Abstract
The worldwide pandemic caused by the novel acute respiratory syndrome coronavirus 2 has resulted in a new and lethal disease termed coronavirus disease-2019 (COVID-19). Although there is an association between cardiovascular disease and COVID-19, the majority of patients who need cardiovascular care for the management of ischemic heart disease may not be infected with this novel coronavirus. The objective of this document is to provide recommendations for a systematic approach for the care of patients with an acute myocardial infarction (AMI) during the COVID-19 pandemic. There is a recognition of two major challenges in providing recommendations for AMI care in the COVID-19 era. Cardiovascular manifestations of COVID-19 are complex with patients presenting with AMI, myocarditis simulating an ST-elevation myocardial infarction (STEMI) presentation, stress cardiomyopathy, non-ischemic cardiomyopathy, coronary spasm, or nonspecific myocardial injury, and the prevalence of COVID-19 disease in the U.S. population remains unknown with risk of asymptomatic spread. This document addresses the care of these patients focusing on 1) the varied clinical presentations; 2) appropriate personal protection equipment (PPE) for health care workers; 3) role of the Emergency Department, Emergency Medical System and the Cardiac Catheterization Laboratory; and 4) Regional STEMI systems of care. During the COVID-19 pandemic, primary PCI remains the standard of care for STEMI patients at PCI capable hospitals when it can be provided in a timely fashion, with an expert team outfitted with PPE in a dedicated CCL room. A fibrinolysis-based strategy may be entertained at non-PCI capable referral hospitals or in specific situations where primary PCI cannot be executed or is not deemed the best option.
Key Words: acute myocardial infarction, COVID-19, emergency medical system, fibrinolysis, percutaneous coronary intervention, STEMI
Abbreviations and Acronyms: AMI, acute myocardial infarction; CCL, cardiac catheterization laboratory; COVID-19, coronavirus disease 2019; CT, computed tomography; D2B, door-to-balloon; ECG, electrocardiogram; ED, emergency department; EMS, emergency medical system; ICU, intensive care unit; NSTEMI, non-ST-elevation myocardial infarction; OHCA, out-of-hospital cardiac arrest; PCI, percutaneous coronary intervention; PPE, personal protective equipment; SARS-CoV-2, severe acute respiratory syndrome-coronavirus-2; STEMI, ST-elevation myocardial infarction
Introduction
The worldwide pandemic caused by the novel severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) has resulted in a new and lethal disease-termed coronavirus disease-2019 (COVID-19). Given the exponential growth of the disease, patients with COVID-19 may overwhelm the emergency department (ED), medical floors, intensive care unit (ICU) resources, personal protective equipment (PPE) supplies, and medical staff. Thus, health care systems are reducing elective procedures and surgeries to prepare for, and manage, infected patients. The United States now has the highest number of documented COVID-19 patients in the world, and it is likely that we will be managing patients with this disease over at least the next 12–18 months.
Patients with cardiovascular disease who develop COVID-19 have a higher risk of mortality (1, 2, 3, 4, 5, 6). However, it is important to emphasize that the majority of patients who need cardiovascular care for the management of ischemic heart disease, peripheral vascular disease, or structural heart disease may not be infected with this novel coronavirus. Furthermore, as we prepare for the care of patients with COVID-19-related illness, we also need to ensure that the overall patient population continues to benefit from the tremendous advancements in cardiovascular care made over the past three decades (7,8).
The objective of this document is to provide recommendations for a systematic approach for the care of patients with an acute myocardial infarction (AMI) during the COVID-19 pandemic. It is critical to: 1) inform the public that we can minimize exposure to the coronavirus so they continue to call the emergency medical system (EMS) for acute ischemic heart disease symptoms and therefore get the appropriate level of cardiac care that their presentation warrants; 2) target the use of primary percutaneous coronary intervention (PCI) or fibrinolysis (at referral or non-PCI-capable hospitals) in patients with ST-elevation myocardial infarction (STEMI) and aim to avoid reperfusion therapy for those with other causes of ST-segment elevation on the electrocardiogram (ECG); and 3) maximize the safety of medical personnel by appropriate masking of patients and the use of personal protection equipment (PPE).
Methods
The writing group for this statement has been organized to ensure diversity of perspectives and demographics, multistakeholder representation, and appropriate balance of relationships with industry. Policies from all three participating societies require that writing group members with a current financial interest are recused from participating in discussions or voting on relevant recommendations. The work of the writing group was supported exclusively by the Society for Cardiovascular Angiography and Interventions (SCAI) and the American College of Cardiology (ACC), nonprofit medical specialty societies, without commercial support.
The ACC, the American College of Emergency Physicians, and the SCAI endorsed the statement as official society guidance in April 2020. Consensus statements are primarily intended to help clinicians make decisions about treatment alternatives; clinicians also must consider the clinical presentation, setting, and preferences of individual patients to make judgments about the optimal approach.
