Abstract
Background
National administrative datasets have demonstrated increased risk-adjusted mortality among patients undergoing interhospital transfer (IHT) compared to patients admitted through the emergency department (ED).
Objective
To investigate the impact of patient-level data not available in larger administrative datasets on the association between IHT status and in-hospital mortality.
Design
Retrospective cohort study with logistic regression analyses to examine the association between IHT status and in-hospital mortality, controlling for covariates that were potential confounders. Model 1: IHT status, admit service. Model 2: model 1 and patient demographics. Model 3: model 2 and disease-specific conditions. Model 4: model 3 and vital signs and laboratory data.
Participants
Nine thousand three hundred twenty-eight adults admitted to Medicine services.
Main Measures
Interhospital transfer status, coded as an unordered categorical variable (IHT vs ED vs clinic), was the independent variable. The primary outcome was in-hospital mortality. Secondary outcomes included unadjusted length of stay and total cost.
Key Results
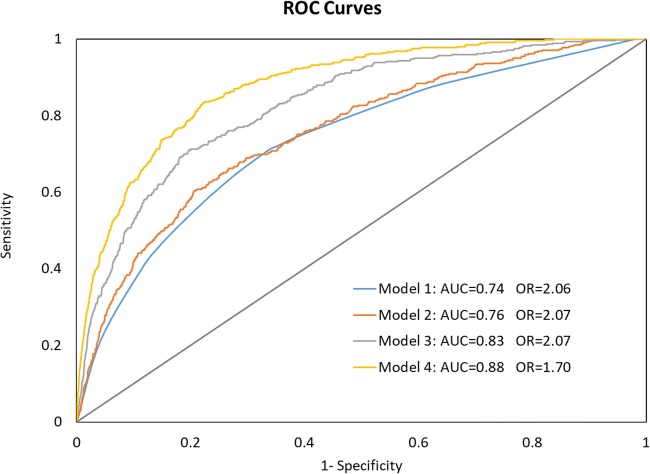
IHT patients accounted for 180 out of 484 (37%) in-hospital deaths, despite accounting for only 17% of total admissions. Unadjusted mean length of stay was 8.4 days vs 5.6 days (p < 0.0001) and mean total cost was $22,647 vs $12,968 (p < 0.0001) for patients admitted via IHT vs ED respectively. The odds ratios (OR) for in-hospital mortality for patients admitted via IHT compared to the ED were as follows: model 1 OR, 2.06 (95% CI 1.66–2.56, p < 0.0001); model 2 OR, 2.07 (95% CI 1.66–2.58, p < 0.0001); model 3 OR, 2.07 (95% CI 1.63–2.61, p < 0.0001); model 4 OR, 1.70 (95% CI 1.31–2.19, p < 0.0001). The AUCs of the models were as follows: model 1, 0.74; model 2, 0.76; model 3, 0.83; model 4, 0.88, consistent with a good prediction model.
Conclusions
Patient-level characteristics affect the association between IHT and in-hospital mortality. After adjusting for patient-level clinical characteristics, IHT status remains associated with in-hospital mortality.
Electronic supplementary material
The online version of this article (10.1007/s11606-020-05659-8) contains supplementary material, which is available to authorized users.
KEY WORDS: cost, hospital medicine, health services research
INTRODUCTION
Interhospital transfer (IHT) is defined as the transfer of hospitalized patients between acute care hospitals 1. Annually, approximately 1.6 million patients are transferred between hospitals.2,3 Several population-wide studies have demonstrated worse outcomes for patients admitted to hospitals following an interhospital transfer compared to patients admitted directly through the emergency department (ED): specifically increased risk-adjusted mortality, adverse events, cost, and length of stay.3–7 In one study utilizing the 2009 Nationwide Inpatient Sample dataset to examine outcomes related to medicine and surgical transfer patients to academic and non-academic medical centers, investigators found a twofold increase in risk-adjusted inpatient mortality among transfer patients.4 In another study utilizing the 2011–2012 University HealthSystem Consortium (UHC) Clinical database, IHT was associated with higher inpatient mortality compared to ED admissions (adjusted OR 1.36).3 Based on these large national datasets, IHT status itself has been independently associated with inpatient mortality. Although national administrative datasets are excellent for preliminary studies, limitations include coding errors, the inability to adjust for disease-specific conditions, or other patient-level clinical characteristics as is possible with smaller studies.8,9 Specifically, the studies highlighted above were unable to take into consideration important variables such as admitting service, detailed demographics, vital signs, or other laboratory data.3,4
Two previous single-center studies performed some two decades ago in the late 1980s and early 1990s were able to control for patient-level characteristics. Using a logistic regression model adjusting for severity of illness and other covariates, one study demonstrated that in-hospital mortality was nearly two times higher (OR 1.99) in IHT patients than in direct admissions.10 Additionally, a similar study in 1993 found that 12% of IHT internal medicine patients experienced in-hospital mortality compared to only 4% in non-transfer patients.11 Since this time, there have been significant improvements to the US healthcare system including implementation of electronic health records, expansion of hospitalists, and enhanced focus on quality improvement and patient safety. Notwithstanding, interhospital transfer outcomes remain poor—suggesting important and long-standing problems that are yet to be identified and addressed.7,12–15
In this study, our goal was to re-evaluate whether IHT status is associated with inpatient mortality, after adjusting for highly detailed patient-level characteristics not available in larger administrative datasets and not assessed in the recent health care climate.
