Abstract
Background
Little is known about the frequency, patterns, and determinants of readmissions among patients initially hospitalized for an ambulatory care-sensitive condition (ACSC). The degree to which hospitalizations in close temporal proximity cluster has also not been studied. Readmission patterns involving clustering likely reflect different underlying determinants than the same number of readmissions more evenly spaced.
Objective
To characterize readmission rates, patterns, and predictors among patients initially hospitalized with an ACSC.
Design
Retrospective analysis of the 2010–2014 Nationwide Readmissions Database.
Participants
Non-pregnant patients aged 18–64 years old during initial ACSC hospitalization and who were discharged alive (N = 5,007,820).
Main Measures
Frequency and pattern of 30-day all-cause readmissions, grouped as 0, 1, 2+ non-clustered, and 2+ clustered readmissions.
Key Results
Approximately 14% of patients had 1 readmission, 2.4% had 2+ non-clustered readmissions, and 3.3% patients had 2+ clustered readmissions during the 270-day follow-up. A higher Elixhauser Comorbidity Index was associated with increased risk for all readmission groups, namely with adjusted odds ratios (AORs) ranging from 1.12 to 3.34. Compared to patients aged 80 years and older, those in younger age groups had increased risk of 2+ non-clustered and 2+ clustered readmissions (AOR range 1.27–2.49). Patients with chronic versus acute ACSCs had an increased odds ratio of all readmission groups compared to those with 0 readmissions (AOR range 1.37–2.69).
Conclusions
Among patients with 2+ 30-day readmissions, factors were differentially distributed between clustered and non-clustered readmissions. Identifying factors that could predict future readmission patterns can inform primary care in the prevention of readmissions following ACSC-related hospitalizations.
KEY WORDS: readmissions, ambulatory care-sensitive conditions, hospitalization
INTRODUCTION
Although a growing body of literature has identified potentially modifiable factors associated with short-term hospital readmission, several key areas remain understudied. First, little is known about the frequency, patterns, and determinants of readmission among adult patients who are initially hospitalized for an ambulatory care-sensitive condition (ACSC). ACSCs are a set of conditions for which timely and effective outpatient care, often facilitated by primary care physicians, can plausibly reduce the likelihood of rehospitalization by managing chronic conditions and preventing acute illness 1, 2. Therefore, research that targets ACSCs is warranted due to the potential for prevention and timely intervention.
Second, the readmission literature has focused predominately on either the high-frequency readmitting population (i.e., three or more readmissions in a calendar year) 3 or the sheer volume of readmissions 4. Few studies have characterized readmission patterns, combining information not only on the readmission frequency 5, 6 but also on the degree to which hospitalizations in close temporal proximity cluster. These patterns are clinically relevant since; given the same number of readmissions over a period of time, readmission clustering (e.g., six hospitalizations within 2 months) likely reflects different underlying social, biological, and environmental determinants than the same number of readmissions more evenly spaced over time. For example, patients who have social issues at home such as not having reliable transportation to primary care visits or do not have electricity may have comparatively higher likelihood of exacerbation of existing conditions and/or failure to resolve the underlying morbidity, thereby resulting in recurring (back-to-back, clustered) readmission patterns. As stated by Saeed Aminzadeh, CEO of Boston-based Decision Point Healthcare Solutions, the keys to reducing readmissions are to “identify and engage the patients as early as possible,” as well as identifying patients with “high risk of multiple, clustered admissions because they have undesirable disease trajectories and histories of engagement challenges (e.g., poor preventative behavior, sporadic visits to the doctor, excessive use of the ER, etc.).” 7 As such, studies that better characterize readmission patterns and identify factors associated with the frequency and intensity of inpatient hospitalization are likely to lead to more effective prevention and intervention strategies.
To address the lack of nationally representative studies that explore readmission behaviors among patients initially hospitalized with ACSCs, we used the largest all-payer inpatient readmissions database in the USA to characterize 30-day readmission subgroups (e.g., those who do not experience readmission, those with 1 readmission, those with two or more non-clustered readmissions, and those with two or more clustered readmissions).
METHODS
Study Overview
This study constitutes a 5-year retrospective analysis of inpatient hospitalizations from 2010 to 2014 using the Nationwide Readmissions Database (NRD), a database from the Healthcare Cost and Utilization Project (HCUP) that is sponsored by the Agency for Healthcare Research and Quality. The NRD includes data from approximately 15 million discharges each year (35 million when weighted), and it provides nationally representative information on readmissions 8. In 2014, this database included 22 geographically dispersed states with verifiable patient linkage numbers; these states accounted for approximately 50% of the total US population 8.
Study Sample and Measures
Using an approach described by the Centers for Medicare and Medicaid Services, index events were defined as hospitalizations taking place between January 1 and March 31 of each calendar year and for which the principal diagnosis was an ACSC 9. Restriction to the 3-month period (January–March) at the beginning of each calendar year for capturing index hospitalizations was implemented to allow for a 270-day follow-up window for each patient. This approach was required because the NRD, published annually, allows for linkage of hospitalizations for a patient within a calendar year; however, since identifiers do not span multiple years, the NRD does not allow linkage of patient information across calendar years. We included all patients aged 18 years and older and who were discharged alive. Last, we excluded patients who expired prior to discharge from the index hospitalization since they were not at risk of the primary study outcome, inpatient readmission. The weighted sample size included in the analysis was N = 5,007,820.
