Abstract
Purpose of Review
The goal of this review is to introduce surgical decision-making pearls for reverse shoulder arthroplasty and describe optimization of surgical exposure for reverse shoulder arthroplasty.
Recent Findings
While the technology of reverse shoulder replacement and the associated prosthetic options have expanded, the principles involved in successfully exposing the humerus and glenoid in arthroplasty remain the same.
Summary
Reverse shoulder replacement should be considered in arthroplasty situations with rotator cuff disease, deformity, bone loss, and instability as part of the diagnosis. Optimal exposure in reverse shoulder arthroplasty can be obtained by (1) releasing deltoid adhesions, (2) removal of humeral osteophytes, (3) generous humeral head cuts, (4) thorough humeral and glenoid capsular release and (5) optimal glenoid retractor placement. Neuromuscular paralysis can also aid glenoid exposure.
Keywords: Reverse shoulder arthroplasty; Reverse shoulder replacement; Indications; Glenoid exposure, lateralized prosthesis; Preoperative planning
Introduction
The reverse shoulder arthroplasty is the most important advance in shoulder arthroplasty in the past 30 years. Originally designed by Grammont, the initial iterations of the reverse device were prone to early failure and loosening [1, 2]. However, since the initial Grammont design, there has been an explosion in reverse replacement technology, increasing the surgical options and complexity of the operation [3]. Improvements in fixation techniques, ingrowth materials, biomaterials, and bearing surfaces have improved the longevity of the prostheses [4–7]. Also, abundant design developments have expanded the surgical options for the shoulder arthroplasty surgeon. Different manufacturers have expanded the options for the shoulder arthroplasty surgeon including different humeral prosthesis neck/shaft angles, bearing diameter, bearing constraint (depth), modular stems convertible between anatomic and reverse TSA, modular tumor reconstruction prostheses, humeral stem length, humeral bearing onlay versus inlay, glenosphere offset, glenosphere laterality, and augmented baseplate components [8•, 9, 10, 11•, 12, 13, 14••]. In addition, preoperative planning software has advanced dramatically, allowing for the development of 3-D printed custom guides and custom implants, and even intraoperative computer guidance of implant placement [15–18].
Surgical Decision Making and Indications
The surgical options available mean that the importance of preoperative decision making is more critical than ever. The most important surgical decision to make when embarking on a shoulder arthroplasty is whether to perform a conventional shoulder replacement versus a reverse shoulder replacement. In our practice, patients are evaluated with a series of four radiographs (A/P, Grashey, scapular-Y, and axillary). In addition to two-dimensional imaging, we also obtain both CT and MRI scans. CT scan enables accurate assessment of bone stock available for reconstruction, classification of the glenoid via the Walch classification, and facilitates modeling and preoperative planning using commercially available planning software [19–21]. In our practice, we evaluate all shoulders with conventional MRI (arthrography is typically not necessary). MRI is used to evaluate the status of the deltoid and each rotator cuff muscle based on the Goutallier classification [22].
Conventional (anatomic) total shoulder arthroplasty is indicated mainly for five diagnoses in our practice (Table 1). The indications for reverse total shoulder arthroplasty are much broader (Table 2). Reverse shoulder arthroplasty should be a strong consideration in any shoulder arthroplasty situation where there is (1) a problem with the rotator cuff, (2) post-traumatic or postsurgical bone loss, (3) shoulder instability, and (4) post-traumatic or postsurgical deformity [10], [23–26].
Table 1.
Indications for anatomic total shoulder arthroplasty
| Diagnosis | Comment |
|---|---|
| Osteoarthritis | Rotator cuff must be intact and glenoid bone stock adequate |
| Inflammatory Arthritis | Rotator cuff more variable than in osteoarthritis and osteopenia may be present |
| Post-traumatic arthritis | Tuberosity/Cuff minimally affected/acceptable deformity |
| Post instability surgery arthritis | Subscapularis often questionable |
| Avascular Necrosis | Occasionally hemiarthroplasty indicated in the very young patient |
Table 2.