There is a paucity of data to provide uniform recommendations. Observational studies from China and Europe have provided some guidance regarding the management of AMI in patients with COVID-19 (1, 2, 3, 4, 5, 6). This writing group has been convened to provide clinical guidance for AMI patients during the COVID-19 pandemic, taking into account the United States health care system. There is a recognition of two major challenges in providing recommendations for AMI care in the COVID-19 era:
-
1.
Cardiovascular manifestations in the COVID-19 patient are complex: patients may present with AMI, myocarditis simulating a STEMI presentation, stress cardiomyopathy, non-ischemic cardiomyopathy, coronary spasm, or myocardial injury without a documented Type I or Type II AMI (1, 2, 3, 4, 5, 6); and
-
2.
The prevalence of COVID-19 disease in the U.S. population remains unknown. In certain regions, community spread of SARS-CoV-2 is prevalent, and the sensitivity of testing is imperfect. Furthermore, patients testing positive for COVID-19 can be asymptomatic despite significant abnormalities noted on chest computed tomography (CT) scan and there appears to be significant risk of asymptomatic transmission of the disease (9,10).
Therefore, a balance must be struck in identifying appropriate patients for invasive approaches to AMI regardless of their COVID-19 status, and maintaining the safety of health care workers (HCWs) who might be exposed to the disease as well as minimizing contamination of cardiac catheterization laboratory (CCL) facilities. The need for additional patient evaluation might translate into some delays in reperfusion. A small study from Hong Kong examining the care of STEMI patients during the COVID-19 outbreak demonstrated a delay in symptom onset to medical contact times, suggesting that there may also be patient and/or systems-related delays in medical care during this pandemic (6). In addition, there has been a reduction in STEMI activations, reflecting a reluctance to seek medical attention or misdiagnoses given the focus on respiratory issues (11). Given this complexity, a reassessment of the current strategies for efficient and effective management of AMI during the COVID-19 pandemic is required. This is addressed with a focus on: a) clinical presentation including STEMI, cardiogenic shock, out-of-hospital cardiac arrest (OHCA), and non-STEMI; b) PPE for HCWs; c) role of the ED, EMS and CCL; and d) regional STEMI systems of care. We conclude with recommendations that balance the benefits and risks of invasive management of ischemic heart disease as well as health care team protections, anticipating these recommendations to be relevant during the entire period of the U.S. COVID-19 pandemic.
Clinical Presentations
3.1. Patients presenting with STEMI to a primary PCI center
Definite STEMI
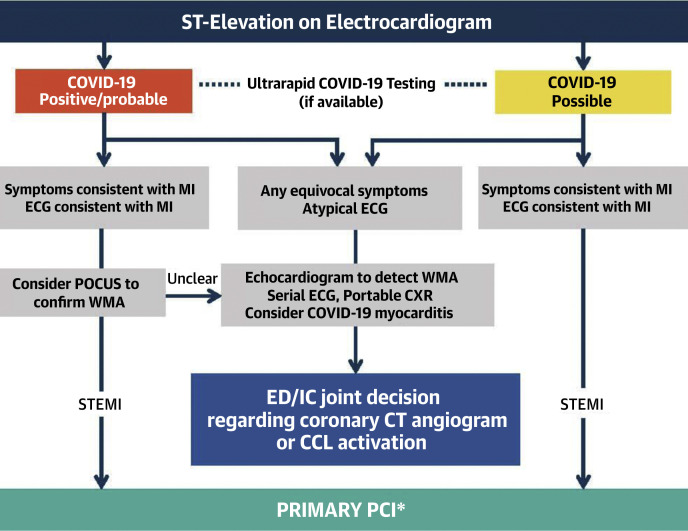
Primary PCI is the standard of care for patients presenting to PCI centers (within 90 min of first medical contact) (7). This should remain the standard of care for STEMI patients during the COVID-19 pandemic with some important caveats (Table 1 , Figures 1 and 2 ). Until we can firmly establish the prevalence of the disease in the general population of the country, all patients presenting with a suspected STEMI should be considered COVID-19 possible. With a primary PCI strategy, ED stays should be focused and patients should be transferred to the CCL as expeditiously as possible. Yet, additional time to establish an AMI diagnosis may be indicated (e.g., in some cases, echocardiography to assess for wall motion), and/or for COVID-19 status assessment and potential treatment (e.g., respiratory support).
Table 1.
Summary of Recommendations for the Care of Patients With Acute Myocardial Infarction During the COVID-19 Pandemic
|
|
|
|
|
|
|
|
CCL = cardiac catheterization laboratory; COVID-19 = coronavirus 2019; ED = emergency department; HCW = health care worker; ICU = intensive care unit; NCDR = National Cardiovascular Data Registry; PAPR = powered air-purifying respirator; PCI = percutaneous coronary intervention; PPE = personal protective equipment; STEMI = ST-elevation myocardial infarction.
