Abstract
Little is known about the impact of adrenocortical carcinoma (ACC) on health-related quality of life (HRQoL), and no disease-specific questionnaire exists. This qualitative study aimed to identify relevant domains of HRQoL for patients with ACC.
In 2 focus group interviews, we discussed concerns regarding living with ACC and its treatments. The first group consisted of 6 patients on mitotane therapy and their partners or relatives, the second group of 4 patients after surgery alone and their partners. Inductive qualitative content analysis was used to analyze the interviews.
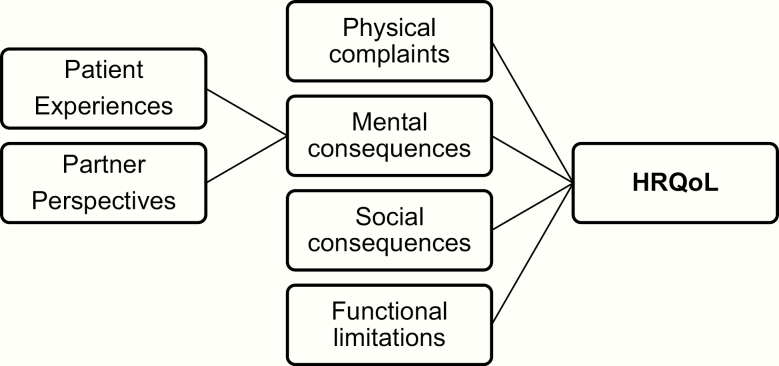
We identified 4 domains related to HRQoL in patients with ACC, namely physical complaints, mental consequences, social consequences, and functional limitations. For example, physical complaints included symptoms of the disease and side effects of mitotane therapy; mental consequences included feeling insecure and living from scan to scan; and functional limitations included daily activities and mobility. We further found that patients’ experiences with the health care system and health care professionals and partner perspectives influence HRQoL.
In conclusion, ACC has a large impact on HRQoL in 4 domains. These results can be used to improve communication about HRQoL issues. We will use our findings to generate a disease-specific questionnaire to measure HRQoL in patients with ACC.
Keywords: adrenocortical carcinoma, health-related quality of life, patient experiences, partner perspectives, adrenalectomy, mitotane therapy
Adrenocortical carcinoma (ACC) is a rare cancer with high morbidity and mortality [1]. Treatment options and prognosis depend on the stage of the disease [2]. Single tumors are treated with surgical adrenalectomy. Depending on the recurrence risk, surgery is followed by at least 2 years of adjuvant mitotane therapy. Irresectable tumors or metastasis can be treated by surgery, radiotherapy, mitotane therapy, or chemotherapy-mitotane combination therapy. Both the symptoms and treatment options of ACC can have an impact on health-related quality of life (HRQoL). For example, tumors can be hormonally active and treatment can induce hormonal deficiencies, which are both associated with impaired HRQoL [3].
We discovered that there have been limited studies on HRQoL in patients with ACC [4]. One randomized controlled trial including 294 patients with advanced ACC indicated an impaired HRQoL compared to the general population and a further impairment due to chemotherapy-mitotane combination therapy [5]. However, there have been very limited studies in patients after surgical therapy and no studies in patients on mitotane monotherapy. We hypothesize that HRQoL research on benign adrenal tumors might not be fully generalizable to patients with ACC. For example, mitotane therapy is used only for ACC and has a unique spectrum of potentially severe side effects. Therefore, the most recent guideline on the management of ACC expressed a need for more research on HRQoL in patients with ACC [2].
Further research can provide information on the influence of different treatment options on HRQoL, which is essential to the process of shared decision making. To conduct this research, patient-reported outcome measures (PROM) are increasingly used to measure HRQoL, both general and disease specific. These PROMs can also be used in the clinical setting to improve treatment guidance and thus improve patient-centered care [6]. To date, no disease-specific PROM exists for measuring HRQoL in patients with ACC. To determine which issues and domains should be included in an HRQoL PROM for ACC, patient input is essential. In this qualitative study, we therefore conducted focus group interviews with patients with ACC and their partners or relatives, with the aim of identifying relevant domains of HRQoL for patients with ACC.
