Abstract
Background
Auditory integration therapy was developed as a technique for improving abnormal sound sensitivity in individuals with behavioural disorders including autism spectrum disorders. Other sound therapies bearing similarities to auditory integration therapy include the Tomatis Method and Samonas Sound Therapy.
Objectives
To determine the effectiveness of auditory integration therapy or other methods of sound therapy in individuals with autism spectrum disorders.
Search methods
For this update, we searched the following databases in September 2010: CENTRAL (2010, Issue 2), MEDLINE (1950 to September week 2, 2010), EMBASE (1980 to Week 38, 2010), CINAHL (1937 to current), PsycINFO (1887 to current), ERIC (1966 to current), LILACS (September 2010) and the reference lists of published papers. One new study was found for inclusion.
Selection criteria
Randomised controlled trials involving adults or children with autism spectrum disorders. Treatment was auditory integration therapy or other sound therapies involving listening to music modified by filtering and modulation. Control groups could involve no treatment, a waiting list, usual therapy or a placebo equivalent. The outcomes were changes in core and associated features of autism spectrum disorders, auditory processing, quality of life and adverse events.
Data collection and analysis
Two independent review authors performed data extraction. All outcome data in the included papers were continuous. We calculated point estimates and standard errors from t‐test scores and post‐intervention means. Meta‐analysis was inappropriate for the available data.
Main results
We identified six randomised comtrolled trials of auditory integration therapy and one of Tomatis therapy, involving a total of 182 individuals aged three to 39 years. Two were cross‐over trials. Five trials had fewer than 20 participants. Allocation concealment was inadequate for all studies. Twenty different outcome measures were used and only two outcomes were used by three or more studies. Meta‐analysis was not possible due to very high heterogeneity or the presentation of data in unusable forms. Three studies (Bettison 1996; Zollweg 1997; Mudford 2000) did not demonstrate any benefit of auditory integration therapy over control conditions. Three studies (Veale 1993; Rimland 1995; Edelson 1999) reported improvements at three months for the auditory integration therapy group based on the Aberrant Behaviour Checklist, but they used a total score rather than subgroup scores, which is of questionable validity, and Veale's results did not reach statistical significance. Rimland 1995 also reported improvements at three months in the auditory integration therapy group for the Aberrant Behaviour Checklist subgroup scores. The study addressing Tomatis therapy (Corbett 2008) described an improvement in language with no difference between treatment and control conditions and did not report on the behavioural outcomes that were used in the auditory integration therapy trials.
Authors' conclusions
There is no evidence that auditory integration therapy or other sound therapies are effective as treatments for autism spectrum disorders. As synthesis of existing data has been limited by the disparate outcome measures used between studies, there is not sufficient evidence to prove that this treatment is not effective. However, of the seven studies including 182 participants that have been reported to date, only two (with an author in common), involving a total of 35 participants, report statistically significant improvements in the auditory intergration therapy group and for only two outcome measures (Aberrant Behaviour Checklist and Fisher's Auditory Problems Checklist). As such, there is no evidence to support the use of auditory integration therapy at this time.
Keywords: Adolescent; Adult; Child; Child, Preschool; Humans; Young Adult; Acoustic Stimulation; Acoustic Stimulation/methods; Autistic Disorder; Autistic Disorder/therapy; Music Therapy; Music Therapy/methods; Randomized Controlled Trials as Topic
Plain language summary
Auditory integration therapy for autism spectrum disorders
People with autism spectrum disorders have difficulties with communication, behaviour and social interaction, and many also experience abnormal responses to sounds. The purpose of this review was to assess the evidence for the effectiveness of auditory integration therapy and therapies like it that have been developed to improve abnormal sound sensitivity and autistic behaviours in such individuals. Seven relatively small studies met the inclusion criteria for the review. These often measured different outcomes and reported mixed results. Benefits for participants receiving auditory integration therapy were only reported in two studies, involving 35 participants, for two outcomes. A study of Tomatis therapy did not measure behavioural outcomes and did not find any difference in language development between intervention and control groups. As such, there is no evidence to support the use of auditory integration therapy or other sound therapies at this time.
Background
Description of the condition
Autism spectrum disorders
Autism refers to a wide spectrum of associated cognitive and behavioural disorders and was first described in the 1940s (Kanner 1943). Core features include impairments in socialisation and verbal and nonverbal communication, and restricted patterns of behaviour (Filipek 1999). DSM‐IV (APA 1994) uses the term "Pervasive Developmental Disorders" to include autistic disorder, Rett's disorder, childhood disintegrative disorder, Asperger's disorder and Pervasive Developmental Disorder Not Otherwise Specified (PDD‐NOS). ICD‐10 has a similar but not identical diagnostic classification system (WHO 1993). More recently, the term autism spectrum disorders (ASD) has been developed because children with the abnormalities of communication, behaviour or social interaction seen in autism but who do not fulfil all the diagnostic criteria for autism have been identified. Most people agree that autism spectrum disorders encompass autistic disorder, Asperger's disorder, semantic‐pragmatic disorder (not included in DSM‐IV) and PDD‐NOS. Childhood disintegrative disorder and Rett's disorder are usually excluded from this grouping. Current practice requires that autism spectrum disorders are diagnosed using either the DSM‐IV (APA 1994) or ICD‐10 (WHO 1993) classification systems. Several diagnostic instruments have also been developed to assist with diagnostic classification. These include a behavioural assessment, the Autism Diagnostic Observation Schedule (ADOS) (Lord 1999); interview tools, the Autism Diagnostic Interview ‐ Revised (ADI‐R) (Lord 1994) and the Diagnostic Interview for Social and Communication Disorders (DISCO) (Wing 1999); and a computerised parent completed questionnaire, the 3Di (Skuse 2004), the Gilliam Autism Rating Scale(GARS) (Gilliam 1995) and the Childhood Autism Rating Scale (CARS) (Schopler 1980). ASD have been reported to affect between 0.7 to 21.1 per 10,000 children (Fombonne 1999). Currently there is no single known cause. Most experts would contend that autistic symptoms are the result of a variety of aetiologies affecting the developing brain (Gillberg 2000).
Abnormal responses to sensory stimuli
Abnormal responses to sensory stimuli (for example, ear covering or screaming, apparent deafness) may be the manifestations of auditory hypersensitivity or hyposensitivity. Such responses are important and are common characteristics encountered in autistic individuals. They do not, however, form part of the core criteria for diagnosis of an ASD. Abnormal responses to other stimuli (including visual perception, temperature or pain) can also be present (Gillberg 2000).
Description of the intervention
Types of therapy for autism spectrum disorders
Given the heterogeneity of ASD and the knowledge that there is no single known aetiology, a range of interventions and therapies have been developed. They include education interventions specifically addressing the core social and communication impairments of autism, pharmacological therapies and a wide range of 'alternative' therapies including diet, vitamins, auditory and sensory integration. Overall, educational and behavioural methods remain the mainstay of treatment (Barker 1995). Pharmacological treatments may be useful adjuncts to behavioural intervention in improving comorbid conditions in individuals with autism, for example, hyperactivity, aggression and obsessive‐compulsive behaviours. They do not necessarily influence the underlying primary social impairments (Gringras 2000). Many of the alternative therapies for autism are time‐consuming and expensive. Anecdotal reports of improvement or cure, however, have ensured their continuation despite a lack of clinical trial‐based evidence. One of these treatments involves a variety of sound or 'auditory integration' therapies. Types of this therapy are listed below.
Auditory integration training (Berard's method)
First developed in France in 1982 (Berard 1982), with a later English translation (Berard 1993), Berard postulated that abnormal sensitivity or insensitivity to certain frequencies of sound waves, regardless of overall hearing ability, was associated with a range of behaviour and learning problems (Berard 1993). Berard believed that his technique of auditory integration training (AIT) would bring about a 're‐education' of the hearing process. No other explanations for how AIT is effective have been put forward. Berard, in most cases, reported an improvement in the behaviour or learning problems. He applied AIT to a variety of disorders including autism, depression, hyperactivity and learning difficulties. Personal accounts have attributed autistic symptoms such as stereotypies, lack of emotional response and inappropriate distress to distorted sensory input. AIT, believed to address abnormal sound sensitivity specifically, may theoretically improve the problem and hence the associated disabling symptoms. The technique gained wide popularity following the publication of Stelhi's book The Sound of a Miracle. A Child's Triumph over Autism, which reported the complete recovery of the author's daughter Georgie (diagnosed with autism and schizophrenia) following 10 hours of training in Berard's clinic (Stehli 1991). AIT involves 10 hours of listening to electronically modified music delivered by headphones during two half‐hour sessions each day for 10 days. The AIT device uses filtering to dampen the peak frequencies to which the individual is 'hypersensitive' and delivers sounds modulated by random dampening of high and low frequencies and intensities (Berard 1993).
Tomatis Method
Tomatis sound therapy, developed by Dr Alfred Tomatis, uses electronically modified human voice and music delivered via the "Electronic Ear" (Baumgaertel 1999). Programmes are individualised with the duration of therapy varying and breaks scheduled between treatment blocks.
Samonas Sound Therapy
Samonas therapy involves listening through headphones to filtered music, voice and sounds of nature recorded on compact discs. Therapy takes place under a therapist's supervision and also at home. The therapy was developed by Steinbach using the work of Tomatis (Boon 2011). The duration and frequency of treatment for each individual patient is at the discretion of the therapist and there are no specific guidelines.
How the intervention might work
In practice, all three methods of AIT involve listening to electronically modified music for varying periods of time and are intended to ameliorate auditory processing defects and improve concentration. Each therapist appears to be practising their own version of these methods and may modify treatment to suit the individual patient. This raises theoretical concerns as to whether such methods are comparable, due to the variation in intensity and exposure time. Nevertheless, most of the proponents of these therapies claim the same benefits. A wide range of disorders, including autism, learning difficulties, hyperactivity disorders and depression, have been addressed by the described methods of AIT.
Objectives
This systematic review aimed to identify, evaluate and, if appropriate, combine any evidence of the effects of AIT or other methods of delivering sound therapy in individuals with autism spectrum disorders.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials.
Types of participants
Adults or children with ASD. ASD included pervasive developmental disorders (as described in the DSM‐IV (APA 1994) and ICD‐10 (WHO 1993) or diagnosed using a standard diagnostic instrument) and excluded child disintegrative disorder and Rett's disorder.
Types of interventions
Auditory integration therapy (AIT) and other sound therapies that involved listening to music modified by filtering and modulation. Filtering involves attenuating sounds at selected frequencies and modulation refers to random alternating of high and low sounds (Berard 1993). Control groups could be from a waiting list or receive no treatment, usual therapy or a placebo equivalent.
Types of outcome measures
1. Cognitive ability 2. Core features of autism (i.e., social interaction, communication and behavioural problems) 3. Hyperacusis 4. Auditory processing 5. Behavioural problems 6. Attention and concentration 7. Activity level 8. Quality of life in both school and home environments 9. Adverse events Short‐, medium‐ and long‐term outcomes were measured (one month, three months and 12 months after therapy).
Types of measures included: 1. standardised diagnostic assessment instruments; 2. standardised communication assessments; 3. quality of life questionnaires; 4. behaviour scales.
Search methods for identification of studies
Typing errors found in the previous search strategies for MEDLINE, CINAHL and ERIC were corrected and all available years of these databases were searched for this update. Searches of the remaining databases were limited to the period following the date of the search for the previous review. The search strategies used for this update are in Appendix 1 and those used for the previous review are in Appendix 2.
Electronic searches
We searched the following databases: Cochrane Central Register of Controlled Trials (CENTRAL) (2010, Issue 2), part of The Cochrane Library, searched 29 September 2010; MEDLINE (1950 to September week 2, 2010) searched 27 September 2010; EMBASE (1980 to Week 38, 2010) searched 27 September 2010; CINAHL Plus (1937 to current) searched 20 September 2010; PsycINFO (1887 to current) searched 20 September 2010; ERIC (1966 to current) searched 27 September 2010; LILACS (1982 to current) searched 29 September 2010.
The aim of the search strategy was for high recall. No language restrictions were applied.
Searching other resources
We searched the reference lists of articles identified through the search strategy for further relevant publications. We contacted authors of the included trials about their research; however we did not specifically write to other known experts.
Data collection and analysis
Selection of studies
Two review authors (YS and NS) independently screened titles and abstracts from the search. We discarded articles that did not fulfil our inclusion criteria. We retrieved potentially relevant articles for full text assessment and data extraction.
Data extraction and management
We analysed data using Review Manager 4.2.2. We developed data extraction forms to collect information about study location, methods, participant characteristics (for example, age, gender), frequency of auditory integration training or other forms of sound therapy, and outcome measures. Two review authors (YS and NS) performed data extraction independently and disagreements were resolved by negotiation with a third review author (KW).
Assessment of risk of bias in included studies
Three review authors assessed the studies found prior to the latest search (according to old guidance) with additional information collected by each assessor about intention‐to‐treat analysis, standardisation and blinding of outcome assessment and per cent lost to follow‐up. Sufficient information was available from that assessment to allow recoding of the risk of bias based on the new criteria presented in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Two review authors (YS, NS) assessed the new included study (Corbett 2008), which was found by the most recent search, according to the latest guidance. The risk of bias assessment was summarised in Figure 1 as high, low or unclear risk for the following categories.
1.