Figure 1.
Care for ST Elevation on ECG at Primary PCI Center
In COVID-19 positive or probable patients, with classic clinical symptoms and ECG findings, a point of care ultrasound (POCUS) evaluation of cardiac function to assess for a regional wall motion abnormality (WMA) consistent with the ECG finding could be considered. Patients with classic clinical presentation and ECG finding consistent with a STEMI who are COVID-19 possible should proceed to primary PCI. Ultrarapid COVID-19 testing (if available) helps determine the use of a dedicated CCL and postprocedural hospital unit placement. With any equivocal symptoms or ECG findings, a transthoracic echocardiogram, portable chest X-ray and serial ECGs should help determine the need for invasive coronary angiography. In consultation between the emergency department and interventional cardiology, consideration to coronary computed tomography (CT) angiography or CCL activation can then be made. ∗Primary PCI should always be performed with the universal use of personal protection equipment (PPE) for aerosolized and droplet precautions for the entire CCL team. COVID-19 = coronavirus 2019; CCL = cardiac catheterization laboratory; ECG = electrocardiogram; PCI = percutaneous coronary intervention; STEMI = ST-elevation myocardial infarction.
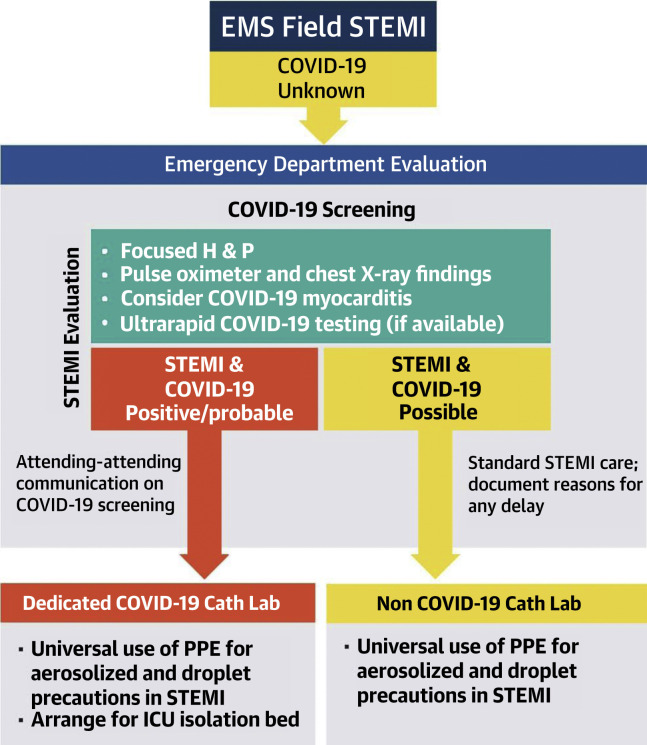
Figure 2.
Management Approach to a Field STEMI
Patients diagnosed as a field STEMI by the emergency medical system personnel need to be evaluated in the emergency department to assess their COVID-19 status and confirm the diagnosis of an STEMI. Individual patient-level decision making can be pursued as outlined in Figure 1. COVID-19 = coronavirus-2019; STEMI = ST-elevation myocardial infarction.
In certain circumstances, a more detailed and confirmatory evaluation in the ED might be required prior to transfer to the CCL. Thus, during the COVID-19 pandemic, there may be longer door-to balloon (D2B) times. D2B times should still be tracked, but we may expect more patient and/or system-related delays documented as appropriate reasons for delay in the ACC National Cardiovascular Data Registry (NCDR) programs (Chest Pain-MI and/or CathPCI). These programs are also working to support direct COVID-19 status documentation to further inform patient risk and local quality of care assessments.
Two point-of-care assays have recently received Food and Drug Administration (FDA) approval for rapidly making the diagnosis of COVID-19 (12). As these tests become widely available, they should be routinely implemented in all STEMI patients to better characterize patient diagnosis and risk, optimize the treatment plan for a given patient (for AMI ± COVID-19), and guide appropriate placement within the hospital, including a dedicated CCL and post-procedure unit.
It is important to emphasize that primary PCI should remain the standard of care, including for COVID-19 confirmed or probable patients. Once primary PCI is performed on the infarct-related artery, if clinically safe and indicated, any high-grade disease in a non-infarct related artery should also be treated during the index procedure to minimize further exposure of the CCL staff during a staged procedure. Primary PCI is superior for establishing normal (TIMI grade 3) coronary flow compared with an initial fibrinolysis strategy and has a significantly lower risk of fatal and nonfatal bleeding complications (7). Furthermore, after a fibrinolysis-based strategy, just over 50% of patients reperfuse resulting in a high proportion of patients requiring rescue PCI (7). This can result in prolonged ICU hospitalization with associated exposure to multiple health care providers and limiting access of ICU beds for COVID-19 patients.
