Short abstract
Objective
This study was performed to compare the clinical effects of locking plates (LPs) with those of hook plates (HPs) in the treatment of Neer type II distal clavicle fractures.
Methods
From August 2014 to April 2018, 64 patients with Neer type II distal clavicle fractures were treated in our department. The clinical effects were assessed with respect to the operation time, intraoperative blood loss, incision length, fracture healing, postoperative pain, postoperative complications, and postoperative shoulder joint function.
Results
There were no significant differences in the healing time, operation time, or intraoperative blood loss between the LP and HP groups. The incision length was significantly shorter in the LP than HP group, and the postoperative complication rate was significantly lower in the LP than HP group. The visual analog scale score, Constant–Murley score, and University of California Los Angeles score were significantly better in the LP than HP group.
Conclusions
Compared with HPs, the use of LPs involves a smaller incision in the treatment of Neer type II distal clavicle fractures and significantly reduces postoperative pain and complications. Therefore, priority can be given to the use of LPs in the treatment of Neer type II distal clavicle fractures.
Keywords: Distal clavicle fracture, locking plate, clavicle hook plate, curative effect, Neer type II, postoperative complications, postoperative pain
Introduction
The clavicle is the only bone scaffold connecting the upper limb and trunk. Fractures are prone to occur when this bone is subjected to external forces. Clavicle fractures account for 2% to 5% of fractures in adults and 10% to 15% of fractures in children.1,2 A distal clavicle fracture is defined as a fracture that occurs in the distal one-third of the lateral clavicle, and such fractures account for 15% to 30% of all clavicle fractures.3 Neer1 divided distal clavicle fractures into three types according to the relationship between the fracture line and the coracoclavicular ligament and acromioclavicular joint: Neer types I, II, and III. Neer type I and III fractures can achieve ideal healing with nonsurgical treatment because the proximal end of the fracture is fixed by the coracoclavicular ligament; however, Neer type II fractures occur in the medial coracoclavicular ligament. Because the distal part of the fracture is pulled by the limbs and proximal trapezius muscle, the fracture ends often become markedly displaced, and the fracture nonunion rate is high. Internal fixation is often needed for such fractures. Several surgical treatments are available for distal clavicle fractures, including a Kirschner wire tension band, coracoclavicular screw, distal clavicle locking plate (LP), clavicle hook plate (HP), and arthroscopic treatment.4 Among these treatments, distal clavicle LPs and clavicle HPs are commonly used for the treatment of Neer type II distal clavicle fractures. The purpose of this study was to compare the clinical efficacy of these two surgical methods in the treatment of Neer type II distal clavicle fractures.
Materials and methods
Patients
This study involved patients with Neer type II distal clavicle fractures who were treated in our department from August 2014 to April 2018. The inclusion criteria were fresh closed fractures diagnosed as Neer type II distal clavicle fractures by a preoperative X-ray examination of the shoulder joint, treatment with an LP or clavicle HP for internal fixation, and postoperative follow-up for treatment and functional exercises. The exclusion criteria were other injuries or diseases that could affect the surgical treatment and prognosis of the clavicle fracture, a preoperative history of shoulder pain, and an inability to complete follow-up. The patients were divided into an LP group and a clavicle HP group using a random grouping method.
Measurement of distal clavicle bone block
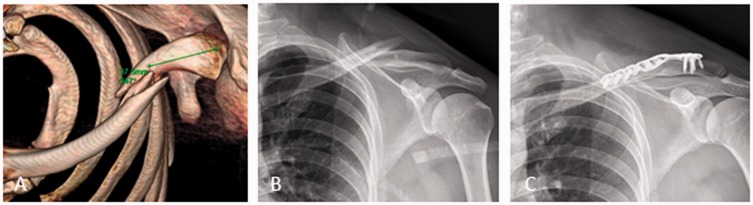
Before surgical treatment, we measured and recorded the length of the distal clavicle fracture block of each patient using our hospital’s preoperative three-dimensional computed tomography imaging system (Figures 1(a), 2(a)).
Figure 1.
Imaging examination of a patient undergoing treatment with a locking plate. (a) Preoperative three-dimensional computed tomography. (b) Preoperative X-ray imaging. (c) Postoperative X-ray imaging. The length of the distal clavicle fracture block was 37.5 mm.
Figure 2.
Imaging examination of a patient undergoing treatment with a hook plate. (a) Preoperative three-dimensional computed tomography. (b) Preoperative X-ray imaging. (c) Postoperative X-ray imaging. The length of the distal clavicle fracture block was 21.0 mm.
