficiency. Advantages of the new micronized form. International Angiology 1989;8(4):61‐5. [PubMed] [Google Scholar]
Cospite 1996 {published data only}
- Cospite M, Milio G. Heparan sulfate vs diosmin: effects on microcirculation in chronic venous insufficiency of the lower extremities. Advances in Therapy 1996;13(3):178‐190. [Google Scholar]
Cospite 1998 {published data only}
- Cospite M, Dominici A. Advantage of micronisation of Daflon 500 mg compared with a simple diosmine in the treatment of venous insufficiency. Double blind study. Phlebologie 1998;51:243‐7. [Google Scholar]
De Anna 1989 {published data only}
- Anna D, Mari F, Intini S, Gasbarro V, Sortini A, Pozza E, et al. Effects of therapy with aminaftone on chronic venous and lymphatic stasis [Effetti della terapia con aminaftone sulla stasi venosa e linfatica cronica]. Minerva Cardioangiologica 1989;37(5):251‐4. [PubMed] [Google Scholar]
- Anna D, Risaliti A, Intini S, Terrosu G, Petri R, Taddeo U, et al. Aminaphtone therapy in venous lymphatic stasis of lower limbs. Phlebologie 1989;2:753‐5. [Google Scholar]
- Anna D, Risaliti A, Intini S, Uzzau A, Terrosu G, Petri R, et al. Aminaphtone therapy in venous and lymphatic stasis of lower limbs. Proceedings of the Union Internationale de Phlebologie ‐ 10th World Congress, Strasbourg, 25‐29‐September 1989. London and Paris: John Libbey Eurotext Ltd, 1989; Vol. 2, issue 251:753‐5.
Delacroix 1981 {published data only}
- Delacroix P. Double‐blind trial of endotelon (TM) in chronic venous insufficiency. La Revue de Medecine 1981;22(27‐28):1793‐802. [Google Scholar]
Delecluse 1991 {published data only}
- Delecluse M, Ducros JJ, Egal G, Hamel H, Junk R, Leroux A, et al. [Clinical study of Diovenor 300 mg versus a mixture of flavonoides in 90 % of diosmine in the treatment of symptoms of chronic venous insufficiency in young active females]. Essai Clinique Pragmatique de Diovenor 300 mg Versus Melange de Flavonoides a 90 % de Diosmine Dans le Traitement des Manifestations d'Insuffisance Veineuse Chronique Chez la Femme Active Jeune 1991;10(7):498‐503. [Google Scholar]
de Parades 1990 {published data only}
- Parades B, Demarez JP, Cauquil J. Comparative analysis of the therapeutic effects of Cyclo 3 Fort and Diosmin 450 mg in combination with hesperidin 50 mg in venous insufficiency of the legs. Vie Medicale 1990;6:226‐32. [Google Scholar]
De Sanctis 2001 {published data only}
- Sanctis MT, Belcaro G, Incandela L, Cesarone MR, Griffin M, Ippolito E, et al. Treatment of edema and increased capillary filtration in venous hypertension with total triterpenic fraction of Centella asiatica: a clinical, prospective, placebo‐controlled, randomized, dose‐ranging trial. Angiology 2001;52(Suppl 2):S55‐9. [PubMed] [Google Scholar]
Duchene 1988 {published data only}
- Duchene Marullaz P, Amiel M, Barbe R. Evaluation of the clinical pharmacological activity of a phlebotonic agent. Application to the study of Daflon 500 mg. International Angiology 1988;7 Suppl 2:25‐32. [PubMed] [Google Scholar]
Dustmann 1984 {published data only}
- Dustmann HO, Godolias G, Seibel K. Foot volume with chronic venous insufficiency while standing: effect of a new treatment. Therapiewoche 1984;34(36):5077‐86. [Google Scholar]
Erdlen 1989 {published data only}
- Erdlen F. Clinical efficacy of venostasin. A double blind trial. Medizinische Welt 1989;40(36):994‐6. [Google Scholar]
Erler 1991 {published data only}
- Erler M. Horse chestnut seed extract in the therapy of the peripheral venous edema ‐ Clinical therapies in comparison. Medizinische Welt 1991;42(7):593‐6. [Google Scholar]
Fitzgerald 1967 {published data only}
- Fitzgerald DE. A clinical trial of troxerutin in venous insufficiency of the lower limb. The Practitioner 1967;198(185):406‐7. [PubMed] [Google Scholar]
Forconi 1977 {published data only}
- Forconi S, Guerrini M, Perri T. Study of the activity of a flavonoid, O‐(beta‐hydroxyethyl)‐rutoside, at high dose levels of venous tone measured by "strain gauge" plethysmography. Vasa 1977;6(3):279‐84. [PubMed] [Google Scholar]
Frausini 1985 {published data only}
- Frausini G, Rotatori P, Oliva S. Controlled trial on clinical‐dynamic effects of three treatments in chronic venous insufficiency. Giornale Italiano di Angiologica 1985;5(2):147‐51. [Google Scholar]
Friederich 1978 {published data only}
- Friederich HC, Vogelsberg H, Neiss A. Evaluation of internally effective venous drugs. Zeitschrift fur Hautkrankheiten 1978;53(11):369‐74. [PubMed] [Google Scholar]
Glinski 1999 {published data only}
- Glinski W, Chodynicka B, Roszkiewicz J, Bogdanowski T, Lecewicz Torun B, Kaszuba A, et al. The beneficial augmentative effect of micronised purified flavonoid fraction (MPFF) on the healing of leg ulcers: an open, multicentre, controlled, randomised study. Phlebology 1999;14(4):151‐7. [Google Scholar]