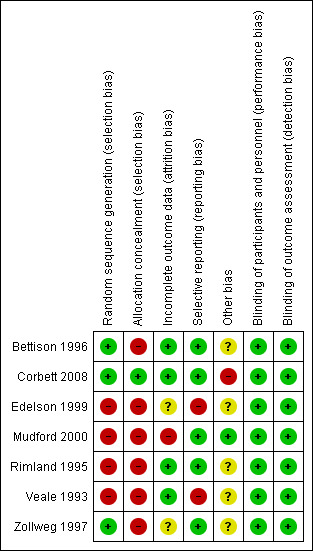
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
1. Random sequence generation and allocation concealment (selection bias). 2. Blinding of participants, personnel and outcome assessment (performance and detection bias). 3. Incomplete outcome data (attrition bias). 4. Selective reporting (reporting bias). 5. Other potential sources of bias (other bias).
Measures of treatment effect
All outcome data reported in the included papers were continuous. Our initial intention was to undertake meta‐analyses using mean difference and standard deviation to take into account differences between the treatment and control groups at baseline. These data were not provided by the authors. Where data were available, we calculated point estimates and standard errors from t‐test scores and post‐intervention means using Comprehensive Meta‐analysis software (Biostat).
Dealing with missing data
Where insufficient data were reported, we contacted researchers via email. Most authors were very willing to help with information about study methods and several provided additional data for outcome measures.
Assessment of heterogeneity
We assessed the consistency of results visually. This was supplemented with a test of homogeneity to determine the strength of evidence that the heterogeneity was genuine. Where heterogeneity was found, the review authors looked for an explanation.
Assessment of reporting biases
While the authors intended to use funnel plots to investigate any relationship between effect size and study precision, the number of studies was too small and the outcome measures used too inconsistent for this method to be viable.
Data synthesis
Meta‐analysis of the Aberrant Behavior Checklist (ABC) subscores was attempted using the inverse variance option and a random‐effects model with 95% confidence intervals. No other meta‐analysis was attempted because the studies used different outcome measures or data were not available in a usable form.
Subgroup analysis and investigation of heterogeneity
As meta‐analysis was not possible, subgroup analysis was not a viable option to assess the impact of planned subgroup analyses including participant inclusion criteria or differences in treatment administration.
Sensitivity analysis
As meta‐analysis was not possible, sensitivity analysis was not a viable option to assess the impact of study quality.
Results
Description of studies
See Characteristics of included studies and Characteristics of excluded studies.
Results of the search
Search results
A total of 278 titles and abstracts were reviewed for the initial publication (Figure 2) with a further 388 records reviewed for the current update (Figure 3). Of the databases searched, the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE, PsycINFO and ERIC yielded relevant abstracts, several of which were replicated between databases. There were no language restrictions for the search however all articles reviewed were written in English. The search strategy was translated into Spanish and Portuguese (in addition to English) for the LILACS database. Of the 278 titles and abstracts initially screened, 264 were not relevant to the review but had been identified by the wide search strategy. We reviewed the remaining 14 studies formally as full papers. We excluded 10 studies as they did not involve sound therapies or individuals with ASD, or were not RCTs. For the current update, we screened 388 titles and abstracts with one RCT of Tomatis therapy formally reviewed as a full paper and one review article of AIT excluded. We included seven trials in the final review, five of which were found via electronic searches as described above. We identified two additional studies from a review of reference lists and unpublished studies (see below). Six of seven included studies focused on AIT; we found one trial involving Tomatis therapy.
2.
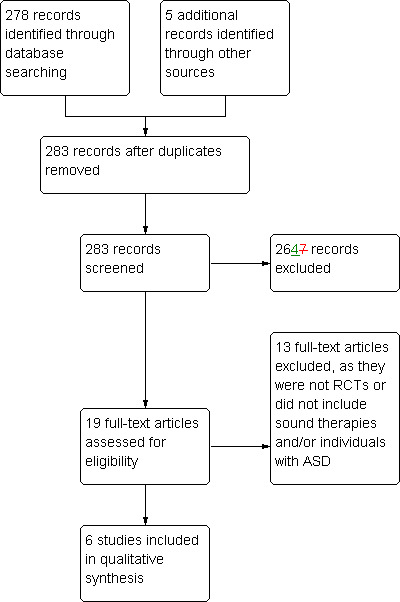
Study flow diagram: original search 2002
3.
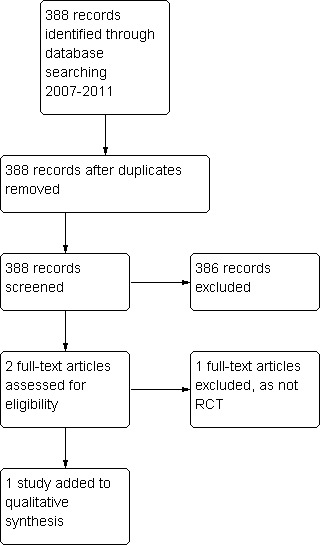
Study flow diagram for 2011 review update
Review of reference lists
Searching the reference lists of articles obtained for the background of the review yielded four studies. These were obtained from the reference lists of papers by Tharpe 1999 and Dawson 2000. Following assessment by two review authors, we excluded three studies because two were not RCTs (Rimland 1994; Gillberg 1997) and one (Yencer 1998) excluded people with autism spectrum disorders.
Unpublished studies
Information concerning relevant unpublished data was obtained from a health technology assessment report (Best 1997). One trial (Veale 1993) fulfilled our inclusion criteria.
Included studies
We included seven studies. The number of participants in the seven studies ranged from 10 (Veale 1993) to 80 (Bettison 1996); most studies had 20 or fewer participants (see the Characteristics of included studies table). Three of the studies included both children and adults (Rimland 1995; Zollweg 1997; Edelson 1999); while the remainder included only children aged three to 17 years (Veale 1993; Bettison 1996; Mudford 2000; Corbett 2008).
Different diagnostic definitions of autism were used for inclusion of participants. One study (Mudford 2000) confirmed diagnosis using DSM‐IV (APA 1994) and ICD‐10 classifications (WHO 1993), with another (Corbett 2008) using DSM‐IV (APA 1994) corroborated by the Autism Diagnostic Observation Schedule (ADOS) and clinical judgement. Two studies (Rimland 1995; Edelson 1999) used the Rimland Diagnostic E‐2 checklist as well as diagnosis from an independent source, for example, a physician or psychologist (Rimland 1971). Bettison confirmed that diagnoses were made by different means, which could not always be precisely determined as they were not made for the purposes of the study (Bettison 1996). Diagnosis was made by unspecified independent agencies in another trial (Veale 1993). The participants in the trial by Zollweg 1997 included 21 'cognitively impaired' individuals and nine autistic individuals. Communication with the author confirmed that all 30 participants would fulfil DSM‐IV criteria for an autism spectrum disorder however some had arrived in the institution prior to DSM‐IV (APA 1994).
The treatment period was uniform for all the AIT trials, consisting of AIT for 10 consecutive days with two 30‐minute sessions per day. Studies differed in regard to the machine model and type of music administered. Control conditions were generally the same across the included studies, that is, listening to unmodified music through headphones for the same time period as the treatment group. In one study (Mudford 2000) the music was played directly within the room for the control group, with non‐functional headphones. The study addressing Tomatis therapy (Corbett 2008) involved the Tomatis Method for four blocks lasting three weeks each, followed by a break for a total of 18 weeks. The placebo condition involved listening to commercially produced compact discs of the same music without an active microphone or the "Electronic Ear".
The outcome measures used in the studies varied considerably, as illustrated in the outcome measures table (Table 1). Five of the trials used the Aberrant Behaviour Checklist (ABC) as an outcome measure (Aman 1986). Three studies (Rimland 1995; Zollweg 1997; Mudford 2000) presented total and subgroup scores, with the remaining two studies including total scores only (Veale 1993; Edelson 1999). In four trials, the ABC was completed by the parents of participants, and in one (Zollweg 1997) the ABC was completed by staff at a residential institution. In the trial by Zollweg 1997, ABC data were collected on a 24‐hour basis by staff for one week at each post‐treatment interval and for four weeks during the pre‐treatment period. Data were collected monthly by parents and one teacher for the duration of the trial by Mudford 2000, except during vacation periods. The period the observers were reporting on was not stated. In three of the studies (Veale 1993; Rimland 1995; Edelson 1999), parents were asked, when completing the ABC, to consider the behaviour of the participant solely over the previous three days. Other outcome measures used in more than one trial included the Fisher's Auditory Problem Checklist (FAPC) (Fisher 1980), which was used in three trials (Veale 1993; Rimland 1995; Edelson 1999); the 'parent' version of the Conners' Rating Scales (Conners 1990), which was used in two trials (Veale 1993; Edelson 1999); the Leiter International Performance scale (Leiter 1980), which was used in two trials (Bettison 1996; Mudford 2000); and the Peabody Picture Vocabulary Test (Bettison 1996; Dunn 1997; Corbett 2008). In addition to standardised outcome measures, one study (Mudford 2000) used the investigators' direct observations of the participants' behaviour and reports by parents.
1. Outcome measures used in sound therapy trials.
| Outcome measure | Veale 1993 | Rimland 1995 | Bettison 1996 | Zollweg 1997 | Edelson 1999 | Mudford 2000 | Corbett 2008 |
| Aberrant Behaviour Checklist | ✔* | ✔* | ✔*** | ✔* | ✔*,** | ||
| Developmental Behaviour Checklist: parent, teacher (Einfeld 1995) |
✔ | ||||||
| Autism Behaviour Checklist | ✔ | ||||||
| Conners' Rating Scales ‐ Parent | ✔ | ✔ | |||||
| Nisonger Child Behaviour Rating Form ‐ Parent (Aman 1996) |
✔ | ||||||
| Fisher's Auditory Problems Checklist ‐ Parent | ✔ | ✔ | ✔ | ||||
| Leiter International Performance Scale | ✔ | ✔ | |||||
| Peabody Picture Vocabulary test | ✔† | ✔‡ | |||||
| Vineland Adaptive Behaviour Scores | ✔ | ||||||
| Reynell Language Developmental Scales III: a) expressive language b) comprehension |
✔ | ||||||
| Sensory problems checklist | ✔ | ||||||
| Hearing sensitivity questionnaire (HSQ) | ✔ | ||||||
| Sound sensitivity questionnaire (version of HSQ) | ✔ | ||||||
| Pure tone discomfort test | ✔ | ✔ | |||||
| Ear occlusion | ✔ | ||||||
| P300 event‐related brain potentials | ✔ | ||||||
| Loudness discomfort levels | ✔ | ||||||
| Autism Diagnostic Observation Schedule‐Generic | ✔ | ||||||
| Stanford‐Binet Intelligence Scale‐Fourth Edition | ✔ | ||||||
| Expressive One Word Vocabulary Test | ✔ |
* parent, ** teacher, *** other, † L, M forms, ‡third edition
Risk of bias in included studies
Allocation
Sequence generation
While all seven studies stated that participants were randomised to the treatment or control group, no information about sequence generation was reported in six of the published papers. Following contact with the authors (Bettison 2002 (pers comm); Edelson 2002 (pers comm); Mudford 2002 (pers comm); Zollweg 2002 (pers comm); Edelson 2003 (pers comm)), we judged that there was a high risk of bias for sequence generation for four of the studies, as defined by guidelines in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Randomisation based on telephone numbers was used in three studies (Veale 1993; Rimland 1995; Edelson 1999). The remaining study (Mudford 2000) used randomisation based alphabetically on each patient's initials, after dividing the children into geographical groups for transport convenience (Mudford 2002 (pers comm)). A random numbers table was used in three studies (Bettison 1996; Zollweg 1997; Corbett 2008).
Allocation concealment
Following contact with the authors (Bettison 2002 (pers comm); Edelson 2002 (pers comm); Mudford 2002 (pers comm); Zollweg 2002 (pers comm); Edelson 2003 (pers comm)), we judged that allocation was not adequately concealed for six studies. For one study (Corbett 2008), the sequence table was held in a sealed envelope in a locked filing cabinet until study completion (Corbett 2011).
Blinding
Outcomes assessors were reported to be blind to the intervention groups for all studies. In four of the included studies (Bettison 1996; Edelson 1999; Rimland 1995; Veale 1993), the principle investigators were not blinded to the intervention but had little or no interaction with the outcomes assessors (as described in the study or confirmed by personal communication with the authors). In these trials, blinding was not considered possible as the investigators needed to set and administer the treatment. In contrast, investigators were blinded in the studies by Zollweg 1997, Mudford 2000 and Corbett 2008.
Incomplete outcome data
The number of participants lost to follow‐up varied. Three studies (Veale 1993; Bettison 1996; Corbett 2008) did not report withdrawal of participants. Mudford 2000 recruited 21 children: five withdrew due to transportation or cooperation problems (24% loss to follow‐up). Loss to follow‐up was 6% for Rimland 1995, with one withdrawal due to transport problems. Results for one patient in the control group in the study by Edelson 1999 were not used (loss to follow‐up of 5%) as analyses were based on matched pairs. For Zollweg 1997, loss to follow‐up was 7% for the ABC as two patients left the institution prior to completion of the trial. There were significantly fewer participants for audiological and sound sensitivity data for two trials (Zollweg 1997; Edelson 1999) due to difficulties in obtaining reliable scores in the patient population. Intention‐to‐treat analysis was not used in four trials (Rimland 1995; Zollweg 1997; Edelson 1999; Mudford 2000).
