Abstract
Early childhood caries (ECC) is a largely preventable condition that occurs when children develop caries in their primary teeth before the age of six. National trends of ECC indicate that prevalence is decreasing, but disparities between various sociodemographic groups may be increasing, despite intervention efforts. Dynamic mechanisms in caries development are hypothesized to be responsible for the observed population distributions of disease. Agent-based models (ABMs) have been utilized to explore similar hypotheses in many areas of health research. Therefore, we developed an ABM of ECC development mechanisms and examined population outcomes of hypothetical preventive intervention scenarios. We found that risk-based targeting had minimal impact on population averages or disparities and was largely due to the strength of the dynamic mechanisms among those considered to be at high caries risk. Universally increasing intervention access reduced population caries prevalence, but increased disparities between different groups of caries risk profiles. We show that population distributions of ECC can emerge as a result of dynamic mechanisms that have been shown to drive disease development. Understanding the effectiveness of a proposed intervention in relation to the hypothesized mechanism(s) that contributes to the outcome of interest is critical to future efforts to address population disparities in ECC.
Keywords: agent-based modeling, computer simulation, dental care for children, dental caries, health status disparities, oral health
Introduction
Early childhood caries (ECC) is the most common chronic disease of childhood and one of the largest unmet healthcare needs for children (Newacheck et al. 2000; Dye et al. 2017). If not properly managed, the condition can progress in severity and culminate in long-lasting health consequences (Casamassimo et al. 2009). Prevalence of ECC in the United States (US) appears to be declining, possibly due to increased availability of effective preventive measures, including topical fluorides (Dye et al. 2017). However, the prevalence and severity of ECC continues to be higher among children from disadvantaged groups, including the poor and certain racial/ethnic minority groups. Epidemiologic studies demonstrate that ECC incidence is much higher, occurs at earlier ages, and once initiated, progresses much faster in disadvantaged than in majority and wealthier populations. Recent efforts to address these disparities through evidence-based behavioral interventions targeting populations experiencing higher disease burdens (e.g., racial/ethnic minorities, people living in poverty) have been unsuccessful (Batliner et al. 2018; Henshaw et al. 2018). Addressing population disparities may require a deeper understanding of the underlying mechanisms responsible for caries development, and better means of identifying intervention targets.
Methodological challenges have hampered a deeper understanding of ECC disparities. Traditional analytic methods (e.g., regression modeling) are not well-suited to evaluate the complex mechanisms that influence caries development because they do not account for dynamic and heterogeneous responses to individual risk factors, and rather, account for the average of such responses (Luke and Stamatakis 2012). However, there exist newer modeling approaches, such as agent-based models (ABMs), which may be more informative. ABMs are computer representations of complex adaptive systems that have been used across a variety of disciplines to describe and study complex systems that are composed of many dynamic and interacting ecological processes. Their focus is not on modeling static associations between 2 or more factors, but rather on modeling dynamic mechanisms, including directionality of feedback, and/or the shape of the interaction. Such models recognize that population health emerges from a complex set of pathways and mechanisms that cut across multiple levels of influence, the distributions of which are not adequately described merely by the sum of the individual parts (Diez Roux 2007; Mabry et al. 2013). This nonadditivity is referred to as “emergence.” Caries development reflects a dynamic process that emerges from feedback mechanisms occurring on multiple levels. Interventions targeting such mechanisms may modulate the social and biological feedback effects on population-level caries outcomes that may account for observed disparities in ECC.
Agent-based models have been highlighted by the Institute of Medicine (IOM 2015), and many others (Galea et al. 2010; Diez Roux 2011; Tracy et al. 2018) as a potential methodological solution to combine risk factors with mechanistic modeling in health to describe complex dynamic systems. Consequently, recognition of the importance of a systems science perspective is gaining momentum in the field of oral health research (Broomhead and Baker 2019). We applied a complex systems science approach to modeling the hypothesized processes and mechanisms driving caries experience in order to 1) promote understanding of how multilevel processes may interact to produce caries outcomes, and 2) demonstrate how targeting those processes via intervention may influence population disparities. We took an ABM approach, which, through computer simulation, allows the user to explore feedback among and between the individual components of the model, while simultaneously allowing evaluations of the emergent properties of the system as a whole. With large heterogeneity within populations related to individual risk for caries development, this approach allows for incorporation of individual-level changes in caries risk at every model time step, while also accounting for the dynamic effects of prevention mechanisms. Thus, use of ABM accounts for heterogeneous response through simple rule definition of competing risk and prevention dynamics, as opposed to a compartmental modeling framework in which hundreds of states may be required to encompass the range of possible states/outcomes. In this way, ABM allows for the study of processes we know to be important within a larger system but are too complex and intertwined to study in traditional statistical models.
