Abstract
Background:
The six-minute walk test (6MWT) is a commonly used clinical assessment of exercise capacity in patients with cardiopulmonary or neuromuscular disease, but normal values are lacking for young adults, who are frequent subjects of testing.
Methods:
In a two-center study, 272 young adults, ages 18–50, underwent American Thoracic Society protocolized six-minute walk testing, and 56 underwent repeat testing. A linear regression model was developed based on anthropomorphic data. This model was compared to existing prediction equations.
Results:
Median 6MWD for the cohort was 637m (IQR 584 – 686m) and was not significantly impacted by age. This is in contrast to existing equations extrapolated from older subjects that predict increasing 6MWD in younger subjects. We found weak correlation of 6MWD with height, weight, BMI, and resting heart rate. Heart rate at completion correlated most strongly with 6MWD (rho 0.53 p <0.0001). Repeat 6MWD was surprisingly variable, with a median difference between tests of 32.5 ± 31.9m. Established reference equations performed poorly in this population, largely because age has much less effect on 6MWD in this group than in older adults.
Conclusions:
Established reference equations should be reconfigured to include data from young adults, as age has minimal effect on 6MWD in this population. Heart rate response may be a valuable measure of effort in normal subjects. Six-minute walk distance, as with pulmonary function and exercise testing, should have predictive equations across the spectrum of age to allow for accurate assessment of exercise limitation.
Keywords: Exercise Test, Reference Values, Cardiorespiratory Fitness
Introduction:
The six-minute walk test (6MWT) is a widely used measurement of exercise capacity in many conditions that affect young adults.1–6 Compared to more comprehensive laboratory tests like cardiopulmonary exercise testing, the 6MWT is easier to administer, less expensive, less invasive, and is easily repeated.7 Six-minute walk distance (6MWD) has been shown to be a reliable predictor of survival in several disease states.1,2,8–10 The change in 6MWD is commonly used as the primary outcome in clinical trials, with 575 trials in clinicaltrials.gov currently using 6MWD as an endpoint. The Federal Drug Administration has approved multiple medications on the basis of trials showing a change in 6MWD.4,11–15
The most commonly used reference values for 6MWD in American adults were derived from a study of 290 men and women aged 40–80 (mean age 61).16 Comparisons of observed-to-expected 6MWD are used to make prognostic statements and treatment decisions for younger patients who were not represented in this cohort.17 Previous studies have demonstrated discrepancy between the observed 6MWD of healthy young adults and the values estimated from these reference equations, but these studies have been limited by small size and patient characteristics that may not generalize to the United States (US).18–22 Thus, we tested the standard US reference equation, derived in older adults, against objective results of 6MWD in healthy young adults, hypothesizing that these equations would over-predict 6MWD in younger adults.16 We then developed comparative reference equations for this patient population based on anthropomorphic data.16
Methods:
This study was approved by the internal review boards at Vanderbilt University (#172128) and the Meharry Medical College (#18–10-866). Informed consent was obtained from all participants.
Study Population
Healthy volunteers were recruited via electronic research distribution lists, flyers, and internal institutional emails. Interested participants were directed to a secure online health survey and informed consent document (see online supplement). The inclusion criteria were healthy adults, ages 18–50. Exclusion criteria included pregnancy or any known cardiovascular, pulmonary, neurologic, metabolic, hematologic, or musculoskeletal diagnosis. Any uncertainties or questions about health status were addressed by the principal investigators, which included disqualification for any medication used to treat the listed chronic medical conditions (e.g. inhalers for mild asthma, anti-hypertensives). Volunteers who met all inclusion criteria and none of the exclusion criteria were contacted to schedule a 6MWT.
Outcomes
The primary outcome was the 6MWD as a function of age, compared to the prediction of current reference equations. A secondary goal was to develop a model based on age, height, weight, BMI and gender. Model fit is reported as Spearman correlation coefficients, R2, and optimism-adjusted R2 based on resampling validation on 300 bootstrap repetitions. Exploratory outcomes were correlation between 6MWD and resting and post-test heart rate, self-reported days of exercise per week, and daily step counts as measured by smartphones and wearable fitness devices.
Data Collection
Six-Minute Walk Test Protocol:
Participants were instructed to wear comfortable clothing and walking shoes, and to not exercise within 12 hours of the test. Prior to testing, all participants had height, weight, resting heart rate (seated) and oxygen saturation measured. Each subject completed a brief demographic survey, which included self-reported days of exercise per week, and average daily step count if available from a smartphone or wearable fitness device. Study personnel assisted participants in finding daily step counts on their devices if needed, and the longest available average (1 month – 1 year) was used.
Testing was performed at Vanderbilt University Medical Center and at Meharry Medical Center. In both locations, testing was performed along a 100ft (30m) indoor track with firm flooring, marked at regular intervals. All participants were read the same standardized instructions, slightly adapted from the American Thoracic Society (ATS) guidelines (see online data supplement).17 Per ERS/ATS guidelines, the test included only scripted encouragement, and at each minute the participants were informed of the time remaining.23 At the conclusion of 6 minutes, the test administrator measured the participant’s heart rate and oxygen saturation, recorded the 6MWD, and administered the Borg Dyspnea and Fatigue scale questionnaires.24
All participants who completed initial testing were contacted electronically and asked to perform a repeat test, with the same protocol as listed above, on a separate day. Study data were collected and managed using REDCap electronic data capture tools.25
Statistical Analyses
Data are presented as median and interquartile range or count and percentage. Differences between paired continuous variables are assessed using the Wilcoxon signed-rank test. Spearman correlation coefficients are reported for the relationship between prediction models and observed 6MWD, as well as heart rates, self-reported activity level, daily step counts and observed 6MWD.