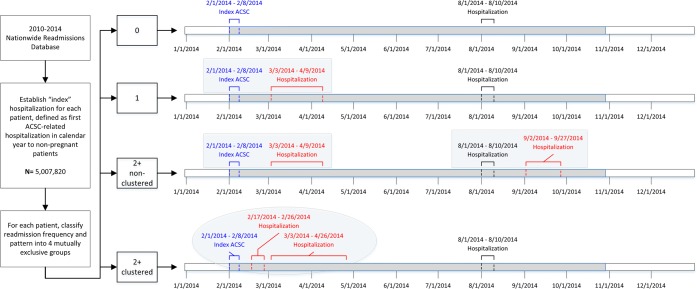
The primary outcome of interest was 30-day all-cause readmission. Readmissions included hospitalizations taking place within 30 days of discharge from the index hospitalization, and that may have been to the same or a different hospital, but within the same state as the index hospitalization. Readmissions to facilities in different states would not be captured in the NRD because it does not incorporate interstate linkages. Consistent with the HCUP methodology for reporting of national readmission rates 8, readmissions themselves can qualify to be index events if they meet index criteria. For each patient, we tracked all readmissions in which the date of hospitalization was within 270 days of the patient’s first ACSC-related hospitalization in the calendar year. Finally, we categorized the frequency and pattern of readmissions into the following mutually exclusive groups: 0 readmissions, 1 readmission, 2+ non-clustered readmissions, and 2+ clustered readmissions. Those in the 0 and 1 readmission categories have zero readmissions and exactly one 30-day readmission, respectively, during the 270-day follow-up period. Both the 2+ groups had more than one 30-day readmission during follow-up; the “clustered” group was differentiated from the “non-clustered” group by having at least one instance in which there were 2 or more readmissions within 30 days of an index hospitalization (Fig. 1).
Fig. 1.
Sample selection flow diagram and readmission outcome definitions.
Covariates
All covariates were taken from the index hospitalization. Social determinants included in the analysis were sex (female or male), zip code–based median household income (lowest quartile, 2nd quartile, 3rd quartile, highest quartile), primary insurance (Medicare, Medicaid, private insurance, self-pay, no charge, other), patient location (large central metropolitan, large fringe metropolitan, medium metropolitan area 250,000–999,999, small metropolitan area 50,000–249,999, micropolitan, not metropolitan or micropolitan), and patient residency in the state of hospitalization (resident or non-resident).
Health status indicators documented during the index hospitalization and included in the analysis were ACSC type (acute or chronic) as defined by the Centers for Medicare and Medicaid Services 9, age in years (18–44, 45–64, 65–79, 80+), Elixhauser Comorbidity Index (ECI) (0, 1, 2, 3–4, 5–6, 7+), and severity of illness (mild, moderate, severe, extreme). Severity of illness is defined as “the extent of physiologic decompensation or organ system loss of function” and is assigned to each hospitalization [10. The severity of illness code is operationalized through a proprietary algorithm, developed by 3M™, using length of stay, principal and secondary diagnoses and procedure codes, and patient age. [10]
Other clinical covariates included in the analysis were discharge disposition (home or self-care; transfer to short-term hospital, skilled nursing, intermediate care, other facility/home healthcare; against medical advice), emergency department (ED) services (ED-related or not ED-related), hospital bed size (small, medium, large), and hospital type (non-metropolitan hospital, metropolitan non-teaching hospital, metropolitan teaching hospital). Since the Hospital Readmissions Reduction Program (HRRP) was implemented in the middle of the study period, we also included a variable that assessed whether the index hospitalization occurred during the pre-HRRP period (January 1, 2010–September 30, 2012) versus the post-HRRP period (October 1, 2012–December 31, 2014).
Statistical Analyses
We estimated the frequencies and percentages of all of the index hospitalizations, readmission subtypes, overall and by social determinant factors, health status indicators, and other clinical factors. All of the hospitalizations were weighted to account for the complex sampling design of the NRD, which allowed for the generation of national estimates.
For each of the 13 covariates selected, bivariate analyses were conducted in order to assess the relationships with the outcome variable and the number/pattern of readmissions. Selection of these covariates was based on a review of the literature, available data, and empirical analyses. Covariates were entered into a survey-weighted multivariable logistic regression to generate adjusted odds ratios (AORs) and 95% confidence intervals (CIs) representing the associations between each covariate and readmission group. The “0 readmissions” group was used as the reference outcome level. Although our outcome was ordinal in nature, we did not use ordinal logistic regression due to the violation of the proportional odds assumption.
The analysis for this paper was generated using SAS® software, version 9.4. Due to the de-identified nature of the NRD, the Baylor College of Medicine Institutional Review Board classified this study as exempt.
RESULTS
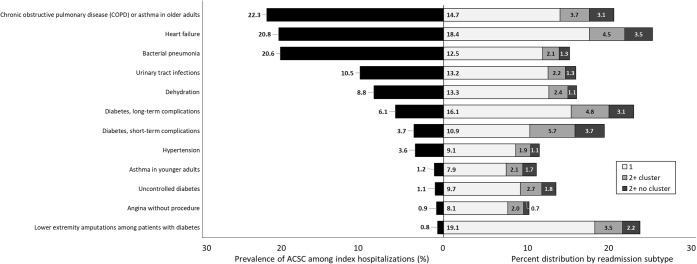
Of the 5,007,820 patients included in this study, 14.3% had 1 readmission, 2.4% had 2+ non-clustered readmissions, and 3.3% patients had 2+ clustered readmissions during the 270-day follow-up window. The study population was mostly female (of older age; 65–79), resided in a low-income zip code, publicly insured (Medicare and Medicaid), had a hospitalization during the pre-HRRP era, and lived in large fringe metropolitan areas (Tables 1 and 2). Subgroups with the highest proportions of patients with multiple 30-day readmissions were those discharged to home or self-care, on government insurance (Medicare/Medicaid), and with increasing numbers of comorbidities and those that had chronic ACSCs. Prevalence of ACSCs during index hospitalizations is presented in Fig. 2.
Table 1.