Selective reporting (reporting bias)
We did not search for the study protocols to compare with the study publication; however, for all studies, the outcomes listed in the methods were reported in the results. Two studies reporting a significant treatment effect (Veale 1993; Edelson 1999) were considered to be at high risk of bias for selective reporting as the total scores for the Aberrant Behaviour Checklist but not the subscores were reported.
Other potential sources of bias
Study design
Five of the trials were parallel design and two (Mudford 2000; Corbett 2008) were cross‐over studies. The study by Mudford included a washout period of at least four months between treatments. For the study by Corbett, there was a period of three weeks between treatment rounds, based on the approach established by proponents of the Tomatis method (Corbett 2011). It is not certain whether a cross‐over design was appropriate or whether the washout period was adequate to minimise a carry‐over effect from the therapy.
Baseline imbalance
For the study by Corbett 2008, the authors report that "although the participants were randomly assigned to the groups, the developmental level appeared to be different for each in that the placebo/treatment group was higher functioning than the treatment/placebo group".
Effects of interventions
Information detailing methods of diagnosis of the participants, randomisation and recruitment was obtained from the authors. Where such data were unavailable in the papers, data relating to outcome measures including the Aberrant Behaviour Checklist (ABC) (Aman 1986), Conners' Rating Scales ‐ Parent (CRS) (Conners 1990) and Fisher's Auditory Problems Checklist (FAPC) (Fisher 1980) were sought at baseline, one month and three months post‐intervention. Only one study (Rimland 1995) reported outcomes in a format suitable for meta‐analysis.
We asked all other authors to provide summary statistics suitable for meta‐analysis or de‐identified raw data prior to publication of the first edition of this review. Data were provided by Edelson (Edelson 2003 (pers comm)) and Zollweg (Zollweg 2003 (pers comm)). We obtained summary statistics from Zollweg (Zollweg 1997) and Edelson (Rimland 1995; Edelson 1999) for the ABC at baseline and three months post‐intervention. Summary statistics were not provided by Mudford (Mudford 2000) or Veale (Veale 1993). Personal communication with a co‐author (Cullen 2003 (pers comm)) on Mudford et al's 2000 study (Mudford 2000) confirmed that limited time and resources made it difficult to access the requested information; while Veale (Veale 2003 (pers comm)) reported that further data analysis had not been performed due to controversy surrounding AIT therapy.
Results are presented for categories of outcome measures
The results for all outcomes are displayed by trial in Table 2.
2. Significance of results for outcomes used in sound therapy trials.
| Outcome | Trial | Tool(s) | Duration of follow‐up | Between group difference |
| Behaviour problems | Bettison 1996 | Autism Behaviour Checklist, Developmental Behaviour Checklist | 12 months | Improved both groups Not significant |
| Edelson 1999 | Aberrant Behaviour Checklist ABC)†, Fisher's Auditory Problems Checklist (FAPC), Conners' Rating Scales ‐ Parent | 3 months | Not significant for FAPC and Conners' Rating Scales, significant improvement for ABC for AIT group | |
| Mudford 2000 | Aberrant Behaviour Checklist‡, Nisonger Child Behaviour Rating Form ‐ Parent, observations from parents | 14 months | No significant improvement for combined behavioural data | |
| Rimland 1995 | Aberrant Behaviour Checklist‡, Fisher's Auditory Problems Checklist | 3 months | Significant improvement for AIT group for both tools (including 4 of 5 subscales of ABC) | |
| Veale 1993 | Fisher's Auditory Problems Checklist, Conners' Rating Scales ‐ Parent, Aberrant Behaviour Checklist† | 3 months | Not significant for all tools. | |
| Zollweg 1997 | Aberrant Behaviour Checklist‡ | 9 months | Improved both groups (including each ABC subscale) Not significant |
|
| Cognitive ability | Mudford 2000 | Leiter International Performance Scale and Vineland Adaptive Behaviour Scores | 14 months | Neither group improved for all tools |
| Bettison 1996 | Leiter International Performance Scale | 12 months | Both groups improved | |
| Corbett 2008 | Stanford‐Binet Intelligence Scale ‐ Fourth Edition | 9 months | Not applicable | |
| Sound sensitivity | Zollweg 1997 | "Loudness discomfort levels" | 9 months | Not significant |
| Bettison 1996 | Sound sensitivity questionnaire | 12 months | Not significant. Improved both groups |
|
| Rimland 1995 | Hearing sensitivity questionnaire and a "Pure Tone Discomfort test" | 3 months | Neither group improved | |
| Listening and comprehension | Rimland 1995 | Subgroup of Fisher's Auditory Problems Checklist | 3 months | Significant improvement for AIT group |
| Language | Corbett 2008 | Peabody Picture Vocabulary test, Expressive One Word Vocabulary Test | 9 months | Not significant for both tools |
| Bettison 1996 | Peabody Picture Vocabulary test | 12 months | Not significant | |
| Adverse events | Bettison 1996 | Parental questionnaire (non‐standardised) | 12 months | Not significant |
| Rimland 1995 | Parental questionnaire | 3 months | Not significant |
† Total scores presented for Aberrant Behaviour Checklist only, ‡ Total and subgroup scores for Aberrant Behaviour Checklist presented
Behavioural problems
All the trials used at least one standardised behaviour scale outcome. Of the five studies (Veale 1993; Rimland 1995; Zollweg 1997; Edelson 1999; Mudford 2000) which used the Aberrant Behavior Checklist (ABC) (Aman 1986), all published the total scores including group means or difference scores. The ABC consists of five subgroup scores. Communication with Dr Michael Aman (Aman 2003 (pers comm)), one of the authors of the Aberrant Behavior Checklist Manual, and review of the manual confirmed that the tool is not designed to calculate a total or grand mean score as the subscales are largely independent, therefore no meta‐analysis of total ABC scores was carried out. Two studies reported outcomes in a useable form for subgroup scores (Rimland 1995; Zollweg 1997) but the third study that reported subgroup analyses (Mudford 2000) did not present data suitable for inclusion in a meta‐analysis.
The largest trial (Bettison 1996) did not use the ABC as an outcome measure and instead used the Autism Behavior Checklist (Krug 1980), which is part of a broader tool, the Autism Screening Instrument for Educational Planning (ASIEP) (Krug 1978). The Autism Behavior Checklist is designed to be completed independently by a parent or a teacher familiar with the child, who then returns it to a trained professional for scoring and interpretation. Although it is primarily designed to identify children with autism within a population of school‐aged children with severe disabilities, the Autism Behavior Checklist has been used with children as young as three years of age. Using this instrument, Bettison 1996 reported an improvement in both groups, but no significant between‐group differences were found when the effects of group and time, and their interaction, were analysed. Rimland 1995 reported a significant improvement (P < 0.05) in the Fisher's Auditory Problems Checklist (FAPC) (Fisher 1980) scores for the treatment group, however data were not collected beyond three months follow‐up.
Veale 1993 reported no significant improvement for the Conners' Rating Scales ‐ Parent (Conners 1990), the FAPC (Fisher 1980) or the ABC (Aman 1986), only a "trending towards positive therapeutic effects"; again data were not collected beyond three months. Mudford 2000 used direct observational data in addition to behaviour rating scales. Overall combined data from parents, teachers and observers did not demonstrate a benefit with AIT. Further problems with data analysis occurred because of the reporting or supply of group means at baseline and post‐treatment, rather than mean differences. In the study by Zollweg (Zollweg 1997), where baseline and three month post‐intervention means were supplied, t‐tests of the between‐group differences at baseline were not significant (P = 0.06). As no data of this type were available for the other trials, it was not possible to assess how large the treatment group differences may have been at baseline. Meta‐analysis of changes in the ABC subgroup scores three months post‐intervention for two eligible studies (Rimland 1995; Zollweg 1997) was deemed inappropriate as inconsistency between these studies was high. This inconsistency may have been due to the many differences between the studies, notably participant characteristics, where Zollweg recruited institutionalised participants with known cognitive impairment (stating in a later personal communication that all participants would have met diagnostic criteria for autism (Zollweg 2002 (pers comm)) while Rimland recruited home‐based participants previously diagnosed with autism. Other differences included data collection: in one case this was undertaken by staff members over a period of a week (Zollweg 1997) and in the other by parents, who had been asked to focus on the previous three days only (Rimland 1995). Finally, data were presented by Zollweg at baseline and post‐treatment in the form of means, while point estimates were imputed from Rimland's reported t‐test scores.
No other outcomes for behavioural problems employed more than one consistently reported measure with data in a suitable form for meta‐analysis.
Cognitive ability
Both Bettison 1996 and Mudford 2000 used the Leiter International Performance Scale (LIPS) (Leiter 1980). Mudford also used the Vineland Adaptive Behaviour Scales (Sparrow 1984) and the Reynell Language Developmental Scales‐III (Edwards 1997). Mudford's trial did not report significant cognitive improvements for either the AIT or control groups after 14 months follow‐up, whereas Bettison described improvements for both groups at six and 12 months. All data were presented as group mean scores pre‐ and post‐intervention. Corbett 2008 used the Stanford‐Binet Intelligence Scale‐Fourth Edition (Thorndike 1986) to measure intellectual ability (IQ); however there was considerable variability in the IQ at baseline, making these data difficult to interpret.
Sound sensitivity
Rimland 1995, Bettison 1996 and Zollweg 1997 reported sound sensitivity outcomes. Zollweg measured 'loudness discomfort levels' and reported no significant differences between the groups. Similarly, Rimland, whose study included a 'Hearing Sensitivity Questionnaire' and a 'Pure Tone Discomfort Test' did not report any reduction in sound sensitivity for either group. Bettison described improvements for both groups using a 'Sound Sensitivity Questionnaire'. As these outcome measures were both diverse and non‐standardised, meta‐analysis was not possible.
Listening and comprehension
Rimland 1995 used a subgroup of the Fisher's Auditory Problems Checklist (Fisher 1980) to assess listening and comprehension at baseline and three months. Results were not useable in this review due to the small sample size and an analysis that focused on the ability of particular questions on the FAPC to detect improvement.
Language
Corbett 2008 measured single word vocabulary using the Peabody Picture Vocabulary test (Dunn 1997) and the Expressive one‐word picture vocabulary test (Brownell 2000) at baseline, the mid‐point and conclusion of the study. Both groups demonstrated an improvement in language skills over time regardless of the treatment condition, with no between‐group difference. Bettison 1996 used the Peabody Picture Vocabulary test (Dunn 1997) measured at baseline, three, six and 12 months after intervention, demonstrating significant improvement at three months for the AIT group and at 12 months for the control group. Data from the Corbett study were not extracted due to baseline differences between groups, despite random assignment, and therefore a meta‐analysis of the Peabody Picture Vocabulary test data for these two studies was not performed.
Adverse events
Two of the trials (Rimland 1995; Bettison 1996) sought to measure adverse effects of therapy. Both Bettison and Rimland asked parents to complete a checklist or questionnaire during the 10 days of AIT therapy in order to collect information on possible side effects. Minor physical complaints were reported in both groups for both studies, and no significant differences were found between groups. Mudford 2000 mentioned minor side effects that were reported anecdotally by parents at the end of the study. Veale 1993, Zollweg 1997 and Edelson 1999 did not report the recording of adverse events in their trials. No study reported specific deterioration in behaviour measured on a standardised test.
Discussion
In this systematic review, data synthesis was limited by statistical and clinical heterogeneity. The studies reported a disparate range of clinical outcomes, many of which were used by only one study. Variation in statistical methods was common between studies and data were presented in forms that could not be converted for use in RevMan software.
The largest studies (Bettison 1996; Zollweg 1997) did not report a difference between treatment and control conditions. One small cross‐over trial (Mudford 2000) also reported no long‐term benefits of AIT. Although three small trials (Veale 1993; Rimland 1995; Edelson 1999) reported an improvement in Aberrant Behavior Checklist (ABC) scores in the AIT group at three months, the clinical relevance of these results is uncertain because the total score of the ABC is not, according to the instrument's developer, a clinically meaningful outcome (Aman 1986). The author of the instrument has stated that the use of a 'total aberrant score' is incorrect and inconsistent with the instrument's design. Results should be presented as the five subscale scores (Aman 1986). The only trial that used such subscales (Rimland 1995) did note an improvement in ABC subscale scores in the AIT group at three months. One small cross‐over study (Corbett 2008) addressed the effect of Tomatis therapy on language and demonstrated no difference between the treatment and placebo groups.
The age range of participants in this review was wide. It was not possible to analyse the results for different age groups, nor was this discussed in any of the studies. This is a concern because there is a general belief that early intervention is best, particularly in the case of language acquisition. Given that language skills are best acquired in young children, it is possible that greater improvements would be seen in a younger sample, or that improvements in language in younger participants might be masked by fewer gains in a generally older sample. Future research that measures language acquisition should be more specific about participant age. Likewise, duration of follow‐up is important for a 'lifetime' condition like autism, and in the trials included in this review it never exceeded 14 months (Mudford 2000).
We only found one small trial addressing Tomatis therapy (Corbett 2008). The failure to find any trials involving the use of other sound therapies for individuals with ASD further illustrates the paucity of peer‐reviewed information. Only one study (Bettison 1996), using two standardised behavioural checklists, performed a power analysis to calculate sample size and included a total of 80 participants. This study did not demonstrate a difference between the treatment and control conditions.