Details of the development of the reference equation can be found in the supplement. In summary, a linear regression model of 6MWD was constructed using demographic and anthropometric variables, as has been done in previous 6MWD reference equations.16,19,20,26,27 These included age, height, weight, and sex. The accuracy of the prediction models in our population were assessed using Spearman correlation coefficients, and R2 or sum of squared errors. Bootstrapping was performed for validation and correction for optimism.
Statistical analyses were performed using STATA statistical software package (Version 15 for Mac) and R version 3.5.2 (R foundation for Statistical Computing, Vienna, Austria).
Results:
Study Population:
Two hundred and seventy-two participants completed an initial 6MWT (Table 1). The median age of the population was 32.5 years (interquartile range (IQR) 27 – 39 years), 70% were female, and the median BMI was 24.9 (IQR 21.8 – 27.9). Most participants reported being at least moderately physically active, and none were current smokers. Forty-nine percent of the participants either wore a fitness watch or had a smartphone app that tracked daily step counts.
Table 1:
Characteristics of the Study Population (n=272)
| Median or % (IQR) | |
|---|---|
| Age (years) | 32.5 (27 – 39) |
| Gender (Female) | 70% |
| Race | |
| White | 69% |
| Black | 15% |
| Asian | 9% |
| Hispanic | 2% |
| Height (cm) | 169 (164 – 176) |
| Weight (kg) | 72 (61 – 84) |
| BMI (kg/m2) | 24.9 (21.8 – 27.9) |
| Ever smoker | 11% |
| Current smoker | 0% |
| Exercise days per week* | |
| 0 | 13% |
| 1 – 2 | 29% |
| 3 – 5 | 44% |
| 6 – 7 | 13% |
| mHealth device † | 49% |
| Daily step count | 7500 (5413 – 10,000) |
| Resting HR | 75 (67 – 85) |
| Resting SPO2 | 98% (98 – 99) |
| Post-test heart rate | 120 (103 – 138) |
| ΔHeart rate (post-test – resting) | 43 (27 – 59) |
| Percent of Maximum heart rate achieved‡ | 64% (55% – 74%) |
| Post-test SPO2 | 98% (98 – 99) |
| Six-minute walk distance (m) | 637 (584 – 686) |
Self-reported “Aerobic or lower body exercise for greater than 20 minutes”
Includes wearable fitness device or smart phone with step counter
Maximum heart rate = 220 – age
Mean 6MWD for the population was 636 ± 88m, and participants increased their heart rate by 45 ± 23 beats per minute to 65% ± 14% of their predicted maximum heart rate (220 – age).
Multivariable Modeling for Prediction of 6MWD:
The linear multiple regression model for the outcome of predicted 6MWD included the 272 initial 6MWTs from all participants. There were no missing data for the variables of interest.
The model incorporates only pre-test demographic and anthropometric variables. The reference equation and model fit characteristics are presented in table 2. To compare effect sizes of the predictors, we calculated the change in predicted 6MWD expected by increasing from the 25th percentile to the 75th percentile of the population of that given variable, while holding all other predictors constant (table 3). This shows that among the anthropometric variables, age has the smallest effect, whereas height, weight, and gender are all significant predictors, with weight having the greatest effect.
Table 2:
Reference Equation
| Prediction Model | Reference equation | Spearman Correlation | Adjusted R2 |
|---|---|---|---|
| Enright Model | 6MWD(m) [female] = (2.11 × height(cm)) – (2.29 × weight(kg)) - (5.78 × age) + 667 6MWD (m) [male] = (7.57 × height(cm)) – (5.02 × age) – (1.76 × weight(kg)) – 309 |
0.335 | n/a |
| Chetta Model | 6MWD(m) [female]= (1.25 × height(cm)) – (2.816 × age) + 479.783 6MWD(m) [male]= (1.25 × height(cm)) – (2.816 × age) + 518.853 |
0.233 | 0.05 |
| Gibbons Model | 6MWD(m) [female] = 794.1 – (age × 2.99) 6MWD(m) [male] = 868.8 – (age × 2.99) |
0.213 | 0.042 |
| Model 1 | 6MWD(m) [female] = (2.64 × height(cm)) – (2.12 × weight(kg)) + (0.12 × age) + 330.2 6MWD(m) [male] = (6.22 × height(cm)) – (2.99 × weight(kg)) – (0.52 × age) – 183.06 |
0.457 | 0.196 |
6MWD = six-minute walk distance
Table 3:
Effect Sizes of Predictor Variables in New Prediction Model
| Predictor | 25th Percentile Value | 75th Percentile Value | Δ6MWD(m) by increasing from 25th to 75th percentile (95% CI)* |
|---|---|---|---|
| Age (years) | 27 | 39 | 1.44m (−15.51 – 18.4) |
| Height (cm) | 164 | 176 | 31.68m (9.31 – 54.06) |
| Weight (kg) | 60.75 | 84 | −49.37m (−67.11 – −31.63) |
| Sex (Male : Female) | 8.76m (−22.87 – 40.39) |
Estimated effect sizes of the predictors as calculated by the change in predicted 6MWD expected by increasing from the 25th percentile to the 75th percentile of the population of that given variable, while holding all other predictors constant
Reference Equation Performance in Healthy Participants:
Our new 6MWD prediction model, incorporating age, height, weight, and sex, had a Spearman correlation coefficient of 0.457, and adjusted R2 of 0.196 (Table 2). Residual plots of predicted vs. observed 6MWD using this model show that it tends to over-predict participants with low 6MWD, and under-predict those with high 6MWD (e-Figure 1).