METHODS
Study Population
This study was conducted at the Medical University of South Carolina (MUSC), an academic, tertiary referral center located in Charleston, South Carolina. The study was submitted to the MUSC Internal Review Board (IRB); it was deemed to fall under the umbrella of quality improvement, and thus the IRB advised that approval for human research was not required.
Adults ≥ 18 years of age admitted to the following services between July 1, 2013, and June 30, 2014, were included: general internal medicine or internal medicine subspecialty services (medical intensive care unit (ICU), cardiology, gastroenterology, hepatology, pulmonary, or hematology/oncology services). Using MUSC’s Enterprise Data Warehouse, data were extracted from two local databases: the Medical University Hospital Authority (MUHA) inpatient database, and the hospital’s patient accounting system.
Outcome Measures
In-hospital mortality was the primary outcome. The independent variable of interest was IHT status coded as an unordered categorical variable (IHT vs ED vs clinic). Secondary outcomes included unadjusted length of stay and total cost retrieved from the hospital’s patient accounting system and derived from univariate analysis. Hospital length of stay was calculated as date of admission to date of discharge. Total hospital costs are the summation of both fixed costs (expenses that do not fluctuate based on level of patient care) and variable costs (expenses driven by specific patient care). Both fixed and variable costs were available for all non-physician components of the hospital stay. These include, but are not limited to, surgical suites, catheterization suites, intensive care units, postoperative or post-procedural floor care, respiratory therapy, physical therapy, nursing and other floor personnel, anesthesia, recovery room, medical and surgical supplies, laboratory costs, pharmaceutical costs, pulmonary functions, telemetry, and social services. All costs are reported in 2014 US dollars.16
Covariates
Age, gender, race, insurance status, source of admission, and admitting service were coded as binary or categorical variables. The admitting service was defined as the service in which the attending physician billed for the admission. Distance from MUSC was modeled by determining miles between the center of the patient’s zip code and the medical campus. Accurate data regarding social determinants of care were limited, so the zip code of the patient’s residence was matched to 2010 Census data as a proxy for poverty status. The poverty variable is dichotomous and given a value of 1 if the zip code has ≥ 25% of its residents below the federal poverty level.17 Poverty status was included as a surrogate for income and socioeconomic status, which has been investigated in previous research 1. For the identified population, ICD-9-CM disease codes were captured from all preceding inpatient encounters, including any index admission encounter data. Dichotomous indicators for Elixhauser comorbidities (excluding cardiac arrhythmias), select Charlson comorbidities (myocardial infarction, cerebrovascular disease, and dementia), asthma, hyperlipidemia, and sickle cell disease were derived by using enhanced ICD-9-CM diagnosis codes.18 Because the goal of this study was to explore the potential effects of individual covariates, each comorbidity was included as a dichotomous variable (i.e., CHF yes/no), as has been used in prior research, as opposed to utilizing a summative comorbidity index.16 Admission vital signs, creatinine, potassium, sodium, blood urea nitrogen, white blood cell count, anion gap, albumin, INR, and total bilirubin were retrieved and coded as continuous variables, as has been used in prior research related to predictive modeling of in-hospital medicine patients.16 The earliest laboratory and clinical data available for the admission were used in the model, with a cut-off of 48 h after admission.
Statistical Analysis
Univariate analysis of demographic, clinical, and laboratory variables was performed to identify variables associated with interhospital transfer. For continuous variables, analysis of variance (ANOVA) was utilized to analyze differences among the means. For categorical variables, Pearson’s chi-square test was performed to determine difference in proportions between the admission groups. Four multivariable logistic regression analyses were performed to examine the independent association between IHT status and in-hospital mortality, controlling for several covariates that were potential confounders to the relationship between transfer and death. Groups of covariates were strategically added based on clinical judgment to assess for potential confounding. Backward selection was not performed and all covariates were retained in each model. Each model was run independently. Model 1: IHT status, admitting service, and the interaction between IHT status and admitting service. Model 2: IHT status, admitting service, and patient demographics (gender, age, race, insurance status, poverty, and distance from MUSC). Model 3: IHT status, admitting service, patient demographics, and disease-specific conditions (Elixhauser and Charlson comorbidities). Model 4: IHT status, admitting service, patient demographics, disease-specific conditions, admission vital signs, and patient laboratory data (Supplemental Fig. 1). Of the 9328 patients admitted to the internal medicine services between July 1, 2013, and June 30, 2014, 1757 patients had a missing vital sign or laboratory data. Analysis was performed to determine if the distribution of covariates differed based on whether or not variables were missing. Using logistic regression, a missing variable indicator was regressed on all of the covariates. Results confirmed there was a statistically significant difference in the distribution of covariates for patients with complete versus incomplete data, suggesting the data was not missing completely at random (MCAR). We hypothesized the data was missing at random (MAR) and performed multiple imputation. Multiple imputation is a general approach to the problem of missing data.19 We utilized the multiple imputation procedure in SAS statistical software (PROC MI) to impute the missing data ten times. All covariates were included in the imputation models. Model comparisons between multiple imputations (9328 patients) and complete case analysis (7571 patients) were performed and results were very similar, indicating it is unlikely the results are missing not at random (MNAR) which further supports the hypothesis the data was missing at random (MAR). Multicollinearity was assessed. Multicollinearity exists when two or more of the predictor variables are moderately or highly correlated, limiting conclusions from the model. To correct for multicollinearity, if two variables exhibited high correlation, one was dropped from the model based on clinical relevance. Receiver operating characteristic (ROC) curves for each model were created by plotting sensitivity against (1-specificity) for assessing the accuracy of predictions. The area under the ROC curve (AUC) was used to determine the quality of predictors. SAS 9.4 (SAS Institute Inc., Cary, NC) was used for statistical analyses.