In addition, some of these patients may have a “STEMI-mimicker” such as focal myocarditis or stress cardiomyopathy known to be associated with COVID-19 (13,14). Fibrinolysis of these patients would provide no benefit to the patient, but still incur bleeding risk and eventual invasive diagnostic catheterization given that the ST-elevation is unlikely to resolve. Each primary PCI center will need to monitor the ability to provide timely primary PCI based on staff and PPE availability, need for additional testing, as well as a designated CCL which will require terminal cleaning after each procedure. In the absence of these resources, a fibrinolysis first approach should be considered.
Possible STEMI
For patients who have an unclear, or equivocal, diagnosis of STEMI due to atypical symptoms, diffuse ST-segment elevation or atypical ECG findings, or a delayed presentation, additional noninvasive evaluation in the ED is recommended (Figure 1). The focus of this evaluation is twofold: a) further risk stratification for COVID-19 status; and b) further evaluation of the diagnosis specifically assessing the potential for coronary thrombotic occlusion versus other pathologies. Either a point-of-care ultrasound (POCUS) of the heart or a traditional transthoracic echocardiographic evaluation to assess for wall motion abnormality consistent with the electrocardiographic change may provide valuable information. Available clinical, ECG, laboratory, and imaging data can inform a decision between the ED physician and interventional cardiologist regarding CCL activation. Coronary CT angiography may be considered in cases where the findings of ST elevation and transthoracic echocardiography are divergent. One clear advantage of an invasive approach to STEMI in the current era is the ability to diagnose a thrombotic coronary occlusion (as opposed to stress cardiomyopathy or myocarditis) before embarking on an early reperfusion approach. Regardless, patients with hemodynamic instability might still require an invasive evaluation in the CCL to make a definitive diagnosis and provide necessary hemodynamic assessment and support.
Futile prognosis
We note that not all COVID-19 patients with ST elevation with/without an acute coronary occlusion will benefit from any reperfusion strategy or advanced mechanical support. In COVID-19 confirmed patients with severe pulmonary decompensation (adult respiratory distress syndrome) or pneumonia who are intubated in the ICU and felt to have an excessively high mortality, consideration for compassionate medical care may be appropriate. This decision is best made by each local health care team based on individual patient's prognosis, patient and family wishes, as well as the resources available at their specific health care system.
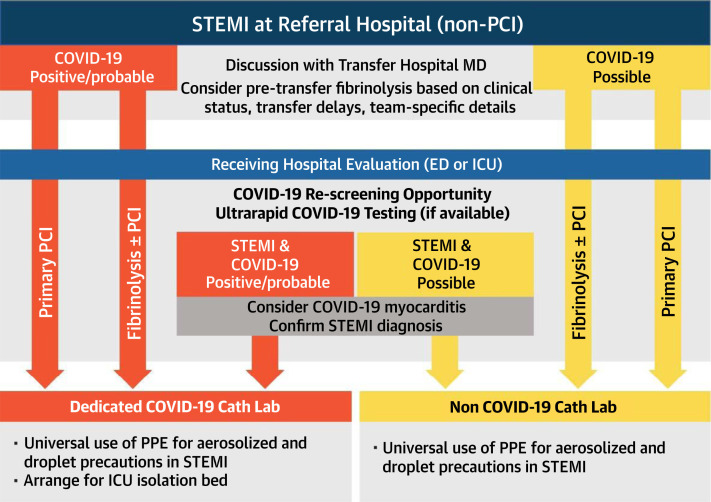
3.2. Patients presenting with STEMI to referral hospitals (non-PCI capable)
Primary PCI is the standard of care for patients transferred rapidly from non-PCI centers (within 120 min of first medical contact at referral hospital) (7). For patients in whom rapid reperfusion with primary PCI is not feasible, a pharmacoinvasive approach is recommended with initial fibrinolysis followed by consideration of transfer to a PCI center (Figure 3 ) (15,16). Transfer to a PCI center following fibrinolysis in the pre-COVID-19 period was generally considered routine and should remain the standard of care. However, patients with STEMI at a referral hospital with established COVID-19 infection should be discussed prior to transfer to a PCI center. Fibrinolysis within 30 min of STEMI diagnosis, and transfer for rescue PCI when necessary, may be preferable for all COVID-19-positive STEMI patients who are at a referral hospital provided the diagnosis of a true STEMI is highly likely.
Figure 3.
