Abstract
As of April 7, 2020, approximately 1,300,000 cases and 80,000 deaths related to coronavirus disease 2019 (COVID-19) have been reported in more than 180 countries/territories. Health care infrastructures and resources, particularly as it relates to the care of the most critically ill patients, are currently being strained globally. In this context, however, there has been little clinical guidance or information regarding life-threatening conditions requiring emergency operation that cannot be delayed. We present a case of acute type A aortic dissection in a patient with COVID-19 to highlight the clinical implications of a true emergent procedure during the COVID-19 outbreak.
As of April 7, 2020, approximately 1,300,000 cases and 80,000 deaths related to coronavirus disease 2019 (COVID-19) have been reported in more than 180 countries/territories.1 Health care infrastructures and resources, particularly as they relate to the care of the most critically ill patients, are currently being strained globally. In this context, in the United States, the American College of Surgeons and the Centers for Medicare and Medicaid Services released recommendations for the management of elective surgical procedures,2 , 3 suggesting delaying all elective procedures without high acuity to focus on more urgent cases, preserve valuable resources, and prevent the spread of COVID-19 among health care providers, patient families, and the public.
In contrast, maintaining emergency operation capabilities is critical for patients who require life-saving operations that cannot be delayed. We present our first case of acute type A aortic dissection in a patient with COVID-19, which was confirmed on postoperative day 6. This report illustrates clinical implications of an emergent procedure during the COVID-19 outbreak.
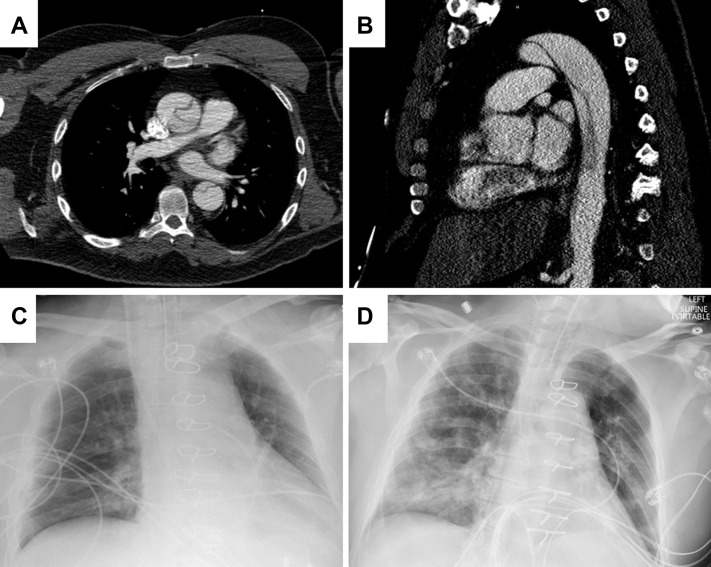
On March 14, 2020, a previously healthy nonsmoking 52-year-old man presented to another facility with severe chest and abdominal pain. He denied fever or shortness of breath. The computed tomographic angiography showed an acute type A (DeBakey type I) aortic dissection with a primary intimal tear at the level of the sinotubular junction, markedly compressed true lumen in the descending thoracoabdominal aorta, a dissection flap extending down into the superior mesenteric and bilateral renal arteries, and poor contrast enhancement of the right kidney (Figure 1A, 1B).
Figure 1.
Relevant imaging studies during the patient’s hospital course. (A) A representative axial image of the preoperative computed tomographic angiography demonstrates type A aortic dissection. (B) A representative sagittal image of the preoperative computed tomographic scan demonstrates a markedly compressed true lumen involving the visceral segment of the thoracoabdominal aorta. Chest roentgenograms (C) immediately after the operation and (D) immediately after reintubation.
He was emergently transferred to the University of Michigan for further management. On arrival, the patient had a low-grade fever (37.6°C) without cough, dyspnea, or recent travel. He did not meet any of our institutional criteria for COVID-19 testing at that time, which included fever higher than 38°C, cough, or dyspnea, or both, without a clear alternative cause, risk factors (such as immunocompromised state or age >70 years) for developing a severe form of disease if infected, recent domestic or international travel, employment as a health care worker, or contact with a known COVID-19 patient, and therefore he was not tested. There were a total of 33 COVID-19 cases in Michigan and no case in our county (Washtenaw County) at that time.4
Ascending and hemiarch aortic repair under moderate hypothermic circulatory arrest with retrograde cerebral perfusion was immediately performed. The procedure was uneventful, with cardiopulmonary bypass, aortic cross-clamp, and circulatory arrest times of 107, 52, and 8 minutes, respectively.