Berard 1993 did not specify the outputs intended for AIT. However, questions have been raised as to the potential harms of AIT (Lucker 1998), particularly regarding whether output levels of the machines exceed safe limits. Lucker 1998 concluded that AIT will not put listeners at risk of hearing loss provided practitioners use lower rather than maximal settings on the equipment. Four of the trial authors described the output used for their machines (Bettison 1996; Zollweg 1997; Edelson 1999; Mudford 2000) and described compliance with manufacturers' recommendations or adjustment to a comfortable level.
A statement issued by the American Academy of Pediatrics (Myers 2007), reaffirmed in 2010, endorsed the lack of benefit of AIT based on the Cochrane review (first published in 2004) and the methodological problems associated with the available research.There are also concerns about the validity and theoretical basis of the therapy (Gravel 1994). AIT continues to be practised worldwide (AIT institute 2011) despite evidence which still shows it to be an experimental treatment at best, and which may only be available at a considerable financial cost to the family.
Authors' conclusions
Implications for practice.
In the absence of evidence, the treatment must be considered experimental and care must be taken not to risk hearing loss. Parents need to be aware of the cost involved in pursuing these treatments.
Implications for research.
Given the lack of evidence that auditory integration training (AIT) or other sound therapies are effective as a treatment for autism, future research is discouraged. However, we suggest that any further trials of AIT should build on existing evidence and provide high level evidence about whether this treatment is effective for outcomes that are relevant to individuals with ASD.
To provide this level of evidence, future trials should: 1. use gold‐standard criteria for diagnosing autism, so that groups can be compared; 2. use sample sizes capable of detecting differences, if these exist; 3. use outcome measures that are valid and clinically meaningful; 4. present information in a way that is accepted for randomised control trials; 5. consider the effect of intellectual ability, age of participant at treatment, severity of symptoms and other potential subgroup variations so that clinically meaningful information is provided; 6. collect information about potential confounders, such as other therapy, so between‐group equivalence can be established.
Feedback
Response to the Review Article by Sinha, Silove, W
Summary
Response to the Review Article by Sinha, Silove, Wheeler and Williams (2004): Auditory Integration Training and Other Sound Therapies for Autism Spectrum Disorders Bernard Rimland and Stephen M. Edelson
Autism Research Institute, San Diego, California
We strongly disagree with the conclusions reached by Sinha, Silove, Wheeler and Williams (2004) in their review of the efficacy of auditory integration training (AIT) as a treatment for autism.
The present authors have recently completed a review of all 28 papers on the efficacy of AIT that we were able to find (January 1993 through August 2004). Twenty‐three reports concluded that AIT benefits various subgroups, three studies reported no benefit, or no benefit over that seen in the control group, and two studies reported rather ambiguous or contradictory results. In our view, the balance of the evidence clearly favors AIT as a useful intervention for autism. (Our review can be seen at www.AutismResearchInstitute.com.)
The review by Sinha et al. covered only 6 of the 28 studies referred to above. Our conclusions about each of these studies are diametrically opposed to the conclusions reached by Sinha et al. We will limit our discussion to these six studies:
All three studies which Sinha et al. claim to provide credible evidence that AIT is ineffective as a treatment for autism fail to do so:
Bettison (1996) could reach no valid conclusion about the efficacy of AIT because none of the measures of efficacy she employed was designed to nor capable of measuring treatment efficacy. (See Note 1 below)
The study by Mudford et al. (2000) was deeply flawed, as we called to Mudford's attention at the time. Mudford and his colleagues reported significant improvement in both the AIT and the placebo group. However, AIT starts a process that often takes a minimum of three months to produce significant results. The significant improvement seen in the "placebo" group could reasonably attributed to these subjects having received AIT in the first phase of the study, prior to the crossover. (See Note 2)
The Zollweg et al. study (1997)'s subject population included fewer than one‐third subjects who were autistic, the remainder being mentally retarded. This was established in a published interview in 1996 with David Palm, the senior researcher. No one has claimed AIT to be a treatment for mentally retarded individuals. (See Note 3)
The three studies which Sinha et al. claim to provide no credible evidence that AIT is effective do, in fact, support the efficacy of AIT:
Edelson et al. (1999), Rimland and Edelson (1995), and Veale (1993): These studies are considered to be of only marginal relevance by Sinha et al., on the grounds that the authors used the Total scores on the Aberrant Behavior Checklist (ABC), rather than the 5 subscale scores, since the 5 subscales are said to be largely independent. That is an invalid argument, akin to claiming that grade‐point average is not a valid measure of student achievement, since it is based on grades in such disparate courses as history, mathematics, philosophy, and geography. Clearly, since the 5 ABC subscales measure various aspects of aberrant behavior, persons with the highest Total scores may be said to exhibit the most aberrant behavior. We discussed this matter with Michael Aman, senior author of the ABC, in the early 1990s, and again more recently (August 12th, 2004). While Aman does prefer that the 5 subscale scores be used, he acknowledges the legitimacy of analyzing the Total scores. In the present instance, where the Total score shows significant differences between the treatment and control groups, he said the findings provided "compelling" evidence of the appropriateness of using the Total ABC score as an index of intervention effectiveness. Aman's annotated bibliography of ABC research (1993) cites, without criticism, our use of the Total score in one of our AIT studies (later published in 1995) that Sinha et al. reject on invalid grounds. (See Note 4)
The rejection by Sinha et al. of the above studies reporting positive results of AIT on the grounds that the authors used ABC Total scores, rather than ABC subtest scores, is inappropriate. We thus disagree with Sinha et al. not only in their conclusion that the studies by Bettison, Mudford and Zollweg serve to discredit AIT, but we also reject Sinha et al.'s conclusion that the studies by Edelson et al., Rimland and Edelson, and Veale fail to demonstrate the efficacy of AIT.
We therefore wish to reiterate the conclusion that we reached after our careful review of the 28 studies we were able to identify:
"Our review of the available literature on AIT has produced 23 studies with positive results and only 3 claiming no benefits from AIT. While none of the research done thus far on AIT is of Nobel Prize quality, the positive studies are far more credible than those with negative results. As we point out in our comments, the three studies that claimed no benefits are deeply flawed, with conclusions that are not supported by the research procedures nor the research data.
AIT does, in fact, appear to be a worthwhile, frequently beneficial intervention which confers improvement on a number of symptoms, in a significant proportion of disorders on the autism spectrum."
In concluding their negative evaluation of AIT, Sinha et al. commented that AIT "may only be available at considerable financial cost to the family." Again, we disagree: Guy Berard, who developed what is now called AIT (the present authors, BR and SME, coined the term 'Auditory Integration Training' or AIT) because Berard thought that a fast, low‐cost alternative treatment to the very expensive, long‐term Tomatis treatment was needed. Berard had been a student of Tomatis before he developed AIT as a short‐term, inexpensive alternative. The Berard AIT treatment is preferably administered in two 30‐minute sessions per day over a 10‐day period, at a cost of approximately $1000 (the cost varies).
In view of all of the above, what is an intelligent and concerned parent to do? We believe, as stated above, that there is sufficient evidence available to justify the continued practice of AIT, although we agree with Sinha et al. that more quality research is needed.
From a parent's viewpoint, their children are alive and growing now. Parents need information now. What is the best information available? Perfect information will never be available. To steer parents away from a safe, inexpensive intervention which is favored by the vast preponderance of available research is counterproductive counsel. A distinction must be made between "not proven to the nth degree" and "worth trying in view of the considerations of safety, cost and convenience." Our assessment, and our advice to parents is, accordingly "If you can afford it, give it a try!"
Note 1 ‐ Bettison (1996)
Bettison's results indicated significant improvement in both the experimental (AIT) and placebo groups, but no differences between the two groups. Bettison attributed these improvements to listening to music in a structured environment. However, critics have interpreted these findings as evidence of 'no benefits' associated with AIT, which is a debatable point.
While Bettison's study is exemplary in many respects, the instruments used to assess changes associated with AIT had severe shortcomings. Bettison (1996) used the Autism Behavior Checklist (Krug, Arick & Almond, 1980) to evaluate changes in behavior. In their review article, Sinha et al. stated that there were improvements in both the experimental (AIT) and placebo groups using this checklist, and there were no differences between the two groups. Sinha and her colleagues did acknowledge that the Autism Behavior Checklist was "primarily designed to identify children with autism," but they did not bring up the validity issue regarding the use of this checklist to evaluate treatment effectiveness. The first author of this checklist, Dave Krug, has stated that the checklist was not designed to evaluate treatment efficacy (Personal communication).
Bettison used a modified version of the Hearing Sensitivity Questionnaire (HSQ) designed by Rimland and Edelson (1991). The HSQ was designed only as a survey of sound sensitivity in the autism population and not as an instrument to evaluate treatment effectiveness. Rimland and Edelson did not use it as an assessment measure in any of their three studies on AIT. Additionally, Bettison employed a scoring method for the HSQ that was said to provide a measure of the person's degree of sound sensitivity. This scoring method lacks even face validity (i.e., the appearance that the checklist is valid). For example, if a parent agreed with the item: 'Have there been certain sounds which the person does not seem to hear?,' this response was considered an indication of hypersensitivity to sounds rather than hyposensitivity to sounds.
Another measure used in Bettison's study, the Developmental Behavior Checklist, had been used previously in clinical settings, but it also was not designed to measure treatment effectiveness.
Note 2 ‐ Mudford et al. (2000)
Although the significant improvements seen in those in the placebo condition were dismissed by Mudford et al., it is quite possible that these improvements may have been due to the subjects having received AIT eight months earlier (i.e., they may have participated in the AIT group prior to the crossover). This is a real possibility given: (a) the two areas of improvement in the placebo group are consistent with findings associated with AIT; and (b) Rimland and Edelson (1995) and Gillberg et al. (1998) have documented improvement up to 9 months following AIT. The present authors called this possibility to Mudford's attention and suggested that the data be reanalyzed to test it. Mudford refused, claiming that additional analyses of the data would increase the likelihood of error. On the contrary, reanalysis of the data would have decreased the likelihood of error.
Sinha and her colleagues also requested the data from the Mudford et al. study, but they were unable to obtain them. According to the guidelines in the American Psychological Association Publication Manual (2001, page 354), guidelines adopted by many scientific journals, researchers must make their published data available to other researchers for at least five years after the publication of their findings.
Note 3 ‐ Zollweg et al. (1997)
There are several severe problems with this study. First, the title should have stated
"… in a Mixed Population" since fewer than a third of the subjects were autistic. One cannot generalize these findings to the autism population. Neither Berard, nor any other responsible investigator, has proposed AIT as a treatment for mental retardation. Second, the volume level was much higher than recommended. The recommended volume level is 80 dB SPL or lower. The decibel level in the Zollweg et al. study was measured as high as 122 dB SPL. Finally, an analysis of the audiograms in their study indicated that 27% of the subjects were given the wrong narrow band filters. Given these methodological flaws, the Zollweg et al. findings are not applicable even to the mentally retarded population.
Sinha et al. stated: "Communication with the author confirmed all 30 participants would fulfill DSM‐IV criteria for an autism spectrum disorder, however some had arrived in the institution prior to DSM‐IV (APA 1994)." However, David Palm, the senior researcher in the study, stated that "the subjects were mildly to profoundly retarded, and some were autistic and had behavioral disturbances" (Gelman, 1996). The recent assertion made by one of the authors, seven years later, that the subjects were autistic, is not credible.
Note 4 ‐ Aman's concern is that by summing the scores across different subscales, an improvement on one subscale may cancel a worsening of behavior on another subscale. True, however, the other side of that coin is that if the Total score is not derived, one risks overlooking non‐significant changes on the subscales that would, in aggregate, reveal a significance between‐ group difference. The best answer: use both Total and subscale scores, as was done in the Rimland and Edelson (1995) study.
References
Aman, M.G. (1993). Annotated bibliography on the Aberrant Behavior Checklist (ABC). The Nisonger Center, Ohio State University, Columbus. Bettison, S. (1996). The long‐term effects of auditory training on children with autism. Journal of Autism and Developmental Disorders, 26, 361‐374. Edelson, S.M., & Rimland, B. The efficacy of auditory integration training: Summaries and critiques of 28 reports (January, 1993 to August, 2004). Paper published on the Internet at: www.AutismResearchInstitute.com Edelson, S.M., Arin, D., Bauman, M., Lukas, S.E., Rudy, J.H., Sholar, M., & Rimland B. (1999). Auditory integration training: a double‐blind study of behavioral, electrophysiological, and audiometric effects in autistic subjects. Focus on Autism and Other Developmental Disabilities, 14, 73‐81. Gelman, J. (1996, January 8). Reining in AIT: Clinicians call for stricter guidelines, more research. ADVANCE for Speech‐Language Pathologists & Audiologists, pp. 4 & 11. Gillberg, C., Johansson, M., Steffenburg, S., & Berlin, O. (1998). Auditory integration training in children with autism: Reply to Rimland and Edelson [Letter to the Editor]. Autism, 2, 93‐94. Krug, D. A., Arick, J.R., & Almond, P.J. (1980). Behavior checklist for identifying severely handicapped individuals with high levels of autistic behavior. Journal of Child Psychology and Psychiatry, 21, 221‐229. Mudford, O., Cross, B., Breen, S., & Cullen, C. (2000). Auditory integration training: No behavioural benefits detected. American Journal on Mental Retardation, 105, 118‐129. Rimland, B., & Edelson, S.M. (1991). Hearing sensitivity questionnaire. San Diego: Autism Research Institute. Rimland, B., & Edelson, S.M. (1994). The effects of auditory integration training in autism. American Journal of Speech‐Language Pathology, 5, 16‐24. Rimland, B., & Edelson, S.M. (1995). Brief report: A pilot study of auditory integration training in autism. Journal of Autism and Developmental Disabilities, 25, 61‐70. Sinha, Y., Silove, N., Wheeler, D., & Williams, K. (2004). Auditory integration training and other sound therapies for autism spectrum disorders. The Cochrane Library, 1, 2004. Chichester, UK: John Wiley & Sons, Ltd. Veale, T. (July, 1993). Effectiveness of AIT using the BCG device (Clark method): A controlled study. Paper presented at the World of Options International Autism Conference, Toronto, Canada. Zollweg, W., Vance, V., & Palm, D. (1997). The efficacy of auditory integration training: A double blind study. American Journal of Audiology, 6, 39‐47.