Methods
We developed an ABM among a cohort of children aged 36 to 72 mo that simulates the progression of sound primary teeth to decayed, filled, or missing teeth (dfmt) due to caries in each child. This modeling approach allows us to account for complex dynamics between the person- and tooth-level that contribute to caries incidence and progression. Both children and their teeth are considered agents in this model, with feedback limited to the tooth-level. Briefly, model parameters are assigned by the researcher and initial parameter values are determined through model fitting procedures. The model is iterative in that it runs over several time-steps in which the initial parameter values in 1 time-step of the model probabilistically determine the initial parameter values at the next time-step. In other words, the starting state of the model’s agents are updated at the end of each time-step. This feature of ABM allows for the incorporation of feedback mechanisms.
Modeling Dental Caries—“Baseline Scenario”
We first developed a baseline model, using data from the 2013 to 2014 National Health and Nutrition Examination Survey (NHANES) that attempts to replicate the natural history of caries incidence and progression in children aged 3 to 6 y. Our model simulated a hypothetical cohort of 2,500 children and followed caries incidence and progression over 36 mo in primary teeth for each child. The mechanisms of the model influence both tooth and person agents. At the tooth-level, a primary tooth can be classified as 1 of 4 binary (yes/no) states: sound, decayed, filled, or missing due to caries. At the person-level, children in our model had 1 binary state of having received fluoride application or not.
Model Assumptions
We began with the following assumptions. Transition of teeth from 1 state to another (e.g., from “sound” to “decayed”) is probabilistic and includes the following feedback assumptions: 1) the more decayed and missing (due to caries) teeth a child has, the more likely sound teeth will become decayed at a future model time-step (positive feedback); and 2) receipt of topical fluoride reduces the probability of future caries equally for all sound teeth per child (negative feedback). We parametrically defined the magnitude of these feedback effects by exploring across a large range of magnitudes of these effects to gauge the patterns of our outcome responses. For model initiation, we assumed that most children had full dentition (20 teeth) at 36 mo and all other children without full dentition were missing teeth due to caries. We also assumed no eruption of permanent teeth. Figure 1 presents a model diagram that depicts the relationship between model parameters, transitions, and feedback loops.
Figure 1.

Model depiction with transitions and feedback. Model structure: probabilities are applied to progression through the stages at both the person- and tooth-level. At the person level, “decay probability” represents the probability of a child developing decay in at least 1 tooth. At each discrete time-step representing 1 mo, the probability of at least 1 tooth becoming decayed is nonzero for every child in the model. Subsequently, “care probability” represents the probability that the child receives restorative care following the development of decay. If the child receives fluoride during the model timeline, then the person-level decay probability will be reduced by the value of the “fluoride effect” parameter. The value of this parameter wanes over time and decay probability returns to its original value 6 mo after each fluoride treatment. On the tooth-level, “decay probability” represents the probability of decay in additional teeth following the person-level development of decay. On the tooth level, decayed teeth can progress to missing due to decay.