- Glinski W, Chodynicka B, Roszkiewicz J, Bogdanowski T, Lecewicz‐Torun B, Kaszuba A, et al. Effectiveness of a micronized purified flavonoid fraction (MPFF) in the healing process of lower limb ulcers. An open multicentre study, controlled and randomized. Minerva Cardioangiologica 2001;49(2):107‐14. [PubMed] [Google Scholar]
Gonzalez‐Fajardo 1990 {published data only}
- Gonzalez‐Fajardo JA, Rodriguez‐Camarero SJ, Marino P, Castro Villamor MA, March Garcia JR, Carpintero Mediavilla L, et al. [Photoplethysmographic evaluation of the effect of a vascular tonic drug]. Angiologia 1990;42(5):167‐71. [PubMed] [Google Scholar]
Gouny 1999 {published data only}
- Gouny AM, Horovitz D, Gouny P, Sauvage E, Nussaume O. Effectiveness and safety of hydroxyethyl‐rutosides in the local treatment of symptoms of venous insufficiency during air travel [Etude d'efficacite et de tolerance des hydroxyethyl‐rutosides dans le traitement local des symptomes d'insuffisance veineuse survenant au cours des transports aeriens]. Journal des Maladies Vasculaires 1999;24(3):214‐20. [PubMed] [Google Scholar]
Granger 1995 {published data only}
- Granger C, Laveille C, Vilain C, Jochemsen R. Correlation between haemodynamic parameters of venous tone and clinical symptoms improvement in patients with chronic venous insufficiency. A controlled randomised study of Daflon 200 mg 2 tablets per day versus placebo during two months of treatment. International Angiology 1995;14 Suppl 1:343. [Google Scholar]
Henriet 1995 {published data only}
- Henriet J‐P. [Functional venous insufficiency: clinical study comparing once a day DIOVENOR 600 mg (600 mg of diosmine d'hemisyntheses) versus two doses per day of a mixture of 500 mg of flavonoides (900 mg of diosmine)]. Phlebologie 1995;48(2):285‐90. [Google Scholar]
Honorato 1990 {published data only}
- Honorato Perez J, Arcas Meca R. Double blind comparative study of hidrosmin‐diosmin in peripheral vein disease. Revista de Medicina de la Universidad de Navarra 1990;34(2):77‐9. [PubMed] [Google Scholar]
Horvath 1985 {published data only}
- Horvath W, Tomschi F. [The postthrombotic state and the effect of dihydroergotamine]. Das Postthrombotische Zustandsbild und Seine Beeinflussung Durch Dihyrdroergotamin 1985;14(1):84‐9. [PubMed] [Google Scholar]
Incandela 1995 {published data only}
- Incandela L, Cesarone MR, Sanctis MT, Laurora G, Ricci A, Gerentes I. Evaluation of the microcirculatory effects of veinamitol 3500 mg in chronic venous insufficiency. International Angiology 1995;14 Suppl 1:98‐9. [Google Scholar]
Incandela 1996 {published data only}
- Incandela L, Sanctis MT, Cesarone MR, Laurora G, Belcaro G, Taccoen A, et al. Efficacy of troxerutin in patients with chronic venous insufficiency: a double‐blind, placebo‐controlled study. Advances in Therapy 1996;13(3):161‐6. [Google Scholar]
Incandela 2001 {published data only}
- Incandela L, Belcaro G, Sanctis MT, Cesarone MR, Griffin M, Ippolito E, et al. Total triterpenic fraction of Centella asiatica in the treatment of venous hypertension: a clinical, prospective, randomized trial using a combined microcirculatory model. Angiology 2001;52 Suppl 2:S61‐7. [PubMed] [Google Scholar]
Incandela 2001a {published data only}
- Incandela L, Belcaro G, Cesarone MR, Sanctis MT, Griffin M. Microvascular alterations in diabetic microangiopathy: topical treatment with Essaven gel‐‐a placebo‐controlled, randomized study. Angiology 2001;52 Suppl 3:S35‐41. [DOI] [PubMed] [Google Scholar]
Incandela 2001b {published data only}
- Incandela L, Belcaro G, Cesarone MR, Sanctis MT, Nargi E, Patricelli P, et al. Treatment of diabetic microangiopathy and edema with total triterpenic fraction of Centella asiatica: a prospective, placebo‐controlled randomized study. Angiology 2001;52 Suppl 2:S27‐31. [PubMed] [Google Scholar]
Incandela 2002 {published data only}
- Incandela L, Belcaro G, Renton S, DeSanctis T, Cesarone MR, Bavera P, et al. HR (Paroven, Venoruton; 0‐(beta‐hydroxyethyl)‐rutosides) in venous hypertensive microangiopathy: a prospective, placebo‐controlled, randomized trial. Journal of Cardiovascular Pharmacology and Therapeutics 2002;7 Suppl 1:7‐10. [DOI] [PubMed] [Google Scholar]
Incandela 2002b {published data only}
- Incandela L, Cesarone MR, DeSanctis MT, Belcaro G, Dugall M, Acerbi G. Treatment of diabetic microangiopathy and edema with HR (Paroven, Venoruton; 0‐(beta‐hydroxyethyl)‐rutosides): a prospective, placebo‐controlled, randomized study. Journal of Cardiovascular Pharmacology and Therapeutics 2002;7 Suppl 1:S11‐5. [DOI] [PubMed] [Google Scholar]
ISRCTN5340167 {published data only}
- ISRCTN53430167. Clinical acceptability study in patients suffering from chronic venous disease (CVD) comparing micronized purified flavonoid fraction (MPFF) 1000 mg, one tablet daily, to MPFF 500 mg tablet twice a day. http://www.isrctn.com/search?q=ISRCTN53430167 (accessed 28 September 2015).