Indications for reverse total shoulder arthroplasty
| Diagnosis | Comment |
|---|---|
| Rotator cuff arthropathy | Classically described as arthritis that develops first at the acromiohumeral interface |
| Massive irreparable rotator cuff tear in the elderly | With or without previous attempt at repair |
| Four part unreconstructable proximal humerus fracture | Particularly in the elderly |
| Chronic shoulder dislocation in the elderly | |
| Reconstruction after tumor resection | |
| Failed previous replacement with cuff failure and/or instability | |
| Any of the diagnoses listed in table one with rotator cuff problem, bone loss, instability, or severe deformity not conducive to anatomic TSA | For example, an elderly patient with intact rotator cuff may be better suited for reverse TSA due to glenoid bone loss due to B2 or B3 glenoid morphology |
A complete discussion of rotator cuff biomechanics is beyond the scope of this review; thorough reviews of this topic have been published [27, 28]. In general, we use an onlay style lateralized reverse shoulder design because we appreciate the benefits of additional prosthetic stability and minimization of scapular notching afforded by lateralization [29••], [30]. However, in the case of the petite, elderly female, we worry about acromial stress fractures and are more apt to use an inlay type humeral component with overall less distalization and lateralization (i.e., less deltoid tension) of the construct [31, 32]. In general, larger bearing surfaces are reserved for larger men and constrained increased depth humeral polyethylene trays are reserved for revisions. We have found that commercially available augmented glenoid baseplate components very useful in managing glenoid bone loss with prosthetic augmentation as opposed to aggressive reaming [14••]. Surgical success can be achieved with any of the diverse array of surgical systems available. Preoperative planning and individualization of the surgery is critical as is extensive familiarity with the chosen implant system. We plan all glenoid implantations using commercially available software based on preoperative CT; custom implant guides and intraoperative navigation are also useful in complex cases [21].
Once the implant system is chosen and preoperative planning is complete, obtaining excellent exposure is critical for a successful implantation of reverse replacement components.
Surgical Pearls to Optimize Exposure in Reverse Shoulder Arthroplasty
Setup and Initial Exposure
We use the beach chair position with the head elevated to 45 degrees [33]. General endotracheal anesthesia is administered in addition to a single shot interscalene block. We ask the anesthesiologist for neuromuscular paralysis especially during glenoid exposure [33, 34]. Our surgical incision begins just above the coracoid process and ends just above the axillary crease [35]. Larger incisions are required for muscular males. A deltopectoral approach is utilized taking the cephalic vein lateral with the deltoid [34]. One centimeter of pectoralis major is released to increase exposure [35]. The coracoacromial ligament if present is usually left intact. At this point it is critical to perform a release of the shoulder “spaces” including the subacromial, subdeltoid, and subconjoint spaces [20, 34, and 36]. These releases are usually accomplished bluntly using finger dissection but occasionally require electrocautery [33]. The deltoid release is particularly critical as deltoid adhesions will prevent posterior humeral translation when it is time to expose the glenoid [20, 33]. Once the deltoid adhesions have been released, a Kolbel self-retaining retractor is placed with one blade under the deltoid and one blade under the conjoint tendon.
Humeral Preparation
Once the self-retaining retractor has been placed, we turn our attention to exposing and preparing the humerus. The long head biceps, if present, is tenotomized from the supraglenoid tubercle and tenodesed to the pectoralis major tendon [35]. A subscapularis peel is performed at this time progressing from superolateral to inferomedial, cauterizing the anterior humeral circumflex vessels at its inferior extent [33, 34]. We have found that subscapularis peel is particularly useful in reverse arthroplasty as it allows us to manage intact and partially torn subscapularis tendons in the same fashion. In addition, lesser tuberosity osteotomy and subscapularis tenotomy are not as useful in reverse arthroplasty as after the implantation of the reverse replacement is complete, the tendon often no longer reaches its native site due to the new relatively inferior and lateral position of the humerus. Once the peel is complete, the subscapularis is tagged for later repair if it is viable [33]. Next, we release the humeral capsule off bone using progressive external rotation and electrocautery. A complete osteophyte resection is then performed; removing humeral osteophytes is another critical step as this decreases the humeral volume and will eventually facilitate improved glenoid exposure [33]. Once the osteophytes have been resected, the humerus is then dislocated [33]. We use multiple blunt Hohman retractors to expose the humerus at this point. The next critical step is the humeral head cut. The biggest advantage the surgeon enjoys when performing a reverse replacement in comparison to an anatomic replacement is that the head cut can be larger because the supraspinatus attachment on the humerus does not need to be preserved. Therefore, our head cut in reverse replacement is typically 5+ mm lower than a cut would be for an anatomic replacement, even removing some of the greater tuberosity. After the generous head cut, the humerus is then broached per manufacturer guidelines with the final broach remaining in place to protect the humeral bone from being crushed by glenoid retractors (Fig. 1).
Fig. 1.