1. Materials and Methods
A. Participant Inclusion
Patients with ACC with all stages of disease being treated as outpatients at Máxima MC the Netherlands were eligible for inclusion. Patients were purposefully selected to create a heterogeneous reflection of the ACC population. We contacted patients face to face and by telephone. Eligible patients received a letter with information about the study. In total, 16 patients were contacted. Two patients were unable to attend on the chosen date, 3 patients did not want to bring up the past, and 1 patient who had received chemotherapy-mitotane combination therapy was unable to attend because of physical illness.
The partner or a relative closely involved in the treatment was also invited. Some patients indicated they were more comfortable talking while their partner was present and partners could help with recall. Secondly, we hypothesized that partner perspectives could influence patients’ experiences and HRQoL. We therefore included the partner perspectives to be able to investigate this phenomenon.
Two focus group interviews were carried out at Máxima MC. The first group consisted of 6 patients who currently or recently received mitotane treatment and their partners or relatives (1 mother, 1 sister). Two patients received mitotane adjuvant after surgery, 4 for metastatic disease. Two patients had also received radiotherapy. The second group consisted of 4 patients who were treated with surgery only and their partners. The sample was heterogeneous in terms of age (mean 57.1 years; range, 26-71 years), sex (7 female, 3 male), time since diagnosis (mean 4.9 years; range, 1-18 years), hormone production (2 cortisol, 1 cortisol and androgens, 7 none), ENSAT (European Network for the Study of Adrenal Tumors) stage (4 stage I-II, 1 stage III, 5 stage IV), and treatment response (5 complete response, 3 stable disease, 2 progressive disease) (Table 1).
Table 1.
Patient Characteristics
| Group 1 | Group 2 | Overall | |
|---|---|---|---|
| Mitotane | Nonmitotane | ||
| (N = 6) | (N = 4) | (N = 10) | |
| Agea, mean (range), y | 55.8 (26-71) | 59 (57-61) | 57.1 (26-71) |
| Female, No. | 4 | 3 | 7 |
| Years since diagnosisa, mean (range) | 3.0 (1-4) | 7.8 (1-18) | 4.9 (1-18) |
| ENSAT stagea, No. | |||
| I | 1 | 2 | 3 |
| II | 0 | 1 | 1 |
| III | 1 | 0 | 1 |
| IV | 4 | 1 | 5 |
| Hormone production, No. | |||
| None | 4 | 3 | 7 |
| Cortisol | 1 | 1 | 2 |
| Cortisol and androgens | 1 | 0 | 1 |
| Therapy, No. | |||
| Surgery | 5 | 4 | 9 |
| Mitotane | 6 | 1b | 7 |
| Radiotherapy | 2 | 0 | 2 |
| Chemotherapy | 0 | 0 | 0 |
| Response (RECIST)a, No. | |||
| Complete response | 2 | 3 | 5 |
| Stable disease | 3 | 0 | 3 |
| Progressive disease | 1 | 1 | 2 |
Abbreviations: ENSAT, European Network for the Study of Adrenal Tumors; RECIST, Response Evaluation Criteria in Solid Tumors.
aAt time of focus group. bDiscontinued after 5 weeks because of side effects.
B. Focus Group Interviews
Both focus group interviews were moderated by a clinical doctor trained at moderating focus groups (M.N.T.K.). The moderator was not involved in ACC treatment and did not know the participants in advance. A co-moderator (R.V.S.) and note-taker were also present during the focus groups. We used a preprepared, semistructured interview guide. The interview questions were inspired by the literature and clinical experience of the research team [4]. During the introduction round, the moderator and co-moderator introduced themselves and explained the aim of the focus group. Patients were then asked to describe their experience with the disease and treatment options, the influence on everyday life, and their concerns regarding HRQoL. The focus group interviews were ended when no new topics came up, which occurred after 2.5 hours in the first group and 2 hours in the second.
