Superiority of ultrasound versus physical examination and X-ray
Currently, many studies have shown the superiority of lung ultrasound as an auxiliary tool to diagnoses in several respiratory diseases, such as those triggered by SARS-CoV-2. This ought to be stated: lung ultrasound leads to higher diagnostic accuracy than to what auscultations and X-rays allow. A representative article1 showed how the specificity, the sensibility and the diagnostic accuracy achieved during a lung ultrasound surpassed 93% in all parameters whereas auscultations and X-rays yield variable and little-supported data. Ultrasound is considered to be the fifth pillar of physical examinations,2 and there is an open debate on whether ultrasound should replace stethoscopes in certain scenarios.3 This same scenario has been shown to happen in echocardiography, where medical students who have trained to recognize cardiovascular disease showed a greater accuracy in their diagnoses using pocket ultrasounds than a trained cardiologist using a traditional physical examination.4 We would like to strongly encourage the medical community to not rely solely on auscultation in patients with dyspnea, reduce their use of X-rays and do selective CT scans in this pandemic. It has been shown that lung ultrasound at the point of care has diminished the use of thorax X-rays by 26%, and a 47% in the use of CT scans that show significant statistical results.5
Binomial examination
Examining a patient in an intensive care unit (ICU) is done by one person, who both explores and controls image capturing. However, this dynamic is not recommended in the context of SARS-CoV-2. In this case, the exploration carried out in pairs is recommended.
They will aid and assist the patient and their environment with the necessary personal protective equipment. An explorer (the professional with the most experience and skill) will manipulate the probe, the gel, and the patient, whereas the second one will only control the commands and the screen, recording images and videos alongside the explorer, who will observe and direct. This second participant should not interact with the patient or the objects around them, minimizing the chance for nosocomial and fomite transmission. The pocket equipment should be placed in protective covers (phones, tablets, probes). Cleaning should be done in proximal-to-distal sweeps without zigzagging. The same procedure should be performed after each new patient.6 Gel must be used carefully in order to prevent its contamination and further dissemination of the virus. Allocating a specific amount of gel for each patient is also recommended, since it prevents the patient's skin, the bottle, and the probe from touching each other.
Examination techniques
If the patient is sitting
The thorax will be explored from three different angles by hemithorax (the anterior, lateral, and posterior faces) and in six different segments (Anterior: superior/inferior; Lateral: superior/inferior. Posterior: superior/middle/inferior). These are fourteen segments in total. The sweep will be performed from median to lateral and downward, placing the probe both transversely and longitudinally, with one mark pointing to the head and in medial position. The findings should be registered according to the segment and the intercostal space in which they were found.
If the patient is in supine or prone decubitus
The thorax is limited to two faces depending on the patient's position (anterior/posterior) the lateral sides can be explored as well (superior and inferior).
BLUE protocol
The BLUE protocol7 is a standardized diagram for the rapid identification of the causes of dyspnea. It shows six persistent pathologies in around 97% (pulmonary edema, pneumonia, pulmonary embolism, COPD, asthma, pneumothorax) of the adult patients that are admitted into hospitals with dyspnea and then progressed into the ICU, the remaining 3% belongs to more rare diseases; the BLUE patterns related to COVID 19 are:
-
•
Multiple, diffuse B-lines in the presence of lung sliding indicated pulmonary edema.
-
•
Anterior alveolar consolidations, anterior diffuse B-lines with abolished lung sliding, anterior asymmetric interstitial patterns, posterior consolidations, or effusions in the absence of anterior diffuse B-lines indicated pneumonia.
-
•
Diffuse, bilateral B-lines (at least in four points of the anterior chest wall) may indicate cardiogenic or noncardiogenic pulmonary edema. Performing echocardiography may be helpful in this case.
-
•
Focal B-lines may indicate interstitial syndrome.