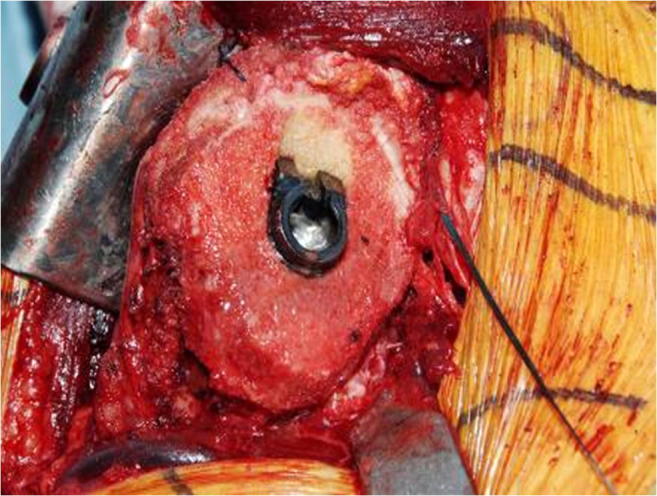
Humeral exposure after capsular release, osteophyte resection, and final broaching
Glenoid Exposure
Prior to placing glenoid retractors, we first reassess the four critical steps for glenoid exposure performed thus far: (1) deltoid release, (2) humeral capsule release, (3) generous head cut, and (4) osteophyte resection (Table 3) [33, 36]. Glenoid retractors of choice are placed provisionally to allow for complete resection of glenoid labrum tissue with electrocautery. Once the labrum has been resected, the anterior capsule and subscapularis are released with a periosteal elevator and electrocautery and a two-prong glenoid retractor is placed along the anterior glenoid neck [34] (Fig. 2). Similarly, the posterior capsule is then released and a posterior glenoid retractor is placed (we prefer another two prong glenoid retractor). Lastly, a careful inferior capsule release is then performed ensuring 1 cm of medial exposure along the bottom of the glenoid, releasing some triceps origin as well. This is important for two reasons: first, this allows low positioning of the glenoid baseplate, and second, this allows clearance for the humeral metaphyseal component in adduction, potentially reducing notching. At this point, the surgeon should have an unobstructed view of the glenoid, but retroverted Walch B2 and B3 glenoids will still sometimes be more difficult to instrument [33].
Table 3.
Critical Steps for Adequate Surgical Exposure in Reverse Shoulder Arthroplasty
| Surgical Step | Comment |
|---|---|
| Neuromuscular Paralysis | We use general endotracheal anesthesia and ask anesthesia to test paralysis upon commencing glenoid exposure |
| Incision Size | Slightly above coracoid to top of axillary crease; large males will require larger incision |
| Subdeltoid release | Releasing deltoid adhesions is critical for obtaining adequate posterior humeral translation |
| Subscapularis peel | Optimal subscapularis management for reverse: tenotomy or lesser tuberosity osteotomy does not line up after reverse is placed due to distalization and lateralization |
| Humeral capsule release | Release off bone with progressive external rotation |
| Osteophyte resection | Reduces humeral volume |
| Large head cut | Can take a larger head cut in reverse because supraspinatus insertion does not have to be spared |
| Complete labrectomy with 270-degree capsule release of glenoid | Include releasing some triceps origin off bone inferiorly to allow for adduction |
| Glenoid retractors |
1)Posterior Fukuda or two-prong 2)Posterosuperior Hohman 3)Anterior two prong 4)Anteroinferior two-prong is added in muscular males |
| Arm position and table tilt | Extension, abduction, some external rotation, but varies case by case. Table tilt away from surgeon can optimize view |
Fig. 2.