Despite the uneventful intraoperative course, he could not be extubated on postoperative day 1 due to persistent hypoxia with high oxygen (fraction of inspired oxygen of 60%) and positive end-expiratory pressure (10 cm H2O) requirements. The chest roentgenogram was unremarkable (Figure 1C). He was diuresed due to higher-than-usual oxygen demands. He was eventually extubated on postoperative day 2.
The patient began ambulating with assistance. Meanwhile, he continued to be diuresed; however, his hypoxemia gradually exacerbated. The chest roentgenogram on postoperative day 5 demonstrated bilateral patchy pulmonary infiltrates, and on that same day, he needed reintubation (Figure 1D). The results of a respiratory virus panel were negative. A real-time reverse-transcriptase polymerase chain reaction test for COVID-19 was performed and was positive.
Several caregivers involved in his care were immediately quarantined afterward, although they were all asymptomatic. His respiratory status rapidly worsened over the ensuing 48 hours (with partial pressure of oxygen of 73 mm Hg, despite 100% fraction of inspired oxygen), and inhaled nitric oxide was initiated. Despite maximum medical therapy, the patient died on postoperative day 11 of multiorgan failure essentially resulting from progressive respiratory failure and acute renal failure.
Comment
We present an acute type A aortic dissection case complicated by acute respiratory distress syndrome in a patient initially not suspected for but later diagnosed with COVID-19. This case clearly illustrated several aspects of emergent cardiac operation during the current COVID-19 outbreak. While perioperative acute respiratory distress syndrome for emergent repair for type A aortic dissection is not exceedingly rare, rapidly progressive respiratory failure on postoperative day 4 and 5 in nonsmoking and otherwise healthy ambulating patients after an uneventful operation is not usual, raising COVID-19 in the differential diagnosis.
Although at what time point our patient acquired COVID-19 is still unclear, we suspect it was preoperatively, given the time course of his clinical deterioration. We thoroughly elicited his medical history and review of systems, but he was not even considered suspicious for COVID-19 at presentation. Despite practicing at a major academic center, we are very limited by the number of available real-time polymerase chain reaction tests and the relatively long processing time.
There are clearly patients with mild symptoms or even asymptomatic patients who are infected with COVID-195 that will not be detected by the current screening process. The currently outlined risk factors for acquisition of the disease are likely no longer relevant, because more than 400,000 cases have occurred in the United States, with that number rapidly rising daily.1
To protect patients, health care providers, and the public, we advocate for more liberal testing for patients who are undergoing major emergent operations. Such patients can then be placed in the appropriate isolation precautions, providers can wear the appropriate personal protective equipment, and procedure rooms can be adequately sterilized postoperatively. In this context, operating surgeons have to be mindful with respect to the COVID-19 test processing time, which significantly varies among institutions, ranging from 2 to 3 hours to days, and the possibility of false-negative results.
This humbling experience and the ongoing spread of COVID-19 highlight how inadequate our preparation was for this pandemic, despite having witnessed the preceding situations in China, South Korea, Iran, Japan, and Europe. In light of the very high mortality associated with nonoperative management of type A aortic dissection and with the lack of existing data regarding concurrent aortic dissection and COVID-19 infection, it remains inconclusive to suggest that cases like the present report be delayed for these dual diagnoses.
However, nonoperative management may be justified in patients with COVID-19 with type A aortic dissection with severe multiple medical comorbidities, advanced age, severe malperfusion syndrome, and daily heavy smoking, because the mortality rate of these patients can be close to 100%. Alternatively, endovascular repair may be considered if anatomically suitable, because the pulmonary burden from cardiopulmonary bypass use and associated induced inflammatory cascade can be avoided. This fact implies the importance of cancelling all nonessential procedures with the goal to preserve and redirect life-saving health care resources. Given the rare incidence of aortic dissections, testing such patients for COVID-19 on presentation would likely not place an excessive burden on the currently limited testing resources. Even more broadly, we may have to assume all patients needing an emergent operation may have been exposed to COVID-19.
References
- 1.World Health Organization Coronavirus Disease 2019 (COVID-19) Situation Report–78. April 7, 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200407-sitrep-78-covid-19.pdf?sfvrsn=bc43e1b_2 Available at:
- 2.American College of Surgeons COVID-19: Recommendations for Management of Elective Surgical Procedures. March 13, 2020. https://www.facs.org/about-acs/covid-19/information-for-surgeons/elective-surgery Available at:
- 3.Centers for Medicare & Medicaid Services Non-Emergent, Elective Medical Services, and Treatment Recommendations. https://www.cms.gov/files/document/31820-cms-adult-elective-surgery-and-procedures-recommendations.pdf Available at:
- 4.Michigan.gov Coronavirus. https://www.michigan.gov/coronavirus/0,9753,7-406-98163-520743--,00.html Available at:
- 5.Bai Y., Yao L., Wei T. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323:1406–1407. doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]