Frequency of ACSC Index Hospitalizations for Readmission Subgroups, by Social Determinant Factors, Health Status Indicators, and Other Clinical Factors (Nationwide Readmissions Database, 2010–2014)
| Overall | Number of readmissions with the 270-day follow-up | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2+ Non-clustered | 2+ Clustered | ||||||
| N | N | C% | N | C% | N | C% | N | C% | |
| Overall | 5,007,820 | 4,008,943 | 100.0 | 715,630 | 100.0 | 117,842 | 100.0 | 165,405 | 100.0 |
| HRRP era | |||||||||
| Pre-HRRP | 3,082,986 | 2,462,200 | 61.4 | 442,503 | 61.8 | 74,475 | 63.2 | 103,809 | 62.8 |
| Post-HRRP | 1,924,834 | 1,546,743 | 38.6 | 273,127 | 38.2 | 43,368 | 36.8 | 61,596 | 37.2 |
| Sex | |||||||||
| Male | 2,167,636 | 1,718,776 | 42.9 | 318,643 | 44.5 | 52,472 | 44.5 | 77,744 | 47.0 |
| Female | 2,840,184 | 2,290,166 | 57.1 | 396,987 | 55.5 | 65,370 | 55.5 | 87,661 | 53.0 |
| Age at admission (years) | |||||||||
| 18–44 | 548,483 | 459,026 | 11.5 | 52,881 | 7.4 | 13,829 | 11.7 | 22,748 | 13.8 |
| 45–64 | 1,455,327 | 1,174,146 | 29.3 | 189,765 | 26.5 | 37,936 | 32.2 | 53,479 | 32.3 |
| 65–79 | 1,537,317 | 1,213,566 | 30.3 | 234,963 | 32.8 | 37,882 | 32.1 | 50,905 | 30.8 |
| 80+ | 1,466,694 | 1,162,204 | 29.0 | 238,021 | 33.3 | 28,195 | 23.9 | 38,274 | 23.1 |
| Zip code–level household income | |||||||||
| Lowest quartile | 1,749,332 | 1,389,665 | 34.7 | 250,486 | 35.0 | 46,132 | 39.1 | 63,049 | 38.1 |
| 2nd quartile | 1,280,947 | 1,030,797 | 25.7 | 180,391 | 25.2 | 29,240 | 24.8 | 40,518 | 24.5 |
| 3rd quartile | 1,063,585 | 853,354 | 21.3 | 153,036 | 21.4 | 23,189 | 19.7 | 34,005 | 20.6 |
| Highest quartile | 834,271 | 670,484 | 16.7 | 121,165 | 16.9 | 17,461 | 14.8 | 25,160 | 15.2 |
| Primary insurance | |||||||||
| Medicare | 3,290,829 | 2,575,931 | 64.3 | 523,366 | 73.1 | 80,956 | 68.7 | 110,577 | 66.9 |
| Medicaid | 536,768 | 409,968 | 10.2 | 77,526 | 10.8 | 19,243 | 16.3 | 30,031 | 18.2 |
| Private insurance | 774,180 | 673,511 | 16.8 | 75,524 | 10.6 | 10,620 | 9.0 | 14,523 | 8.8 |
| Self-pay, no charge, other | 406,043 | 349,533 | 8.7 | 39,214 | 5.5 | 7022 | 6.0 | 10,274 | 6.2 |
| Discharge disposition | |||||||||
| Discharged to home or self-care | 3,132,653 | 2,597,327 | 64.8 | 374,338 | 52.3 | 67,728 | 57.5 | 93,259 | 56.4 |
| Transfer/home health | 1,810,700 | 1,366,685 | 34.1 | 329,585 | 46.1 | 47,596 | 40.4 | 66,835 | 40.4 |
| Against medical advice | 64,467 | 44,930 | 1.1 | 11,707 | 1.6 | 2518 | 2.1 | 5312 | 3.2 |
| Emergency department services | |||||||||
| ED-related | 4,158,489 | 3,303,577 | 82.4 | 606,678 | 84.8 | 102,562 | 87.0 | 145,672 | 88.1 |
| Not ED-related | 849,331 | 705,366 | 17.6 | 108,952 | 15.2 | 15,280 | 13.0 | 19,733 | 11.9 |
| Patient location | |||||||||
| Large central metro | 1,230,108 | 963,809 | 24.0 | 184,188 | 25.7 | 33,241 | 28.2 | 48,870 | 29.5 |
| Large fringe metro | 1,237,639 | 981,512 | 24.5 | 183,325 | 25.6 | 29,598 | 25.1 | 43,205 | 26.1 |
| Medium metro | 960,422 | 771,528 | 19.2 | 136,792 | 19.1 | 21,812 | 18.5 | 30,291 | 18.3 |
| Small metro | 458,977 | 369,541 | 9.2 | 64,640 | 9.0 | 10,424 | 8.8 | 14,371 | 8.7 |
| Micropolitan | 603,536 | 493,168 | 12.3 | 80,845 | 11.3 | 13,080 | 11.1 | 16,442 | 9.9 |
| Non-core | 505,892 | 420,671 | 10.5 | 64,358 | 9.0 | 9358 | 7.9 | 11,505 | 7.0 |
| Patient residency | |||||||||
| Resident | 4,822,802 | 3,849,210 | 96.0 | 696,290 | 97.3 | 115,476 | 98.0 | 161,826 | 97.8 |
| Not a resident | 185,018 | 159,732 | 4.0 | 19,340 | 2.7 | 2366 | 2.0 | 3580 | 2.2 |
| Severity of illness | |||||||||
| Minor loss of function | 659,504 | 582,139 | 14.5 | 56,224 | 7.9 | 9158 | 7.8 | 11,983 | 7.2 |
| Moderate loss of function | 2,184,605 | 1,794,762 | 44.8 | 278,658 | 38.9 | 46,716 | 39.6 | 64,469 | 39.0 |
| Major loss of function | 1,899,524 | 1,443,967 | 36.0 | 325,597 | 45.5 | 53,590 | 45.5 | 76,371 | 46.2 |
| Extreme loss of function | 263,909 | 187,818 | 4.7 | 55,142 | 7.7 | 8372 | 7.1 | 12,578 | 7.6 |
| Hospital bed size | |||||||||
| Small | 840,751 | 689,978 | 17.2 | 111,783 | 15.6 | 16,393 | 13.9 | 22,598 | 13.7 |
| Medium | 1,280,120 | 1,026,624 | 25.6 | 181,012 | 25.3 | 30,159 | 25.6 | 42,325 | 25.6 |
| Large | 2,886,950 | 2,292,341 | 57.2 | 422,835 | 59.1 | 71,291 | 60.5 | 100,483 | 60.7 |
| Hospital type | |||||||||
| Metropolitan non-teaching | 2,031,057 | 1,622,020 | 40.5 | 292,716 | 40.9 | 47,817 | 40.6 | 68,504 | 41.4 |
| Metropolitan teaching | 2,050,062 | 1,621,580 | 40.4 | 303,094 | 42.4 | 51,339 | 43.6 | 74,049 | 44.8 |
| Non-metropolitan hospital | 926,701 | 765,342 | 19.1 | 119,820 | 16.7 | 18,686 | 15.9 | 22,853 | 13.8 |
| Prevention quality indicator subtype | |||||||||
| ACSC acute | 1,999,771 | 1,674,109 | 41.8 | 256,777 | 35.9 | 25,359 | 21.5 | 43,526 | 26.3 |
| ACSC chronic | 3,008,136 | 2,334,891 | 58.2 | 458,872 | 64.1 | 92,485 | 78.5 | 121,887 | 73.7 |
| ECI number | |||||||||
| 0 | 670,620 | 550,067 | 13.7 | 81,946 | 11.5 | 16,767 | 14.2 | 21,840 | 13.2 |
| 1 | 938,362 | 802,450 | 20.0 | 98,653 | 13.8 | 16,020 | 13.6 | 21,239 | 12.8 |
| 2 | 1,481,419 | 1,201,172 | 30.0 | 200,762 | 28.1 | 33,702 | 28.6 | 45,783 | 27.7 |
| 3–4 | 1,435,800 | 1,103,060 | 27.5 | 239,725 | 33.5 | 38,093 | 32.3 | 54,921 | 33.2 |
| 5–6 | 481,618 | 352,193 | 8.8 | 94,545 | 13.2 | 13,259 | 11.3 | 21,621 | 13.1 |
| 7+ | 670,620 | 550,067 | 13.7 | 81,946 | 11.5 | 16,767 | 14.2 | 21,840 | 13.2 |
The table includes national estimates of frequencies. Numbers may not sum to the expected total, and percentage may not add to 100% due to missing data
Table 2.