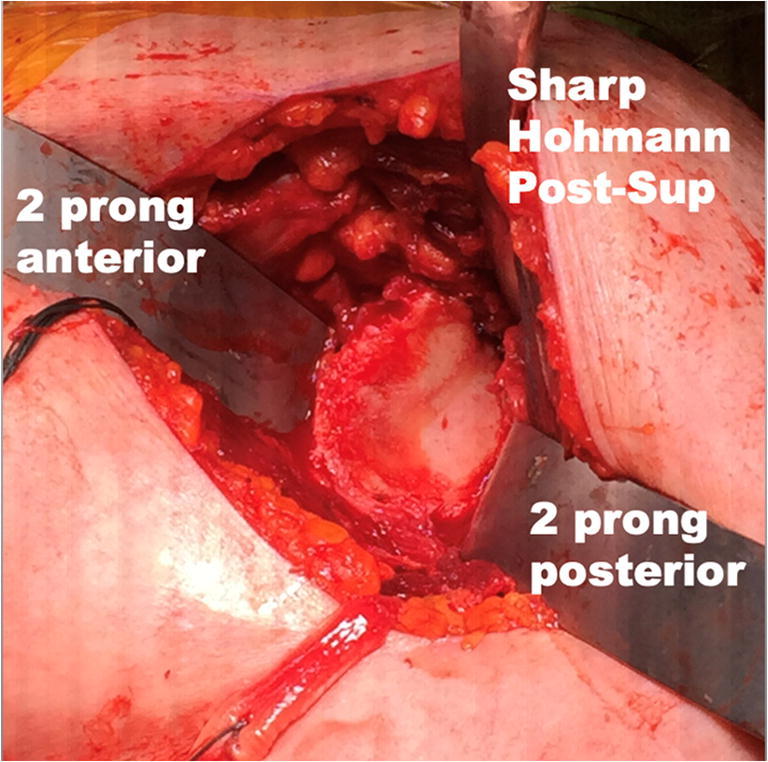
Basic glenoid retractor placement
Anterior and posterior glenoid retractors are placed as well as a posterosuperior sharp Hohmann retractor behind the coracoid process. Capsular release on humerus and glenoid, deltoid release, adequate head cut, and osteophyte resection are more important than the specific type of glenoid retractor used
We typically place the definitive baseplate and the definitive glenosphere at the time of the initial glenoid exposure based on the preoperative templating rather than using trial glenoid implants. We prefer to trial on the humeral side and set optimal tension of the shoulder with added polyethylene thickness. Prior to placing the definitive humeral stem however, it is important to make sure the shoulder will reduce before placing definitive humeral implant because the optimal way to decrease tension in a shoulder that will not reduce is to recut the humerus rather than release more soft tissue from the humerus. Implant tensioning proceeds as follows; the shoulder should be semi-difficult to reduce but not impossible and difficult but not impossible to dislocate. Overstuffing can lead to traction neuropraxia and/or acromial stress fracture [32, 37]. Intraoperative stability should be tested prior to closure.
Conclusion
Reverse shoulder replacement should be considered in arthroplasty situations with rotator cuff disease, deformity, bone loss, and instability as part of the diagnosis. Optimal exposure in reverse shoulder arthroplasty can be obtained by (1) releasing deltoid adhesions, (2) removal of humeral osteophytes, (3) generous humeral head cuts, (4) thorough humeral and glenoid capsular release and (5) optimal glenoid retractor placement. Neuromuscular paralysis can also aid glenoid exposure.
Compliance with Ethical Standards
Conflict of Interest
Harshvardhan Chawla and Seth Gamradt declare that they have no conflict of interest. Seth Gamradt receives consultancy fees from Zimmer Biomet Holdings, Inc. and Arthrex, Inc. outside of the submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Reverse Shoulder Arthroplasty
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Harshvardhan Chawla, Email: harshvardhan.chawla@med.usc.edu.
Seth Gamradt, Email: seth.gamradt@med.usc.edu.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Grammont P, Troiulloud P, Laffay J, Deries X. Study and development of a new shoulder prosthesis. Rheumatologie. 1987;39:407–418. [Google Scholar]
- 2.Flatow EL, Harrison AK. A history of Reverse Total shoulder arthroplasty. Clin Orthop Relat Res. 2011;469(9):2432–9. [DOI] [PMC free article] [PubMed]
- 3.Schairer WW, Nwachukwu BU, Lyman S, Craig EV, Gulotta LV. National utilization of reverse total shoulder arthroplasty in the United States. J Shoulder Elb Surg. 2015;24(1):91–97. doi: 10.1016/j.jse.2014.08.026. [DOI] [PubMed] [Google Scholar]
- 4.Lung TS, Cruickshank D, Grant HJ, Rainbow MJ, Bryant TJ, Bicknell RT. Factors contributing to glenoid baseplate micromotion in reverse shoulder arthroplasty : a biomechanical study. J Shoulder Elb Surg. 2019;28(4):648–653. doi: 10.1016/j.jse.2018.09.012. [DOI] [PubMed] [Google Scholar]
- 5.Wiater JM, Jr JEM, Budge MD, Koueiter DM, Marcantonio D, Wiater BP. Clinical and radiographic results of cementless reverse total shoulder arthroplasty : a comparative study with 2 to 5 years of follow-up. J Shoulder Elb Surg. 2014;23(8):1208–14. [DOI] [PubMed]