RESULTS
A total of 9328 patients were admitted to medicine services from July 1, 2013, to June 30, 2014. Of these, 1548 patients (17%) were admitted via interhospital transfer, 4913 patients (53%) were admitted via the emergency department, and 2867 patients (30%) were admitted via clinic (Table 1). There was no difference in the age of patients based on source of admission. There were statistically significant differences in other demographics based on the location from which a patient was admitted. White patients were more likely to be admitted via IHT or clinic than were Black patients, while Black patients had a higher rate of admission from the ED (p < 0.0001). Additionally, more men than women were admitted via IHT or clinic (p < 0.0001). There were also significant differences in regard to admitting service based on the location from which a patient was admitted. IHT patients were most often admitted to cardiology or pulmonary critical care services, while ED patients were most often admitted to internal medicine services. Patients from clinic were admitted to cardiology, internal medicine, and hematology-oncology services with similar frequency (p < 0.0001) (Table 1).
Table 1.
Demographics
| Clinic (n = 2867) | ED (n = 4913) | IHT (n = 1548) | p value | |
|---|---|---|---|---|
| Age (mean, SD) | 56.3 ± 17.3 | 56.4 ± 18.0 | 56.4 ± 17.0 | 0.8929 |
| Age group (%) | 0.6216 | |||
| 18–34 | 14.9 | 15.1 | 14.0 | |
| 35–44 | 9.2 | 10.0 | 9.8 | |
| 45–54 | 15.6 | 16.6 | 16.7 | |
| 55–64 | 23.4 | 22.5 | 24.2 | |
| 65 + | 36.9 | 35.8 | 35.3 | |
| Gender (%) | < 0.0001 | |||
| Female | 45.7 | 49.7 | 44.2 | |
| Male | 54.3 | 50.3 | 55.8 | |
| Race (%) | < 0.0001 | |||
| Black | 36.0 | 46.7 | 37.5 | |
| Other | 3.0 | 2.2 | 3.2 | |
| White | 61.0 | 51.2 | 59.2 | |
| Insurance status (%) | < 0.0001 | |||
| Medicaid | 14.4 | 15.7 | 15.6 | |
| Medicare | 53.0 | 53.4 | 50.7 | |
| Commercial | 28.0 | 20.2 | 25.6 | |
| Uninsured | 4.7 | 10.7 | 8.1 | |
| Admitting service (%) | < 0.0001 | |||
| Cardiology | 27.3 | 18.7 | 29.5 | |
| Gastrointestinal | 5.0 | 6.4 | 13.4 | |
| Internal medicine | 27.6 | 48.9 | 20.4 | |
| Hematology-oncology | 25.6 | 10.3 | 8.4 | |
| Pulmonary critical care | 14.6 | 15.7 | 28.4 | |
| Distance (mean, SD) | 62.4 ± 112 | 40.5 ± 117 | 87.4 ± 100 | < 0.0001 |
| Far to MUSC (Distance > 50 miles) | 44.2 | 20.2 | 75.6 | < 0.0001 |
| Poverty (%) | 28.1 | 33.7 | 27.1 | < 0.0001 |
| Quarter of the admit date | 0.0202 | |||
| Jan–Mar | 23.4 | 24.9 | 24.9 | |
| Apr–Jun | 27.4 | 24.3 | 26.4 | |
| Jul–Sep | 25.0 | 26.2 | 22.9 | |
| Oct–Dec | 24.2 | 24.7 | 25.8 |
***p values represent a statistically significant difference between the 3 groups, based on ANOVA for continuous variables and chi-square for categorical variables
As might be expected, IHT patients often came from further distances away from MUSC than patients admitted via the ED or clinic (p < 0.0001). Patients from all sources were admitted with approximately equal frequency throughout the year despite statistical significance (p = 0.0202) (Table 1). Several comorbid diseases were more common in patients admitted via IHT compared to patients admitted via ED and clinic, including diseases such as renal failure, congestive heart failure, liver disease, coagulopathy, neurologic disorders, among others (Table 2).
Table 2.