Janssens 1999 {published data only}
- Janssens D, Michiels C, Guillaume G, Cuisinier B, Louagie Y, Remacle J. Increase in circulating endothelial cells in patients with primary chronic venous insufficiency: protective effect of Ginkor Fort in a randomized double‐blind, placebo‐controlled clinical trial. Journal of Cardiovascular Pharmacology 1999;33(1):7‐11. [DOI] [PubMed] [Google Scholar]
Janssens 1999a {published data only}
- Janssens D, Michiels C, Guillaume G, Cuisinier B, Louagie Y, Remacle J. Increase in circulating endothelial cells in patients with primary chronic venous insufficiency: protective effect of Ginkor Fort in a randomized double‐blind, placebo‐controlled clinical trial. Journal of Cardiovascular Pharmacology 1999;33(1):7‐11. [DOI] [PubMed] [Google Scholar]
Jantet 2000 {published data only}
- Jantet G. RELIEF study: first consolidated European data. Reflux assEssment and quaLity of lIfe improvement with micronized Flavonoids. Angiology 2000;51(1):31‐7. [DOI] [PubMed] [Google Scholar]
Kalus 2004 {published data only}
- Kalus U, Koscielny J, Grigorov A, Schaefer E, Peil H, Kiesewetter H. Improvement of cutaneous microcirculation and oxygen supply in patients with chronic venous insufficiency by oral therapy with red wine leaf extract AS 195. Vasomed 2004;16(1):20‐1. [DOI] [PubMed] [Google Scholar]
- Kalus U, Koscielny J, Grigorov A, Schaefer E, Peil H, Kiesewetter H. Improvement of cutaneous microcirculation and oxygen supply in patients with chronic venous insufficiency by orally administered extract of red vine leaves AS 195: a randomised, double‐blind, placebo‐controlled, crossover study. Drugs in R & D 2004;5(2):63‐71. [DOI] [PubMed] [Google Scholar]
Kiesewetter 2000 {published data only}
- Kiesewetter H, Koscielny J, Kalus U, Vix JM, Peil H, Petrini O, et al. Efficacy of orally administered extract of red vine leaf AS 195 (folia vitis viniferae) in chronic venous insufficiency (stages I‐II). A randomized, double‐blind, placebo‐controlled trial. Arzneimittel‐Forschung 2000;50(2):109‐17. [DOI] [PubMed] [Google Scholar]
Koch 2002 {published data only}
- Koch R. Comparative study of Venostasin and Pycnogenol in chronic venous insufficiency. Phytotherapy Research 2002;16 Suppl 1:S1‐5. [DOI] [PubMed] [Google Scholar]
Koltringer 1993 {published data only}
- Koltringer P, Langsteger W, Klima G, Reisecker F, Eber O. Hemorheologic effects of ginkgo biloba extract EGb 761. Dose‐ dependent effect of EGb 761 on microcirculation and viscoelasticity of blood. [German]. Fortschritte der Medizin 1993;111(10):170‐2. [PubMed] [Google Scholar]
Kostering 1985 {published data only}
- Kostering H, Bandura B, Merten HA, Wieding JU. The behaviour of blood clotting and its inhibitors under long‐term with 5,6‐benzo‐alpha‐pyrone (coumarin). Double‐blind study. Arzneimittel‐Forschung 1985;35(8):1303‐6. [PubMed] [Google Scholar]
Krähenbühl 1975 {published data only}
- Krähenbühl B. Chronic arterial insufficiency of lower limbs: treatment by bencyclan (fludilat). Schweizerische Rundschau fur Medizin Praxis 1975;64(20):632‐4. [PubMed] [Google Scholar]
Kranendonk 1993 {published data only}
- Kranendonk SE, Koster AM. A double‐blind clinical trial of the efficacy and tolerability of O‐(beta‐hydroxyethyl)‐rutosides and compression stockings in the treatment of leg oedema and symptoms following surgery for varicose veins. Phlebology 1993;8(2):77‐81. [Google Scholar]
Krcílek 1973 {published data only}
- Krcílek A, Smejkal V. Therapeutic effects of venotonics in clinical pharmacotherapeutical evaluations by double‐blind tests. Casopis Lekaru Ceskych 1973;112:930‐3. [PubMed] [Google Scholar]
Lambelet 1973 {published data only}
- Lambelet F. Le traitement des troubles circulatoires veineux: une étude en double‐insu avec le Sandovène. Praxis 1973;62:925‐9. [PubMed] [Google Scholar]
Languillat 1988b {published data only}
- Languillat N, Zucarrelli F. Etude en double aveugle contre placebo de l'activite veinotonique due veliten: evolution de la permeabilite capillare et de lat vitesse de circulation veineuse. Acta Medica Internationale Angiologie 1988;5(83):3‐5. [Google Scholar]
Languillat 1989 {published data only}
- Languillat N, Zuccarelli F, Hariton C. Radioisotopic comparative double‐blind study of venous capillary permeability and circulation rate after treatment by Veliten (R) in venous insufficiency of inferior limbs. Proceedings of the Union Internationale de Phlebologie ‐ 10th World Congress, Strasbourg, 25‐29 September. 1989.