The study protocol has been approved by the local Medical Ethics Committee. Written consent was obtained from all patients and all quotations have been anonymized. Partners have been indicated with a “p.”
C. Analysis
Both focus group interviews were audiotaped and transcribed smooth verbatim with comments on nonverbal observations. A total of 4.5 hours of audiotape resulted in 2218 lines of transcribed text. The participants were not asked to provide feedback on the transcripts or the findings.
Inductive qualitative content analysis was used to analyze the transcripts using QDA Miner Software Lite, v2.0.5 [7-9]. Using an open coding method, codes were given to each line of transcription hypothesis free to label the meaning of the phrase. These codes were then grouped in subcategories and categories related to HRQoL (Table 2). The final coding framework was used to establish an overview of HRQoL domains relevant for patients with ACC.
Table 2.
Example of Inductive Coding Framework
| Examples of translated quotes | Code | Subcategory | Category | Domain |
|---|---|---|---|---|
| 3: I took mitotane only at night, … then I woke up every night with diarrhea, fell back asleep again, and functioned better during the day. 5: I get diarrhea attacks. … This morning while traveling here, we got out of traffic just in time for me to run to a bathroom. 6: When the dose (mitotane) is increased, I get diarrhea at night. | Diarrhea | Gastrointestinal | Side effects of mitotane | Physical complaints |
| 4: Mitotane makes me nauseous. | Nausea | |||
| 3: I thought I was walking straight, but I walked straight into a door. 4: At night I have to shuffle forward. 4p: And you have to hold on to something. 6: It feels like I’m drunk. | Loss of coordination | Neurological | ||
| 3: With the mitotane I had neurological complaints, I had no concentrations. 5: It is a lack in concentration, with a newspaper I have to stop every once in a while and read it again. | Loss of concentration | |||
| 2p: He had a loss of balance, dizziness. 8: What bothered me most was the dizziness and therefore not being allowed to drive a car. | Balance disturbances and dizziness |
Coding was performed independently by 2 researchers (R.V.S. and L.A.M.) and discrepancies were handled by discussion. After reviewing the initial coding framework, significant overlap between the patient experiences and the existing Cancer Patient Experiences Questionnaire (CPEQ) was discovered [10]. Similarly, an overlap existed between the partner perspectives and the existing Cancer Support Person’s Unmet Needs Survey—Short Form (SPUNS-SF) questionnaire [11]. We therefore used the main categories of these existing questionnaires to recode the patient experiences and partner perspectives.
2. Results
We identified 4 domains related to HRQoL in patients with ACC, namely physical complaints, mental consequences, social consequences, and functional limitations. We further found that patients’ experiences with the health care system and health care professionals and partner perspectives influence HRQoL, mostly through effects on the mental consequences domain. A conceptual model of HRQoL in ACC is represented in Fig. 1.
Figure 1.
Conceptual model of health-related quality of life domains in adrenocortical carcinoma. Abbreviation: HRQoL, health-related quality of life.
A. Physical Complaints
The physical complaints domain comprised 5 categories: symptoms of the disease, recovery and complications after surgery and radiotherapy, side effects of mitotane, symptoms of cortisol production and supplementation, and long-term consequences.
The disease presented in most patients with abdominal pain: “1: I thought I had kidney stones, because of the pain I felt in my left abdomen.” Other presenting symptoms included headaches, fatigue, sleep problems, fever, nausea and vomiting, difficulty eating or loss of appetite, and increased abdominal size. One patient had androgen production; she therefore also presented with acne and excessive hair growth. Symptoms due to cortisol production were also mentioned and will be discussed later.
HRQoL was influenced by complications after surgery, side effects of painkillers, wound problems, scar problems, nausea, pain, and hiccups. Recovery time after surgery varied between the patients. Some made a good recovery, whereas others suffered from the aftermath for weeks: “8: I couldn’t get out of bed, only to eat and shower. It took 6 weeks for me to get out of the house for a walk.” The 2 patients who received radiation therapy made a good recovery.