Comorbidities
| Clinic (n = 2867) | ED (n = 4913) | IHT (n = 1548) | p value | |
|---|---|---|---|---|
| Comorbidities | ||||
| Congestive heart failure (%) | 26.4 | 27.0 | 31.1 | 0.0020 |
| Valvular heart disease (%) | 10.3 | 8.7 | 11.1 | 0.0083 |
| Pulmonary circulation disorders (%) | 14.9 | 13.4 | 15.7 | 0.0339 |
| Peripheral vascular disorders (%) | 9.1 | 10.8 | 9.0 | 0.0229 |
| Hypertension, uncomplicated (%) | 47.5 | 47.8 | 44.8 | 0.1104 |
| Hypertension, complicated (%) | 25.9 | 28.2 | 28.0 | 0.0744 |
| Paralysis (%) | 2.0 | 2.6 | 2.8 | 0.1614 |
| Other neurological disorders (%) | 12.6 | 18.4 | 15.6 | < 0.0001 |
| Chronic pulmonary disease (%) | 31.4 | 31.5 | 30.1 | 0.5651 |
| Diabetes, uncomplicated (%) | 26.7 | 30.6 | 30.3 | 0.0008 |
| Diabetes, complicated (%) | 9.8 | 13.2 | 9.4 | < 0.0001 |
| Hypothyroidism (%) | 12.9 | 12.3 | 13.6 | 0.3533 |
| Renal failure (%) | 28.6 | 30.6 | 32.6 | 0.0202 |
| Liver disease (%) | 12.8 | 15.1 | 23.1 | < 0.0001 |
| Peptic ulcer disease, excluding bleeding (%) | 2.4 | 3.5 | 4.1 | 0.0036 |
| AIDS/HIV (%) | 1.0 | 2.1 | 0.7 | < 0.0001 |
| Cancer (%) | 25.4 | 15.5 | 13.2 | < 0.0001 |
| Rheumatoid arthritis/collagen vascular diseases (%) | 5.5 | 6.3 | 7.2 | 0.0735 |
| Coagulopathy (%) | 17.7 | 13.8 | 21.8 | < 0.0001 |
| Obesity (%) | 11.0 | 13.1 | 14.1 | 0.0044 |
| Weight loss (%) | 20.2 | 21.3 | 20.6 | 0.4887 |
| Fluid and electrolyte disorders (%) | 49.8 | 54.2 | 48.7 | < 0.0001 |
| Blood loss anemia (%) | 2.8 | 3.6 | 4.3 | 0.0168 |
| Deficiency anemia (%) | 13.2 | 16.4 | 13.4 | 0.0002 |
| Alcohol abuse (%) | 6.6 | 11.7 | 11.7 | < 0.0001 |
| Drug abuse (%) | 7.9 | 12.0 | 7.6 | < 0.0001 |
| Psychoses (%) | 2.3 | 3.9 | 1.6 | < 0.0001 |
| Depression (%) | 26.3 | 28.7 | 22.5 | < 0.0001 |
| Asthma (%) | 9.7 | 10.7 | 5.0 | < 0.0001 |
| Hyperlipidemia (%) | 42.1 | 41.3 | 40.2 | 0.4508 |
| Sickle cell disease (%) | 3.5 | 4.4 | 1.6 | < 0.0001 |
| Myocardial infarction (%) | 13.6 | 17.9 | 20.2 | < 0.0001 |
| Dementia (%) | 0.6 | 1.3 | 0.7 | 0.0041 |
| Cerebrovascular disease (%) | 6.4 | 8.9 | 7.0 | 0.0002 |
Notable clinical characteristics were identified in IHT patients as compared to patients admitted from the ED and clinic (Table 3). The respiratory rate among IHT patients was higher than that in patients admitted via the ED or clinic (p < 0.0001). IHT patients had a higher WBC (p < 0.0001), BUN (p < 0.0001), and creatinine (p < 0.0001) levels than those patients admitted via the ED and/or clinic. Additionally, the serum albumin was lower in IHT patients compared to ED and clinic patients (2.8 g/dL vs. 3.1 g/dL vs. 3.1 g/dL, p < 0.0001).
Table 3.
Clinical Data
| Clinic (n = 2867) | ED (n = 4913) | IHT (n = 1548) | p value | |
|---|---|---|---|---|
| Vitals and labs* (mean, SD) | ||||
| Systolic BP, n = 9171 | 127.8 ± 24.3 | 129.8 ± 26.0 | 127.9 ± 26.0 | 0.0048 |
| Diastolic BP, n = 9289 | 65.0 ± 24.2 | 67.2 ± 22.6 | 65.6 ± 24.9 | 0.2852 |
| Respirations, n = 9288 | 18.7 ± 3.1 | 19.0 ± 4.1 | 19.5 ± 4.4 | < 0.0001 |
| Anion Gap, n = 9262 | 8.7 ± 3.5 | 10.4 ± 4.3 | 9.2 ± 3.5 | < 0.0001 |
| Creatinine, n = 9273 | 1.6 ± 1.8 | 1.9 ± 2.6 | 1.9 ± 2.2 | < 0.0001 |
| Potassium, n = 9280 | 4.07 ± 0.71 | 4.12 ± 0.80 | 4.12 ± 0.76 | 0.1659 |
| Sodium, n = 9279 | 137.0 ± 4.5 | 136.7 ± 4.9 | 136.9 ± 4.7 | 0.0233 |
| BUN, n = 9230 | 23.0 ± 21.4 | 25.1 ± 24.8 | 27.0 ± 23.7 | < 0.0001 |
| WBC, n = 9243 | 9.5 ± 11.8 | 10.9 ± 12.4 | 13.0 ± 25.5 | < 0.0001 |
| Albumin Serum, n = 7835 | 3.1 ± 0.7 | 3.1 ± 0.7 | 2.8 ± 0.7 | < 0.0001 |
| Total Bilirubin, n = 7819 | 1.5 ± 2.9 | 1.7 ± 3.3 | 2.7 ± 5.3 | < 0.0001 |
***1757 patients had a missing vital sign or laboratory data so the number varies per measure
Differences in unadjusted secondary outcomes were identified in IHT patients as compared to patients admitted from the ED and clinic (Table 4). While the mean and median lengths of stay for IHT patients were 8.4 and 5 days, respectively, those for patients admitted via ED were 5.6 and 3 days, respectively, and those for clinic admitted via clinic were 6.4 and 3.9 respectively (p < 0.001). There were significant differences in hospital costs between IHT patients as compared to patients admitted from the ED and clinic. The mean and median total costs for IHT patients were $22,647 and $12,662, respectively, those for ED patients were $12,968 and $7736, respectively, and those for clinic patients were $16,878 and $9822 respectively (p < 0.0001).