Frequency (by Row Percent) of ACSC Index Hospitalizations for Readmission Subgroups, by Social Determinant Factors, Health Status Indicators, and Other Clinical Factors (Nationwide Readmissions Database, 2010–2014)
| Number of readmissions with the 270-day follow-up | ||||
|---|---|---|---|---|
| 0 | 1 | 2+ Non-clustered | 2+ Clustered | |
| R% | R% | R% | R% | |
| Overall | 80.1 | 14.3 | 2.4 | 3.3 |
| HRRP era | ||||
| Pre-HRRP | 79.9 | 14.4 | 2.4 | 3.4 |
| Post-HRRP | 80.4 | 14.2 | 2.3 | 3.2 |
| Sex | ||||
| Male | 79.3 | 14.7 | 2.4 | 3.6 |
| Female | 80.6 | 14.0 | 2.3 | 3.1 |
| Age at admission =(years) | ||||
| 18–44 | 83.7 | 9.6 | 2.5 | 4.1 |
| 45–64 | 80.7 | 13.0 | 2.6 | 3.7 |
| 65–79 | 78.9 | 15.3 | 2.5 | 3.3 |
| 80+ | 79.2 | 16.2 | 1.9 | 2.6 |
| Zip code–level household income | ||||
| Lowest quartile | 79.4 | 14.3 | 2.6 | 3.6 |
| 2nd quartile | 80.5 | 14.1 | 2.3 | 3.2 |
| 3rd quartile | 80.2 | 14.4 | 2.2 | 3.2 |
| Highest quartile | 80.4 | 14.5 | 2.1 | 3.0 |
| Primary insurance | ||||
| Medicare | 78.3 | 15.9 | 2.5 | 3.4 |
| Medicaid | 76.4 | 14.4 | 3.6 | 5.6 |
| Private insurance | 87.0 | 9.8 | 1.4 | 1.9 |
| Self-pay, no charge, other | 86.1 | 9.7 | 1.7 | 2.5 |
| Discharge disposition | ||||
| Discharged to home or self-care | 82.9 | 11.9 | 2.2 | 3.0 |
| Transfer/home health | 75.5 | 18.2 | 2.6 | 3.7 |
| Against medical advice | 69.7 | 18.2 | 3.9 | 8.2 |
| Emergency department services | ||||
| ED-related | 79.4 | 14.6 | 2.5 | 3.5 |
| Not ED-related | 83.0 | 12.8 | 1.8 | 2.3 |
| Patient location | ||||
| Large central metro | 78.4 | 15.0 | 2.7 | 4.0 |
| Large fringe metro | 79.3 | 14.8 | 2.4 | 3.5 |
| Medium metro | 80.3 | 14.2 | 2.3 | 3.2 |
| Small metro | 80.5 | 14.1 | 2.3 | 3.1 |
| Micropolitan | 81.7 | 13.4 | 2.2 | 2.7 |
| Non-core | 83.2 | 12.7 | 1.8 | 2.3 |
| Patient residency | ||||
| Resident | 79.8 | 14.4 | 2.4 | 3.4 |
| Not a resident | 86.3 | 10.5 | 1.3 | 1.9 |
| Severity of illness | ||||
| Minor loss of function | 88.3 | 8.5 | 1.4 | 1.8 |
| Moderate loss of function | 82.2 | 12.8 | 2.1 | 3.0 |
| Major loss of function | 76.0 | 17.1 | 2.8 | 4.0 |
| Extreme loss of function | 71.2 | 20.9 | 3.2 | 4.8 |
| Hospital bed size | ||||
| Small | 82.1 | 13.3 | 1.9 | 2.7 |
| Medium | 80.2 | 14.1 | 2.4 | 3.3 |
| Large | 79.4 | 14.6 | 2.5 | 3.5 |
| Hospital type | ||||
| Metropolitan non-teaching | 79.9 | 14.4 | 2.4 | 3.4 |
| Metropolitan teaching | 79.1 | 14.8 | 2.5 | 3.6 |
| Non-metropolitan hospital | 82.6 | 12.9 | 2.0 | 2.5 |
| Prevention quality indicator subtype | ||||
| ACSC acute | 83.7 | 12.8 | 1.3 | 2.2 |
| ACSC chronic | 77.6 | 15.3 | 3.1 | 4.1 |
| ECI number | ||||
| 0 | 88.5 | 8.4 | 1.4 | 1.7 |
| 1 | 85.8 | 10.4 | 1.6 | 2.1 |
| 2 | 82.9 | 12.5 | 2.0 | 2.6 |
| 3–4 | 78.7 | 15.2 | 2.5 | 3.5 |
| 5–6 | 73.4 | 18.6 | 3.3 | 4.7 |
| 7+ | 68.6 | 21.7 | 3.8 | 5.9 |
The table includes national estimates of frequencies. Numbers may not sum to the expected total, and percentage may not add to 100% due to missing data
Fig. 2.