Surgical methods
LP group
After satisfactory brachial plexus anesthesia, the patient was placed in the supine position. Shoulder pads were used to raise the affected side, and the patient’s head was leaned toward the healthy side. In the operative area, the skin incision over the upper clavicle extended from the lateral clavicle to the lateral acromioclavicular margin. The acromioclavicular joint capsule was not incised. After clearing the hematoma at the broken end of the fracture, the fracture was anatomically reduced and temporarily fixed with reduction forceps or Kirschner wires. A titanium LP (Tianjin Walkman Biomaterial Co., Ltd., Tianjin, China) was placed on the clavicle, and several locking screws were screwed into the distal and proximal ends of the fracture. During the operation, C-arm fluoroscopy was used to confirm that the positions of the plate and screws were satisfactory and that no screw had entered the acromioclavicular joint. A large amount of saline was used to wash the wound and suture the wound layer by layer (Figure 1).
HP group
After satisfactory brachial plexus anesthesia, the patient was placed in the supine position. Shoulder pads were used to raise the affected side, and the patient’s head was leaned toward the healthy side. Routine disinfection and towel-laying were performed in the operative area. A skin incision was made with the fracture end as the center. The fracture end and acromioclavicular joint were exposed layer by layer. After clearing the hematoma at the broken end of the fracture, the fracture was anatomically repositioned, and the appropriate type of titanium clavicle HP (Tianjin Walkman Biomaterial Co., Ltd.) was selected. After proper shaping, the hook was inserted into the subacromioclavicular joint along the posterior side of the acromioclavicular joint, and the plate was pressed down to reduce the fracture. The plate was placed on the lateral upper edge of the clavicle. During the operation, C-arm fluoroscopy was used to confirm the accurate position of the clavicle HP. Finally, the plate was fixed with screws, a large amount of saline was used to wash the wound, and the incision was sutured layer by layer (Figure 2).
Postoperative management
Forearm suspension was used for 3 weeks after the operation. On postoperative day 3, passive exercise within pain tolerance limits was performed. After 3 weeks, active functional exercise was performed. When a callus formed at the fracture end, the range of motion was gradually increased. Finally, intensive resistance training was carried out. After 2 months, active range-of-motion and shoulder extension exercises were performed. After 3 months, the imaging examination showed that the degree of fracture healing allowed participation in sports activities. X-ray films of the shoulder joint were obtained and reviewed regularly in the outpatient clinic to continue observing the fracture healing and guide the patients in performing functional exercises.
Observation and evaluation indexes
All operations in this study were performed by the same doctor. The operation time, intraoperative bleeding volume, and incision length were collected. Before the operation, the sterile gauze was weighed. After the operation, the blood-soaked gauze was weighed again. The difference between the weight of the sterile gauze and blood-soaked gauze was used to calculate the intraoperative bleeding volume. All patients were followed up at 2 weeks, 4 weeks, 8 weeks, 10 weeks, 3 months, 6 months, and 12 months after the operation. X-ray imagery of the shoulder joint was taken. Complications and fracture healing were assessed based on the follow-up and X-ray findings. The incidence of postoperative complications was statistically analyzed at 12 months after the operation. Fracture healing was indicated by no obvious tenderness, disappearance of the fracture line, and callus formation. Pain perception and shoulder function were evaluated by the visual analog scale score, Constant–Murley score, and University of California Los Angeles (UCLA) score at 3 and 6 months after the operation.5
Statistical analysis
SPSS 17.0 statistical analysis software (SPSS Inc., Chicago, IL, USA) was used for the data analysis. Measurement data are expressed as mean ± standard deviation. An independent-samples t test was used for normally distributed data, a rank sum test was used for non-normally distributed data, and an χ2 test was used for comparisons of count data. A P value of <0.05 indicated statistical significance.
Ethics statements
The study protocol was approved by the ethics committee of the Second Affiliated Hospital of Guilin Medical University. All patients participating in the study provided verbal informed consent.
Results
Patient characteristics
Sixty-four patients with Neer type II distal clavicle fractures were included in the study. The LP group comprised 31 patients (19 male and 12 female patients) ranging in age from 17 to 55 years (mean age, 38.77 ± 8.55 years). The fracture was present on the left side in 17 patients and on the right side in 14 patients. The causes of injury were falls in 21 patients, traffic accidents in nine, and other in one. The HP group comprised 33 patients (21 male and 12 female patients) ranging in age from 18 to 58 years (mean age, 37.03 ± 10.01 years). The fracture was present on the left side in 19 patients and on the right side in 14 patients. The causes of injury were falls in 23 patients, traffic accidents in eight, and other in two. There were no significant differences in the general data between the two groups (Table 1).