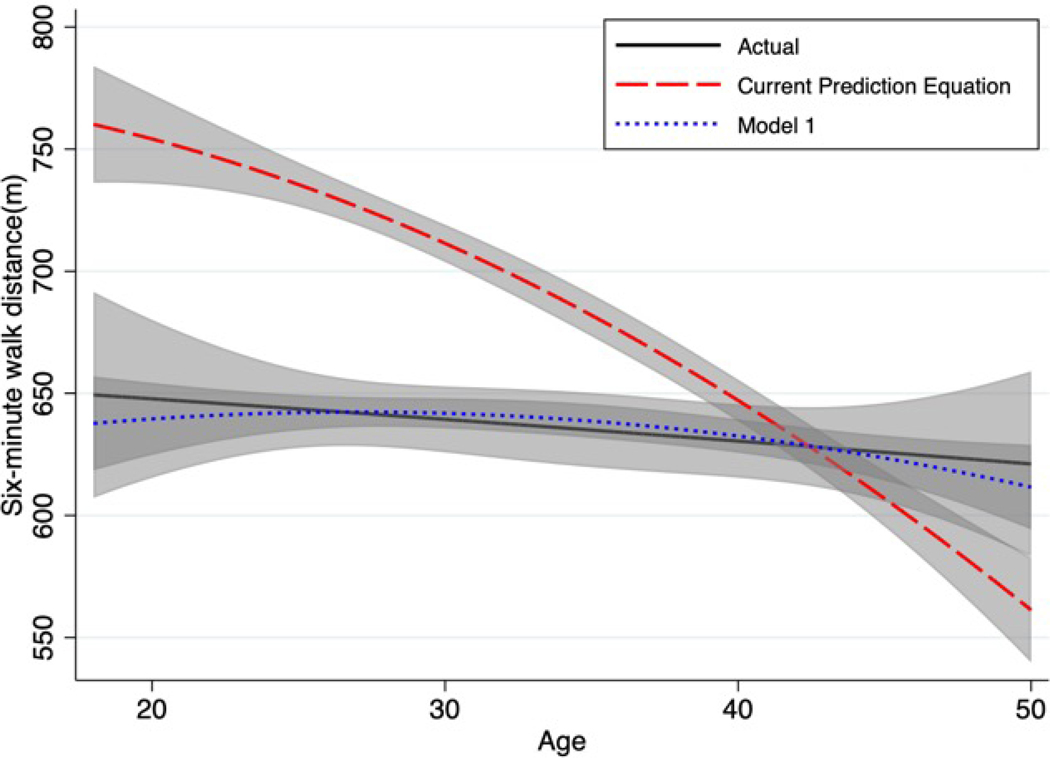
We tested the most commonly used 6MWD prediction model in our population, which yielded a Spearman correlation coefficient of 0.335.16 The sum square of errors for this model was greater than the total sum of squared errors for the sample, so R2 could not be calculated. We also tested the reference equations developed by Chetta and Gibbons in younger adults, and these also did not accurately predict 6MWD in our population (Table 2).18,19 When comparing the most common US prediction model to our prediction model, it over-estimated 6MWD in younger participants (Figure 1).
Figure 1:
Prediction models for six-minute walk distance versus age in the study population. Lines represent quadratic regression fit, and shaded areas represent 95% CI of the mean.