Bernard Rimland and I (Stephen M. Edelson) certify that we have no affiliations with or involvement in any organisation or entity with a direct financial interest in the subject matter of my criticisms.
Reply
We write in reply to Dr Edelson's comments. We believe his criticisms can be addressed under the following five areas:
1. Inclusion of data only from randomised controlled trials: Dr Edelson suggests that the findings from this review do not present a complete view of all evidence in favour of AIT as we present only data from randomised controlled trials (RCTs). Cochrane reviews typically include only data from RCTs because such trials are at lower risk of bias compared to study designs such as uncontrolled or unblinded cohort or case control studies. As such, RCTs provide data that is more likely to be valid. Of the 23 studies Dr Edelson refers to as supporting AIT to treat autism, 14 are uncontrolled or have no placebo group, two are single‐subject studies, two are animal studies, one is a survey and one uses children with central auditory processing disorder. Only two studies are randomised controlled trials and thus eligible for inclusion in our systematic review.
2. Inclusion of data from a mixed population: Dr Edelson states that the population detailed in the Zollweg 1997 study consisted of participants who may not have all been autistic. The participants did have multiple disabilities and the publication states their primary diagnosis based on DSM III criteria, that is, either autistic or cognitively impaired. In our communication with Prof Zollweg (15th August 2002) he states many participants arrived at the Chileda Institute, where the trial was conducted, prior to the DSM‐IV, and that "all subjects would have had a primary diagnosis of ASD". It is based on this information that this trial was included.
3. Problems with outcome measures: The authors of this review acknowledge that many of the tools used to assess treatment in the included trials are not designed for this purpose and may, therefore, not detect a clinically significant improvement. With the possible exception of the Aberrant Behaviour Checklist (see point 4), many of the tools used are essentially diagnostic or screening tools. However, the authors of the included trials used those tests available at the time. Systematic reviews can comment on limitations of existing studies but cannot change the outcome measures used. The lack of sensitive, validated tools to assess treatment effect in children and adults with autism is a legitimate problem in autism research. It results in the use of many different outcome measures both within and across RCTs. In this systematic review, six trials used 17 different outcome measures. Other systematic reviews in preparation further highlight this problem. More assessments and analysis performed in the pursuit of a positive treatment effect result in undermining the validity of a study's findings as this process increases the likelihood of type 1 error, that is, finding a positive result where no clinical improvement exists. It is crucial to the continued evaluation of treatments for autism that outcome measures be developed or re‐evaluated for their ability to assess change, the clinical importance of such change to carers and clinicians, and that consumers be involved in this process. Until this time, the use of multiple outcome measures remains inappropriate.
4. Aberrant Behaviour Checklist Total Scores: Dr Edelson contends that Dr Michael Aman, the author of the Aberrant Behaviour Checklist (Aman and Singh 1986) recently agreed with him that it was 'legitimate' to analyse total ABC scores. Our discussions with Dr Aman do not reflect this view. Dr Aman states that "the scale lacks validity if the subscales are not retained" (M. Aman, personal communication 1, 2nd December 2004)
Further, "the Manual [Aberrant Behaviour Checklist] has no norms for Total scores for a reason. We have published several normative and comparison studies and have never reported Total scores. I maintain an Annotated Bibliography on the ABC, which has about 145 studies summarized. Almost none of the studies included there have reported Total scores." (M Aman, personal communication 2, 2nd December 2004).
It is possible that differences resulting from treatment with AIT were not detected in any study because the ABC subscales used to assess change post treatment were not sufficiently sensitive. However, this problem cannot be resolved by adding the subscales to provide a total when the tool has not been designed or validated for this purpose. To do so increases the potential for type 1 error.
5. Cross‐over. We acknowledge the possibility of carry‐over of improvement from AIT treatment to the placebo group in cross‐over studies and believe there is not yet sufficient evidence to designate a defined wash‐out period of the effects of AIT. This is why results prior to cross‐over were sought and used where possible, and why meta‐analysis was not attempted when only cross‐over data were available.
The authors of this review made every attempt to access data from AIT and control groups prior to any cross‐over of treatment. Access to such data was not possible for the Mudford study. While this is unfortunate, there was no deliberate obstruction by trialists. The first author does not reside in the country where the data is stored, research staff have moved‐on due to funding constraints and data has been stored in an inaccessible place because of a paucity of working space.
However, the overall findings of the Mudford trial were included in the systematic review because we do not agree with Dr Edelson that there is sufficient documented improvement up to 9 months following AIT to dismiss the findings of this study based on potential carry‐over of improvement. The authors of one study cited by Dr Edelson to support this claim do not agree that their study shows either clinical or statistical improvement at nine months (Gillberg 1998).
All treatments have associated 'costs' including monetary expenditure (AIT currently costs $US1300 for a two‐session treatment block), change to life‐style, feelings of hope that may not be justified if treatments are not effective, and feelings of guilt, frustration and anger if treatments can not be accessed. We agree with Dr Edelson that parents of children and individuals affected by autism deserve best level evidence about treatment effectiveness so they can make well informed decisions about treatment options. Service providers also need this evidence to make informed decisions about prioritising treatments offered. We do not agree that the 'vast preponderance of available research' supports AIT. Our review shows that the best available evidence of treatment effect, RCTs, which used outcome measures to assess change in diagnostic features of autism and other behaviours, and incorporated parent reports, do not support AIT as an effective treatment for autism. Thus, AIT can not be recommended as an effective treatment at this time. This review will be updated to accommodate new evidence about treatment effectiveness if/when it becomes available.
References Aman M, Singh N (1986) Aberrant Behaviour Checklist; Manual. Slosson Educational Publications, New York Gillberg C, Johnasson M. Steffenburg S, Berlin O (1998) Autism 2:93‐94
Contributors
Drs Yashwant Sinha, Natalie Silove, Danielle Wheeler, and Katrina Williams
What's new
| Date | Event | Description |
|---|---|---|
| 2 November 2011 | New search has been performed | New search carried out. |
| 2 November 2011 | New citation required but conclusions have not changed | New study added. Author order changed. Risk of bias assessments brought in line with new guidance from Cochrane handbook. |
History
Protocol first published: Issue 2, 2002 Review first published: Issue 1, 2004
| Date | Event | Description |
|---|---|---|
| 12 September 2008 | Amended | Converted to new review format. |
| 31 May 2007 | Amended | Searches were rerun for this review in June 2007 prior to its inclusion in an 'umbrella review' published in 'Evidence Based Child Health' in 2008. No new studies were found. It is anticipated that a full update of this review will appear in 2009. |
| 12 January 2005 | Amended | The version of this review appearing in Issue 2, 2005, contains a criticism of the review made late in 2004 by Drs S Edelson and B Rimland. The authors have responded in full, and no substantive change has been made to the review as a result of the criticism received. |
| 9 September 2003 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
Danielle Wheeler who co‐authored the original review, including data extraction, statistical analysis and text. Dr Jon Deeks, University of Sydney, who provided advice and assistance with the meta‐analysis. Jane Dennis, Jo Abbott, Laura MacDonald and Margaret Anderson of the Cochrane Developmental, Psychosocial and Learning Problems Group. Authors involved in the trials: Dr Tina Veale, Dr Sue Bettison, Dr Stephen Edelson, Dr Bill Zollweg, Dr Oliver Mudford, Professor Blythe Corbett.
Appendices
Appendix 1. Search strategies September 2010
Cochrane Central Register of Controlled Trials (CENTRAL), part of The Cochrane Library
#1 MeSH descriptor Child Development Disorders, Pervasive explode all trees
#2 MeSH descriptor Speech Disorders explode tree 1
#3 autis*
#4 pdd
#5 pervasive developmental disorder*
#6 language NEAR delay*
#7 ((communicat* or speech) NEAR disorder*)
#8 (childhood NEXT schizophrenia)
#9 kanner*
#10 asperg*
#11 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10)
#12 MeSH descriptor Acoustic Stimulation explode tree 3
#13 (auditory NEXT (discriminat* or perception* or train*))
#14 (aural NEXT learn*)
#15 ((hearing or sound) NEXT therap*)
#16 (language NEXT acqui*)
#17 ((acoustic or auditory) NEXT stimulat* )
#18 listen* NEAR comprehen*
#19 (perceptual NEAR impair*)
#20 sensory near integrat*
#21 (tomatis or samonas)
#22 (#12 OR #13 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21)
#23 (#11 AND #22)
MEDLINE (Ovid)
1 exp Child Development Disorders, Pervasive/
2 pervasive development$ disorder$.tw.
3 exp Speech Disorders/
4 autis$.tw.
5 pdd.tw.
6 (language adj1 delay$).tw.
7 ((communicat$ or speech) adj1 disorder$).tw.
8 (childhood adj1 schizophrenia).tw.
9 kanner$.tw.
10 asperg$.tw.
11 or/1‐10
12 exp Acoustic Stimulation/
13 (auditory adj (discriminat$ or perception$ or train$)).mp.
14 (aural adj learn$).mp.
15 ((hearing or sound) adj therap$).mp.
16 (language adj3 acqui$).mp.
17 ((acoustic or auditory) adj stimulat$).mp.
18 (listen$ adj3 comprehen$).mp.
19 (perceptual adj3 impair$).mp.
20 (sensory adj integrat$).mp.
21 (tomatis or samonas).mp.
22 or/12‐21
23 11 and 22
24 randomized controlled trial.pt.
25 controlled clinical trial.pt.
26 randomi#ed.ab.
27 placebo$.ab.
28 drug therapy.fs.
29 randomly.ab.
30 trial.ab.
31 groups.ab.
32 or/24‐31
33 exp animals/ not humans.sh.
34 32 not 33
35 23 and 34
EMBASE (OVID)
1 autis$.tw.
2 pervasive developmental disorder$.tw.
3 PDD.tw.
4 (language adj3 delay$).tw.
5 (communicat$ adj3 disorder$).tw.
6 (speech adj3 disorder$).tw.
7 childhood schizophrenia.tw.
8 kanner$.tw.
9 asperg$.tw.
10 acoustic stimulat$.tw.
11 auditory stimulat$.tw.
12 (auditory adj (discriminat$ or perception$ or train$)).tw.
13 aural learn$.tw.
14 ((hearing or sound) adj3 therap$).tw.
15 (language adj3 acqui$).tw.
16 (listen$ adj3 comprehen$).tw.
17 (perceptual adj3 impair$).tw.
18 sensory integrat$.tw.
19 (tomatis or samonas).tw.
20 Clinical trial/
21 Randomized controlled trial/
22 Randomization/
23 Single blind procedure/
24 Double blind procedure/
25 Crossover procedure/
26 Placebo/
27 Randomi#ed.tw.
28 RCT.tw.
29 (random$ adj3 (allocat$ or assign$)).tw.
30 randomly.ab.
31 groups.ab.
32 trial.ab. (255303)
33 ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw.
34 Placebo$.tw.
35 Prospective study/
36 (crossover or cross‐over).tw.
37 prospective.tw.