- 6.Peers S, Moravek JE Jr, Budge MD, Newton MD, Kurdziel MD, Baker KC, Wiater JM. Wear rates of highly cross-linked polyethylene humeral liners subjected to alternating cycles of glenohumeral flexion and abduction. J Shoulder Elb Surg. 2015;24(1):143–149. doi: 10.1016/j.jse.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 7.Carpenter SR, Urits I, Murthi AM. Porous metals and alternate bearing surfaces in shoulder arthroplasty. Curr Rev Musculoskelet Med. 2016;9:59–66. doi: 10.1007/s12178-016-9319-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Werner BS, Chaoui J, Walch G. The influence of humeral neck shaft angle and glenoid lateralization on range of motion in reverse shoulder arthroplasty. J Shoulder Elb Surg. 2017;26(10):1726–1731. doi: 10.1016/j.jse.2017.03.032. [DOI] [PubMed] [Google Scholar]
- 9.Werner BC, Dines JS, Dines DM, Werner BC. Platform systems in shoulder arthroplasty. Curr Rev Musculoskelet Med. 2016;9:49–53. doi: 10.1007/s12178-016-9317-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grosel TW, Darren BS, Joel RP, Scharschmidt TJ, Barlow JD Oncologic reconstruction of the proximal humerus with a reverse total shoulder arthroplasty megaprosthesis. J Surg Oncol 2018;118(6):867–872. 10.1002/jso.25061. [DOI] [PubMed]
- 11.Gagliano JR, Helms SM, Colbath GP, Przestrzelski BT, Hawkins RJ, Desjardins JD. BASIC SCIENCE A comparison of onlay versus inlay glenoid component loosening in total shoulder arthroplasty. J Shoulder Elb Surg. 2017;26(7):1113–1120. doi: 10.1016/j.jse.2017.01.018. [DOI] [PubMed] [Google Scholar]
- 12.Collin P, Liu X, Denard PJ, Gain S, Nowak A, Lädermann A. Standard versus bony increased-offset reverse shoulder arthroplasty : a retrospective comparative cohort study. J Shoulder Elb Surg. 2018;27(1):59–64. doi: 10.1016/j.jse.2017.07.020. [DOI] [PubMed] [Google Scholar]
- 13.Werthel J et al. Lateralization in reverse shoulder arthroplasty : a descriptive analysis of different implants in current practice. Int Orthop 2019;43(10):2349–2360. 10.1007/s00264-019-04365-3. [DOI] [PubMed]
- 14.Ivaldo N, Mangano T, Caione G, Rossoni M, Ligas A. Customized tantalum-augmented reverse shoulder arthroplasty for glenoid bone defect and excessive medialization : description of the technique. Musculoskelet Surg. 2016;100(s1):13–18. doi: 10.1007/s12306-016-0404-5. [DOI] [PubMed] [Google Scholar]
- 15.Nashikkar PS, Scholes CJ, Haber MD. Role of intraoperative navigation in the fixation of the glenoid component in reverse total shoulder arthroplasty : a clinical case-control study. J Shoulder Elb Surg. 2019;28(9):1685–91. 10.1016/j.jse.2019.03.013. [DOI] [PubMed]
- 16.Venne G, Rasquinha BJ, Pichora D, Ellis RE, Bicknell R. Comparing conventional and computer-assisted surgery baseplate and screw placement in reverse shoulder arthroplasty. J Shoulder Elb Surg. 2015;24(7):1112–1119. doi: 10.1016/j.jse.2014.10.012. [DOI] [PubMed] [Google Scholar]
- 17.Verborgt O, De Smedt T, Vanhees M, Clockaerts S, Parizel PM, Van Glabbeek F. Accuracy of placement of the glenoid component in reversed shoulder arthroplasty with and without navigation. J Shoulder Elb Surg. 2011;20(1):21–26. doi: 10.1016/j.jse.2010.07.014. [DOI] [PubMed] [Google Scholar]
- 18.Levy JC, Everding NG, Frankle MA, Keppler LJ. Accuracy of patient-specific guided glenoid baseplate positioning for reverse shoulder arthroplasty. J Shoulder Elb Surg. 2014;23(10):1563–1567. doi: 10.1016/j.jse.2014.01.051. [DOI] [PubMed] [Google Scholar]
- 19.Walch G, Badet R, Boulahia A. Morphologic Study of the Glenoid in Primary Glenohumeral Osteoarthritis. J Arthroplast. 1999;14(6):756–760. doi: 10.1016/S0883-5403(99)90232-2. [DOI] [PubMed] [Google Scholar]