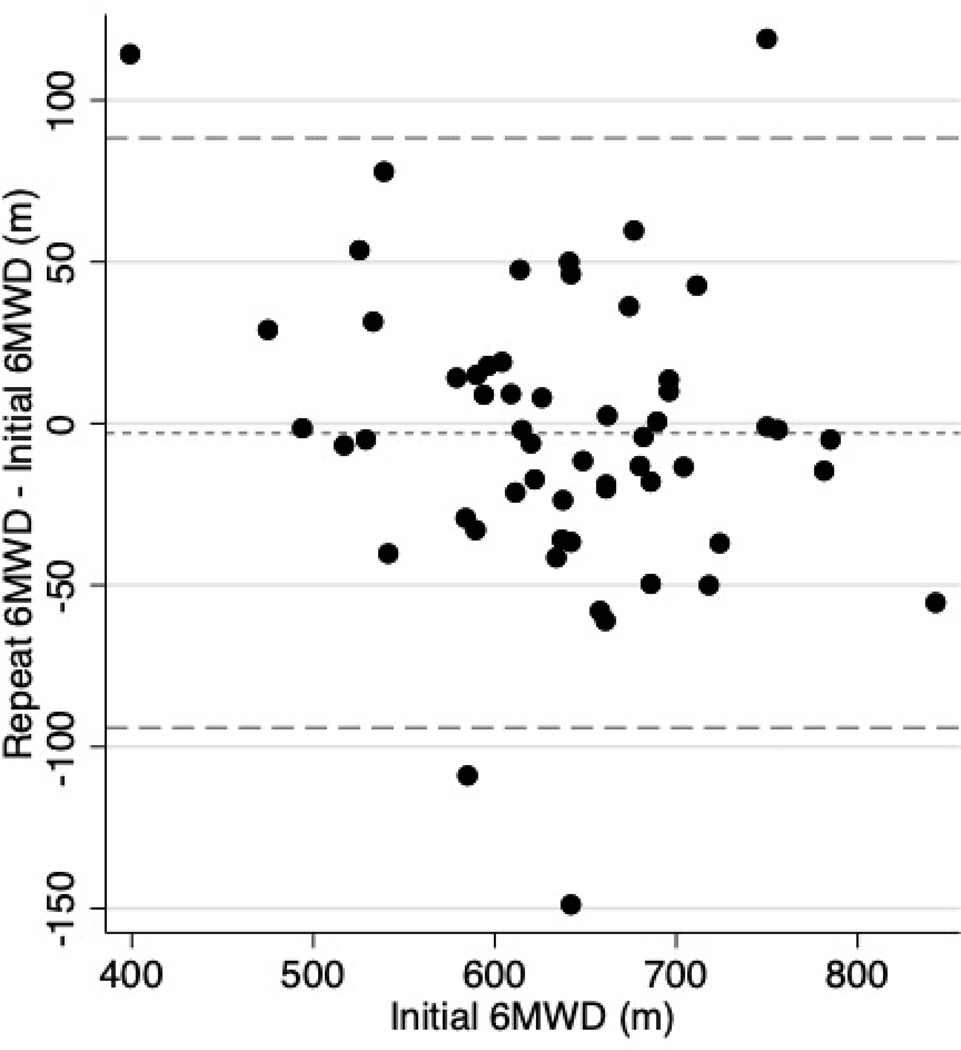
Reproducibility of 6MWT
Among the 56 participants who underwent repeat testing (median time between tests = 147 days, IQR 121 to 168 days) we found no significant difference in mean 6MWD between the first and second test (642m vs. 621m, p=0.436), however, there was intra-individual variability in 6MWD, with an average difference between tests of 32.5 ± 31.9m (Figure 2).
Figure 2:
Bland-Altman plot of change in six-minute walk distance (6MWD) between the first and second tests versus initial 6MWD among participants whom underwent repeat testing (n=56). Dotted lines represent the mean change in 6MWD and 95% confidence interval.
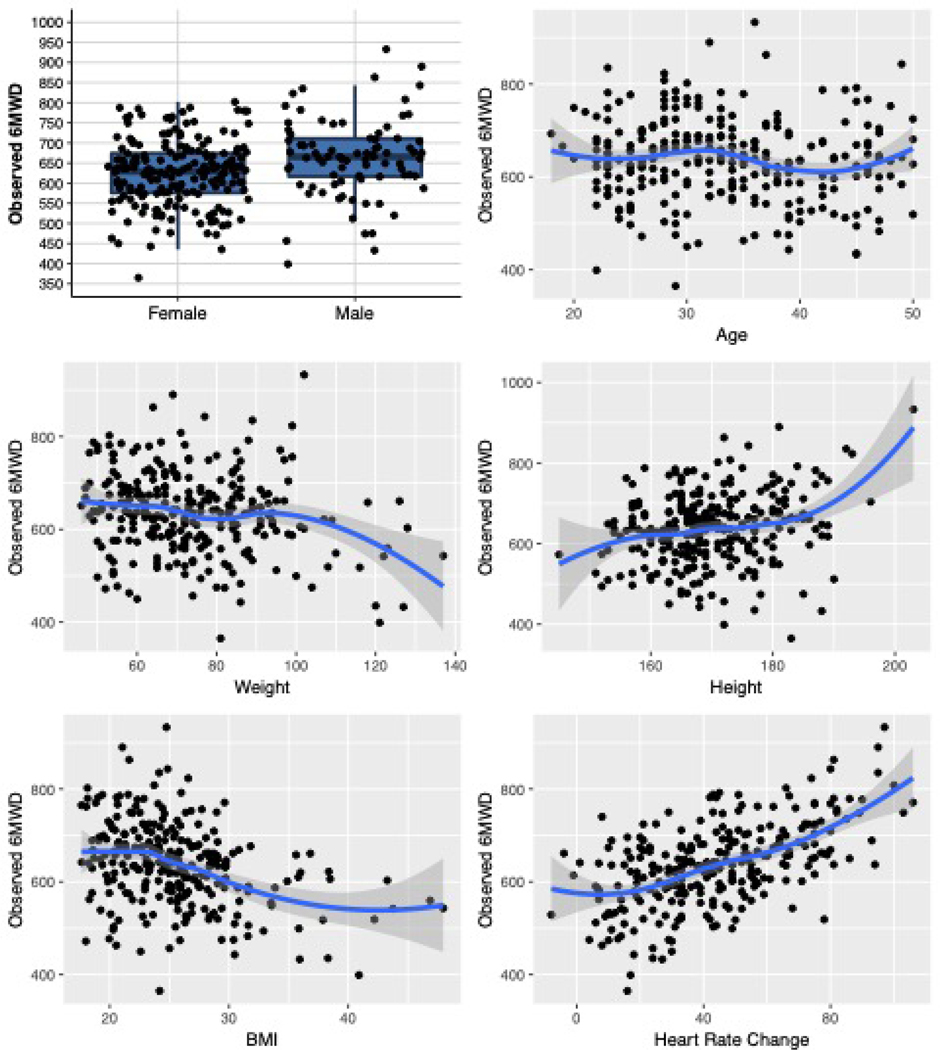
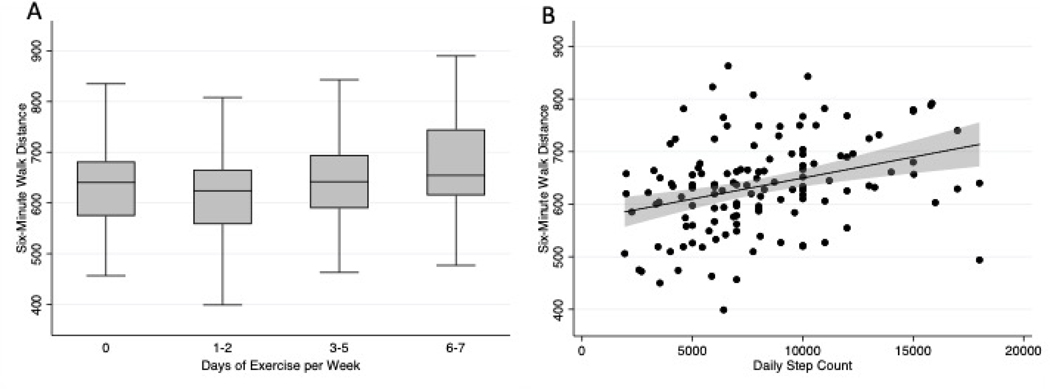
Exploratory Outcomes and Associations with 6MWD
Higher resting heart rate correlated with shorter 6MWD (rho −0.23 p = 0.0001). Increase in heart rate during testing (from resting to immediately post-test) correlated more strongly with 6MWD than any other single variable (rho 0.53 p <0.0001) (Figure 3). Number of self-reported exercise days per week (rho 0.15 p = 0.02), and daily step counts from smartphones or wearable fitness devices (rho 0.35 p < 0.0001) are both correlated with 6MWD (Figure 4).
Figure 3:
Univariate plots of observed 6MWD vs. predictor variables. Lines represent fitted spline regression with 95% confidence interval of the mean.
Figure 4 A&B:
A: Six-minute walk distance by number of self-reported days of exercise per week.
B: Six-minute walk distance versus average daily step count obtained from participants’ smartphone or wearable fitness device. The line represents a linear prediction with 95% confidence interval of the mean.
Discussion:
This data reveals that the existing reference equation for predicted 6MWD in American adults over-predicts 6MWD in a younger population, age 18–50.16 Other reference equations developed for predicting 6MWD in younger adults in smaller, international populations also did not accurately predict 6MWD in our cohort.18,19 Consistent with prior studies, we found that height, weight, and gender correlate with 6MWD. Age, however, which has been strongly predictive of 6MWD in most studies, especially among older adults, had minimal effect in our cohort.28 We have shown that the ability of any model using only anthropometric variables to predict 6MWD in healthy participants is likely to be limited, and this is largely due to variation in participant effort. This is suggested by the strong correlation between increase in heart rate during testing and 6MWD, and intra-individual repeat testing variability.