Care Pathway for STEMI at Referral Hospital (Non-PCI Center)
The decision to proceed with an initial fibrinolysis or direct transfer to a PCI center is multifactorial, and it will likely vary in different regions. The treatment decision also depends on whether the patient is COVID-19 positive or probable and should be made between the referral hospital physician and PCI center physician. On transfer of a patient with an STEMI from a referral hospital to a PCI center, the patient should be reevaluated for the COVID-19 status and STEMI diagnosis. The patient can then be taken for primary PCI, pharmacoinvasive PCI, or rescue PCI, as indicated. COVID-19 = coronavirus 2019; PCI = percutaneous coronary intervention; STEMI = ST-elevation myocardial infarction.
Although fibrinolysis first as a therapeutic strategy has been proposed for COVID-19 STEMI patients based on the experience from Sichuan hospital in China (17), this might be more applicable in regions with limited primary PCI centers. In the United States, we propose that an initial fibrinolysis therapy be used in non-PCI-capable hospitals if the first medical contact to reperfusion is felt to be >120 min. In the era of COVID-19, each regional STEMI system will need to closely monitor transfer processes and times with active adjustment to a fibrinolysis first approach if delays ensue that might not have been present prior to the pandemic. As outlined earlier, in the presence of an equivocal diagnosis of a STEMI in a COVID-19-positive or probable patient, additional noninvasive imaging should help determine if the patient is likely to have ST elevation associated with an occluded coronary artery, and therefore might benefit from a fibrinolysis reperfusion approach.
Patients with cardiogenic shock and/or out-of-hospital cardiac arrest
Patients with resuscitated out-of-hospital cardiac arrest (OHCA) and/or cardiogenic shock will continue to be the highest risk subgroup of AMI patients. These patients will also be the highest risk for droplet-based spread of COVID-19. Patients with resuscitated OHCA should be selectively considered for CCL activation in the presence of persistent ST elevation on their ECG, and a concomitant wall motion abnormality on echocardiographic evaluation. We recommend that OHCA patients without ST elevation not receive a routine early invasive approach unless hemodynamic instability ensues, an acute coronary occlusion remains high on the differential diagnosis, and a multidisciplinary team concurs (18,19). Appropriate PPE for the health care team in the ED and the CCL are required regardless of COVID-19 status since history may be limited in these patients. Consideration of revascularization and potential mechanical circulatory support (MCS) for patients in cardiogenic shock should proceed with PPE and special precautions for high droplet components of the procedure (i.e., intubation and extubation in negative pressure room by anesthesia if possible; intubation prior to arrival in the CCL).
For known COVID-19-positive or probable patient, while MCS might be considered for a cardiomyopathy and cardiogenic shock, venous–venous (V–V) extracorporeal membrane oxygenation (ECMO) should be considered for severe pulmonary decompensation and failure to oxygenate. When feasible, bedside placement of MCS or ECMO might decrease the risk of exposure to the CCL or cardiothoracic surgical team. The approach is dependent on local resources and the COVID-19 disease burden in the community. Finally, there are not enough data at this time to state whether advanced support devices for COVID-19-associated cardiovascular pathology will positively impact mortality rates and thus individual patient risk assessment is required.
Patients with non-ST-elevation acute myocardial infarction
A significant portion of patients with COVID-19 have elevated biomarkers of cardiac injury; an elevated troponin test is a poor prognostic marker in this patient group (3,4). Acute myocardial injury during COVID-19 infection is of unclear etiology: while a Type I AMI due to plaque rupture is possible, current studies have not determined the incidence of Type I AMI versus myocarditis, stress cardiomyopathy, coronary spasm, left ventricular strain, right heart failure, or Type II AMI due to severe illness. Hence, until additional data are available, COVID-19-positive or probable patients with a non-ST-elevation acute myocardial infarction (NSTEMI) presentation should be managed medically and only taken for urgent coronary angiography and possible PCI in the presence of high-risk clinical features (Global Registry of Acute Coronary Events [GRACE] score >140) (20) or hemodynamic instability. Patients with unstable angina or NSTEMI without high-risk features can be initially managed with AMI guideline-indicated medical therapies. Once stabilized, outpatient work-up and coronary angiography can be pursued at a future date when the infection is resolved.
In contrast, patients admitted with an acute coronary syndrome who are felt to be COVID-19 possible should continue to get standard medical therapy with an early invasive approach as clinically indicated. As rapid testing for COVID-19 becomes more easily available, it should be performed as soon as possible to establish diagnosis, inform risk assessment, and guide placement within the hospital. As the prevalence of COVID-19 remains unknown, we recommend that all medical staff taking care of AMI patients (regardless of COVID-19 positive, probable or possible) should have PPE in place during cardiovascular procedures, regardless of specific location (e.g., ED, CCL, ICU/CCU, hospital ward).