Table 1.
Comparison of general data between the LP and HP groups.
|
Sex |
Side |
Causes of injury |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Group | M | F | Age, years | L | R | Fall | Accident | Other | |
| LP | 19 | 12 | 38.77 ± 8.55 | 17 | 14 | 21 | 9 | 1 | |
| HP | 21 | 12 | 37.03 ± 10.01 | 19 | 14 | 23 | 8 | 2 | |
| P | 1.000 | 0.458 | 1.000 | 1.000 | |||||
Data are presented as n or mean ± standard deviation.
LP, locking plate; HP, hook plate; M, male; F, female; L, left; R, right.
Perioperative conditions
In all patients, the operation was completed smoothly with no complications. The mean length of the distal bone block was 33.21 ± 4.15 mm in the LP group and 31.17 ± 3.97 mm in the HP group, with no significant difference between the two groups. The mean operative time was 63.16 ± 5.97 minutes in the LP group and 62.33 ± 7.85 minutes in the HP group, with no significant difference between the two groups. The mean intraoperative bleeding volume was 79.68 ± 7.67 mL in the LP group and 82.97 ± 7.15 mL in the HP group, with no significant difference between the two groups. The mean operative incision length was 6.63 ± 0.32 cm in the LP group, which was significantly shorter than that in the HP group (7.28 ±0.45 cm, P < 0.05) (Table 2). All patients were discharged from the hospital 3 to 5 days after the operation, and no wound healing complications occurred.
Table 2.
Comparison of operative indexes between the LP and HP groups.
| Group | Length of distal bone block, mm | Operation time, minutes | Bleeding volume, mL | Length of incision, cm | Healing time, weeks |
|---|---|---|---|---|---|
| LP | 33.21 ± 4.15 | 63.16 ± 5.97 | 79.68 ± 7.67 | 6.63 ± 0.32 | 9.87 ± 1.06 |
| HP | 31.17 ± 3.97 | 62.33 ± 7.85 | 82.97 ± 7.15 | 7.28 ± 0.45 | 9.76 ± 1.48 |
| P | 0.261 | 0.638 | 0.081 | <0.001* | 0.727 |
Data are presented as n or mean ± standard deviation.
*P < 0.05 in comparison of LP group and HP group.
LP, locking plate; HP, hook plate.
Postoperative follow-up
The follow-up period was at least 12 months, and all patients completed the follow-up successfully without loss to follow-up. All fractures healed well; the healing time in the LP and HP groups was 9.87 ± 1.06 and 9.76 ± 1.48 weeks, respectively, with no significant difference between the two groups (Table 2).
The mean visual analog scale score, Constant–Murley score, and UCLA score in the LP group were 1.90 ± 0.49, 82.13 ± 5.21, and 28.26 ± 3.67, respectively, at 3 months postoperatively. All of these scores were significantly better than those in the HP group (2.53 ± 0.99, 72.58 ± 4.14, and 25.67 ± 4.14, respectively; P < 0.05) (Table 3). However, there were no significant differences in any scores between the two groups at 6 months postoperatively (Table 3). At the last follow-up (12 months postoperatively), two patients in the LP group had shoulder joint pain, and the main manifestation was pain during shoulder abduction without obvious limitation of movement. In the HP group, three patients had subacromial osteolysis and nine had shoulder joint pain, and the main manifestation was pain during shoulder abduction with mild limitation of shoulder movement. The incidence of complications was significantly lower in the LP than HP group (P < 0.05) (Table 4).
Table 3.
Postoperative pain and shoulder function scores in the LP and HP groups.
| Group |
3 months postoperatively |
6 months postoperatively |
||||
|---|---|---|---|---|---|---|
| VAS score | Constant–Murley score | UCLA score | VAS score | Constant–Murley score | UCLA score | |
| LP | 1.90 ± 0.49 | 82.13 ± 5.21 | 28.26 ± 3.67 | 1.15 ± 0.39 | 90.00 ± 4.16 | 31.77 ± 2.09 |
| HP | 2.53 ± 0.99 | 72.58 ± 4.14 | 25.67 ± 4.14 | 1.18 ± 0.32 | 88.91 ± 5.24 | 30.88 ± 3.36 |
| P | 0.002* | <0.001* | 0.010* | 0.734 | 0.362 | 0.209 |
Data are presented as mean ± standard deviation.
