
“Nothing captures the nature of health inequities as clearly as the persistent life expectancy gap between whites and blacks.”
—Alan R. Weil, JD, MPP (1)
The tragic higher coronavirus disease-2019 (COVID-19) mortality in African Americans (AAs) and other racial/ethnic minorities confirms inadequate societal efforts to eliminate disparities in cardiovascular disease (CVD) and is a sentinel event, highlighting deep-rooted U.S. health care failures. The Joint Commission defines a sentinel event as an unexpected occurrence resulting in death or serious physical or psychological injury, or the risk thereof (2). Conventionally identified sentinel events, such as unintended retention of foreign objects and fall-related events, are used to evaluate quality in hospital care. Similarly, disparate AA COVID-19 mortality reflects long-standing, unacceptable U.S. racial/ethnic and socioeconomic CVD inequities and unmasks system failures and unacceptable care to be caught and mitigated.
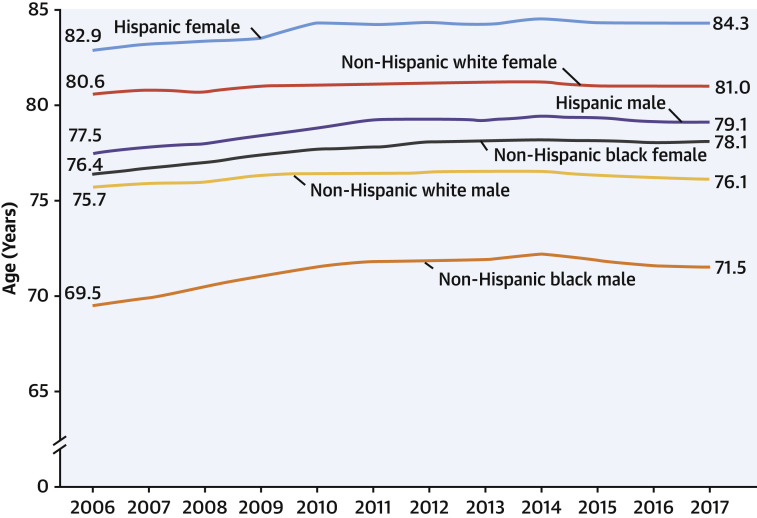
A toxic gumbo of CVD and environment profoundly diminishes overall AA life expectancy. Unfortunately, diminished AA life expectancy predates the COVID-19 pandemic for decades (3). The 1985 landmark Report of the Secretary’s Task Force on Black and Minority Health documented higher racial/ethnic mortality rates, and called such disparities “an affront both to our ideals and to the ongoing genius of American medicine” (3). Despite some progress, the groundbreaking Report’s national goal of reducing and eventually eliminating racial/ethnic disparities has not been realized. Primarily affected by CVD mortality, in 2017, the life expectancy for white women was 81.0 years compared with 78.1 years for black women and 76.1 to 71.5 years for men (Figure 1 ).
Figure 1.
Life Expectancy, by Race and Hispanic Origin and Sex: United States, 2006–2017
Arias E, Xu J. United States life tables 2017. Washington, DC: National Center for Health Statistics, 2017.
Although AAs appear to be infected more often, social determinants of health are powerful predictors of COVID-19 infectivity and mortality. The impact of COVID-19 goes well beyond the viral infection itself, reflecting the dynamics of a long-standing adverse host environment, including access to limited resources (i.e., money, food, education, health care, job flexibility), making disadvantaged communities more vulnerable in the pandemic. AAs and many people of color are more likely to provide high-risk essential services, including low-wage jobs that cannot be done remotely, and have fewer financial resources to draw on in the event of health problems or economic disruption. The underlying comorbid conditions, such as CVD, hypertension, diabetes, obesity, and asthma, are reflections of structural societal flaws beyond simply poor lifestyle choices, and ultimately lead to higher COVID-19 AA mortality in both urban and rural environments. People of color are neither genetically nor biologically predisposed to get COVID-19, but are socially prone to coronavirus exposure and have higher incidence of the very comorbidities fueling complications. Notably, minorities are more likely to be uninsured compared with non-Hispanic whites, and uninsured adults are less likely to have CVD risks controlled. The comorbidities that make COVID-19 more deadly are linked to the segregation and concentrated poverty that still mark these disparate communities. Hence, maintenance and continuity of CVD care during this crisis is absolutely required.
Impacts of CVD Risk
Mechanistically, patients with diabetes, often associated with obesity and hypertension, may be more susceptible to an inflammatory storm eventually leading to rapid progression and adverse prognosis of COVID-19 (4). Thus, effective control of these metabolic parameters may represent a specific and mechanistic approach to prevent and ameliorate the acute effects of COVID-19. Despite advancement in risk factor identification and availability of effective therapies, mortality associated with uncontrolled and more severe hypertension in AAs, with comorbid diabetes, is causal for stroke, heart failure, chronic kidney disease, and end-stage renal disease. Although hypertension is the most prevalent and potent risk factor in AAs (5), the COVID-19–hypertension link is not necessarily a causal relationship, because age is such a powerful risk for both conditions. Regardless, hypertension control remains an essential component of optimal health. Unfortunately, COVID-19 exposed the pernicious disparities in the health of our multiethnic society. Ahmad et al. (6) observed the correlation between poverty and heart failure outcomes, with lower socioeconomic status linked to increased CVD-related hospitalization and mortality.