Prevalence of ACSCs during index hospitalizations.
Our multivariable regression analyses exploring factors associated with readmission frequency and patterns are presented in Table 3. The measures of association for the social determinant factors varied. Women had decreased odds of having 1 readmission (AOR = 0.93; CI = 0.92, 0.94), 2+ non-clustered readmissions (AOR = 0.97; CI = 0.95, 0.99), and 2+ clustered readmissions (AOR = 0.87; CI = 0.86, 0.89) than men. Patients living in zip codes reporting the lowest household income quartiles, compared to reporting the highest, had increased odds of having 1 readmission (AOR = 1.09; CI = 1.07, 1.10) and 2+ non-clustered readmissions (AOR = 1.24; CI = 1.20, 1.29) and higher odds of 2+ clustered readmissions (AOR = 1.21; CI = 1.18, 1.26). Differences were observed by insurance type; patients with any insurance other than private had increased odds of having 1 readmission (Medicare: AOR = 1.43, CI = 1.40, 1.46; Medicaid: AOR = 1.53, CI = 1.50, 1.56; self-pay/no charge/other: AOR = 1.01, CI = 0.99, 1.04), 2+ non-clustered readmissions (Medicare: AOR = 2.04, CI = 1.95, 2.13; Medicaid: AOR = 2.29, CI = 2.20, 2.40; self-pay/no charge/other: AOR = 1.13, CI = 1.07, 1.19), and 2+ clustered readmissions (Medicare: AOR = 2.12, CI = 1.18, 1.26; Medicaid: AOR = 2.57, CI = 2.47, 2.67; self-pay/no charge/other: AOR = 1.18, CI = 1.13, 1.24). Patients who lived in large central metropolitan areas, compared to those living in smaller populated areas, experience decreased odds of 1 readmission and 2+ clustered readmissions, compared to 0 readmissions.
Table 3.
Adjusted Odds Ratios and 95% Confidence Intervals from Survey Logistic Regression Representing Factors Associated with Readmission Frequency and Patterns (Nationwide Readmissions Database, 2010–2014)
| Number of readmissions with the 270-day follow-up | |||
|---|---|---|---|
| 1 | 2+ Non-clustered | 2+ Clustered | |
| HRRP era | |||
| Pre-HRRP | Ref | Ref | Ref |
| Post-HRRP | 0.95 (0.93, 0.96)* | 0.87 (0.85, 0.89)* | 0.88 (0.86, 0.90)* |
| Sex | |||
| Female | 0.93 (0.92, 0.94)* | 0.97 (0.95, 0.99)* | 0.87 (0.86, 0.89)* |
| Age at admission (years) | |||
| 18–44 | 0.89 (0.87, 0.92)* | 2.03 (1.94, 2.13)* | 2.49 (2.39, 2.58)* |
| 45–64 | 1.01 (0.99, 1.02) | 1.61 (1.55, 1.67)* | 1.70 (1.65, 1.75)* |
| 65–79 | 1.00 (0.99, 1.01) | 1.27 (1.23, 1.31)* | 1.28 (1.25, 1.32)* |
| 80+ | Ref | Ref | Ref |
| Zip code–level household income | |||
| Lowest quartile | 1.09 (1.07, 1.10)* | 1.24 (1.20, 1.29)* | 1.21 (1.18, 1.26)* |
| 2nd quartile | 1.04 (1.02, 1.06)* | 1.11 (1.07, 1.15)* | 1.10 (1.06, 1.13)* |
| 3rd quartile | 1.03 (1.01, 1.04)* | 1.03 (0.99, 1.07) | 1.06 (1.02, 1.09)* |
| Highest quartile | Ref | Ref | Ref |
| Primary insurance | |||
| Medicare | 1.43 (1.40, 1.46)* | 2.04 (1.95, 2.13)* | 2.12 (2.04, 2.19)* |
| Medicaid | 1.53 (1.50, 1.56)* | 2.29 (2.20, 2.40)* | 2.57 (2.47, 2.67)* |
| Private | Ref | Ref | Ref |
| Self-pay, no charge, other | 1.01 (0.99, 1.04) | 1.13 (1.07, 1.19)* | 1.18 (1.13, 1.24)* |
| Discharge disposition | |||
| Home/self-care | Ref | Ref | Ref |
| Transfer/home health | 1.35 (1.34, 1.37)* | 1.26 (1.22, 1.29)* | 1.28 (1.26, 1.31)* |
| Against medical advice | 1.84 (1.78, 1.91)* | 1.81 (1.68, 1.94)* | 2.62 (2.49, 2.75)* |
| Emergency department services | |||
| ED-related | 1.11 (1.09, 1.12)* | 1.32 (1.28, 1.37)* | 1.38 (1.34, 1.43)* |
| Patient location | |||
| Large central metro | Ref | Ref | Ref |
| Large fringe metro | 1.03 (1.01, 1.05)* | 1.03 (0.99, 1.06) | 1.03 (0.99, 1.06) |
| Medium metro | 0.95 (0.94, 0.97)* | 0.90 (0.87, 0.94)* | 0.86 (0.83, 0.89)* |
| Small metro | 0.95 (0.93, 0.97)* | 0.90 (0.86, 0.94)* | 0.86 (0.82, 0.89)* |
| Micropolitan | 0.92 (0.89, 0.95)* | 0.83 (0.77, 0.88)* | 0.78 (0.73, 0.83)* |
| Non-core | 0.91 (0.88, 0.94)* | 0.78 (0.73, 0.84)* | 0.72 (0.68, 0.77)* |
| Patient residency | |||
| Resident | 1.45 (1.40, 1.50)* | 1.87 (1.70, 2.07)* | 1.75 (1.63, 1.88)* |
| Severity of illness | |||
| Minor loss of function | Ref | Ref | Ref |
| Moderate loss of function | 1.33 (1.31, 1.36)* | 1.47 (1.40, 1.53)* | 1.51 (1.46, 1.57)* |
| Major loss of function | 1.64 (1.61, 1.68)* | 1.79 (1.71, 1.88)* | 1.87 (1.79, 1.94)* |
| Extreme loss of function | 1.86 (1.81, 1.91)* | 1.79 (1.69, 1.90)* | 1.94 (1.85, 2.04)* |
| Hospital bed size | |||
| Small | Ref | Ref | Ref |
| Medium | 1.01 (0.99, 1.03) | 1.06 (1.01, 1.10)* | 1.06 (1.02, 1.10)* |
| Large | 1.05 (1.03, 1.07)* | 1.08 (1.04, 1.12)* | 1.09 (1.05, 1.13)* |
| Hospital type | |||
| Non-metro hospital | Ref | Ref | Ref |
| Metro non-teaching | 1.01 (0.98, 1.04) | 0.94 (0.89, 1.01) | 1.04 (0.98, 1.10) |
| Metro teaching | 1.04 (1.00, 1.07)* | 0.96 (0.90, 1.03) | 1.05 (0.99, 1.12) |
| ACSC type | |||
| Chronic | 1.37 (1.36, 1.39)* | 2.69 (2.62, 2.76)* | 2.03 (1.99, 2.07)* |
| Acute | Ref | Ref | Ref |
| ECI number | |||
| 0 | Ref | Ref | Ref |
| 1 | 1.12 (1.09, 1.15)* | 1.15 (1.07, 1.23)* | 1.21 (1.14, 1.28)* |