At initialization, 50,000 teeth (i.e., 20 teeth per child for 2,500 children) are probabilistically assigned a caries status based on distributions of untreated decay, missing due to caries, and the percentage of sound teeth among 3 y-olds in NHANES in 2013. At each discrete time-step representing 1 mo, the probability of at least 1 tooth becoming decayed is nonzero for every child in the model, that is, person-level “decay probability.” Upon initial decay, additional instances of decay may occur within the child (among other sound teeth), that is, tooth-level “decay probability.” The probability that a child receives restorative care, that is, “care probability,” reflects a researcher-defined parameter value assuming the child has at least 1 instance of untreated decay. If the child probabilistically seeks restorative treatment for decay, we assumed all other decayed teeth are restored simultaneously. In our baseline model, children probabilistically seeking treatment will also receive a topical fluoride application at the time of care. Any receipt of fluoride will decrease the sound-to-decayed rate for that child by the value of a fluoride parameter, that is, “fluoride effect.” In our model, fluoride effects decrease exponentially over time, eventually reaching 0 after 6 mo. Additional fluoride applications at subsequent points refresh the effectiveness of fluoride to the maximum level of preventive effectiveness (as set by the researcher). Transition between states is probabilistic and determined by a combination of the decay states of other teeth in the mouth. The cycle of decay experience and the opportunity to obtain dental care repeats for 36 total time-steps, each time-step representing 1 mo. Model statistics are collected at the end of each discrete time-step.
Model Outcomes
This model assessed 2 commonly used oral health outcome measures: prevalence of caries experience and average number of teeth with untreated decay (i.e., magnitude of caries burden). Caries experience is defined as a child having had any dfmt (due to caries) at any time-point during the model.
Model Calibration
To estimate baseline parameters for dfmt, we fit 3 model outcomes to the NHANES data: prevalence of caries experience at the person-level, and percentage of untreated decay and sound teeth at the tooth-level. Using the Nelder-Mead optimizer, we minimized the sum-squared error between the model outcomes and the data. We used Latin hypercube sampling in order to identify a parameter value set within a range that reflected reasonable real-life values (e.g., monthly probability of decay and care-seeking probability) and the generated caries experience, and the percentage of decayed and sound teeth outcomes that approximated longitudinal values obtained from the NHANES data. While Latin hypercube sampling is commonly used to identify initial values for parameter estimation, we used it to identify baseline parameter values that both represent a reasonable qualitative fit, and are aligned in magnitude with existing knowledge of decay and care-seeking probabilities. Due to parameter unidentifiability (Kao and Eisenberg 2018), the absolute values of these parameters are not meant to be extrapolated as estimates of true population caries incidence rates, but rather, a representation of a quantitative value that we modify in order to better understand the processes that caries incidence contributes to. Additional information on model calibration methods, fitted model parameter values (Appendix Table S1), and additional results, can be found in the supplemental Appendix.
Fluoride Intervention Scenarios
In addition to the baseline scenario, in which fluoride was only received alongside restorative care, 2 additional intervention scenarios were evaluated. These scenarios approximated approaches to intervention in the real world in which different children in the model were targeted to receive increased access to preventive fluoride applications. Specifically, we evaluated the effects of providing increased access to fluoride applications for children who were considered “high-risk” at model initialization (i.e., “high-risk targeting”), and when receipt of fluoride for the same percentage of children at any point in time was randomly assigned (i.e., “universal targeting”). Children were considered high risk if they had at least 1 tooth with untreated decay at initialization. The models maintain a record of when each child received fluoride, and its effect over time. Importantly, we characterized disparities in our model as the absolute difference in oral health outcome measures between high- and low-risk agent populations.
Sensitivity Analyses
To assess the impact of our assumptions on our results, we explored a range of model outcomes associated with the parameter values by perturbing multiple parameter values: 1) the rate at which fluoride effectiveness decreases over time; 2) the length of time that it takes for the effectiveness of a single fluoride application to reach zero; 3) the maximum value that fluoride can decrease the decay probability; and 4) the effect of increasing care-seeking behavior.
Results
Model outcomes fit the trends of the NHANES data within 95% confidence intervals for the prevalence of caries experience and the percentage of untreated decay (Fig. 2). However, the model underestimated the percentage of sound teeth by an absolute value of approximately 9%. This is likely due to assumptions related to having a complete primary dentition by age 3 and the care probability at each time-step of the model. That is, to properly fit caries experience and untreated decay in this population, we needed to overestimate the amount of care-seeking behavior to prevent feedback of untreated decay from increasing beyond the data.
Figure 2.