38 or/20‐37
39 or/1‐9
40 or/10‐19
41 38 and 39 and 40
CINAHL Plus (EbscoHost)
S40 S25 and S39
S39 S26 or S27 or S28 or S29 or S30 or S31 or S32 or S33 or S34 or S35 or S36 or S37 or S38
S38 "cross over*"
S37 crossover*
S36 (MH "Crossover Design")
S35 (tripl* N3 mask*) or (tripl* N3 blind*)
S34 (trebl* N3 mask*) or (trebl* N3 blind*)
S33 (doubl* N3 mask*) or (doubl* N3 blind*)
S32 (singl* N3 mask*) or (singl* N3 blind*)
S31 (clinic* N3 trial*) or (control* N3 trial*)
S30 (random* N3 allocat* ) or (random* N3 assign*)
S29 randomis* or randomiz*
S28 (MH "Meta Analysis")
S27 (MH "Clinical Trials+")
S26 MH random assignment
S25 S23 and S24
S24 S13 or S14 or S15 or S16 or S17 or S18 or S19 or S20 or S21 or S22
S23 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 or S10 or S11 or S12
S22 TI (tomatis or samonas) Or AB (tomatis or samonas)
S21 TI(sensory integrat*) OR AB (sensory integrat*)
S20 TI(perceptual N3 impair*) or AB (perceptual N3 impair*)
S19 TI (language N3 acqui*) OR AB (language N3 acqui*)
S18 TI(hearing therap* or sound therap*) OR AB (hearing therap* or sound therap*)
S17 TI(aural learn*) or Ab(aural learn*)
S16 AB(auditory discriminat* or auditory percept* or auditory train*)
S15 TI(auditory discriminat* or auditory percept* or auditory train*)
S14 TI(auditory stimulat*) or AB(auditory stimulat*)
S13 TI(acoustic stimulat*) or AB(acoustic stimulat*)
S12 TI(asperg*) or AB(asperg*)
S11 TI(kanner*) or AB(kanner*)
S10 TI(childhood N3 schizophrenia) or AB (childhood N3 schizophrenia)
S9 TI (language N3 disorder*) or AB (language N3 disorder*)
S8 TI (speech N3 delay*) or AB (speech N3 delay*)
S7 TI (speech N3 disorder*) or AB (speech N3 disorder*) or TI (communicat* N3 disorder*) or AB (communicat* N3 disorder*)
S6 TI (language N3 delay*) or AB (language N3 delay)
S5 TI(pdd) or AB (pdd)
S4 TI (pervasive development* disorder* ) or AB(pervasive development* disorder* )
S3 TI (autis*) or AB(autis*)
S2 (MH "Speech Disorders+")
S1 (MH "Child Development Disorders, Pervasive") OR (MH "Asperger
Syndrome") OR (MH "Autistic Disorder") OR (MH "Schizophrenia, Childhood")
PsycINF0 (EbscoHost)
S40 S25 and S39
S39 S26 or S27 or S28 or S29 or S30 or S31 or S32 or S33 or S34 or S35 or
S36 or S37 or S38
S38 (evaluation N3 stud* or evaluation N3 research*)
S37 (effectiveness N3 stud* or effectiveness N3 research*)
S36 DE "Placebo" or DE "Evaluation" or DE "Program Evaluation" OR DE "Educational Program Evaluation" OR DE "Mental Health Program Evaluation"
S35 DE "Random Sampling" or DE "Clinical Trials" or DE "Experiment Controls”
S34 "cross over*"
S33 crossover*
S32 (tripl* N3 mask*) or (tripl* N3 blind*)
S31 (trebl* N3 mask*) or (trebl* N3 blind*)
S30 (doubl* N3 mask*) or (doubl* N3 blind*)
S29 (singl* N3 mask*) or (singl* N3 blind*)
S28 (clinic* N3 trial*) or (control* N3 trial*)
S27 (random* N3 allocat* ) or (random* N3 assign*)
S26 randomis* or randomiz*
S25 S13 and S24
S24 S14 or S15 or S16 or S17 or S18 or S19 or S20 or S21 or S22 or S23
S23 TI (tomatis or samonas) Or AB (tomatis or samonas)
S22 TI(sensory integrat*) OR AB(sensory integrat*)
S21 TI(perceptual N3 impair*) or AB (perceptual N3 impair*)
S20 TI (language N3 acqui*) OR AB(language N3 acqui*)
S19 TI(hearing therap* or sound therap*) OR Ab(hearing therap* or sound therap*)
S18 TI(aural learn*) or Ab(aural learn*)
S17 TI(auditory discriminat* or auditory percept* or auditory train*) or AB(auditory discriminat* or auditory percept* or auditory train*)
S16 TI(auditory stimulat*) or AB(auditory stimulat*)
S15 TI(acoustic stimulat*) or AB(acoustic stimulat*)
S14 DE "Auditory Perception" OR DE "Auditory Perception" OR DE "AuditoryAcuity" OR DE "Auditory Discrimination" OR DE "Auditory Localization" OR DE "Auditory Scene Analysis" OR DE "Loudness Perception" OR DE "Music Perception" OR DE "Pitch Perception" OR DE "Speech Perception"
S13 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 or S10 or S11 or S12
S12 TI(asperg*) or AB(asperg*)
S11 TI(childhood N3 schizophrenia) or AB (childhood N3 schizophrenia)
S10 TI (language N3 disorder*) or AB (language N3 disorder*)
S9 TI (speech N3 delay*) or AB (speech N3 delay*)
S8 TI (speech N3 disorder*) or AB (speech N3 disorder*) or TI (communicat* N3 disorder*) or AB (communicat* N3 disorder*)
S7 TI (language N3 delay*) or AB (language N3 delay*)
S6 TI(pdd) or AB (pdd)
S5 TI (pervasive development* disorder* ) or AB(pervasive development* disorder*)
S4 TI (autis*) or AB(autis*)
S3 (DE "Speech Disorders" OR DE "Language Disorders")
S2 TI (kanner*) or AB (kanner*)
S1 DE "Pervasive Developmental Disorders" OR DE "Aspergers Syndrome" OR DE "Autism" OR DE "Rett Syndrome"
ERIC (Dialog Datastar)
((auditory ADJ discrimination) OR (AUDITORY‐DISCRIMINATION.DE. OR AUDITORY‐STIMULI.DE. OR AUDITORY‐PERCEPTION.DE.) OR (Language‐Acquisition.DE.) OR (SENSORY‐INTEGRATION.DE.) OR (listening ADJ comprehension) OR (LISTENING‐COMPREHENSION.DE.) OR (( acoustic OR auditory ) NEAR stimul$) OR (auditory NEAR ( discriminat$ OR perception$ OR train$ )) OR (aural ADJ learn$) OR (( hearing OR sound ) NEAR therap$) OR (language NEAR acqui$) OR (listen$ NEAR comprehen$) OR (perceptual NEAR impair$) OR (sensory ADJ integrat$) OR (tomatis OR samonas))
AND
((Developmental‐Disabilities.DE.) OR (Autism.W..DE.) OR (Communication‐Disorders.DE.) OR (Delayed‐Speech.DE.) OR (pervasive ADJ developmental ADJ disorder$) OR (pdd) OR (language ADJ delay$) OR (( communicat$ OR speech ) ADJ disorder$) OR (childhood ADJ schizophrenia) OR (kanner$ OR asperg$))
AND
(Intervention.DE. OR Outcomes‐of‐Treatment.DE. OR EXPERIMENTAL‐GROUPS.DE. OR CONTROL‐GROUPS.DE. OR PROGRAM‐EFFECTIVENESS.DE. OR COMPARATIVE‐ANALYSIS.DE. OR EVALUATION.W..DE. OR EVALUATION‐METHODS.DE. OR random$ OR trial$ OR compar$ OR research$ OR evaluat$ OR outcome$ OR intervent$ OR effectiv$)
LILACS
(Mh autistic disorder or Mh asperger syndrome or Mh infantile autism or Tw autism or Tw autistic or Tw kanner$ or Tw asperger$) and (Mh Acoustic Stimulation or Mh auditory stimulation or Tw acoustic or Tw auditory or Tw sensory or Tw sound )
Appendix 2. Search strategies June 2007
Cochrane Central Register of Controlled Trials (CENTRAL)
1 CHILD‐DEVELOPMENT‐DISORDERS‐PERVASIVE*:ME 2 SPEECH‐DISORDERS*:ME 3 AUTIS* 4 (PERVASIVE and (DEVELOPMENTAL and DISORDER*)) 5 PDD 6 (LANGUAGE next DELAY*) 7 ((COMMUNICAT* next DISORDER*) or (SPEECH next DISORDER*)) 8 (CHILDHOOD next SCHIZOPHRENIA) 9 KANNER* 10 ASPERG* 11 (((((((((#1 or #2) or #3) or #4) or #5) or #6) or #7) or #8) or #9) or#10) 12 ((ACOUSTIC or AUDITORY) and STIMULAT*) 13 (AUDITORY and ((DISCRIMINAT* or PERCEPTION*) or TRAIN*)) 14 (AURAL next LEARN*) 15 ((HEARING or SOUND) and THERAP*) 16 (LANGUAGE near ACQUI*) 17 (LISTEN* near COMPREHEN*) 18 (PERCEPTUAL near IMPAIR*) 19 (SENSORY next INTEGRAT*) 20 TOMATIS or SAMONAS 21 (((((((#12 or #13) or #14) or #15) or #16) or #17) or #18) or #19) or #20) 22(#11 and #21)
MEDLINE (Ovid)
1 exp Child Development Disorders, Pervasive/
2 exp Speech Disorders/ (15285)
3 autis$.tw.
4 (pervasive and (developmental and disorder$)).tw.
5 pdd.tw.
6 (language adj1 delay$).tw.
7 ((comunicat$ or speech) adj1 disorder$).tw.
8 (childhood adj1 schizophrenia).tw.
9 kaner$.tw.
10 asperg$.tw.
11 or/1‐10
12 exp Acoustic Stimulation/
13 ((accoustic or auditory) adj stimulat$).tw.
14 (auditory adj (discriminat$ or perception$ or train$)).mp.
15 (aural adj learn$).tw.
16 ((hearing or sound) adj therap$).tw.
17 (language adj3 acqui$).mp.
18 (listen$ adj3 comprehen$).mp.
19 (perceptual adj3 impair$).mp.
20 (sensory adj intergrat$).mp.
21 (tomatis or samonas).mp.
22 or/12‐21
23 22 and 11
24 randomized controlled trial.pt.
25 controlled clinical trial.pt.
26 randomized controlled trials.sh.
27 random allocation.sh.
28 double blind method.sh.
29 single‐blind method.sh.
30 or/24‐29
31 (animal not human).sh.
32 30 not 31
33 clinical trial.pt.
34 exp clinical trials/
35 (clin$ adj25 trial$).ti,ab.
36 ((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).ti,ab.
37 Placebos.sh.
38 placebo$.ti,ab.
39 random$.ti,ab.
40 research design.sh.
41 or/33‐40
42 41 not 31
43 42 not 32
44 comparative study.sh.
45 exp evaluation studies/
46 follow up studies.sh.
47 prospective studies.sh.
48 (control$ or prospectiv$ or volunteer$).ti,ab.
49 or/44‐48
50 49 not 31
51 50 not (32 or 43)
52 32 or 43 or 51
53 23 and 52
EMBASE (Ovid)
1 autis$.tw.
2 pervasive developmental disorder$.tw.
3 PDD.tw.
4 (language adj3 delay$).tw.
5 (communicat$ adj3 disorder$).tw.
6 (speech adj3 disorder$).tw.
7 childhood schizophrenia.tw.
8 kanner$.tw.
9 asperg$.tw.
10 acoustic stimulat$.tw.
11 auditory stimulat$.tw.
12 (auditory adj (discriminat$ or perception$ or train$)).tw.
13 aural learn$.tw.
14 ((hearing or sound) adj3 therap$).tw.
15 (language adj3 acqui$).tw.
16 (listen$ adj3 comprehen$).tw.
17 (perceptual adj3 impair$).tw.
18 sensory integrat$.tw.
19 (tomatis or samonas).tw.
20 or/10‐19
21 Autism/
22 exp Speech Disorder/
23 (or/1‐9) or 22 or 22
24 20 and 23
25 clin$.tw.
26 trial$.tw.
27 (clin$ adj3 trial$).tw.
28 singl$.tw.
29 doubl$.tw.
30 trebl$.tw.
31 tripl$.tw.
32 blind$.tw.
33 mask$.tw.
34 ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw.
35 randomi$.tw.
36 random$.tw.
37 allocat$.tw.
38 assign$.tw.
39 (random$ adj3 (allocat$ or assign$)).tw.
40 crossover.tw.
41 40 or 39 or 35 or 34 or 27
42 exp Randomized Controlled Trial/
43 exp Double Blind Procedure/
44 exp Crossover Procedure/
45 exp Single Blind Procedure/
46 exp RANDOMIZATION/
47 42 or 43 or 44 or 45 or 46 or 41
48 24 and 47
CINAHL
1 autis$.tw.
2 (pervasive and (developmental and disorder$)).tw.
3 pdd.tw.
4 (language adj1 delay$).tw.
5 ((comunicat$ or speech) adj1 disorder$).tw.
6 (childhood adj1 schizophrenia).tw.
7 kaner$.tw.
8 asperg$.tw.
9 ((accoustic or auditory) adj stimulat$).tw.
10 (auditory adj (discriminat$ or perception$ or train$)).mp.
11 (aural adj learn$).tw.
12 ((hearing or sound) adj therap$).tw.
13 (language adj3 acqui$).mp.
14 (listen$ adj3 comprehen$).mp.
15 (perceptual adj3 impair$).mp.
16 (sensory adj intergrat$).mp.
17 (tomatis or samonas).mp.
18 exp Speech Disorders/
19 exp Autism/
20 exp Child Development Disorders/
21 or/1‐8
22 or/18‐20
23 or/21‐22
24 exp Rehabilitation of Hearing Impaired/
25 exp Sensory Motor Integration/
26 or/9‐17
27 or/24‐25
28 or/26‐27
29 28 and 23
30 randomi$.mp.
31 clin$.mp.
32 trial$.mp.
33 (clin$ adj3 trial$).mp.
34 singl$.mp.
35 doubl$.mp.
36 tripl$.mp.
37 trebl$.mp.
38 mask$.mp.
39 blind$.mp.
40 (34 or 35 or 36 or 37) and (38 or 39)
41 crossover.mp.
42 random$.mp.
43 allocate$.mp.
44 assign$.mp.
45 (random$ adj3 (allocate$ or assign$)).mp.
46 Random Assignment/
47 exp Clinical Trials/
48 exp Meta Analysis/
49 45 or 41 or 40 or 33 or 30 or 46 or 47 or 48
50 29 and 49
ERIC (Ovid)
1 exp developmental disabilities/
2 exp autism/
3 exp communication disorders/
4 exp delayed speech/
5 "PERVASIVE DEVELOPMENTAL DISORDER$".mp.