| 2 | 1.25 (1.21, 1.28)* | 1.37 (1.29, 1.47)* | 1.49 (1.40, 1.58)* |
| 3–4 | 1.44 (1.40, 1.48)* | 1.74 (1.63, 1.85)* | 1.98 (1.87, 2.09)* |
| 5–6 | 1.70 (1.65, 1.74)* | 2.26 (2.11, 2.42)* | 2.60 (2.45, 2.76)* |
| 7+ | 1.97 (1.91, 2.05)* | 2.76 (2.55, 2.98)* | 3.34 (3.13, 3.57)* |
The 0 readmissions group is the reference outcome level
*Significance at p < 0.05
Several health status factors were associated with increased odds of readmission. Compared to those aged 80+ years, all other younger age groups had increased odds for 2+ non-clustered readmissions (18–44 years: AOR = 2.03, CI = 1.94, 2.13; 45–64 years: AOR = 1.61, CI = 1.55, 1.67; 65–79 years: AOR = 1.27, CI = 1.23, 1.31) and 2+ clustered readmissions (18–44 years: AOR = 2.49, CI = 2.39, 2.58; 45–64 years: AOR = 1.70, CI = 1.65, 1.75; 65–79 years: AOR = 1.28, CI = 1.25, 1.32). Those with more substantial loss of function—a proxy for severity of the condition resulting in the index hospitalization—experienced increased odds for 1 readmission (moderate: AOR = 1.33, CI = 1.31, 1.36; major: AOR = 1.64, CI = 1.61, 1.68; extreme: AOR = 1.86, CI = 1.81, 1.91), 2+ non-clustered readmissions (moderate: AOR = 1.47, CI = 1.40, 1.53; major: AOR = 1.79, CI = 1.71, 1.88; extreme: AOR = 1.79, CI = 1.69, 1.90), and 2+ clustered readmissions (moderate: AOR = 1.51, CI = 1.46, 1.57; major: AOR = 1.87, CI = 1.79, 1.94; extreme: AOR = 1.94, CI = 1.85, 2.04). Patients with chronic ACSCs, compared to acute ACSCs, had higher odds of 1 readmission (AOR = 1.37; CI = 1.36, 1.39), 2+ non-clustered readmissions (AOR = 2.69; CI = 2.62, 2.76), and 2+ clustered readmissions (AOR = 2.03; CI = 1.99, 2.07). Similarly, there was a direct association between increased numbers of Elixhauser comorbidities—reflecting the patient’s co-occurring conditions not directly tied to the index hospitalization’s principal diagnosis—and both the frequency of readmissions and the likelihood of clustering of readmissions (Table 3).
Other clinical factors were also associated with readmission patterns. Patients sent to home health or transferred to another facility and left against medical advice had higher odds, compared to those sent home, for 1 readmission (transfer/home health: AOR = 1.35, CI = 1.34, 1.37; against medical advice: AOR = 1.84, CI = 1.78, 1.91), 2+ non-clustered readmissions (transfer/home health: AOR = 1.26, CI = 1.22, 1.29; against medical advice: AOR = 1.81, CI = 1.68, 1.94), and 2+ clustered readmissions (transfer/home health: AOR = 1.28, CI = 1.26, 1.31; against medical advice: AOR = 2.62, CI = 2.49, 2.75), compared to 0 readmissions. Patients whose index hospitalizations required emergency department services and those who received care at larger, metropolitan teaching hospitals were at highest odds of experiencing multiple and/or clustered readmissions.
Compared to the pre-HRRP, patients in the post-HRRP period had lower odds for all readmission types: for 1 readmission, 0.95 (0.93, 0.96); for 2+ non-clustered readmissions, 0.87 (0.85, 0.89); and for 2+ clustered readmissions, 0.88 (0.86, 0.90).
CONCLUSIONS
Through a comprehensive analysis of 5 years of a nationally representative, all-payer database, this study explored readmissions following an initial ACSC-related hospitalization to characterize the most common types of primary care–preventable readmission patterns in the USA. Adjusted regression models suggested that selected sociodemographic factors, social determinants of health, health status factors, and other clinical measures were associated with readmission patterns. As supported in the current literature, factors such as comorbidity burden, insurance type, and loss of function were associated with readmission phenotype 11, 12.
However, some results were contrary to what might be expected based on the readmission literature. We suspected that as patients aged, their decline in functional status, quality of life, and overall well-being would result in increased readmission rates 13. However, younger, as opposed to older, patients experienced increased odds in more frequent and higher-intensity readmissions. There is an increasing view that middle age is a pivotal period in the life course in terms of balancing growth and decline, linking earlier and later periods of life, and bridging younger and older generations 14. Thus, at older ages, there may be increased focus on health promotion and well-being, which can have a positive health impact, thereby decreasing the likelihood of readmission 14. Results from a recent study support this supposition, reporting that patients of younger adult ages have increased risk of all-cause readmissions 15. Younger working adult ages may have a worse primary care follow-up (e.g., millennials less likely to have primary care physicians), 16 and since more comprehensive care among family physicians (i.e., ambulatory care) has been purported to results in fewer hospitalizations 17, they disproportionately have fewer opportunities to prevent ACSC-related readmissions.