- 20.Nové-josserand L, Clavert P. Glenoid exposure in total shoulder arthroplasty. Orthop Traumatol Surg Res. 2018;104(1):S129–S135. doi: 10.1016/j.otsr.2017.10.008. [DOI] [PubMed] [Google Scholar]
- 21.Berhouet J, et al. Preoperative planning for accurate glenoid component positioning in reverse shoulder arthroplasty. Orthop Traumatol Surg Res. 2017;103(3):407–413. doi: 10.1016/j.otsr.2016.12.019. [DOI] [PubMed] [Google Scholar]
- 22.Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78–83. [PubMed]
- 23.Neer Cuff-Tear. 1983; J Bone Joint Surg Am. 1983;65(9):1232–1244. [PubMed]
- 24.Mulieri P, Dunning P, Klein S, Pupello D, Reverse FM. Shoulder arthroplasty for the treatment of irreparable rotator cuff tear without Glenohumeral arthritis. J Bone Joint Surg Am. 2010;92(15):2544–56. 10.2106/JBJS.I.00912. [DOI] [PubMed]
- 25.Kontakis G, Tosounidis T, Galanakis I. Prosthetic replacement for proximal humeral fractures. Preoperative planning for accurate glenoid component positioning in reverse shoulder arthroplasty. Orthop Traumatol Surg Res. 2017;103(3):407–13. 10.1016/j.otsr.2016.12.019. [DOI] [PubMed]
- 26.Boileau P, Chuinard C, Bicknell R, Frcs C, Walch G. Reverse total shoulder arthroplasty after failed rotator cuff surgery. J Shoulder Elb Surg. 2009;18:600–606. doi: 10.1016/j.jse.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 27.Hansen ML, Routman H. The biomechanics of current reverse shoulder replacement options. Annals of Joint. 2019;4:1–7.
- 28.Berliner JL, Regalado-magdos A, Ma CB, Feeley BT. Biomechanics of reverse total shoulder arthroplasty. J Shoulder Elb Surg. 2015;24(1):150–160. doi: 10.1016/j.jse.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 29.Ferle M, Pastor M, Hagenah J, Hurschler C, Smith T. Effect of the humeral neck-shaft angle and glenosphere lateralization on stability of reverse shoulder arthroplasty : a cadaveric study. J Shoulder Elb Surg. 2019;28(5):966–973. doi: 10.1016/j.jse.2018.10.025. [DOI] [PubMed] [Google Scholar]
- 30.Berhouet J, Garaud P, Favard L. Evaluation of the role of glenosphere design and humeral component retroversion in avoiding scapular notching during reverse shoulder arthroplasty. J Shoulder Elb Surg. 2014;23(2):151–158. doi: 10.1016/j.jse.2013.05.009. [DOI] [PubMed] [Google Scholar]
- 31.Werthel J, et al. Acromial fractures in Reverse shoulder arthroplasty : A clinical and radiographic analysis. Journal of Shoulder and Elbow Arthroplasty. 2018;2:1–9.
- 32.Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. Neer Award 2005 : The Grammont reverse shoulder prosthesis : Results in cuff tear arthritis , fracture sequelae , and revision arthroplasty. J Shoulder Elb Surg. 2006;15:527–540. doi: 10.1016/j.jse.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 33.Birmingham P, Sperling JW, Craig E, Care P. Glenoid exposure in shoulder arthroplasty. Techniques in Shoulder and Elbow Surgery. 2010;11(3):92–6.
- 34.Nové-josserand L. Instructional lecture : Shoulder & Elbow Exposing the glenoid in shoulder arthroplasty. EFORT Open Rev. 2019;4(6):248–53. 10.1302/2058-5241.4.180057. [DOI] [PMC free article] [PubMed]
- 35.Gadea F, Bouju Y, Berhouet J. Deltopectoral approach for shoulder arthroplasty : anatomic basis. Int Orthop. 2015;39(2):215–25. 10.1007/s00264-014-2654-x. [DOI] [PubMed]
- 36.Williams GR., Jr Top ten tips for glenoid exposure in shoulder arthroplasty. Semin Arthroplast. 2017;28(3):124–127. doi: 10.1053/j.sart.2017.12.009. [DOI] [Google Scholar]
- 37.Nagda SH et al. Peripheral nerve function during shoulder arthroplasty using intraoperative nerve monitoring. J Shoulder Elb Surg. 2007;16(3Suppl):S2–S8. [DOI] [PubMed]