6 "PDD".mp.
7 language delay$.mp.
8 ((communicat$ or speech) adj disorder$).mp.
9 childhood schizophrenia.mp.
10 (kanner$ or asperg$).mp.
11 or/1‐10
12 exp auditory discrimination/ or exp auditory perception/ or exp auditory stimuli/
13 exp language acquisition/
14 exp sensory integration/
15 exp listening comprehension/
16 ((acoustic or auditory) adj3 stimul$).mp.
17 (auditory adj3 (discriminat$ or perception$ or train$)).mp.
18 (aural adj learn$).mp.
19 ((hearing or sound) adj3 therap$).mp.
20 (language adj3 acqui$).mp.
21 (listen$ adj3 comprehen$).mp.
22 (perceptual adj3 impair$).mp.
23 sensory intergrat$.mp.
24 (tomatis or samonas).mp.
25 or/12‐24
LILACS
(Pervasive developmental disorder$ or autism or autistic or childhood schizophrenia or kanner$ or asperg$)
AND
(accoustic stimulation or auditory stimulation or hearing therapy or sound therapy or sensory integration or language acquisition)
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bettison 1996.
| Methods | Randomised controlled trial. Randomisation by random numbers table Blinding: outcome assessors were blinded, investigator not blinded Duration: 12 mths | |
| Participants | Diagnosis: autism or Asperger syndrome diagnosed by an independent agency Age: 3‐17 years n=80 | |
| Interventions | 1. AIT: 2 30min sessions for 10 consecutive days 2. Control: as above, but music unmodified | |
| Outcomes | Standardised tests assessing behaviour, sensory measures and cognitive ability (see outcomes table) | |
| Notes | No loss to follow‐up | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Personal communication with study author (Bettison 2002): "a table of random numbers was used to allocate each child to either condition A or B." |
| Allocation concealment (selection bias) | High risk | Inadequate following communication with study author (Bettison 2002) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participant withdrawal |
| Selective reporting (reporting bias) | Low risk | Study protocol not available. Pre‐specified outcomes described in methods are reported in results |
| Other bias | Unclear risk | Financial support from the Commonwealth Department of Health, Housing and Community Services, an Apex Trust for Autism Grant and the Autistic Association of New South Wales |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Investigators not blinded. Personal communication with study author (Bettison 2002): blinding not possible as they needed to set and administer treatment. Parents and teachers unaware of which treatment each child was receiving |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcomes assessors blinded |
Corbett 2008.
| Methods | Randomised controlled trial (cross‐over) | |
| Participants | Diagnosis: autistic disorder based on DSM‐IV criteria, Autism Diagnostic Observation Schedule‐Generic (ADOS‐G) and clinical judgement Age: 3‐7 years n=11 |
|
| Interventions | 1. Tomatis Method: filtered music, "Electronic Ear" headphone, auditory feedback, specially produced compact discs of Mozart and Gregorian chants 4 three‐week treatment blocks, total duration: 18 weeks 2. Placebo: commercially produced Mozart and Gregorian chant compact discs, no active microphone or "Electronic Ear", schedule as for treatment group |
|
| Outcomes | Standardised tests assessing core features of autism, cognitive ability and language | |
| Notes | No loss to follow‐up | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation table provided by a independent statistician (personal communication with study author) |
| Allocation concealment (selection bias) | Low risk | Sequence table held in a sealed envelope in locked filing cabinet until study completion |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | Low risk | The outcomes listed in the methods are reported in the results |
| Other bias | High risk | The authors report that "although the participants were randomly assigned to the groups, the developmental level appeared to be different for each in that the placebo/treatment group was higher functioning than the treatment/placebo group." The study was a crossover design and it is unclear whether there was sufficient washout between each treatment period |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Parents blinded until conclusion of the study. Individuals administering the music were not blinded but were not affiliated with the M.I.N.D. institute (Corbett 2011) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | M.I.N.D. institute researchers remained blind until the conclusion of the study |
Edelson 1999.
| Methods | Randomised controlled trial. Randomisation based on telephone number Blinding: investigator not blinded, outcome assessors blinded. Duration: 3 months | |
| Participants | Diagnosis: autism Age: 4‐39 years n=18 | |
| Interventions | 1. AIT 2 30‐min sessions for 10 consecutive days 2. Control: as above, but music unmodified | |
| Outcomes | Standardised tests assessing behaviour, auditory problems, electrophysiological recordings (P300 ERP) | |
| Notes | Data from 1 control participant excluded due to no match in the AIT group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomisation based on telephone number |
| Allocation concealment (selection bias) | High risk | Inadequate, following communication with the author (Edelson 2002 (pers comm)) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Nil loss to follow‐up but results for one patient in the control group were not used as analyses were based on matched pairs. Only 5 participants able to complete electrophysiological tasks and audiometric assessments due to poor language and attention skills |
| Selective reporting (reporting bias) | High risk | Total scores presented for Aberrant Behaviour Checklist only |
| Other bias | Unclear risk | "A comparison of the pre‐assessment total scores (reflecting the number of behavioural or auditory problems) was conducted for all three questionnaires and indicated no a priori significant differences between the experimnetal (AIT) and the placebo groups)" however no raw data is provided Partial funding support provided by the Nancy Lurie Marks Charitable Trust |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Investigator provided processed or unprocessed music to each participant but "did not interact with parents, guardians or participants after group assignment was determined". Parents and guardians unaware of the group to which participants were assigned |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Evaluators unaware of group assignment for participants |
Mudford 2000.
| Methods | Randomised controlled trial (cross‐over) Methods: geographically divided into groups, then into subgroups alphabetically by the first letter of their name Blinding: investigators and outcomes assessors Duration: 14mths |
|
| Participants | Diagnosis: autism (DSM4 or ICD10) Age: 5.75‐13.92 years n=16 | |
| Interventions | 1. AIT: 2 30min sessions for 10 consecutive days 2. Control: as above, but headphones non‐functional and unmodified music played in the room (not through AIT device) | |
| Outcomes | Standardised tests assessing behaviour, language and cognitive ability, parental reports, observations by investigators | |
| Notes | 5 lost to follow‐up due to lack of cooperation, safety issues, transport problems | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Participants geographically divided into groups, then into subgroups alphabetically by the first letter of their name |
| Allocation concealment (selection bias) | High risk | Inadequate, following communication with the author (Mudford 2002 (pers comm)) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 5 of 21 participants (24%) lost to follow‐up due to lack of cooperation, safety issues, transport problems |
| Selective reporting (reporting bias) | Low risk | Pre‐specified outcomes described in methods are reported in results |
| Other bias | Low risk | Funded by a research grant from National Health Service Research and Development Programme for People with Physical and Complex Disabilities. Treatment providers (who assisted with the study) from Honormead Schools have ceased to provide auditory integration training |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Investigators blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcomes assessors blinded |
Rimland 1995.
| Methods | Randomised controlled trial. Randomised by last 2 digits of their telephone number Blinding: outcomes assessors blinded, investigator not blinded Duration: 3 months | |
| Participants | Diagnosis: autism Age: 4‐21 years n=17 | |
| Interventions | 1. AIT: 2 30 min sessions for 10 consecutive days 2. Control: as above, but music unmodified | |
| Outcomes | Standardised tests of behaviour, auditory problems | |
| Notes | 1 lost to follow‐up due to transport problems | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomisation sequence based on last 2 digits of telephone number |
| Allocation concealment (selection bias) | High risk | Inadequate, following communication with the author (Edelson 2002 (pers comm)) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1 lost to follow‐up due to transport problems |
| Selective reporting (reporting bias) | Low risk | The outcomes listed in the methods are reported in the results |
| Other bias | Unclear risk | "Funding was provided in part by the Adriana Foundation and the Alex Kunin Fund." |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Parents were blinded. Investigators not blinded as they were required to set and administer treatment. Investigators did not conduct pre‐ or post‐assessments |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcomes assessors blinded |
Veale 1993.
| Methods | Randomised controlled trial. Randomised by last 2 digits of their telephone number Blinding: investigators not blinded. Outcomes assessors blinded. Duration: 3 months | |
| Participants | Diagnosis: autism age: approx 6‐10 years n=10 | |
| Interventions | 1. AIT 2 30min sessions for 10 consecutive days 2. Control: as above, but music unmodified | |
| Outcomes | Standardised tests of behaviour, auditory problems | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomisation sequence based on last 2 digits of telephone number |
| Allocation concealment (selection bias) | High risk | Inadequate |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No loss to follow‐up |
| Selective reporting (reporting bias) | High risk | Total scores presented for Aberrant Behaviour Checklist only |
| Other bias | Unclear risk | Funding source for study not stated. Subjects were matched for age, sex and language level however raw data were not provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Parents unaware of treatment assignment of their child until completion of study. The investigator assigned children to groups and administered the therapy but did not conduct evaluations |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcomes assessors blinded |
Zollweg 1997.
| Methods | Randomised controlled trial. Randomised using a random numbers table Blinding: investigators and outcomes assessors blinded Duration: 9 months | |
| Participants | Diagnosis: cognitive impairment including autism spectrum disorder. Age: 7‐24 years n=30 | |
| Interventions | 1. AIT 2 30 min sessions for 10 consecutive days 2. Control: as above but music unmodified |
|
| Outcomes | Standardised tests of behaviour, sound sensitivity, measurement of pure tone thresholds | |
| Notes | 28 analysed for ABC at 9mths 22 analysed for loudness discomfort 14 analysed for pure tone thresholds | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table |
| Allocation concealment (selection bias) | High risk | Inadequate, following communication with study author (Zollweg 2002 (pers comm)) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 2 patients lost to follow‐up (1 from each group) prior to completion of study. There were fewer participants for audiological and sound sensitivity data due to illness or poor cooperation |
| Selective reporting (reporting bias) | Low risk | The outcomes listed in the methods are reported in the results |
| Other bias | Unclear risk | Treatment group included 9 cognitively impaired and 6 autistic patients, control group included 12 cognitively impaired and 3 autistic patients. Correspondence with author confirmed that all participants had been diagnosed with autism |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Investigators blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcomes assessors blinded |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| AAP 1998b | Not a randomised controlled trial (RCT). |
| Berkell 1996 | Not a randomised controlled trial (RCT). |
| Best 1997 | Not RCT. |
| Courchesne 1984 | A controlled trial involving measurement of event‐related brain potentials elicited by auditory stimuli (ie not AIT or sound therapy). Control group involved normal participants. |
| Fassler 1971 | A controlled trial involving "reduced auditory input" for autistic children rather than AIT or sound therapy. |
| Gillberg 1997 | Individuals with autistic disorder received AIT, however there was no control group. |
| Lincoln 1993 | A controlled trial which did not involve AIT or sound therapy. Participants in control group were not autistic. |
| Max 1997 | A controlled trial involving 'Virtual Reality' technologies rather than AIT or sound therapy. Control group were non‐autistic children. |
| Nober 1981 | A controlled trial which did not involve AIT or sound therapy. Participants in control group were not autistic. |
| Novick 1980 | A study that did not involve AIT or sound therapy and was not a RCT. |
| Rimland 1994 | AIT administered to individuals with autism, however there was no control group. Control group data from a previous study were used. |
| Smith 1985 | A RCT involving an 'auditory trainer' for autistic children rather than AIT or sound therapy. |
| Thaut 1987 | A controlled trial which did not involve AIT or sound therapy. Participants in control group were not autistic. |
| Yencer 1998 | A randomised controlled trial involving AIT administered to children with central auditory processing disorders. Children with autism spectrum disorders were excluded. |
Differences between protocol and review
This updated review was prepared using the Cochrane 'Risk of bias' tool with assessments of methodological quality from the original review updated in 'Risk of bias' tables using RevMan 5.1.
Contributions of authors
The updated review was jointly prepared by Yashwant Sinha, Natalie Silove, Andrew Hayen and Katrina Williams. Yashwant Sinha and Natalie Silove reviewed titles and abstracts and assessed the validity of papers with Katrina Williams. All authors contributed to the text of the review. Andrew Hayen provided advice and assistance with meta‐analysis.
Declarations of interest
Yashwant Sinha ‐ none known Natalie Silove ‐ none known Andrew Hayen ‐ none known Katrina Williams ‐ nNone known
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Bettison 1996 {published data only}
- Bettison S. The long‐term effects of auditory training on children with autism. Journal of Autism and Developmental Disorders 1996;26(3):361‐74. [DOI] [PubMed] [Google Scholar]
Corbett 2008 {published data only}
- Corbett BA, Shickman K, Ferrer E. Brief report: the effects of Tomatis Sound Therapy on language in children with autism. Journal of Autism and Developmental Disorders 2008;38(3):562‐6. [DOI] [PubMed] [Google Scholar]
Edelson 1999 {published data only}
- Edelson S, Arin D, Bauman M, Lukas S, Rudy J, Sholar M, et al. Auditory integration training: a double‐blind study of behavioural and electrophysiological effects in people with autism. Focus on Autism and Other Developmental Disabilities 1999;14(2):73‐81. [Google Scholar]
Mudford 2000 {published data only}
- Mudford O, Cross B, Breen S, Cullen C. Auditory integration training for children with autism: no behavioural benefits detected. American Journal on Mental Retardation 2000;105(2):118‐29. [DOI] [PubMed] [Google Scholar]
Rimland 1995 {published data only}
- Rimland B, Edelson S. Brief report: a pilot study of auditory integration training in autism. Journal of Autism and Developmental Disorders 1995;25(1):61‐70. [DOI] [PubMed] [Google Scholar]
Veale 1993 {unpublished data only}
- Veale T. Effectiveness of AIT using the BCG device (Clark method): a controlled study. World of Options International Autism Conference, Toronto, Canada (1993). Canada, 1993.