The patients on mitotane therapy felt a large burden on their HRQoL due to the side effects. Gastrointestinal side effects included diarrhea, flatulence, nausea, vomiting, changes in taste, liver toxicity, and elevated cholesterol. Neurological side effects included loss of coordination, loss of concentration, balance disturbances and dizziness, forgetfulness, slowing, and difficulty speaking: “8: What bothered me most was the dizziness and therefore not being able to drive a car. This makes me dependent on everyone, which I cannot stand.” Some patients further reported a loss of sexuality and menstrual disturbances.
The effects of cortisol-producing tumors and cortisol replacement therapy had overlapping effects on HRQoL in our patients and will therefore be discussed together. Patients were mostly hindered by the increased incidence of infections, resulting in the need for immediate medical attention and higher supplementation dosages: “3p: What we find annoying about the cortisol supplementation is that we have to go straight to the hospital when she gets a simple flu.” Other symptoms that were reported were poor wound healing, palpitations, rushed feeling, edema, weight gain, and dry, fragile, and itchy skin.
Long-term effects of ACC mostly involved minor to severe fatigue, loss of physical fitness, and weakness: “4: I have to ask my husband to do everything because I am too tired. Even taking a shower exhausts me.”
B. Mental Consequences
All patients and partners reported feeling insecure at some point during the diagnostic procedures, treatment, or follow-up. They felt insecure about the cause and consequences of their physical complaints, about their diagnosis, and mostly about the future. Especially when new scans approach, the feeling of insecurity returns. Patients feel like they are living from scan to scan: “7: When it is time for the tests and scans again, the uncertainty returns. Then I am worried about what the next scan will show.”
After receiving the diagnosis patients and partners felt worried or even startled and some had difficulty accepting the situation: “10: My body cannot do what I want it to do anymore, … but accepting that is difficult.” Some patients further reported getting emotional or irritated more easily since being diagnosed with cancer. On the other hand, continuing life and staying optimistic was widely expressed in both groups: “5: I don’t know how long it will take and what I can expect, but at the moment I feel really good, the tumor is gone and I remain positive.”
Some treatment options were viewed with caution or even fear. For example, all patients were afraid of complications of radiation therapy and some partners felt relieved when no radiation therapy was necessary. Patients also reported aversion toward taking their medication, including mitotane therapy, cortisol replacement therapy, and supportive medication. Four patients suffered from mental side effects of treatment such as mood disturbances, panic attacks, and even burnout: “3p: Before the diagnosis she didn’t recognize herself due to the mood swings and panic attacks. 3: Even now when my supplementation dose is too high, I get a crazy temper.”
C. Social Consequences
Suffering from ACC had a large impact on family life. Among others, this was due to changes in role functioning such as performing household chores and looking after (grand)children. But their families also provided energy to patients: “10p: The disease had a lot of impact, but together we can live through anything.” Outside the family, patients experienced compassion from their neighbors and friends. However, they sometimes experienced a lack of understanding due to the disease being rare and not clearly visible: “6: I sometimes struggle with the fact that people can’t see that I am sick. Don’t get me wrong, I am glad that I am not bald from chemotherapy, but people don’t notice that I am sick. … People judge me for that, like why can you look good and go to work, but you can’t clean your own windows.” The disease being rare also results in a lack of contact with other patients; this was reported as disappointing by some patients and partners.
D. Functional Limitations
Patients were limited in their daily living due to consequences of ACC; this included work and daily activities such as housework and babysitting grandchildren. Leisure activities such as holidays, hobbies, and going out for dinner were also limited by the disease. Patients further experienced a lack in mobility due to an inability to walk, cycle, drive, or travel long distances. Staying independent even with physical limitations was perceived as very important.
These functional limitations could be consequences of various aspects of the disease. Some patients were limited by fatigue or (neurological) side effects of mitotane therapy: “4: I am not allowed to cycle anymore, because I drove right into parked cars.” Others experienced limitations due to mental issues or had to adjust activities and meals based on medication. Owing to these limitations, patients had to make different choices and adjust their lifestyle, which influenced their HRQoL.