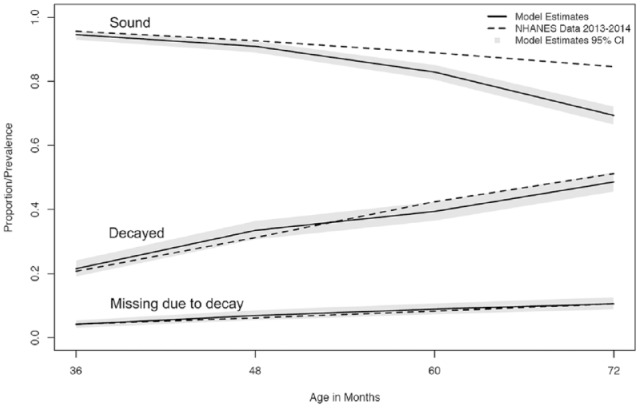
Caries model fit (baseline scenario) to National Health and Nutrition Examination Survey (NHANES) data.
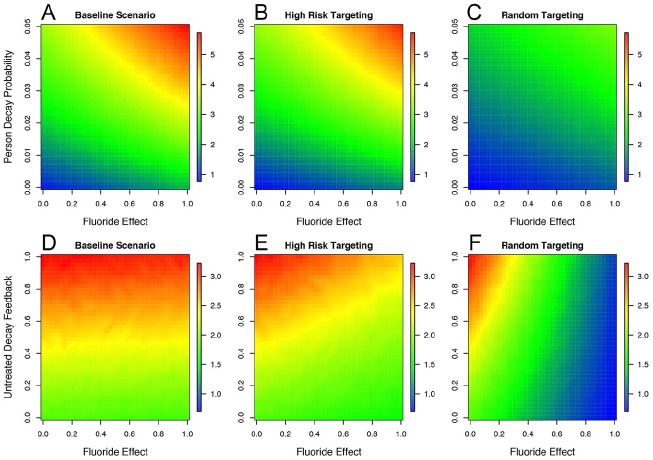
Heat maps (Fig. 3) illustrate the range of caries experience prevalence for combinations of 4 parameter values. Panels 3A through 3C illustrate the caries experience prevalence outcomes by fluoride effect and person-level decay probability parameter values (see Fig. 1) under each intervention scenario. These parameters represent the percentage decrease in risk of caries progression in sound teeth due to fluoride, and the baseline risk of caries incidence in sound teeth, respectively. We found that the outcome of caries experience relies primarily on the average person-level decay probability in the population and not on the effectiveness of fluoride. While the parameters have similar effects on the outcome when targeting high-risk children relative to the baseline scenario, we found that universal targeting of fluoride (panel 3C) results in broadly lower caries experience prevalence than both high-risk targeting and the baseline scenario when the average decay probability is high. At lower values, the patterns of caries experience are equivalent.
Figure 3.
Heat maps of the average caries experience prevalence for each fluoride targeting scenario according to values of person-level decay probability and fluoride effect. Caries experience prevalence (heat color bar) across a range of parameter values for person-level decay probability (y-axis) in interaction with fluoride effect (x-axis) for the baseline model scenario (A), the high-risk targeting scenario (B), and the universal targeting scenario (C). Caries experience prevalence (heat color bar) across parameter values for untreated decay feedback (y-axis) in interaction with fluoride effect (x-axis) are shown for the baseline model scenario (D), the high-risk targeting scenario (E), and the universal targeting scenario (F).
Panels 3D through 3F illustrate caries experience prevalence outcomes by the strength of the positive feedback between additional untreated decay (tooth level) and future decay probability (person level), and the size of the fluoride effect. Across all 3 scenarios, the positive feedback due to untreated decay has no effect on caries experience prevalence. The effectiveness of fluoride, however, results in substantially different caries experience outcomes under universal targeting (panel 3F), compared to the baseline and high-risk targeting scenarios.
Figure 4 illustrates the average number of teeth with untreated decay per child, by the same parameters as Figure 3. In panels 4A through 4C, we found that, similar to caries experience prevalence, high-risk targeting and the baseline scenario do not differ qualitatively in terms of color patterning of the outcome. However, universal targeting results in a substantially lower caries burden overall. For all intervention scenarios, greater effectiveness of fluoride increases the average caries burden in the population. This outcome is further explored in panels 4D through 4F, showing that when fluoride effectiveness is high, the effect of the positive feedback due to untreated decay in both high-risk and universal targeting is mitigated, compared to the baseline. However, the effects are much larger in universal targeting than in high-risk targeting.