Le Dévéhat 1989 {published data only}
- Devehat C, Lemoine A. Effet hemorheological de la troxerutine dans l'insuffisance veineuse [Effet hemorheological de la troxerutine dans l'insuffisance veineuse]. In: Negus D, Jantet G editor(s). Phlebology 1985. Herts, UK: John Libbey and Co Ltd, 1986:850‐2. [Google Scholar]
- Dévéhat C, Vimeux M, Bandoux G. Hemoreological effects of oral troxerutin treatment versus placebo in venous insufficiency of the lower limbs. Clinical Hemorrheology 1989;9(4):543‐52. [Google Scholar]
- Dévéhat C, Vimeux M, Bondoux G, Khodabandehlou T. Hemorheological effects of oral troxerutin treatment in venous insufficiency of the lower limbs. Phlebologie 1989;2:766‐8. [Google Scholar]
Le Dévéhat 1997 {published data only}
- Devehat C, Khodabandehlou T, Vimeux M, Kempf C. Evaluation of haemorheological and microcirculatory disturbances in chronic venous insufficiency: activity of Daflon 500 mg. International Journal of Microcirculation: Clinical and Experimental 1997;17(Suppl 1):27‐33. [DOI] [PubMed] [Google Scholar]
Lefebvre 1991 {published data only}
- Lefebvre G, Lacombe C. Venous insufficiency during pregnancy. Rheological improvement by troxerutine. Revue Française de Gynecologie et d'Obstetrique 1991;86:206‐8. [PubMed] [Google Scholar]
Marastoni 1982 {published data only}
- Marastoni F, Crespi B, Montorsi M, Stefano A. A clinical and instrumental assessment of the effect of dihydroergotamine in lower extremity venous insufficiency. Archivio per le Scienze Mediche 1982;139(2):165‐74. [PubMed] [Google Scholar]
Marastoni 1982a {published data only}
- Marastoni F, Baldo A, Redaelli G, Ghiringhelli L. Centella asiatica extract in venous pathology of the lower limbs and its evaluation as compared with tribenoside. Minerva Cardioangiologica 1982;30(4):201‐7. [PubMed] [Google Scholar]
Menyhei 1994 {published data only}
- Menyhei G, Acsady G, Hetenyi A, Dubeaux D, Rado G. Chronobiology and clinical activity of daflon 500 mg in chronic venous insufficiency. Phlebology 1994;9 Suppl 1:15‐8. [Google Scholar]
Monreal 1994 {published data only}
- Monreal M, Callejas JM, Martorell A, Lisbona C, Lerma R. A prospective study of the long‐term efficacy of two different venoactive drugs in patients with post‐thrombotic syndrome. Phlebology 1994;9:37‐40. [Google Scholar]
Monreal 1997 {published data only}
- Monreal M, Callejas JM, Martorell A, Sahuquillo JC, Contel E. Prevention of post‐thrombotic syndrome with hidrosmina: a prospective pilot study. Phlebology 1997;12(1):21‐4. [Google Scholar]
Monteil‐Seurin 1993 {published data only}
- Monteil‐Seurin J. Lymphatic venous insufficiency: comparative study of Cyclo 3 Fort(TM) versus diosmin. Comptes Rendus de Therapeutique et de Pharmacologie Clinique 1993;11(109):3‐7. [Google Scholar]
Monteverde 1987 {published data only}
- Monteverde A, Occhipinti P, Rossi F, Vellata D. Comparison between Extract of Centella Asiatica and O‐(beta‐ hydroxyethyl) rutoside in the treatment of venous insufficiency of the lower limbs. Acta Therapeutica 1987;13(6):629‐36. [Google Scholar]
Morales 1993 {published data only}
- Morales CA, Barros RM. Efficacy and safety on use of dried horse chestnut extract in the treatment of chronic venous insufficiency of the limbs [Eficácia e segurança do extracto seco da semente de castanha‐da‐India no tratamento da insuficiencia venosa crônica de membros inferiores]. Revista Brasileira de Medicina 1993;50(11):1563‐5. [Google Scholar]
Muschietti 1978 {published data only}
- Muschietti B. [Clinical double blind trial with natural diosmin, synthetic diosmin and tribenoside]. Comparaison Clinique en Double Insu Entre la Diosmine Naturelle et Synthetique et le Tribenoside 1978;67:1449‐52. [PubMed] [Google Scholar]
Naser‐Hijazi 2004 {published data only}
- Naser‐Hijazi B, Gallenkemper G, Rieckemann B, Vanscheidt W. In contrast to its derivatives, coumarin does not influence prothrombin time: results from a randomised placebo‐controlled study. Phlebologie 2004;33(1):17‐22. [Google Scholar]
- Schmeck‐Lindenau HJ, Naser‐Hijazi B, Becker EW, Henneicke von HH, Schnitker J. Safety aspects of a coumarin‐troxerutin combination regarding liver function in a double‐blind placebo‐controlled study. International Journal of Clinical Pharmacology and Therapeutics 2003;41(5):193‐9. [DOI] [PubMed] [Google Scholar]
NCT01654016 {published data only}
- NCT01654016. Study of antiinflammatory effects of Detralex (Daflon). https://clinicaltrials.gov/ct2/show/NCT01654016 (accessed 9 September 2015).
NCT02191163 {published data only}
- NCT02191163. Efficacy of Antlstax In improving microcirculation of the skin in the leg in patients suffering from chronic venous insufficiency. https://clinicaltrials.gov/ct2/show/NCT02191163 (accessed 9 Sepember 2015).
NCT02191254 {published data only}
- NCT02191254. Efficacy and tolerablllty of Antlstax in male and female patients sufferlng from chronlc venous insufllclency. https://clinicaltrials.gov/ct2/show/NCT02191254 (accessed 9 September 2015).
NCT02191280 {published data only}
- NCT02191280. Antistax In patlents wlth chronlc venous insutflclency. https://clinicaltrials.gov/ct2/show/NCT02191280 (accessed 9 September 2015).