E. Patient Experiences
Patients’ experiences with the health care system and health care professionals influenced their HRQoL. After reviewing the initial coding framework, significant overlap between the patient experiences codes and the existing CPEQ was discovered [10]. Experiences that patients valued most were related to good contact with their doctor, proper information about the diagnosis and treatment options, and good organization of care. Less mentioned were the importance of patient safety, good nurse contact, contact with next of kin, and hospital standards. Patients described their experiences mostly in relation to the mental consequences of ACC, for example, a good relation with their doctor and receiving proper information leading to feeling less worried: “3: Between appointments questions start pilling-up and I start worrying, so I send an email and my doctor replies with a reassuring message, then I can relax again.”
F. Partner Perspectives
During the interviews, partners and relatives shared their perspectives on coping with the disease. An overlap existed between the partner perspectives and the existing SPUNS-SF questionnaire [11]. The partners mostly expressed their emotional and personal needs, the importance of proper information, access and continuity of health care, and worries about the future. Work and financial needs were mentioned less by the partners in our groups.
Partners’ perspectives influenced not only their own HRQoL but also the HRQoL of the patient. For example, a partner worrying about treatment side effects might have led to the patient feeling insecure about the treatment: “2p: I was so opposed to him taking the medication, that I think I might have made it more difficult.”
3. Discussion
In this qualitative study, we identified 4 domains related to HRQoL in patients with ACC, namely physical complaints, mental consequences, social consequences, and functional limitations. This is in line with established models on HRQoL [12-14]. Thus far, there has been limited information about the influence of ACC on HRQoL. This information is important in the process of shared decision making and communication about HRQoL issues so that patient-centered care can be provided.
HRQoL can be measured using general or disease-specific PROMs. One example of a general HRQoL PROM for use in cancer patients is the EORTC-QLQ-C30 (European Organisation for Research and Treatment of Cancer core quality of life questionnaire). This questionnaire includes general issues that cancer patients experience as a result of their disease. We found that our results had a large overlap with the items in the EORTC-QLQ-C30. We therefore hypothesize that this questionnaire can be a good tool to measure HRQoL in patients with ACC to get a general overview of all relevant domains. However, not all relevant issues we found are included in the EORTC-QLQ-C30. This questionnaire does not include issues that are more specific to one type of cancer, such as in ACC the neurological side effects of mitotane or the effects of cortisol production or supplementation. Therefore, the EORTC has the option to develop disease-specific models that can be used in addition to the EORTC-QLQ-C30 questionnaire to obtain a better understanding of the full range of HRQoL issues patients face [15]. The results of our qualitative study can be used as a first effort to create an ACC-specific model to be used in addition to the EORTC-QLQ-C30.
Future research using an HRQoL PROM appropriate for use in patients with ACC will provide much needed information on the effects of different treatment options on HRQoL. This information is essential in the process of shared decision making for health care professionals and patients. The results of this study and a disease-specific HRQoL PROM can also aid patient-centered care by improving guidance of individual therapies [6]. For example, almost all patients reported the importance of regaining their physical and mental fitness. Receiving aftercare by a rehabilitation specialist, physical therapist, or psychologist trained in treating cancer patients was viewed as a positive contribution to reaching these goals by our participants. Research has shown that exercise-based or multidimensional rehabilitation programs are beneficial to HRQoL in cancer patients [16, 17]. A change in fatigue or weakness can be used as a signal that referral to a cancer aftercare program might be beneficial.
We found that patient experiences and partner perspectives influence HRQoL, especially through the mental consequences domain. This is in line with other studies that found a positive association between patient experiences and clinical or patient-reported outcomes [18, 19]. It is therefore important to also measure patient and partner experiences to gain information about the full range of a patients’ well-being or better interpret a change in the mental domain. For example, when a doctor properly tailors the information to a specific patient’s needs and creates clear expectations, this might result in less worry about the future and a higher HRQoL [20, 21]. Measuring and communicating about these experiences could therefore play a role in improving HRQoL [22]. We found a large overlap with the experiences our participants reported and the CPEQ and SPUNS-SF questionnaires [10, 11]. We therefore suggest using these or similar questionnaires when measuring patients experiences and partner perspectives in ACC research and practice.