Personal Protective Equipment
Ensuring adequate protection of all HCWs in the EMS, transfer hospitals, PCI center ED, and the CCL team is critical. Cardiovascular teams in China developed policies and procedures for performing interventional cardiovascular procedures in the safest possible environment to optimize clinical outcomes and minimize the risk of infection of CCL teams, but these involved access to rapid testing protocols for the diagnosis of COVID-19 (17). Given the current delays in testing for COVID-19 in the United States, it is not feasible to await results of testing for STEMI, shock, or OHCA patients as has been proposed in protocols used in China (17). Therefore, all patients requiring emergent activation of the CCL should be treated as COVID-19 possible. Since the start of the COVID-19 outbreak, the World Health Organization maintains the recommendation of using medical masks for regular care of COVID-19 patients in the context of droplet and contact precautions, and respirators (N95, FFP2, or FFP3) for circumstances and settings where aerosol generation can occur (21,22). The latter include patients on bi-level or continuous positive pressure ventilation, those requiring intubation/extubation, defibrillation with need for CPR, and airway suctioning—all of these high-risk situations can be encountered during primary PCI for STEMI and OHCA (23). We note that intubation and extubation are both considered high risk for aerosol generation and whenever possible, a powered air-purifying respirator (PAPR) should be used with endotracheal intubation. In addition, the minimum number of personnel should be in the room at the time of intubation/extubation. Given the potential risk of aerosol generation during all emergency AMI procedures, this writing group recommends PPE with aerosolization protection for the entire CCL staff during PCI for all STEMI patients during this COVID-19 pandemic as per the previously published ACC/SCAI guidelines for managing CCL patients during the COVID-19 epidemic (24). Finally, we note that teams should consider minimizing the number of physician and staff potentially exposed during invasive cardiovascular procedures; this may include limiting the involvement of trainees in high-risk procedures and patients.
5. ED and EMS Collaboration
The ED is the place of initial medical contact for the majority of patients with STEMI in the United States. For the past two decades, the priority in emergency medicine in caring for these patients has been to rapidly diagnose STEMI and aim for urgent reperfusion. However, as mentioned previously, the electrocardiographic diagnosis of STEMI is more difficult in the presence of COVID-19. It is important to emphasize that liberal use of the ECG in both the prehospital setting and the ED is still encouraged. Respiratory viral infections are known to increase the incidence of true STEMI (i.e., acute coronary occlusion) (25), but myocarditis has been reported in cases of COVID-19 (2,13). As the electrocardiographic distinction between a true STEMI versus COVID-19-associated myocarditis can be challenging, additional noninvasive testing in consultation with a cardiologist may be warranted.
Prehospital care providers who respond to calls for cardiac complaints will typically have no forewarning that a patient with a potential AMI may also have symptoms of COVID-19. Therefore, we recommend that prehospital care providers have a low threshold for wearing appropriate protective equipment whenever responding to patients with a primary cardiac complaint. In the setting of cardiac arrest, the use of PPE is even more critical for the reasons stated earlier.
Certain EMS STEMI protocols around the United States allow the prehospital care providers to activate their local hospital CCL when diagnosing STEMI in the field and directly transport the patient from the ambulance to the CCL (“ED Bypass”). This has contributed to reductions in first medical contact-to-balloon time and improved patient care. However, due to the logistical issues and time delays secondary to diagnostic uncertainty of STEMI with COVID-19, direct transport of the patient to the CCL is not felt to be prudent at this time. Therefore, we recommend initial assessment of all STEMI patients in the ED during the COVID-19 pandemic to ensure the correct diagnosis and care plan (Figure 2). The attending interventional cardiologist should be notified, but without activation of the entire STEMI team until the plan for CCL activation is confirmed.
6. Regional STEMI Systems of Care
Regional systems of care for patients with STEMI have emphasized efficiency and simplicity (8,26). A fundamental strength of regional STEMI systems has been the ability to standardize protocols and provide quality improvement for a wide range of non-PCI hospitals, including community hospitals without on-site PCI (8). The COVID-19 epidemic has quickly altered the landscape for regional STEMI care and systems, and interventional cardiology teams are now faced with a new set of circumstances in which modified recommendations for care are expected and warranted. Regional systems of care for STEMI require close integration of EMS, ED providers, and STEMI referral hospitals in conjunction with the PCI center team. Each component of the regional STEMI system has its own inherent risk of COVID-19 infection/spread, as well as its own potential for delay in reperfusion for patients with STEMI.
Based on early experience in China and Europe, key challenges include the availability of ICU beds, ventilators, ECMO, and the risk to HCWs (including EMS personnel, ED staff, and specialized diagnostic and treatment units like the CCL). As the U.S. experience with COVID-19 is rapidly evolving, definitive best practices are clearly challenging and require flexibility for a complex regional care system. Based on these new operational risks and patient comorbidities, it is imperative to consider immediate adjustments that maximize treatment options for patients with acute cardiovascular emergencies while protecting the safety of patients and providers. We propose the following guiding principles for Transfer STEMI Regional Systems of Care in the era of coronavirus (Table 2 , Figure 3).