Neumann 1988 {published data only}
- Neumann HAM, Broek MTJB. Double blind study of the influence of O‐(beta‐hydroxyethyl)‐rutosides on the TcpO2 and LRR curve in patients with chronic venous insufficiency. International Angiology 1988;7(4):9. [Google Scholar]
Neumann 1990 {published data only}
- Neuman HAM, Broek MJTB. Evaluation of O‐(beta‐hydroxyethyl)‐rutosides in chronic venous insufficiency by means of non‐invasive techniques. Phlebology 1990;5 Suppl 1:13‐20. [Google Scholar]
Neumann 1995 {published data only}
- Neumann HAM, Broek MJTB. A comparative clinical trial of graduated compression stockings and O‐(beta‐hydroxy‐ethyl)‐rutosides (HR) in the treatment of patients with chronic venous insufficiency. Phlébologie 1995;24(3):78‐81. [PubMed] [Google Scholar]
- Neumann HAM, Broek MJTB. A comparative clinical trial of graduated compression stockings and O‐(beta‐hydroxyethyl)‐rutosides (HR) in the treatment of patients with chronic venous insufficiency. Zeitschrift fur Lymphologie 1995;19(1):8‐11. [PubMed] [Google Scholar]
Neumann‐Mangoldt 1979 {published data only}
- Neumann‐Mangoldt VP. Treatment of venous disorders of the lower extremities with Essaven‐capsules, results of a double blind trial. Fortschritte der Medizin 1979;97(45):2117‐20. [PubMed] [Google Scholar]
Nill 1970 {published data only}
- Nill HJ, Fischer H, Nill HJ, Fischer H. Comparative investigations concerning the effect of extract of horse chestnut upon the pressure‐volume‐diagram of patients with venous disorders. [German]. Arztliche Forschung 1970;24(5):141‐3. [PubMed] [Google Scholar]
Ottillinger 2001 {published data only}
- Ottillinger B, Greeske K. Rational therapy of chronic venous insufficiency‐‐chances and limits of the therapeutic use of horse‐chestnut seeds extract. BMC Cardiovascular Disorders 2001;1(1):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Paciaroni 1982 {published data only}
- Paciaroni E, Marini M. Topical therapy for phlebopathies. Results of a controlled clinical study. Policlinico ‐ Sezione Medica 1982;89:255‐64. [ID: 8761] [Google Scholar]
Partsch 1981 {published data only}
- Partsch H. Improvement of venous insufficiency with oral dehydroergotamine [Besserung der venosen insuffizienz durch orales dihydroergotamin]. Die Medizinische Welt 1981;32:1668‐71. [PubMed] [Google Scholar]
Paul 1983 {published data only}
- Paul V, Lange A. Benzarone in edema of the legs due to chronic venous insufficiency. Munchener Medizinische Wochenschrift 1983;125(16):343‐4. [PubMed] [Google Scholar]
Pauschinger 1987 {published data only}
- Pauschinger P. Clinical and experimental examination of the effect of horse‐chestnut extract on the transcapillary filtratrion and the intravasel volume in patients with chronic venous insufficiency [Klinisch experimentelle Untersuchungen zur Wirkung von Rosskastanien‐samenextrakt auf die transkapilläre Filtration und das intravasale Volumen an Parienten mit chronisch venöser Insuffizienz]. Phlebol Proktol 1987;16:57‐61. [Google Scholar]
Pecking 1998 {published data only}
- Pecking AP, Fevrier B, Wargon C, Pillion G. Efficacy of daflon 500 mg in the treatment of lymphedema (secondary to conventonal therapy of breast cancer) [Efficacite de daflon 500 mg dans le traitment du lymphoedeme (secondaire au traitement conventionnel du cancer du sein)]. Phlébologie 1998;51(4):519‐23. [Google Scholar]
Petruzzellis 1990 {published data only}
- Petruzzellis V, Quaranta D, Sacchetta AC, Candiani C. Therapeutic activity of O‐(beta‐hydroxyethyl)‐rutosides in acute superficial phlebitis in patients suffering from chronic venous insufficiency. Giornale Italiano di Angiologia 1990;10(2‐3):81‐91. [Google Scholar]
Petruzzellis 2002 {published data only}
- Petruzzellis V, Troccoli T, Candiani C, Guarisco R, Lospalluti M, Belcaro G, et al. Oxerutins (Venoruton): efficacy in chronic venous insufficiency ‐ a double‐blind, randomized, controlled study. Angiology 2002;53(3):257‐63. [DOI] [PubMed] [Google Scholar]
Pointel 1987b {published data only}
- Pointel JP, Got I, Ziegler OI, Fontaine M, Benedetti F, Drouin P, et al. Double‐blind controlled study of a combination of vitamin C, Ruscus aculeatus and Ribes nigrum anthocyanosides on capillary filtration in venous insufficiency [Essai controle en double insu d'une association vitamine C, ruscus aculeatus et anthocyanosides de ribes nigrum sur la filtration capillaire dans l'insuffisance veineuse]. Arteres et veines 1987;6(5):395‐7. [Google Scholar]
Pokrovskii 2005 {published data only}
- Pokrovskii AV, Sapelkin SV, Galaktionova LA, Fedorov EE. The assessment of medical therapy effectiveness of patients with lower limb chronic venous insufficiency: the results of prospective study with Ginkor Fort. [Russian]. Angiologiia i Sosudistaia Khirurgiia/Angiology and Vascular Surgery 2005;11(3):47‐52. [PubMed] [Google Scholar]
Pollastri 1982 {published data only}
- Pollastri M, Cipriani C, Barletta S, Borgioli A, Boscarino A, Tesi CU, et al. A clinical contribution to the pharmacology of chronic venous insufficiency: the effects of disodium flavodate. Gazzetta Medica Italiana 1982;141(4):153‐6. [Google Scholar]
Questel 1983 {published data only}
- Questel R, Walrant P. Randomized, placebo‐controlled trial of extracts of Ruscus aculeatus and Ribes nigrum plus ascorbic acid in venous insufficiency: Observation of microcirculation by conjunctival capillarography. Gazette Medicale de France 1983;90(6):508‐14. [Google Scholar]
Rabe 2011b {published data only}
- Rabe E, Stucker M, Esperester A, Schafer E, Ottillinger B. Efficacy and tolerability of a red‐vine‐leaf extract in patients suffering from chronic venous insufficiency ‐ results of a double‐blind placebo‐controlled study. European Journal of Vascular and Endovascular Surgery 2011;41(4):540‐7. [DOI] [PubMed] [Google Scholar]
Rehn 1993 {published data only}
- Rehn D, Golden G, Nocker W, Diebschlag W, Lehmacher W. Comparison between the efficacy and tolerability of oxerutins and troxerutin in the treatment of patients with chronic venous insufficiency. Arzneimittel‐Forschung 1993;43(10):1060‐3. [PubMed] [Google Scholar]
Rehn 1993b {published data only}
- Rehn D, Nocker W, Diebschlag W, Golden G. Time course of the anti‐oedematous effect of different dose regimens of O‐(beta‐hydroxyethyl) rutosides in healthy volunteers. Arzneimittel‐Forschung 1993;43(3):335‐8. [PubMed] [Google Scholar]
Rehn 1996 {published data only}
- Rehn D, Brunnauer H, Diebschlag W, Lehmacher W. Investigation of the therapeutic equivalence of different galenical preparations of O‐(beta‐hydroxyethyl)‐rutosides following multiple dose peroral administration. Arzneimittel‐Forschung 1996;46(5):488‐92. [PubMed] [Google Scholar]