A potential limitation of this study is the limited number of participants in the focus group interviews. For model development, usually inclusion of 20 patients or more is recommended [23]. However, ACC is a rare cancer, with an incidence of 1 per million person-years and an overall median survival of 17 months [1]. Our study thus included one-tenth of the estimated population of ACC survivors in the Netherlands. Furthermore, the participants were a heterogeneous sample of the population and both focus groups were continued until no new topics came up to improve data saturation.
A second limitation is the potential selection of healthier patients with fewer HRQoL concerns. We aimed to limit this phenomenon by purposefully selecting patients with all disease stages and treatment options. The only exception was that no patient on chemotherapy was included because of physical illness at the time of the focus group interviews. We hypothesize that patients on chemotherapy-mitotane combination therapy experience the same HRQoL issues as discussed during the focus groups but with different intensity [5]. We therefore expect the results would not have differed if the patient on chemotherapy had been included. Furthermore, the EORTC-QLQ-C30 has been developed with patients on a wide range of chemotherapy regimens [15]. Most relevant issues for patients on chemotherapy will therefore already be included in the questionnaire.
Finally, the presence of the partners or relatives might result in patients not discussing severe HRQoL concerns to spare the others [24]. Although this is a well-known phenomenon, we do not feel this occurred during our focus group interviews. In our experience, patients felt more comfortable in the presence of their partner or relative. In addition, the partners and relatives were helpful with recalling memories and finding the correct words to describe HRQoL concerns, especially for the patients suffering from impaired memory and concentration due to mitotane side effects.
In conclusion, ACC has a large impact on HRQoL. We identified 4 HRQoL domains relevant to patients with ACC. With this knowledge, doctors can improve communication about relevant HRQoL issues. Furthermore, we will use these domains to generate a disease-specific model as an addition to the EORTC-QLQ-C30 questionnaire to measure HRQoL in patients with ACC. With this we aim to improve patient-centered care in this specific patient group.
Acknowledgment
We thank Narcis Serafras (Maastricht University, medical intern Máxima MC, Department of Internal Medicine) for her assistance as note-taker during the focus group interviews.
Financial Support: This work received no specific grant from a funding agency in the commercial or not-for-profit sector.
Glossary
Abbreviations
- ACC
adrenocortical carcinoma
- CPEQ
Cancer Patient Experiences Questionnaire
- EORTC-QLQ-C30
European Organisation for Research and Treatment of Cancer core quality of life questionnaire
- HRQoL
health-related quality of life
- PROM
patient-reported outcome measures
- SPUNS-SF
Cancer Support Person’s Unmet Needs Survey—Short Form
Additional Information
Disclosure Summary: The authors have nothing to disclose.
Data Availability: Research data are not shared because of privacy restrictions.