Figure 4.
Heat maps of the average population’s untreated decay burden (i.e., untreated decay count per child) for each fluoride targeting scenario according to values of person-level decay probability and fluoride effect. The average number of teeth with untreated decay per child (heat color bar) outcome across a range of parameter values for person decay probability (y-axis) in interaction with fluoride effect (x-axis) for the baseline model scenario (A), the high-risk targeting scenario (B), and the universal targeting scenario (C). The average number of teeth with untreated decay per child (heat color bar) across parameter values for untreated decay feedback (y-axis) in interaction with fluoride effect (x-axis) are shown for the baseline model scenario (D), the high-risk fluoride targeting scenario (E), and the universal fluoride targeting scenario (F).
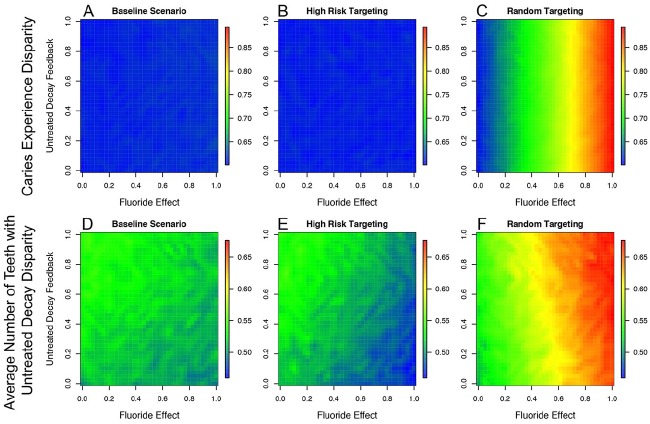
Figure 5 illustrates the disparities in caries experience and in untreated caries between high- and low-risk children in the population for each intervention scenario. With respect to the prevalence of caries experience, panels 5A and 5B indicate that targeting high-risk children has no effect on the population disparity in caries experience prevalence between high- and low-risk children relative to the baseline model, regardless of the average probability of decay in the population and the effectiveness of fluoride. Increasing population access to the intervention through universal targeting (panel 5C), however, increases the population disparity in the outcome between high- and low-risk children with increasing effectiveness of fluoride. With respect to caries burden (5D through 5F), targeting high-risk children in the population minimally reduces the population disparity in caries burden relative to the baseline model. In both cases (5D and 5E), the disparity in caries burden between high- and low-risk children decreases with increasing fluoride effectiveness, the magnitude of which is dependent on the average probability of decay in the population. Populations with greater risk of decay, on average, will see greater reductions in disparities due to the intervention compared to lower risk populations. Similar to caries experience, increasing access to the intervention via universal targeting (5F) will increase the disparity in caries burden between high- and low-risk children in the population. The magnitude of the difference is dependent on the average risk of decay in the population and the effectiveness of the fluoride intervention.
Figure 5.
Heat maps of disparities in caries experience and untreated decay burden between high and low risk children in the population for each scenario. The size of the disparity in ECC outcome between high- and low-risk children at model initialization (heat color bar) across a range of parameter values for untreated decay feedback (y-axis) in interaction with fluoride effect (x-axis). Disparities in caries experience prevalence between high- and low-risk children are depicted for the baseline scenario (A), the high-risk scenario (B), and the universal targeting scenario (C). Whereas disparities in average number of teeth with untreated decay are depicted in D, E and F, respectively. ECC, early childhood caries.
Discussion
Our model indicates that increasing population-wide access to effective intervention would decrease population averages of the outcome, but potentially increase within-population disparities in the outcome. Targeting interventions to those at highest risk had minimal effect on reducing population averages or disparities. Additionally, the presence and magnitude of any intervention effect on improving population outcomes due to intervention targeting was dependent on the particular outcome under study, the mechanisms driving the studied outcomes, and the presence or absence of any interaction between the intervention effectiveness and the caries-producing mechanisms. Lastly, the shape of the interaction between the intervention effectiveness and the strength of the feedback mechanisms appeared to dictate whether targeting segments of the population would reduce population disparities, and to what degree.