Table 4.
Outcomes
| Clinic (n = 2867) | ED (n = 4913) | IHT (n = 1548) | p value | |
|---|---|---|---|---|
| Length of stay (mean; median ± SD) | 6.4; 3.9 ± 15.8 | 5.6; 3.6 ± 9.1 | 8.4; 5.0 ± 11.3 | < 0.0001 |
| Total cost (mean; median ± SD) | 16,878; 9822 ± 27,444 | 12,968; 7736 ± 21,971 | 22,647; 12,662 ± 31,186 | < 0.0001 |
| Mortality (%) | 83 (2.9) | 221 (4.5) | 180 (11.6) | < 0.0001 |
There was a statistically significant difference in in-hospital mortality based on the location from which a patient was admitted. Patients admitted via IHT had significantly higher in-hospital mortality (11.6%) than those admitted from the emergency department (4.5%) or clinic (2.9%) (p < 0.0001) (Table 4). Based on regression analysis, compared to patients admitted via the emergency department, patients admitted via IHT had 2.06 times the odds of experiencing in-hospital mortality after adjusting for admitting service (model 1—OR 2.06, 95% CI 1.66–2.56, p value < 0.0001). The interaction between IHT status and admitting service was not statistically significant and therefore not included in model 1. After additionally adjusting for patient demographics in model 2, patients admitted via IHT similarly had 2.07 times of the odds of experiencing in-hospital mortality compared to patients admitted via the emergency department (model 2—OR 2.07, 95% CI 1.66–2.58, p value < 0.0001). The estimated odds of in-hospital mortality for IHT patients in model 3, which additionally controlled for disease-specific conditions, was unchanged at 2.07 times that for patients admitted via the ED (model 3—OR 2.07, 95% CI 1.63–2.61, p value < 0.0001). The final model, which additionally adjusted for patient laboratory data and vital signs, found that patients admitted via interhospital transfer had 1.70 times the odds of experiencing in-hospital mortality (model 4—OR 1.70, 95% CI 1.31–2.19, p value < 0.0001) (Table 5). The AUCs of the four regression models to evaluate prediction capability for in-hospital mortality were as follows: model 1, 0.74; model 2, 0.76; model 3, 0.83; model 4, 0.88 (Fig. 1), consistent with a good prediction model.]-->
Table 5.
Clinical Variables Associated with In-hospital Mortality (9328 Patients)
| Estimate | Std. error | Odds ratio (OR) | 95% lower OR | 95% upper OR | p value | |
|---|---|---|---|---|---|---|
| Admit source: ED (ref.) | ||||||
| Clinic | − 2.265 | 0.490 | 0.744 | 0.558 | 0.992 | 0.044 |
| Transfer from Hospital | − 0.296 | 0.147 | 1.695 | 1.312 | 2.191 | < 0.0001 |
| Admit service: GIM (ref.) | ||||||
| Cardiology | 0.528 | 0.131 | 1.839 | 1.246 | 2.714 | 0.002 |
| Gastrointestinal | 0.609 | 0.199 | 1.840 | 1.156 | 2.928 | 0.010 |
| Hematology-oncology | 0.610 | 0.237 | 1.517 | 0.995 | 2.314 | 0.053 |
| Pulmonary critical care | 0.417 | 0.215 | 3.330 | 2.436 | 4.551 | < 00001 |
| Age group (ref. 55–64) | ||||||
| 18–34 | 1.203 | 0.159 | 0.539 | 0.338 | 0.859 | 0.009 |
| 35–44 | − 0.618 | 0.238 | 0.614 | 0.390 | 0.968 | 0.036 |
| 45–54 | − 0.488 | 0.232 | 0.662 | 0.461 | 0.952 | 0.026 |
| 65 + | − 0.412 | 0.185 | 1.398 | 1.020 | 1.916 | 0.037 |
| Sex: male (ref) | 0.335 | 0.161 | 0.985 | 0.784 | 1.237 | 0.897 |
| Race: White (ref.) | ||||||
| Black | − 0.015 | 0.116 | 0.980 | 0.761 | 1.263 | 0.878 |
| Other | − 0.020 | 0.129 | 0.934 | 0.481 | 1.815 | 0.841 |
| Payor: commercial (ref.) | ||||||
| Medicaid | − 0.068 | 0.339 | 0.847 | 0.571 | 1.254 | 0.407 |
| Medicare | − 0.167 | 0.201 | 0.859 | 0.619 | 1.192 | 0.363 |
| Self-pay | − 0.152 | 0.167 | 1.174 | 0.739 | 1.865 | 0.497 |
| Poverty | 0.160 | 0.236 | 1.074 | 0.845 | 1.364 | 0.559 |
| Distance | 0.071 | 0.122 | 1.000 | 1.000 | 1.001 | 0.279 |
| Quarter of the admit date: Jul–Sep (ref.) | ||||||
| Jan–Mar | 0.000 | 0.000 | 1.211 | 0.891 | 1.644 | 0.221 |
| Apr–Jun | 0.191 | 0.156 | 1.219 | 0.896 | 1.659 | 0.207 |
| Oct–Dec | 0.198 | 0.157 | 1.384 | 1.026 | 1.866 | 0.033 |
| Congestive heart failure | 0.325 | 0.152 | 1.394 | 1.063 | 1.827 | 0.016 |
| Peripheral vascular disorders | 0.332 | 0.138 | 0.996 | 0.706 | 1.406 | 0.982 |
| Hypertension, uncomplicated | − 0.004 | 0.176 | 0.959 | 0.748 | 1.229 | 0.741 |