Riccioni 2004 {published data only}
- Riccioni C, Sarcinella R, Izzo A, Palermo G, Liguori M. Effectiveness of Troxerutin in association with Pycnogenol in the pharmacological treatment of venous insufficiency. Minerva Cardioangiologica 2004;52(1):43‐8. [PubMed] [Google Scholar]
Rish 1972 {published data only}
- Rish L, Rodriguez JC. Effect of O‐(beta‐hydroxyethyl)‐rutosides on oedema in chronic venous insufficiency of the lower limb. A double blind trial. Angiologica 1972;9(1):62‐6. [DOI] [PubMed] [Google Scholar]
Roztocil 1977 {published data only}
- Roztocil K, Prerovsky I, Oliva I. The effect of hydroxyethylrutosides on capillary filtration rate in the lower limb of man. European Journal of Clinical Pharmacology 1977;11:435‐8. [DOI] [PubMed] [Google Scholar]
Roztocil 2003 {published data only}
- Roztocil K, Stvrtinova V, Strejcek J. Efficacy of a 6‐month treatment with Daflon 500 mg in patients with venous leg ulcers associated with chronic venous insufficiency. International Angiology 2003;22(1):24‐31. [PubMed] [Google Scholar]
Sadoun 1993 {published data only}
- Sadoun S, Allaert FA, Danel P, Mercier M. Venous and trophic disease, efficacy of chromocarbe diethylamine on functional and organic symptoms [Maladie veineuse et troubles trophiques, efficacite du chromocarbe diethylamine sur la symptomatologie fonctionnelle et organique]. Artères et Veines 1993;12(4):225‐32. [ ISSN 0293‐5090 ] [Google Scholar]
Sanctis 2001 {published data only}
- Sanctis MT, Cesarone MR, Incandela L, Belcaro G, Ricci A, Griffin M. Four‐week treatment with Essaven gel in diabetic microangiopathy‐‐a placebo‐controlled, randomized study. Angiology 2001;52 Suppl 3:S49‐55. [DOI] [PubMed] [Google Scholar]
Schmeck‐Lindenau 2003 {published data only}
- Schmeck‐Lindenau HJ, Naser‐Hijazi B, Becker EW, Henneicke von HH, Schnitker J. Safety aspects of a coumarin‐troxerutin combination regarding liver function in a double‐blind placebo‐controlled study. International Journal of Clinical Pharmacology and Therapeutics 2003;41(5):193‐9. [DOI] [PubMed] [Google Scholar]
Seydewitz 1992 {published data only}
- Seydewitz V, Berg D, Staubesand J, Welbers P. Impact of drug treatment on the activity of lysosomal enzymes in the wall of varicose veins [Einflub einer medikamentösen therapie auf die aktivität lysosomaler enzyme in der varikös veränderten Venenwand]. Phlebologie 1992;21(6):288‐92. [Google Scholar]
Stefanini 1996 {published data only}
- Stefanini L, Gigli P, Galassi A, Pierallini F, Tillieci A, Scalabrino F, et al. Pharmacologic treatment and/or balneotherapy of chronic venous insufficiency. Gazzetta Medica Italiana 1996;155(4):179‐85. [Google Scholar]
Stegmann 1987 {published data only}
- Stegmann W, Hubner K, Deichmann B, Muller B. Efficacy of O‐(beta‐hydroxyethyl)‐rutosides in the treatment of venous leg ulcers [L'efficacite des O‐(beta‐hydroxyethyl)‐rutosides dans le traitement de l'ulcere de jambe veineux]. Phlebologie 1987;40(1):149‐56. [PubMed] [Google Scholar]
Steiner 1986 {published data only}
- Steiner M, Hillemans HG. Tests for antiedema action of a vein drug. Münchener Medizinische Wochenschrift 1986;128(31):39. [Google Scholar]
Steiner 1990 {published data only}
- Steiner M. Investigation on the edema‐reducing and edema‐protective effect of horse chestnut seed extract. Phlebol Proktol 1990;19(5):239‐42. [Google Scholar]
Steiner 1992 {published data only}
- Steiner M. The Extent of the Edema Protective Effect of Horse Chestnut Seed Extract. Vol. 2, Paris: John Libbey Eurotext, 1992:715. [Google Scholar]
Steru 1988 {published data only}
- Steru D, Steru L. Evaluation clinique d'un phlebotrope: application a l'etude du veinamitol [Evaluation clinique d'un phlebotrope: application a l'etude du veinamitol]. Arteres et Veines 1988;7(4):362‐4. [Google Scholar]
Strauss 1992 {published data only}
- Strauss AL, Rieder H. Antiedematous effect of a drug combination in the orthostatic test. Phlebologie 1992;21(5):247‐51. [Google Scholar]
Strefezza 2010 {published data only}
- Strefezza EF. Comparative study of the formulations of diosmin/hesperidin and sachet in the treatment of the pain and edema of inferior members in the chronic venous disease [Portuguese]. Revista Brasileira de Medicina 2010;67(1‐2):21‐2. [Google Scholar]
Topalov 1990 {published data only}
- Topalov Y, Marinov H, Stanchev S. Troxesamol. Clinical application of the preparation in patients with vascular insufficiency of the lower extremities. Medico Biologie Information 1990;4(4):22‐5. [Google Scholar]
Tsukanov 2010 {published data only}
- Tsukanov IuT, Tsukanov AI, Vasilevich VV. Assessment of dose‐dependent effect during phlebotropic therapy of chronic diseases of lower‐limb veins. [Russian]. Angiologiia i Sosudistaia Khirurgiia/Angiology & Vascular Surgery 2010;16(3):71‐5. [PubMed] [Google Scholar]
Turio 2000 {published data only}
- Turio E, Romanelli M, Barachini P. Clinical arid instrumental evaluation of the efficacy of a vasoactive drug containing vitamin PP, vitamin C and phyto‐therapeutic extracts titrated in escin, bromelain and anthocyanosides for the treatment of varicose leg ulcers. Giornale Italiano di Dermatologia e Venereologia 2000;135(1):101‐5. [Google Scholar]
Weindorf 1987 {published data only}
- Weindorf N, Schultz Ehrenburg U. Controlled study of increasing venous tone in primary varicose veins by oral administration of Ruscus aculeatus and trimethylhespiridinchalcone. Zeitschrift fur Hautkrankheiten 1987;62:28‐38. [PubMed] [Google Scholar]
Widmer 1972 {published data only}
- Widmer LK, Glaus L, Raps E. Local treatment of leg disorders and chronic venous insufficiency. Double blind study of 55 patients. Schweizerische Rundschau fur Medizin Praxis 1972;61(42):1300‐4. [PubMed] [Google Scholar]
Zicot 1993 {published data only}
- Zicot M. Multicenter study of the efficacy and tolerance of naftazone (Mediaven 10 mg). Comparison of 2 dosage schemes. Revue Medicale de Liege 1993;48(4):224‐8. [PubMed] [Google Scholar]
Zuccarelli 1996 {published data only}
- Zuccarelli F. Evaluation of the effectiveness of Ginkor Fort on the symptoms of chronic venous insufficiency. Phlébologie 1996;49(1):105‐10. [Google Scholar]
References to ongoing studies
ISRCTN18841175 {published data only}
- ISRCTN18841175. Effects of micronised purified flavonoic fraction on microcirculation in women suffering from chronic venous disease. http://www.isrctn.com/ISRCTN18841175 (date accessed 28 October 2014).