Our model results replicate what has been observed in US-based population surveillance of ECC: overall prevalence has decreased, but disparities in prevalence between socioeconomic and racial/ethnic groups appear to be increasing (Dye et al. 2017). By its inclusion of dynamic mechanisms, our model may provide insight into why ECC intervention efforts in high-risk populations (Batliner et al. 2018; Henshaw et al. 2018) have had limited effects. For example, the observed differences in caries burden across high- and low-risk children are primarily a result of differences in the strength of the positive feedback mechanism on future risk of decay due to untreated caries. Whereas, the strength of fluoride effectiveness on risk of future decay is the same for every child. In our model, an additional 25% of children received topical fluoride applications in both intervention scenarios relative to the baseline. In the case of universal targeting, all children have the same probability of receiving the intervention. We find that greater fluoride effectiveness actually increases caries burden, which, while surprising, highlights the importance of the role of the interactive effect of dynamic feedback. That is, among low-risk children, the application of fluoride in concert with low existing risk of future caries, results in absolute risk reduction, whereas the interactive effects among high-risk children on the risk of future decay are nearly null. Therefore, relative to the baseline scenario, the population disparity in caries burden between high- and low-risk children increases, but population averages decrease. This is exacerbated by the fact that high-risk children are a population minority; therefore, fewer high-risk children are receiving the intervention compared to low-risk children. For these same reasons, population effects of the intervention relative to the baseline scenario are minimal in the case of high-risk targeting.
Our model highlights that changes to population outcomes are mechanism dependent. Positive feedback mechanisms on the probability of future decay due to additional untreated decay does not have an impact on population prevalence of caries experience as defined in this model in that it relates to only the first occurrence of caries. Whereas caries burden is affected by subsequent or additional occurrences of untreated decay. Therefore, targeting interventions to populations with a higher caries risk may be ineffective if the goal is to reduce caries experience, that is, prevent first occurrence of caries. On the other hand, we would expect that universal targeting would generally delay the onset of caries to later ages, thereby further reducing the overall prevalence and burden. The absolute difference in caries prevalence between high- and low-risk children, however, will increase because of the preventive effects of the intervention among low-risk children and the lack of effect among high-risk children. We observe similar trends in the US as access to preventive services has increased over time. These findings corroborate those of Cerdá et al. (2014), which suggest that while universal targeting reduces undesirable outcomes more than targeted experiments, neither decrease inequality.
Our study has important limitations. This model is a simplified representation of the dynamic, heterogeneous, and individual-specific process of caries development in children. As such, the model results are not meant to be predictive or provide statistical estimates. Rather, we aim to demonstrate how and when dynamic, multi-level feedback responses to a preventive intervention lead to interdependent biological and social processes contributing to caries outcomes. By highlighting the important mechanisms of caries experience and care-seeking behavior, the absolute values of the percentage of sound teeth and care-seeking behavior should not affect our results. Furthermore, our results and discussion emphasize outcomes relative to a baseline scenario fit to empirical data and represent the parameter- and model-specific outcomes relative to this fit. Thus, our parameter values are data-specific, and should not be interpreted as absolute estimates. Lastly, our model presents feedback processes to be abstract, and applied as a homogeneous effect for all individuals, whereas existing caries create higher risk for additional caries incidence in the same child. In real populations, this feedback may manifest because of social factors, such as socioeconomic status, access to care, differences in family priorities related to dental behaviors, and diet. Future iterations of this model will operationalize this feedback as a complex interaction between multiple social factors, and function heterogeneously by child because of these interactions.
Our model illustrates how effectiveness of an intervention reducing ECC outcomes within a population is dependent on what mechanisms are responsible for variations in the outcome, as well as the strength of those mechanisms in the population targeted by the intervention. Understanding the effectiveness of a proposed preventive intervention in relation to the hypothesized mechanism(s) driving the outcome of interest may be critical to future efforts to address population disparities in ECC between groups with varying caries risk profiles.
Author Contributions
B. Heaton, contributed to conception, design, data acquisition, analysis, and interpretation, drafted and critically revised the manuscript; S.T. Cherng, contributed to design, data analysis, and interpretation, drafted and critically revised the manuscript; W. Sohn, contributed to data interpretation, critically revised the manuscript; R.I. Garcia, S. Galea, contributed to design and data interpretation, critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work.