| Paralysis | − 0.042 | 0.127 | 0.659 | 0.345 | 1.258 | 0.207 |
| Other neurological disorders | − 0.417 | 0.330 | 2.002 | 1.566 | 2.560 | < 0.0001 |
| COPD | 0.694 | 0.125 | 1.061 | 0.837 | 1.345 | 0.625 |
| Diabetes, uncomplicated | 0.059 | 0.121 | 0.836 | 0.657 | 1.065 | 0.147 |
| Hypothyroidism | − 0.179 | 0.123 | 1.004 | 0.728 | 1.384 | 0.982 |
| Renal failure | 0.004 | 0.164 | 0.847 | 0.629 | 1.142 | 0.277 |
| Peptic ulcer disease, excluding bleeding | − 0.166 | 0.152 | 0.393 | 0.192 | 0.805 | 0.011 |
| AIDS/HIV | − 0.934 | 0.366 | 1.408 | 0.588 | 3.373 | 0.442 |
| Cancer | 0.342 | 0.446 | 1.108 | 0.821 | 1.494 | 0.503 |
| Rheumatoid arthritis/collagen vascular | 0.102 | 0.153 | 1.032 | 0.667 | 1.596 | 0.889 |
| Coagulopathy | 0.031 | 0.223 | 1.639 | 1.280 | 2.098 | < 0.0001 |
| Obesity | 0.494 | 0.126 | 0.810 | 0.573 | 1.144 | 0.232 |
| Weight loss | − 0.211 | 0.176 | 1.157 | 0.903 | 1.482 | 0.250 |
| Fluid and electrolyte Disorders | 0.146 | 0.126 | 1.834 | 1.411 | 2.384 | < 0.0001 |
| Blood loss anemia | 0.606 | 0.134 | 1.338 | 0.828 | 2.161 | 0.234 |
| Deficiency anemia | 0.291 | 0.245 | 0.549 | 0.392 | 0.768 | 0.001 |
| Alcohol abuse | − 0.600 | 0.172 | 1.073 | 0.752 | 1.533 | 0.696 |
| Drug abuse | 0.071 | 0.182 | 0.553 | 0.341 | 0.897 | 0.016 |
| Psychoses | − 0.592 | 0.246 | 0.889 | 0.468 | 1.689 | 0.720 |
| Depression | − 0.117 | 0.327 | 0.643 | 0.491 | 0.844 | 0.001 |
| Sickle cell | − 0.441 | 0.138 | 1.580 | 0.622 | 4.012 | 0.336 |
| Myocardial infarction | 0.457 | 0.476 | 1.295 | 0.989 | 1.696 | 0.061 |
| Dementia | 0.258 | 0.138 | 0.745 | 0.294 | 1.891 | 0.536 |
| Cerebrovascular disease | − 0.294 | 0.475 | 1.136 | 0.792 | 1.630 | 0.488 |
| Systolic BP (10-unit increase) | 0.128 | 0.184 | 0.903 | 0.864 | 0.944 | < 0.0001 |
| Respiration (2-unit increase) | − 0.102 | 0.023 | 1.115 | 1.074 | 1.158 | < 0.0001 |
| Anion gap (2-unit increase) | 0.109 | 0.019 | 1.209 | 1.147 | 1.274 | < 0.0001 |
| Creatinine | 0.190 | 0.027 | 0.940 | 0.879 | 1.006 | 0.075 |
| BUN | − 0.061 | 0.034 | 1.003 | 0.999 | 1.008 | 0.156 |
| White blood cell count (2-unit increase) | 0.003 | 0.002 | 1.012 | 1.004 | 1.020 | 0.002 |
| Serum albumin | 0.012 | 0.004 | 0.356 | 0.295 | 0.429 | < 0.0001 |
| Total bilirubin | − 1.032 | 0.095 | 1.030 | 1.008 | 1.051 | 0.006 |
Figure 1.
Comparison of receiver-operating characteristic curves of the four predictive models
Compared to admission to the general medicine service, admission to the pulmonary critical care service (OR 3.33, 95% CI 2.43–4.55, p value < 0.0001), gastrointestinal service (OR 1.84, 95% CI 1.16–2.93, p value = 0.0100), and cardiology service (OR 1.84, 95% CI 1.25–2.71, p value = 0.002) was associated with increased in-hospital mortality. Patients with other neurologic disorders (OR 2.00, 95% CI 1.57–2.56, p value < 0.0001), fluid and electrolyte disorders (OR 1.83, 95% CI 1.41–2.38, p value < 0.0001), coagulopathy (OR 1.64, 95% CI 1.28–2.10, p value < 0.0001), and congestive heart failure (OR 1.39, 95% CI 1.06–1.83, p value 0.0160) were also more likely to experience in-hospital mortality. Measures of association for all covariates included in the final model are reported in Table 5.
DISCUSSION
Our study demonstrates an association between IHT status and in-hospital mortality before and after adjusting for patient-level clinical characteristics. Patients admitted via interhospital transfer had 1.70 times the odds of experiencing in-hospital mortality compared to patients admitted via the emergency department, after adjusting for demographics, individual comorbidities, vital signs, and laboratory data. Our findings align with previous work in the area of outcomes associated with interhospital transfer utilizing both the Nationwide Inpatient Sample and University HealthSystem Consortium (UHC) Clinical administrative datasets.3,4 While these results could be explained by additional unmeasured, confounding patient characteristics, the consistent nature of these findings with those described in national administrative data reinforces the need to investigate this relationship further.