For decades, American health care has failed minority communities in both primary and secondary CVD prevention. It is essential in this pandemic and in the future that clinicians ensure continuation of CVD medications, including antihypertensive agents, antiplatelets and anticoagulation medications, statins, and other lipid modifying agents, and if possible, prescribe 90-day supplies with sufficient refills.
COVID-19 Mortality in AAs
Recent national data demonstrate that 90% of hospitalized COVID-19 patients have some underlying condition (7). Disturbingly, higher mortality from COVID-19 has been locally documented in AA populations from New Orleans, Louisiana; Chicago, Illinois; Milwaukee, Wisconsin; Detroit, Michigan; and even rural Albany, Georgia. For example, 70% of the people who have died from coronavirus in Louisiana are black, a striking disparity for a state where AAs make up only 32% of the population (8). Similarly, AAs compromise 14% of the population in Michigan, but represent 40% of COVID-19 deaths, and like Louisiana, Michigan recently formed a task force to tackle racial COVID-19 disparities (9). The top 3 underlying conditions among COVID-19 Louisiana deaths are hypertension (59.76%), diabetes (38.10%), and chronic kidney disease (22.50%) (9). In view of a specific medical code for COVID-19, documenting racial/ethnic variations in testing and treatment is essential. Furthermore, once there is a vaccine, these surveillance data must be used to monitor disparities and identify discrimination.
Ring the Alarm: Immediate Positive Actions to Move Beyond COVID-19
The American College of Cardiology Cardiosmart COVID-19 materials (10) urge patients needing critical care for myocardial infarction or strokes to not delay due to COVID-19 fears or barriers. In addition, the Association of Black Cardiologists, with its long history of combating disparities, has initiated efforts to educate clinicians and the public about the pandemic’s effect in AAs’ diaspora and other underserved groups. Ultimately, to stave off future unnecessary loss of life, the COVID-19 crisis must be seen as an opportunity to finally fully address CVD disparities and the underlying structural factors (Table 1).
“Of all the forms of inequality, injustice in health is the most shocking and inhuman.”
—Dr. Martin Luther King (11)
Table 1.
Ring the Alarm: Immediate Positive Actions to Move Beyond COVID-19
| Targeted culturally-sensitive, literacy-level appropriate mitigation education: social distancing, masks, hand washing to minimize exposure risk |
| Mandated personal protection for essential service workers: custodial and clerical staff, mass transit operators, sanitation workers, food service workers |
| Financial protection and permanent insurance for presently noncovered workers |
| Targeted testing in crowded housing environments with limited ability to socially isolate |
| Testing beyond symptomatic individuals and development of walk-in facilities, considering disadvantaged persons may lack private automobiles for transportation |
| Testing essential workers and their family members for diagnosis and immunity as employment expands |
| Encourage team-approach telemedicine, including home blood pressure monitoring and home scales; encourage heart-healthy eating patterns and control CVD risk factors; and seek emergency care for CVD concerns outside of COVID-19 |
| Identify and suggest low-cost or free virtual physical activities online |
| Encourage thermometers and even pulse oximeters (although limited availability) to monitor COVID-19 status in affected patients |
| Support local and state task forces to correct racial/ethnic COVID-19 disparities |
COVID-19 = coronavirus disease-2019; CVD = cardiovascular disease.
Footnotes
Dr. Ferdinand has received a grant from Boehringer Ingelheim; and has served as consultant for Amgen, Sanofi, Boehringer Ingelheim, Quantum Genomics, Novartis, and Eli Lily. Dr. Nasser has reported that she has no relationships relevant to the contents of this paper to disclose.
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the JACCauthor instructions page.
References
- 1.Weil A.R. Disparities, hospital financing and more. Health Aff. 2016;35:1347. doi: 10.1377/hlthaff.2016.0890. [DOI] [PubMed] [Google Scholar]
- 2.Joint Commission . 2020. Sentinel event policy and procedures.http://www.jointcommission.org/Sentinel_Event_Policy_and_Procedures/ Available at: [PubMed] [Google Scholar]
- 3.Heckler M. U.S. Department of Health and Human Services; Washington, DC: 1985. Report of the Secretary's Task Force on Black & Minority Health. Vol. 4. [Google Scholar]
- 4.Bornstein S.R., Dalan R., Hopkins D. Endocrine and metabolic link to coronavirus infection. Nat Rev Endocrinol. 2020 Apr 2 doi: 10.1038/s41574-020-0353-9. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention African American Heart Disease and Stroke Fact Sheet. https://www.cdc.gov/nchs/fastats/black-health.htm Available at:
- 6.Ahmad K., Chen E.W., Nazir U. Regional variation in the association of poverty and heart failure mortality in the 3135 counties of the United States. J Am Heart Assoc. 2019;8 doi: 10.1161/JAHA.119.012422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garg S., Kim L., Whitaker M. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed coronavirus disease 2019 — COVID-NET, 14 states, March 1–30, 2020. MMWR Morb Mortal Wkly Rep. 2020 Apr 8 doi: 10.15585/mmwr.mm6915e3. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Louisiana Department of Health Coronavirus (COVID-19) http://ldh.la.gov/coronavirus Available at:
- 9.Kaiser Family Foundation Communities of color at higher risk for health and economic challenges due to COVID-19. https://www.kff.org/disparities-policy/issue-brief/communities-of-color-at-higher-risk-for-health-and-economic-challenges-due-to-covid-19/ Available at:
- 10.The American College of Cardiology Coronavirus disease 2019. CardioSmart. https://www.cardiosmart.org/coronavirus/ Available at:
- 11.King M.L. March 25, 1966. Address to the Medical Committee for Human Rights. Chicago, IL. [Google Scholar]