Clinical interpretation of a 6MWT is contingent on comparing a patient’s actual six-minute walk distance to a set reference value, and without accurate refence values a clinician’s ability to prognosticate and guide treatment is hampered, and clinical trial data interpretation may be limited. We have developed a reference equation for our cohort, and propose that further experiments are warranted to increase the cohort size, parse variables such as gender, and make new associations with subject physical activity and basal heart rate. As with predictive equations in pulmonary function and exercise testing, this information will improve assessment of the functional limitation of younger patients with cardiopulmonary disease. 17
We speculate on why the 6MWD is relatively flat compared to age in our cohort. The kilometers per hour (kph) corresponding to the mean speed of 642m/6 min is 6.4 kph. In most studies of locomotion, the speed threshold for converting from rapid walking to jogging is about 6.4 – 7.2 kph.29 Thus, the 6-minute walk speed is not linear, and has a ceiling before a subject finds jogging more comfortable.30 It seems likely that this walking speed limit influences the data we have generated, and makes the extrapolations from reference equations developed in older populations unrealistically high. At age 20 in current predictions, the predicted mean 6MWD for our cohort is roughly 760m, which equates to a walking speed of 7.6 kph.16 Also, it is well recognized that exercise capacity declines with age, however it is likely that this decline is not linear. The aerobic capacity lost between ages 20 and 40 is not proportional to that lost between ages 50 and 70, for example. This has been previously shown among non-sedentary adults, though few longitudinal exercise studies have examined varying rates of decline over time.31,32
The importance of using percent of predicted 6MWD to guide treatment and prognostication can also be seen by applying these reference equations to our study population. The “minimal important difference” for change in 6MWD has been determined for diseases such as pulmonary arterial hypertension, congestive heart failure, COPD, and diffuse parenchymal lung diseases, and typically ranges from 2536m.33–37 These studies treat the minimal important difference as an absolute value across the entire population, however, a 30m change from baseline would represent a 3.4% change in predicted 6MWD for one participant in our study, and a 6.3% change in another, based off their height, weight, sex, and age. A more personalized approach to treatment would entail determining what an individual’s 6MWD is compared to a population-appropriate reference equation, and interpreting change in 6MWD as relative to the reference value.