NCT01532882 {published data only}
- NCT01532882. Efficacy and safety of Diosmin 600mg versus placebo on painful symptomatology in patients with chronic venous disease of lower limbs (EDEN). http://clinicaltrials.gov/show/NCT01532882 (date accessed 28 October 2014).
NCT01848210 {published data only}
- NCT01848210. Efficacy and safety of Coumarin and Troxerutin in the symptomatic treatment of chronic venous insufficiency. http://clinicaltrials.gov/ct2/results?term=NCT01848210 (date accessed 28 October 2014).
Additional references
ATC 2015
- Anatomical Therapeutic Chemical (ATC) system classification. http://www.whocc.no/atc_ddd_index/?code=C05 (accessed December 2015).
Aziz 2015
- Aziz Z, Tang WL, Chong NJ, Tho LY. A systematic review of the efficacy and tolerability of hydroxyethylrutosides for improvement of the signs and symptoms of chronic venous insufficiency. Journal of Clinical Pharmacy and Therapeutics 2015;40(2):177‐85. [DOI] [PubMed] [Google Scholar]
Behar 1988
- Behar A, Lagrue G, Cohen‐Boulakia F, Baillet J. Capillary filtration in idiopathic cyclic edema ‐ effects of Daflon 500 mg. Nuklearmedizin 1988;27(3):105‐7. [PubMed] [Google Scholar]
Boada 1999
- Boada JN, Nazco GJ. Therapeutic effect of venotonics in chronic venous insufficiency. A meta‐analysis. Clinical Drug Investigation 1999;18(6):413‐32. [Google Scholar]
Brand 1988
- Brand FN, Dannenberg AL, Abbott RD, Kannel WB. The epidemiology of varicose veins: the Framingham Study. American Journal of Preventive Medicine 1988;4(2):96‐101. [PubMed] [Google Scholar]
Carpentier 2000
- Carpentier PH. Epidemiology and physiopathology of chronic venous leg diseases. Revue du Praticien 2000;50(11):1176‐81. [PubMed] [Google Scholar]
Ciapponi 2004
- Ciapponi A, Laffaire E, Roque M. Calcium dobesilate for chronic venous insuffciency: a systematic review. Angiology 2004;55(2):147‐54. [DOI] [PubMed] [Google Scholar]
Clarke 2003
- Clarke M, Oxman AD, editors. Cochrane Reviewers’ Handbook [updated March 2003]. Oxford, UK: The Cochrane Library. The Cochrane Collaboration. Update Software; Issue 2, 2003.
DerSimonian 1986
- DerSimonian R, Laird N. Meta‐analysis in clinical trials. Controlled Clinical Trials 1986;7(3):177‐88. [DOI] [PubMed] [Google Scholar]
Diehm 1996b
- Diehm C. The role of oedema protective drugs in the treatment of chronic venous insufficiency: a review of evidence based on placebo‐controlled clinical trials with regard to efficacy and tolerance. Phlebology 1996;11(1):23‐9. [Google Scholar]
Eklöf 2004
- Eklöf B, Rutherford RB, Bergan JJ, Carpentier PH, Gloviczki P, Kistner RL, et al. American Venous Forum International Ad Hoc Committee for Revision of the CEAP Classification. Revision of the CEAP classification for chronic venous disorders: consensus statement. Journal of Vascular Surgery 2004;40(6):1248‐52. [DOI] [PubMed] [Google Scholar]
Evans 1999
- Evans CJ, Fowkes FG, Ruckley CV, Lee AJ. Prevalence of varicose veins and chronic venous insufficiency in men and women in the general population: Edinburgh Vein Study. Journal of Epidemiology and Community Health 1999;53(3):149‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro 2008 [Computer program]
- Brozek J, Oxman A, Schünemann H. GRADEpro Version 3.2 for Windows [GRADEpro. www.gradepro.org].]. Ontario, Canada: McMaster University, 2008.
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane‐handbook.org.
Higgins 2011b
- Deeks JJ, Higgins JPT, Altman DG, on behalf of the Cochrane Statistical Methods Group (editors). Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane‐handbook.org.