Of particular interest, women had lower odds of being classified non-zero readmissions groups, compared to men. Previous literature has not been clear on the role of sex. Some analyses have shown that men are at higher risk of all-cause readmissions among adult patients (e.g., Medicaid men have an increased risk of all-cause hospital readmissions) 18. However, a study conducted in an Italian department of medicine reported women to have higher risk of readmissions 19. In terms of primary care prevention, this disparity between men and women may be because men visit the primary care doctor less than women do. Reasons for men not visiting the primary care doctor have included being too busy and not wanting to veer from traditional perceptions of independence and masculinity 2022. Appreciation and consideration of sex differences in primary care-seeking behavior can help inform prevention efforts to focus on getting men into their primary care physician’s clinic more regularly.
Another significant finding of this study, as it pertains to primary care prevention of readmission, is the role of discharge against medical advice (AMA), which increased the odds of all non-zero readmissions patterns by a factor of 1.8 to 2.6. Research supports this finding that those who leave AMA are more likely to be readmitted 23. Patients who leave AMA may not have had the underlying reason for hospitalization addressed prior to their departure, resulting in an increased risk of readmission. For effective transition of care and prevention of subsequent hospitalizations, guidelines recommend assurance of appropriate disposition 11, 24, 25. The Agency for Healthcare Research and Quality (AHRQ)’s Hospital Guide to Reducing Medicaid Readmissions specifically requires staff to record patients’ disposition because it is a major factor in preventing readmissions 11. Yet, for patients who leave AMA, elucidating reasons as to why patients leave early (e.g., lack of trust in the medical community and relationship with primary care) is needed to help inform subsequent primary care outreach and intervention efforts. Additionally, to better classify the types of ACSCs to target for prevention, it should be noted that chronic ACSCs have higher odds of all readmission types. Although the granularity of identifying ACSC type is needed, improved ACSC-type classifications are needed to better understand potentially preventable admissions [26].
A novel aspect of this investigation is the exploration of factors that contribute not only to the frequency of readmissions but also to their tendency to cluster (frequent back-to-back hospitalizations). Among patients with two or more 30-day readmissions during follow-up, we observed factors that were differentially distributed between those with clustered versus non-clustered readmissions. As might be expected, increased severity of the condition for which the patient was hospitalized and a higher comorbidity burden were more likely to result in readmission clustering. Understanding factors related to the clustered versus non-clustered groups can assist primary care in targeting prevention efforts appropriately. For example, when patient A presents with three non-clustered readmissions and patient B presents with three clustered readmissions, the care plans could vary greatly between the two patients. Potentially, the conditions that patient A has can be intervened by regular follow-up with a primary care physician and health extenders 27, whereas patient B may have conditions that only inpatient care can act upon and no amount of primary care follow-up can assist. These differentiating factors can not only help to identify the viable patients for primary care intervention, but it can also lead to more deliberate use of the already scarce primary care resources available.
There were many strengths in this study, including the use of the five consecutive years of the largest all-payer readmissions database (NRD) in the USA. The focus on ACSC-related readmissions over a 9-month window is of great value compared to other disease-specific readmission studies since ACSCs constitute arguably the greatest opportunity for readmission prevention through effective primary care. Additionally, this is the first study to our knowledge to innovatively classify and characterize 30-day readmissions by tendency to cluster versus sheer volume. This attention to readmission behavior adds to the precision of intervention efforts as well as stewardship of scarce primary care resources.
Our findings must, however, be considered in light of several limitations. First, this study was limited in the breadth of variables available for analysis. The NRD is a nationwide database, and the database distributer, HCUP, did not include variables (e.g., race, ethnicity, and state of residence) that may improve characterization of ACSC-related readmissions. Another limitation is the database-induced requirement to analyze readmissions in annual cross sections as opposed to having a multi-year, longitudinally-linked database. As such, determining the true index hospitalization and implementing longer-term follow-up were not possible. However, with the robust 5 years of data and the 270-day follow-up window, our study was likely to capture factors that have a tendency to increase or decrease the frequency and/or intensity of 30-day readmissions.
For future directions, we recommend the use of other data sources with more robust social determinants or capable of investigating the impact of factors relating to health behaviors between the initial ACSC-related hospitalization and readmission (e.g., number of attended primary care clinic appointments). Electronic health records (EHRs) may prove a valuable research commodity that would increase the variability in the breadth of data analyzed as well as lengthen the window through which readmission patterns are assessed. Additionally, comparisons between ambulatory care-sensitive and non-ambulatory care-sensitive–related readmissions should be analyzed in order to identify the overall burden the different readmission types have on the healthcare system. We also suggest incorporating a mixed methods approach (i.e., qualitative data). EHR data is limited to how healthcare providers record information in the health record; therefore, additional information collected from both patients and providers can fill in these gaps. With the use of these various information sources, there would be an improvement in the understanding of reasons for and the development of targeted strategies for reducing potentially preventable (ACSC) readmissions.
Funding Information
This research was supported by the H. James Free Center for Primary Care Education and Innovation and the Department of Community Health and Family Medicine of University of Florida (Denny Fe G. Agana’s PhD funding). The funding sources had no role in the writing of this manuscript or in the decision to submit the manuscript for publication. This research was also supported by the Health Resources and Services Administration, an agency of the US Department of Health and Human Services, grant number T32 HP10031 (Denny Fe G. Agana’s postdoctoral funding). The funding source/study sponsor had no role in the writing of this manuscript or in the decision to submit the manuscript for publication.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Billings J, Zeitel L, Lukomnik J, Carey TS, Blank AE, Newman L. Impact of socioeconomic status on hospital use in New York City. Health Aff (Millwood). 1993;12(1):162–173. doi: 10.1377/hlthaff.12.1.162. [DOI] [PubMed] [Google Scholar]
- 2.Freund T, Campbell SM, Geissler S, et al. Strategies for Reducing Potentially Avoidable Hospitalizations for Ambulatory Care–Sensitive Conditions. Ann Fam Med. 2013;11(4):363–370. doi: 10.1370/afm.1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hines A, Barrett M, Jiang H, Steiner C. Conditions With the Largest Number of Adult Hospital Readmissions by Payer, 2011. HCUP Statistical Brief #172. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb172-Conditions-Readmissions-Payer.pdf. Published April 2014. Accessed May 1, 2018. [PubMed]
- 4.James J. Health Policy Brief: Medicare Hospital Readmissions Reduction Program. Health Affairs. http://healthaffairs.org/healthpolicybriefs/brief_pdfs/healthpolicybrief_102.pdf. Published November 12, 2013. Accessed January 6, 2018.