Our study found surprising variability in 6MWD with repeat testing, in tests performed weeks to months apart. Previous studies have shown a significant learning effect in both healthy and diseased populations, but primarily in repeat tests within the same day.38,39 Our study may be more reflective of clinical practice, where patients are more likely to perform one 6MWT per visit, and repeat it once at a follow-up visit. Our data suggests that the repeat test effect is less pronounced when testing is carried out in this manner, at least among healthy participants. However, it also notable that intra-individual variability in 6MWD between tests can be quite high among this healthy population, upwards of 50–100m. This finding further suggests that measuring effort, which may vary from one visit to the next, should be an important aspect of clinical six-minute walk testing.
We have presented data that assessments of physical fitness, such as resting heart rate and self-reported days of exercise per week correlate with 6MWD in this population. While using self-reported variables such as exercise is exploratory, and prone to bias, all of the available data points towards physical fitness significantly affecting 6MWD, even in otherwise healthy young adults.
Daily step counts from wearable devices with accelerometers have previously been shown to correlate with 6MWD in diseased populations, and our study suggests that this may be true in healthy populations as well.40,41 With the increasing availability and use of mobile health devices, utilizing data from these devices to assess patient’s health status may be of clinical interest, and merits further investigation.
Our study has a number of limitations. Participants were recruited from two academic medical centers, and may not be reflective of a broader national population. However, this is the largest study to date of 6MWD in healthy young American adults, and is more demographically diverse than most previous studies. We also have limited observations of individuals at the extremes of height and weight. A relatively small number of subjects underwent repeat 6MWD testing (56 out of 272), which limits the generalizability of our findings of high intra-individual 6MWD variability. Although participants were provided with a structured questionnaire about health conditions at screening, they did not undergo physical examinations, and medical records were not reviewed. It is therefore possible that some of the self-reported “healthy” participants had a disqualifying medical condition. Lastly, our prediction model did not perform particularly well, even within the study population from which it was derived (adjusted R2 of 0.196), and this has been seen in other reference equations as well.18,19,26 This suggests that developing a highly accurate prediction model for 6MWD in this population is probably not feasible, due to unmeasured variables such as participant effort. Future efforts to develop reference equations should find ways to incorporate objective measures of participant effort, and perhaps modify the current scripted instructions to ensure more consistent understanding among subjects. Clinically, the available reference equations are still useful for approximation of a patient’s level of debility and prognosis, and trends in 6MWD on serial evaluations provide additional prognostic information.5,8,42,43
Conclusions:
Established reference equations for 6MWD dramatically over-predict 6MWD in healthy young adults. A reference equation developed from our cohort differs significantly from those developed in populations of older adults because age does not have a strong effect on 6MWD in adults aged 18–50. This may be due to a ceiling effect of walk speed at the threshold of jogging. This information may improve assessment of exercise limitation with age-appropriate reference values.
Supplementary Material
Highlights:
Current reference equations for six-minute walk distance (6MWD) dramatically over-estimate 6MWD in healthy young adults
Age has minimal impact on walking speed in healthy young adults.
Reference equations for 6MWD should be revised to include broader demographics.
Acknowledgments
Funding Information:
This study was supported in part by the Vanderbilt CTSA grant UL1TR002243 from NCATS/NIH
SJH was supported by NIH T32 HL087738–12; ELB is supported by NIH grant R34HL136989–01, American Heart Association (13FTF16070002), Gilead Sciences Scholars Program in Pulmonary Arterial Hypertension. ARH is supported by NIH grant UO1HL125212–01.
Abbreviations List:
- 6MWD
Six-minute walk distance
- 6MWT
Six-Minute walk test
- ATS
American Thoracic Society
- COPD
Chronic obstructive pulmonary disease
- ERS
European Respiratory Society
- IQR
Interquartile range
- US
United States
Footnotes
An earlier version of these findings was published in abstract form and presented at the ATS International Conference in Dallas, TX. on May 21, 2019.
This article has an online data supplement.