Ibañez 2000
- Ibañez L, Ballarín E, Vidal X, Laporte JR. Agranulocytosis associated with calcium dobesilate. Clinical course and risk estimation with the case‐control and the case‐population approaches. European Journal of Clinical Pharmacology 2000;56(9‐10):763‐7. [DOI] [PubMed] [Google Scholar]
Ibáñez 2005
- Ibáñez L, Vidal X, Ballarín E, Laporte JR. Population‐based drug‐induced agranulocytosis. Archives of Internal Medicine 2005;165(8):869‐74. [DOI] [PubMed] [Google Scholar]
Jadad 1996
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary?. Controlled Clinical Trials 1996;17(1):1‐12. [DOI] [PubMed] [Google Scholar]
Kaufman 1991
- Kaufman DW, Kelly JP, Levy Shapiro S. The Drug Ethiology of Agranulocytosis and Aplastic Anemia. New York: Oxford University Press, 1991. [Google Scholar]
Kurz 1999
- Kurz X, Kahn SR, Abenhaim L, Clement D, Norgren L, Baccaglini U, et al. Chronic venous disorders of the leg: epidemiology, outcomes, diagnosis and management. Summary of an evidence‐based report of the VEINES task force. Venous Insufficiency Epidemiologic and Economic Studies. International Angiology 1999;18(2):83‐102. [PubMed] [Google Scholar]
Markwardt 1996
- Markwardt F. Pharmacology of oedema protective drugs. Phlebology 1996;11(1):10‐5. [Google Scholar]
Nicolaides 2000
- Nicolaides AN. Cardiovascular Disease Educational and Research Trust. European Society of Vascular Surgery. The International Angiology Scientific Activity Congress Organization. International Union of Angiology. Union Internationale de Phlebologie at the Abbaye des Vaux de Cernay. Investigation of chronic venous insufficiency: a consensus statement (France, March 5‐9, 1997). Circulation 2000;102(20):E126‐63. [DOI] [PubMed] [Google Scholar]
Pittler 1998
- Pittler MH, Ernst E. Horse‐Chestnut seed extract for chronic venous insufficiency: a criteria‐based systematic review. Archives of Dermatology 1998;134(11):1356‐60. [DOI] [PubMed] [Google Scholar]
Pittler 2012
- Pittler MH, Ernst E. Horse chestnut seed extract for chronic venous insufficiency. Cochrane Database of Systematic Reviews 2012, Issue 11. [DOI: 10.1002/14651858.CD003230.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Porter 1995
- Porter JM, Moneta GL. Reporting standards in venous disease: an update. International Consensus Committee on Chronic Venous Disease. Journal of Vascular Surgery 1995;21(4):635‐45. [DOI] [PubMed] [Google Scholar]
Poynard 1994
- Poynard T, Valterio C. Meta‐analysis of hydroxyethylrutosides in the treatment of chronic venous insufficiency. Vasa 1994;23(3):244‐50. [PubMed] [Google Scholar]
Rabe 2013
- Rabe E, Guex JJ, Morrison N, Ramelet AA, Schuller‐Petrovic S, Scuderi A, et al. Treatment of chronic venous disease with flavonoids: recommendations for treatment and further studies. [Review]. Phlebology 2013;28(6):308‐19. [DOI] [PubMed] [Google Scholar]
Robertson 2014
- Robertson LA, Evans CJ, Lee AJ, Allan PL, Ruckley CV, Fowkes FG. Incidence and risk factors for venous reflux in the general population: Edinburgh Vein Study. European Journal of Vascular and Endovascular Surgery 2014;48(2):208‐14. [DOI] [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Higgins JPT, Vist GE, Glasziou P, Guyatt GH. Chapter 11: Presenting results and “Summary of findings” tables. Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of interventions Version 5.1.0. London, UK: The Cochrane Collaboration. www.cochrane‐handbook.org, 2011. [Google Scholar]
Scott 1995
- Scott TE, LaMorte WW, Gorin DR, Menzoain JO. Risk factors for chronic venous insufficiency: a dual case‐control study. Journal of Vascular Surgery 1995;22(5):622‐8. [DOI] [PubMed] [Google Scholar]
Spanish Min. Health
- Re‐evaluation of the risk‐benefit relationship of oral phlebotonic agents [Re‐evaluación de la relación benefico‐riesgo de los agentes flebotónicos para administración por vía oral]. http://www.hsanmillan.es/farma/flebotonicos.htm (accessed May 2005).
Stanhope 1975
- Stanhope JM. Varicose veins in a population of New Guinea. International Journal of Epidemiology 1975;4(3):221‐5. [DOI] [PubMed] [Google Scholar]
Tsouderos 1991
- Tsouredos Y. Venous tone: are the phlebotonics properties predictive of a therapeutic benefit? A comprehensive view of our experience with Daflon 500 mg. Zeitschrift fur Kardiologie 1991;80 Suppl 7:95‐101. [PubMed] [Google Scholar]
Van den Oever 1998
- Oever R, Hepp B, Debbaut B, Simon I. Socio‐economic impact of chronic venous insufficiency. An underestimated public health problem. International Angiology 1998;17(3):161‐7. [PubMed] [Google Scholar]
Vasquez 2010
- Vasquez MA, Rabe E, McLafferty RB, Shortell CK, Marston WA, Gillespie D, et al. Revision of the venous clinical severity score: venous outcomes consensus statement: special communication of the American Venous Forum Ad Hoc Outcomes Working Group. Journal of Vascular Surgery 2010;52(5):1387‐96. [DOI] [PubMed] [Google Scholar]
Wadworth 1992
- Wadworth AN, Faulds D. Hydroxyethylrutosides. A review of its pharmacology and therapeutic efficacy in venous insufficiency and related disorders. Drugs 1992;44(6):1013‐32. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Martinez 2001
- Martinez MJ, Bonfill X, Moreno RM, Cachà A, Vargas E, Capellà D. Phlebotonics for venous insufficiency. Cochrane Database of Systematic Reviews 2001, Issue 1. [DOI: 10.1002/14651858.CD003229] [DOI] [PubMed] [Google Scholar]
Martinez‐Zapata 2005
- Martinez‐Zapata MJ, Bonfill Cosp X, Moreno RM, Vargas E, Capellà D. Phlebotonics for venous insufficiency. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD003229.pub2] [DOI] [PubMed] [Google Scholar]