Zollweg 1997 {published data only}
- Zollweg W, Palm D, Vance V. The efficacy of auditory integration training: a double blind study. American Journal of Audiology 1997;6(3):39‐47. [Google Scholar]
References to studies excluded from this review
AAP 1998b {published data only}
- American Academy of Pediatrics: Committee on Children with Disabilities. Auditory integration training and facilitated communication for autism. Pediatrics 1998;102(2):431‐3. [PubMed] [Google Scholar]
Berkell 1996 {published data only}
- Berkell, DE, Malgeri, SE, Streit, MK. Auditory Integration Training for Individuals with Autism. ERIC database 1996;31(1):66‐70. [Google Scholar]
Best 1997 {published data only}
- Best L, Milne R. Auditory integration training in autism. DEC Report No. 66. Wessex Institute for Health Research and Development, University of Southampton, UK, 1997.
Courchesne 1984 {published data only}
- Courchesne E, Kilman B, Galambos R, Lincoln A. Autism: processing of novel auditory information assessed by event‐related brain potentials. Electroencephalography and Clinical Neurophysiology 1984;59(3):238‐48. [DOI] [PubMed] [Google Scholar]
Fassler 1971 {published data only}
- Fassler J, Bryant D. Disturbed children under reduced auditory input: a pilot study. Exceptional Children 1971;38(3):197‐204. [DOI] [PubMed] [Google Scholar]
Gillberg 1997 {published data only}
- Gillberg C, Johansson M, Steffenburg S, Berlin O. Auditory integration training in children with autism. Brief report of an open pilot study. Autism 1997;1(1):97‐100. [Google Scholar]
Lincoln 1993 {published data only}
- Lincoln A, Courchesne E, Harms L, Allen M. Contextual probability evaluation on autistic, receptive developmental language disoder, and control children: event‐related brain potential evidence. Journal of Autism and Developmental Disorders 1993;23(1):37‐58. [DOI] [PubMed] [Google Scholar]
Max 1997 {published data only}
- Max M, Burke J. Virtual reality for autism communication and education, with lessons from medical training simulators. In: KS Morgan, et al. editor(s). Medicine Meets Virtual Reality. Burke, Virginia,USA: IOS Press, 1997. [PubMed] [Google Scholar]
Nober 1981 {published data only}
- Nober E, Simmons J. Comparison of auditory stimulus processing in normal and autistics adolescents. Journal of Autism and Developmental Disorders 1981;11(2):175‐89. [DOI] [PubMed] [Google Scholar]
Novick 1980 {published data only}
- Novick B, Vaughan HG Jr, Kurtzberg D, Simson R. An electrophysiologic indication of auditory processing defects in autism. Psychiatry Research 1980;3(1):107‐14. [DOI] [PubMed] [Google Scholar]
Rimland 1994 {published data only}
- Rimland B, Edelson S. The effects of auditory integration training on autism. American Journal of Speech‐Language Pathology 1994;3(2):16‐24. [Google Scholar]
Smith 1985 {published data only}
- Smith D, McConnell J, Walter T, Miller S. Effect of using an auditory trainer on the attentional, language and social behaviours of autistic children. Journal of Autism and Developmental Disorders 1985;15(3):285‐302. [DOI] [PubMed] [Google Scholar]
Thaut 1987 {published data only}
- Thaut M. Visual versus auditory (musical) stimulus preferences in autistic children: a pilot study. Journal of Autism and Developmental Disorders 1987;17(3):425‐32. [DOI] [PubMed] [Google Scholar]
Yencer 1998 {published data only}
- Yencer K. The effects of auditory integration training for children with central processing disorders. American Journal of Audiology 1998;7(2):32‐4. [DOI] [PubMed] [Google Scholar]
Additional references
AIT institute 2011
- AIT Institute. Auditory Integration Training. http://www.aitinstitute.org/ait_international.htm (Accessed April 2011).
Aman 1986
- Aman M, Singh N. Aberrant Behaviour Checklist: Manual. New York: Slosson Educational Publications, 1986. [Google Scholar]
Aman 1996
- Aman MG, Tass EMJ, Hammer D, Rojahn J. The Nisonger CBRF: A child behavior rating form for children with developmental disabilities. Research in Developmental Disabilities 1996;17(1):41‐57. [DOI] [PubMed] [Google Scholar]
Aman 2003 (pers comm)
- Aman M. Re: Query re Aberrant Behaviour Checklist (personal communication). Email to Y Sinha. 24 June 2003.
APA 1994
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th Edition. Washington, DC: American Psychiatric Association, 1994. [Google Scholar]
Barker 1995
- Barker P. Chapter 11: Pervasive Developmental Disorders. Basic Child Psychiatry. Sixth. Cambridge: Blackwell Science, 1995:131‐144. [Google Scholar]
Baumgaertel 1999
- Baumgaertel A. Alternative and controversial treatments for attention deficit/hyperactivity disorder. Pediatric Clinics of North America 1999;46(5):977‐92. [DOI] [PubMed] [Google Scholar]
Berard 1982
- Berard G. Audition Égale Comportement. Sainte‐Ruffine: Maisonneuve, 1982. [Google Scholar]
Berard 1993
- Berard G. Hearing Equals Behaviour. New Canaan, Connecticut: Keats Publishing, 1993. [Google Scholar]
Bettison 2002 (pers comm)
- Bettison S. Personal communication. Email to Y Sinha 16 September 2002.
Boon 2011
- Boon R. Learning Discoveries Psychological Services: Samonas Sound Therapy. http://learningdiscoveries.com.au/non‐psychological‐interventions/samonas‐sound‐therapy/ (Accessed June 2011).
Brownell 2000
- Brownell R. Expressive One‐Word Picture Vocabulary Test. 3rd Edition. Novato: Academic Therapy Publications, 2000. [Google Scholar]
Conners 1990
- Conners CK. Manual for Conners Rating Scales. Toronto: Multi‐Health Systems Inc, 1990. [Google Scholar]
Corbett 2011
- Corbett, B. Re: Tomatis therapy publication for inclusion in systematic review [personal communication]. Email to: Y Sinha. 30th March 2011.
Cullen 2003 (pers comm)
- Cullen C. AIT systematic review (personal communication). Email to Y Sinha. 6 June 2003.
Dawson 2000
- Dawson G, Watling R. Interventions to facilitate auditory, visual and motor integration in autism: a review of the evidence. Journal of Autism and Developmental Disorders 2000;30(5):415‐21. [DOI] [PubMed] [Google Scholar]
Dunn 1997
- Dunn LM, Dunn LM. Peabody Picture Vocabulary Test (PPVT‐III). 3rd Edition. Circle Pines, MN, USA: American Guidance Service, 1997. [Google Scholar]
Edelson 2002 (pers comm)
- Edelson S. (personal communication). Email to Y Sinha. September 21 2002.
Edelson 2003 (pers comm)
- Edelson S. AIT results (personal communication). Email to Y Sinha. 9 May 2003.
Edwards 1997
- Edwards S, Fletcher P, Garman M, Hughes A, Letts C, Sinka I. The Reynell Developmental Language Scales III. Windsor: NFER‐Nelson, 1997. [Google Scholar]
Einfeld 1995
- Einfeld SL, Tonge BJ. The Developmental Behaviour Checklist: The development and validation of an instrument to assess behavioural and emotional disturbance in children and adolescents with mental retardation. Journal of Autism and Developmental Disorders 1995;25(2):81‐104. [DOI] [PubMed] [Google Scholar]
Filipek 1999
- Filipek PA, Accardo PJ, Baranek GT, Cook EH Jr, Dawson G, Gordon B, et al. The screening and diagnosis of autistic spectrum disorders. Journal of Autism and Developmental Disorders 1999;29(6):439‐84. [DOI] [PubMed] [Google Scholar]
Fisher 1980
- Fisher L. Fisher's Auditory Problems Checklist (FAPC). Cedar Rapids, IA: Grant Woods Area Education Agency, 1980. [Google Scholar]
Fombonne 1999
- Fombonne E. The epidemiology of autism: a review. Psychological Medicine 1999;29(4):769‐86. [DOI] [PubMed] [Google Scholar]
Gillberg 2000
- Gillberg C, Coleman M. Chapter 19: The neurology of autism. The Biology of Autistic Syndromes. 3rd Edition. London: MacKeith Press, 2000:291‐309. [Google Scholar]
Gilliam 1995
- Gilliam, JE. Gilliam autism rating scale. Austin, TX: Pro‐ed, 1995. [Google Scholar]
Gravel 1994
- Gravel J. Auditory integration training: placing the burden of proof. American Journal of Speech‐Language Pathology 1994;3:25‐9. [Google Scholar]
Gringras 2000
- Gringras P. Practical paediatric psychopharmacological prescribing in autism: the potential and the pitfalls. Autism 2000;4(3):229‐47. [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011] The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. Wiley.
Kanner 1943
- Kanner L. Autistic disturbances of affective conduct. Nervous Child 1943;2:217‐50. [Google Scholar]
Krug 1978
- Krug DA, Arick J, Almond P. Autism Screening Instrument for Educational Planning. Los Angeles: Western Psychological Services, 1978. [Google Scholar]
Krug 1980
- Krug DA, Arick J, Almond P. Behavior checklist for identifying severely handicapped individuals with high levels of autistic behavior. Journal of Child Psychology and Psychiatry 1980;21(3):221‐9. [DOI] [PubMed] [Google Scholar]
Leiter 1980
- Leiter 1980. Leiter International Performance Scale Instruction manual. revised. Wood Dale, IL: Stoelting, 1980. [Google Scholar]
Lord 1994
- Lord C, Rutter M, Couteur A. Autism diagnostic interview ‐ revised: a revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. Journal of Autism and Developmental Disorders 1994;24(5):659‐85. [DOI] [PubMed] [Google Scholar]
Lord 1999
- Lord C, Rutter M, DiLavore PC, Risi S. Autism Diagnostic Observation Schedule ‐ WPS. Los Angeles: Western Psychological Services, 1999. [Google Scholar]
Lucker 1998
- Lucker J. Is auditory integration training safe?. Journal of Autism and Developmental Disorders 1998;28(3):267‐8. [DOI] [PubMed] [Google Scholar]
Mudford 2002 (pers comm)
- Mudford O. Cochrane review on AIT (personal communication). Email to Y Sinha. 5 September 2002.
Myers 2007
- Myers SM, Johnson CP, American Academy of Pediatrics Council on Children with Disabilities. Management of children with autism spectrum disorders. Pediatrics 2007;120(5):1162‐82. [DOI] [PubMed] [Google Scholar]
Rimland 1971
- Rimland B. Diagnostic Checklist for Behavior‐Disturbed Children (Form E‐2). 1971. http://www.patientcenters.com/autism/news/diag_tools.html#ARI. San Diego: ARI (Autism Research Institute), (accessed November 2003).
Schopler 1980
- Schopler E, Reichler, RJ, DeVellis RF, Daly, K. Toward objective classification of childhood autism: Childhood Autism Rating Scale (CARS). Journal of Autism and Developmental Disorders 1980;10(1):91‐103. [DOI] [PubMed] [Google Scholar]
Skuse 2004
- Skuse D, Warrington R, Bishop D, Chowdhury U. Lau J, Mandy W, et al. The developmental, dimensional and diagnostic interview (3di): a novel computerized assessment for autism spectrum disorders. Journal of the American Academy of Child and Adolescent Psychiatry 2004;43(5):548‐58. [DOI] [PubMed] [Google Scholar]
Sparrow 1984
- Sparrow SS, Balla DA, Cicchetti DV. Vineland Adaptive Behaviour Scales: Interview edition: expanded form manual. Circle Pines, MN: American Guidance Service, 1984. [Google Scholar]
Stehli 1991
- Stehli A. The Sound of a Miracle. A Child's Triumph over Autism. New York: Doubleday, 1991. [Google Scholar]
Tharpe 1999
- Tharpe A. Auditory integration training: the magical mystery cure. Language, Speech and Hearing Services in Schools 1999;30(4):378‐82. [DOI] [PubMed] [Google Scholar]
Thorndike 1986
- Thorndike R, Hagen E, Sattler J. The Stanford‐Binet intelligence Scale. 4th Edition. Itasca: The Riverside Publishing Company, 1986. [Google Scholar]
Veale 2003 (pers comm)
- Veale T. Re: AIT review (personal communication). Email to Y Sinha 15 April 2003.
WHO 1993
- World Health Organization. The ICD‐10 Classification of Mental and Behaviour Disorders: Diagnostic Criteria for Research. Geneva: World Health Organisation, 1993. [Google Scholar]
Wing 1999
- Wing L. Diagnostic Interview for Social and Communication Disorders. 10th Edition. London: The National Autistic Society, 1999. [Google Scholar]
Zollweg 2002 (pers comm)
- Zollweg W. (personal communication). Email to J Dennis. 15 August 2002.
Zollweg 2003 (pers comm)
- Zollweg W. Re: Meta‐analysis of AIT (personal communication). Email to Y Sinha. 12 March 2003.