Conflicts of interest:
SJH reports no conflicts of interest. ARH has served as a consultant to Actelion, Bayer, GSK, Accleron, United Therapeutics and Pfizer. She has received research/grant support from the NIH and Cardiovascular Medical Research and Education Fund. ELB has served as a consultant for Hovione Pharmaceuticals.
References:
- 1.Kadikar A, Maurer J, Kesten S. The six-minute walk test: a guide to assessment for lung transplantation. The Journal of heart and lung transplantation : the official publication of the International Society for Heart Transplantation. 1997;16(3):313–319. [PubMed] [Google Scholar]
- 2.Cahalin L, Pappagianopoulos P, Prevost S, Wain J, Ginns L. The relationship of the 6-min walk test to maximal oxygen consumption in transplant candidates with end-stage lung disease. Chest. 1995;108(2):452–459. [DOI] [PubMed] [Google Scholar]
- 3.Guyatt GH, Sullivan MJ, Thompson PJ, et al. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Canadian Medical Association journal. 1985;132(8):919–923. [PMC free article] [PubMed] [Google Scholar]
- 4.Mathai SC, Puhan MA, Lam D, Wise RA. The Minimal Important Difference in the 6-Minute Walk Test for Patients with Pulmonary Arterial Hypertension. American Journal of Respiratory and Critical Care Medicine. 2012;186(5):428–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martin C, Chapron J, Hubert D, et al. Prognostic value of six minute walk test in cystic fibrosis adults. Respiratory medicine. 2013;107(12):1881–1887. [DOI] [PubMed] [Google Scholar]
- 6.Montes J, McDermott MP, Martens WB, et al. Six-Minute Walk Test demonstrates motor fatigue in spinal muscular atrophy. Neurology. 2010;74(10):833–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Galie N, Humbert M, Vachiery JL, et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). European heart journal. 2016;37(1):67–119. [DOI] [PubMed] [Google Scholar]
- 8.Castleberry AW, Englum BR, Snyder LD, et al. The utility of preoperative six-minute-walk distance in lung transplantation. American journal of respiratory and critical care medicine. 2015;192(7):843–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bittner V, Weiner DH, Yusuf S, et al. Prediction of mortality and morbidity with a 6-minute walk test in patients with left ventricular dysfunction. SOLVD Investigators. Jama. 1993;270(14):1702–1707. [PubMed] [Google Scholar]
- 10.Cahalin LP, Mathier MA, Semigran MJ, Dec GW, DiSalvo TG. The six-minute walk test predicts peak oxygen uptake and survival in patients with advanced heart failure. Chest. 1996;110(2):325–332. [DOI] [PubMed] [Google Scholar]
- 11.Galiè N, Ghofrani HA, Torbicki A, et al. Sildenafil Citrate Therapy for Pulmonary Arterial Hypertension. New England Journal of Medicine. 2005;353(20):2148–2157. [DOI] [PubMed] [Google Scholar]
- 12.Galie N, Brundage BH, Ghofrani HA, et al. Tadalafil therapy for pulmonary arterial hypertension. Circulation. 2009;119(22):2894–2903. [DOI] [PubMed] [Google Scholar]
- 13.Rubin LJ, Badesch DB, Barst RJ, et al. Bosentan therapy for pulmonary arterial hypertension. N Engl J Med. 2002;346(12):896–903. [DOI] [PubMed] [Google Scholar]
- 14.Simonneau G, Rubin LJ, Galie N, et al. Addition of sildenafil to long-term intravenous epoprostenol therapy in patients with pulmonary arterial hypertension: a randomized trial. Annals of internal medicine. 2008;149(8):521–530. [DOI] [PubMed] [Google Scholar]
- 15.Galie N, Badesch D, Oudiz R, et al. Ambrisentan therapy for pulmonary arterial hypertension. Journal of the American College of Cardiology. 2005;46(3):529–535. [DOI] [PubMed] [Google Scholar]
- 16.Enright PL, Sherrill DL. Reference equations for the six-minute walk in healthy adults. American journal of respiratory and critical care medicine. 1998;158(5 Pt 1):1384–1387. [DOI] [PubMed] [Google Scholar]
- 17.Statement ATS. American journal of respiratory and critical care medicine. 2002;166(1):111–117. [DOI] [PubMed] [Google Scholar]
- 18.Chetta A, Zanini A, Pisi G, et al. Reference values for the 6-min walk test in healthy subjects 20–50 years old. Respiratory medicine. 2006;100(9):1573–1578. [DOI] [PubMed] [Google Scholar]
- 19.Gibbons WJ, Fruchter N, Sloan S, Levy RD. Reference values for a multiple repetition 6-minute walk test in healthy adults older than 20 years. Journal of cardiopulmonary rehabilitation. 2001;21(2):87–93. [DOI] [PubMed] [Google Scholar]
- 20.Zou H, Zhang J, Chen X, et al. Reference Equations for the Six-Minute Walk Distance in the Healthy Chinese Han Population, Aged 18–30 Years. BMC pulmonary medicine. 2017;17(1):119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cote CG, Casanova C, Marin JM, et al. Validation and comparison of reference equations for the 6-min walk distance test. The European respiratory journal. 2008;31(3):571–578. [DOI] [PubMed] [Google Scholar]