Supplemental Material
Supplemental material, DS_10.1177_0022034520909841 for Complex Systems Model of Dynamic Mechanisms of Early Childhood Caries Development by B. Heaton, S.T. Cherng, W. Sohn, R.I. Garcia and S. Galea in Journal of Dental Research
Footnotes
A supplemental appendix to this article is available online.
This report reflects research funded by the National Institute of Dental and Craniofacial Research (K99DE025917, R00DE 025917).
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
ORCID iD: B. Heaton  https://orcid.org/0000-0002-3097-4717
https://orcid.org/0000-0002-3097-4717
References
- Batliner TS, Tiwari T, Henderson WG, Wilson AR, Gregorich SE, Fehringer KA, Brega AG, Swyers E, Zacher T, Harper MM, et al. 2018. Randomized trial of motivational interviewing to prevent early childhood caries in American Indian children. JDR Clin Trans Res. 3(4):366–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broomhead T, Baker SR. 2019. Systems science and oral health: implications for dental public health? Community Dent Health. 36(1):55–62. [DOI] [PubMed] [Google Scholar]
- Casamassimo PS, Thikkurissy S, Edelstein BL, Maiorini E. 2009. Beyond the dmft: the human and economic cost of early childhood caries. J Am Dent Assoc. 140(6):650–657. [DOI] [PubMed] [Google Scholar]
- Cerdá M, Tracy M, Ahern J, Galea S. 2014. Addressing population health and health inequalities: the role of fundamental causes. Am J Public Health. 104(Suppl 4): S609–S619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux AV. 2007. Integrating social and biologic factors in health research: a systems view. Ann Epidemiol. 17(7):569–574. [DOI] [PubMed] [Google Scholar]
- Diez Roux AV. 2011. Complex systems thinking and current impasses in health disparities research. Am J Public Health. 101(9):1627–1634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dye BA, Mitnik GL, Iafolla TJ, Vargas CM. 2017. Trends in dental caries in children and adolescents according to poverty status in the United States from 1999 through 2004 and from 2011 through 2014. J Am Dent Assoc. 148(8):550–565.e7. [DOI] [PubMed] [Google Scholar]
- Galea S, Riddle M, Kaplan GA. 2010. Causal thinking and complex system approaches in epidemiology. Int J Epidemiol. 39(1):97–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henshaw MM, Borrelli B, Gregorich SE, Heaton B, Tooley EM, Santo W, Cheng NF, Rasmussen M, Helman S, Shain S, et al. 2018. Randomized trial of motivational interviewing to prevent early childhood caries in public housing. JDR Clin Trans Res. 3(4):353–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IOM (Institute of Medicine). 2015. Assessing the use of agent-based models for tobacco regulation. Washington (DC): The National Academies Press. [PubMed] [Google Scholar]
- Kao YH, Eisenberg MC. 2018. Practical unidentifiability of a simple vector-borne disease model: implications for parameter estimation and intervention assessment. Epidemics. 25:89–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luke DA, Stamatakis KA. 2012. Systems science methods in public health: dynamics, networks, and agents. Ann Rev Public Health. 33:357–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mabry PL, Milstein B, Abraido-Lanza AF, Livingood WC, Allegrante JP. 2013. Opening a window on systems science research in health promotion and public health. Health Educ Behav. 40(1 Suppl):5S–8S. [DOI] [PubMed] [Google Scholar]
- Newacheck PW, Hughes DC, Hung YY, Wong S, Stoddard JJ. 2000. The unmet health needs of America’s children. Pediatrics. 105(4 Pt 2):989–997. [PubMed] [Google Scholar]
- Tracy M, Cerdá M, Keyes KM. 2018. Agent-based modeling in public health: current applications and future directions. Ann Rev Public Health. 39:77–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, DS_10.1177_0022034520909841 for Complex Systems Model of Dynamic Mechanisms of Early Childhood Caries Development by B. Heaton, S.T. Cherng, W. Sohn, R.I. Garcia and S. Galea in Journal of Dental Research