- 5.Porter M, Quillen D, Agana DF, et al. Are Patients Frequently Readmitted to the Hospital Different from the Other Admitted Patients? J Am Board Fam Med. 2019;32(1):58–64. doi: 10.3122/jabfm.2019.01.180052. [DOI] [PubMed] [Google Scholar]
- 6.Agana DFG, Salemi JL, Striley CW. From primary care to the revolving door of hospital readmission: Relevance of Geoffrey Rose’s call for a population strategy. Prev Med Rep. 2019;14. doi:10.1016/j.pmedr.2019.100848 [DOI] [PMC free article] [PubMed]
- 7.Loria K. Nine Ways to Reduce Hospital Readmissions from Hospital Executives. Managed Healthcare Executive. https://www.managedhealthcareexecutive.com/article/nine-ways-reduce-hospital-readmissions-hospital-executives. Published September 6, 2018. Accessed July 16, 2019.
- 8.THE HCUP NATIONWIDE READMISSIONS DATABASE (NRD), 2014. https://www.hcup-us.ahrq.gov/db/nation/nrd/NRD_Introduction_2010-2014.jsp. Accessed April 22, 2019.
- 9.Centers for Medicare, Baltimore MS 7500 SB, Usa M. Hospital Readmission Reduction Program. https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/value-based-programs/hrrp/hospital-readmission-reduction-program.html. Published December 4, 2018. Accessed March 14, 2019.
- 10.3M All Patient Refined Diagnosis Related Groups (APR DRGs). Presented at the: October 2016. https://www.forwardhealth.wi.gov/kw/pdf/handouts/3M_APR_DRG_Presentation.pdf. Accessed November 1, 2019.
- 11.Agency for Healthcare Reasearch and Quality. Hospital Guide to Reducing Medicaid Readmissions. August 2014:82.
- 12.Betancourt J, Tan-McGrory A, Kenst B. Guide to Preventing Readmissions among Racially and Ethnically Diverse Medicare Beneficiaries. September 2015:30.
- 13.Squires D, Anderson C. U.S. Health Care from a Global Perspective: Spending, Use of Services, Prices, and Health in 13 Countries. Issue Brief (Commonwealth Fund) 2015;15:1–15. [PubMed] [Google Scholar]
- 14.Lachman ME, Teshale S, Agrigoroaei S. Midlife as a Pivotal Period in the Life Course: Balancing Growth and Decline at the Crossroads of Youth and Old Age. Int J Behav Dev. 2015;39(1):20–31. doi: 10.1177/0165025414533223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Berry JG, Gay JC, Maddox KJ, et al. Age trends in 30 day hospital readmissions: US national retrospective analysis. BMJ. 2018;360:k497. doi: 10.1136/bmj.k497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bhuyan N. Millennials Don’t Have PCPs; Here’s Why They Should. AAFP. https://www.aafp.org/news/blogs/freshperspectives/entry/20181022fp-millennials.html. Published October 22, 2018. Accessed April 23, 2019.
- 17.Bazemore A, Petterson S, Peterson LE, Phillips RL. More Comprehensive Care Among Family Physicians is Associated with Lower Costs and Fewer Hospitalizations. Ann Fam Med. 2015;13(3):206–213. doi: 10.1370/afm.1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jiang HJ, Wier LM. All-Cause Hospital Readmissions among Non-Elderly Medicaid Patients, 2007: Statistical Brief #89. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006. http://www.ncbi.nlm.nih.gov/books/NBK53601/. Accessed April 24, 2017. [PubMed]
- 19.De Giorgi A, Boari B, Tiseo R, et al. Hospital readmissions to internal medicine departments: a higher risk for females? Eur Rev Med Pharmacol Sci. 2016;20(21):4557–4564. [PubMed] [Google Scholar]
- 20.Brahmbhatt J. Why Avoiding the Doctor is Men’s #1 Health Problem. Orlando Health. https://www.orlandohealth.com/content-hub/why-avoiding-the-doctor-is-mens-number-1-health-problem. Published June 30, 2016. Accessed April 23, 2019.
- 21.Himmelstein MS, Sanchez DT. Masculinity impediments: Internalized masculinity contributes to healthcare avoidance in men and women. Journal of Health Psychology. 2016;21(7):1283–1292. doi: 10.1177/1359105314551623. [DOI] [PubMed] [Google Scholar]
- 22.Himmelstein MS, Sanchez DT. Masculinity in the doctor’s office: Masculinity, gendered doctor preference and doctor–patient communication. Preventive Medicine. 2016;84:34–40. doi: 10.1016/j.ypmed.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 23.Alfandre DJ. “I’m Going Home”: Discharges Against Medical Advice. Mayo Clin Proc. 2009;84(3):255–260. doi: 10.4065/84.3.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Discharge Against Medical Advice in the United States, 2002-2011—ClinicalKey. https://www.clinicalkey.com/#!/content/playContent/1-s2.0-S0025619617300733?returnurl=null&referrer=null. Accessed April 24, 2019.
- 25.Alper E, O’Malley T, Greenwald J. Hospital discharge and readmission. UpToDate. https://www.uptodate.com/contents/hospital-discharge-and-readmission#H9. Accessed June 1, 2018.
- 26.Longman JM, Passey ME, Ewald DP, Rix E, Morgan GG. Admissions for chronic ambulatory care sensitive conditions - a useful measure of potentially preventable admission? BMC Health Serv Res. 2015;15. doi:10.1186/s12913-015-1137-0 [DOI] [PMC free article] [PubMed]
- 27.Ferrante JM, Shaw EK, Bayly JE, et al. Barriers and Facilitators to Expanding Roles of Medical Assistants in Patient-Centered Medical Homes (PCMHs) The Journal of the American Board of Family Medicine. 2018;31(2):226–235. doi: 10.3122/jabfm.2018.02.170341. [DOI] [PubMed] [Google Scholar]