Table 2.
STEMI Regional Systems of Care
| System-wide: emergency medical services, STEMI referral hospitals, and PCI centers |
|
| Emergency medical services, field-activated STEMI, and referral (non-PCI) hospitals |
|
CDC = Centers for Disease Control and Prevention; CCL = cardiac catheterization laboratory; COVID-19 = coronavirus 2019; ED = emergency department; EMS = emergency medical system; ICU = intensive care unit; PCI = percutaneous coronary intervention; PPE = personal protective equipment; STEMI = ST-elevation myocardial infarction.
These recommendations will need to be adapted to each regional system's PCI centers, STEMI referral hospitals, and EMS system and need to be communicated clearly between cardiology and emergency medicine providers within each hospital. As the COVID-19 pandemic grows or recedes, this algorithm will need to be updated and adapted but will eventually return to the principles of simplicity and efficiency previously outlined in the STEMI accelerator program and the ACC/AHA guidelines (7,8,26). For now, each system must recognize the competing and equally important principles of: a) timely reperfusion of STEMI patients; b) safe regional transport and treatment of potentially high-risk patients; and c) additional emphasis on protection and safety of all health care personnel.
Conclusions
During the COVID-19 pandemic, primary PCI remains the standard of care for STEMI patients at PCI-capable hospitals when it could be provided in a timely manner, with an expert team outfitted with PPE in a dedicated CCL room. A fibrinolysis-based strategy may be entertained at non-PCI-capable referral hospitals or in specific situations where primary PCI cannot be executed or is not deemed the best option. Clinicians should recognize that patients with COVID-19 are inherently complex: a broad differential diagnosis for ST elevations (including COVID-19 associated myocarditis) should be considered in the ED prior to choosing a reperfusion strategy. In the absence of hemodynamic instability or ongoing ischemic symptoms, NSTEMI patients who are COVID-19 positive or probable are optimally managed with an initial medical stabilization strategy. It is imperative that HCWs use appropriate PPE for all invasive procedures during this pandemic, and that new rapid COVID-19 testing be expeditiously disseminated to all hospitals involved in the care of patients with AMI. Finally, we believe that each regional STEMI care network needs to revise their suggested algorithm for its local environment and ensure that EMS and referral hospital teams are facile with a balanced and standardized approach toward STEMI care during the COVID-19 pandemic.
Acknowledgment
The authors acknowledge Lawrence Ang, MD, FACC, FSCAI, for his assistance in the drafting of the figures.
Disclosure of Interest
E.M. reports clinical trial research support (Corindus, Abbott Vascular, CSI), consulting (Medtronic), consulting and equity (Abiomed). H.L.D. reports research grants and consulting (Boston Scientific and Medtronic). F.G.P.W. reports clinical trial support (Medtronic) and advisory board (Medtronic). J.C.M. and S.V.R. report no relevant disclosures. C.G. reports advisory board (Phillips and Abiomed). A.M. reports no relevant disclosures. A.J.K. reports Institutional funding to Columbia University and/or Cardiovascular Research Foundation from Medtronic, Boston Scientific, Abbott Vascular, Abiomed, CSI, Philips, ReCor Medical. Personal: CME/conference honoraria and travel/meals only. R.J. reports no relevant disclosure; P.M. reports research and educational grants (Abiomed, Medtronic); I.C.R., J.R., and T.D.H. report no relevant disclosures.
Footnotes
This article has been co-published in Catheterization and Cardiovascular Interventions and the Journal of the American College of Cardiology.
Frederick G.P. Welt, Ajay J. Kirtane, John S. Rumsfeld and Timothy D. Henry are representatives of the American College of Cardiology. Amal Mattu is a representative of the American College of Emergency Physicians. Ehtisham Mahmud, John C. Messenger, Sunil V. Rao, Cindy Grines, and Timothy D. Henry are representatives of the Society of Cardiovascular Angiography & Interventions. This document was endorsed by the American College of Cardiology (ACC), the American College of Emergency Physicians (ACEP), and the Society for Cardiovascular Angiography & Interventions (SCAI) in April 2020.