*P < 0.05 in comparison of LP group and HP group.
LP, locking plate; HP, hook plate; VAS, visual analog scale; UCLA, University of California Los Angeles.
Table 4.
Comparison of postoperative complications between the LP and HP groups.
| Group | Postoperative complication | Fracture nonunion | Plate loosening | Osteolysis | Shoulder joint pain |
|---|---|---|---|---|---|
| LP | 2 (6.45) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 2 (6.45) |
| HP | 12 (36.36) | 0 (0.00) | 0 (0.00) | 3 (9.09) | 9 (27.27) |
| P | 0.006* | – | – | 0.239 | 0.045* |
Data are presented as n (%).
*P < 0.05 in comparison of LP group and HP group.
LP, locking plate; HP, hook plate.
Discussion
Neer type II distal clavicle fractures are often accompanied by obvious fracture displacement, a high rate of fracture nonunion, a poor response to conservative treatment, and the need for additional surgical internal fixation. The purpose of surgical internal fixation is to stabilize the fracture and promote healing and early functional exercise of the shoulder joint. Although various surgical methods are available, each has its own advantages and disadvantages. Therefore, the choice of the optimal internal fixation method remains controversial.6
A clavicle HP is a commonly used internal fixation method for distal clavicle fractures.5 The principle of treatment with an HP is insertion of the distal tip hook of the steel plate into the subacromial space and fixation of the proximal end with multiple screws. With the help of the pressure under the steel plate, the fracture can be reduced with maintenance of stability. However, because of the design characteristics of the clavicle HP, acromial morphology, and placement of the hook end of the clavicle HP under the acromion, complications such as subacromial impact and friction, rotator cuff injury, and shoulder pain are prone to occur during the use of clavicle HPs.7,8 The incidence of complications after clavicle HP surgery can reportedly reach 50%,9 which influences patients’ treatment experience and quality of life. In the present study, three patients had subacromial osteolysis and nine patients had shoulder pain at 1 year after treatment with a clavicle HP, and the incidence of postoperative complications was significantly higher in the clavicle HP group than in the LP group (36.36% vs. 6.45%, respectively; P < 0.05). There is a consensus that the clavicle HP should be removed as soon as possible after fracture healing.10 We usually suggest that the clavicle HP should be removed 10 to 12 months after the operation. In this study, among the 33 patients treated with a clavicle HP, 26 patients underwent removal of the clavicle HP 1 year later; the remaining seven patients refused removal of the clavicle HP. Of the 26 patients who underwent removal of the clavicle HP, 12 had postoperative complications that were relieved after removal. No postoperative complications occurred in the seven patients who did not undergo removal of the clavicle HP.
With the continuous development of internal fracture fixation materials, distal clavicle LPs are being increasingly used for distal clavicle fractures. In a Neer type II distal clavicle fracture, the fragments are very small, and it is difficult to achieve solid internal fixation with an ordinary clavicle LP. The small lateral screw of the distal clavicle LP can be locked freely in many directions, which ensures the holding force of the screw. The distal clavicle LP is neither exposed to the acromioclavicular joint nor interferes with the subacromial structure.11 In this study, the incision length in the LP group was significantly shorter than that in the clavicle HP group (P < 0.05), and the short-term pain and shoulder joint function scores in the LP group were significantly better than those in the clavicle HP group (P < 0.05). As time passed during follow-up, although the number of complications did not decrease in the clavicle HP group, the degree of shoulder joint pain with limited activity significantly decreased. We speculate that this was related to the patients’ performance of functional exercises and their gradual adaptation to the implants. Among the 31 patients treated with an LP, 10 patients underwent removal of the clavicle LP 1 year later. Of the 10 patients who underwent removal of the clavicle LP, two developed postoperative shoulder pain without significant shoulder joint mobility limitation, and this pain was relieved after removal of the LP. No postoperative complications occurred in the patients who did not undergo removal of the LP. Therefore, the use of a distal clavicle LP can provide patients with a better treatment experience.