POCUS findings in COVID-19
The main ultrasound findings reported are summarized in (Table 1 ). Danilo Buonsenso reported6 an irregular pleural line with small sub pleural consolidations both in the anterior and posterior thorax, a great presence of vertical artifacts, several areas of preserved tissue mixed with sick tissue, and some typical images of interstitial alveolar damage (the same present in some Chinese patients),8 who also reported to have diminished local blood flow, as observed by Doppler.9 Add a transverse probe rotation improves the visualization of consolidations increasing in the number of signs visualized (greater length of pleura visualized and constant). One limitation is the detection of deep lesions due to the blockage of the sonic transmission in an aerated lung, however, makes an excellent tool to observe sub pleural lesions, and vertical artifacts, since most reported cases show that the posterior-inferior fields of the lung are focal points for the disease. If the pneumonia extends beyond the pleural line and the ultrasound does not provide enough clarity in order to understand the clinical course of the disease, a thorax CT scan will be needed. The ultrasound patterns found in the course of COVID-19 were significantly different to those of other lesions reported in the literature.10
Table 1.
Main findings of lung ultrasound in COVID-19.
| Main findings on lung ultrasound related to SARS-CoV-2 |
|---|
| Subpleural consolidations of varied presentation (large, small) or multifocal. |
| Bilateral alveolar-interstitial patterns. |
| Irregularity or complete interruption of the pleural line. |
| Focal, multifocal and confluent patterns of B lines (vertical artifacts), patchy areas of white lung. |
| Decrease of lines B (vertical artifacts) and reappearance of lines A in the recovery phase. |
| Decreased or absent Doppler signal in Lung Consolidations (preliminary findings). |
| Pleural effusions are rare. |
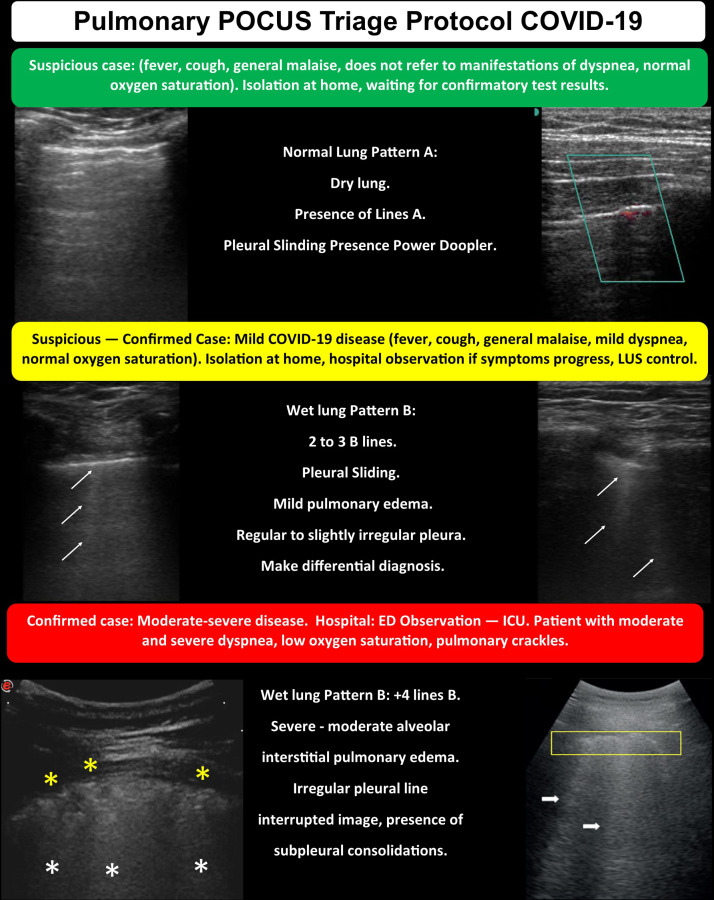
POCUS triage for COVID-19
This system will be useful in emerging economies or systems lacking resources, avoiding the saturation of medical services; it is based on an intuitive triage by virtue of the several ultrasound patterns related to COVID-19 (Fig. 1 ). POCUS triage can help professionals pick out low-risk (green) cases at first contact, which can lead to considering them “negative by lung ultrasound” get the test and the subject can be put in isolation; those “suggestive or positive by lung ultrasound” (yellow and red) with abnormal patterns ought to be early admitted into ER or ICU. This system allows professionals to determine the severity even at an out-of-hospital phase due to the acknowledgment of any suggestive imaging highly suspicious of severity. With portable or pocket devices at the patient's bedside the exploration allows re-asses in real time the condition of the critically ill in the ICU reducing time, money and the risk to a nosocomial exposure to the virus through the portable X-ray machines or in non-selective transport to CT scan room.