References
- 1. Kerkhofs TM, Verhoeven RH, Van der Zwan JM, et al. Adrenocortical carcinoma: a population-based study on incidence and survival in the Netherlands since 1993. Eur J Cancer. 2013;49(11):2579-2586. [DOI] [PubMed] [Google Scholar]
- 2. Fassnacht M, Dekkers OM, Else T, et al. European Society of Endocrinology clinical practice guidelines on the management of adrenocortical carcinoma in adults, in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol. 2018;179(4):G1-G46. [DOI] [PubMed] [Google Scholar]
- 3. Ho W, Druce M. Quality of life in patients with adrenal disease: a systematic review. Clin Endocrinol (Oxf). 2018;89(2):119-128. [DOI] [PubMed] [Google Scholar]
- 4. Steenaard RV, Michon LA, Haak HR. Health-related quality of life in adrenocortical carcinoma. Cancers (Basel). 2019;11(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fassnacht M, Terzolo M, Allolio B, et al. ; FIRM-ACT Study Group Combination chemotherapy in advanced adrenocortical carcinoma. N Engl J Med. 2012;366(23):2189-2197. [DOI] [PubMed] [Google Scholar]
- 6. Greenhalgh J, Gooding K, Gibbons E, et al. How do patient reported outcome measures (PROMs) support clinician-patient communication and patient care? A realist synthesis. J Patient Rep Outcomes. 2018;2:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107-115. [DOI] [PubMed] [Google Scholar]
- 8. Krippendorf K. Content Analysis: An Introduction to its Methodology. Thousand Oaks, CA: SAGE; 2013. [Google Scholar]
- 9. Mayring P. Qualitative Content Analysis: Theoretical Foundation, Basic Procedures and Software Solution. Klagenfurt, Austria: Philipp Mayring; 2014. [Google Scholar]
- 10. Iversen HH, Holmboe O, Bjertnæs ØA. The Cancer Patient Experiences Questionnaire (CPEQ): reliability and construct validity following a national survey to assess hospital cancer care from the patient perspective. BMJ Open. 2012;2(5):e001437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Campbell SH, Carey M, Sanson-Fisher R, et al. Measuring the unmet supportive care needs of cancer support persons: the development of the support person’s unmet needs survey–short form. Eur J Cancer Care (Engl). 2014;23(2):255-262. [DOI] [PubMed] [Google Scholar]
- 12. Testa MA, Simonson DC. Assessment of quality-of-life outcomes. N Engl J Med. 1996;334(13):835-840. [DOI] [PubMed] [Google Scholar]
- 13. Ferrell BR. The quality of lives: 1,525 voices of cancer. Oncol Nurs Forum. 1996;23(6):909-916. [PubMed] [Google Scholar]
- 14. The World Health Organization Quality of Life Assessment (WHOQOL): development and general psychometric properties. Soc Sci Med. 1998;46(12):1569-1585. [DOI] [PubMed] [Google Scholar]
- 15. Johnson C, Aaronson N, Blazeby JM, et al. EORTC Quality of Life Group guidelines for developing questionnaire modules. 4th ed. Eur J Cancer. 2011. [Google Scholar]
- 16. Mishra SI, Scherer RW, Geigle PM, et al. Exercise interventions on health‐related quality of life for cancer survivors. Cochrane Database Syst Rev. 2012(8):CD007566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Scott DA, Mills M, Black A, et al. Multidimensional rehabilitation programmes for adult cancer survivors. Cochrane Database Syst Rev. 2013(3):CD007730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kremers MNT, Zaalberg T, van den Ende ES, et al. Patient’s perspective on improving the quality of acute medical care: determining patient reported outcomes. BMJ Open Qual. 2019;8(3):e000736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Faller H, Koch U, Brähler E, et al. Satisfaction with information and unmet information needs in men and women with cancer. J Cancer Surviv. 2016;10(1):62-70. [DOI] [PubMed] [Google Scholar]
- 21. de Rooij BH, Ezendam NPM, Nicolaije KAH, et al. Survivorship care plans have a negative impact on long-term quality of life and anxiety through more threatening illness perceptions in gynecological cancer patients: the ROGY Care trial. Qual Life Res. 2018;27(6):1533-1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Von Essen L, Larsson G, Oberg K, Sjödén PO. ‘Satisfaction with care’: associations with health-related quality of life and psychosocial function among Swedish patients with endocrine gastrointestinal tumours. Eur J Cancer Care (Engl). 2002;11(2):91-99. [DOI] [PubMed] [Google Scholar]
- 23. Kerr C, Nixon A, Wild D. Assessing and demonstrating data saturation in qualitative inquiry supporting patient-reported outcomes research. Expert Rev Pharmacoecon Outcomes Res. 2010;10(3):269-281. [DOI] [PubMed] [Google Scholar]
- 24. Norlyk A, Haahr A, Hall E. Interviewing with or without the partner present? An underexposed dilemma between ethics and methodology in nursing research. J Adv Nurs. 2016;72(4):936-945. [DOI] [PubMed] [Google Scholar]