In the treatment of a distal clavicle fracture with a distal clavicle LP, it is necessary to consider whether enough locking screws can be inserted into the distal clavicle fragment length to obtain sufficient stability. In this study, the length of the distal clavicle bone block was measured by preoperative three-dimensional computed tomography. We found that when the length of the distal clavicle bone block was >20 mm, an LP could be used. No loosening of the internal fixation occurred after the operation. Therefore, we recommend that a >20-mm-long distal clavicle fragment should be used as a reference index for the application of LPs. We choose the length of the plate to be used according to the following principles. When an LP is used, at least four screws should be placed in the distal fracture block and three screws in the proximal fracture block. When a clavicle HP is used, at least three screws should be placed in the proximal fracture block; if the distal fracture block is stable enough after fracture reduction, there is no need to insert any screws in the distal fracture block, otherwise, two to three screws should be inserted. In meeting the above conditions, we choose a shorter plate whenever possible to reduce the length of the surgical incision, which is conducive to postoperative rehabilitation.
This study had two main limitations. First, the sample size was small, and more samples are needed to support our conclusions. Second, the follow-up duration was short, especially for patients who did not undergo removal of the clavicle HP. A longer follow-up time is needed to increase our understanding of how leaving the clavicle HP in place affects shoulder function in the long term.
In summary, both LPs and clavicle HPs can provide satisfactory clinical results in the treatment of Neer type II distal clavicle fractures. There were no significant differences in the operative time, intraoperative bleeding volume, or long-term follow-up between the two plate groups. However, the LP group was superior to the clavicle HP group in terms of the incision length, incidence of complications, short-term pain, and shoulder joint function scores. Therefore, LPs should be given priority in the treatment of Neer type II distal clavicle fractures.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This study was supported by the National Natural Science Fund (No. 81960172) and the Guangxi Provincial Health Office with a self-raised fund (No. Z2013470).
ORCID iD
Hong-Kai Wang https://orcid.org/0000-0001-6225-7985
References
- 1.Neer CS., 2nd. Fractures of the distal third of the clavicle. Clin Orthop Relat Res 1968; 58: 43–50. [PubMed] [Google Scholar]
- 2.Postacchini F, Gumina S, De Santis P, et al. Epidemiology of clavicle fractures. J Shoulder Elbow Surg 2002; 11: 452–456. [DOI] [PubMed] [Google Scholar]
- 3.Robinson CM, Cairns DA. Primary nonoperative treatment of displaced lateral fractures of the clavicle. J Bone Joint Surg Am 2004; 86-A: 778–782. [DOI] [PubMed] [Google Scholar]
- 4.Xiong J, Chen JH, Dang Y, et al. Treatment of unstable distal clavicle fractures (Neer type II): a comparison of three internal fixation methods. J Int Med Res 2018; 46: 4678–4683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee W, Choi CH, Choi YR, et al. Clavicle hook plate fixation for distal-third clavicle fracture (Neer type II): comparison of clinical and radiologic outcomes between Neer types IIA and IIB. J Shoulder Elbow Surg 2017; 26: 1210–1215. [DOI] [PubMed] [Google Scholar]
- 6.Sandstrom CK, Gross JA, Kennedy SA. Distal clavicle fracture radiography and treatment: a pictorial essay. Emerg Radiol 2018; 25: 311–319. [DOI] [PubMed] [Google Scholar]
- 7.Zhang C, Huang J, Luo Y, et al. Comparison of the efficacy of a distal clavicular locking plate versus a clavicular hook plate in the treatment of unstable distal clavicle fractures and a systematic literature review. Int Orthop 2014; 38: 1461–1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lopiz Y, Checa P, Garcia-Fernandez C, et al. Complications with the clavicle hook plate after fixation of Neer type II clavicle fractures. Int Orthop 2019; 43: 1701–1708. [DOI] [PubMed] [Google Scholar]
- 9.Lin HY, Wong PK, Ho WP, et al. Clavicular hook plate may induce subacromial shoulder impingement and rotator cuff lesion–dynamic sonographic evaluation. J Orthop Surg Res 2014; 9: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sukur E, Ozturkmen Y, Akman YE, et al. Clinical and radiological results on the fixation of Neer type 2 distal clavicle fractures with a hook plate. Acta Orthop Traumatol Turc 2016; 50: 489–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schliemann B, Rosslenbroich SB, Schneider KN, et al. Surgical treatment of vertically unstable lateral clavicle fractures (Neer 2b) with locked plate fixation and coracoclavicular ligament reconstruction. Arch Orthop Trauma Surg 2013; 133: 935–939. [DOI] [PubMed] [Google Scholar]