Figure 1.
POCUS triage protocol for COVID-19.
Funding
The present manuscript received no funding.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgment
Sergio Omar Paz Ortega, for the revision of the original manuscript from which this point of view derives.
References
- 1.Lichtenstein D., Goldstein I., Mourgeon E., Cluzel P., Grenier P., Rouby J.J. Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology. 2004;1:9–15. doi: 10.1097/00000542-200401000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Narula J., Chandrashekhar Y., Braunwald E. Time to add a fifth pillar to bedside physical examination: inspection, palpation, percussion auscultation, and insonation. JAMA Cardiol. 2018;3:346–435. doi: 10.1001/jamacardio.2018.0001. [DOI] [PubMed] [Google Scholar]
- 3.Cox E.G.M., Koster G., Baron A., et al. Should the ultrasound probe replace your stethoscope? A SICS-I sub-study comparing lung ultrasound and pulmonary auscultation in the critically ill. Crit Care. 2020;24:14. doi: 10.1186/s13054-019-2719-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kobal S.L., Trento L., Baharami S., Tolstrup K., Naqvi T.Z., Cercek B. Comparison of effectiveness of hand-carried ultrasound to bedside cardiovascular physical examination. Am J Cardiol. 2005;96:1002–1006. doi: 10.1016/j.amjcard.2005.05.060. [DOI] [PubMed] [Google Scholar]
- 5.Peris A., Tutino L., Zagli G., Batacchi S., Cianchi G., Spina R., et al. The use of point-of-care bedside lung ultrasound significantly reduces the number of radiographs and computed tomography scans in critically ill patients. Anesth Analg. 2010;111:687–692. doi: 10.1213/ANE.0b013e3181e7cc42. [DOI] [PubMed] [Google Scholar]
- 6.Buonsenso D., Piano A., Raffaelli F., Bonadia N., de Gaetano Donati K., Franceschi F. Point-of-Care Lung Ultrasound findings in novel coronavirus disease-19 pnemoniae: a case report and potential applications during COVID-19 outbreak. Eur Rev Med Pharmacol Sci. 2020;24:2776–2780. doi: 10.26355/eurrev_202003_20549. [DOI] [PubMed] [Google Scholar]
- 7.Lichtenstein D. Novel approaches to ultrasonography of the lung and pleural space: where are we now? Breathe (Sheff) 2017;13:100–111. doi: 10.1183/20734735.004717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peng Q., Wang X., Zhang L. Findings of lung ultrasonography of novel coronavirus pneumonia during the 2019-2020 epidemic. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05996-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang Y., Wang S., Liu Y., Zhang Y., Zheng C., Zheng Y., et al. A preliminary study on the ultrasonic manifestations of peripulmonary lesions of non-critical novel coronavirus pneumonia (COVID-19) Res Square[Preprint] 2020 doi: 10.21203/rs.2.24369/v1. [DOI] [Google Scholar]
- 10.Wang P., Liu Dw X.T., Yu K.J., et al. Consensus on severe diseases from Chinese ultrasound experts. Clin Focus. 2017;5:369–383. [Google Scholar]