Our study is unique in that we were able to reveal certain patient-level characteristics do play a role in the relationship between IHT status and in-hospital mortality. Model 4, which additionally adjusted for vital signs and laboratory data, depicts a reduced odds ratio of in-hospital mortality for interhospital transfer patients compared to patients admitted from the emergency department from 2.08 to 1.70. This illustrates that vital signs and laboratory data do have some influence on the relationship between IHT status and in-hospital mortality and should be controlled for in future studies. However, even after adjusting for patient demographics, individual conditions, vital signs, and laboratory data, our final model indicates that interhospital transfer is associated with in-hospital mortality. Our findings on the importance of controlling for patient-level characteristics confirm the two previous single-center studies done two decades ago as mentioned in the introduction, proposing a long-standing problem yet to be fixed despite significant advances in our healthcare system.10,11 Our study suggests that the interhospital transfer process remains dangerous.
Our study does not provide an underlying etiology for the increased risk of in-hospital mortality for IHT patients. Prior hypotheses include (1) patients selected for IHT were at higher risk of death in a manner that was not captured by mortality risk scores, (2) physicians at transferring institutions provided substandard care, and (3) the transfer process itself was potentially harmful.3,20,21 Because our study focused on more patient-level characteristics as compared to mortality risk scores, we feel the first hypothesis is less likely. Our concern is that factors associated with the transfer process itself are potentially harmful including day of week of transfer, time of day of transfer, time delay from acceptance to transfer, interhospital communication, availability of outside records, reason for transfer, and other.22–26 Existent data on interhospital transfers that report worse outcomes than similar patients admitted directly from the emergency department suggest that the poor outcomes are due, at least in part, to the discontinuity of care for interhospital transfer patients.3 It has also been recently shown that nighttime transfer was associated with increased odds of ICU transfer and 30-day mortality.27 Unfortunately, we were unable to control for these residual variables.
We recognize limitations to this study. First, this was a retrospective study, and therefore residual confounding cannot be completely controlled. For instance, although the admitting service was defined as the service in which the attending physician billed for the admission, there were a few instances in which a patient was admitted to one service and immediately transferred to a different service and we were unable to control for this. Second, this study was performed at a single urban tertiary care center in the southeast that accepts a significant number of referrals from outside hospitals, potentially limiting generalizability to other types of hospitals. Third, we were unable to control for variables of the transferring hospital and transfer process itself.
Future directions for the current work include using regional and national data to confirm our findings. Additionally, we plan to develop a cumulative predictive model controlling for variables associated with the transferring hospital, the transfer process itself, and patient-level data to better evaluate the association between interhospital transfer and in-hospital mortality.
In summary, our study suggests that patient-level characteristics including individual diagnoses, vital signs, and laboratory data do affect the association between IHT and in-hospital mortality. After adjusting for patient-level clinical characteristics, IHT status remains independently associated with in-hospital mortality.
Electronic Supplementary Material
Covariates included in the four predictive models (DOCX 202 kb)
Acknowledgments
All contributors to this study are authors. All authors had access to the data and played a role in writing this Original Research manuscript. All authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Author Contributions
Marc Heincelman—study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content
Mulugeta Gebregziabher—study concept and design; analysis and interpretation of data; critical revision of the manuscript for important intellectual content
Elizabeth Kirkland—study concept and design; critical revision of the manuscript for important intellectual content
Skip Schumann—study concept and design; critical revision of the manuscript for important intellectual content
Andrew Schreiner—study concept and design; critical revision of the manuscript for important intellectual content
Phillip Warr—study concept and design; critical revision of the manuscript for important intellectual content
Jingwen Zhang—study concept and design; analysis and interpretation of data; critical revision of the manuscript for important intellectual content
Patrick Mauldin—study concept and design; analysis and interpretation of data; critical revision of the manuscript for important intellectual content
William P. Moran—study concept and design; analysis and interpretation of data; critical revision of the manuscript for important intellectual content
Don C. Rockey—study concept and design; analysis and interpretation of data; critical revision of the manuscript for important intellectual content