References
- 1.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ruan Q., Yang K., Wang W., Jiang L., Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46:846–848. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang D., Hu B., Hu C. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shi S., Qin M., Shen B. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020 Mar 25 doi: 10.1001/jamacardio.2020.0950. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guo T., Fan Y., Chen M. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 Mar 27 [E-pub ahead print] doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tam C.F., Cheung K.S., Lam S. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O'Gara P.T., Kushner F.G., Ascheim D.D. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61:e78–e140. doi: 10.1016/j.jacc.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 8.Henry T.D. From concept to reality: a decade of progress in regional ST-elevation myocardial infarction systems. Circulation. 2012;126:166–168. doi: 10.1161/CIRCULATIONAHA.112.114140. [DOI] [PubMed] [Google Scholar]
- 9.Inui S., Fujikawa A., Jitsu M. Chest CT findings in cases from the cruise ship “diamond princess” with coronavirus disease 2019 (COVID-19) Radiol Cardiothorac Imaging. 2020 Mar 17 [E-pub ahead of print] doi: 10.1148/ryct.2020204002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bai Y., Yao L., Wei T. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323:1406–1407. doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.FDA approval of rapid COVID-19 testing. Accessed google search April 8, 2020.
- 13.Madjid M., Safavi-Naeini P., Solomon S.D., Vardeny O. Potential effects of coronaviruses on the cardiovascular system. JAMA Cardiol. 2020 Mar 27 doi: 10.1001/jamacardio.2020.1286. [E-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 14.Fried J.A., Ramasubbu K., Bhatt R. The variety of cardiovascular manifestations of COVID-19. Circulation. 2020;141:1930–1936. doi: 10.1161/CIRCULATIONAHA.120.047164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dauerman H.L., Sobel B.E. Synergistic treatment of ST-segment elevation myocardial infarction with pharmacoinvasive recanalization. J Am Coll Cardiol. 2003;42:646–651. doi: 10.1016/s0735-1097(03)00762-9. [DOI] [PubMed] [Google Scholar]
- 16.Larson D.M., Duval S., Sharkey S.W. Safety and efficacy of a pharmaco-invasive reperfusion strategy in rural ST-elevation myocardial infarction patients with expected delays due to long-distance transfers. Eur Heart J. 2012;33:1232–1240. doi: 10.1093/eurheartj/ehr403. [DOI] [PubMed] [Google Scholar]
- 17.Zeng J., Huang J., Pan L. How to balance acute myocardial infarction and COVID-19: the protocols from Sichuan provincial People's hospital. Intensive Care Med. 2020:1–3. doi: 10.1007/s00134-020-05993-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rab T., Kern K.B., Tamis-Holland J.E. Cardiac arrest: a treatment algorithm for emergent cardiac procedures in the resuscitated comatose patient. J Am Coll Cardiol. 2015;66:62–73. doi: 10.1016/j.jacc.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 19.Lemkes J.S., Janssens G.N., van der Hoeven N.W. Coronary angiography after cardiac arrest without ST-segment elevation. N Engl J Med. 2019;380:1397–1407. doi: 10.1056/NEJMoa1816897. [DOI] [PubMed] [Google Scholar]
- 20.Mehta S.R., Granger C.B., Boden W.E. Early versus delayed invasive intervention in acute coronary syndromes. N Engl J Med. 2009;360:2165–2175. doi: 10.1056/NEJMoa0807986. [DOI] [PubMed] [Google Scholar]
- 21.Coronavirus disease 2019 (COVID-19) Situation Report-66. https://www.who.int/docs/default-source/coronaviruse/situationreports/20200326-sitrep-66-covid-19.pdf?sfvrsn=81b94e61_2 Available at:
- 22.WHO Infection Prevention and Control Guidance for COVID-19. https://www.who.int/emergencies/diseases/novel-coronavirus2019/technical-guidance/infection-prevention-and-control Available at:
- 23.Tran K., Cimon K., Severn M., Pessoa-Silva C.L., Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS ONE. 2012;7 doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Welt F.G.P., Shah P.B., Aronow H.D. Catheterizatiion laboratory considerations during the coronavirus (COVID-19) pandemic. From the ACC's interventional council and SCAI. J Am Coll Cardiol. 2020;75:2372–2375. doi: 10.1016/j.jacc.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kwong J.C., Schwartz K.L., Campitelli M.A. Acute myocardial infarction after laboratory-confirmed influenza infection. N Engl J Med. 2018;378:345–353. doi: 10.1056/NEJMoa1702090. [DOI] [PubMed] [Google Scholar]
- 26.Jollis J.G., Al-Khalidi H.R., Roettig M.L. Regional systems of care demonstration project: American Heart Association Mission: lifeline STEMI systems accelerator. Circulation. 2016;134:365–374. doi: 10.1161/CIRCULATIONAHA.115.019474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ebinger J.E., Strauss C.E., Garberich R.R. Value-based ST-segmentelevation myocardial infarction care using risk-guided triage and early discharge. Circ Cardiovasc Qual Outcomes. 2018;11 doi: 10.1161/CIRCOUTCOMES.118.004553. [DOI] [PMC free article] [PubMed] [Google Scholar]