- 22.Alameri H, Al-Majed S, Al-Howaikan A. Six-min walk test in a healthy adult Arab population. Respiratory medicine. 2009;103(7):1041–1046. [DOI] [PubMed] [Google Scholar]
- 23.Holland AE, Spruit MA, Troosters T, et al. An official European Respiratory Society/American Thoracic Society technical standard: field walking tests in chronic respiratory disease. The European respiratory journal. 2014;44(6):1428–1446. [DOI] [PubMed] [Google Scholar]
- 24.Borg GA. Psychophysical bases of perceived exertion. Medicine and science in sports and exercise. 1982;14(5):377–381. [PubMed] [Google Scholar]
- 25.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Casanova C, Celli BR, Barria P, et al. The 6-min walk distance in healthy subjects: reference standards from seven countries. The European respiratory journal. 2011;37(1):150–156. [DOI] [PubMed] [Google Scholar]
- 27.Troosters T, Gosselink R, Decramer M. Six minute walking distance in healthy elderly subjects. European Respiratory Journal. 1999;14(2):270–274. [DOI] [PubMed] [Google Scholar]
- 28.Singh SJ, Puhan MA, Andrianopoulos V, et al. An official systematic review of the European Respiratory Society/American Thoracic Society: measurement properties of field walking tests in chronic respiratory disease. The European respiratory journal. 2014;44(6):1447–1478. [DOI] [PubMed] [Google Scholar]
- 29.THORSTENSSON A, ROBERTHSON H. Adaptations to changing speed in human locomotion: speed of transition between walking and running. Acta Physiologica Scandinavica. 1987;131(2):211–214. [DOI] [PubMed] [Google Scholar]
- 30.Frost AE, Langleben D, Oudiz R, et al. The 6-min walk test (6MW) as an efficacy endpoint in pulmonary arterial hypertension clinical trials: demonstration of a ceiling effect. Vascular pharmacology. 2005;43(1):36–39. [DOI] [PubMed] [Google Scholar]
- 31.Pimentel AE, Gentile CL, Tanaka H, Seals DR, Gates PE. Greater rate of decline in maximal aerobic capacity with age in endurance-trained than in sedentary men. Journal of Applied Physiology. 2003;94(6):2406–2413. [DOI] [PubMed] [Google Scholar]
- 32.Wilson TM, Tanaka H. Meta-analysis of the age-associated decline in maximal aerobic capacity in men: relation to training status. American Journal of Physiology-Heart and Circulatory Physiology. 2000;278(3):H829–H834. [DOI] [PubMed] [Google Scholar]
- 33.Holland AE, Hill CJ, Rasekaba T, Lee A, Naughton MT, McDonald CF. Updating the Minimal Important Difference for Six-Minute Walk Distance in Patients With Chronic Obstructive Pulmonary Disease. Archives of Physical Medicine and Rehabilitation. 2010;91(2):221–225. [DOI] [PubMed] [Google Scholar]
- 34.Mathai SC, Puhan MA, Lam D, Wise RA. The minimal important difference in the 6-minute walk test for patients with pulmonary arterial hypertension. American journal of respiratory and critical care medicine. 2012;186(5):428–433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Polkey MI, Spruit MA, Edwards LD, et al. Six-Minute-Walk Test in Chronic Obstructive Pulmonary Disease. American journal of respiratory and critical care medicine. 2013;187(4):382–386. [DOI] [PubMed] [Google Scholar]
- 36.Holland AE, Hill CJ, Conron M, Munro P, McDonald CF. Small changes in six-minute walk distance are important in diffuse parenchymal lung disease. Respiratory medicine. 2009;103(10):1430–1435. [DOI] [PubMed] [Google Scholar]
- 37.Täger T, Hanholz W, Cebola R, et al. Minimal important difference for 6-minute walk test distances among patients with chronic heart failure. International journal of cardiology. 2014;176(1):94–98. [DOI] [PubMed] [Google Scholar]
- 38.Wu G, Sanderson B, Bittner V. The 6-minute walk test: how important is the learning effect? American heart journal. 2003;146(1):129–133. [DOI] [PubMed] [Google Scholar]
- 39.Knox AJ, Morrison JF, Muers MF. Reproducibility of walking test results in chronic obstructive airways disease. Thorax. 1988;43(5):388–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mudge S, Stott NS. Timed Walking Tests Correlate With Daily Step Activity In Persons With Stroke. Archives of Physical Medicine and Rehabilitation. 2009;90(2):296–301. [DOI] [PubMed] [Google Scholar]
- 41.Mainguy V, Provencher S, Maltais F, Malenfant S, Saey D. Assessment of daily life physical activities in pulmonary arterial hypertension. PloS one. 2011;6(11):e27993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lee WT, Peacock AJ, Johnson MK. The role of per cent predicted 6-min walk distance in pulmonary arterial hypertension. The European respiratory journal. 2010;36(6):12941301. [DOI] [PubMed] [Google Scholar]
- 43.Lederer DJ, Arcasoy SM, Wilt JS, D’Ovidio F, Sonett JR, Kawut SM. Six-Minute-Walk Distance Predicts Waiting List Survival in Idiopathic Pulmonary Fibrosis. American journal of respiratory and critical care medicine. 2006;174(6):659–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.