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mueller SK, Zheng J, Orav EJ, Schnipper JL. Rates, Predictors and Variability of Interhospital Transfers: A National Evaluation. J Hosp Med. 2017;12(6):435–442. doi: 10.12788/jhm.2747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Usher M, Sahni N, Herrigel D, et al. Diagnostic Discordance, Health Information Exchange, and Inter-Hospital Transfer Outcomes: a Population Study. J Gen Intern Med. 2018;33(9):1447–1453. doi: 10.1007/s11606-018-4491-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sokol-Hessner L, White AA, Davis KF, Herzig SJ, Hohmann SF. Interhospital transfer patients discharged by academic hospitalists and general internists: Characteristics and outcomes. J Hosp Med. 2016;11(4):245–250. doi: 10.1002/jhm.2515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hernandez-Boussard T, Davies S, McDonald K, Wang NE. Interhospital Facility Transfers in the United States: A Nationwide Outcomes Study. J Patient Saf. 2017;13(4):187–191. doi: 10.1097/PTS.0000000000000148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Durairaj L, Will JG, Torner JC, Doebbeling BN. Prognostic factors for mortality following interhospital transfers to the medical intensive care unit of a tertiary referral center. Crit Care Med. 2003;31(7):1981–1986. doi: 10.1097/01.CCM.0000069730.02769.16. [DOI] [PubMed] [Google Scholar]
- 6.Golestanian E, Scruggs JE, Gangnon RE, Mak RP, Wood KE. Effect of interhospital transfer on resource utilization and outcomes at a tertiary care referral center. Crit Care Med. 2007;35(6):1470–1476. doi: 10.1097/01.CCM.0000265741.16192.D9. [DOI] [PubMed] [Google Scholar]
- 7.Mueller S, Zheng J, Orav EJ, Schnipper JL. Inter-hospital transfer and patient outcomes: a retrospective cohort study. BMJ Quality & Safety. 2018:bmjqs-2018-008087. [DOI] [PMC free article] [PubMed]
- 8.Memtsoudis SG. Limitations associated with the analysis of data from administrative databases. Anesthesiology. 2009;111(2):449. doi: 10.1097/ALN.0b013e3181adf739. [DOI] [PubMed] [Google Scholar]
- 9.Hashimoto RE, Brodt ED, Skelly AC, Dettori JR. Administrative database studies: goldmine or goose chase? Evidence-based spine-care journal. 2014;5(2):74–76. doi: 10.1055/s-0034-1390027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gordon HS, Rosenthal GE. Impact of interhospital transfers on outcomes in an academic medical center. Implications for profiling hospital quality. Med Care. 1996;34(4):295–309. doi: 10.1097/00005650-199604000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Bernard AM, Hayward RA, Rosevear J, Chun H, McMahon LF. Comparing the hospitalizations of transfer and non-transfer patients in an academic medical center. Acad Med. 1996;71(3):262–266. doi: 10.1097/00001888-199603000-00019. [DOI] [PubMed] [Google Scholar]
- 12.Yanamadala S, Morrison D, Curtin C, McDonald K, Hernandez-Boussard T. Electronic Health Records and Quality of Care: An Observational Study Modeling Impact on Mortality, Readmissions, and Complications. Medicine. 2016;95(19):e3332–e3332. doi: 10.1097/MD.0000000000003332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sehgal NL, Wachter RM. The expanding role of hospitalists in the United States. Swiss Med Wkly. 2006;136(37–38):591–596. doi: 10.4414/smw.2006.11190. [DOI] [PubMed] [Google Scholar]
- 14.Stevens JP, Nyweide DJ, Maresh S, Hatfield LA, Howell MD, Landon BE. Comparison of hospital resource use and outcomes among hospitalists, primary care physicians, and other generalists. JAMA Internal Medicine. 2017;177(12):1781–1787. doi: 10.1001/jamainternmed.2017.5824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Beitler JR, Link N, Bails DB, Hurdle K, Chong DH. Reduction in hospital-wide mortality after implementation of a rapid response team: a long-term cohort study. Critical care (London, England) 2011;15(6):R269–R269. doi: 10.1186/cc10547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Heincelman M, Schumann SO, Riley J, et al. Identification of High Utilization Inpatients on Internal Medicine Services. Am J Med Sci. 2016;352(1):63–70. doi: 10.1016/j.amjms.2016.04.020. [DOI] [PubMed] [Google Scholar]
- 17.United States Census Bureau. American Fact Finder. Available at:. https://factfinder.census.gov/bkmk/table/1.0/en/ACS/10_3YR/S1701/0100000US.05000.003. Accessed November 20, 2019.
- 18.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 19.Sterne JAC, White IR, Carlin JB, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ. 2009;338:b2393. doi: 10.1136/bmj.b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hanmer J, Lu X, Rosenthal GE, Cram P. Insurance status and the transfer of hospitalized patients: an observational study. Ann Intern Med. 2014;160(2):81–90. doi: 10.7326/M12-1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singh JM, MacDonald RD. Pro/con debate: do the benefits of regionalized critical care delivery outweigh the risks of interfacility patient transport? Critical care (London, England) 2009;13(4):219–219. doi: 10.1186/cc7883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ehrmann DE. Overwhelmed and uninspired by lack of coordinated care: a call to action for new physicians. Acad Med. 2013;88(11):1600–1602. doi: 10.1097/ACM.0b013e3182a7f389. [DOI] [PubMed] [Google Scholar]
- 23.Iwashyna TJ. The incomplete infrastructure for interhospital patient transfer. Crit Care Med. 2012;40(8):2470–2478. doi: 10.1097/CCM.0b013e318254516f. [DOI] [PubMed] [Google Scholar]
- 24.Herrigel DJ, Carroll M, Fanning C, Steinberg MB, Parikh A, Usher M. Interhospital transfer handoff practices among US tertiary care centers: A descriptive survey. J Hosp Med. 2016;11(6):413–417. doi: 10.1002/jhm.2577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wagner J, Iwashyna TJ, Kahn JM. Reasons underlying interhospital transfers to an academic medical intensive care unit. J Crit Care. 2013;28(2):202–208. doi: 10.1016/j.jcrc.2012.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bosk EA, Veinot T, Iwashyna TJ. Which patients and where: a qualitative study of patient transfers from community hospitals. Med Care. 2011;49(6):592–598. doi: 10.1097/MLR.0b013e31820fb71b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mueller SK, Fiskio J, Schnipper J. Interhospital Transfer: Transfer Processes and Patient Outcomes. Journal of hospital medicine. 2019;14:E1–E6. doi: 10.12788/jhm.3192. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Covariates included in the four predictive models (DOCX 202 kb)